Professional Documents
Culture Documents
Maternal and Child Health Nursing: Sudden Pregnancy Complications
Uploaded by
IconMaico0 ratings0% found this document useful (0 votes)
9 views35 pagesSUDDEN PREGNANCY COMPLICATIONS
Original Title
MATERNAL AND CHILD HEALTH NURSING: SUDDEN PREGNANCY COMPLICATIONS
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentSUDDEN PREGNANCY COMPLICATIONS
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views35 pagesMaternal and Child Health Nursing: Sudden Pregnancy Complications
Uploaded by
IconMaicoSUDDEN PREGNANCY COMPLICATIONS
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 35
MCHN CHAPTER 21
Ma. Concepcion A. Maico-Bacus, EdD, MAN, RN, COHN
MCA Maico-Bacus, EdD, MAN, RN, COHN
SUDDEN PREGNANCY
COMPLICATIONS
MCA Maico-Bacus, EdD, MAN, RN, COHN
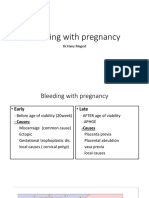
BLEEDING DURING PREGNANCY
KEY POINTS • Signs of shock:
• Always a deviation from • 10% blood volume or
normal, potentially serious, approximately 2 units have
been lost
may occur at any point in • Fetal distress occurs (at 25%
pregnancy blood loss)
• Potential emergency
• May mean placenta has
loosened and cut off
nourishment to the fetus
• Visualized blood may only be a
fraction
MCA Maico-Bacus, EdD, MAN, RN, COHN
MCA Maico-Bacus, EdD, MAN, RN, COHN
BLEEDING DURING PREGNANCY
THERAPEUTIC MANAGEMENT • If respirations are rapid: O2
FOR HYPOVOLEMIC SHOCK by mask and monitor O2
• Monitor urine output saturation levels by pulse
oximetry
• Obtain hgb and hct levels
• Frequent vs and fetal
• Blood typing and cross- monitoring (external
matching monitoring device)
• IV replacement: D5LR/LR • Rest: left lateral side-lying
• Large-gauge Angiocath (16 or position or FOB with pillow or
18) for rapid fluid expansion wedge under right hip
and to prepare for BT
MCA Maico-Bacus, EdD, MAN, RN, COHN
BLEEDING DURING PREGNANCY
Inserted p bleeding is halted:
• Central venous pressure
catheter (measures the
right atrial pressure or the
pressure of blood within the
vena cava): 1-6 mmHg
• Pulmonary capillary wedge
catheter (measures the
pressure in the left atrium
or the filling process of the
left ventricle): 6-12 mmHg
MCA Maico-Bacus, EdD, MAN, RN, COHN
EMERGENCY INTERVENTIONS FOR BLEEDING IN
PREGNANCY
• Alert healthcare team of • Withhold oral fluid
emergency situation • Order type and cross-match
• Place woman FOB on her side of 2 units FWB (fresh whole
• Begin IV D5LR/LR with 16-18 blood)
gauge Angiocath • Measure I&O
• Administer O2 as necessary at • Assess vs q 15mins; apply pulse
6-10L/min by face mask oximeter and automatic BP
• Monitor uterine contractions cuff as necessary
and FHR by external • Assist with placement of CVP
monitoring or PA catheter and blood
• Omit vaginal exam determinations
MCA Maico-Bacus, EdD, MAN, RN, COHN
EMERGENCY INTERVENTIONS FOR BLEEDING IN
PREGNANCY
• Measure maternal blood loss
by weighing perineal pads; save
any tissue passed
• Assist with ultrasound
examination
• Maintain positive attitude
about fetal outcome
• Support woman’s self-esteem;
provide emotional support to
woman and her support
person/s
MCA Maico-Bacus, EdD, MAN, RN, COHN
SPONTANEOUS MISCARRIAGE
KEY POINTS • Early miscarriage –
• Abortion – any interruption occurring before week 16
of a pregnancy before a • Late miscarriage – between
fetus is viable (a viable weeks 16 and 20
fetus is >20-24 weeks of • Bleeding before 6 weeks is
gestation or weighs at least rarely severe; after 12
500g à a fetus born before weeks is profuse
this point is considered a
miscarriage or is termed
premature or immature
birth)
MCA Maico-Bacus, EdD, MAN, RN, COHN
SPONTANEOUS MISCARRIAGE
COMMON CAUSES • Ingestion of alcohol at the
• 1ST Trimester – abnormal time of conception can
fetal development dt contribute to pregnancy loss
