Professional Documents
Culture Documents
Respiratory Pathology ARDS
Uploaded by
Pranav PunjabiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Respiratory Pathology ARDS
Uploaded by
Pranav PunjabiCopyright:
Available Formats
Last edited: 11/5/2021
13. ACUTE RESPIRATORY DISTRESS SYNDROME (ARDS)
Acute Respiratory Distress Syndrome (ARDS) Medical Editor: Sohani Kashi Puranic
OUTLINE
I) OVERVIEW
II) DEFINITION
III) CAUSES
IV) PATHOPHYSIOLOGY
V) DIAGNOSIS
VI) TREATMENT
VII) SUMMARY
VIII) APPENDIX
IX) REVIEW QUESTIONS
X) REFERENCES
I) OVERVIEW Figure 1. Pneumonia causing ARDS
Diffuse damage to the alveolar capillary interface is the (2) Aspiration Pneumonia
main cause of Acute Respiratory Distress Syndrome Aspiration of gastric contents
(ARDS) o Gastric acid, bacteria→ Injury to lung parenchyma
It is often secondary to a variety of disease processes
including sepsis, infection, shock, trauma, aspiration,
pancreatitis, DIC, hypersensitivity reactions and drugs
Treatment includes addressing the underlying cause and
ventilation
[Pathoma]
II) DEFINITION
ACUTE RESPIRATORY DISTRESS SYNDROME (ARDS) is a
manifestation of severe ACUTE LUNG I NJURY (ALI)
ALI is characterized by the abrupt onset of hypoxemia
and bilateral pulmonary edema in absence of cardiac Figure 2. Aspiration Pneumonia causing ARDS
failure (non- cardiogenic pulmonary edema)
(3) Lung Contusions
Trauma→ Injury to lung parenchyma
The major underlying pathology in ARDS is
DIFFUSE ALVEOLAR DAMAGE
[Robbins]
Figure 3. Lung Contusions causing ARDS
III) CAUSES
(4) Near Drowning
ARDS is produced as a consequence of Acute Lung
Injury (i) Drowning in Sea Water
Injury to the lung can be
a. Direct
b. Indirect
(A) DIRECT CAUSES
(1) Pneumonia
(ii) Drowning in Fresh Water
(i) Streptococcus pneumoniae
(ii) Staphylococcus aureus
(iii) Pneumocystis jiroveci
(iv) SARS- CoV-2
(v) Mycobacterium tuberculosis
Figure 4. Near Drowning causing ARDS
Acute Respiratory Distress Syndrome (ARDS) RESPIRATORY PATHOLOGY: Note #13. 1 of 12
(5) Toxic Smoke (2) Pancreatitis
(i) Oxygen toxicity Can cause ARDS by:
(ii) Smoke (i) Release of Cytokines
(iii) Irritant gases and Chemicals (ii) Release of Pancreatic Enzymes
Both cause
(i) Capillaries to become leaky, due to:
(a) Vasodilation
(b) ↑ Vascular Permeability
(ii) Damage to:
(a) Capillary endothelium
Figure 5. Toxic Smoke causing ARDS (b) Alveolar epithelium
(B) INDIRECT CAUSES Damaged and leaky capillaries cause
Indirect causes of ARDS include systemic conditions
where there is:
These cause damage to capillary endothelium and
subsequently, alveolar epithelium
(1) Sepsis
Infectious pathogen enters the body
IL-1
IL-6
TNF-α Figure 7. Acute Pancreatitis causing ARDS
(3) Multiple long bone Fractures
(i) Capillaries to become leaky, due to: Due to multiple fractures, fat globules from the medulla
leak out
(a) Vasodilation
(b) ↑ Vascular Permeability
(ii) Damage to:
(a) Capillary endothelium Damaged and leaky capillaries cause
(b) Alveolar epithelium
SEPSIS is the MOST COMMON cause of ARDS
Figure 8. Long bone fractures causing ARDS
Figure 6. Sepsis causing ARDS
2 of 12 RESPIRATORY PATHOLOGY: Note #13. Acute Respiratory Distress Syndrome (ARDS)
(4) TRALI (A) INJURY TO PNEUMOCYTES
T RANSFUSION ASSOCIATED LUNG I NJURY (1) Pneumocytes
Most commonly seen in transfusions of:
Type 1 Type 2
(i) Fresh Frozen Plasma Pneumocyte Pneumocyte
(ii) Cryoprecipitate Cell Type Simple Squamous Cuboidal
