Professional Documents
Culture Documents
2116 Manuscript 17522 1 10 20200911
Uploaded by
sibon M amrilOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2116 Manuscript 17522 1 10 20200911
Uploaded by
sibon M amrilCopyright:
Available Formats
Original Article
J Nepal Health Res Counc 2020 Apr-Jun;18(47): 233-7
DOI: https://doi.org/10.33314/jnhrc.v18i2.2116
Comparative Study of Slow Infusion versus Bolus
Doses of Albumin and Furosemide Infusion to
Mobilize Refractory Ascites in Decompensated
Chronic Liver Disease
Rahul Pathak,1 Ajay Kumar Yadav,2 Sabin Thapaliya,2 Brindeshwari Kafle,1 Anurag Jha,1 Prem Khadga1
1
Department of Gastroenterology, Tribhuvan University Teaching Hospital, Maharajgunj, Kathmandu,
2
Department of Internal Medicine, Tribhuvan University Teaching Hospital, Maharajgunj, Kathmandu, Nepal.
ABSTRACT
Background: Combined use of furosemide with albumin is an approved therapy to overcome diuretic resistance
in treatment of ascites in decompensated chronic liver disease. Bolus dosing of diuretics has its own limitations due
to pre-existing hypotension, post diuretic sodium retention and braking phenomenon. Slow albumin and furosemide
Infusion has been shown to mobilize large ascites with improved diuresis and hemodynamic stability in decompensated
chronic liver disease. This study was undertaken to compare efficacy and safety of infusion therapy vs bolus therapy in
term the management of refractory ascites.
Methods: Decompensated chronic liver disease patients with refractory ascites were randomly assigned into two
groups of 15 each - Bolus therapy (intravenous albumin and furosemide as boluses) and Infusion therapy (furosemide
infusion at 2mg/hour and albumin at 2g/hour for three days). Diuresis, natriuresis, change in abdominal girth and
body weight, and hemodynamic stability (change in SBP) were compared between the two groups.
Results: Infusion therapy, as compared to bolus therapy, showed a significantly better diuresis (mean urinary output
increment 483ml vs 243ml, p <0.001), natriuresis (mean urinary sodium excretion increment 35.2 mEq/L vs 16.6
mEq/L, p = 0.004),decrease in abdominal circumference (6.1cm vs 3.0cm, p<0.001) and decrease in body weight
(5.53 Kg vs 2.86 Kg, p < 0.001). The complications of renal impairment were also lower in the Infusion group.
Conclusion: Infusion of furosemide and albumin is a potential safer and effective therapeutic option in the
management of refractory ascites with better natriuresis, higher urine output, and higher decrement in abdominal
circumference and body weight, and lesser side effects.
Keywords: Bolus dose; continuous infusion; decompensated chronic liver disease; refractory ascites.
INTRODUCTION progressively after first 1-2 hours with post-diuretic
compensatory sodium retention.12,13 Continuous infusion
Ascites is the most common presentation of maintains an effective rate of furosemide metabolism
decompensated CLD.1 Treatment modalities for ascites and inhibition of sodium retention over time with 30%
have their own limitations and complications.2-5 increase in sodium excretion.14 Meta-analysis were of
Combined use of furosemide and albumin has shown the opinion that infusions were more effective than
better results in different conditions of fluid overload intermittent boluses.15
than furosemide alone.6-8 Bolus dosing is limited by pre-
treatment hypotension and complications.9 Few studies This study was done to compare the efficacy (ascites
show improved diuresis and hemodynamic stability with fluid mobilization, abdominal girth reduction, diuresis/
slow infusions of albumin and furosemide in refractory natriuresis) and safety (hemodynamic stability and
ascites.10,11 dyselectrolytemia) of slow infusions with standard bolus
therapy in the management of ascites in decompensated
With furosemide boluses, sodium excretion declines CLD.
Correspondence: Dr Rahul Pathak, Department of Gastroenterology,
Tribhuvan University Teaching Hospital, Maharajgunj, Kathmandu, Nepal.
Email: pathak.drrahul@gmail.com.
JNHRC Vol. 18 No. 2 Issue 47 Apr - Jun 2020 233
Slow Infusion versus Bolus Doses of Albumin and Furosemide Infusion to Mobilize Refractory Ascites in Decompensated Chronic Liver Disease
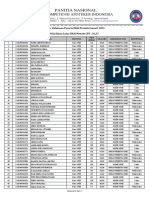
METHODS diagnoses of decompensated CLD with refractory ascites
were divided into two groups (Bolus Group and Infusion
This was a quasi-experimental study and was carried Group) of 15 each. All the baseline characteristics were
out at the Department of Gastroenterology, Tribhuvan comparable between the two groups - Bolus and Infusion
University Teaching Hospital, Maharajgunj, Kathmandu, group as summarized in the following table (Table 1).
Nepal after IRB approval. 30 patients (15 in Infusion
Group and 15 in Bolus Therapy Group) admitted to the Table 1. Table showing comparison of baseline
hospital meeting the criteria during the period from characteristics of the patients included in the two groups
- Bolus and Infusion group.