teratogenic factor or a • UTI
chromosomal aberration; • Systemic infections –
immunologic factors; rubella, syphilis,
rejection of the embryo poliomyelitis,
through an immune response cytomegalovirus,
(APS or antiphospholipid toxoplasmosis
syndrome); implantation
abnormalities
MCA Maico-Bacus, EdD, MAN, RN, COHN
SPONTANEOUS MISCARRIAGE
CLINICAL THERAPEUTIC
MANIFESTATIONS MANAGEMENT
• Spotting (contact • Determined by the primary
healthcare provider at first healthcare provider
indication)
• Read: immediate assessment
of vaginal bleeding
MCA Maico-Bacus, EdD, MAN, RN, COHN
SPONTANEOUS MISCARRIAGE
DIAGNOSIS: Threatened Management
miscarriage • Avoidance of strenuous
• Begin as vaginal bleeding, activity for 24-48 hrs
scant, bright red, slight • Bleeding may stop within 24-
cramping, no cervical dilatation 48hrs if the woman reduces
• May be asked to come to the activity
clinic for fetal heart sound • Normal activity resumption
assessment or an ultrasound to once bleeding stops
determine fetal viability
• Coitus may be restricted for 2
• Blood test: HCG hormone at weeks
the start of the bleeding and
again in 48hrs
MCA Maico-Bacus, EdD, MAN, RN, COHN
SPONTANEOUS MISCARRIAGE
DIAGNOSIS: Imminent Management
(Inevitable) Miscarriage • Inform the woman that
• Bleeding with uterine pregnancy has already been
contractions and cervical lost and procedures are to
dilatation clean the uterus and prevent
• The loss of the products of further complications (not to
conception cannot be halted end the pregnancy)
• Primary healthcare provider • Save any tissue fragments
may offer medication to help passed in the labor room
the pregnancy pass or perform • After discharge: woman should
dilatation & curettage (D&C) assess amount of vaginal
or dilatation & evacuation bleeding by recording the
(D&E) number of pads
MCA Maico-Bacus, EdD, MAN, RN, COHN
SPONTANEOUS MISCARRIAGE
DIAGNOSIS: Complete Management
Miscarriage • No therapy is needed
• The entire products of • Advise woman to report
conception )fetus, heavy bleeding
membranes, and placenta)
are expelled spontaneously
without any assistance
• Bleeding usually slows within
2 hrs and then ceases within
a few days after passage of
the products of conception
MCA Maico-Bacus, EdD, MAN, RN, COHN
SPONTANEOUS MISCARRIAGE
DIAGNOSIS: Incomplete Management
Miscarriage • Be certain the woman knows
• Part of the conceptus (usually the pregnancy is already lost
the fetus) is expelled, but the and that procedures are being
membranes or placenta are done to protect her from
retained in the uterus hemorrhage and infection, not
• Danger of maternal to end the pregnancy
hemorrhage
• D&C or suction curettage to
evacuate the remainder of the
pregnancy
MCA Maico-Bacus, EdD, MAN, RN, COHN
SPONTANEOUS MISCARRIAGE
DIAGNOSIS: Missed Management
Miscarriage • After ultrasound establishes
• Also referred to as early the fetus has no HR, D&C or
pregnancy failure D&E may be done
• The fetus dies in utero but is • If pregnancy is over 14 weeks,
not expelled labor is induced by a
• Usually discovered at prenatal prostaglandin suppository or
exam when the fundal height misoprostol (Cytotec)
is measured and no increase in introduced into the posterior
size can be demonstrated or fornix of the vagina to cause
previously-heard fetal heart dilatation, followed by
sounds can no longer be heard oxytocin stimulation or
administration of mifepristone
MCA Maico-Bacus, EdD, MAN, RN, COHN
SPONTANEOUS MISCARRIAGE
DIAGNOSIS: Recurrent
Pregnancy Loss
• Causes:
• Defective spermatozoa or ova
• Endocrine factors
• Deviations of the uterus
(septate or bicornuate uterus)
• Resistance to uterine artery
blood flow
• Chorioamnionitis or uterine
infection
• Autoimmune disorders (lupus
anticoagulant and