Number 95% 5%
Function Production of
Gas Exchange
Surfactant
Consequence
No Gas Exchange Alveolar Collapse
of Damage
Ability to Yes, they are
No- Amitotic
Divide Stem cells
Appearance
(a) Cytokines
(b) Proteases
(c) Reactive Oxygen Species (ROS)
(2) Injury to Pneumocytes
The etiological agents cause damage to the Type I and
Type II Pneumocytes. Due to this:
(i) Triggers release of Cytokines/ Recognition particles
(ii) Cytokines activate Alveolar Macrophages
Alveolar macrophages are activated
1. By Cytokines
2. Directly by the pathogen
Macrophages then release:
1. IL-1
2. IL-6
3. IL-8
4. TNF-α
Figure 9. TRALI resulting in ARDS
(5) Drugs (i) Affect Endothelium
(i) Cocaine o ↑ Capillary Permeability
o ↑ Cell Adhesion Molecule (CAM)
(ii) Opioids expression
(iii) Aspirin toxicity
(ii) Activate Neutrophils
(iii) Damage channels on Type II
Pneumocytes
o When there is ↑ fluid in alveoli, the fluid is
taken up by Type II Pneumocytes by
channels and then expelled from the
alveoli
o When these channels are damaged, the
excess fluid accumulated is not
reabsorbed
(iii) These processes cause INFLAMMATION & EDEMA
Figure 10. Drugs causing ARDS
IV) PATHOPHYSIOLOGY
Figure 11. Time course for development and resolution of
ARDS
[Harrison's Principles of Internal Medicine, p. 2031 Fig. 294-1]
Figure 12. Injury to Pneumocytes
Acute Respiratory Distress Syndrome (ARDS) RESPIRATORY PATHOLOGY: Note #13. 3 of 12
(B) EXUDATIVE PHASE
(1) IL-1, IL-6, TNF-α
(i) ↑ Capillary Permeability
(ii) ↑ Expression of Cell Adhesion Molecules
(2) IL-8
Causes Chemotaxis Figure 13. Diffuse alveolar damage. Hyaline Membrane shown
by arrows.
[Robbins & Cotran Pathologic Basis of Disease. p. 677 Fig. 15.4]
(3) Neutrophils in Alveoli
(i) Neutrophils enter Alveoli
By action of IL-1, IL-6, TNF-α, IL-8
(ii) Degranulation of Neutrophils
Neutrophils then release:
(a) Reactive Oxygen Species (ROS)
(b) Proteases
(c) Neutrophil Extracellular Traps (NETs)
These damage Type I & Type II Pneumocytes
(iii) Damage of alveolar epithelium
(iv) Fluid accumulates in Alveoli
Fluid collected in interstitium leaks into alveoli
through damaged epithelium
(v) Formation of Hyaline Membrane
Fluid from interstitium accumulates in alveoli
This edematous fluid contains Proteins, which
also accumulates
Fibrin deposition occurs Figure 14. Exudative Phase with Formation of Hyaline
Cellular debris (dead cells) collects as Type I & II Membrane
Pneumocytes are destroyed
WBCs accumulate as they are recruited (C) PATHOGENESIS OF SIGNS AND SYMPTOMS
Few RBCs are collected (1) Hypoxemia
(i) Damage to Type II Pneumocytes
(vi) Hypoxemia
When Oxygen enters the alveoli, it has to pass
through a greater distance due to formation of (ii) Fluid accumulating in alveoli washes away
hyaline membrane surfactant
(iii) Surface Tension ↑
Hyaline Membrane =
Edematous Fluid + Proteins+ Fibrin+
Cellular Debris + WBCs + RBCs
Figure 15. Surfactant
4 of 12 RESPIRATORY PATHOLOGY: Note #13. Acute Respiratory Distress Syndrome (ARDS)
(D) PHASE OF PROLIFERATION
(1) Resolution
LAPLACE LAW
(i) Re-epithelialization
𝟐𝟐𝟐𝟐 Repair of Type I & Type II Pneumocytes
𝑷𝑷 =
𝑹𝑹
P= Collapsing Pressure
T= Surface Tension
(ii) Removal of fluid from alveoli
R= Radius of Alveoli
Type II Pneumocytes reabsorb the fluid and
expel it from the alveoli
When T↑, P also ↑ as it is directly
(E) PHASE OF FIBROSIS
proportional
