Professional Documents
Culture Documents
Pharm 00 A15
Uploaded by
DonkeyManOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharm 00 A15
Uploaded by
DonkeyManCopyright:
Available Formats
Pharm-00A15: Describe the effects of opioids on the respiratory system 75%
Opioids → exogenous substance (natural and synthetic) that has an affinity for opioid receptors
Mechanism of action:
- Opioid agonists act on opioid receptors (μ, κ, δ) which are located widespread in CNS
(supraspinal and spinal locations) → all are membrane-bound GPCR (Gi) → receptor
activation causes inhibition of adenylyl cyclase → ↓ IC [cAMP] → causes (i) opening of
VG-K+ channels and (ii) closure of VG-Ca2+ channels → ↓ neuronal activity
- μ and δ receptors are 1°ly responsible for respiratory effects
Effects of opioids on respiratory system:
Important to note → * Effects on respiratory system are dose-dependent
* Respiratory effects occur within therapeutic doses for analgesia →
this is b/c opioids have a narrow therapeutic index
* Tolerance to respiratory effects of opioids occurs
(1) Respiratory depression → due to direct inhibition of medullary ventilatory centres →
produces ↓ RR with compensatory ↑ TV, which leads to net ↓ MV (due to incomplete
compensatory ↑ MV) → causes apnoea (and death 2° to respiratory arrest) at excessive doses
Note: * Phenylpiperidine-derivatives (Eg. pethidine, fentanyl, remifentanil, Etc.) more potent
respiratory depressants cf. morphine or codeine
* Fentanyl and sufentanil → risk of persistent/recurrent respiratory depression 2° to
washout from pulmonary stores
* Tramadol and oxycodone have minimal respiratory depression
(2) ↓ ventilatory drive to ↑ PaCO2 and ↓ PaO2 → due to ↓ ACh from medullary neurons in
response to ↑ CO2 and/or ↓ O2 → causes ↑ resting PaCO2 (2° to right shift in MV vs PaCO2)
and ↓ resting PaO2
Note – CO2 chemoreceptor sensitivity is affected more cf. O2 → thus, supplementary O2
removes hypoxic stimulus to breathe → potentiates respiratory depression
(3) Anti-tussive effects → due to depression of medullary cough centre → prominent with codeine
(4) Chest and abdominal wall muscle rigidity (causing difficult PPV) → due to opioid receptor
interaction with DA and GABA pathways in substantia nigra and striatum → prominent with
phenylpiperidine-derivatives (Ie. remifentanil, fentanyl, alfentanil, Etc.) at high-doses
(5) Impaired upper airway reflexes → due to sedation and suppression of cough reflex →
permits instrumentation of airway BUT risk of aspiration and airway obstruction
(6) ↑ airway resistance → due to direct bronchial SM effect and histamine effect (2° to mast cell
degranulation), which causes bronchoconstriction (possess issue with asthma/COPD) →
prominent with morphine cf. phenylpiperidine-derivatives
(7) ↓ ciliary activity → mucous plugging
Effects on respiratory system vary with:
- (1) Type of opioid used (see above for examples) and doses used (↑ effects with ↑ doses)
- (2) Route of administration:
o Neuraxial opioids → Early respiratory depression (within 2 hr) occurs with lipid-
soluble opioids (Eg. fentanyl) due to systemic opioid absorption and subsequent
interaction with opioid receptors in medulla; delayed respiratory depression (> 2
hrs) occurs with less lipid-soluble opioids (Eg. morphine) due to cephalad
migration of opioid and subsequent interaction with opioid receptors in medulla
o IV/IM opioids have faster onset and ↑ pronounced respiratory effects vs PO opioids
- (3) Lack of opioid tolerance → ↑ respiratory effects
- (4) Age → advanced ages have ↑ sensitivity to these effects due to immature BBB or ↑
