Professional Documents
Culture Documents
KRONOS Study - Paper
Uploaded by
Radu CiprianOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
KRONOS Study - Paper
Uploaded by
Radu CiprianCopyright:
Available Formats
Articles
Triple therapy with budesonide/glycopyrrolate/formoterol
fumarate with co-suspension delivery technology versus
dual therapies in chronic obstructive pulmonary disease
(KRONOS): a double-blind, parallel-group, multicentre,
phase 3 randomised controlled trial
Gary T Ferguson, Klaus F Rabe, Fernando J Martinez, Leonardo M Fabbri, Chen Wang, Masakazu Ichinose, Eric Bourne, Shaila Ballal,
Patrick Darken, Kiernan DeAngelis, Magnus Aurivillius, Paul Dorinsky, Colin Reisner
Summary
Background Inhaled corticosteroids have been used in patients with chronic obstructive pulmonary disease (COPD), Lancet Respir Med 2018
but the potential benefits of their use in triple therapy are not well known. We aimed to compare the efficacy of a Published Online
triple therapy with corresponding dual therapies in symptomatic patients with moderate to very severe COPD, September 16, 2018
http://dx.doi.org/10.1016/
without a requirement for a history of exacerbations.
S2213-2600(18)30327-8
See Online/Comment
Methods In this double-blind, parallel-group, multicentre phase 3 randomised controlled trial, we recruited patients http://dx.doi.org/10.1016/
from hospitals and care centres in Canada, China, Japan, and the USA. Eligible patients were 40–80 years of age, were S2213-2600(18)30370-9
current or former smokers (with a smoking history of ≥10 pack-years), had an established clinical history of COPD, Pulmonary Research Institute
and were symptomatic for COPD, despite receiving two or more inhaled maintenance therapies for at least 6 weeks of Southeast Michigan,
before screening. We randomly assigned patients (2:2:1:1) using an interactive web response system to receive Farmington Hills, MI, USA
(Prof G T Ferguson MD);
budesonide/glycopyrrolate/formoterol fumarate metered-dose inhaler 320/18/9·6 μg (BGF MDI), glycopyrrolate/ LungenClinic Grosshansdorf
formoterol fumarate metered-dose inhaler 18/9·6 μg (GFF MDI), budesonide/formoterol fumarate metered-dose and Christian-Albrechts
inhaler 320/9·6 μg (BFF MDI), or open-label budesonide/formoterol fumarate dry-powder inhaler 400/12 μg University Kiel, Airway
(BUD/ FORM DPI). Primary endpoints for the Europe/Canada statistical analysis approach were FEV1 area under the Research Center North,
Member of the German Center
curve from 0–4 h (AUC0–4) for BGF MDI versus BFF MDI and BGF MDI versus BUD/FORM DPI over 24 weeks; and for Lung Research (DZL),
change from baseline in morning pre-dose trough FEV1 for BGF MDI versus GFF MDI and non-inferiority of BFF Germany (Prof K F Rabe MD);
MDI versus BUD/FORM DPI (margin of –50 mL from lower bound of 95% CI) over 24 weeks. Comparisons with Joan and Sanford I. Weill
Department of Medicine, Weill
BUD/FORM DPI were made for the Europe/Canada statistical analysis approach only. This study is registered with
Cornell Medicine, New York,
ClinicalTrials.gov, number NCT02497001. NY, USA (Prof F J Martinez MD);
Sahlgrenska University
Findings Between Aug 20, 2015, and Jan 5, 2018, 3047 patients were screened from 215 sites, and 1902 were randomly Hospital, Gothenburg, Sweden;
Department of Medicine,
assigned to receive BGF MDI (n=640), GFF MDI (n=627), BFF MDI (n=316), or BUD/FORM DPI (n=319). Over
University Hospital, Ferrara,
24 weeks, BGF MDI significantly improved FEV1 AUC0–4 versus BFF MDI (least squares mean difference 104 mL, 95% CI Italy (Prof L M Fabbri MD);
77 to 131; p<0·0001) and BUD/FORM DPI (91 mL, 64 to 117; p<0·0001). BGF MDI also significantly improved pre-dose National Clinical Research
trough FEV1 versus GFF MDI (22 mL, 4 to 39; p=0·0139) and was non-inferior to BUD/FORM DPI (–10 mL, –36 to 16; Centre for Respiratory Diseases,
China-Japan Friendship
p=0·4390). At week 24, patients in the BGF MDI group had a significantly improved FEV1 AUC0–4 compared with patients
Hospital, Beijing, China
receiving BFF MDI (116 mL, 95% CI 80 to 152; p<0·0001); there was a non-significant improvement in the change from (Prof C Wang MD); Department
baseline in morning pre-dose trough FEV1 at week 24 versus GFF MDI (13 mL, –9 to 36 mL; p=0·2375). The most of Respiratory Medicine,
common treatment-emergent adverse events were nasopharyngitis (n=49 [8%] in the BGF MDI group; n=41 [7%] in the Tohoku University Graduate
School of Medicine, Sendai,
GFF MDI group; n=26 [8%] in the BFF MDI group; and n=30 [9%] in the BUD/FORM DPI group) and upper respiratory Japan (Prof M Ichinose MD);
tract infection (n=65 [10%]; n=38 [6%]; n=18 [6%]; and n=22 [7%]). Pneumonia incidence was low (<2%) and similar Pearl—a member of the
across treatments. There were two treatment-related deaths, both in the GFF MDI group. AstraZeneca Group, Durham,
NC, USA (E Bourne MS,
K DeAngelis MD, P Dorinsky MD);
Interpretation BGF MDI was efficacious, well tolerated, and could be a more appropriate treatment than the corresponding Pearl—a member of the
dual therapies for symptomatic patients with moderate to very severe COPD, irrespective of exacerbation history. AstraZeneca Group,
Morristown, NJ, USA
Funding Pearl—a member of the AstraZeneca Group. (S Ballal MS, P Darken PhD,
C Reisner MD); AstraZeneca
Gothenburg, Mölndal, Sweden
Copyright © 2018 Elsevier Ltd. All rights reserved. (M Aurivillius MD); and
AstraZeneca, Gaithersburg,
Introduction β2-agonists (LABAs), used alone or in combination, play MD, USA (C Reisner)
Long-acting bronchodilators, including long-acting an important part in the maintenance treatment of
muscarinic antagonists (LAMAs) and long-acting chronic obstructive pulmonary disease (COPD) at all
www.thelancet.com/respiratory Published online September 16, 2018 http://dx.doi.org/10.1016/S2213-2600(18)30327-8 1
Articles
Correspondence to:
Prof Gary T Ferguson, Pulmonary Research in context
Research Institute of Southeast
Michigan, Farmington Hills, Evidence before this study entry. The study population is representative of the majority of
MI 48336, USA. The benefits of therapies containing inhaled corticosteroids patients with moderate to very severe COPD who are seen in a
garytferguson@msn.com
have been shown in patients with chronic obstructive clinical setting. More than 80% of the patients in KRONOS were
pulmonary disease (COPD), but concern regarding the symptomatic patients with moderate to very severe COPD who
risk-to-benefit ratio of long-term administration of inhaled were not at high risk of exacerbations, a population that has
corticosteroids has led to their recommended use only as a not previously been the focus of phase 3 studies of triple
treatment option in patients with a history of exacerbations therapies. We also did a prespecified subgroup analysis to
who continue to experience disease symptoms or investigate the relationship between blood eosinophil counts
exacerbations. However, real-world evidence suggests that and treatment effects on lung function and exacerbation rates.
inhaled corticosteroids are prescribed to patients with COPD
Implications of all the available evidence
across the spectrum of symptom severity and exacerbation risk.
Triple therapy improved lung function and symptoms, and
Potential benefits of fixed-dose combination triple therapy
reduced COPD exacerbations compared with dual fixed-dose
(inhaled corticosteroid, long-acting muscarinic antagonist
combination therapies of inhaled corticosteroid and LABA, and
[LAMA], and long-acting β2-agonist [LABA]), compared with
LAMA and LABA, and was well tolerated in this patient
fixed-dose combination dual therapies (LAMA and LABA or
population. The improvements in pre-dose trough FEV1 for
inhaled corticosteroid and LABA), are not well defined in
BGF MDI versus GFF MDI were mainly in patients with baseline
symptomatic patients with COPD, particularly those with low
eosinophil levels higher than approximately 250 cells/mm3,
exacerbation risk. Furthermore, the role of blood eosinophil
whereas improvements in pre-dose trough FEV1 for BGF MDI
counts as a predictor of patient response to inhaled
versus BFF MDI were evident over a broad range of eosinophil
corticosteroid therapy is unclear and largely based on
levels. There were reductions of approximately 20% in the rate of
retrospective analyses.
moderate or severe exacerbations in the BGF MDI group versus
Added value of this study the GFF MDI group, associated with eosinophil concentrations
To our knowledge, KRONOS is the first phase 3 study of a triple that most patients exceeded. This finding suggests that triple
fixed-dose combination inhaled corticosteroid, LAMA, and therapy with BGF MDI could be more effective in improving lung
LABA therapy in which the trial population was not enriched for function and reducing the exacerbation risk than LAMA/LABA
patients who had COPD exacerbations in the year before study dual therapy in most patients with COPD.
stages of disease severity.1 Triple therapy containing Triple fixed-dose combinations of inhaled corticosteroid,
dual bronchodilators and an inhaled corticosteroid is LAMA, and LABA have been developed for COPD,13–16 but
recommended only as a treatment option for patients the potential benefits of triple versus dual fixed-dose
with high exacerbation risk who continue to have combination therapies (LAMA and LABA, or inhaled
symptoms or exacerbations while receiving treatment, corticosteroid and LABA) are not well characterised across
particularly LAMA and LABA, or inhaled corticosteroid the spectrum of patients with COPD, with most studies
and LABA.1 Despite guidance relating to which patients to date focused on patients with a high frequency of
benefit from the addition of an inhaled corticosteroid to exacerbations or severe or very severe airflow limitation,
other treatments, real-world evidence suggests that or both.13–17 Budesonide/glycopyrrolate/formoterol fumar
inhaled corticosteroids are commonly prescribed to ate metered-dose inhaler (BGF MDI), formulated with co-
patients with high or low exacerbation risk,2 often as an suspension delivery tech nology, is a triple fixed-dose
open triple therapy with a fixed-dose combination of combination of inhaled corticosteroid, LAMA, and LABA
inhaled corticosteroid with a LABA and a LAMA.3 that is in development as a maintenance therapy for
Although adding an inhaled corticosteroid to a LABA patients with COPD. Co-suspension delivery technology
has repeatedly been shown to improve airflow limitation,4,5 facilitates the formulation of multiple drugs into a single
quality of life,4,5 and exacerbation rates4,6,7 compared with MDI device that provides consistent aerosol performance18
use of a LABA alone, questions remain relating to the and drug deposition throughout the lungs.19
long-term use of inhaled corticosteroids in COPD, In this study, we aimed to compare triple therapy
especially given the pneumonia risk reported in some (BGF MDI) with dual therapies (glycopyrrolate/
studies8,9 and the apparent limited effect of an inhaled formoterol fumarate [GFF] MDI and budesonide/
corticosteroid and LABA on reducing exacerbations formoterol fumarate [BFF] MDI), in symptomatic
compared with a dual LAMA and LABA combination, as patients with moderate to very severe COPD, irrespect
reported in one large study.10 It continues to be debated ive of exacerbation history, measuring lung function,
whether peripheral eosinophil counts can be used to exacerbations, symptoms, and quality of life, and
predict exacerbation risk or to identify patients with COPD analysing the potential effect of peripheral eosinophil
who might clinically respond to inhaled corticosteroids.11,12 counts on treatment outcomes.