antiphospholipid anitbodies)
MCA Maico-Bacus, EdD, MAN, RN, COHN
MCA Maico-Bacus, EdD, MAN, RN, COHN
COMPLICATIONS OF MISCARRIAGE
HEMMORHAGE • If bleeding doesn’t halt, D&C
• Monitor vs for changes to or suction curettage
detect hypovolemic shock • Transfusion; direct
• If excessive bleeding occurs: replacement of fibrinogen or
immediately position the another clotting factor
woman flat and massage the • Health education: bleeding
uterine fundus amount, color, odor, passing of
• Applying pneumatic antishock large clots
garments can help maintain BP • Health education: medication,
methylergonovine maleate
(Methergine)
MCA Maico-Bacus, EdD, MAN, RN, COHN
COMPLICATIONS OF MISCARRIAGE
INFECTION • Advise not to use tampons
• May develop most often in
women who have lost an
appreciable amount of blood
• Signs: fever higher than 38C,
abdominal pain or tenderness,
foul-smelling vaginal discharge
• E. coli or group A
streptococcus
• Wiping perineal area from
front to back
MCA Maico-Bacus, EdD, MAN, RN, COHN
COMPLICATIONS OF MISCARRIAGE
SEPTIC ABORTION • Uterus will feel tender to
• An abortion complicated by palpation
an infection • May lead to toxic shock
• More frequently occurs in syndrome, septicemia,
women who have tried to kidney failure, and death if
self-abort or whose infection is left untreated
pregnancy was aborted • CBC, serum electrolytes,
illegally using a nonsterile serum creatinine, blood type
instrument and cross-match; cervical,
• Symptoms of fever and vaginal, and urine culture
crampy abdominal pain are obtained
MCA Maico-Bacus, EdD, MAN, RN, COHN
COMPLICATIONS OF MISCARRIAGE
• Foley catheter may be • CVP or PA catheter may be
inserted to monitor urine inserted to monitor left atrial
output hourly to assess kidney filling pressure and
function hemodynamic status
• IVF to restore fluid volume • D&C or D&E
and provide route for high- • Tetanus toxoid SQ or tetanus
dose, broad-spectrum immune globulin IM:
antibiotic therapy is begun prophylaxis against tetanus
• Combination of penicillin, • Dopamine and digitalis to
gentamicin, and clindamycin is maintain cardiac output
commonly prescribed
• O2 and ventilation support
MCA Maico-Bacus, EdD, MAN, RN, COHN
COMPLICATIONS OF MISCARRIAGE
• Final result may be
infertility or uterine
scarring or fibrotic scarring
of the fallopian tubes
• Follow up social work
counseling
MCA Maico-Bacus, EdD, MAN, RN, COHN
COMPLICATIONS OF MISCARRIAGE
ISOIMMUNIZATION POWERLESSNESS OR
• The production of ANXIETY
antibodies against Rh- • Assess a woman’s
positive blood adjustment to a spontaneous
• After miscarriage, all miscarriage
women with Rh- blood should • Assess the partner or the
receive Rh (D antigen) family’s feelings as well
immune globulin (RhIG)
MCA Maico-Bacus, EdD, MAN, RN, COHN
ECTOPIC PREGNANCY
KEY POINTS
• Implantation outside the
uterine cavity; fallopian
tube is the most common
site
• Obstruction; malformations;
scars
• Increasing rate: increasing
pelvic inflammatory disease,
in vitro fertilization, women
who smoke
MCA Maico-Bacus, EdD, MAN, RN, COHN
ECTOPIC PREGNANCY
• No unusual symptoms at the • Manifestations: sharp,
time of implantation stabbing pain in one of her
• Diagnosis: early pregnancy lower abdominal quadrants
ultrasound, MRI at the time of rupture,
followed by scant vaginal
• Rupture of fallopian tube (6- spotting; hypotension from
12 weeks of pregnancy) à blood loss, light-headedness,
bleeding rapid PR (signs of
• Implantation at the hypovolemic shock);
interstitial portion of the leukocytosis may be
tube: severe intraperitoneal present, normal temp
bleeding
MCA Maico-Bacus, EdD, MAN, RN, COHN
ECTOPIC PREGNANCY
• Transvaginal ultrasound: • If a woman waits for a time
ruptured tube and blood before seeking help, her
