Professional Documents
Culture Documents
Alfa Blocker Vs Alfa Blocker + 5 Alfa Reductase
Uploaded by
monia agni wiyatamiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Alfa Blocker Vs Alfa Blocker + 5 Alfa Reductase
Uploaded by
monia agni wiyatamiCopyright:
Available Formats
www.kjurology.
org
http://dx.doi.org/10.4111/kju.2012.53.4.248
Voiding Dysfunction
α-Blocker Monotherapy and α-Blocker Plus 5-Alpha-Reductase
Inhibitor Combination Treatment in Benign Prostatic Hyperplasia;
10 Years’ Long-Term Results
Teak Jun Shin, Chun Il Kim, Choal Hee Park, Byung Hoon Kim, Young Kee Kwon
Department of Urology, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
Purpose: We compared the effects of alpha-adrenergic receptor blocker (α-blocker) mon- Article History:
otherapy with those of combination therapy with α-blocker and 5-alpha-reductase in- received 11 April, 2011
accepted 21 November, 2011
hibitor (5-ARI) on benign prostatic hyperplasia (BPH) progression for over 10 years.
Materials and Methods: A total of 620 patients with BPH who received α-blocker mono-
therapy (α-blocker group, n=368) or combination therapy (combination group, n=252)
as their initial treatment were enrolled from January 1989 to June 2000. The incidences
of acute urinary retention (AUR) and BPH-related surgery were compared between the
two groups. Incidences stratified by follow-up period, prostate-specific antigen (PSA),
and prostate volume (PV) were compared between the two groups.
Results: The incidence of AUR was 13.6% (50/368) in the α-blocker group and 2.8%
(7/252) in the combination group (p<0.001). A total of 8.4% (31/368) and 3.2% (8/252)
of patients underwent BPH-related surgery in the α-blocker and combination groups,
respectively (p=0.008). According to the follow-up period, the incidence of AUR was sig-
nificantly decreased in combination group. However, the incidence of BPH-related sur-
gery was significantly reduced after 7 years of combination therapy. Cutoff levels of
PSA and PV for reducing the incidences of AUR and BPH-related surgery were 2.0 ng/ml
and 35 g, respectively (p<0.001).
Conclusions: Long-term combination therapy with α-blocker and 5-ARI can suppress
the progression of BPH more efficiently than α-blocker monotherapy. For patients with
BPH with PSA >2.0 ng/ml or PV >35 ml, combination therapy promises a better effect Corresponding Author:
Chun Il Kim
for reducing the risk of BPH progression.
Department of Urology, Dongsan
Medical Center, Keimyung University
Key Words: Adrenergic alpha-1 receptor antagonists; 5-alpha reductase inhibitors;
School of Medicine, 56 Dalseong-ro,
Prostatic hyperplasia Jung-gu, Daegu 700-712, Korea
TEL: +82-53-250-7646
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial
License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, FAX: +82-53-250-7643
distribution, and reproduction in any medium, provided the original work is properly cited. E-mail: cikim@dsmc.or.kr
INTRODUCTION many studies, including a Veterans Affairs Cooperative
study and a Prospective European Doxazosin and Combi-
Benign prostatic hyperplasia (BPH) is a progressive dis- nation Therapy Trial study, that reported no significant
ease that can cause acute urinary retention (AUR) and that difference in short-term effects on the treatment of BPH be-
leads to BPH-related surgery [1-3]. At present, alpha-adre- tween α-blocker monotherapy and the combination ther-
nergic receptor blockers (α-blockers) and 5-alpha-reduc- apy with an α-blocker and 5-ARI [4,5]. In contrast to these
tase inhibitors (5-ARIs) are used in the medical therapy of reports, the Medical Therapy of Prostatic Symptoms
BPH. Most doctors in the 1990s, however, preferred α-bloc- (MTOPS) study reported that during 4.5 years of follow-up,
ker monotherapy to the combination therapy of α-blockers the progression of BPH, the worsening of symptoms, and
and 5-ARIs. This preference was based on the results of BPH-related surgeries decreased more in the doxazosin
Korean Journal of Urology
Ⓒ The Korean Urological Association, 2012 248 Korean J Urol 2012;53:248-252
α-Blocker Monotherapy vs. 5-ARI Combination Treatment 249
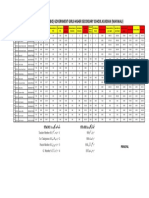
TABLE 1. Incidence of AUR and BPH-related surgery in the α-blocker monotherapy and combination treatment groups
No. of patients (%)
Event Parameter α-blocker group Combination group p-value
n=358 n=252
AUR All 50 (13.6) 7 (2.8) <0.001
PSA≤2.0 ng/ml 13 (6.0) 2 (1.7) 0.065
PSA>2.0 ng/ml 37 (24.2) 5 (3.8) <0.001
PV≤35 ml 12 (5.3) 1 (1.0) 0.064
PV>35 ml 38 (27.0) 6 (4.0) <0.001
BPH-related surgery All 31 (8.4) 8 (3.2) 0.008
PSA≤2.0 ng/ml 5 (2.3) 3 (2.6) 0.902
PSA>2.0 ng/ml 26 (17.0) 5 (3.8) <0.001
PV≤35 ml 2 (0.9) 1 (1.0) 0.921
PV>35 ml 29 (20.6) 7 (4.7) <0.001
AUR, acute urinary retention; BPH, benign prostatic hyperplasia; PSA, prostate-specific antigen; PV, prostate volume.