2 www.thelancet.com/respiratory Published online September 16, 2018 http://dx.doi.org/10.1016/S2213-2600(18)30327-8
Articles
Methods budesonide/formoterol fumarate dry-powder inhaler
Study design and participants (BUD/FORM DPI). Randomisation was stratified by
KRONOS was a randomised, double-blind, parallel- reversibility to salbutamol sulphate (yes/no), country, and
group, phase 3 randomised controlled trial done in disease severity (post-bronchodilator percent predicted
215 sites across four countries (Canada, China, Japan, FEV1 ≥50% or <50%). There was no enrichment for blood
and the USA). Study sites included hospitals (n=108) and eosinophils as part of the study protocol. Patients, study
other care centres (n=107; mainly primary care and site personnel, and the study sponsor were masked to
specialty centres). treatment assignment for BGF MDI, GFF MDI, and BFF
Eligible patients were aged 40–80 years; were current MDI, since all were administered from matching MDIs.
or former smokers (with a smoking history of ≥10 pack- BUD/FORM DPI (Symbicort Turbuhaler, AstraZeneca,
years); had an established clinical history of COPD, as AB, Södertälje, Sweden) was administered open-label.
defined by the American Thoracic Society (ATS)/ Since BFF MDI is not an approved therapy, BUD/FORM
European Respiratory Society20 or by locally applicable DPI was included in this study as an active comparator
guidelines21 and confirmed by the investigator; and had approved for COPD, to support BFF MDI use as an active
mild to very severe COPD, as defined post-bronchodilator comparator for BGF MDI.
FEV1 less than 80% and 25% or more, according to
predicted normal values using National Health and Procedures
Nutrition Examination Survey III reference equations,22 Eligible patients discontinued prohibited medications for
or applicable reference norms for Japan21,23 and China COPD, which included LAMAs, LABAs, or both, for
(adjustment factor of 0·88).24 Patients were symptomatic the study duration and had their COPD maintenance
(COPD Assessment Test score ≥10) despite receiving two therapy adjusted for the screening period (appendix).
or more inhaled maintenance therapies for at least Briefly, all patients received sponsor-provided, open-label
6 weeks before screening (appendix). Patients were not ipratropium bromide (34 μg ex-actuator; Atrovent hydro- See Online for appendix
required to have had a COPD exacerbation within the fluoroalkane [Boehringer Ingelheim Pharmaceuticals Inc,
preceding year. Ridgefield, CT, USA] or equivalent product) administered
Exclusion criteria included a current diagnosis of four times daily for maintenance of COPD, and were
asthma or a diagnosis of any respiratory disease or permitted to continue using inhaled corticosteroids during
condition other than COPD, which in the opinion of the screening (providing they had been on a stable dose of
investigator could influence the results. Patients were also inhaled corticosteroid for 4 weeks before screening).
excluded if they had acute worsening of COPD that Ipratropium and inhaled corticosteroid were stopped
required treatment with oral corticosteroids or antibiotics before randomisation.
less than 6 weeks before screening, with less than a 4-week After randomisation, patients received BGF MDI
washout of corticosteroids or antibiotics before Visit 1, or 320/18/9·6 µg (equivalent to budesonide/glycopyrronium/
during screening. Patients were excluded if they were formoterol fumarate dihydrate 320/14·4/10 µg; inhaled
hospitalised because of COPD within 3 months before or corticosteroid, LAMA, and LABA triple therapy), GFF MDI
during screening, as were patients unable to show 18/9·6 µg (LAMA and LABA dual therapy), BFF MDI
baseline FEV1 stability or perform acceptable spirometry.25 320/9·6 µg (inhaled corticosteroid and LABA dual therapy),
Patients had to show that they could use an MDI correctly, or open-label BUD/FORM DPI 400/12 μg (inhaled
with training provided if needed. We excluded patients corticosteroid and LABA) as two inhalations twice-daily for
who required a spacer device because they were unable to 24 weeks (appendix). All patients received sponsor-provided
use the MDI correctly. Other exclusion criteria included salbutamol sulphate (90 μg salbutamol base ex-actuator;
change in smoking status within 6 weeks of or during Ventolin hydrofluoroalkane [GlaxoSmithKline, Research
screening, and the need for long-term oxygen therapy Triangle Park, NC, USA]), for rescue use as needed
(>15 h/day). Full details can be found in the study protocol. throughout the study. Rescue medication had to be For the study protocol see
The study was done in accordance with Good Clinical withheld for at least 6 h before the start of test day https://astrazenecagrouptrials.
pharmacm.com/ST/Submission/
Practice, including the Declaration of Helsinki. The procedures. The last dose of study drug must have been View?id=25410
protocol and informed consent form were approved by taken as scheduled the evening before test day procedures.
appropriate institutional review boards or independent At each visit from randomisation onwards, spirometry
ethics committees (appendix). All patients provided written was assessed by study personnel, the St George’s
informed consent before screening. Protocol amendments Respiratory Questionnaire (SGRQ) was completed by the
pertaining to study endpoints or data analyses are shown participant, and electronic diary review was completed by
in the appendix. study personnel, and occurrences of COPD exacerbations,
medication changes, and adverse events were recorded.
Randomisation and masking The Baseline Dyspnoea Index (BDI) questionnaire was
Study site personnel randomly assigned patients (2:2:1:1) completed at screening and the Transition Dyspnoea
using an interactive web response system to treatment Index (TDI) questionnaire was completed at the remaining
with BGF MDI, GFF MDI, BFF MDI, or visits. Spirometry was done in accordance with ATS
www.thelancet.com/respiratory Published online September 16, 2018 http://dx.doi.org/10.1016/S2213-2600(18)30327-8 3
Articles
criteria,25 and all sites were provided with identical systems Additional prespecified analyses included examining the
that met or exceeded the ATS minimum performance relationship of responses (morning pre-dose trough FEV1
recommendations. Patients recorded daily rescue med and rate of moderate or severe exacerbations) to baseline
ication use and Evaluating Respiratory Symptoms COPD blood eosinophil counts. Safety endpoints included ad
(E-RS: COPD) scores in the electronic diary. verse events, 12-lead electrocardiograms (ECGs), clinical
There were predefined criteria for identifying and laboratory testing, and vital sign measurements.
reporting exacerbations, pneumonia, and major adverse
cardiovascular events (appendix). An external data mon Statistical analysis
itor
ing committee oversaw the safety assessment. An Patients from all countries were included in all statistical
independent clinical endpoint committee reviewed all analysis approaches. We did all analyses using SAS
adverse events reported as pneumonia or that potentially (version 9.4 or later). All efficacy assessments were relative
met criteria for major adverse cardiovascular events. to pre-dose baseline values obtained at randomisation
Blood eosinophil counts were measured at screening (FEV1, BDI, and SGRQ), or over the last 7 days of
Visit 1 (of three planned visits) and at randomisation; the screening (rescue medication use and RS-Total score).
mean of non-missing values was recorded as the baseline Baseline FEV1 was defined as the average of non-missing
blood eosinophil count. A history of COPD exacerbations values obtained 60 min and 30 min before dosing on
in the previous year was obtained to characterise the day 1 of treatment.
study population. The primary estimand of interest for superiority
testing was the efficacy estimand, which was defined
Outcomes as the hypothetical effect of the randomised treatment
Primary and secondary endpoints and treatment in all patients assuming continuation of randomised
comparisons of interest differed according to regulatory treatments for the duration of the study, regardless of
registration requirements (appendix). The primary end actual compliance. We did the primary efficacy analysis
points for the Europe and Canada statistical analysis for the efficacy estimand using the modified intention-
approach were FEV1 area under the curve from 0 to 4 h to-treat population (all patients with post-randomisation
(AUC0–4) over 24 weeks (BGF MDI vs BFF MDI and BGF data obtained before discontinuation from treatment).
MDI vs BUD/FORM DPI) and change from baseline in We analysed patients according to assigned treatment
morning pre-dose trough FEV1 over 24 weeks (BGF MDI group. The second estimand of interest for superiority
vs GFF MDI and BFF MDI vs BUD/FORM DPI [non- testing was the attributable estimand, which we also
inferiority]). assessed in the modified intention-to-treat population,
Secondary endpoints for the Europe and Canada accounting for patients who discontinued treatment
statistical analysis approach were change from baseline because of lack of efficacy or tolerability (unfavourable
in morning pre-dose trough FEV1 (BGF MDI vs BFF outcomes), and imputing missing data; patients without
MDI), peak change from baseline in FEV1 within 4 h after data after randomisation were not included in
dosing, rate of moderate or severe COPD exacerbations, the attributable estimand (appendix). The per-protocol
TDI focal score (Europe statistical analysis approach estimand was the primary estimand for the non-
only), change from baseline in daily rescue medication inferiority analyses of BFF MDI compared with BUD/
use, change from baseline in SGRQ total score, E-RS: FORM DPI, and used the per-protocol population (all
COPD total score (RS-Total score), and time to clinically patients who were randomly assigned to treatment,
important deterioration (BGF MDI vs GFF MDI, used any amount of study treatment, and had post-
vs BFF MDI, and vs BUD/FORM DPI), all over 24 weeks, randomisation data obtained before any major protocol
and time to onset of action on Day 1 (the first post-dose deviations).
timepoint at which the mean change from baseline in For the primary efficacy analyses, all comparisons
FEV1 exceeded 100 mL). CID was defined as a decrease of were for superiority except for the comparison of BFF
100 mL or more from baseline in trough FEV1, an MDI versus BUD/FORM DPI, which was for non-
increase of 4 points or more from baseline in SGRQ total inferiority (margin of –50 mL from lower bound of
score, a TDI focal score of –1 point or less, or a treatment- 95% CI). We analysed the change from baseline in
emergent moderate or severe COPD exacerbation morning pre-dose trough FEV1 using a linear model
occurring up to week 24. Time to first moderate or severe with repeated measures. The model included treatment,
exacerbation was an additional efficacy endpoint. visit, treatment by visit interaction, and inhaled corti
FEV1 AUC0–4 at week 24 (BGF MDI vs BFF MDI) and costeroid use at screening as categorical covariates, and
change from baseline in morning pre-dose trough FEV1 baseline FEV1, percent reversibility to salbutamol, and
at week 24 (BGF MDI vs GFF MDI) were primary baseline eosinophil counts as continuous covariates. We
endpoints for the US approach. Secondary endpoints for used an unstructured covariance matrix to model
the US approach are shown in the appendix. correlation within a patient. We calculated two-sided
Details of the endpoints for the China/Japan statistical p values and point estimates with 95% CIs for each
analysis approach are provided in the protocol. treatment difference.
