Professional Documents
Culture Documents
Arie Utariani, Bambang Pudjo Semedi, Yoppie Prim Avidar, Nanang Nurofik
Uploaded by
Zanuba AlyzahulOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Arie Utariani, Bambang Pudjo Semedi, Yoppie Prim Avidar, Nanang Nurofik
Uploaded by
Zanuba AlyzahulCopyright:
Available Formats
Crit Care Shock (2020) 23:35-42
Correlation between middle cerebral artery pulsatility index and optic
nerve sheath diameter with intracranial pressure in traumatic and
non-traumatic brain injury patients of Dr. Soetomo General Hospital
Surabaya
Hamzah, Arie Utariani, Bambang Pudjo Semedi, Yoppie Prim Avidar, Nanang Nurofik
Abstract and optic nerve sheath diameter were investi-
Background: Patients with brain injury experi- gated.
ence pathology of increased intracranial pres- Results: Thirty patients with various intracra-
sure (ICP), which is the cause of secondary nial pathology, who underwent intraventricular
brain injury, brain herniation at the risk of catheter placement, were included in the study.
brain damage. Intracranial pressure control A total of 86 intracranial pressure examina-
and monitoring is one of the most important tions, middle cerebral artery pulsatility index,
strategies in managing patients in the neurosur- and optic nerve sheath diameter were conduct-
gery and neurointensive care fields. Intracranial ed. A significant correlation was found between
pressure monitoring in Dr. Soetomo General pulsatility index and intracranial pressure with
Hospital Surabaya is still limited by intra- a correlation coefficient of 0.639; intracranial
ventricular catheter installation, which is inva- pressure = 9.23 x PI + 4 mmHg. Pulsatility in-
sive. The middle cerebral artery pulsatility in- dex sensitivity was 93.2% with specificity
dex (PI) and sonographic optic nerve sheath 75.0%. Cut-off point was >1.11 for pulsatility
diameter enable non-invasive monitoring of in- index to detect increased intracranial pressure.
tracranial pressure. This study aimed to find The optic nerve sheath diameter and intracra-
out the correlation between middle cerebral ar- nial pressure correlation coefficient is 0.746;
tery pulsatility index and optic nerve sheath di- intracranial pressure = 7.88 x optic nerve
ameter with intracranial pressure. sheath diameter - 26.84 mmHg with sensitivity
Methods: Transcranial doppler measurement 92.3% and specificity 95.83%. Optic nerve
was made transtemporally to measure middle sheath diameter cut-off value was 5.4 mm.
cerebral artery pulsatility index. Optic nerve Conclusion: There was a correlation between
sheath diameter was measured 3 mm behind the middle cerebral artery pulsatility index and op-
globe using 12 MHz US probe. Intracranial tic nerve sheath diameter with intracranial
pressure was measured using intraventricular pressure. Pulsatility index and optic nerve
catheter. The correlation and regression be- sheath diameter can be used as alternative for
tween intracranial pressure, pulsatility index, ICP monitoring.
.
Key words: Pulsatility index, middle cerebral artery, optic nerve sheath diameter, intracranial pressure.
From Departement of Anaesthesiology and Reanimation, Fac- Introduction
ulty of Medicine - Dr. Soetomo General Hospital, Universitas Intracranial pathologies such as traumatic brain
Airlangga, Surabaya (Hamzah, Arie Utariani, Bambang Pudjo
Semedi, Yoppie Prim Avidar, Nanang Nurofik).
injury (TBI), stroke, meningitis, and brain tumor
are a cause of high mortality. The incidence of
Address for correspondence: stroke in United States of America (USA) is men-
Hamzah, MD., PhD tioned every 40 seconds and death occurs every 4
Departement of Anaesthesiology and Reanimation, Faculty of minutes. (1) Estimated, around 1.5 million people
Medicine - Dr. Soetomo General Hospital, Universitas Air- suffer from TBI every year in USA. More than
langga, Surabaya
Jalan Mayjend Prof. Dr. Moestopo No. 6-8, Airlangga, Gu-
50,000 people die every year as a result of TBI,
beng, Surabaya, Jawa Timur 60285 and other 80,000 have disability. (2) Whilst in In-
Tel : +6231-5501503; 5501504 donesia, the incidence is still not known certainly.
MP: +62811343135 (3) Data from resuscitation room in Emergency
.