August 2017 to August 2018 were studied. Written
informed consent was taken from each patient or their Bolus group Infusion P
Variables
(N=15) group (N=15) value
relatives prior to enrollment in study. Patients were
Age 53 (74-40) 55 (74-40) 0.7
selected by non-probability sampling.
Sex
Patients of decompensated CLD, aged ≥18 years, who Male 12 (80) 13 (87)
Female 3 (20) 2 (13)
were hemodynamically stable for at least 24h (absence
of persistent [>1h] hypotension [systolic blood pressure Alcohol consumer 13 (87) 13 (87)
<90 mmHg), not currently on vasopressors, with Hemoglobin (g/dl) 10 (7-13) 10 (7-11) 0.43
hypoproteinemia (serum albumin <30g/L or total protein Platelet (×103/cu
107 (31-175) 110 (39-153) 0.84
< 60 g/L) and requiring diuresis for refractory ascites, mm)
those not responding to diuretics alone were included Serum Sodium 134 (126- 131 (125-
0.40
in the study. (mEq/l) 143) 140)
Serum potassium
4.2 (3.7-5.2) 4 (3.5-4.5) 0.50
Patients aged < 18 years, those with pregnancy, Acute (mEq/l)
kidney injury (increase in serum creatinine > 0.3 mg/dl Blood urea
5.6 (2.3-9) 4.8 (3-8) 0.18
in 48 hours) without any improvement in past 24 hours, (µmol/l)
or otherwise expected to necessitate dialysis within 48 Creatinine
74 (30-99) 74 (50-99) 0.94
hours in opinion of treating physician, Chronic kidney (µmol/l)
disease, hepatic encephalopathy, active UGI bleed, Total Bilirubin
77 (21-131) 80 (33-178) 0.83
spontaneous bacterial peritonitis (SBP), pre-treatment (mmol/l)
sodium <125 mEq/L, any previous hypersensitivity to ALT ( U/L) 86 (11-207) 55 (14-127) 0.08
albumin or furosemide and those who didn’t give consent AST ( U/L) 142 (21-399) 127 (26-255) 0.68
were excluded. ALP ( U/L) 229 (58-453) 219 (80-460)
Patients in Infusion Group received furosemide infusion GGT ( U/L) 97 (24-294) 105 (19-248) 0.77
at 2 mg/hour and albumin 2g/hour for 3 days while Serum albumin
24 (19-30) 24 (18-29) 0.73
(g/l)
patients in Bolus Therapy Group received similar
cumulative dosage divided in boluses (furosemide 40mg INR 1.8 (0.9-3.3) 1.7 (1.2-2.6) 0.49
twice a day and albumin 20g BD for 3 days). Patients were USG abdomen
assessed for diuresis and hemodynamic stability (systolic Moderate ascites 12 (80) 9 (60) 0.82
Severe ascites 3 (20) 6 (40)
BP and urine output at 24 hours). Urine sodium (UNa),
MELD score 19 (6-37) 18 (9-23) 0.42
Abdominal girth (AG), Body weight (BW), systolic BP and
urine output were assessed at 72 hours. We compared MELD-Na score 21 (6-38) 21 (13-30) 0.90
urinary sodium (UNa), Abdominal girth and body weight CTP score
before and after 72 hours of initiating therapy in the two B 8 (53) 5 (33)
C 7 (47) 10 (67)
groups for measurement of diuresis.
Urinary Sodium
41 (20-69) 35 (17-66) 0.28
(UNa) in mEq/L
Statistical analysis was performed using IBM SPSS
(Statistical Package for Social Science) software. Urinary output 1080 (500- 983 (600-
0.93
in ml 2000) 1800)
Descriptive statistics were expressed as mean (range)
or number (%). Comparison of pre-treatment and post- Abdominal girth
92 ( 78-113) 96 (76-117) 0.33
in cm
treatment variables was done using paired samples
Body weight in kg 61 (45-88) 60 (40-85) 0.88
t-tests. Ninety-five percent confidence intervals were
used in all analyses. Systolic Blood
Pressure 103 (90-130) 105 (90-130) 0.72
(mm hg)
RESULTS
Patients were treated with either boluses of furosemide
A total of 30 patients admitted in medical wards with the
234 JNHRC Vol. 18 No. 2 Issue 47 Apr - Jun 2020
Slow Infusion versus Bolus Doses of Albumin and Furosemide Infusion to Mobilize Refractory Ascites in Decompensated Chronic Liver Disease
and albumin or with infusions of furosemide (2mg/h) and after 72 hours were compared (Table 3).
albumin(2g/h) for 72 hours.
Table 2. Table showing comparison of characteristics
of the patients at initiation of therapy and 72 hours of
therapy in the two groups – Bolus group and Infusion
group.