collecting in the peritoneum abdomen gradually becomes
• Either a falling HCG or rigid and the umbilicus may
serum progesterone levels develop a bluish-tinged hue
indicate the pregnancy has (Cullen sign); may have
ended continuing extensive or dull
vaginal or abdominal pain;
• Laparoscopy or culdoscopy movement of the cervix on
• Ultrasound pelvic exam causes
excruciating pain
MCA Maico-Bacus, EdD, MAN, RN, COHN
ECTOPIC PREGNANCY
• Pain on the shoulders as well THERAPEUTIC
as blood in the peritoneal MANAGEMENT
cavity • Some have no treatment
• Tender mass is palpable in • If detected early in
Douglas cul-de-sac on pregnancy: IM or oral
vaginal examination administration of
methotrexate; treated until
a negative HCG titer is
achieved
• Hysterosalpingogram or
UTS
MCA Maico-Bacus, EdD, MAN, RN, COHN
ECTOPIC PREGNANCY
• If the ectopic pregnancy is • If detected early in
discovered only when it pregnancy: IM or oral
ruptures, it creates an methotrexate; treated until
emergency situation a negative HCG titer is
achieved
THERAPEUTIC • Hysterosalpingogram or
MANAGEMENT UTS (to assess tube if
pregnancy is no longer
• Some have no treatment present and tube patency)
• Hgb level; blood typing & • IVF using large-gauge
cross-matching, hCG level catheter
MCA Maico-Bacus, EdD, MAN, RN, COHN
ECTOPIC PREGNANCY
• Ruptured ectopic pregnancy:
laparoscopy: to ligate the
bleeding vessels and to
remove/repair damaged
fallopian tube
• RhIG/RhoGAM after
ectopic pregnancy for
isoimmunization protection
in future chilbearing
MCA Maico-Bacus, EdD, MAN, RN, COHN
ABDOMINAL PREGNANCY
• Fetus grows in the pelvic • MRI: fetus outside the uterus
cavity • Danger: the placenta could
• Fetal outline is usually easily infiltrate and erode a major
palpable blood vessel in the abdomen à
• Woman may not be aware of of hemorrhage
movements; she may • Intestine: may cause bowel
experience painful fetal perforation, leaking of
movements and abdominal intestinal contents, peritonitis
cramping with fetal • High risk fetus: growth
movements; sudden lower deformity or growth
quadrant pain restriction
MCA Maico-Bacus, EdD, MAN, RN, COHN
ABDOMINAL PREGNANCY
• Infant born via laparotomy
• Placenta may be left in place
and allowed to absorb in 2-3
months; ff-up UTS to check
• Methotrexate: helps
placenta absorb
MCA Maico-Bacus, EdD, MAN, RN, COHN
GESTATIONAL TROPHOBLASTIC DISEASE
KEY POINTS • 2 types: complete and partial
• H. mole (hydatidiform mole) • Complete: all trophoblastic villi
swell and become cystic; father-
• Abnormal proliferation and only chromosome; fertilization
then degeneration of of an empty ovum
trophoblastic villi • Partial: some villi form normally;
syncytiotrophoblastic villi appear
• Associated with swollen and misshapen; 69
choriocarcinoma chromosomes (3 chromosomes);
rarely lead to choriocarcinoma
• Tend to occur in women with
low protein intake, >35 yo, • hCG titers are lower in partial;
Asian heritage, A women who return to normal faster after
marry O men evacuation
MCA Maico-Bacus, EdD, MAN, RN, COHN
GESTATIONAL TROPHOBLASTIC DISEASE
ASSESSMENT • UTS: dense growth (snowflake
• Uterus expands further than pattern), but no fetal growth; no
usual; reaches landmark before FH sounds; no viable fetus
the usual time
• Serum or urine test of hCG for
pregnancy will be strongly
positive (1-2M; normal is at
400,000); continues to be
strongly positive after day 100
• Marked N&V
• Symptoms of GHPN: increased
BP, edema, proteinuria (usually
not present before 20th week in
normal pregnancy)
MCA Maico-Bacus, EdD, MAN, RN, COHN
GESTATIONAL TROPHOBLASTIC DISEASE
THERAPEUTIC MANAGEMENT • While waiting for hCG decline,
• Suction curettage; after: woman should use oral
baseline pelvic exam, serum contraceptive (E/P)
test for beta subunit of hCG • If hCG levels are negative