Crit Care Shock 2020 Vol. 23 No. 1 35
Department Dr. Soetomo General Hospital Sura- resulting in increasing PI. (14) Furthermore, in-
baya stated that during period of July until Decem- creased ICP can cause diameter changes of optic
ber 2018 as many as 6.49% from total 2035 patients nerve sheath, which can be visualized using ultra-
who entered resuscitation room were TBI patients sound. Optic nerve is a part of the central nervous
with a mortality rate of 16.7%. system and coated with duramater. Subarachnoid
Patient with brain trauma has an increased intracra- space including cerebrospinal fluid (CSF) separate
nial pressure (ICP), which is the cause of secondary white matter and duramater for about 0.1-0.2 mm.
brain injury, brain herniation, and a risk of brain Some studies have shown an association between
damage and related to bad outcome. (4) ICP moni- diameter of optic nerve sheath with measurement of
toring and controlling are essential component of ICP invasively. (15)
neurocritical care patient management. ICP moni- As to the author knows, until now monitoring and
toring is increasingly included in protocols for man- examination of ICP in Dr. Soetomo General Hospi-
agement of subarachnoid haemorrhage (SAH) and tal Surabaya still limited by performed intraventric-
intracranial haemorrhage (ICH) critical care. (5) In- ular catheter requiring operating procedure in oper-
creased ICP can cause impaired blood circulation, ating theatre. TCD and sonography of optic nerve
decreased perfusion pressure, venous reflux ob- sheath diameter (ONSD) still not used in Emer-
struction, intracranial delayed blood flow, brain gency Department of Dr. Soetomo General Hospital
damage, brain shifting, and brain herniation. (6) ICP in management of brain injury patient, thus it is not
monitoring in traumatic brain injury patients were possible to examine ICP for emergency patient. (2)
reported to decrease mortality and resulted in over- There are no studies that assess correlation between
all better outcome. (7) ICP monitoring can also re- PI and ONSD with ICP in brain injury patients in
duce the rate of electrolyte imbalance and renal fail- Intensive Observation Room. For that, the author in-
ure. (8) tend to make this research.
The standard ICP monitoring technique uses ven-
tricular catheter, however, due to its invasive tech- Methods
nique, which requires surgical procedure in an op- This research is observational analytic with cross-
erating theater, the monitoring is not commonly sectional design. The study population were patients
done. In addition, placing intraventricular catheter age 17 to 65-year-old diagnosed with brain injury
poses multiple potentially fatal complications in- with ICP monitoring in Intensive Observation
cluding infection and bleeding. The procedure is Room Dr. Soetomo General Hospital Surabaya.
also contraindicated in patients with hematological Sampling technique using consecutive sampling.
abnormalities and trombocytopenia. (9) It is, there- Furthermore, inclusion criteria were patient age 17
fore, crucial to find an alternative to the invasive to 65-year-old diagnosed with brain injury with ICP
technique, preferably using a non-invasive tech- monitoring in Intensive Observation Room Dr. Soe-
nique. tomo General Hospital Surabaya and willing to sign
The non-invasive technique to monitor ICP is tran- the consent form to take part in the research, whilst
scranial Doppler (TCD). TCD is one of the non-in- the exclusion criteria were post cardiac arrest pa-
vasive tool used to assess flow velocity (FV) that tient, eye injury, post decompressive craniectomy
represents cerebral blood flow (CBF) value. TCD patient, and patient with cranial base fracture asso-
can be referred to as a stethoscope and become one ciated with CSF leakage. The amount of sample us-
of the main non-invasive CBF examination meth- Zα+Zβ 2
ods. (10) TCD allows to a real-time examination, ing formula n=[ 1+r- ] + 3, which n=minimum
0.5ln 1-r
portable, and inexpensive compared to other meth- sample value, α=0.05, so Zα=1.96; β=20%, so
ods. (11) TCD can be used to evaluate and monitor Zβ=0.84; r=correlation coefficient of previous re-
changes in cerebral blood vessel circulation, sub- search 0.52927, then from the formula obtained a
arachnoid haemorrhage (SAH) diagnostic test, vas- sample of 26, fulfilled to 30. The variable of this
ospasm monitoring and increased ICP detection, study was independent variable, ICP, and dependent
evaluating cerebral hemodynamic on brain injury, variables were PI and ONSD. The instruments of
and to determine brain death. (12) this study were ultrasonography (GE Vivid Q) and
Pulsatility index (PI) is a difference between sys- intraventricular catheter (Phycon ventricular drain-
tolic and diastolic flow velocity divided by the mean age tube [Fuji System Corporation]) with M size
flow velocity of middle cerebral artery (MCA), also (2.0-3.3 mm) and length 40 cm. This research was
known related to the result of invasive ICP meas- conducted in Intensive Observation Room Emer-
urements. (13) Increased ICP causes resistance to gency Department Dr. Soetomo General Hospital
CBF and decreasing flow velocity diastolic (FVd), Surabaya in April-May 2019. The data collection
. .