Variables Bolus Group Infusion Group (N
(N=15) =15)
0 hour 72 hours 0 hour 72 hours
Urinary sodium 41 (20- 50 (24- 35 (17- 70 (18-
(UNa) in mEq/l 69) 88) 66) 145)
Urinary output 1080 1426 983 1450 Figure 2. Bar diagram showing comparison of urine
in ml (500- (800- (600- (1000-
2000) 2700) 1800) 2500) output after 24 and 72 hours of therapy.
Abdominal 92 (78- 89 (76- 96 (76- 90 (73- There was no incidence of hemodynamic instability in
girth in cm 113) 109) 117) 111)
both the group during the period of therapy. There were
Body weight 61 (45- 58 (44- 60 (40- 57 (35- three events of acute kidney injury seen after third day
in Kg 88) 85) 85) 80)
of therapy in bolus group (serum creatinine was seen to
Systolic BP in 103 (90- 100 (80- 105 (90- 101 (90- increase by > 50% of baseline after 72 hours of therapy).
mmHg 130) 130) 130) 134)
The mean urinary sodium excretion increment after 72 Table 3.Table showing comparison of mean difference
hours of therapy in the Infusion group (35.2 mEq/L) was in characteristics values at 72 hours of therapy from
baseline in two groups.
significantly higher (p=0.004) than Bolus group (16.6
mEq/L). Variables Bolus group Infusion P
(N=15) group (N=15) value
Increase in Urinary 16.60 35.20 0.004
Sodium (UNa) in
mEq/l
Increase in Urine 243 483 <0.001
output in ml
Decrease in 3.0 6.1 <0.001
Abdominal girth
(AG) in cm
Decrease in body 2.86 5.53 <0.001
weight (BW) in kg
Figure 1. Bar diagram showing comparison of urinary DISCUSSION
sodium excretion.
In our study, patients receiving infusions of albumin and
The mean increment in urine output at 24 and 72 hours furosemide over a period of 3 days showed a significantly
in Bolus group was 140 ml and 250 ml respectively. In better diuresis and natriuresis (p = 0.004; p < 0.001) as
Infusion group, mean urine output increment at 24 compared to bolus doses. Infusion therapy also resulted
and 72 hours was 243 and 483 ml respectively. There in a significant decrement in abdominal circumference
was significantly higher urine output in Infusion group and body weight (p< 0.001; p <0.001) than bolus doses.
compared to Bolus group at both 24 and 72 hours of
initiation of therapy (p<0.001; p<0.001). Among the several complications of chronic liver
disease (CLD), ascites is the most common. Due to
There was significantly higher decrement in abdominal altered hemodynamics, splanchnic vasodilation and
circumference at 72 hours in Infusion group as compared hyperdynamic state, decompensated CLD patients usually
to bolus group (6.1 cm vs. 3.0 cm, p <0.001). Also, have blood pressure in the lower range. Decompensated
significantly more decrement in weight in Infusion group CLD is a state of chronic inflammation with increased
than bolus group after 72 hours of therapy (2.86 kg vs. circulating levels of pro-inflammatory cytokine and
5.5 kg, p<0.001) was noted. chemokine.16 These pro-inflammatory markers along
with certain bacterial products attach with receptors
The mean of their urine output, abdominal girth, body of immune cells that once activated, release pro-
weight and urinary sodium at initiation of therapy and inflammatory molecules, along with reactive oxygen and
JNHRC Vol. 18 No. 2 Issue 47 Apr - Jun 2020 235
Slow Infusion versus Bolus Doses of Albumin and Furosemide Infusion to Mobilize Refractory Ascites in Decompensated Chronic Liver Disease
nitrogen species. This series of events contributes to the therapy (88.4% vs 66%, p =0.001).20
development of circulatory dysfunction and, along with
it, promotes the development of multi- organ failure.17 Standard medical therapy for ascites in decompensated
CLD is often associated with complications like
Due to the associated complications and limiting electrolyte imbalance (hyponatremia, hypokalemia, and
factors associated with bolus therapy of diuretics, there hypomagnesaemia), hepatic encephalopathy and renal
has been recent advocacy in the literature about the failure.21 Three patients in the bolus group in our study
use of infusions of furosemide and albumin. This can also developed acute kidney injury. No such event was
overcome the limitations of bolus use of furosemide seen in the infusion group.
and albumin, while at the same time improving diuresis
and natriuresis.10,11,15,18 It is more so useful in cases A review article by Elwell et. al states that the
of refractory ascites where, there can be diuretic combination of furosemide and albumin may remain a
resistance. The causes of diuretic resistance include safe therapeutic option that provides clinical benefit
poor adherence to drug therapy or dietary sodium for the hypo-albuminemic patient with recalcitrant
restriction, pharmacokinetic issues, and compensatory edema or ascites.6 The results of this study corroborated
increases in sodium reabsorption at nephron sites that with the findings from other studies done on albumin
are not blocked by the diuretic.19 and furosemide infusion. However, this study was not
blinded. So, for robust analysis, more strict and blinded
Studies with slow infusion of albumin and furosemide study with placebo control would have been a better
infusion over bolus infusion in decompensated chronic study design. Also, the sample size of our study was
liver disease, have initially come up with encouraging small, so studies with larger study population would be
results in regards to mobilizing ascites, overcoming required to substantiate our result.
