0% found this document useful (0 votes)
61 views4 pagesFluid Volume Deficit in Older Adults
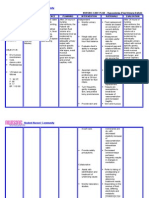
1. The patient presented with signs and symptoms of fluid volume deficit including weakness, fever, inability to drink liquids due to nausea and vomiting, low blood pressure, dry mucous membranes, reduced urine output, and elevated hematocrit.
2. The plan was for the patient to receive 5 liters of fluid replacement over 30 minutes. Monitoring included urine and blood analysis and vital signs. Outcomes would be evaluated based on normalization of vital signs and adequate urine output.
3. After treatment, the patient's blood pressure, pulse, respirations, and urine output improved, indicating resolution of the fluid volume deficit. Further monitoring and encouraging oral fluid intake was recommended to fully restore fluid balance.
Uploaded by
jessa alcazarCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
61 views4 pagesFluid Volume Deficit in Older Adults
1. The patient presented with signs and symptoms of fluid volume deficit including weakness, fever, inability to drink liquids due to nausea and vomiting, low blood pressure, dry mucous membranes, reduced urine output, and elevated hematocrit.
2. The plan was for the patient to receive 5 liters of fluid replacement over 30 minutes. Monitoring included urine and blood analysis and vital signs. Outcomes would be evaluated based on normalization of vital signs and adequate urine output.
3. After treatment, the patient's blood pressure, pulse, respirations, and urine output improved, indicating resolution of the fluid volume deficit. Further monitoring and encouraging oral fluid intake was recommended to fully restore fluid balance.
Uploaded by
jessa alcazarCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd