Professional Documents
Culture Documents
Define The Mechanisms of Action and Adverse Effects of Metoprolol, GTN, and Diltiazem When Used To Manage MI
Uploaded by
DonkeyManOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Define The Mechanisms of Action and Adverse Effects of Metoprolol, GTN, and Diltiazem When Used To Manage MI
Uploaded by
DonkeyManCopyright:
Available Formats
Metoprolol
o Selective B1 blocker (but B2 effects at higher doses), no intrinsic sympathomimetic activity, has
membrane stabilising effects (but not at clinical doses)
o B adrenoreceptors are Gs, thus B blockers decrease AC, cAMP, decreases protein kinase activity,
decreases IC [Ca], causing decreased inotropy/chronotropy/dromotropy
o Used in MI because it
reduces myocardial oxygen demand by decreasing HR, inotropy, dromotropy
increases oxygen supply by increasing diastolic time
prevents LV remodelling a/w MI
o adverse side effects
CVS – hypotension (blunts BRR, decreases CO, decreases renin release), bradycardia, heart
block, asystole, blunts sympathetic response to hypoglycaemia
Resp – can cause bronchoconstriction at high doses
CNS – has high lipid solubility, thus can cause depression, fatigue, confusion
Other – can get rebound tachycardia and HTN if suddenly ceased, decreases effectiveness of
inotropes/vassopressors, additive –ve inotropy with ketamine/volatiles/IV anaesthetic
agents
GTN
o Organic nitrate, relies on nitrate reductase in liver and vascular smooth muscle to release NO. NO
acts on VSM to increase GC, increase cGMP, increase activity of protein kinases, decrease IC [Ca]
causing venodilation > vasodilation
o Used in MI because it venodilates, decreases VR, decreases CO and LV wall tension, thus
decreasing myocardial oxygen demand. Also vasodilates large coronary arteries to increase supply,
without coronary steal
In high doses will also vasodilate, decrease SVR/MAP, trigger BRR with increased HR and
inotropy, thus can decrease CBF (due to decreased diastolic time and decreased diastolic
pressure), and increase myocardial O2 demand
o Adverse effects
CVS – hypotension, at high doses can decrease coronary BF
Resp – impairs HPV, worsens VQ mismatch, hypoxia
CNS – headache, NV, flushing, increased ICP/CBF
Haem – decreased platelet aggregation
Other – rarely MetHb, tolerance after 24 hours, contraindicated in HOCM/AS/hypovolaemia
Diltiazem
o L type calcium channel blocker, with equal effects on heart and periphery
o Binds to cytoplasmic site of Ca channel when it is open, keeps it in inactive/closed state, decreases
Ca influx, decreases IC [Ca], thus decreases inotropy, SAN automaticity, and AVN conduction/HR
(decreases myocardial oxygen demand), and causes vasodilation (decreases afterload). Note: less
venodilation
o Adverse effects
CVS – hypotension, bradycardia, heart block, asystole, LVF failure
Resp – impairs HPV, worsens VQ mismatch
CNS – increased CBF/ICP, NV, headache, prolongs NDNMBs
Other – decreases inotropy with other anaesthetic agents
You might also like
- Pharmacology SummaryDocument16 pagesPharmacology Summaryshenric16No ratings yet
- Systolic Dysfunction:: Types of Heart FailureDocument13 pagesSystolic Dysfunction:: Types of Heart FailureElisabeth F. OjhaNo ratings yet