diuretic resistance and improving hemodynamic
stability.10,11,18 Major advantages of infusions of albumin CONCLUSIONS
and furosemide are postulated as the improved
Our study showed continuous infusion of furosemide
hemodynamic stability, where the drugs can even be
and albumin resulted in better natriuresis, higher
used in patients with low BP (SBP<90 mm hg) which
urine output, increased decrement in abdominal
is the usual range in patients of decompensated CLD.
circumference and body weight without development
Post-diuretic sodium retention can also be overcome by
of any side effects proving it to be a potential safer
continuous infusion.
and effective therapeutic option in management of
Few studies comparing albumin and furosemide infusions refractory ascites.
and terlipressin with standard medical therapy are
available. In a study, by Pande et. al (n=41), marked
REFERENCES
improvement in urine output, urinary sodium excretion 1. Ginés P, Quintero E, Arroyo V, Terés J, Bruguera M,
and weight loss was observed with continuous infusions Rimola A, et al. Compensated cirrhosis: natural history
of albumin and furosemide.10 In our study also continuous and prognostic factors. Hepatology. 1987;7(1):122-8.
infusion group showed marked improvement, in terms [DOI]
of urine output, urinary sodium excretion, weight loss
and reduction in abdominal girth, without any significant 2. Spahr L, Villeneuve J-P, Tran HK, Pomier-Layrargues
side effect in that group. G. Furosemide-induced natriuresis as a test to identify
cirrhotic patients with refractory ascites. Hepatology.
In another study by Pande et. al (n=70), although slow 2001;33(1):28-31. [DOI]
infusions of albumin and furosemide was seen to be safe
3. Moore K, Wong F, Gines P, Bernardi M, Ochs A, Salerno
and effective, 51 among the 70 patients needed addition
of terlipressin in the regimen.11 In our study we did not
F, et al. The management of ascites in cirrhosis: Report
add terlipressin to the regimen. In another study by on the consensus conference of the International Ascites
the same author (n=84), addition of noradrenaline and Club. Hepatology. 2003;38(1):258-66. [DOI]
terlipressin to infusions of albumin and furosemide was 4. Arroyo V, Ginès P, Gerbes AL, Dudley FJ, Gentilini P, Laffi
found to be non-inferior to terlipressin plus infusions G, et al. Definition and diagnostic criteria of refractory
of albumin and furosemide in patients with acute-on- ascites and hepatorenal syndrome in cirrhosis. Hepatology.
chronic liver failure (ACLF).19 Another study in patients 1996;23(1):164-76.[DOI]
with ACLF (n=240) showed significantly higher 28 day
survival in patients treated with infusions of albumin and 5. Salerno F, Borroni G, Moser P, Badalamenti S, Cassarà
furosemide than those treated with standard medical L, Maggi A, et al. Survival and prognostic factors of
cirrhotic patients with ascites: a study of 134 outpatients.
236 JNHRC Vol. 18 No. 2 Issue 47 Apr - Jun 2020
Slow Infusion versus Bolus Doses of Albumin and Furosemide Infusion to Mobilize Refractory Ascites in Decompensated Chronic Liver Disease
Am J Gastroenterol. 1993;88(4):514-9. PMID: 8470631 15. Alqahtani F, Koulouridis I, Susantitaphong P, Dahal K,
[PubMed] Jaber BL. A meta-analysis of continuous vs intermittent
infusion of loop diuretics in hospitalized patients. J Crit
6. Elwell RJ, Spencer AP, Eisele G. Combined furosemide and
Care. 2014;29(1):10-7. doi: 10.1016/j.jcrc.2013.03.015.
human albumin treatment for diuretic-resistant edema.
PMID: 23683555 [PubMed]
Ann Pharmacother. 2003;37(5):695-700. [DOI]
16. Clària J, Stauber RE, Coenraad MJ, Moreau R, Jalan R,
7. Gentilini P, Casini-Raggi V, Di Fiore G, Romanelli RG,
Pavesi M, et al. Systemic inflammation in decompensated
Buzzelli G, Pinzani M, et al. Albumin improves the
cirrhosis: characterization and role in acute‐on‐ chronic
response to diuretics in patients with cirrhosis and ascites:
liver failure. Hepatology. 2016;64(4):1249-64. PMID:
results of a randomized, controlled trial. J Hepatol.