opioid sensitivity
- (5) Co-morbidities (esp underlying respiratory disease, obesity, sleep apnoea,
encephalopathy, Etc.) → ↑ respiratory effects
- (6) Level of CNS stimulation → sleep, lack of pain, delirium, Etc. → ↑ respiratory effects
- (7) Concurrent use of drugs that cause sedation/respiratory depression (Eg. other
opioids, benzodiazepines, EtOH, volatile agents, IV induction agents, Etc.) → interact
additively or synergistically to cause respiratory effects
You might also like
- OpiodsDocument15 pagesOpiodssash34No ratings yet
- CC Final Study Guide 1Document21 pagesCC Final Study Guide 1api-402814755No ratings yet
- InhalationalDocument87 pagesInhalationalsourabh jakharNo ratings yet
- L P 5 Analgesics Final - 22Document32 pagesL P 5 Analgesics Final - 22Zakria Al-HadadNo ratings yet
- Inhalational LectureDocument71 pagesInhalational LectureGosa MohammedNo ratings yet
- 25) Regulation of RespirationDocument61 pages25) Regulation of Respirationdr_mksinhaNo ratings yet
- Falla Respiratoria Fisiopato Trend Anaesth Crit Care 2013Document5 pagesFalla Respiratoria Fisiopato Trend Anaesth Crit Care 2013Alexis Villagran ArancibiaNo ratings yet
- Pharmacokinetics of Inhalation AnestheticsDocument24 pagesPharmacokinetics of Inhalation AnestheticsKinanta DewiNo ratings yet
- Asthma + COPDDocument60 pagesAsthma + COPDNur HasanahNo ratings yet
- ARDS PresentationDocument89 pagesARDS Presentationalexandriaputera30No ratings yet
- Drugs Affecting The Respiratory System PPPDocument35 pagesDrugs Affecting The Respiratory System PPPChristopher VelonzaNo ratings yet
- Respiratory DisordersDocument8 pagesRespiratory DisordersDonna DayudayNo ratings yet
- 7a COPDDocument45 pages7a COPDDerrick GramataNo ratings yet
- DR DR Pramod Pramod K Sharma K SharmaDocument77 pagesDR DR Pramod Pramod K Sharma K SharmaSaurabh Gautam100% (1)
- Inhaled Anesthetics and Gases: Harry Singh, MD Dept. of Anesthesiology UtmbDocument57 pagesInhaled Anesthetics and Gases: Harry Singh, MD Dept. of Anesthesiology Utmbreenujohney100% (1)
- Respiratory DrugsDocument140 pagesRespiratory Drugsmoncalshareen3No ratings yet
- ATI Respiratory PowerpointDocument90 pagesATI Respiratory PowerpointAnn KelseaNo ratings yet
- The Role of High Flow Nasal CannulaDocument57 pagesThe Role of High Flow Nasal CannulaAhmad IrfanNo ratings yet
- Opioid DrugsDocument12 pagesOpioid DrugsSF170riyandaNo ratings yet
- Drugs Affecting The Respiratory Systems: Kuntarti, SKP, MbiomedDocument32 pagesDrugs Affecting The Respiratory Systems: Kuntarti, SKP, MbiomedRichard BungaNo ratings yet
- #6 Copd 11 PDFDocument11 pages#6 Copd 11 PDFOmar BasimNo ratings yet
- Chronic Obstructive Pulmonary DeseaseDocument30 pagesChronic Obstructive Pulmonary DeseaseShinta DewiNo ratings yet
- Inhalational Agents: General PrinciplesDocument13 pagesInhalational Agents: General PrinciplesShuvashishSunuwarNo ratings yet
- ANALGESIC DRUGS (DR - Dlawer)Document37 pagesANALGESIC DRUGS (DR - Dlawer)OMAR NASSERNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument27 pagesChronic Obstructive Pulmonary DiseaseMelissa MakhoulNo ratings yet
- Inhaled Anesthetics by HannanDocument92 pagesInhaled Anesthetics by HannanHafiz Abdul HannanNo ratings yet
- Immediate Management of Acute Severe AsthmaDocument44 pagesImmediate Management of Acute Severe Asthmasnowlover boyNo ratings yet
- Asthma SIM AnswersDocument4 pagesAsthma SIM Answersscorpioaj133No ratings yet
- Unit-Seven (Vii) : Drugs Affecting The Respiratory SystemDocument55 pagesUnit-Seven (Vii) : Drugs Affecting The Respiratory Systemdinberu tadesseNo ratings yet