- L7 Heart Failure Practice EssayDocument2 pagesL7 Heart Failure Practice EssaymoshlingmomoNo ratings yet
- Cvs DrugsDocument106 pagesCvs DrugsIkoona ivanNo ratings yet
- Cardiac Care and COVID-19: Perspectives in Medical PracticeFrom EverandCardiac Care and COVID-19: Perspectives in Medical PracticeNo ratings yet
- Heart Failure: Low Output HF High Output HFDocument7 pagesHeart Failure: Low Output HF High Output HFJake BurrNo ratings yet
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtFrom EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtRating: 5 out of 5 stars5/5 (1)
- CVPR Prototype Drugs TableDocument27 pagesCVPR Prototype Drugs TablethommyvaNo ratings yet
- 4 - Anti-AnginaDocument6 pages4 - Anti-AnginaJericho De GuzmanNo ratings yet
- Pharm Guide Quiz 1 Parasyp and Symp Nervous SystemDocument5 pagesPharm Guide Quiz 1 Parasyp and Symp Nervous SystemMaryNguyenNo ratings yet
- Mechanism of Action: Cerebral VasospasmDocument1 pageMechanism of Action: Cerebral VasospasmArjay Oamil GuerreroNo ratings yet
- CarvedilolDocument4 pagesCarvedilolGoNo ratings yet
- CombinepdfDocument27 pagesCombinepdfMICHAEL ANGELO CUBIONo ratings yet
- Cardio Lab MedsDocument11 pagesCardio Lab MedsDianne Erika MeguinesNo ratings yet
- Heart Failure: Mohammad DiahDocument50 pagesHeart Failure: Mohammad DiahAdityaNo ratings yet
- Cardiotonics - DR Anoosha BhandarkarDocument60 pagesCardiotonics - DR Anoosha BhandarkaranooshabhandarkarNo ratings yet
- HypertensionDocument43 pagesHypertensionAbin PNo ratings yet
- CVS & Hypolipidemic Drugs-NursingDocument71 pagesCVS & Hypolipidemic Drugs-NursingManikanta Guptha100% (1)
- Cardiac ReflexesDocument2 pagesCardiac ReflexesfeliciaNo ratings yet
- 6 Beta Adrenergic BlockersDocument19 pages6 Beta Adrenergic Blockersmatchees-gone rogue100% (1)
- Pharm 00 B14Document2 pagesPharm 00 B14DonkeyManNo ratings yet
- Department of Clinical Pharmacology: Pharmacotherapy of Chronic Ischemic Heart DiseaseDocument84 pagesDepartment of Clinical Pharmacology: Pharmacotherapy of Chronic Ischemic Heart DiseasePatty ReyesNo ratings yet
- Congestive Heart FailureDocument30 pagesCongestive Heart FailurePh OmarNo ratings yet
- Anti Anginal Drugs - Wards HandooutDocument24 pagesAnti Anginal Drugs - Wards HandooutDharun RanganathanNo ratings yet
- Drugs Used in HF IIDocument40 pagesDrugs Used in HF IIJamal LudinNo ratings yet
- PharmaAntianginal DrugsDocument175 pagesPharmaAntianginal DrugsNidal AbboudNo ratings yet
- 11A Drugs Acting On The Cardiovascular SystemDocument85 pages11A Drugs Acting On The Cardiovascular SystemJaps De la CruzNo ratings yet
- Pharmacologyofccf 181227034555Document43 pagesPharmacologyofccf 181227034555MohammedMujahedNo ratings yet
- Heart Failure: Kalaiselvan OtDocument46 pagesHeart Failure: Kalaiselvan Otplayme_nowNo ratings yet
- Beta-Adrenergic BlockersDocument14 pagesBeta-Adrenergic BlockersAnonymous NVAWeVWNo ratings yet
- Cardiology Review: HTN: Julia Akaah M.DDocument40 pagesCardiology Review: HTN: Julia Akaah M.DJose LunaNo ratings yet
- Vasodilators and The Treatment of Angina PectorisDocument39 pagesVasodilators and The Treatment of Angina PectorisRose AnnNo ratings yet
- Meds #1 NotesDocument4 pagesMeds #1 NotesAnh TrinhNo ratings yet