27483394 [DOI] [PubMed]
1999;30(4):639-45.[DOI]
17. Bernardi M, Moreau R, Angeli P, Schnabl B, Arroyo
8. Phakdeekitcharoen B, Boonyawat K.The added-up albumin
V. Mechanisms of decompensation and organ failure in
enhances the diuretic effect of furosemide in patients with
cirrhosis: From peripheral arterial vasodilation to systemic
hypoalbuminemic chronic kidney disease: a randomized
inflammation hypothesis. J Hepatol. 2015;63(5):1272-84.
controlled study. BMC Nephrol. 2012;13(1):92. [DOI]
PMID: 26192220 [DOI] [PubMed]
9. European Association for the Study of the Liver. EASL
18. Pandey G, Kumar A, Durgappa M, Singh A, Nehra A, Vp A,
clinical practice guidelines on the management of ascites,
et al. Non inferiority of combination of slow continuous
spontaneous bacterial peritonitis, and hepatorenal
albumin, furosemide with low dose terlipressin with
syndrome in cirrhosis. J Hepatol. 2010;53(3):397-417.
noradrenaaline infusion in ACLF patients in comparison
[DOI]
to slow continuous albumin, furosemide and terlipressin. J
10. Pande G, Kumar K, Nayak H, Mohindra S, Saraswat V. Slow, Hepatol. 2018;68:S105. [DOI]
continuous low-dose albumin and furosemide infusion
19. Hoorn EJ, Ellison DH. Diuretic Resistance. Am J Kidney
(SCLAFI) mobilizes large ascites safely in decompensated
Dis. 2017;69(1):136-142. [DOI]
liver cirrhosis. J Clin Exp Hepatol. 2015;5:S43. [DOI]
20. Pandey G, Sharma A, Nehra A, Kumar K, Mohindra S,
11. Pandey G, Kumar K, Krishna VP, Sharma PN, Kumar A,
Ghoshal UC, et al. Slow infusion of furosemide and albumin
Nayak HK, et al. Slow, continuous low-dose albumin and
with or without terlipressin in acute on chronic liver
furosemide infusion (SCLAFI) with/without terlipressin
failure patients with organ failure (s): Safety and efficacy
mobilizes refractory ascites safely in decompensated liver
in ascites mobilization and effect on 28 day survival. J Clin
cirrhosis. J Clin Exp Hepatol. 2017;7:S69.[DOI]
Exp Hepatol. 2017;7:S6. [DOI]
12. Chalasani N, Gorski JC, Horlander JC Sr, Craven R, Hoen
21. Angeli P, Bernardi M, Villanueva C, Francoz C, Mookerjee
H, Maya J, et al. Effects of albumin/furosemide mixtures
RP, Trebicka J, et al. Corrigendum to “EASL Clinical
on responses to furosemide in hypoalbuminemic patients.
Practice Guidelines for the management of patients with
J Am Soc Nephrol. 2001;12(5):1010-6. PMID: 11316860
decompensated cirrhosis”[J Hepatol 69 (2018) 406–460].
[PubMed]
J Hepatol. 2018;69(5):1207.[DOI]
13. Wilcox CS, Mitch WE, Kelly RA, Skorecki K, Meyer TW,
Friedman PA, et al. Response of the kidney to furosemide:
I. Effects of salt intake and renal compensation. J Lab Clin
Med. 1983;102(3):450-8. PMID: 6886524 [PubMed]
14. Rudy DW, Voelker JR, Greene PK, Esparza FA, Brater DC.
Loop diuretics for chronic renal insufficiency: a continuous
infusion is more efficacious than bolus therapy. Ann Intern
Med. 1991;115(5):360-6. PMID: 1863026 [PubMed]
JNHRC Vol. 18 No. 2 Issue 47 Apr - Jun 2020 237
You might also like
- Idei GeneraleDocument7 pagesIdei GeneraleGeorgiana FrăţilăNo ratings yet
- Furosemid With AlbuminDocument10 pagesFurosemid With Albuminale_rhdNo ratings yet
- Atorvastatin Combined With Poly Unsaturated Fatty Acid Confers Better Omprovement of Dyslipidemia and Endothelium FunctionDocument6 pagesAtorvastatin Combined With Poly Unsaturated Fatty Acid Confers Better Omprovement of Dyslipidemia and Endothelium FunctionShinichi Ferry RoferdiNo ratings yet
- JURNALDocument5 pagesJURNALMita Restuning AjiNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Jurnal Tatalaksana 3Document5 pagesJurnal Tatalaksana 3winny kartikaNo ratings yet
- GOUT UloricPlaceboAllo28wkDocument9 pagesGOUT UloricPlaceboAllo28wkJay SejpalNo ratings yet
- Alimentary Pharmacology & TherapeuticsDocument12 pagesAlimentary Pharmacology & TherapeuticsMoy VillanuevaNo ratings yet
- The Comparison Between The Effect of AtorvastatinDocument5 pagesThe Comparison Between The Effect of AtorvastatinAiman ShoiabNo ratings yet