and finasteride combination group than in the doxazosin group, who received combination therapy of α-blocker and
or finasteride monotherapy group [6]. Furthermore, Kim 5-ARI. The incidences of AUR and BPH-related surgeries
et al. [7] reported that the incidences of AUR and BPH-re- were compared between these two groups and also between
lated surgeries in a combination therapy group were sig- patients who were classified by PV and serum PSA level.
nificantly decreased for 6 to 8 years. To calculate PV, transrectal ultrasonography was per-
In the present study, the authors analyzed the long-term formed. The anteroposterior (H) and transverse (W) leng-
effects of α-blocker monotherapy and combination therapy ths were measured from the longest transverse image of
with an α-blocker and 5-ARI in actual clinical studies for the prostate. The horizontal length from the proximal to
over 10 years and examined the incidences of AUR and the distal parts of the prostate in the midline sagittal scan
BPH-related surgeries by prostate volume (PV) and pros- was regarded as the longitudinal (L) length. To calculate
tate-specific antigen (PSA) level. PV, the following equation was used: PV=π/6x HxWxL.
To stratify PSA levels and PV, their relationships with
MATERIALS AND METHODS AUR and BPH-related surgeries were examined by using
receiver operating characteristic (ROC) curves.
This study investigated the medical records of 620 BPH pa-
tients who received medical therapy for at least 1 year be- RESULTS
tween January 1989 and July 2010, retrospectively. This
study excluded patients who were under 40 years of age; Of the 620 patients, 368 belonged to the α-blocker group
those with an International Prostate Symptom Score and 252 to the combination group. In the α-blocker and
(IPSS) of 7 or lower; those whose maximal urinary flow rate combination groups, respectively, the mean age was 64.2
(Qmax) was 15 ml/s or higher; patients who had received years (range, 29 to 91 years) and 64.8 years (range, 40 to
medical treatment for BPH previously; patients who had 89 years) (p=0.470), and the average follow-up period was
received combination medication with anticholinergics; 108.6 months (range, 12 to 216 months) and 113.1 months
patients who had undergone BPH-related surgery, urinary (range, 12 to 170 months) (p=0.206). The PSA levels at the
bladder surgery, urethroplasty, or diathermy; and pa- first visit of the α-blocker group and the combination group
tients who had lower urinary tract symptoms (LUTS) due were 2.2 ng/ml and 2.9 ng/ml (p=0.082), respectively, and
to causes other than BPH. Also excluded were patients who the PVs were 37.5 ml and 42.9 ml (p=0.064), respectively.
had AUR or who had undergone a BPH-related surgery AUR developed in 9.2% (57/620) of the total group: 13.6%
within 12 months after beginning medical treatment and (50/368) in the α-blocker group and 2.8% (7/252) in the com-
patients who were confirmed to have prostate cancer and bination group. Thus, the hazard ratio of the combination
BPH simultaneously. group was lower by 79.4% than that of the α-blocker group
The follow-up period of this study was determined by the (p<0.001) (Table 1, Fig. 1). The incidence of BPH-related
AUR onset date, BPH-related surgery date, or last visit surgeries was 8.4% (31/368) for the α-blocker group and
date in the medical records. For subjects who were not fol- 3.2% (8/252) for the combination group. Thus, the hazard
lowed up, information on the continuation of medical treat- ratio of the combination group was 61.9% lower than that
ment, AUR, or BPH-related surgery was collected via mail of the α-blocker group (p=0.008) (Fig. 2).
or phone surveys. The incidence of BPH-related surgery was 5.4% for the
The patients were divided into the α-blocker group, who α-blocker group and 2.4% for the combination group for up
received α-blocker monotherapy, and the combination to 7 years of follow-up and the difference was not signifi-
Korean J Urol 2012;53:248-252
250 Shin et al
FIG. 1. Cumulative incidences of acute urinary retention (AUR) FIG. 2. Cumulative incidences of benign prostatic hyperplasia
in the α-blocker monotherapy and combination treatment (BPH) related surgery in the α-blocker monotherapy and
groups. combination treatment groups.