• hCG is analyzed q 2wks until after 6months, woman is
levels are normal theoretically free from the
risk of malignancy
• Serum hCG is then assessed q
4wks for the next 6-12months • By 12months, she can begin to
to see if it is declining plan pregnancy
• If the level increases = • Methotrexate; dactinomycin
malignant transformation
MCA Maico-Bacus, EdD, MAN, RN, COHN
You might also like
- Leininger, Madeleine M. - McFarland, Marilyn R-Transcultural Nursing - Concepts, Theories, Research and practice-McGraw-H PDFDocument648 pagesLeininger, Madeleine M. - McFarland, Marilyn R-Transcultural Nursing - Concepts, Theories, Research and practice-McGraw-H PDFAviati Faradhika100% (10)
- Nursing Care for At-Risk Mothers and ChildrenDocument19 pagesNursing Care for At-Risk Mothers and ChildrenChelleyOllitro100% (7)
- Obstetrical Emergencies Maternity NursingDocument100 pagesObstetrical Emergencies Maternity Nursingsanthiyasandy100% (4)
- Tmbool's Notes in Obstetrics and Gynecology PDFDocument113 pagesTmbool's Notes in Obstetrics and Gynecology PDFOsman SomiNo ratings yet
- Obstetric Emergencies and Anesthetic Management: Co-Ordinator: DR - Navab Singh (M.D.) Speaker: Dr. UdayDocument35 pagesObstetric Emergencies and Anesthetic Management: Co-Ordinator: DR - Navab Singh (M.D.) Speaker: Dr. UdayKutumela MolebogengNo ratings yet
- Antepartum HaemorrhageDocument65 pagesAntepartum HaemorrhageAmit RamrattanNo ratings yet
- Nursing 311 Techniques of Therapeutic Communication: Technique Description ExampleDocument4 pagesNursing 311 Techniques of Therapeutic Communication: Technique Description ExampleIconMaico100% (1)
- NITI AayogDocument6 pagesNITI Aayogs100% (1)
- By Gemechu M (MD)Document26 pagesBy Gemechu M (MD)Semon YohannesNo ratings yet
- Definition: Genital Tract Bleeding From 28th Incidence: 2 - 3 % of All PregnanciesDocument31 pagesDefinition: Genital Tract Bleeding From 28th Incidence: 2 - 3 % of All PregnanciesMRT RadiologyNo ratings yet
- Maternity 2 Ante-Partum Haemorrhage (Aph) 26.3.2021Document29 pagesMaternity 2 Ante-Partum Haemorrhage (Aph) 26.3.2021Siti Nur Amalia FaizalNo ratings yet
- Antepartum Haemorrhage: DR Nurul Iftida Basri Lecturer and Specialist Obstetrics & Gynaecology DepartmentDocument27 pagesAntepartum Haemorrhage: DR Nurul Iftida Basri Lecturer and Specialist Obstetrics & Gynaecology DepartmentAishwarya SivakumarNo ratings yet
- By: Huzaifa HamidDocument31 pagesBy: Huzaifa Hamidرفاعي آكرمNo ratings yet
- Antipartum Heamorrhage: Presenter Nsubuga Ivan MBCHB Stud 3.2 Kiu Lira Center Date 23 / 2 /2022Document49 pagesAntipartum Heamorrhage: Presenter Nsubuga Ivan MBCHB Stud 3.2 Kiu Lira Center Date 23 / 2 /2022Nsubuga IvanNo ratings yet
- APH&PPHDocument77 pagesAPH&PPHKåbåñå TürüñåNo ratings yet
- Understanding Post-term Pregnancy ManagementDocument16 pagesUnderstanding Post-term Pregnancy Managementahmed shorsh100% (1)
- OBSTETRICAL HEMORRHAGE REVISED ScribdDocument34 pagesOBSTETRICAL HEMORRHAGE REVISED Scribdindah.obginuh.jul20No ratings yet
- Umbilical Cord AccidentsDocument16 pagesUmbilical Cord Accidentschebetnaomi945No ratings yet
- Dysfunction of The Genito-Urinary Tract: Dejene Edosa (BSC, MSC in CMW) July 2021Document25 pagesDysfunction of The Genito-Urinary Tract: Dejene Edosa (BSC, MSC in CMW) July 2021michaelNo ratings yet
- Management of Pregnancy Related BleedingDocument75 pagesManagement of Pregnancy Related BleedingChuah Wei Hong100% (1)
- Antepartum Haemorrhage MXDocument22 pagesAntepartum Haemorrhage MXAmir Hilmi Abd AzizNo ratings yet
- Antepartum BleedingDocument55 pagesAntepartum BleedingMunfaati AbdiyahNo ratings yet
- Ante-Partum HaemorrhageDocument42 pagesAnte-Partum HaemorrhageSerenna DehalooNo ratings yet