4 www.thelancet.com/respiratory Published online September 16, 2018 http://dx.doi.org/10.1016/S2213-2600(18)30327-8
Articles
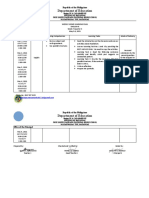
3047 patients assessed for eligibility
1145 excluded
1139 ineligible
6 screen failure
1902 randomly assigned
640 randomised to BGF MDI 627 randomised to GFF MDI 316 randomised to BFF MDI 319 randomised to open-label
320/18/9·6 µg 18/9·6 µg 320/9·6 µg BUD/FORM DPI 400/12 µg
639 treated with BGF MDI 627 treated* with GFF MDI 315 treated* with BFF MDI 318 treated with open-label
320/18/9·6 µg 18/9·6 µg 320/9·6 µg BUD/FORM DPI 400/12 µg
73 discontinued 101 discontinued 48 discontinued 40 discontinued
14 patient discretion 37 patient discretion 19 patient discretion 15 patient discretion
28 adverse events 30 adverse events 11 adverse events 11 adverse events
3 protocol-specified criteria 1 protocol-specified criteria 3 protocol-specified criteria 1 protocol-specified criteria
10 lost to follow-up 2 lost to follow-up 6 lack of efficacy 2 lost to follow-up
10 lack of efficacy 16 lack of efficacy 4 major protocol violation 6 ack of efficacy
3 major protocol violation 4 major protocol violation 5 investigator discretion 4 major protocol violation
5 investigator discretion 11 investigator discretion 1 investigator discretion
566 completed treatment 524 completed treatment 266 completed treatment 278 completed treatment
639 included in the safety 625 included in the safety 314 included in the safety 318 included in the
population population population safety population
639 included in the modified 625 included in the modified 314 included in the 318 included in the modified
intention-to-treat intention-to-treat modified intention-to- intention-to-treat
population population treat population population
608 included in the 587 included in the 298 included in the 295 included in the per-
per-protocol population per-protocol population per-protocol population protocol population
Figure 1: Trial profile
BGF=budesonide/glycopyrrolate/formoterol fumarate. MDI=metered-dose inhaler. GFF=glycopyrrolate/formoterol fumarate. BFF=budesonide/formoterol fumarate. BUD/FORM DPI=budesonide/formoterol
fumarate dry-powder inhaler. *Two patients in the GFF MDI group and one patient in the BFF MDI group participated in multiple sponsor-led studies and were excluded from all analysis populations.
We analysed change from baseline in FEV1 AUC0–4 Results
over 24 weeks and at week 24 using a similar approach Between Aug 20, 2015, and Jan 5, 2018, 3047 patients
to that used for morning pre-dose trough FEV1. We were screened, of whom 1902 were randomly assigned to
calculated AUC using the trapezoidal rule and receive BGF MDI (n=640), GFF MDI (n=627), BFF MDI
normalised it by dividing by the time (h) from dosing to (n=316), or BUD/FORM DPI (n=319; figure 1).
the last measurement included. Details of the secondary Overall, 1411 (74%) of 1896 patients in the modified
endpoint statistical analyses, non-inferiority margins, intention-to-treat population had no exacerbations in the
type I error control, and sample size calculation are preceding 12 months, and 88% had no severe exacer
shown in the appendix. Treatment comparisons for bations and 1 or 0 moderate exacerbations in the
which p values of 0·05 were reported wre considered as preceding 12 months, 71·8% were receiving inhaled
significant if they satisfied the type I error control corticosteroids at screening, and 51·8% had baseline
strategy. Comparisons for which p was less than 0·05, blood eosinophil counts ≥150 cells/mm³. There were no
which either failed or were not included in the type I clinically relevant differences across treatment groups at
error control strategy, are reported as nominally signifi baseline (table 1).
cant. This study is registered with ClinicalTrials.gov, Over 24 weeks, BGF MDI significantly improved FEV1
number NCT02497001. AUC0–4 versus BFF MDI (least squares mean [LSM]
difference 104 mL, 95% CI 77 to 131; p<0·0001) and
Role of the funding source BUD/FORM DPI (91 mL, 64 to 117; p<0·0001; figure 2A;
The funder of the study had a role in study design, data table 2). The change from baseline in morning pre-dose
collection, data analysis, data interpretation, and writing trough FEV1 over 24 weeks was significantly improved by
of the report. The corresponding author had full access BGF MDI versus GFF MDI (22 mL, 4–39 mL; p=0·0139)
to all the data in the study and had final responsibility for and BFF MDI (74 mL, 52 to 95 mL; p<0·0001; figure 2B;
the decision to submit for publication. table 2). BFF MDI was non-inferior to BUD/FORM DPI
www.thelancet.com/respiratory Published online September 16, 2018 http://dx.doi.org/10.1016/S2213-2600(18)30327-8 5
Articles
for the change from baseline in morning pre-dose trough
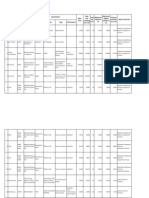
BGF MDI GFF MDI BFF MDI Open-label
320/18/9·6 µg 18/9·6 µg 320/9·6 µg BUD/FORM DPI FEV1 over 24 weeks (per-protocol estimand LSM
(n=639) (n=625) (n=314) 400/12 µg difference –10 mL, 95% CI –36 to 16; p=0·4390). There
(n=318) were consistent results from the secondary analyses of
Mean age, years 64·9 (7·8) 65·1 (7·7) 65·2 (7·2) 65·9 (7·7) these endpoints with the attributable estimand (table 2).
Sex Treatment differences were generally consistent over
Male 460 (72·0%) 430 (68·8%) 224 (71·3%) 236 (74·2%) time: patients in the BGF MDI group had a significantly
Female 179 (28·0%) 195 (31·2%) 90 (28·7%) 82 (25·8%) improved FEV1 AUC0–4 at week 24 compared with patients
Ethnicity receiving BFF MDI (LSM difference 116 mL, 95% CI
White 329 (51·5%) 301 (48·2%) 157 (50·0%) 163 (51·3%) 80 to 152; p<0·0001; figure 2A; appendix). Regarding the
Black 23 (3·6%) 38 (6·1%) 15 (4·8%) 14 (4·4%) other primary endpoint for the US approach, there was a
Asian 284 (44·4%) 285 (45·6%) 142 (45·2%) 141 (44·3%) non-significant improvement in the change from
Other 3 (0·5%) 1 (0·2%) 0 0 baseline in morning pre-dose trough FEV1 at week 24
Mean body mass 26·1 (6·7) 26·3 (6·4) 26·1 (5·8) 26·2 (6·3) versus GFF MDI (13 mL, –9 to 36 mL; p=0·2375;
index, kg/m² figure 2B; appendix); in the secondary analyses, there
Current smoker 256 (40·1%) 257 (41·1%) 115 (36·6%) 122 (38·4%) was a nominally significant improvement in this end
Median number of 45·0 (10·0–256·0) 45·0 (10·0–171·0) 45·0 (10·0–192·0) 45·0 (10·0–180·0) point (24 mL, 1 to 46 mL; p=0·0370; appendix).
pack-years smoked* BGF MDI significantly increased peak change from
COPD severity baseline in FEV1 over 24 weeks versus BFF MDI (LSM
Mild 2 (0·3%) 0 1 (0·3%) 0 difference 105 mL, 95% CI 78–133; p<0·0001), but not
Moderate 310 (48·5%) 306 (49·0%) 154 (49·0%) 160 (50·3%) versus GFF MDI (table 2). The time to onset of action on
Severe 275 (43·0%) 267 (42·7%) 133 (42·4%) 138 (43·4%) day 1 was within 5 min for all treatments (table 2).
Very severe 52 (8·1%) 52 (8·3%) 26 (8·3%) 20 (6·3%) The model-estimated rates of moderate or severe
Mean COPD 7·1 (6·0) 6·5 (5·4) 7·3 (6·2) 6·7 (5·5) exacerbations were 0·46 per year for BGF MDI, 0·95
duration, years per year for GFF MDI, 0·56 per year for BFF MDI, and
Moderate or severe COPD exacerbations in the past 12 months 0·55 per year for BUD/FORM DPI (table 3). The rate of
0 469 (73·4%) 473 (75·7%) 235 (74·8%) 234 (73·6%) moderate or severe exacerbations was significantly lower
1 125 (19·6%) 108 (17·3%) 61 (19·4%) 59 (18·6%) during treatment with BGF MDI versus GFF MDI
≥2 45 (7·0%) 44 (7·0%) 18 (5·7%) 25 (7·9%) (table 3). BGF MDI reduced the rate of moderate or severe
Moderate or severe exacerbation rate exacerbations compared with BFF MDI and BUD/FORM
Mean 0·4 (0·8) 0·3 (0·7) 0·3 (0·6) 0·4 (0·8) DPI, but these reductions were not significant (table 3).
Median 0·0 (0–8) 0·0 (0–5) 0·0 (0–4) 0·0 (0–8) For the additional endpoint of time to first moderate or
Eosinophils severe exacerbation of COPD, the risk during treatment
Median cells 150·0 155·0 152·5 150·0 with BGF MDI was nominally significantly lower versus
per mm³ (10·0–2815·0) (15·0–2490·0) (15·0–920·0) (35·0–1100·0) GFF MDI (hazard ratio [HR] 0·593; p<0·0001 [Cox
<150 cells/mm³ 314 (49·1%) 291 (46·6%) 151 (48·1%) 157 (49·4%) regression] and p=0·0001 [log rank]) and numerically
≥150 cells/mm³ 325 (50·9%) 334 (53·4%) 163 (51·9%) 161 (50·6%) lower versus BFF MDI (HR 0·747; p=0·0635 [Cox
Post-salbutamol FEV1, % predicted regression] and p=0·0281 [log rank]; figure 3).