In some cases, is granulation tissue doesn’t resolve, it
leads to fibrosis
(2) Consequences of Hypoxemia o Macrophages, Neutrophils
(i) Cyanosis
Bluish discoloration of mucus membranes
(ii) Reflex Compensatory Mechanisms
(i) Compression of vessels
(a) Tachypnoea (ii) Makes lungs very rigid
(iii) Decreased lung compliance
(b) Tachycardia
(iii) ‘Crackles’ on Auscultation
Fluid accumulation in alveoli
↑ work of respiration
Figure 17. Resolution and Fibrosis
Figure 16. Signs and Symptoms of ARDS
Acute Respiratory Distress Syndrome (ARDS) RESPIRATORY PATHOLOGY: Note #13. 5 of 12
V) DIAGNOSIS
BERLIN CRITERIA FOR ARDS
(1) Acute Respiratory Failure
o Diagnose the initial cause. Ex, for Sepsis:
Figure 18. Acute Respiratory Failure
(2) Bilateral Opacities Figure 20. Chest X-Ray in ARDS
(ii) CT
o Imaging includes:
GROUND- GLASS APPEARANCE
Bilateral consolidation
Figure 19. Bilateral Opacities
(i) Chest X-Ray
CHEST X-RAY
Indications: all patients suspected of having ARDS
Findings:
(i) Acute findings (1–7 days)
Often normal in the first 24 hours
Diffuse bilateral symmetrical infiltrates Figure 21. CT Scan in ARDS
In severe cases: bilateral attenuations that make
the lung appear white on x-ray (“WHITE LUNG”)
Air bronchograms may be visible (iii) Ultrasound
B- LINES
(ii) Intermediate (8–14 days) to late (> 15 days)
findings Supportive evidence for ARDS:
Typical course: Acute features remain stable, then
resolve
Fibrotic course: RETICULAR OPACITIES begin to
appear and may become permanent
(iii) Findings supportive of ARDS rather than CHF
Predominantly peripheral opacities
Small or absent pleural effusions
No cardiomegaly or septal lines
[AMBOSS]
6 of 12 RESPIRATORY PATHOLOGY: Note #13. Acute Respiratory Distress Syndrome (ARDS)
(3) ↓P/F Ratio (4) Non-Cardiogenic Pulmonary Edema
Rule out cardiogenic causes of respiratory failure
𝑃𝑃 𝑃𝑃𝑃𝑃𝑃𝑃2
= (i) ECHO
𝐹𝐹 𝐹𝐹𝐹𝐹𝐹𝐹2 Left Ventricular Ejection Fraction (LVEF)- should
PAO2= Partial Pressure of Oxygen be normal
FIO2= Fraction of Inspired Oxygen
Example, normally: (ii) BNP
𝑃𝑃 100 Should be normal
= = 476
𝐹𝐹 0.21 Increased in Congestive Heart Failure (CHF)
(i) Mild ARDS
P/F: 200-300 (iii) PCWP
𝑃𝑃 100 Pulmonary Capillary Wedge Pressure- should be
= = 250
𝐹𝐹 0.40 <18mmHg
(ii) Moderate ARDS
Estimated by Swan Ganz Catheter
P/F: 100-200
𝑃𝑃 100
= = 166
𝐹𝐹 0.60
(iii) Severe ARDS
P/F: <100
𝑃𝑃 90
= = 90
𝐹𝐹 1
Figure 23. Non-Cardiogenic Pulmonary Edema
Mnemonic for Berlin Criteria
“ARDS”
Abnormal Chest X-Ray
Respiratory Failure that ensues <1 week of initial cause
Decreased P/F ratio
Should exclude CHF
Figure 22. Decreased P/F ratio
Figure 24. Diagnostic Criteria for ARDS
[Harrison's Principles of Internal Medicine, p. 2031 Table. 294-2]
Acute Respiratory Distress Syndrome (ARDS) RESPIRATORY PATHOLOGY: Note #13. 7 of 12
VI) TREATMENT
Figure 25. Treatment of ARDS
Mild ARDS
(B) NIPPV
(1) Hemodynamically Stable
NON-I NVASIVE POSITIVE PRESSURE VENTILATION
(1) High Flow Nasal Canula (HFNC)
(2) Hemodynamically Unstable (i) ↑ flow rate of oxygen
(50-60L/min)
(ii) ↓ Dead space
(iii) ↑ PEEP
Intubation- Lung Protective Ventilation
POSITIVE -END EXPIRATORY PRESSURE
(1) If P/F< 150:
(i) Reduces work of breathing
(ii) Improves Oxygenation
(2) If patient has COVID, additional medications should
be given: (iv) Can control FIO2
up to 100%
(2) Bi- Level Positive Airway Pressure (BIPAP)
Used if there is atelectasis
(i) IPAP + EPEP (PEEP)