36 Crit Care Shock 2020 Vol. 23 No. 1
procedure of PI using TCD, examined by one per- Simple linear regression analysis showed that math-
son who had attended a TCD examination training ematically ICP value was 9.23 times of PI plus 4.
using ultrasound with a low-frequency probe. Receiver operating characteristic (ROC) curve be-
ONSD measurement using linear probe with 7-10 tween PI and ICP showed that PI sensitivity on de-
MHz by one person who had attended an ONSD ex- tecting increased ICP (ICP>15 mmHg) was 92.3%
amination training. ICP measured by looking at the (95% CI 79.1-98.4, p<0.0001, and specificity
undulation of CSF in an ICP monitor catheter with 75.0% (95% CI 60.4-86.4, p<0.0001). Area under
zero point as high as the acousticus externus meatus. the curve (AUC) 0.884 (95% CI 0.798-0.943,
Data was collected through a specific data collec- p<0.0001) (Figure 2). Youden’s index maximum
tion sheet. The results were presented in table, dia- value for ROC curve between PI and ICP was 0.673
gram/chart, text/writing that explained the chart/di- on PI criteria >1.11 with sensitivity level 92.3% and
agram, then the collected data was processed using specificity level 75.0%.
computer software with Pearson correlation test.
This research has had a permission from Research Correlation between optic nerve sheath diameter
Ethics Committee Dr. Soetomo General Hospital with intracranial pressure
Surabaya. The confidentiality of research data sub- The Kolmogorov-Smirnov statistic test to ONSD
ject was maintained by only including the respond- variable and ICP variable showed that both data nor-
ent’s initial. This data was only used for scientific mally distributed with p value =0.25 for ONSD and
purposes. 0.07 for ICP, so correlation test between ONSD and
ICP was done using the Pearson correlation test.
Results Pearson correlation test showed that a positive rela-
This study was an observational analytic done to the tion between ONSD and ICP with coefficient corre-
patient with intracranial abnormalities that under- lation R 0.746 and p value 0.0001 (Figure 3). Sim-
went intraventricular catheter insertion. Thirty pa- ple linear regression analysis showed that mathe-
tients with various intracranial abnormalities matically ICP value was 7.88 times of ONSD minus
(trauma, stroke, and infection) underwent intra- 26.84.
ventricular catheter placement were included in this ROC curve between ONSD and ICP showed that
study. The subject characteristic in this study was ONSD sensitivity in detecting increased ICP
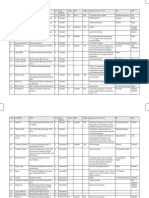
listed on the Table 1. (ICP>15 mmHg) was 92.3% (95% CI 79.1-98.4,
There were thirty patients with intracranial abnor- p<0.0001), and specificity 95.83% (95% CI 85.7-
malities in this study. They were divided into 3 99.5, p<0.0001). AUC 0.982 (95% CI 0.927-0.999,
groups intracranial abnormalities including trauma p<0.0001) (Figure 4). Youden’s index maximum
36.7%, stroke 50%, and infection 13.3%. Intracra- value for ROC curve between ONSD and ICP was
nial pathology due to trauma dominated by male, 0.897 on ONSD criteria >5.4 mm with sensitivity
which was 81.8% with an average age 37.73±15.96 89.74% and specificity 100%.
year.