- Controlled Hypotension: Moderator: DR V. Y. Srinivas Presenter: Dr. Ann Susan MathewDocument49 pagesControlled Hypotension: Moderator: DR V. Y. Srinivas Presenter: Dr. Ann Susan MathewAnn Susan MathewNo ratings yet
- Calcium Channel BlockersDocument4 pagesCalcium Channel BlockersHarold LinNo ratings yet
- Drugs For Heart Failure & Angina: Department of Pharmacology Liming Zhou 2010,3Document47 pagesDrugs For Heart Failure & Angina: Department of Pharmacology Liming Zhou 2010,3DR Muhammad Abdul BasitNo ratings yet
- شDocument16 pagesشhqzcgdh6gvNo ratings yet
- Heart Failure: S. Soliman MDDocument46 pagesHeart Failure: S. Soliman MDRamli HusenNo ratings yet
- Heart Failure New SlidesDocument41 pagesHeart Failure New SlidesjawadNo ratings yet
- Heart FailureDocument9 pagesHeart Failuregmqkxq6wshNo ratings yet
- Beta Blockers BPTHDocument45 pagesBeta Blockers BPTHjyb5kcxbgtNo ratings yet
- Heart Failure: DR - Liu LixinDocument46 pagesHeart Failure: DR - Liu LixinsanjivdasNo ratings yet
- Antihypertensive DrugsDocument7 pagesAntihypertensive Drugshamadadodo7No ratings yet
- Cardio CHF Angina Drugs MegDocument3 pagesCardio CHF Angina Drugs MegJhonny pingolNo ratings yet
- Lecture #12Document3 pagesLecture #12yeeticusfinchlmaoNo ratings yet
- 4.heart Failure HandoutDocument108 pages4.heart Failure HandoutGetachewNo ratings yet
- Pharmacotherapy of Hypertention TerbaruDocument45 pagesPharmacotherapy of Hypertention TerbarulisaNo ratings yet
- Calcium Channel BlockersDocument28 pagesCalcium Channel Blockershap hazardNo ratings yet
- USMLE Step 1 NotesDocument5 pagesUSMLE Step 1 NotesMarie SantoroNo ratings yet
- Inotropic Agents - Blockers Renin InhibitorsDocument19 pagesInotropic Agents - Blockers Renin InhibitorsTanyir MarieClaireNo ratings yet
- Inotropic Agents - Blockers Renin InhibitorsDocument19 pagesInotropic Agents - Blockers Renin InhibitorslitaNo ratings yet
- Pharmacology RCR1 RenalDocument6 pagesPharmacology RCR1 RenaleamcrawleyNo ratings yet
- SyncopeDocument44 pagesSyncopeSap ModulesNo ratings yet
- Anti-Arrhythmic Agents For Pharmacy PDFDocument41 pagesAnti-Arrhythmic Agents For Pharmacy PDFKelvinTMaikanaNo ratings yet
- 5 Hypertension Handout PDFDocument20 pages5 Hypertension Handout PDFMd Sakil AminNo ratings yet
- Cardio, Otis, Ortho, and GI Drug ListsDocument4 pagesCardio, Otis, Ortho, and GI Drug ListsJodi Gugel DeMarrowNo ratings yet
- CEACCP - Intrathecal Opioids in The Management of Acute Postoperative PainDocument5 pagesCEACCP - Intrathecal Opioids in The Management of Acute Postoperative PainDonkeyManNo ratings yet
- Pharm 02 A10Document2 pagesPharm 02 A10DonkeyManNo ratings yet
- CEACCP - Latex AllergyDocument4 pagesCEACCP - Latex AllergyDonkeyManNo ratings yet
- Physiol 93 B3Document1 pagePhysiol 93 B3DonkeyManNo ratings yet
- CEACCP - KetamineDocument5 pagesCEACCP - KetamineDonkeyManNo ratings yet
- CEACCP - Illegal Substances in Anaesthetic and Intensive Care PracticesDocument5 pagesCEACCP - Illegal Substances in Anaesthetic and Intensive Care PracticesDonkeyManNo ratings yet
- Pharm 00 B15Document2 pagesPharm 00 B15DonkeyManNo ratings yet
- Pharm 00 B14Document2 pagesPharm 00 B14DonkeyManNo ratings yet
- Pharm 02 A11Document4 pagesPharm 02 A11DonkeyManNo ratings yet
- Pharm 00 A15Document2 pagesPharm 00 A15DonkeyManNo ratings yet