IPAP= I NSPIRATORY P OSITIVE AIRWAY
PRESSURE
EPAP= EXPIRATORY P OSITIVE AIRWAY
PRESSURE
(ii) Can control FIO2
up to 100%
Disadvantage:
BIPAP would push the mucus down the airway,
forming a plus
This would cause ↓↓ SpO2
Figure 26. Algorithm for Management of ARDS
[Harrison's Principles of Internal Medicine, p. 2034 Fig. 294-5]
Figure 27. NIPPV
8 of 12 RESPIRATORY PATHOLOGY: Note #13. Acute Respiratory Distress Syndrome (ARDS)
(C) LUNG PROTECTIVE VENTILATION (3) FIO2
(1) Tidal Volume (TV)
Goal: ↑ FiO2
Ideal: ≥ 60%
Goal: Low TV Strategies
SpO2 target: 85-95%
Ideal: 4-6cc/kg of Ideal Body
Weight
Augments oxygenation
Tidal Volume is the best indicator for mortality
(i) Consequences of ↑ TV
(ii) Consequences of ↓ TV
Figure 29. Lung Protective Ventilation
MAINTENANCE OF PRESSURES
(i) Plateau Pressure (PPLAT)
For measurement of degree of lung injury
↑ PPLAT
i. T IDAL V OLUME - most significant
ii. PEEP- when highly increased, it raises
PPLAT
Causes lung injury
Lower TV
Figure 28. P-V curve of lungs in a patient undergoing If TV is at minimum, then lower PEEP
Mechanical Ventilation
[Harrison's Principles of Internal Medicine, p. 2036 Fig. 295-1] (ii) Driving Pressure (DP)
(2) Positive End-Expiratory Pressure (PEEP) DP = PPLAT – PEEP
When DP= 15 cmH2O, there is reduced mortality
Goal: ↑↑ PEEP
Ideal: ≥ 5cm H2O
PEEP is the pressure at the END of expiration
Function:
(i) During Inspiration
(ii) During Expiration
• This ↓ work of breathing
• Augments oxygenation
↑ PEEP ⇒ ↑O2
Acute Respiratory Distress Syndrome (ARDS) RESPIRATORY PATHOLOGY: Note #13. 9 of 12
(D) PRONE POSITIONING (F) PARALYTICS
Prone positioning reduces mortality Lung Protective Ventilation adopts a low TV strategy
The dependent position of lungs is the Posterior Lung
Fields Due to decreased oxygen concentration, the
patient’s body tries to respire OVER the ventilator
(1) Supine Position
This is achieved by:
In supine position, heart presses on consolidated lung
(1) Sedation
tissue
(i) Propofol
(2) Prone Position (ii) Midazolam
In prone position, heart presses anteriorly (iii) Opioid bolus
(2) Paralysis of Respiratory Muscles
(i) Cisatracurium besylate
Figure 30. Prone Positioning
(E) INHALED PULMONARY VASODILATORS
(i) Nitric Oxide
(ii) PGI2
Figure 32. Paralytics
(G) ECMO
EXTRA CORPOREAL MEMBRANE OXYGENATION
Figure 31. Inhaled Pulmonary Vasodilators
Figure 33. ECMO
10 of 12 RESPIRATORY PATHOLOGY: Note #13. Acute Respiratory Distress Syndrome (ARDS)
VII) SUMMARY
(A) CAUSES
(C) DIAGNOSIS
(1) Direct Causes Berlin Criteria
Pneumonia Acute Respiratory Failure
Aspiration pneumonia Bilateral opacities
Lung Contusions Decreased P/F ratio
Near drowning Should exclude cardiogenic causes of pulmonary edema
Toxic smoke
(D) TREATMENT
(2) Indirect causes
NIPPV
Sepsis
Pancreatitis
Multiple long bone fractures
TRALI Intubation
Drugs Lung Protective Ventilation
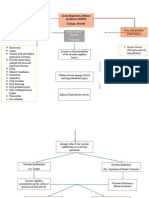
(B) PATHOGENESIS
Prone positioning
Inhaled pulmonary vasodilators
Paralytics
ECMO
VIII) APPENDIX
Figure 34. Pathogenesis of ARDS
The normal alveolus (left side) compared with the injured alveolus in the early phase of acute lung injury and acute respiratory distress
syndrome. IL-1, Interleukin-1; ROS, reactive oxygen species; TNF, tumor necrosis factor. (Modified with permission from Matthay MA, Ware LB, Zimmerman GA: The
acute respiratory distress syndrome, J Clin Invest 122:2731, 2012.)