Table 2 shows that each sample run three examina- Discussion
tions, so that the total examination was 87 times be- Increasing ICP can cause impaired blood circula-
cause one sample was only examined once and one tion, decreasing perfusion pressure, venous reflux
outlier was discarded. Mean TCD profile in normal obstruction, delayed intracranial blood flow, brain
and increased ICP showed a significant difference damage, brain shifting, and cerebral herniation. In
in the two groups, except on peak systolic velocity the sector of neurointensive care, ICP is one of the
(PSV). Result on ONSD also showed a statistically crucial parameter for management and treatment the
significant differences between two groups. patient. ICP monitoring using invasive method with
external ventricular drainage (EVD) is the gold
Correlation between middle cerebral artery pulsa- standard for ICP examination. The catheter place-
tility index and intracranial pressure ment is associated with the risk of infection and
The Kolmogorov-Smirnov statistic test to PI varia- bleeding. Hematology abnormality, for example
ble and ICP indicated that both data were normally prolong hemostasis function and thrombocytopenia,
distributed with p value =0.08 for PI and 0.07 for is also contraindicated in installation of ICP moni-
ICP, so correlation test between PI and ICP was per- toring. (9)
formed using the Pearson correlation test. Pearson Development in medical technology have made it
correlation test showed a positive relation between possible to detect an increased ICP by using non-
PI and ICP with the value of the correlation coeffi- invasive instrument, which possibly to do in limited
cient R 0.639 and p value 0.0001 (Figure 1). health facility that do not have neurosurgeons to do
.
Crit Care Shock 2020 Vol. 23 No. 1 37
ICP monitoring invasively. TCD is one of non-in- been proven as initial manifestation of increased
vasive instrument used to assess FV referred to CBF ICP. (11) In this study ONSD on patient with nor-
values. In this study, the author found that there was mal ICP were in range between 4.35-5.35 mm, with
linear correlation between PI and MCA with ICP. mean 5.0 mm. Patient with increased ICP, mean
Statistical test using Pearson’s correlation showed ONSD was 5.8 mm with range 5.2-6.5 mm. This is
that the correlation coefficient between PI and MCA similar with research by Lee et al (2016) showed
with ICP was 0.639. This result showed there was a that patient with increased ICP mean ONSD was 5.9
potent positive correlation between PI and MCA (5.8-6.2), while patient with normal ICP mean
with ICP. Simple linear regression analysis showed ONSD was 4.9 (4.6-5.2). (5,20) Pearson coefficient
that mathematically ICP can be written as 9.23PI + correlation show R=0.746 between ONSD and ICP
4 mmHg. This equal with a result of a former study mentioned that potent correlation. This was bigger
showing that there was a significant correlation be- if compared with PI.
tween PI and ICP (p<0.0001) with a correlation co- Simple linear regression analysis showed that ICP =
efficient of 0.938. (13) Gura et al (2011) mentioned 7.88 x ONSD - 26.84. Geeraerts et al (2008) men-
that correlation coefficient between PI and ICP var- tioned that there was a potent correlation (r=0.74)
ied with potent correlation, mentioned that correla- between ONSD changes and ICP variety. (21,22)
tion coefficient PI and ICP were 0.567, 0.529, and ROC curve between ONSD and ICP showing
0.779 on the first day, third day, and fifth day post ONSD sensitivity in detection of increased ICP
operative. (14,16) Some studies showed that PI and (ICP>15 mmHg) was 92.3% (95% CI 79.1-98.4,
ICP had potent correlation and had some linear cor- p<0.0001), and specificity 95.83% (95% CI 85.7-
relation between PI and ICP. (17) 99.5, p<0.0001). AUC was 0.982 (95% CI 0.927-
Some study reported that decreased blood flow in- 0.999, p<0.0001). Based on Youden’s index, ONSD
dicating increased ICP and intracranial hyperten- value >5.4 mm can be used as cut-off point on de-
sion related to increased PI. (18) This corresponded tecting increased PI.
to result of this study showing that PSV and EDV
values on patient with increased ICP were signifi- Conclusion
cantly lower than patient with normal ICP. ROC MCA-PI has positive correlation with ICP
curve between PI and ICP showed that PI sensitivity (R=0.639) and simple linear regression analysis
for detection of increased ICP (ICP>15 mmHg) was shows that ICP = 9.23PI + 4 mmHg. Whilst ONSD
92.3% (95% CI 79.1-98.4, p<0.0001, and specific- has positive correlation with ICP (R=0.746) and
ity 75% (95% CI 60.4-86.4, p<0.0001) for PI value simple linear regression analysis shows that ICP =
>1.11. Based on Youden’s index, this PI value 7.88 x ONSD - 26.84 mmHg. This study can be a
>1.11 could be used as cut-off point on detecting in- reference to future research with more homogenous
creased ICP. and bigger sample. This can be a clinical application
Optic nerve is a part of the central nervous system for the use of PI and ONSD to detect and evaluate
and coated with duramater. Increased PI will be ICP on patient in emergency room who has not per-
transmitted to subarachnoid space, mainly formed the placement of invasive ICP monitoring,
retrobulbar segment, and causing changes of optic and a study to determine ONSD and PI normal value
nerve sheath diameter that can be visualized with ul- to Indonesian people.
trasound. (19) Dilated myelin optic nerve sheath has
.