- Terlipressin Effect On Hepato-Renal Syndrome, Updated Meta-Analysis of Randomized Controlled TrialsDocument6 pagesTerlipressin Effect On Hepato-Renal Syndrome, Updated Meta-Analysis of Randomized Controlled TrialsGASPAR ARRIAGADA GONZALEZNo ratings yet
- A Systematic Review and Meta-Analysis of Metolazone Compared To Chlorothiazide For Treatment of Acute Decompensated Heart FailureDocument12 pagesA Systematic Review and Meta-Analysis of Metolazone Compared To Chlorothiazide For Treatment of Acute Decompensated Heart FailureAlejandro Lara LópezNo ratings yet
- Aqua AhfDocument8 pagesAqua AhfRinzyNo ratings yet
- Turkjmedsci-50-354 PubmedDocument6 pagesTurkjmedsci-50-354 PubmedRizka Uda'aNo ratings yet
- Jpkedokterangg110218 PDFDocument5 pagesJpkedokterangg110218 PDFFasya ShidqiNo ratings yet
- Current Pharmacologic Therapies For Hepatorenal Syndrome Acute KidneyDocument8 pagesCurrent Pharmacologic Therapies For Hepatorenal Syndrome Acute KidneyEdgar QuezadaNo ratings yet
- J Nucl Med-1992-Lee-739-43Document6 pagesJ Nucl Med-1992-Lee-739-43felixwinataNo ratings yet
- Terapia Combinada en Obeso 1Document6 pagesTerapia Combinada en Obeso 1Diana LizNo ratings yet
- Valsartan (Hedaya) 320 MGDocument16 pagesValsartan (Hedaya) 320 MGAntonio SanchezNo ratings yet
- 述评 Human Albumin Infusion Strategy in Liver Cirrhosis Liberal or RestrictiveDocument3 pages述评 Human Albumin Infusion Strategy in Liver Cirrhosis Liberal or Restrictive倪沁赟No ratings yet
- Wa0013Document4 pagesWa0013Sastra WijayaNo ratings yet
- Rai2016 PDFDocument25 pagesRai2016 PDFPrasanna BhatNo ratings yet
- Seminars in Arthritis and Rheumatism: X Xfernando Perez-Ruiz XX, X Xnicola Dalbeth XXDocument11 pagesSeminars in Arthritis and Rheumatism: X Xfernando Perez-Ruiz XX, X Xnicola Dalbeth XXambmarNo ratings yet
- Upper GI BleedsDocument17 pagesUpper GI BleedsSharayu DhobleNo ratings yet
- Non-Linear PharmacokineticsDocument6 pagesNon-Linear PharmacokineticsaristapasisingiNo ratings yet
- Diuretici U Bubrežnoj InsuficijencijiDocument5 pagesDiuretici U Bubrežnoj InsuficijencijiBastaDaninocNo ratings yet
- Alfa Blocker Vs Alfa Blocker + 5 Alfa ReductaseDocument5 pagesAlfa Blocker Vs Alfa Blocker + 5 Alfa Reductasemonia agni wiyatamiNo ratings yet
- Link To Publication in University of Groningen/UMCG Research DatabaseDocument21 pagesLink To Publication in University of Groningen/UMCG Research DatabaseKukuh Prasetyo WibowoNo ratings yet
- CLC 4960230910Document7 pagesCLC 4960230910walnut21No ratings yet
- Fluid Management of Neurosurgical Patient, Recent Update: Taeha. RyuDocument73 pagesFluid Management of Neurosurgical Patient, Recent Update: Taeha. RyuMada Oktav CakradwipaNo ratings yet
- Effectiveness and Safety of Low-Dose Pravastatin and Squalene, Alone and in Combination, in Elderly Patients With HypercholesterolemiaDocument6 pagesEffectiveness and Safety of Low-Dose Pravastatin and Squalene, Alone and in Combination, in Elderly Patients With HypercholesterolemiaeduardochocincoNo ratings yet
- Articulo PatoDocument3 pagesArticulo PatoElizabeth Orellana PisconteNo ratings yet
- El Indice Predicto de Hemorragia DigestivaDocument1 pageEl Indice Predicto de Hemorragia DigestivaOlga SamameNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Cefotaxime Renal ImpairmentDocument6 pagesCefotaxime Renal ImpairmentChristine LilyanaNo ratings yet
- qt753782f6 NosplashDocument4 pagesqt753782f6 NosplashGeorge E. FergusonNo ratings yet
- Loop Diuretic Resistance Complicating Acute Heart FailureDocument13 pagesLoop Diuretic Resistance Complicating Acute Heart Failuredhimas satriaNo ratings yet
- Research/Practice ReportsDocument4 pagesResearch/Practice ReportsDaniela HernandezNo ratings yet
- Analysis of Biochemical Markers Related To Fatty Liver PatientsDocument4 pagesAnalysis of Biochemical Markers Related To Fatty Liver PatientsZhuly DiazNo ratings yet
- Tolvaptan PDFDocument8 pagesTolvaptan PDFDaniel Rico FuentesNo ratings yet
- Curcumin LNDocument8 pagesCurcumin LNHend MahranNo ratings yet