- Pharm 00 A12Document1 pagePharm 00 A12DonkeyManNo ratings yet
- Compare and Contrast Neostigmine and The Organophosphate CompoundsDocument1 pageCompare and Contrast Neostigmine and The Organophosphate CompoundsDonkeyManNo ratings yet
- Pharm 00 A14Document2 pagesPharm 00 A14DonkeyManNo ratings yet
- Outline The Physiological Consequences of Hyperosmolar Diabetic KetoacidosisDocument2 pagesOutline The Physiological Consequences of Hyperosmolar Diabetic KetoacidosisDonkeyManNo ratings yet
- Compare and Contrast The Pharmacology of Esmolol and PropanololDocument1 pageCompare and Contrast The Pharmacology of Esmolol and PropanololDonkeyManNo ratings yet
- Pharm 00 B11Document1 pagePharm 00 B11DonkeyManNo ratings yet
- Pharm 00 A9Document2 pagesPharm 00 A9DonkeyManNo ratings yet
- Compare and Contrast Atropine and Glycopyrulate, and Discuss The Clinical ImplicationsDocument2 pagesCompare and Contrast Atropine and Glycopyrulate, and Discuss The Clinical ImplicationsDonkeyManNo ratings yet
- Compare and Contrast The Pharamcology of Ephedrine and NoradrenalineDocument1 pageCompare and Contrast The Pharamcology of Ephedrine and NoradrenalineDonkeyManNo ratings yet
- VOLATILEAGENTSDocument4 pagesVOLATILEAGENTSDonkeyManNo ratings yet
- FS Antimicrobial Dosing Obesity AMS Updates Issue4 - Nov2018Document4 pagesFS Antimicrobial Dosing Obesity AMS Updates Issue4 - Nov2018DonkeyManNo ratings yet
- Palliative Care HandbookDocument82 pagesPalliative Care HandbookDonkeyManNo ratings yet
- The Physiology of The GIT and The Liver QuestionsDocument44 pagesThe Physiology of The GIT and The Liver QuestionsDonkeyManNo ratings yet
- Comparative Pharmacokinetics of Fentanyl and Alfentanil: Br. J. Anaesth. (1982), 54, 871Document7 pagesComparative Pharmacokinetics of Fentanyl and Alfentanil: Br. J. Anaesth. (1982), 54, 871DonkeyManNo ratings yet
- Cholinergic Agents: Cholinergic Receptors Types of Receptor Muscarinic Receptor Nicotinic ReceptorDocument4 pagesCholinergic Agents: Cholinergic Receptors Types of Receptor Muscarinic Receptor Nicotinic ReceptorDonkeyManNo ratings yet
- Base Excess (Be) Measure of Metabolic Acid-Base Status: Dr. David LynessDocument1 pageBase Excess (Be) Measure of Metabolic Acid-Base Status: Dr. David LynessDonkeyManNo ratings yet
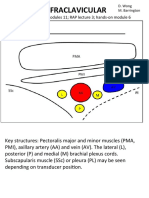
- Infraclavicular: Toolbox: Online Modules 11 RAP Lecture 3 Hands - On Module 6Document4 pagesInfraclavicular: Toolbox: Online Modules 11 RAP Lecture 3 Hands - On Module 6DonkeyManNo ratings yet
- HEARTDocument11 pagesHEART1NC21IS038 POLATHALA MOUNIKANo ratings yet
- The ESC Textbook of Sports CardiologyDocument478 pagesThe ESC Textbook of Sports CardiologyIBFiS100% (1)
- Case Study With ECG Reading OcañaDocument3 pagesCase Study With ECG Reading OcañaNicole Chloe OcanaNo ratings yet
- The Cardiovascular System: Elaine N. MariebDocument46 pagesThe Cardiovascular System: Elaine N. MariebIvann Chan MunarNo ratings yet
- Biventricular Pacing For Atrioventricular Block and Systolic DysfunctionDocument9 pagesBiventricular Pacing For Atrioventricular Block and Systolic DysfunctionRaul OrtegaNo ratings yet
- Nursing Care Plan AnswerDocument6 pagesNursing Care Plan Answercoosa liquorsNo ratings yet