cant. For longer periods of follow-up, however, the in- tion therapy for 12 months decreased the American Urolo-
cidence of BPH-related surgery was significantly lower in gical Association symptom score to 6.1 and 6.2, and in-
the combination group. The incidence of AUR was sig- creased Qmax to 2.7 and 3.2, with no significant differences
nificantly lower in the combination group for follow-up pe- between the two therapies [4]. The Prospective European
riods of 2 years or longer. Doxazosin and Combination Therapy Trial reported that
The cutoff level of PSA and PV for the hazards of AUR α-blocker monotherapy and 5-ARI combination therapy in-
and BPH-related surgery were 2.0 ng/ml and 35 ml, creased Qmax to 3.6 and 3.8 ml/s, and decreased IPSS to
respectively. When the PSA level was higher than 2.0 8.3 and 8.5, with no significant differences between the two
ng/ml, the incidence of AUR in the α-blocker and combina- therapies [5]. These studies, however, compared the effects
tion groups was 24.2% (37/153) and 3.8% (5/133), respec- of drug treatment for short periods of 1 year or less and fo-
tively; when the PV was higher than 35 ml, the incidence cused on comparing the changes in LUTS and Qmax rather
of AUR was 27.0% (38/141) and 4.0% (6/150), respectively than on the complications of BPH.
(p<0.001). When the PSA level was higher than 2.0 ng/ml, The effects of 5-ARIs were described better in the Proscar
the incidence of BPH-related surgery in the α-blocker and Long-Term Efficacy and Safety Study [2]. This study used
combination groups was 17.0% (26/153) and 3.8% (5/133), finasteride for 4 years, which decreased PV by 18% com-
respectively; when the PV was higher than 35 ml, the in- pared with the placebo group and decreased the incidences
cidence of BPH-related surgery was 20.6% (29/141) and of AUR and BPH-related surgeries to 57% and 55%,
4.7% (7/150), respectively (p<0.001). respectively. Later, the MTOPS study also reported the ef-
Of the 39 patients who underwent BPH-related sur- fects of treatments with α-blocker and 5-ARI for 4.5 years
geries, 10 received surgeries due to AUR, and the other 29 [6]. Compared with that in the doxazosin group, the AUR
received surgeries due to insufficient efficacy of drug hazard of the combination group decreased by 75%, and the
treatment. hazard of BPH-related surgeries decreased by 64% and
67% in the finasteride monotherapy group and the combi-
DISCUSSION nation therapy group, respectively. The PV increased by
24% in the placebo group and the doxazosin group but de-
BPH can cause various complications, such as AUR, creased by 13% and 16% in the finasteride group and the
BPH-related surgeries, urinary incontinence, and urinary combination group, respectively.
tract infection [8]. Between α-blockers and 5-ARIs, which AUR is not only a serious complication of BPH, but also
are the representative drug treatments for BPH, 5-ARIs an important indication for BPH-related surgery. Among
are being spotlighted in that they can prevent BPH the many causes of AUR, BPH accounts for 50% [9]. The
progression. In the past, however, most studies were skep- PSA level in the serum has shown a close correlation with
tical about the effects of combination therapy with α-block- PV [10]. Roehrborn et al. [11] reported that the risk of AUR
ers and 5-ARIs. The Veterans Affairs Cooperative Study in patients whose PSA level was 3.4 ng/ml or higher was
showed that α-blocker monotherapy and 5-ARI combina- 4 times that of patients whose PSA level was 1.2 ng/ml or
Korean J Urol 2012;53:248-252
α-Blocker Monotherapy vs. 5-ARI Combination Treatment 251
lower. Furthermore, they reported that the risk of AUR in BPH-related surgeries decreased by 77.2% and 77.6%,
the patients whose PV was 57 g or higher was 3.5 times that respectively.
of the patients whose PV was 34 g or lower. Jacobsen et al. The present study was meaningful because it was a
[12] also reported that when PV exceeded 30 g, the AUR in- long-term study of 10 years of actual clinical data rather
cidence increased at least 3 times. The European Associa- than a prospective random contrast study. The incidences
tion of Urology Guidelines strongly recommended drug of AUR and BPH-related surgeries in the BPH patients
treatment with finasteride for patients who have BPH and who received combination therapy with 5-ARI were sig-
serious LUTS and whose PV is greater than 40 g. Bartch nificantly lower than those in the patients who received
et al. [13] suggested that the treatment with 5-ARI would α-blocker monotherapy. These results are similar to those
prevent the progress of potential BPH for patients whose of previous studies and show that combination therapy
serum PSA level is 1.5 ng/ml or higher or whose PV is 30 with 5-ARI is helpful even with long-term treatment of 10
g or greater. To determine the effect of the treatment meth- years.