Number 639 624 314 318 BGF MDI significantly improved TDI focal score
Mean 50·2 (14·3) 50·2 (13·8) 50·0 (14·0) 50·7 (13·8) versus BUD/FORM DPI, but not versus GFF MDI and
Reversibility to salbutamol BFF MDI, and provided nominally significant
Number 639 623 314 317 improvements in change from baseline in RS-Total
Mean difference in 199·7 (144·5) 191·7 (154·2) 195·8 (162·1) 212·2 (152·7) score over 24 weeks versus GFF MDI but not BFF MDI
FEV1 before and or BUD/FORM DPI (table 3). BGF MDI also resulted in
after salbutamol,
mL
nominally significant improvements in SGRQ total
Reversible† 286 (44·8%) 266 (42·6%) 130 (41·4%) 140 (44·0%)
score over 24 weeks versus GFF MDI but not BFF MDI
Use of inhaled 464 (72·6%) 447 (71·5%) 225 (71·7%) 225 (70·8%)
or BUD/FORM DPI (table 3).
corticosteroid at Time to clinically important deterioration was
screening nominally significantly reduced by BGF MDI versus BFF
BDI focal score MDI and BUD/FORM DPI, but there was no difference
Number 614 587 296 291 compared with GFF MDI (table 3). There was no
Mean 6·4 (2·1) 6·5 (2·1) 6·4 (2·2) 6·3 (2·2) significant difference between groups in the average
SGRQ total score puffs per day of daily rescue medication (table 3).
Number 621 595 298 297 BFF MDI was non-inferior to BUD/FORM DPI over
Mean 44·1 (17·0) 43·9 (16·4) 43·5 (17·0) 43·9 (17·5) 24 weeks for most other applicable type I error controlled
(Table 1 continues on next page) endpoints (FEV1 AUC0−4 [primary endpoint], TDI focal
score, SGRQ total score, and RS-Total score; appendix).
6 www.thelancet.com/respiratory Published online September 16, 2018 http://dx.doi.org/10.1016/S2213-2600(18)30327-8
Articles
Non-inferiority was not shown for average daily rescue
BGF MDI GFF MDI BFF MDI Open-label
medication use or risk of clinically important deterioration, 320/18/9·6 µg 18/9·6 µg 320/9·6 µg BUD/FORM DPI
although for the latter there was insufficient evidence to (n=639) (n=625) (n=314) 400/12 µg
conclude that treatment effects differed and the former (n=318)
might have been influenced by the open-label nature of (Continued from previous page)
BUD/FORM DPI. Mean CAT total score 18·7 (6·4) 18·1 (6·1) 18·4 (6·6) 18·0 (6·4)
The prespecified subgroup analysis of treatment Rescue medication use‡
responses by blood eosinophil count showed that im Number 293 269 141 155
provements in change from baseline in morning pre- Median puffs 3·6 (1·0–13·0) 3·7 (1·0–18·4) 3·9 (1·0–17·7) 3·9 (1·0–20·3)
dose trough FEV1 for BGF MDI relative to GFF MDI were per day
driven by patients with at least 150 cells/mm³ (appendix).
Data are mean (SD), median (range), or n (%), unless otherwise indicated. BGF=budesonide/glycopyrrolate/formoterol
Further analyses of response by continuous baseline fumarate. MDI=metered dose inhaler. GFF=glycopyrrolate/formoterol fumarate. BFF=budesonide/formoterol
eosinophil count with locally weighted scatter-plot fumarate. BUD/FORM DPI=budesonide/formoterol fumarate dry powder inhaler. COPD=chronic obstructive
smoothing (LOESS) showed that the differences in pulmonary disease. BDI=Baseline Dyspnoea Index. SGRQ=St George’s Respiratory Questionnaire. CAT=COPD
Assessment Test. *Number of pack-years smoked=(number of cigarettes each day/20) × number of years smoked.
improvements in morning pre-dose trough FEV1 between †Reversible was defined as improvement in FEV1 after salbutamol administration (compared with before salbutamol
BGF MDI and GFF MDI over 24 weeks increased with administration) of 12% or more and 200 mL or more. ‡Rescue medication user population.
blood eosinophil counts and occurred primarily at
Table 1: Demographic and baseline disease characteristics of the modified intention-to-treat population
eosinophil counts above approximately 250 cells/mm³
(figure 4A). By contrast, improvements in morning pre-
dose trough FEV1 with BGF MDI versus BFF MDI A
occurred across a broad range of eosinophil counts 400 BGF MDI 320/18/9·6 µg
(figure 4B; appendix). The LOESS curves for BGF MDI GFF MDI 18/9·6 µg
BFF MDI 320/9·6 µg
and BFF MDI converged from around 400 cells per mm³ 350 Open-label BUD/FORM DPI 400/12 µg
Adjusted mean FEV1 AUC0–4 (mL)
but these results should be interpreted with caution
because of the variability that resulted from only
300
approximately 5% of patients having blood eosinophil
levels of 400 cells per mm3 or more.
250
The rates of moderate or severe exacerbations with BGF
MDI were lower than with GFF MDI for patients in both
eosinophil subgroups (appendix), with locally weighted 200
scatter-plot smoothing showing that treatment differences
increased with baseline blood eosinophil concentrations; 150
beginning at approximately 75–100 cells/mm³ (figure 4C), a
level exceeded by more than 75% of patients (figure 4C; B
200
appendix). No apparent differences were seen between
180
BGF MDI and GFF MDI below these concentration
Adjusted mean change from baseline in
morning pre-dose trough FEV1 (mL)
thresholds. Differences between BGF MDI and BFF MDI 160
in the rate of moderate or severe exacerbations were similar 140
across most eosinophil counts (figure 4D; appendix). 120
The incidence of treatment-emergent adverse events, 100
treatment-related adverse events, serious treatment- 80
emergent adverse events, and treatment-emergent adverse 60
events leading to discontinuation was similar across 40
treatments (table 4). The most common treatment-emerg 20
ent adverse events were nasopharyngitis (n=49 [8%] in the
0
BGF MDI group; n=41 [7%] in the GFF MDI group; n=26 Day 1 4 8 12 16 20 24 Over Over
[8%] in the BFF MDI group; and n=30 [9%] in the BUD/ weeks 24 weeks
12–24
FORM DPI group) and upper respiratory tract infection Number of weeks after dose
(n=65 [10%]; n=38 [6%]; n=18 [6%]; and n=22 [7%]). The
incidence of severe treatment-emergent adverse events Figure 2: Primary lung function endpoints over time, in the modified intention-to-treat population
(A) FEV1 AUC0–4. (B) Change from baseline in morning pre-dose trough FEV1. Error bars represent SE. AUC0–4=area
was similar across treatments (ranging from 18 [5·7%] of
under the curve 0–4 h. BGF=budesonide/glycopyrrolate/formoterol fumarate. MDI=metered-dose inhaler.
314 patients in the BFF MDI group to 60 [9·6%] of GFF=glycopyrrolate/formoterol fumarate. BFF=budesonide/formoterol fumarate.
625 patients in the GFF MDI group). BUD/FORM DPI=budesonide/formoterol fumarate dry-powder inhaler.
The most frequently reported serious treatment-
emergent adverse events were COPD (70 [3·7%] of cardiovascular events and pneumonia, confirmed by the
1896 patients) and pneumonia (15 [0·8%] patients; clinical endpoint committee, were low and similar across
table 4; appendix). The rates of cases of major adverse treatments (table 4). Non-adjudicated major adverse
www.thelancet.com/respiratory Published online September 16, 2018 http://dx.doi.org/10.1016/S2213-2600(18)30327-8 7
Articles
MDI group). There were two deaths in the GFF MDI
BGF MDI GFF MDI BFF MDI Open-label
320/18/9·6 µg 18/9·6 µg 320/9·6 µg BUD/FORM DPI group, both caused by worsening of COPD, which
(n=639) (n=625) (n=314) 400/12 µg were judged by the investigator to be related to study
(n=318) drug treatment.
Primary endpoints BGF MDI was not associated with clinically meaningful
FEV1 AUC0−4, mL changes in haematology, clinical chemistry, kidney
Number of patients 501 485 245 248 function, or urinalysis variables. Effects on vital signs
LSM 305 288 201 214 (heart rate or blood pressure) and ECG parameters
SE 8·4 8·5 11·7 11·5 (QTcF, PR, or QRS interval prolongation) were small and
LSM (95% CI); p value NA 16 (–6 to 38); 104 (77 to 131); 91 (64 to 117); similar across treatments (data not shown).
p=0·1448 p<0·0001* p<0·0001*
Change from baseline in morning pre-dose trough FEV1, mL Discussion
Number of patients 622 601 300 301 BGF MDI provided clinically meaningful improvements
LSM 147 125 73 88 in lung function versus BFF MDI and BUD/FORM DPI,
SE 6·5 6·6 9·2 9·1 with modest improvements reported for BGF MDI
LSM (95% CI); p value NA 22 (4 to 39); 74† (52 to 95); 59 (38 to 80); versus GFF MDI. However, the primary reason for
p=0·0139* p<0·0001* p<0·0001‡ inhaled corticosteroid use in COPD is to control
Secondary endpoints exacerbations, and there were significant reductions in
FEV1 AUC0−4, mL§ exacerbation rates for BGF MDI versus GFF MDI. BFF
Number of patients 501 485 245 248 MDI was non-inferior to BUD/FORM DPI for the
LSM 293 271 189 204 primary and most secondary endpoints.
SE 8·4 8·4 11·6 11·4 Unlike previous phase 3 trials of triple therapies (fixed-
LSM (95% CI); p value NA 22 (0 to 43); 104 (77 to 130); 89 (63 to 116); dose combination inhaled corticosteroid, LAMA, and
p=0·0488‡ p<0·0001* p<0·0001* LABA), KRONOS was not restricted to patients with a
Change from baseline in morning pre-dose trough FEV1, mL§ history of COPD exacerbations.13–17 Therefore, in addition
Number of patients 622 601 300 301 to supporting the use of triple therapy in patients with
LSM 137 110 63 80 high exacerbation risk, the results of this study are
SE 6·6 6·6 9·3 9·2 particularly important for patients with low exacerbation
LSM (95% CI); p value NA 27 (9 to 45); 74 (52 to 96); 56 (35 to 78); risk. Patients entering the study were required to be
p=0·0027* p<0·0001 p<0·0001‡ symptomatic despite being on two or more inhaled
Peak change from baseline in FEV1 <4 h after dose, mL maintenance therapies. This requirement arguably
Number of patients 501 485 245 248 represents a patient who, because of continued symptoms
LSM 381 364 275 291 or exacerbation risk, would be considered for additional
SE 8·8 8·9 12·2 12·0 treatment options, such as triple fixed-dose combination
LSM (95% CI); p value NA 17 (–6 to 40); 105 (78 to 133); 90 (62 to 118); therapy. KRONOS is the second study published that
p=0·1425 p<0·0001 p<0·0001
compares triple therapy with corresponding dual
Time to onset of action on day 1 (change from baseline in FEV1 at 5 min after dose, mL) therapies delivered by the same platform. This study
Number of patients 429 417 220 210 design ensures that improvements observed with the
Mean 175 180 160 164 triple versus dual therapies were due to the combined
SD 122 131 116 122 effect of active compounds rather than differences in
Least squares mean results are for the treatment difference for BGF MDI versus comparators. Results are for efficacy device, drug, or dosing strategy.