[Robbins & Cotran Pathologic Basis of Disease. p. 677 Fig. 15.3]
Acute Respiratory Distress Syndrome (ARDS) RESPIRATORY PATHOLOGY: Note #13. 11 of 12
IX) REVIEW QUESTIONS
6) A 62-year-old woman was diagnosed with ARDS was
1) What is the main pathomechanism of ARDS? put on mechanical ventilation. What is the long-term
a) Thickening of pleura complication due to her condition?
b) Diffuse alveolar damage a) Increased compliance of lung
c) Granuloma formation b) Interstitial lung disease
d) Autoimmune mechanism c) Granuloma formation
d) Sepsis
2) What does Hyaline Membrane comprise of?
a) Hyaline cartilage of trachea present within alveoli 7) A 48-year-old man comes to the ER with complaints
b) Transudate, fibrin and cellular debris of sudden onset abdominal pain, which radiates
c) Exudate, fibrin and necrotic epithelial cells through the back to the shoulders. He gives history
d) Aspirated fluid, fibrin, WBCs, RBCs of vomiting the previous day. He also complains of
nausea and dyspnea. What is the most likely finding
in this patient?
3) Which is the most common cause of ARDS?
a) Myocardial ischemia
a) Sepsis
b) Accumulation of fluid in interstitial spaces of alveoli
b) Acute Pancreatitis
c) Heart failure
c) Pneumonia
d) Thickening of pleura and accumulation of fluid in
d) Trauma
pleural cavity
4) Which is the most significant factor for maintaining
8) A patient with ARDS is started on oxygen therapy.
Plateau Pressure?
His hypoxemia however, does NOT improve. What
a) Tidal Volume
could be the reason for this, owing to the disease?
b) PEEP
a) Ventilation-perfusion mismatch
c) FIO2
b) Low concentration of oxygen given
d) Both a & b
c) Block in the tracheobronchial tree
d) Past history of asthma
5) All are signs & symptoms of ARDS, EXCEPT:
a) Cyanosis X) REFERENCES
b) Tachypnoea ● Kumar, V., Abbas, A. K., & Aster, J. C. (2021). Robbins and
c) Respiratory acidosis Cotran pathologic basis of disease (tenth edition.). Philadelphia, PA:
d) Respiratory alkalosis Elsevier/Saunders.
● Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL,
Loscalzo J. Harrison's Principles of Internal Medicine, Twentieth
Edition (Vol.1 & Vol.2). McGraw-Hill Education / Medical; 2018
● Pathoma.com (2021)
● Le, Tao; Bhushan, Vikas; and Sochat, Matthew. First Aid for the
USMLE Step 1 2021. New York: McGraw-Hill Education, 2021.
12 of 12 RESPIRATORY PATHOLOGY: Note #13. Acute Respiratory Distress Syndrome (ARDS)
You might also like
- MR Loveday Little Outing Day AnalysisDocument4 pagesMR Loveday Little Outing Day AnalysisLorenaGeninSantaCruz40% (10)
- Lung - PathologyDocument34 pagesLung - Pathologyjmosser100% (3)
- Checklist For Local Anesthetic Toxicity Treatment 1-18-12Document2 pagesChecklist For Local Anesthetic Toxicity Treatment 1-18-12Akilesh RamasamyNo ratings yet
- Cardiovascular Pathology - 025) Valvular Heart Diseases Overview (Notes)Document18 pagesCardiovascular Pathology - 025) Valvular Heart Diseases Overview (Notes)Geraldine HernandezNo ratings yet
- Non-Modifiable Risk Factor Modifiable Risk Factors: Acute Respiratory Distress Syndrome (ARDS) (Lungs Alveoli)Document3 pagesNon-Modifiable Risk Factor Modifiable Risk Factors: Acute Respiratory Distress Syndrome (ARDS) (Lungs Alveoli)joyrena ochondraNo ratings yet
- Ards PDFDocument20 pagesArds PDFRuki HartawanNo ratings yet
- Acute/Adulth Respiratory Distress Syndrome (ARDS) : RohmanDocument54 pagesAcute/Adulth Respiratory Distress Syndrome (ARDS) : RohmanMuhammad Rizki Junaidi SaputraNo ratings yet
- 1.04 GEN PATH LAB REALLS-Fluid and Hemodynamics UEDocument5 pages1.04 GEN PATH LAB REALLS-Fluid and Hemodynamics UEAllysa Marie CotandaNo ratings yet