- Experience With A Chest Pain CenterDocument8 pagesExperience With A Chest Pain CenterGabriel Cadavid GilNo ratings yet
- Clinical Application of The EchocardiogtamDocument39 pagesClinical Application of The EchocardiogtamStella CooKeyNo ratings yet
- Basic Life Support Program - Andhra Medical CollegeDocument6 pagesBasic Life Support Program - Andhra Medical CollegeRajasekhar BandiNo ratings yet
- ECG Physician's Guide (Japanese)Document49 pagesECG Physician's Guide (Japanese)Mohammad NasriNo ratings yet
- Congestive Heart FailureDocument25 pagesCongestive Heart FailuredevianiamalinaNo ratings yet
- Nuclear Cardiology: Role in The World of Multimodality Cardiac ImagingDocument5 pagesNuclear Cardiology: Role in The World of Multimodality Cardiac ImagingElena FlorentinaNo ratings yet
- NCLEX Based 1000 MCQs Part-2Document12 pagesNCLEX Based 1000 MCQs Part-2AkashNo ratings yet
- Angiografi Koroner: Indikasi, Kontraindikasi, Dan Proteksi Terhadap RadiasiDocument6 pagesAngiografi Koroner: Indikasi, Kontraindikasi, Dan Proteksi Terhadap Radiasihindri royiah fatmaNo ratings yet
- Pathologt of The HeartDocument40 pagesPathologt of The HeartJudithNo ratings yet
- Systolic MurmursDocument10 pagesSystolic MurmursRizqan Fahlevvi AkbarNo ratings yet
- Amiodarone Vs Sotalol GroupDocument12 pagesAmiodarone Vs Sotalol GroupIrving H Torres LopezNo ratings yet
- Coarctation of Aorta: Seoul National University Hospital Department of Thoracic & Cardiovascular SurgeryDocument39 pagesCoarctation of Aorta: Seoul National University Hospital Department of Thoracic & Cardiovascular Surgeryprencess_jeny5006No ratings yet
- Heart Disease and Stroke Statistics-2023 Update: A Report From The American Heart AssociationDocument529 pagesHeart Disease and Stroke Statistics-2023 Update: A Report From The American Heart Association涂育寬No ratings yet
- 4 - Congenital Heart DefectDocument42 pages4 - Congenital Heart DefectAlfiya HasnaNo ratings yet
- Anesthesiology: Linda S. Aglio Richard D. UrmanDocument457 pagesAnesthesiology: Linda S. Aglio Richard D. UrmanDaia DaiaNo ratings yet
- Heart Lung InteractionDocument39 pagesHeart Lung InteractionziadNo ratings yet
- Biology Investigatory Project: Congenital Heart DiseaseDocument16 pagesBiology Investigatory Project: Congenital Heart DiseaseDraco MalfoyNo ratings yet
- Cardiac Drug FunctionDocument2 pagesCardiac Drug FunctionShanda Rieder KozickiNo ratings yet
- Acute Inferior Myocardial InfarctionDocument1 pageAcute Inferior Myocardial InfarctionLogadarshini VeerasamyNo ratings yet
- Cardiac Cycle by Preetibala Sahu-1Document17 pagesCardiac Cycle by Preetibala Sahu-1aksahu01234No ratings yet
- Short Cases in Clinical Exams of Internal Medicine (PDFDrive)Document185 pagesShort Cases in Clinical Exams of Internal Medicine (PDFDrive)Nadhirah ZulkifliNo ratings yet
- Perimount Theon: Carpentier-Edwards Mitral Pericardial BioprosthesisDocument4 pagesPerimount Theon: Carpentier-Edwards Mitral Pericardial BioprosthesisJose Miguel GonzalezNo ratings yet
- Circulation: Ms. Jonalyn P. SantosDocument18 pagesCirculation: Ms. Jonalyn P. SantosHoward John M. RamiterreNo ratings yet
- NR 161:cardiology Study Guide Cardiology Study GuideDocument6 pagesNR 161:cardiology Study Guide Cardiology Study GuideApril Danielle TeschNo ratings yet