estimand, unless otherwise stated. BGF=budesonide/glycopyrrolate/formoterol fumarate. MDI=metered dose inhaler. Somewhat surprisingly for this population, the addition
GFF=glycopyrrolate/formoterol fumarate. BFF=budesonide/formoterol fumarate. BUD/FORM DPI=budesonide/
formoterol fumarate dry powder inhaler. AUC0–4=area under the curve from 0 to 4 h. LSM=least squares mean. NA=not
of inhaled corticosteroid to LAMA and LABA dual therapy
applicable. *Prespecified comparison. †Prespecified secondary endpoint. ‡Nominally significant (ie, not significant (BGF MDI vs GFF MDI) showed a marked reduction in
after type I error control or not included in the type I error control strategy). §Attributable estimand. exacerbation frequency. There was a similar trend in
Table 2: Primary endpoints and lung function secondary endpoints exacerbation rates for triple therapy versus dual therapies
in the TRIBUTE13 and IMPACT16 studies, both done over
52 weeks in patients with a high risk of COPD exacerbation.
cardiovascular events and pneumonia rates are shown in The difference in exacerbation rates with BGF MDI versus
the appendix. BFF MDI and versus BUD/FORM DPI was not significant,
12 deaths occurred during the study, caused by cancer probably because a larger sample size would have been
(n=2 in the BGF MDI group, n=2 in the BFF MDI required, but the magnitude of effect between triple
group), cardiovascular disease (n=2 in the BGF MDI therapy and dual therapies was similar to those seen in
group, n=1 in the GFF MDI group), worsening of IMPACT16 and the 52-week TRILOGY study.14 Additionally,
COPD (n=2 in the GFF MDI group), pneumonia in our study, in which patients discontinued any previous
(n=1 in the BUD/FORM DPI group), or other causes inhaled corticosteroid at randomisation, the time to first
(n=1 smoke inhalation and n=1 sepsis, both in the BGF moderate or severe exacerbation showed a cumulative
8 www.thelancet.com/respiratory Published online September 16, 2018 http://dx.doi.org/10.1016/S2213-2600(18)30327-8
Articles
incidence of exacerbations for GFF MDI, BFF MDI, and
BGF MDI GFF MDI BFF MDI Open-label BUD/
BUD/FORM DPI that diverged over time, not just in the 320/18/9·6 µg 18/9·6 µg 320/9·6 µg FORM DPI
first 4 weeks, indicating that results were not driven solely 400/12 µg
by withdrawal of inhaled corticosteroid, as postulated Model-estimated rate of moderate or severe COPD exacerbations
previously for IMPACT.26 Our finding, that adding a LAMA Number of patients 639 625 314 318
to inhaled corticoisteroid and LABA (BGF MDI vs BFF Rate, per year 0·46 0·95 0·56 0·55
MDI) improved lung function, is consistent with previous Rate ratio (95% CI); NA 0·48 0·82 0·83
triple fixed-dose combination therapy studies.14,16 p value* (0·37 to 0·64); (0·58 to 1·17); (0·59 to 1·18);
There were notable changes from baseline for symptom- p<0·0001 p=0·2792 p=0·3120
based endpoints for all treatments. However, in studies TDI focal score
with only active treatment groups, the magnitude of Number of patients 614 587 296 291
differences between treatments can be small and thus LSM 1·25 1·07 1·01 0·78
these endpoints might not always act as sensitive SE 0·09 0·09 0·13 0·13
differentiators between active treatments. Nonetheless, LSM (95% CI); p value* NA 0·18 0·24 0·46
numerical improvements in symptoms and quality-of-life (–0·07 to 0·43); (–0·07 to 0·54); (0·16 to 0·77);
p=0·1621 p=0·1283 p=0·0031
endpoints generally favoured BGF MDI relative to the
Change from baseline in RS-Total score
comparators.
Number of patients 638 621 313 313
The exacerbation history captured from the year before
LSM –1·1 –0·7 –1·0 –1·0
study entry was lower than the model-estimated exacer
bation rates observed during the study, especially with SE 0·13 0·14 0·19 0·19
GFF MDI. This finding raises the point of whether LSM (95% CI); p value* NA –0·38 –0·16 –0·16
(–0·74 to –0·01); (–0·61 to 0·28); (–0·60 to 0·29);
asking patients standard questions about exacerbations p=0·0430† p=0·4790 p=0·4923
and acute COPD treatments are an accurate measure of Change from baseline in SGRQ total score
exacerbation risk, since they require patients to recall Number of patients 621 595 298 297
these details correctly. Alternatively, as noted in the LSM –7·5 –6·3 –7·1 –6·3
ECLIPSE study,27 exacerbation variability might simply SE 0·47 0·47 0·61 0·62
be a function of time, with divergent exacerbation LSM (95% CI); p value* NA –1·22 –0·45 –1·26
patterns in many patients on a year-by-year basis.27 (–2·30 to –0·15); (–1·78 to 0·87); (–2·58 to 0·06);
Notwithstanding the reason for the trend in exacerbation p=0·0259† p=0·5036 p=0·0617
rates before and during this study, results support the Time to CID‡
importance of therapies containing inhaled cortico Number of patients 639 625 314 318
steroids for preventing exacerbations in symptomatic Patients with CID, n (%) 411 (64·3%) 413 (66·1%) 216 (68·8%) 225 (70·8%)
patients with COPD. Hazard ratio (95% CI); NA 0·88 0·83 0·81
The role of peripheral blood eosinophils as a predictor of p value* (0·76 to 1·00); (0·70 to 0·98); (0·69 to 0·96);
p=0·0593 p=0·0276† p=0·0119†
clinical response is uncertain, with findings both for and
Change from baseline in average daily rescue medication use, puffs per day§
against their use as a biomarker in patients with COPD.11,12
Number of patients 293 269 141 155
Our LOESS regression showed an association between
LSM –1·3 –1·1 –1·1 –1·6
blood eosinophil counts and improve ments in lung
function and COPD exacerbation rates with combinations SE 0·13 0·13 0·18 0·17
containing inhaled corticosteroids (ie, BGF MDI and BFF LSM (95% CI); p value* NA –0·25 –0·24 0·23
(–0·60 to 0·09); (–0·65 to 0·18); (–0·17 to 0·63);
MDI), consistent with findings from a post-hoc analysis.28 p=0·1446 p=0·2661 p=0·2667
The relationship between blood eosinophil levels and the
Results are for the efficacy estimand. CID=clinically important deterioration. BGF=budesonide/glycopyrrolate/
rate of moderate or severe COPD exacerbations will be formoterol fumarate. MDI=metered dose inhaler. GFF=glycopyrrolate/formoterol fumarate. BFF=budesonide/
further characterised in the 52-week phase 3 ETHOS formoterol fumarate. BUD/FORM DPI=budesonide/formoterol fumarate dry powder inhaler. COPD=chronic
study (NCT02465567), which is investigating two doses of obstructive pulmonary disease. NA=not applicable. TDI=Transition Dyspnoea Index. LSM=least squares mean. RS-Total
score=Evaluating Respiratory Symptoms in COPD Total score. SGRQ=St George’s Respiratory Questionnaire.
BGF MDI compared with BFF MDI and GFF MDI and *Treatment difference for BGF MDI versus comparators. †Nominally significant (ie, not significant after type I error
aims to randomly assign more than 2000 patients per control or not included in the type I error control strategy). ‡CID was defined as a decrease of 100 mL or more from
treatment group. baseline in trough FEV1, an increase of 4 points or more from baseline in SGRQ total score, a TDI focal score of –1 point
or less, or a treatment-emergent moderate or severe COPD exacerbation occurring up to week 24. §Rescue medication
Overall, the safety profile of BGF MDI was comparable
user population.
with the well established profiles of the approved
products GFF MDI and BUD/FORM DPI, as well as BFF Table 3: Exacerbations, symptoms, quality of life, and CID endpoints, over 24 weeks
MDI. The incidence of major adverse cardiovascular
events was low and similar across treatments, supporting
previous studies of GFF MDI that showed that potential pneumonia were low and comparable between BGF MDI
class effects of LAMAs and LABAs on cardiovascular (2%) and GFF MDI (2%), suggesting that the budesonide
safety were not observed in healthy participants or dose used in the triple therapy was not associated with an
patients with COPD.29 Notably, incidences of adjudicated appreciably increased risk of pneumonia compared with
www.thelancet.com/respiratory Published online September 16, 2018 http://dx.doi.org/10.1016/S2213-2600(18)30327-8 9
Articles
35
dual bronchodilator therapy. This finding is consistent
BGF MDI 320/18/9·6 µg
GFF MDI 18/9·6 µg with pneumonia rates reported for budesonide/
30 BFF MDI 320/9·6 µg formoterol compared with formoterol monotherapy in
Open-label BUD/FORM DPI 400/12 µg
Patients who had a moderate or
studies over 6 and 12 months.4,6 In IMPACT,16 the
25
severe exacerbation (%)
incidence of pneumonia over 52 weeks in the fluticasone
20 furoate-containing treatment arms (fluticasone furoate,
umeclidinium, and vilanterol [inhaled corticosteroid,
15
LAMA, and LABA] and fluticasone furoate and vilanterol
10 [inhaled corticosteroid and LABA]) was higher than with
umeclidinium and vilanterol (LAMA and LABA).16
5
Limitations included the shorter study duration of
+Censored
0 KRONOS (24 weeks) than other phase 3 studies of triple
0 4 8 12 16 20 24 fixed-dose combination therapies for chronic obstructive
Number at risk Weeks pulmonary disease (52 weeks),13–17 especially when con
BGF MDI 320/18/9·6 µg 639 620 590 561 526 498 428
GFF MDI 18/9·6 µg 625 585 532 492 463 446 371
sider
ing exacerbations and long-term risks. However,
BFF MDI 320/9·6 µg 314 295 277 260 242 233 196 the exacerbation rates observed in KRONOS were
Open-label BUD/FORM 318 297 282 271 257 241 203 consistent with those from longer-term studies13,16 and
DPI 400/12 µg
most patients (>70%) were taking an inhaled corticos
Figure 3: Time to first exacerbation of chronic obstructive pulmonary disease teroid before study participation. Additionally, although
BGF=budesonide/glycopyrrolate/formoterol fumarate. MDI=metered-dose inhaler. GFF=glycopyrrolate/formoterol we assessed the associations between lung function,
fumarate. BFF=budesonide/formoterol fumarate. BUD/FORM DPI=budesonide/formoterol fumarate dry-powder
inhaler. exacerbations, and eosinophil levels using blood
eosinophil levels at baseline, we did not use eosinophil
levels to prospectively stratify therapy. Such studies,
A B
300 300
Adjusted mean change from baseline in
morning pre-dose trough FEV1 (mL)
250 250
200 200
150 150
100 100
50 50
0 0
BGF MDI 320/18/9·6 µg BGF MDI 320/18/9·6 µg
–50 –50
GFF MDI 18/9·6 µg BFF MDI 320/9·6 µg
–100 –100
0
50
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
00
0
50
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
00
10
15
20
25
30
35
40
45
50
55
60
65
70
75
80
85
90
95
10
15
20
25
30
35
40
45
50
55
60
65
70
75
80
85
90
95
10
10
C D
2·0 2·0
Annualised rate of moderate or severe COPD
BGF MDI 320/18/9·6 µg BGF MDI 320/18/9·6 µg
1·8 GFF MDI 18/9·6 µg 1·8 BFF MDI 320/9·6 µg
1·6 1·6
exacerbation (banded)
Rate ratio
1·4 0·784 1·4
1·2 1·2
1·0 1·0
0·8 0·8
0·6 0·6
0·4 0·4
0·2 0·2
0 0
0
50
0
50
0
10
15
20
25
30
35
40
45
50
55
60
65
70
75
80
10
15
20
25
30
35
40
45
50
55
60
65
70
75
80
Baseline eosinophil count (cells mm3) Baseline eosinophil count (cells mm3)
Figure 4: Lung function and exacerbation responses by blood eosinophil counts, in the modified intention-to-treat population
Change from baseline in morning pre-dose trough FEV1 for BGF MDI versus GFF MDI (A) and BGF MDI versus BFF MDI (B), and rate of moderate or severe COPD exacerbations for BGF MDI versus
GFF MDI (C) and BGF MDI versus BFF MDI (D). The banded areas represent 95% CIs. BGF=budesonide/glycopyrrolate/formoterol fumarate. MDI=metered-dose inhaler. GFF=glycopyrrolate/formoterol
fumarate. BFF=budesonide/formoterol fumarate. COPD=chronic obstructive pulmonary disease.