- Pollution - Solved-Examples Solved-ExampleDocument6 pagesPollution - Solved-Examples Solved-ExampleBharati GulajkarNo ratings yet
- Covid and Ebola MsDocument7 pagesCovid and Ebola MsAimee Rochelle MaesaNo ratings yet
- 2 Respiratory Medicine: Streptococcus Pneumoniae Klebsiella Pneumoniae Legionella Pneumophila Mycoplasma PneumoniaeDocument24 pages2 Respiratory Medicine: Streptococcus Pneumoniae Klebsiella Pneumoniae Legionella Pneumophila Mycoplasma Pneumoniaesultan khabeeb100% (1)
- Respiratory-Renal Block, Practical IDocument37 pagesRespiratory-Renal Block, Practical Imina mounirNo ratings yet
- A Tricompartmental Model of Lung Oxygenation Disruption To Explain Pulmonary and Systemic Pathology in Severe COVID-19Document8 pagesA Tricompartmental Model of Lung Oxygenation Disruption To Explain Pulmonary and Systemic Pathology in Severe COVID-19alvaro millanNo ratings yet
- Path Lung McqsDocument24 pagesPath Lung McqsShafaque IrfanNo ratings yet
- Doxycycline: From Ocular Rosacea To COVID-19 Anosmia. New Insight Into The Coronavirus OutbreakDocument4 pagesDoxycycline: From Ocular Rosacea To COVID-19 Anosmia. New Insight Into The Coronavirus OutbreakAndhi Riawan Eko WiikramatunggadewaNo ratings yet
- Chronic Obstructive Pulmonary Disease: Iman Galal, MDDocument60 pagesChronic Obstructive Pulmonary Disease: Iman Galal, MDYan Sheng HoNo ratings yet
- Covid Fisiopato InglesDocument8 pagesCovid Fisiopato InglesaarongondraNo ratings yet
- Answer: CHAPTER 1 Stimuli and ResponsesDocument8 pagesAnswer: CHAPTER 1 Stimuli and Responses林柄洲No ratings yet
- Endothelial Dysfunction in COVID-19 Potential Mechanisms and Possible Therapeutic OptionsDocument24 pagesEndothelial Dysfunction in COVID-19 Potential Mechanisms and Possible Therapeutic OptionssamuelNo ratings yet
- Lobar Pneumonia: Deevon M. Cariaga FEU-NRMF Institute of MedicineDocument12 pagesLobar Pneumonia: Deevon M. Cariaga FEU-NRMF Institute of MedicinedeevoncNo ratings yet
- Pathophysiology of COVID19: Deekshya Devkota 8025Document2 pagesPathophysiology of COVID19: Deekshya Devkota 8025Deekshya DevkotaNo ratings yet
- Coomon Diseases & DescriptionsDocument1 pageCoomon Diseases & Descriptionsdheeraj kumarNo ratings yet
- Test 7 XI - Unit5Document9 pagesTest 7 XI - Unit5Tamal NayakNo ratings yet
- Neet Class 11 Morning Batch 1705736322Document15 pagesNeet Class 11 Morning Batch 1705736322thetom1245No ratings yet
- UntitledDocument34 pagesUntitledDr.younes95 RekaaneyNo ratings yet
- Hnizdo 2003Document8 pagesHnizdo 2003Dang QuanNo ratings yet
- Pneumonia Parient BasedDocument2 pagesPneumonia Parient BasedKismet SummonsNo ratings yet
- Articulo Fisiopatologia de La Enfermedad 2Document5 pagesArticulo Fisiopatologia de La Enfermedad 2ivanNo ratings yet
- ICU Department ICU DepartmentDocument48 pagesICU Department ICU DepartmentEmad ElhusseinNo ratings yet
- Diseases MSDocument6 pagesDiseases MSKajolNo ratings yet
- Emergency Radiologic Approach To Sinus Disease: Matthew R. Mccann Alexander T. Kessler Alok A. BhattDocument8 pagesEmergency Radiologic Approach To Sinus Disease: Matthew R. Mccann Alexander T. Kessler Alok A. BhattVidya PasaribuNo ratings yet
- Pulmonary Immuno-Thrombosis in COVID-19 ARDS PathogenesisDocument4 pagesPulmonary Immuno-Thrombosis in COVID-19 ARDS PathogenesisXavier AbrilNo ratings yet
- Subcutaneous Emphysema Complicated by COVID-19 Infection Case Report and Literature ReviewDocument3 pagesSubcutaneous Emphysema Complicated by COVID-19 Infection Case Report and Literature ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Supplemental Chapter 2 Intersitial Lung Disease: A Picture BookDocument13 pagesSupplemental Chapter 2 Intersitial Lung Disease: A Picture Bookpablo carednasNo ratings yet