od, Kaplan et al. [14] divided patients into three groups (PV The data of our study, including PSA change, prostate
smaller than 25 g, 25 to 40 g, or greater than 40 g) for the size change, IPSS change, residual urine change, and flow
results of the MTOPS study. The hazard of BPH pro- rate change, are not enough because the study was retro-
gression of the group whose PV was smaller than 25 g did spective. Thus, our study has limitations concerning abso-
not significantly change between the combination group lute assessment. Therefore, more extensive research is be-
and the doxazosin or finasteride group; however, in the lieved to be necessary in the future.
group whose PV was greater than 25 g, the hazard of BPH
progression of the combination group decreased compared CONCLUSIONS
with that of the doxazosin or finasteride group. Further-
more, the incidence of invasive surgeries in the combina- With the use of actual clinical data, the present study found
tion group decreased by 70% compared with the doxazosin that the combination group that used an α-blocker and a
group. 5-ARI for a long period of 10 years had a decreased hazard
A recent CombAT study set the cutoff level for patients of BPH progression, such as AUR and BPH-related sur-
with a high hazard of disease progression as a serum PSA geries, compared with the α-blocker monotherapy group.
value of 1.5 g/l or higher and a PV of 30 ml or greater [15]. Furthermore, in patients whose PV and serum PSA level
A 4-year study with these patients found that the incidence exceeded 35 g and 2.0 ng/ml, respectively, combination
of BPH progression (IPSS score 4 or higher, AUR, incon- therapy was more effective than monotherapy in decreas-
tinence, relapsing urinary tract infection, or renal in- ing the incidences of AUR and BPH-related surgeries.
adequacy) was 12.6% in the combination group treated
with dutasteride and tamsulosin, 17.8% in the dutasteride CONFLICTS OF INTEREST
group, and 21.5% in the tamsulosin group. In the combina- The authors have nothing to disclose.
tion group, the decrease in the hazard associated with pros-
tate progression was statistically significant. Compared REFERENCES
with that in the tamsulosin group, the AUR hazard,
BPH-related surgeries, and IPSS score of the combination 1. Djavan B, Fong YK, Harik M, Milani S, Reissigl A, Chaudry A,
group decreased by 67.8%, 70.6%, and 41.3%, respectively et al. Longitudinal study of men with mild symptoms of bladder
outlet obstruction treated with watchful waiting for four years.
[16].
Urology 2004;64:1144-8.
The study by Lee et al. [17] that was conducted at 5 medi-
2. McConnell JD, Bruskewitz Z, Walsh P, Andriole G, Lieber M,
cal centers in Korea compared an α-blocker monotherapy Holtgrewe HL, et al. The effect of finasteride on the risk of acute
group and a combination therapy group according to PV, urinary retention and the need for surgical treatment among men
PSA, IPSS, and Qmax. During the 4-year follow-up, the with benign prostatic hyperplasia. N Engl J Med 1998;338:557-
IPSS score of the monotherapy group decreased by 6.1, but 63.
that of the combination group decreased by 11.5, which was 3. Roehrborn CG, McConnell JD, Lieber M, Kaplan S, Geller J,
an improved result. Malek GH, et al. Serum prostate-specific antigen concentration
The present study compared an α-blocker group with a is a powerful predictor of acute urinary retention and need for sur-
combination group: the AUR incidence was 13.6% and gery in men with clinical benign prostatic hyperplasia. PLESS
2.8%, respectively, and the incidence of BPH-related sur- Study Group. Urology 1999;53:473-80.
4. Lepor H, Willford WO, Barry MJ, Brawer MK, Dixon CM,
geries was 8.4% and 3.2%, respectively. The authors did not
Gormley G, et al. The efficacy of terazosin, finasteride, or both in
find significant differences in the length of AUR incidence
benign prostatic hyperplasia. Veterans Affairs Cooperative
between the two groups of patients whose PV was 35 g or Studes Benign Prostatic Hyperplasia Study Group. N Engl J Med
lower and serum PSA level was 2.0 ng/ml or lower. Compa- 1996;335:533-9.