10 www.thelancet.com/respiratory Published online September 16, 2018 http://dx.doi.org/10.1016/S2213-2600(18)30327-8
Articles
BGF MDI GFF MDI BFF MDI Open-label
320/18/9·6 µg 18/9·6 µg 320/9·6 µg BUD/FORM DPI
(n=639) (n=625) (n=314) 400/12 µg
(n=318)
Treatment-emergent adverse events*
Patients with ≥1 treatment-emergent adverse event 388 (61%) 384 (61%) 175 (56%) 183 (58%)
Patients with treatment-emergent adverse events related† to study treatment 112 (18%) 91 (15%) 48 (15%) 40 (13%)
Patients with serious treatment-emergent adverse events 55 (9%) 68 (11%) 21 (7%) 29 (9%)
Patients with serious treatment-emergent adverse events related† to study treatment 7 (1%) 12 (2%) 3 (1%) 6 (2%)
Patients with treatment-emergent adverse events that led to early discontinuation 30 (5%) 30 (5%) 11 (4%) 11 (3%)
Patients with confirmed major adverse cardiovascular event‡ 2 (<1%) 3 (<1%) 2 (1%) 2 (1%)
Patients with confirmed pneumonia‡ 12 (2%) 10 (2%) 6 (2%) 4 (1%)
Deaths (all causes) 6 (1%) 3 (<1%) 2 (1%) 1 (<1%)
Adverse events occurring in ≥2% of patients§
Nasopharyngitis 49 (8%) 41 (7%) 26 (8%) 30 (9%)
Upper respiratory tract infection 65 (10%) 38 (6%) 18 (6%) 22 (7%)
Chronic obstructive pulmonary disease 17 (3%) 32 (5%) 8 (3%) 13 (4%)
Bronchitis 20 (3%) 15 (2%) 12 (4%) 9 (3%)
Muscle spasms 21 (3%) 8 (1%) 17 (5%) 6 (2%)
Dysphonia 20 (3%) 5 (1%) 15 (5%) 6 (2%)
Hypertension 13 (2%) 10 (2%) 8 (3%) 4 (1%)
Dyspnoea 9 (1%) 9 (1%) 8 (3%) 8 (3%)
Back pain 8 (1%) 12 (2%) 4 (1%) 8 (3%)
Nausea 7 (1%) 3 (<1%) 4 (1%) 7 (2%)
Data are n (%). BGF=budesonide/glycopyrrolate/formoterol fumarate. MDI=metered dose inhaler. GFF=glycopyrrolate/formoterol fumarate. BFF=budesonide/formoterol
fumarate. BUD/FORM DPI=budesonide/formoterol fumarate dry powder inhaler. COPD=chronic obstructive pulmonary disease. *Numbers are number of patients. †Possibly,
probably, or definitely related in the opinion of the investigator. ‡Confirmed by clinical endpoint committee. §By preferred term.
Table 4: Summary of adverse events (safety population)
including the ongoing ETHOS study (NCT02465567), FJM, EB, SB, KD, MA, PDa analysed the data. GTF, KFR, FJM, LMF,
will help to further elucidate the use of eosinophils as a CW, EB, SB, KD, MA, PDa, PDo, and CR interpreted the data. GTF,
LMF, KFR, FJM, KD, and PDo drafted the manuscript, and GTF, KFR,
biomarker in chronic obstructive pulmonary disease. FJM, LMF, CW, MI, EB, SB, PDa, KD, MA, PDo, and CR critically
A history of exacerbations was not an entry requirement revised it for important intellectual content and approved it for
for KRONOS, which might have influenced exacerbation publication. GTF, KFR, FJM, LMF, CW, MI, EB, SB, PDa, KD, MA, PDo,
results compared with other studies. However, we believe and CR agree to be accountable for all aspects of the work.
that the patient population is a strength of the trial design, Declaration of interests
since it encompassed a broader range of disease severity GTF reports grants, personal fees, and non-financial support from
AstraZeneca during the conduct of the study; grants, personal fees and
compared with other triple fixed-dose combination non-financial support from AstraZeneca, Boehringer Ingelheim,
studies.13–16 The results suggest that previous treatment Novartis, Pearl—a member of the AstraZeneca Group, and Sunovion;
with inhaled corticosteroids might be indicative of an grants and personal fees from Theravance; and personal fees from
exacerbation risk that is not accurately captured by Circassia, GlaxoSmithKline, Innoviva, Mylan, and Verona, outside of the
submitted work. KFR reports personal fees from AstraZeneca,
history alone. Berlin-Chemie, Boehringer Ingelheim, Chiesi Pharmaceuticals,
The results of this study challenge recommendations InterMune, Novartis, Sanofi, and Teva; and grants from Ministry of
that inhaled corticosteroids should be considered only as Education and Science, Germany, outside of the submitted work.
a treatment option for patients with high exacerbation FJM reports grants from AstraZeneca during the conduct of the study;
personal fees and non-financial support from American College of Chest
risk. The findings show that a much broader patient Physicians, AstraZeneca, Boehringer Ingelheim, Chiesi, Concert,
population than currently recommended could benefit Continuing Education, Genentech, GlaxoSmithKline, Inova Fairfax
from triple fixed-dose combination therapy, and might Health System, Miller Communications, National Association for
identify the potential role for triple fixed-dose combination Continuing Education, Novartis, Pearl—a member of the AstraZeneca
Group, PeerView Communications, Prime Communications,
therapy in symptomatic patients whose condition is not Puerto Rican Respiratory Society, Roche, Sunovion, and Theravance;
adequately controlled by dual therapy, irrespective of non-financial support from ProterixBio; personal fees from American
exacerbation risk. Thoracic Society, Columbia University, Haymarket Communications,
Integritas, inThought Research, MD Magazine, Methodist Hospital
Contributors Brooklyn, New York University, Unity, UpToDate, WebMD/MedScape,
GTF, KFR, LMF, CW, MI, EB, SB, PDa, CR, and PDo conceived and and Western Connecticut Health Network; and grants from National
designed the study. GTF, CW, MI, EB, and KD acquired the data. GTF,
www.thelancet.com/respiratory Published online September 16, 2018 http://dx.doi.org/10.1016/S2213-2600(18)30327-8 11
Articles
Institutes of Health, outside of the submitted work. LMF reports 12 Brusselle G, Pavord ID, Landis S, et al. Blood eosinophil levels as a
research or conference funding from AstraZeneca, Boehringer biomarker in COPD. Respir Med 2018; 138: 21–31.
Ingelheim, Chiesi, Dompè, GlaxoSmithKline, Guidotti e Malesci, 13 Papi A, Vestbo J, Fabbri L, et al. Extrafine inhaled triple therapy
Menarini, Novartis, Pearl—a member of the AstraZeneca Group, versus dual bronchodilator therapy in chronic obstructive
Takeda, and Zambon; consulting or lecture fees from AstraZeneca, pulmonary disease (TRIBUTE): a double-blind, parallel group,
Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Guidotti e Malesci, randomised controlled trial. Lancet 2018; 391: 1076–84.
Menarini, Novartis, Pearl—a member of the AstraZeneca Group, 14 Singh D, Papi A, Corradi M, et al. Single inhaler triple therapy
Takeda, and Zambon. MI reports personal fees from AstraZeneca, versus inhaled corticosteroid plus long-acting β2-agonist therapy for
during the conduct of the study; and personal fees from Kyorin, Nippon chronic obstructive pulmonary disease (TRILOGY): a double-blind,
parallel group, randomised controlled trial. Lancet 2016;
Boehringer Ingelheim, and Novartis Pharma, outside of the submitted
388: 963–73.
work. EB, SB, PDa, KD, PDo, and CR are employed by Pearl—a member
15 Vestbo J, Papi A, Corradi M, et al. Single inhaler extrafine triple
of the AstraZeneca Group, the sponsor of the study. MA is employed by
therapy versus long-acting muscarinic antagonist therapy for chronic
AstraZeneca. CW declares no competing interests. obstructive pulmonary disease (TRINITY): a double-blind, parallel
Acknowledgments group, randomised controlled trial. Lancet 2017; 389: 1919–29.
We thank all the patients and their families and the team of 16 Lipson DA, Barnhart F, Brealey N, et al. Once-daily single-inhaler
investigators, research nurses, and operations staff involved in these triple versus dual therapy in patients with COPD. N Engl J Med
studies. The KRONOS study was supported by Pearl–a member of the 2018; 378: 1671–80.
AstraZeneca Group. Medical writing support, under the direction of the 17 Lipson DA, Barnacle H, Birk R, et al. FULFIL trial: once-daily triple
authors, was provided by Thomas Owens, PhD, of CMC CONNECT, therapy for patients with chronic obstructive pulmonary disease.
a division of Complete Medical Communications Ltd, Manchester, UK, Am J Respir Crit Care Med 2017; 196: 438–46.
funded by AstraZeneca, Cambridge, UK, in accordance with Good 18 Doty A, Schroeder J, Vang K, et al. Drug delivery from an innovative
Publication Practice (GPP3) guidelines.30 LAMA/LABA co-suspension delivery technology fixed-dose
combination MDI: evidence of consistency, robustness, and
References reliability. AAPS PharmSciTech 2018; 19: 837–44.