- 5 THDocument6 pages5 THArnav GuptaNo ratings yet
- Interstitial Lung DiseaseDocument66 pagesInterstitial Lung DiseaseGrant Wynn ArnucoNo ratings yet
- FC Rad Diag (SA) Part II Past Papers - 2021 1st Semester 30 11 2022Document4 pagesFC Rad Diag (SA) Part II Past Papers - 2021 1st Semester 30 11 2022asdsaNo ratings yet
- Acute Respiratory Distress Syndrome by Mr. Ashish RoyDocument45 pagesAcute Respiratory Distress Syndrome by Mr. Ashish RoySyedzulqurnainhussainshah ZulqurnainNo ratings yet
- Assignmnet 2 Soltn - ESC 202Document4 pagesAssignmnet 2 Soltn - ESC 202Nidhi MalikNo ratings yet
- Y11 Biology Mock Exam Questions and MS-RRRDocument75 pagesY11 Biology Mock Exam Questions and MS-RRRsaeedshahidNo ratings yet
- Atrial Fibrillation AtfDocument11 pagesAtrial Fibrillation AtfChristine MagnoNo ratings yet
- Norma, PathoDocument3 pagesNorma, PathoHazelyn CayleNo ratings yet
- Atelectasis: Contraction Atelectasis (Or Cicatrization Atelectasis)Document10 pagesAtelectasis: Contraction Atelectasis (Or Cicatrization Atelectasis)Gan BangNo ratings yet
- 0052 - Kadek Diana Susilawati - LP Luka BakarDocument11 pages0052 - Kadek Diana Susilawati - LP Luka BakarDiana IdNo ratings yet
- Cell Injury Electronic or Printed Copies of These Slides!!: Pathology I ImagesDocument20 pagesCell Injury Electronic or Printed Copies of These Slides!!: Pathology I ImagesMiile EstrellitaaNo ratings yet
- Necropsy of The Pig - EoDocument6 pagesNecropsy of The Pig - EoMaverick LastimosaNo ratings yet
- Chapter13 and 14 HeiDocument90 pagesChapter13 and 14 HeiAyieMz Iverson SolisNo ratings yet
- The Pathology of Lung Diseases: I. Restrictive Lung Diseas ESDocument65 pagesThe Pathology of Lung Diseases: I. Restrictive Lung Diseas ESLiana Ika SuwandyNo ratings yet
- Amy and Kisham: Worksheets AnswersDocument8 pagesAmy and Kisham: Worksheets AnswersAnas Ahmed MamdouhNo ratings yet
- XII - Biology - Module - 5 - Environmental Issues - SolutionsDocument17 pagesXII - Biology - Module - 5 - Environmental Issues - SolutionsShreyashNo ratings yet
- COVID-19: Hemoglobin, Iron, and Hypoxia Beyond Inflammation. A Narrative ReviewDocument7 pagesCOVID-19: Hemoglobin, Iron, and Hypoxia Beyond Inflammation. A Narrative ReviewAlejandroNo ratings yet
- Module 4Document34 pagesModule 4xtnreyesNo ratings yet
- Jurnal ARDSDocument17 pagesJurnal ARDSwahyuNo ratings yet
- Pulmonary EmbolismDocument12 pagesPulmonary EmbolismJohn Paul MatienzoNo ratings yet
- Cardiovascular Pathology - 020) Aortic Valve Stenosis and Regurgitation (Notes)Document13 pagesCardiovascular Pathology - 020) Aortic Valve Stenosis and Regurgitation (Notes)arga setyo adjiNo ratings yet
- 1082 Medical Surgical Nursing Eye & Ent & Integumentary System DDocument16 pages1082 Medical Surgical Nursing Eye & Ent & Integumentary System DdhavalsagthiaaNo ratings yet
- CCR Landoni120 June v6-2Document3 pagesCCR Landoni120 June v6-2Rara AuliaNo ratings yet
- Pangpangdeo Shanne Delle B. - Worksheet 5 ArdsDocument7 pagesPangpangdeo Shanne Delle B. - Worksheet 5 ArdsPANGPANGDEO Shanne Delle B.No ratings yet
- 07-Pollution of Air & WaterDocument3 pages07-Pollution of Air & WatervarshavishuNo ratings yet
- Assignmnet 2 Ques - ESC 202Document4 pagesAssignmnet 2 Ques - ESC 202Nidhi MalikNo ratings yet
- 粉尘与尘肺Document59 pages粉尘与尘肺api-3735745No ratings yet
- 246 - Respiratory Pathology Pneumonia - Treatment and PreventionDocument4 pages246 - Respiratory Pathology Pneumonia - Treatment and PreventionPranav PunjabiNo ratings yet