- ANAPHY Lec Session #19 - SAS (Agdana, Nicole Ken)Document7 pagesANAPHY Lec Session #19 - SAS (Agdana, Nicole Ken)Nicole Ken AgdanaNo ratings yet
- Asthma ApproachDocument7 pagesAsthma ApproachpNo ratings yet
- Presented byDocument71 pagesPresented byRun HajNo ratings yet
- Desktop BioDocument8 pagesDesktop Biofdbp42kfs6No ratings yet
- Acute Respiratory Failure-PRINTDocument5 pagesAcute Respiratory Failure-PRINTJan SicatNo ratings yet
- Nasal High Ow Oxygen in Acute Respiratory Failure: Thematic Series: HOW I DO IT. Serie Editor: Stefano NavaDocument8 pagesNasal High Ow Oxygen in Acute Respiratory Failure: Thematic Series: HOW I DO IT. Serie Editor: Stefano NavaHector VillamarinNo ratings yet
- General Anesthetics TRANSDocument15 pagesGeneral Anesthetics TRANSNikki Tuazon BartolomeNo ratings yet
- (NS) AsthmaCOPDPneumonia Tutorial QuestionsDocument25 pages(NS) AsthmaCOPDPneumonia Tutorial QuestionsJoei “Jojo” GohNo ratings yet
- DR Ambreen Shams NephrologistDocument58 pagesDR Ambreen Shams NephrologistAamer NaeemNo ratings yet
- Non Respi O2 CO2 TransportDocument13 pagesNon Respi O2 CO2 TransportRicky JalecoNo ratings yet
- Doxovent M MedicalDocument38 pagesDoxovent M MedicalkurutalaNo ratings yet
- Lecture 2 Respiratory FailureDocument70 pagesLecture 2 Respiratory Failurej.doe.hex_87100% (1)
- Ija 59 574Document10 pagesIja 59 574Vasu DevanNo ratings yet
- AnstheticsDocument39 pagesAnstheticsAdduNo ratings yet
- PHC461 - Principles of Pharmacology CBL2Document12 pagesPHC461 - Principles of Pharmacology CBL2beyonduckNo ratings yet
- Approach Considerations: Respiratory Acidosis Treatment & ManagementDocument8 pagesApproach Considerations: Respiratory Acidosis Treatment & Managementprince1500No ratings yet
- By Linda S. Costanzo 5th Edition Published by Elsevier: PhysiologyDocument9 pagesBy Linda S. Costanzo 5th Edition Published by Elsevier: PhysiologyhavizafrizalNo ratings yet
- Treatment - of - Asthma (TUSOM - Pharmwiki)Document29 pagesTreatment - of - Asthma (TUSOM - Pharmwiki)AngelicaElizabetVelasquezNo ratings yet
- Resp Objectives Adn 253Document4 pagesResp Objectives Adn 253christian_zarate_2No ratings yet
- 1.respiratory SystemDocument42 pages1.respiratory SystemAlexandra AlexaNo ratings yet
- Giu 2986 62 16130 2024-02-22T14 46 59Document18 pagesGiu 2986 62 16130 2024-02-22T14 46 59amoraaloushNo ratings yet
- Drug Acting in Respiratory SystemDocument30 pagesDrug Acting in Respiratory SystemYunita WidyastutiNo ratings yet
- Heart-Lung Interactions : M.R.PinskyDocument2 pagesHeart-Lung Interactions : M.R.PinskyAnonymous qemC1CybLNo ratings yet
- AsthmaDocument6 pagesAsthmaJay Hipulan QuiranteNo ratings yet
- Applied Respiratory PhysiologyDocument4 pagesApplied Respiratory PhysiologyMitul JainNo ratings yet
- OpioidDocument12 pagesOpioidputriNo ratings yet
- Hyperoxia Intensive Care EmergeDocument14 pagesHyperoxia Intensive Care EmergeEdsonR GhNo ratings yet
- Acute/Adulth Respiratory Distress Syndrome (ARDS) : RohmanDocument54 pagesAcute/Adulth Respiratory Distress Syndrome (ARDS) : RohmanMuhammad Rizki Junaidi SaputraNo ratings yet
- Respiratory Failure PDFDocument5 pagesRespiratory Failure PDFOxana Turcu100% (1)
- THE BUTEYKO METHOD (Translated): The secret of controlled breathing for health, well-being and vitalityFrom EverandTHE BUTEYKO METHOD (Translated): The secret of controlled breathing for health, well-being and vitalityNo ratings yet
- Medical Mnemonic Sketches : Pulmonary DiseasesFrom EverandMedical Mnemonic Sketches : Pulmonary DiseasesNo ratings yet