red with that in the α-blocker group, the AUR incidence in 5. Kirby RS, Roehrborn C, Boyle P, Bartsch G, Jardin A, Cary MM,
the combination group decreased by 85.2% and 84.3% in pa- et al. Efficacy and tolerability of doxazosin and finasteride, alone
tients whose PV exceeded 35 g and whose serum PSA level or in combination, in treatment of symptomatic benign prostatic
exceeded 2.0 ng/ml, respectively, and the incidence of hyperplasia: the Prospective European Doxazosin and Combina-
Korean J Urol 2012;53:248-252
252 Shin et al
tion Therapy (PREDICT) trial. Urology 2003;61:119-26. 13. Bartch G, Fitzpaatrick JM, Schalken JA, Isaacs J, Nordling J,
6. McConnell JD, Roehrborn CG, Bautista OM, Andriole GL Jr, Roehrborn CG. Consensus statement: the role of prostate-specific
Dixon CM, Kusek JW, et al. The long-term effect of doxazosin, fi- antigen in managing the patient with benign prostatic hyper-
nasteride and combination therapy on the clinical progression of plasia. BJU Int 2004;93(suppl):27-9.
benign prostatic hyperplasia. N Engl J Med 2003;349:2387-98. 14. Kaplan SA, McConnell JD, Roehrborn CG, Meehan AG, Lee MW,
7. Kim CI, Chang HS, Kim BK, Park CH. Long-term results of medi- Noble WR, et al. Combination therapy with doxazosin and finas-
cal treatment in benign prostatic hyperplasia. Urology 2006;68: teride for benign prostatic hyperplasia in patients with lower uri-
1015-9. nary tract symptoms and a baseline total prostate volume of 25
8. Welch G, Weinger K, Barry MJ. Quality-of-life impact of lower uri- ml or greater. J Urol 2006;175:217-20.
nary tract symptom severity: results from the Health Professio- 15. Roehrborn CG, Siami P, Barkin J, Damiao R, Major-Walker K,
nals Follow-up Study. Urology 2002;59:245-50. Morrill B, et al. The effects of dutasteride, tamsulosin and combi-
9. Berum L, Klarskov P, Munck LK, Nielsen TH, Nordestgaard AG. nation therapy on lower urinary tract symptoms in men with be-
Significance of acute urinary retention due to intravesical ob- nign prostatic hyperplasia and prostatic enlargement: 2-year re-
struction. Scand J Urol Nephrol 1982;16:21-4. sults from the CombAT study. J Urol 2008;179:616-21.
10. Roehrborn CG, Boyle P, Gould AL, Waldstreicher J. Serum pros- 16. Roehrborn CG, Siami P, Barkin J, Damião R, Major-Walker K,
tate-specific antigen as a predictor of prostate volume in men with Nandy I, et al. The effects of combination therapy with dutas-
benign prostatic hyperplasia. Urology 1999;53:581-9. teride and tamsulosin on clinical outcomes in men with sympto-
11. Roehrborn CG, McConnell J, Bonilla J, Rosenblatt S, Hudson PB, matic benign prostatic hyperplasia: 4-year results from the
Malek GH, et al. Serum prostatic specific antigen is a strong pre- CombAT study. Eur Urol 2010;57:123-31.
dictor of future prostate growth in men with benign prostatic 17. Lee JY, Lee SH, Kim SJ, Kim CS, Lee HM, Kim CI, et al. Change
hyperplasia. PROSCAR long-term efficacy and safety study. J in International Prostate Symptom storage subscore after
Urol 2000;163:13-20. long-term medical therapy in BPH patients: finasteride and
12. Jacobsen SJ, Jacobson DJ, Girman CJ, Roberts RO, Rhodes T, Alpha-blocker combination therapy in men with moderate-to-se-
Guess HA, et al. Natural history of prostatism: risk factors for vere LUTS/BPH in Korea. J Urol 2011;77:171-6.
acute urinary retention. J Urol 1997;158:481-7.