- Effects On Serum Uric Acid by Difference of The Renal Protective Effects With Atorvastatin and Rosuvastatin in Chronic Kidney Disease PatientsDocument6 pagesEffects On Serum Uric Acid by Difference of The Renal Protective Effects With Atorvastatin and Rosuvastatin in Chronic Kidney Disease PatientsAnonymous ZbhBxeEVNo ratings yet
- 2 Article Presentation (Chlorthalidone)Document26 pages2 Article Presentation (Chlorthalidone)Palak GuptaNo ratings yet
- Baltes 2001Document9 pagesBaltes 2001Brahma Hakim Yuanda HutabaratNo ratings yet
- OmprazoleDocument8 pagesOmprazoleIndah Whidysenandri SitepuNo ratings yet
- AKI TreatDocument2 pagesAKI TreatNama ManaNo ratings yet
- Anethum Graveolens and Hyperlipidemia: A Randomized Clinical TrialDocument13 pagesAnethum Graveolens and Hyperlipidemia: A Randomized Clinical TrialYuliantikha Nurul QomariahNo ratings yet
- Effects of Correction of Metabolic Acidosis On Blood Urea and Bone Metabolism in Patients With Mild To Moderate Chronic Kidney Disease A ProspectiveDocument7 pagesEffects of Correction of Metabolic Acidosis On Blood Urea and Bone Metabolism in Patients With Mild To Moderate Chronic Kidney Disease A ProspectiveHigh LowNo ratings yet
- StatinDocument15 pagesStatindrsandiptaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderFrom EverandComplementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderNo ratings yet
- Bioequivalence of Two Brands of Valsartan 80 MG Coated Breakable Tablets in 15 Healthy Algerian Volunteers: A Pilot StudyDocument7 pagesBioequivalence of Two Brands of Valsartan 80 MG Coated Breakable Tablets in 15 Healthy Algerian Volunteers: A Pilot StudySabrina JonesNo ratings yet
- The Effect of Intraoperative Alkali Treatment On Recovery From Atracurium-Induced Neuromuscular Blockade in Renal Transplantation: A Randomized TrialDocument4 pagesThe Effect of Intraoperative Alkali Treatment On Recovery From Atracurium-Induced Neuromuscular Blockade in Renal Transplantation: A Randomized Trialakhirul_733759154No ratings yet
- 5.furosemide in Critically Ill Sheraton 2018Document43 pages5.furosemide in Critically Ill Sheraton 2018MuhammadHazmiAnzhariNo ratings yet
- Acute Kidney InjuryDocument102 pagesAcute Kidney InjuryMichelleValeriaFredy100% (2)
- Daprodustat For The Treatment of Anemia in PatientsDocument16 pagesDaprodustat For The Treatment of Anemia in PatientsVstreamhdNo ratings yet
- 11-HEPATOLO1G99Y1 1 3llol-1105.Document5 pages11-HEPATOLO1G99Y1 1 3llol-1105.Mohammad ElghazalyNo ratings yet
- The SPARK Study: A Phase II Randomized Blinded Controlled Trial of The Effect of Furosemide in Critically Ill Patients With Early Acute Kidney InjuryDocument10 pagesThe SPARK Study: A Phase II Randomized Blinded Controlled Trial of The Effect of Furosemide in Critically Ill Patients With Early Acute Kidney InjuryGanda SilitongaNo ratings yet
- Dumbre - 2012 - Effect of Chandraprabha Vati in Experimental Prostatic Hyperplasia and Inflammation in RatsDocument3 pagesDumbre - 2012 - Effect of Chandraprabha Vati in Experimental Prostatic Hyperplasia and Inflammation in RatsHendra Wana Nur'aminNo ratings yet
- Annals of Medicine and SurgeryDocument4 pagesAnnals of Medicine and SurgeryRadu MiricaNo ratings yet
- Gastrointestinal Motility Disorders: An Update: Brian E. Lacy Kirsten WeiserDocument15 pagesGastrointestinal Motility Disorders: An Update: Brian E. Lacy Kirsten WeiserTri Anna FitrianiNo ratings yet
- Rundown Simposium bite up II final 23-4-24Document5 pagesRundown Simposium bite up II final 23-4-24sibon M amrilNo ratings yet
- Tungadi - 2018 - Transdermal Delivery of Snakehead Fish (Ophiocephalus Striatus) Nanoemulgel Containing Hydrophobic Powder For Burn WoundDocument12 pagesTungadi - 2018 - Transdermal Delivery of Snakehead Fish (Ophiocephalus Striatus) Nanoemulgel Containing Hydrophobic Powder For Burn Woundsibon M amrilNo ratings yet
- Standar Formularium 2019Document21 pagesStandar Formularium 2019sibon M amrilNo ratings yet
- Univ. YPIBDocument2 pagesUniv. YPIBsibon M amrilNo ratings yet
- Adhitya Pradana 22010110120064 Bab 8 Kti PDFDocument28 pagesAdhitya Pradana 22010110120064 Bab 8 Kti PDFsibon M amrilNo ratings yet