- CEACCP - KetamineDocument5 pagesCEACCP - KetamineDonkeyManNo ratings yet
- CEACCP - Latex AllergyDocument4 pagesCEACCP - Latex AllergyDonkeyManNo ratings yet
- Physiol 93 B3Document1 pagePhysiol 93 B3DonkeyManNo ratings yet
- Pharm 00 B15Document2 pagesPharm 00 B15DonkeyManNo ratings yet
- Pharm 02 A10Document2 pagesPharm 02 A10DonkeyManNo ratings yet
- CEACCP - Illegal Substances in Anaesthetic and Intensive Care PracticesDocument5 pagesCEACCP - Illegal Substances in Anaesthetic and Intensive Care PracticesDonkeyManNo ratings yet
- CEACCP - Intrathecal Opioids in The Management of Acute Postoperative PainDocument5 pagesCEACCP - Intrathecal Opioids in The Management of Acute Postoperative PainDonkeyManNo ratings yet
- Pharm 00 A12Document1 pagePharm 00 A12DonkeyManNo ratings yet
- Pharm 02 A11Document4 pagesPharm 02 A11DonkeyManNo ratings yet
- Pharm 00 A14Document2 pagesPharm 00 A14DonkeyManNo ratings yet
- Outline The Physiological Consequences of Hyperosmolar Diabetic KetoacidosisDocument2 pagesOutline The Physiological Consequences of Hyperosmolar Diabetic KetoacidosisDonkeyManNo ratings yet
- Pharm 00 B11Document1 pagePharm 00 B11DonkeyManNo ratings yet
- Pharm 00 B14Document2 pagesPharm 00 B14DonkeyManNo ratings yet
- Pharm 00 A9Document2 pagesPharm 00 A9DonkeyManNo ratings yet
- Compare and Contrast Atropine and Glycopyrulate, and Discuss The Clinical ImplicationsDocument2 pagesCompare and Contrast Atropine and Glycopyrulate, and Discuss The Clinical ImplicationsDonkeyManNo ratings yet
- Compare and Contrast The Pharamcology of Ephedrine and NoradrenalineDocument1 pageCompare and Contrast The Pharamcology of Ephedrine and NoradrenalineDonkeyManNo ratings yet
- Compare and Contrast Neostigmine and The Organophosphate CompoundsDocument1 pageCompare and Contrast Neostigmine and The Organophosphate CompoundsDonkeyManNo ratings yet
- Define The Mechanisms of Action and Adverse Effects of Metoprolol, GTN, and Diltiazem When Used To Manage MIDocument2 pagesDefine The Mechanisms of Action and Adverse Effects of Metoprolol, GTN, and Diltiazem When Used To Manage MIDonkeyManNo ratings yet
- FS Antimicrobial Dosing Obesity AMS Updates Issue4 - Nov2018Document4 pagesFS Antimicrobial Dosing Obesity AMS Updates Issue4 - Nov2018DonkeyManNo ratings yet
- Compare and Contrast The Pharmacology of Esmolol and PropanololDocument1 pageCompare and Contrast The Pharmacology of Esmolol and PropanololDonkeyManNo ratings yet
- Base Excess (Be) Measure of Metabolic Acid-Base Status: Dr. David LynessDocument1 pageBase Excess (Be) Measure of Metabolic Acid-Base Status: Dr. David LynessDonkeyManNo ratings yet
- VOLATILEAGENTSDocument4 pagesVOLATILEAGENTSDonkeyManNo ratings yet
- Cholinergic Agents: Cholinergic Receptors Types of Receptor Muscarinic Receptor Nicotinic ReceptorDocument4 pagesCholinergic Agents: Cholinergic Receptors Types of Receptor Muscarinic Receptor Nicotinic ReceptorDonkeyManNo ratings yet
- Comparative Pharmacokinetics of Fentanyl and Alfentanil: Br. J. Anaesth. (1982), 54, 871Document7 pagesComparative Pharmacokinetics of Fentanyl and Alfentanil: Br. J. Anaesth. (1982), 54, 871DonkeyManNo ratings yet
- Palliative Care HandbookDocument82 pagesPalliative Care HandbookDonkeyManNo ratings yet
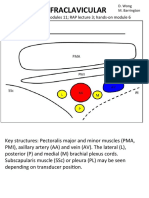
- Infraclavicular: Toolbox: Online Modules 11 RAP Lecture 3 Hands - On Module 6Document4 pagesInfraclavicular: Toolbox: Online Modules 11 RAP Lecture 3 Hands - On Module 6DonkeyManNo ratings yet
- The Physiology of The GIT and The Liver QuestionsDocument44 pagesThe Physiology of The GIT and The Liver QuestionsDonkeyManNo ratings yet