Korean J Urol 2012;53:248-252
You might also like
- Dutta's Textbook of Gynecology-6th Ed Jaypee 12Document1 pageDutta's Textbook of Gynecology-6th Ed Jaypee 12Safwan Shaikh50% (2)
- Benign Prostatic Hyperplasia Concept MapDocument1 pageBenign Prostatic Hyperplasia Concept MapJason A. AdoyoganNo ratings yet
- Pathophysiology - PyelonephritisDocument2 pagesPathophysiology - PyelonephritisFrancis Kevin Sagudo92% (13)
- Development of Uterus and Congenital Anomalies: Done By: Jabir AL Araimi ID# 0333145Document21 pagesDevelopment of Uterus and Congenital Anomalies: Done By: Jabir AL Araimi ID# 0333145jabirNo ratings yet
- Benign Prostatic Hypertrophy: An Update On Drug TherapyDocument2 pagesBenign Prostatic Hypertrophy: An Update On Drug TherapyAjieRnie IDNo ratings yet
- TadalafilDocument13 pagesTadalafildrngNo ratings yet
- A2 (Comparison of Prostatic Artery Embolisation (PAE) Versus Transurethral Resection of The Prostate (TURP) For Benign Prostatic Hyperplasia Randomised, Open Label, Non-Inferiority Trial)Document10 pagesA2 (Comparison of Prostatic Artery Embolisation (PAE) Versus Transurethral Resection of The Prostate (TURP) For Benign Prostatic Hyperplasia Randomised, Open Label, Non-Inferiority Trial)NadanNadhifahNo ratings yet
- Hamed Alabad BPHDocument47 pagesHamed Alabad BPHHamed AlabadNo ratings yet
- BJU International - 2017 - Roehrborn - A Prospective Randomised Placebo Controlled Study of The Impact of DutasterideDocument12 pagesBJU International - 2017 - Roehrborn - A Prospective Randomised Placebo Controlled Study of The Impact of DutasterideBayu HernawanNo ratings yet
- A Systematic Review and Meta Analysis 1625134013Document13 pagesA Systematic Review and Meta Analysis 1625134013bannour_No ratings yet
- JURNALDocument5 pagesJURNALMita Restuning AjiNo ratings yet
- Current Status of 5 of Lower Urinary Tract Symptoms and BPH: - Reductase Inhibitors in The ManagementDocument8 pagesCurrent Status of 5 of Lower Urinary Tract Symptoms and BPH: - Reductase Inhibitors in The ManagementApriani BahoriNo ratings yet
- Benign Prostatic Hypertrophy Comprehensive Management Guide 2Document9 pagesBenign Prostatic Hypertrophy Comprehensive Management Guide 2Thanakorn WongsombutNo ratings yet
- Kim 2017Document5 pagesKim 2017kanaNo ratings yet
- 9th JC Paper - Katoh Et Al. Cardiovascular Safety of Mirabegron Add-On Therapy To Tamsulosin For The Treatment of Overactive Bladder in Men WithDocument10 pages9th JC Paper - Katoh Et Al. Cardiovascular Safety of Mirabegron Add-On Therapy To Tamsulosin For The Treatment of Overactive Bladder in Men WithWai Kit CheongNo ratings yet
- Medical Therapy For Benign Prostatic Hyperplasia: A ReviewDocument11 pagesMedical Therapy For Benign Prostatic Hyperplasia: A ReviewEfson Sustera IrawanNo ratings yet
- Uti 14 80Document7 pagesUti 14 80patrickNo ratings yet
- Efficacy and Tolerability of Tamsulosin 0.4 MG in Patients With Symptomatic Benign Prostatic HyperplasiaDocument6 pagesEfficacy and Tolerability of Tamsulosin 0.4 MG in Patients With Symptomatic Benign Prostatic HyperplasiawanggaNo ratings yet
- Holep Estandar Vs MosesDocument10 pagesHolep Estandar Vs MosesUROLOGIA JAROCHANo ratings yet
- Primary and Secondary Prevention of Benign Prostatic HyperplasiaDocument2 pagesPrimary and Secondary Prevention of Benign Prostatic HyperplasiaNina MelinaNo ratings yet
- Intravesical Prostate ProtrusionDocument9 pagesIntravesical Prostate ProtrusionFelly FelixNo ratings yet
- Is Early Surgical Treatment For Benign Prostatic Hyperplasia Preferable Medical Therapy - Pros and ConsDocument11 pagesIs Early Surgical Treatment For Benign Prostatic Hyperplasia Preferable Medical Therapy - Pros and ConsClaudia FreyonaNo ratings yet
- BPH JournalDocument8 pagesBPH JournalJuliaNo ratings yet
- A Mathematical Model of Intermittent Androgen SuppDocument23 pagesA Mathematical Model of Intermittent Androgen SuppalexNo ratings yet