- 243 - Respiratory Pathology COPD - Treatment and PreventionDocument3 pages243 - Respiratory Pathology COPD - Treatment and PreventionPranav PunjabiNo ratings yet
- Renal Pathology Acute Kidney Injury AKIDocument14 pagesRenal Pathology Acute Kidney Injury AKIPranav PunjabiNo ratings yet
- 242 - Respiratory Pathology COPD - Clinical FeaturesDocument3 pages242 - Respiratory Pathology COPD - Clinical FeaturesPranav PunjabiNo ratings yet
- Barth BulimiaDocument13 pagesBarth BulimiaFernando Mišel PessoaNo ratings yet
- Langley-Evans-2015-Journal of Human Nutrition and Dietetics PDFDocument14 pagesLangley-Evans-2015-Journal of Human Nutrition and Dietetics PDFPriscila Lemasson DuranteNo ratings yet
- Role Play PDFDocument18 pagesRole Play PDFTin TinNo ratings yet
- Cdmp2015 HandbookDocument90 pagesCdmp2015 HandbookTony NgNo ratings yet
- Insignis PCM3 Dengue, Blood Donation, HIV, Mental Health, NBS, LeprosyDocument133 pagesInsignis PCM3 Dengue, Blood Donation, HIV, Mental Health, NBS, LeprosyNibshian Dela RosaNo ratings yet
- Contraindications To Air TravelDocument15 pagesContraindications To Air TravelsDamnNo ratings yet
- Hypertension JDHHDDDocument5 pagesHypertension JDHHDDabcxyz15021999No ratings yet
- Drug Study Lab, NCP - Bronchial AsthmaDocument6 pagesDrug Study Lab, NCP - Bronchial AsthmaRichelle Sandriel C. de CastroNo ratings yet
- Denagard Amoxicillin MICs For Respiratory PathogensDocument2 pagesDenagard Amoxicillin MICs For Respiratory Pathogensnick224No ratings yet
- Nurture and ConnectionDocument4 pagesNurture and Connectionparents021100% (1)
- Mobic 15 MG Tablets - Summary of Product Characteristics (SPC)Document11 pagesMobic 15 MG Tablets - Summary of Product Characteristics (SPC)zxvcazcf0% (1)
- Diagnostic Value of Non Invasive Liver Function Tests in Liver Fibrosis and Changes in These Parameters Post Metabolic SurgeryDocument7 pagesDiagnostic Value of Non Invasive Liver Function Tests in Liver Fibrosis and Changes in These Parameters Post Metabolic SurgeryTan BulNo ratings yet
- Bells PalsyDocument66 pagesBells PalsyanshikaNo ratings yet
- Early Onset SchizophreniaDocument3 pagesEarly Onset SchizophreniaDoc Prince CaballeroNo ratings yet
- Nursing Care PlanDocument1 pageNursing Care Planapi-248135371No ratings yet
- Parathyroid Glands: Serum PTH Levels Are Inappropriately Elevated For The LevelDocument4 pagesParathyroid Glands: Serum PTH Levels Are Inappropriately Elevated For The LevelNada MuchNo ratings yet
- Forgein Bodies PPDDocument22 pagesForgein Bodies PPDVishuNo ratings yet
- Case Study 5 Year Boy With CoughDocument3 pagesCase Study 5 Year Boy With CoughAryl Eduarte100% (1)
- Title: HypoglycemiaDocument13 pagesTitle: Hypoglycemia025 MUHAMAD HAZIQ BIN AHMAD AZMANNo ratings yet
- Recurrent Pregnancy LossDocument18 pagesRecurrent Pregnancy LossNap91No ratings yet
- Mr. Jones Case StudyDocument4 pagesMr. Jones Case StudyDiane JaravataNo ratings yet
- A Critique PaperDocument1 pageA Critique PaperAyessa Nedine SalazarNo ratings yet
- 1-Normality and Mental HealthDocument7 pages1-Normality and Mental HealthRoland GealonNo ratings yet
- Getweightloss in Intragastric BalloonDocument2 pagesGetweightloss in Intragastric Balloongetweightloss2023No ratings yet
- AR para ManosDocument22 pagesAR para ManosAndres CasteloNo ratings yet
- Diarrhea: On This PageDocument6 pagesDiarrhea: On This PageKristine AlejandroNo ratings yet
- Cards RQs For INDEBDocument38 pagesCards RQs For INDEBJanderson LeiteNo ratings yet
- Algorithm For Anemia in Children Based On MCV - UpToDateDocument2 pagesAlgorithm For Anemia in Children Based On MCV - UpToDatefabsscribdworksNo ratings yet