- Umbilical Cord Accidents-1Document16 pagesUmbilical Cord Accidents-1chebetnaomi945No ratings yet
- Bleeding Causes and ManagementDocument90 pagesBleeding Causes and ManagementAbdullah GadNo ratings yet
- Hyperemesis, Hmole, Placenta PreviaDocument12 pagesHyperemesis, Hmole, Placenta Previadanica grace gubaNo ratings yet
- Placenta IsuogDocument40 pagesPlacenta IsuogKARINA BASTIDAS IBARRA100% (1)
- Ectopic Pregnancy: Causes, Symptoms and Treatment OptionsDocument2 pagesEctopic Pregnancy: Causes, Symptoms and Treatment OptionsKrista P. AguinaldoNo ratings yet
- Ectopic Pregnancy: Causes, Symptoms and Treatment OptionsDocument2 pagesEctopic Pregnancy: Causes, Symptoms and Treatment OptionsLuis PadillaNo ratings yet
- Antepartum Haemorrhage PDFDocument5 pagesAntepartum Haemorrhage PDFRaditya TaslimNo ratings yet
- Female Pelvic Anatomy GuideDocument60 pagesFemale Pelvic Anatomy Guidekatherine nunnNo ratings yet
- Bleeding in PregnancyDocument15 pagesBleeding in PregnancyMalaika NoorNo ratings yet
- 1.antepartum HeamorrhageDocument26 pages1.antepartum Heamorrhagems khanNo ratings yet
- Bleeding in Early and Late: PregnancyDocument31 pagesBleeding in Early and Late: Pregnancysny007No ratings yet
- 2 - Pre Gestational ConditionDocument11 pages2 - Pre Gestational ConditionAngelica Dalit MendozaNo ratings yet
- 1 Chapter 21 Pregnancy Complication BLEEDING DURING PREGNANCYDocument76 pages1 Chapter 21 Pregnancy Complication BLEEDING DURING PREGNANCYCAÑADA, JOHANNELYN M.No ratings yet
- Maternal MidtermDocument253 pagesMaternal MidtermTrishaNo ratings yet
- PERDARAHAN AWAL DAN AKHIR KEHAMILAN Wo SoalDocument31 pagesPERDARAHAN AWAL DAN AKHIR KEHAMILAN Wo SoalPutri MeutiaNo ratings yet
- Ectopic Pregnancy Diagnosis and ManagementDocument44 pagesEctopic Pregnancy Diagnosis and ManagementDegefaw BikoyNo ratings yet
- Antepartum HemorrhageDocument22 pagesAntepartum HemorrhageGetaneh LiknawNo ratings yet
- Neonatal Sepsis: Alan Chan, MDDocument28 pagesNeonatal Sepsis: Alan Chan, MDashaba sysonNo ratings yet
- Abnormal Ob HandoutsDocument3 pagesAbnormal Ob HandoutsBoy MadNo ratings yet
- Abortionme 200907085856Document77 pagesAbortionme 200907085856tengizbaindurishviliNo ratings yet
- Seminar 11 APH and PPHDocument61 pagesSeminar 11 APH and PPHIshak IzharNo ratings yet
- High Risk Pregnancy FinaleDocument149 pagesHigh Risk Pregnancy FinaleQuolette Constante100% (1)
- Vaginal Birth After Caesarean Section (Vbac)Document16 pagesVaginal Birth After Caesarean Section (Vbac)api-370504650% (2)
- Caesarean SectionDocument73 pagesCaesarean SectionBhattarai Shrinkhala100% (2)
- Obstetric Highlights, Elmar P. SakalaDocument47 pagesObstetric Highlights, Elmar P. Sakaladukelist5660% (1)
- 240 243Document5 pages240 243Rika WulandariNo ratings yet
- Managing Obstetrical Emergencies & Its ChallengesDocument58 pagesManaging Obstetrical Emergencies & Its Challengessanthiyasandy100% (1)
- Management of Placenta Previa During PregnancyDocument14 pagesManagement of Placenta Previa During Pregnancykhaira_nNo ratings yet
- Antepartum Haemorrhage PolicyDocument5 pagesAntepartum Haemorrhage PolicyubayyumrNo ratings yet
- 1hemorragic Obstetric EmergencyDocument50 pages1hemorragic Obstetric EmergencyRaguNo ratings yet
- Antepartum HemorrhageDocument5 pagesAntepartum Hemorrhagecode-24No ratings yet
- CA MaternalDocument156 pagesCA MaternalLovely Hope LugatimanNo ratings yet
- POSTPARTUM-HEMORRHAGE LecDocument13 pagesPOSTPARTUM-HEMORRHAGE LecMay MayNo ratings yet
- Postterm Pregnancy Risks and ManagementDocument29 pagesPostterm Pregnancy Risks and ManagementNur Agami100% (1)
- Tmbool's Notes in Obstetrics and GynecologyDocument113 pagesTmbool's Notes in Obstetrics and GynecologyFrom HumanNo ratings yet
- MiscarriageDocument42 pagesMiscarriageAnonymous pJfAvl100% (3)