1 Global Initiative for Chronic Obstructive Lung Disease. 19 Taylor G, Warren S, Dwivedi S, et al. Gamma scintigraphic
Global strategy for the diagnosis, management and prevention of pulmonary deposition study of glycopyrronium/formoterol metered
COPD, 2018. https://goldcopd.org/wp-content/uploads/2017/11/ dose inhaler formulated using co-suspension delivery technology.
GOLD-2018-v6.0-FINAL-revised-20-Nov_WMS.pdf (accessed Eur J Pharm Sci 2018; 111: 450–57.
July 5, 2018). 20 Celli BR, MacNee W, and Committee members. Standards for the
2 Ding B, Small M, Holmgren U. A cross-sectional survey of current diagnosis and treatment of patients with COPD: a summary of the
treatment and symptom burden of patients with COPD consulting ATS/ERS position paper. Eur Respir J 2004; 23: 932–46.
for routine care according to GOLD 2014 classifications. 21 The Japanese Respiratory Society. Guidelines for the diagnosis and
Int J Chron Obstruct Pulmon Dis 2017; 12: 1527–37. treatment of COPD, 4th Edition, 2013. http://www.jrs.or.jp/uploads/
3 Brusselle G, Price D, Gruffydd-Jones K, et al. The inevitable drift to uploads/files/guidelines/copd_summary_e.pdf (accessed
triple therapy in COPD: an analysis of prescribing pathways in the July 5, 2018).
UK. Int J Chron Obstruct Pulmon Dis 2015; 10: 2207–17. 22 Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference
4 Rennard SI, Tashkin DP, McElhattan J, et al. Efficacy and values from a sample of the general U.S. population.
tolerability of budesonide/formoterol in one hydrofluoroalkane Am J Respir Crit Care Med 1999; 159: 179–87.
pressurized metered-dose inhaler in patients with chronic 23 Sasaki H, Nakamura M, Kida K. Reference values for spirogram and
obstructive pulmonary disease: results from a 1-year randomized blood gas analysis in Japanese adults. J Jpn Respir Soc 2001; 39: S1–17.
controlled clinical trial. Drugs 2009; 69: 549–65.
24 Hankinson JL, Kawut SM, Shahar E, Smith LJ, Stukovsky KH,
5 Calverley PMA, Anderson JA, Celli B, et al. Salmeterol and Barr RG. Performance of American Thoracic Society-recommended
fluticasone propionate and survival in chronic obstructive spirometry reference values in a multiethnic sample of adults:
pulmonary disease. N Engl J Med 2007; 356: 775–89. the multi-ethnic study of atherosclerosis (MESA) lung study.
6 Ferguson GT, Tashkin DP, Skärby T, et al. Effect of Chest 2010; 137: 138–45.
budesonide/formoterol pressurized metered-dose inhaler on 25 Miller MR, Hankinson J, Brusasco V, et al. Standardisation of
exacerbations versus formoterol in chronic obstructive pulmonary spirometry. Eur Respir J 2005; 26: 319–38.
disease: the 6-month, randomized RISE (Revealing the Impact of
26 Suissa S, Drazen JM. Making sense of triple inhaled therapy for
Symbicort in reducing Exacerbations in COPD) study. Respir Med
COPD. N Engl J Med 2018; 378: 1723–24.
2017; 132: 31–41.
27 Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation
7 Ferguson GT, Anzueto A, Fei R, Emmett A, Knobil K, Kalberg C.
in chronic obstructive pulmonary disease. N Engl J Med 2010;
Effect of fluticasone propionate/salmeterol (250/50 µg) or
363: 1128–38.
salmeterol (50 µg) on COPD exacerbations. Respir Med 2008;
102: 1099–108. 28 Bafadhel M, Peterson S, De Blas MA, et al. Predictors of
exacerbation risk and response to budesonide in patients with
8 Crim C, Calverley PM, Anderson JA, et al. Pneumonia risk in
chronic obstructive pulmonary disease: a post-hoc analysis of three
COPD patients receiving inhaled corticosteroids alone or in
randomised trials. Lancet Respir Med 2018; 6: 117–26.
combination: TORCH study results. Eur Respir J 2009; 34: 641–47.
29 Ferguson GT, Reisner C, Pearle J, DePetrillo P, Maes A, Martin UJ.
9 Ernst P, Gonzalez AV, Brassard P, Suissa S. Inhaled corticosteroid
Cardiovascular safety profile of a fixed-dose combination of
use in chronic obstructive pulmonary disease and the risk of
glycopyrrolate and formoterol fumarate delivered via metered dose
hospitalization for pneumonia. Am J Respir Crit Care Med 2007;
inhaler using co-suspension delivery technology.
176: 162–66.
Pulm Pharmacol Ther 2018; 49: 67–74.
10 Wedzicha JA, Banerji D, Chapman KR, et al.
30 Battisti WP, Wager E, Baltzer L, et al. Good publication practice for
Indacaterol-glycopyrronium versus salmeterol-fluticasone for
communicating company-sponsored medical research: GPP3.
COPD. N Engl J Med 2016; 374: 2222–34.
Ann Intern Med 2015; 163: 461–64.
11 Bafadhel M, Pavord ID, Russell REK. Eosinophils in COPD:
just another biomarker? Lancet Respir Med 2017; 5: 747–59.
12 www.thelancet.com/respiratory Published online September 16, 2018 http://dx.doi.org/10.1016/S2213-2600(18)30327-8
You might also like
- Tribute TrialDocument9 pagesTribute TrialMr. LNo ratings yet
- Ethos 2020Document14 pagesEthos 2020Radu CiprianNo ratings yet
- Paper Alumnos 5Document14 pagesPaper Alumnos 5Victor Martinez HagenNo ratings yet
- TRIBUTE Manuscript Peer Amends 19 Jan 2018 PostDocument28 pagesTRIBUTE Manuscript Peer Amends 19 Jan 2018 PostOdessa EnriquezNo ratings yet
- Antacid Therapy and Disease Progression in Patients With Idiopathic Pulmonary Fibrosis Who Received PirfenidoneDocument9 pagesAntacid Therapy and Disease Progression in Patients With Idiopathic Pulmonary Fibrosis Who Received PirfenidoneAquiles CastroNo ratings yet
- Colistin Monotherapy Versus Combination Therapy For Carbapenem-Resistant Organisms NEJM EvidenceDocument27 pagesColistin Monotherapy Versus Combination Therapy For Carbapenem-Resistant Organisms NEJM Evidencerac.oncologyNo ratings yet
- Respiratory Medicine: SciencedirectDocument8 pagesRespiratory Medicine: SciencedirectVasincuAlexandruNo ratings yet
- Terapia Triple para EPOCDocument14 pagesTerapia Triple para EPOCSebastian Cebrian GuerreroNo ratings yet
- Critical Apraisal KLPDocument11 pagesCritical Apraisal KLPANA SRI RAHAYUNo ratings yet
- Real World Experiences Pirfenidone and Nintedanib Are Effective and Well Tolerated Treatments For Idiopathic Pulmonary FibrosisDocument12 pagesReal World Experiences Pirfenidone and Nintedanib Are Effective and Well Tolerated Treatments For Idiopathic Pulmonary FibrosismaleticjNo ratings yet
- PIIS2213260017304745Document10 pagesPIIS2213260017304745Juan Pablo CasanovaNo ratings yet
- Outpatient Treatment of COVID-19 and Incidence of post-COVID-19 Condition Over 10 MonthsDocument11 pagesOutpatient Treatment of COVID-19 and Incidence of post-COVID-19 Condition Over 10 MonthsStavya DubeyNo ratings yet
- Rifampicina TBMR NEJM 2019Document13 pagesRifampicina TBMR NEJM 2019carolinaNo ratings yet
- Asthma Control SABA UseDocument9 pagesAsthma Control SABA UsemapuxdNo ratings yet
- Paper Alumnos 3 PDFDocument10 pagesPaper Alumnos 3 PDFVictor Martinez HagenNo ratings yet
- Paper Alumnos 2Document11 pagesPaper Alumnos 2Victor Martinez HagenNo ratings yet
- 2017 Article 141 Part1Document5 pages2017 Article 141 Part1Karina MonasaNo ratings yet
- 22 - Effect of Noninvasive Respiratory Strategies On Intubation or Mortality Among Patients With Acute Hypoxemic Respiratory Failure and COVID-19 - The RECOVERY-RS RCT - JAMADocument13 pages22 - Effect of Noninvasive Respiratory Strategies On Intubation or Mortality Among Patients With Acute Hypoxemic Respiratory Failure and COVID-19 - The RECOVERY-RS RCT - JAMAThaís CarvalhoNo ratings yet
- A New Strategy in Reliever Therapy Budesonide/Formoterol Maintenance PlusDocument13 pagesA New Strategy in Reliever Therapy Budesonide/Formoterol Maintenance PlusLinto JohnNo ratings yet
- Estrat Gias Ventilat Rias N o Invasivas X Covid 19 1643582558Document13 pagesEstrat Gias Ventilat Rias N o Invasivas X Covid 19 1643582558Thaís CarvalhoNo ratings yet
- Kevin Murphy, MD Michael Noonan, MD Philip E. Silkoff, MD and Thomas Uryniak, MSDocument14 pagesKevin Murphy, MD Michael Noonan, MD Philip E. Silkoff, MD and Thomas Uryniak, MStariqaslNo ratings yet
- A Placebo-Controlled Trial of Oral Fingolimod in Relapsing Multiple SclerosisDocument15 pagesA Placebo-Controlled Trial of Oral Fingolimod in Relapsing Multiple SclerosisNidia BracamonteNo ratings yet
- Ok O'ByrneDocument12 pagesOk O'ByrneChristian OliveiraNo ratings yet
- Jama Naggie 2022 Oi 220112 1665760895.44932Document9 pagesJama Naggie 2022 Oi 220112 1665760895.44932Jeancarlo Ore LazoNo ratings yet
- 10 1056@NEJMoa1715274Document12 pages10 1056@NEJMoa1715274Paul ParrasNo ratings yet
- MeduriDocument4 pagesMeduriSilvia Leticia BrunoNo ratings yet
- Jurnal 4Document7 pagesJurnal 4Lutfi MalefoNo ratings yet
- Copd 16 79Document11 pagesCopd 16 79Karina UtariNo ratings yet
- Thorax 2010 Chapman 747 52 PDFDocument7 pagesThorax 2010 Chapman 747 52 PDFnetifarhatiiNo ratings yet
- Ahmad 2018Document14 pagesAhmad 2018Cristopher OchoaNo ratings yet
- Uji Klinis 4Document9 pagesUji Klinis 4Verliatesya TugasNo ratings yet