- Journal Pone 0189126Document13 pagesJournal Pone 0189126Mohamad Syaikhul IslamNo ratings yet
- BPH Smith English-6-15Document10 pagesBPH Smith English-6-15novi camiumNo ratings yet
- 1 s2.0 S2049080122008974 MainDocument4 pages1 s2.0 S2049080122008974 MainGregory AssonitisNo ratings yet
- Journal Pre-Proof: International Journal of Radiation Oncology, Biology, PhysicsDocument42 pagesJournal Pre-Proof: International Journal of Radiation Oncology, Biology, PhysicsMilan JovicNo ratings yet
- BPH, Pdui 2017Document36 pagesBPH, Pdui 2017basirNo ratings yet
- BPH, Pdui 2017 PDFDocument36 pagesBPH, Pdui 2017 PDFcyndra erisNo ratings yet
- JournalDocument8 pagesJournalFentiNo ratings yet
- Issues and Unmet Needs in Advanced Prostate CancerDocument9 pagesIssues and Unmet Needs in Advanced Prostate CancerMuhammad MosliNo ratings yet
- Benign Prostatic Hyperplasia: Urology Division, Department of Surgery, Faculty of Medicine, University of Sumatera UtaraDocument38 pagesBenign Prostatic Hyperplasia: Urology Division, Department of Surgery, Faculty of Medicine, University of Sumatera UtaraSalwa Zahra TsamaraNo ratings yet
- Determination of Prostate VolumeDocument6 pagesDetermination of Prostate VolumeChristian ToalongoNo ratings yet
- M T O P S: The Edical Herapy F Rostatic Ymptoms (MTOPS) TrialDocument21 pagesM T O P S: The Edical Herapy F Rostatic Ymptoms (MTOPS) TrialLeandro FerroNo ratings yet
- BPH UpdateDocument69 pagesBPH Updateathe_triiaNo ratings yet
- Ceju 66 00246Document4 pagesCeju 66 00246Àlex MataNo ratings yet
- 1 s2.0 S2590280622000079 MainDocument10 pages1 s2.0 S2590280622000079 MainDimas Bintoro KyhNo ratings yet
- Meta 5 - Song S - 2022Document12 pagesMeta 5 - Song S - 2022matheus.verasNo ratings yet
- Combination Medical Therapy For Lower Urinary Tract Symptoms and Benign Prostatic HyperplasiaDocument9 pagesCombination Medical Therapy For Lower Urinary Tract Symptoms and Benign Prostatic HyperplasiaganangahimsaNo ratings yet
- De La Rosette Et Al. Eur Urol 2001-40-256 263. EAU Guidelines On Benign Prostatic Hyperplasia BPHDocument8 pagesDe La Rosette Et Al. Eur Urol 2001-40-256 263. EAU Guidelines On Benign Prostatic Hyperplasia BPHMuhamad Iqbal BaihaqiNo ratings yet
- Matsukawa 2017Document33 pagesMatsukawa 2017kanaNo ratings yet
- 2116 Manuscript 17522 1 10 20200911Document5 pages2116 Manuscript 17522 1 10 20200911sibon M amrilNo ratings yet
- Benign Prostatic HyperplasiaDocument6 pagesBenign Prostatic HyperplasiaAnonymous 9OkFvNzdsNo ratings yet
- 1Document10 pages1Ade Triansyah EmsilNo ratings yet
- PaeDocument10 pagesPaeMr. LNo ratings yet
- Treatment of Benign Prostatic HyperplasiaDocument6 pagesTreatment of Benign Prostatic HyperplasiaDea IrbahNo ratings yet
- Soliman 2020Document6 pagesSoliman 2020Naufal NanditaNo ratings yet
- Conservative Treatment For BPHDocument4 pagesConservative Treatment For BPHSamir AggouneNo ratings yet
- Prostataarterienembolisation: Indikation, Technik Und Klinische ErgebnisseDocument9 pagesProstataarterienembolisation: Indikation, Technik Und Klinische ErgebnisseEliana Solange FouzNo ratings yet
- VTE Is Asa Helpful BJH 2009Document8 pagesVTE Is Asa Helpful BJH 2009kans72No ratings yet
- Clinical Case of Evidence Based MedicineDocument6 pagesClinical Case of Evidence Based MedicinempNo ratings yet
- Ipp And Changes In Ipss In Benign Prostatic Hyperplasia (Bph) Patients Treated With Α1-BlockerDocument11 pagesIpp And Changes In Ipss In Benign Prostatic Hyperplasia (Bph) Patients Treated With Α1-BlockerNur LaylaNo ratings yet
- Benign Prostatic HyperplasiaDocument15 pagesBenign Prostatic HyperplasiaPediatrics - Pediatric SurgeryNo ratings yet
- BPH JournalDocument4 pagesBPH JournalTiffany ValentinaNo ratings yet
- Cesium 131 Prostate BrachytherapyDocument7 pagesCesium 131 Prostate BrachytherapyPablo Del PozoNo ratings yet
- ContentServer - Asp 2Document9 pagesContentServer - Asp 2witaparamitaNo ratings yet
- BPH-Diagnosis and TreatmentDocument7 pagesBPH-Diagnosis and TreatmentMedissa MothNo ratings yet