- Prenatal Screening: HM Sulchan Sofoewan Divisi Feto-Maternal Bagian Obstetri Dan Ginekologi FK UGMDocument54 pagesPrenatal Screening: HM Sulchan Sofoewan Divisi Feto-Maternal Bagian Obstetri Dan Ginekologi FK UGMTahta PambudiNo ratings yet
- Post-Partum Hemorrhage (PPH) : 6/25/22 1 Fentahun ADocument30 pagesPost-Partum Hemorrhage (PPH) : 6/25/22 1 Fentahun ADani AsmareNo ratings yet
- Acute Gynaecological EmergenciesDocument22 pagesAcute Gynaecological EmergenciesMuhammad AmeenNo ratings yet
- Comprehensive Abortion Care GuideDocument42 pagesComprehensive Abortion Care GuideKate SantosNo ratings yet
- Complications of Labor and BirthDocument54 pagesComplications of Labor and BirthIconMaicoNo ratings yet
- GI DrugsDocument35 pagesGI DrugsIconMaicoNo ratings yet
- Chapter 8 - Clarifying Quantitative Research DesignsDocument61 pagesChapter 8 - Clarifying Quantitative Research DesignsIconMaicoNo ratings yet
- 200p Hba UscherpinesDocument59 pages200p Hba UscherpinesIconMaicoNo ratings yet
- Cell Structure and Taxonomy ExplainedDocument46 pagesCell Structure and Taxonomy ExplainedIconMaicoNo ratings yet
- FHT:Fundal HT QuestionsDocument2 pagesFHT:Fundal HT QuestionsIconMaicoNo ratings yet
- Caring For The Woman Experiencing Complications During Labor and BirthDocument26 pagesCaring For The Woman Experiencing Complications During Labor and BirthIconMaicoNo ratings yet
- Healthcare-Associated Infections GuideDocument25 pagesHealthcare-Associated Infections GuideIconMaicoNo ratings yet
- NCM 109 Course OutlineDocument2 pagesNCM 109 Course OutlineIconMaicoNo ratings yet
- Introduction To Microbiology: Ma. Concepcion A. Maico, RN, Man, EddDocument24 pagesIntroduction To Microbiology: Ma. Concepcion A. Maico, RN, Man, EddIconMaicoNo ratings yet
- Caregiving Through The 5 Stages of Ageing - Brain SparksDocument8 pagesCaregiving Through The 5 Stages of Ageing - Brain SparksIconMaicoNo ratings yet
- Inside Out - A Psychological InsightDocument6 pagesInside Out - A Psychological InsightIconMaicoNo ratings yet
- Lab Manual Microbiology For Allied Health Students 1.3Document115 pagesLab Manual Microbiology For Allied Health Students 1.3IconMaicoNo ratings yet
- Microscopy Basics Biology Laboratory 1 PowerPointDocument17 pagesMicroscopy Basics Biology Laboratory 1 PowerPointIconMaicoNo ratings yet
- The Importance of Self-Awareness in Psychiatric Nursing 1996Document4 pagesThe Importance of Self-Awareness in Psychiatric Nursing 1996IconMaicoNo ratings yet
- Caregiving Through The 5 Stages of Ageing - Brain SparksDocument8 pagesCaregiving Through The 5 Stages of Ageing - Brain SparksIconMaicoNo ratings yet
- Erikson Summary ChartDocument1 pageErikson Summary ChartIconMaicoNo ratings yet
- RLE Activity Personality DisorderDocument5 pagesRLE Activity Personality DisorderIconMaicoNo ratings yet
- Activity Participation and Older AdultsDocument8 pagesActivity Participation and Older AdultsIconMaicoNo ratings yet
- 2019 Dec ERIA Ageing and Health in The PhilippinesDocument276 pages2019 Dec ERIA Ageing and Health in The PhilippineshexenejenineNo ratings yet
- FEG PPCommunication With Older PeopleDocument21 pagesFEG PPCommunication With Older PeopleroarkesNo ratings yet
- Harry Potter Psychoanalytical ApproachDocument12 pagesHarry Potter Psychoanalytical ApproachIconMaicoNo ratings yet
- Aging in The Philippines - PSADocument33 pagesAging in The Philippines - PSAIconMaicoNo ratings yet
- Theoretical Foundations of Transcultural NursingDocument19 pagesTheoretical Foundations of Transcultural NursingIconMaicoNo ratings yet
- Sunrise Enabler in EthnonursingDocument28 pagesSunrise Enabler in EthnonursingIconMaicoNo ratings yet
- 5 Stages of Aging - Tealridge Retirement CommunityDocument3 pages5 Stages of Aging - Tealridge Retirement CommunityIconMaicoNo ratings yet