- Proposal VaksinDocument35 pagesProposal Vaksinsibon M amrilNo ratings yet
- The Role of Hatcheries in The Success or Failure of The Indian Shrimp IndustryDocument37 pagesThe Role of Hatcheries in The Success or Failure of The Indian Shrimp IndustryGlen ChoNo ratings yet
- M265 Lec 17 - Specimen Collection Handling For The Microbiology Laboratory PDFDocument17 pagesM265 Lec 17 - Specimen Collection Handling For The Microbiology Laboratory PDFHãnëën Twalbeh100% (2)
- Milno Et AlDocument9 pagesMilno Et AlLara SilveiraNo ratings yet
- Interindividual Differences in Caffeine Metabolism and Factors Driving Caffeine ConsumptionDocument28 pagesInterindividual Differences in Caffeine Metabolism and Factors Driving Caffeine ConsumptionSeema YadavNo ratings yet
- Sugar Types On Ethanol ProductionDocument5 pagesSugar Types On Ethanol ProductionGabriella NaomiNo ratings yet
- Virtual Water Testing LabsDocument3 pagesVirtual Water Testing Labsapi-235669157No ratings yet
- TheLowCortisolLifestyle PDFDocument51 pagesTheLowCortisolLifestyle PDFthomas100% (2)
- 2022 SJ L4 NovemberDocument52 pages2022 SJ L4 NovemberbelindanNo ratings yet
- Definition of Basic Terms in LogicDocument52 pagesDefinition of Basic Terms in LogicAlnour Kilas100% (1)
- MLS 044 - Clinical Bacteriology (LABORATORY) Staining TechniquesDocument3 pagesMLS 044 - Clinical Bacteriology (LABORATORY) Staining Techniqueslorraine del rosarioNo ratings yet
- Sylvain Vauthey Et Al - Molecular Self-Assembly of Surfactant-Like Peptides To Form Nanotubes and NanovesiclesDocument6 pagesSylvain Vauthey Et Al - Molecular Self-Assembly of Surfactant-Like Peptides To Form Nanotubes and NanovesiclesGmewop30mNo ratings yet
- Chapter 11: Parenteral Administration: Intradermal, Subcutaneous, and Intramuscular Routes Test BankDocument7 pagesChapter 11: Parenteral Administration: Intradermal, Subcutaneous, and Intramuscular Routes Test BankLuna TunaNo ratings yet
- Marsupials: Preєєosdcptj KDocument16 pagesMarsupials: Preєєosdcptj KGeorge V. GrantNo ratings yet
- Beltran-Garcia2021 Article NitrogenFertilizationAndStressDocument12 pagesBeltran-Garcia2021 Article NitrogenFertilizationAndStressLALUKISNo ratings yet
- Vedantu Ncert PDF SheetDocument13 pagesVedantu Ncert PDF SheetKshreeNo ratings yet
- Parasitism, Commensalism, and Mutualism: Exploring The Many Shades of SymbiosesDocument9 pagesParasitism, Commensalism, and Mutualism: Exploring The Many Shades of SymbiosesBen OusoNo ratings yet
- Intergumentary SystemDocument36 pagesIntergumentary SystemKudzai MashayaNo ratings yet
- PDF 100 HypertrophyDocument110 pagesPDF 100 Hypertrophyroyvillafranca94% (16)
- Eupatorium Leonardii - Brittonia 2012Document8 pagesEupatorium Leonardii - Brittonia 2012Richelle FigueroaNo ratings yet
- Imobilisasi Lipase Pada Kitosan Serbuk Dengan MetoDocument16 pagesImobilisasi Lipase Pada Kitosan Serbuk Dengan MetoAulia RahmiNo ratings yet
- Forensic Mycology - The Use of Fungi in Criminal Investigations.Document11 pagesForensic Mycology - The Use of Fungi in Criminal Investigations.Carlos MolinaNo ratings yet
- CANITA - 3PTC - Piaget - S Stages of Cognitive DevelopmentDocument14 pagesCANITA - 3PTC - Piaget - S Stages of Cognitive Developmentim. EliasNo ratings yet
- Is 1068 1993 PDFDocument21 pagesIs 1068 1993 PDFAnonymous YRQknJ100% (1)
- HerbariumDocument6 pagesHerbariumartheha salyaNo ratings yet
- What Is AlbinismDocument6 pagesWhat Is AlbinismOsi Aulia SiwiNo ratings yet
- The Role of Bismuth in The SOHIO ProcessDocument39 pagesThe Role of Bismuth in The SOHIO ProcessMarnel Roy MayorNo ratings yet
- Absorption of Digested FoodDocument2 pagesAbsorption of Digested FoodAmmar SyahmiNo ratings yet
- Art Integrated Project: Topic-GeneticsDocument10 pagesArt Integrated Project: Topic-GeneticsShifa SiddiquiNo ratings yet
- Class 12 Biology Chapter 14 NotesDocument23 pagesClass 12 Biology Chapter 14 NotesSyed Atta Ur RahmanNo ratings yet
- Buffer in Biological & Pharmaceutical SystemsDocument28 pagesBuffer in Biological & Pharmaceutical Systemshamam salih badriNo ratings yet