- Kju 53 109Document5 pagesKju 53 109AnggaFaletraNo ratings yet
- Dapagliflozin - Effect On Uric AcidDocument4 pagesDapagliflozin - Effect On Uric AcidCintia TakedaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 17: OncologyFrom EverandComplementary and Alternative Medical Lab Testing Part 17: OncologyNo ratings yet
- Male Lower Urinary Tract Symptoms and Benign Prostatic HyperplasiaFrom EverandMale Lower Urinary Tract Symptoms and Benign Prostatic HyperplasiaSteven A. KaplanNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Role of Statins in Coronary Artery DiseaseDocument6 pagesRole of Statins in Coronary Artery Diseasemonia agni wiyatamiNo ratings yet
- Periocular Ulcerative Dermatitis Associated With Gentamicin Ointment Prophylaxis in NewbornsDocument4 pagesPeriocular Ulcerative Dermatitis Associated With Gentamicin Ointment Prophylaxis in Newbornsmonia agni wiyatamiNo ratings yet
- 105 116 Acute Gastrointestinal BleedingDocument12 pages105 116 Acute Gastrointestinal Bleedingmonia agni wiyatamiNo ratings yet
- Esa Anemia CKDDocument6 pagesEsa Anemia CKDmonia agni wiyatamiNo ratings yet
- KetosterilDocument2 pagesKetosterilmonia agni wiyatamiNo ratings yet
- Short Notes and Short Cases in GynaecologyDocument163 pagesShort Notes and Short Cases in Gynaecologysalah subbahNo ratings yet
- Urogynecology Division AyuDocument4 pagesUrogynecology Division AyuDwickyNo ratings yet
- Report 2302407663 1Document2 pagesReport 2302407663 1crystal monteiroNo ratings yet
- 07Document24 pages07Esteban CayuelasNo ratings yet
- (Jurnal) Sonography in Male InfertilityDocument25 pages(Jurnal) Sonography in Male InfertilityIrni Dwi Aprianty IbrahimNo ratings yet
- Kuliah ST Reproduksi WanitaDocument103 pagesKuliah ST Reproduksi Wanitaanon_88598530100% (1)
- Urology PDFDocument188 pagesUrology PDFAmr BashaNo ratings yet
- Nejm 2016:374:562Document9 pagesNejm 2016:374:562Piya TangNo ratings yet
- Poster Fer Kogi 18Document2 pagesPoster Fer Kogi 18wiwikNo ratings yet
- Merit List Stis (Bio) Government Girls Higher Secondary School Kundian (Mianwali)Document1 pageMerit List Stis (Bio) Government Girls Higher Secondary School Kundian (Mianwali)Malik AsadNo ratings yet
- Fertility and Sterility Treating Hydrosalpinx With A Manual Physical TherapyDocument1 pageFertility and Sterility Treating Hydrosalpinx With A Manual Physical TherapyClearPassageNo ratings yet
- Urology For Medical Student Hora 19-12-2008Document77 pagesUrology For Medical Student Hora 19-12-2008Adriana SantosNo ratings yet
- Enuresis (Bedwetting) I. DefinitionDocument3 pagesEnuresis (Bedwetting) I. DefinitionPrincess Angel LucanasNo ratings yet
- Renal MCQDocument6 pagesRenal MCQMikiyas TeferaNo ratings yet
- Gynaecology QuestionsDocument19 pagesGynaecology QuestionsShaik AmreenNo ratings yet
- ObyGyn - OSCE (FG2)Document23 pagesObyGyn - OSCE (FG2)roorian100% (1)
- Renal Pathology-Mreh 32104: Disorders of KidneyDocument3 pagesRenal Pathology-Mreh 32104: Disorders of KidneyArvinth Guna SegaranNo ratings yet
- UrologyDocument35 pagesUrologymiansk100% (1)
- Truths: Every Parent Must KnowDocument1 pageTruths: Every Parent Must KnowDanielle TeigenNo ratings yet
- Urinary SystemDocument2 pagesUrinary SystemнастяNo ratings yet
- Dr. YeshwiniDocument34 pagesDr. YeshwiniSai RakshikaNo ratings yet
- Urinary System and Disorders IntroductionDocument23 pagesUrinary System and Disorders IntroductionHananya ManroeNo ratings yet
- Basuki B Purnomo Department of Urology Medical School Brawijaya University/Saiful Anwar Hospital MalangDocument44 pagesBasuki B Purnomo Department of Urology Medical School Brawijaya University/Saiful Anwar Hospital MalangChangi RenandaNo ratings yet
- Name Address City State Zipcode Toll Free Website DescriptionDocument21 pagesName Address City State Zipcode Toll Free Website Descriptionapi-18351628No ratings yet
- Insersi PesariumDocument21 pagesInsersi PesariumiFha AM.No ratings yet