- Nick & Sammy - Baby You Love Me (Bass Tab)Document6 pagesNick & Sammy - Baby You Love Me (Bass Tab)Martin MalenfantNo ratings yet
- Hydraulic Pumps Lec NotesDocument30 pagesHydraulic Pumps Lec NotesDarsh MenonNo ratings yet
- Inventory Costs and ControlDocument7 pagesInventory Costs and ControlEden Dela CruzNo ratings yet
- ARTS8 Q4 MOD2Document32 pagesARTS8 Q4 MOD2eoghannolascoNo ratings yet
- Black Magic v03n04 1967-01.american Art AgencyDocument82 pagesBlack Magic v03n04 1967-01.american Art AgencyJulieta de la HuertaNo ratings yet
- Unit 2.ieltsDocument11 pagesUnit 2.ieltsKarina HrishkovskaNo ratings yet
- The Epic Story of Hinilawod, the Hiligaynon Nation's Epic PoemDocument18 pagesThe Epic Story of Hinilawod, the Hiligaynon Nation's Epic PoemMark Lexter A. PinzonNo ratings yet
- Balara - Mechanical Drawings - IFC PDFDocument6 pagesBalara - Mechanical Drawings - IFC PDFjomer john estoneloNo ratings yet
- Individual and Market Demand: Chapter OutlineDocument57 pagesIndividual and Market Demand: Chapter OutlineAbdullahiNo ratings yet
- Remedies in TortDocument4 pagesRemedies in TortAhmad Irtaza Adil100% (2)
- RecipesDocument102 pagesRecipesmajaklipa100% (3)
- Wax Rolls For Your Success: Yarn Yearns For The One and OnlyDocument9 pagesWax Rolls For Your Success: Yarn Yearns For The One and Onlyangga widayantoNo ratings yet
- Pike County Sheriff Forms Major Crimes Task Force For Unsolved MurdersDocument2 pagesPike County Sheriff Forms Major Crimes Task Force For Unsolved MurdersAndy Burgoon100% (1)
- Dokumen - Tips - Chapter 17 Job Order Costing Costing Chapter 17 Learning Objectives 1 DistinguishDocument25 pagesDokumen - Tips - Chapter 17 Job Order Costing Costing Chapter 17 Learning Objectives 1 DistinguishNouman SheikhNo ratings yet
- DLP Pe - 1 & 2Document1 pageDLP Pe - 1 & 2Dn AngelNo ratings yet
- L46 - Whitefield Lab Home Visit Sy No. 18/1B, K R Puram, Hobli, Sree Sai Harsha Tower, White FieldDocument4 pagesL46 - Whitefield Lab Home Visit Sy No. 18/1B, K R Puram, Hobli, Sree Sai Harsha Tower, White FieldSayantan BanerjeeNo ratings yet
- Order Setting Trial - State V Matthew J. Wessels - Fecr012392Document22 pagesOrder Setting Trial - State V Matthew J. Wessels - Fecr012392thesacnewsNo ratings yet
- Energy Conservation Techniques For Manufacturing IndustriesDocument11 pagesEnergy Conservation Techniques For Manufacturing IndustriesIJRASETPublicationsNo ratings yet
- About The Rosary of Our LadyDocument2 pagesAbout The Rosary of Our LadyINONG235No ratings yet
- Effect of Low Pressure Alkaline Delignification Process On TheDocument15 pagesEffect of Low Pressure Alkaline Delignification Process On Thenurshiyama89No ratings yet
- Vegetable Salad RecipesDocument11 pagesVegetable Salad RecipesPraneet NagdevNo ratings yet
- SCHNEIDER NABCEP PV Resource Guide 10 4 16 W PDFDocument174 pagesSCHNEIDER NABCEP PV Resource Guide 10 4 16 W PDFbacuoc.nguyen356100% (1)
- Horno Industrial HC1 v1.1Document30 pagesHorno Industrial HC1 v1.1Cristian urielNo ratings yet
- 16.11.22 - EDT - Prof. Ziad Al-Ani - NotesDocument3 pages16.11.22 - EDT - Prof. Ziad Al-Ani - NotesAarya Haridasan NairNo ratings yet
- Ravi KantDocument1 pageRavi KanthimeltoujoursperitusNo ratings yet
- Negotiation Self-Assessment and Vision Report - by Umang DharDocument1 pageNegotiation Self-Assessment and Vision Report - by Umang Dharumangdhar8No ratings yet
- Agenda DP Consultation Visit - Nov 2013Document2 pagesAgenda DP Consultation Visit - Nov 2013api-236337064No ratings yet
- Malbog Sulfuric Hot SpringDocument2 pagesMalbog Sulfuric Hot SpringMark-Christopher Roi Pelobello MontemayorNo ratings yet
- Republic Act No. 7611Document27 pagesRepublic Act No. 7611Paul John Page PachecoNo ratings yet