- Jamainternal Ortigoza 2021 Oi 210071 1643648313.72397Document12 pagesJamainternal Ortigoza 2021 Oi 210071 1643648313.72397Joaquin OlivaresNo ratings yet
- Tugas RCT SenaDocument10 pagesTugas RCT SenaArfad El HabibieNo ratings yet
- No 2Document6 pagesNo 2Raven RavenNo ratings yet
- PIIS0954611118301215Document9 pagesPIIS0954611118301215TheRainMelodyNo ratings yet
- Article 6Document8 pagesArticle 6Yasmine SlhNo ratings yet
- Nejmoa 2201737Document10 pagesNejmoa 2201737Muthia Farah AshmaNo ratings yet
- E AungDocument9 pagesE AungDr.Hemant SharmaNo ratings yet
- Okour 2019Document18 pagesOkour 2019Carlos EmilioNo ratings yet
- Okour2019 PDFDocument18 pagesOkour2019 PDFCarlos EmilioNo ratings yet
- Nejmoa 1811867Document13 pagesNejmoa 1811867yasserNo ratings yet
- Atorvastatin Improves Sputum Conversion and Chest X-Ray Severity ScoreDocument6 pagesAtorvastatin Improves Sputum Conversion and Chest X-Ray Severity Scorecharmainemargaret.parreno.medNo ratings yet
- Efficacy and Safety of Budesonide Formoterol PMDI Vs Budesonide in Asthmatic ChildrenDocument12 pagesEfficacy and Safety of Budesonide Formoterol PMDI Vs Budesonide in Asthmatic ChildrenmariskaNo ratings yet
- New and Repurposed Drugs To Treat Multidrug-And Extensively Drug-Resistant TuberculosisDocument8 pagesNew and Repurposed Drugs To Treat Multidrug-And Extensively Drug-Resistant TuberculosisJUAN SARMIENTONo ratings yet
- Ashina2020 Article EfficacyTolerabilityAndSafetyODocument9 pagesAshina2020 Article EfficacyTolerabilityAndSafetyOFirjatullahNo ratings yet
- Articulo NeumologiaDocument11 pagesArticulo NeumologiaHernandoJoseViloriaSanchezNo ratings yet
- BMJ j3887 FullDocument10 pagesBMJ j3887 FullRiri Maisytoh PutriNo ratings yet
- Adalimumab Plus Methotrexate For Uveitis in Juvenile Idiopathic ArthritisDocument17 pagesAdalimumab Plus Methotrexate For Uveitis in Juvenile Idiopathic ArthritisaisNo ratings yet
- Extrafine Triple Therapy Delays Copd Clinically Important Deterioration Vs Ics/Laba, Lama, or Laba/LamaDocument16 pagesExtrafine Triple Therapy Delays Copd Clinically Important Deterioration Vs Ics/Laba, Lama, or Laba/LamatriNo ratings yet
- A Randomized, Controlled Trial of Liraglutide For Adolescents With ObesityDocument12 pagesA Randomized, Controlled Trial of Liraglutide For Adolescents With ObesityWarun KumarNo ratings yet
- A Ten-Year Survey of Treatment Outcome in A Tuberculosis and Leprosy Referral Hospital Implementing Directly Observed Therapy Short (DOTS) CourseDocument5 pagesA Ten-Year Survey of Treatment Outcome in A Tuberculosis and Leprosy Referral Hospital Implementing Directly Observed Therapy Short (DOTS) CourseInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Jamainternal Qian 2022 Oi 220014 1649953506.76147Document10 pagesJamainternal Qian 2022 Oi 220014 1649953506.76147Mesan KoNo ratings yet
- JournalDocument3 pagesJournalKurt ZepedaNo ratings yet
- 131 135Document5 pages131 135Hananto DwiandonoNo ratings yet
- 360 1442 2 PBDocument8 pages360 1442 2 PBEghar EverydayishellNo ratings yet
- Original Contributions: A Randomized Trial Comparing Metered Dose Inhalers and Breath Actuated NebulizersDocument8 pagesOriginal Contributions: A Randomized Trial Comparing Metered Dose Inhalers and Breath Actuated NebulizersDesmiyati AdoeNo ratings yet
- Efficacy and Safety of SildenafilDocument9 pagesEfficacy and Safety of SildenafilArif Nurhadi AtmokoNo ratings yet
- FichaDocument9 pagesFichamariaNo ratings yet
- Tantalizing Therapeutics in Bronchopulmonary DysplasiaFrom EverandTantalizing Therapeutics in Bronchopulmonary DysplasiaVineet BhandariNo ratings yet
- Management of Fungal Infections in MCS and Cardiothoracic Organ Transplant Recipients: ISHLT Monograph Series (Volume 12)From EverandManagement of Fungal Infections in MCS and Cardiothoracic Organ Transplant Recipients: ISHLT Monograph Series (Volume 12)No ratings yet
- Ferguson 2018 Co-SuspensieDocument8 pagesFerguson 2018 Co-SuspensieRadu CiprianNo ratings yet
- Usmani 2021 AerosphereDocument12 pagesUsmani 2021 AerosphereRadu CiprianNo ratings yet
- Martinez 2021Document11 pagesMartinez 2021Radu CiprianNo ratings yet
- Stone Champion PH PDFDocument10 pagesStone Champion PH PDFRadu CiprianNo ratings yet
- Dargaville 2021Document10 pagesDargaville 2021Radu CiprianNo ratings yet
- Pediatric Pulmonology 2021, Dell'ortoDocument8 pagesPediatric Pulmonology 2021, Dell'ortoRadu CiprianNo ratings yet
- Webster 2010 Horizons-AmiDocument1 pageWebster 2010 Horizons-AmiRadu CiprianNo ratings yet
- Price Et Al., International Journal of Chronic Obstructive Pulmonary Disease 2022Document16 pagesPrice Et Al., International Journal of Chronic Obstructive Pulmonary Disease 2022Radu CiprianNo ratings yet
- Singh 2015 PDFDocument83 pagesSingh 2015 PDFRadu CiprianNo ratings yet
- Canadian Guidelines 2021Document7 pagesCanadian Guidelines 2021Radu CiprianNo ratings yet
- Gunther H., Elsevier, Pharmacokinetic and Pharmacodynamic Properties Important For ICSDocument9 pagesGunther H., Elsevier, Pharmacokinetic and Pharmacodynamic Properties Important For ICSRadu CiprianNo ratings yet
- Abdullah A. K., Et Al, 2007, J. Asthma, Evidence-Based Selection of Inhaled Corticosteroid For Treatment of Chronic AsthmaDocument13 pagesAbdullah A. K., Et Al, 2007, J. Asthma, Evidence-Based Selection of Inhaled Corticosteroid For Treatment of Chronic AsthmaRadu CiprianNo ratings yet
- Kuna P. Et Al, Pharmacokinetics of Extrafine Beclometasone Dipropionate Formoterol FumarateDocument8 pagesKuna P. Et Al, Pharmacokinetics of Extrafine Beclometasone Dipropionate Formoterol FumarateRadu CiprianNo ratings yet
- Fly 10 Your Super FutureDocument3 pagesFly 10 Your Super FutureRichard Colón67% (3)
- 18 Empathy Statements That Help Improve CustomerDocument4 pages18 Empathy Statements That Help Improve Customeriammiguelsalac100% (3)
- Natural Lighting at The Kimbell Museum: Gifford Pierce of IdahoDocument5 pagesNatural Lighting at The Kimbell Museum: Gifford Pierce of IdahoPriscilia ElisabethNo ratings yet
- Manufacturing MethodsDocument33 pagesManufacturing MethodsRafiqueNo ratings yet
- Self Healing ConcreteDocument20 pagesSelf Healing ConcreteshivangNo ratings yet
- Pellet PLNT ManualDocument19 pagesPellet PLNT ManualsubhankarprustyNo ratings yet
- Department of Education: Republic of The PhilippinesDocument4 pagesDepartment of Education: Republic of The PhilippinesEllen Cabatian BanaguasNo ratings yet
- Saptamsa and Navamsa Charts PDFDocument37 pagesSaptamsa and Navamsa Charts PDFjyothiNo ratings yet
- Law of Insurance Eighth Semester SyllabusDocument3 pagesLaw of Insurance Eighth Semester SyllabusAastha PrakashNo ratings yet
- The Trouble With UV LightDocument3 pagesThe Trouble With UV LightSàkâtã ÁbéŕàNo ratings yet
- 80312A-ENUS Error LogDocument10 pages80312A-ENUS Error LogSafdar HussainNo ratings yet
- MagnetismDocument30 pagesMagnetismManiratna RoyNo ratings yet
- GL Poseidon User ManualDocument256 pagesGL Poseidon User ManualIrina MaltopolNo ratings yet
- Experiment No. 2 Introduction To Combinational Circuits: Group Name: Group 7 Group Leader: JOSE DOROSAN Group MemberDocument11 pagesExperiment No. 2 Introduction To Combinational Circuits: Group Name: Group 7 Group Leader: JOSE DOROSAN Group MemberJoy PeconcilloNo ratings yet
- 11 - NRG - Cathodic Protection DesignDocument15 pages11 - NRG - Cathodic Protection DesignBalan100% (1)
- 2011 2012 Machinery SubsidyDocument130 pages2011 2012 Machinery SubsidyanbugobiNo ratings yet
- Behavior of RC Shallow and Deep Beams WiDocument26 pagesBehavior of RC Shallow and Deep Beams WiSebastião SimãoNo ratings yet
- Lord Dyrron Baratheon, Warden of the StormlandsDocument2 pagesLord Dyrron Baratheon, Warden of the StormlandsDaniel AthertonNo ratings yet
- VI. 07. Synchronous Machine PDFDocument16 pagesVI. 07. Synchronous Machine PDFDesi HertianiNo ratings yet
- How Society Is Organized Chapter 5Document18 pagesHow Society Is Organized Chapter 5Anne MoralesNo ratings yet
- CYPE Box CulvertsDocument4 pagesCYPE Box CulvertsEng Venance MasanjaNo ratings yet
- Career PlanDocument1 pageCareer Planapi-367263216No ratings yet
- ASCO Switch CatalogDocument38 pagesASCO Switch Catalogjohnnie0% (1)
- ) Perational Vlaintena, Nce Manual: I UGRK SeriesDocument22 pages) Perational Vlaintena, Nce Manual: I UGRK Seriessharan kommiNo ratings yet
- Autotrol PerformaLOGIX 740 760 ManualDocument68 pagesAutotrol PerformaLOGIX 740 760 ManualHyacinthe KOSSINo ratings yet
- Concrete Mix Design Report for M20 GradeDocument5 pagesConcrete Mix Design Report for M20 GradesatishNo ratings yet
- PSD SiemensDocument45 pagesPSD Siemensbrijendra2185% (13)
- Vector Network AnalyzersDocument33 pagesVector Network AnalyzersRea Gusti HermawanNo ratings yet
- Control Systems GEDocument482 pagesControl Systems GECarlos ACNo ratings yet
- 4EA1 01R Que 20180606Document20 pages4EA1 01R Que 20180606Shriyans GadnisNo ratings yet