38 Crit Care Shock 2020 Vol. 23 No. 1
Table 1. Subject characteristic
Subject characteristic n/mean
Age (year) 46.4±17.11
Sex
- Male 16 (53.3)
- Female 14 (46.7)
Comorbidity factor
- Diabetes mellitus 3 (10)
- Hypertension 12 (40)
- Anemia 3 (10)
- Obesity 1 (3.3)
Type of intracranial pathology
- Brain injury 11 (36.7)
- Stroke 15 (50.0)
- Infection 4 (13.3)
Early GCS 7.47±1.76
Transcranial Doppler
- PSV (cm/s) 78.05±27.61
- EDV (cm/s) 27.36±12.97
- FVm (cm/s) 44.63±18.85
- PI 1.25±0.38
ONSD (mm) 5.37±0.52
ICP (mmHg) 15.49±5.45
- Normal (<15 mmHg) 48 (55.17)
- Increased (>15 mmHg) 39 (44.83)
MAP (mmHg) 94.53±9.51
CPP (mmHg) 79.04±11.27
PaCO2 (mmHg) 36.67±5.29
Hematocrit (%) 34.26±6.39
Legend: GCS=Glasgow coma scale; PSV=peak systolic velocity; EDV=end diastolic velocity; FVm=mean
flow velocity; PI=pulsatility index; ONSD=optic nerve sheath diameter; ICP=intracranial pressure;
MAP=mean arterial pressure; CPP=cerebral perfusion pressure; PaCO2=arterial partial pressure of carbon
dioxide
Table 2. TCD and ONSD profile based on ICP category
Profile ICP p
<15 mmHg >15 mmHg
TCD
- PSV (cm/s) 78.95±27.14 76.94±28.5 0.738
- EDV (cm/s) 31.68±11.88 22.04±12.37 0.0001
- FVm (cm/s) 49.13±18.74 39.10±17.68 0.013
- PI 1.03±0.23 1.52±0.35 0.0001
ONSD (mm) 5.00±0.27 5.84±0.34 0.0001
Legend: TCD=transcranial Doppler; PSV=peak systolic velocity; EDV=end diastolic velocity; FVm=mean
flow velocity; PI=pulsatility index; ONSD=optic nerve sheath diameter; ICP=intracranial pressure
Crit Care Shock 2020 Vol. 23 No. 1 39
Figure 1. Simple regression between MCA-PI (X) and ICP (Y)
ICP
PI
Legend: MCA=middle cerebral artery; PI=pulsatility index; ICP=intracranial pressure
Figure 2. ROC curve PI to ICP
Legend: ROC=receiver operating characteristic; PI=pulsatility index; ICP=intracranial pressure
40 Crit Care Shock 2020 Vol. 23 No. 1
Figure 3. Simple regression between ONSD (X) and ICP (Y)
ICP
ONSD
Legend: ONSD=optic nerve sheath diameter; ICP=intracranial pressure
Figure 4. ROC curve of ONSD and ICP
Legend: ROC=receiver operating characteristic; ONSD=optic nerve sheath diameter; ICP=intracranial
pressure
Crit Care Shock 2020 Vol. 23 No. 1 41
References
1. Bhatia A, Gupta AK. Neuromonitoring in the lege of Surgeons Trauma Quality Improvement
intensive care unit: Intracranial pressure and Program. J Neurotrauma 2013; 30:1737-46.
cerebral blood flow monitoring. Intensive Care 13. Brain Trauma Foundation, American Associa-
Med 2007;33:1263-71. tion of Neurological Surgeons, Congress of
2. Apriawan T, Sufarnap E. Cedera Otak. Seri 1: Neurological Surgeons, Joint Section on Neu-
Perdarahan Intrakranial dan Manajemen Pem- rotrauma and Critical Care, AANS/CNS, Brat-
bedahan. Surabaya: Airlangga University ton SL, et al. Guidelines for the management
Press; 2018. P. 1-15. of severe traumatic brain injury. VI. Indica-
3. Smith M. Monitoring intracranial pressure in tions for intracranial pressure monitoring. J
traumatic brain injury. Anesth Analg 2008; Neurotrauma 2007;24:S37-44.
106:240-8. 14. Kattah JC, Pula JH, Mejico LJ, McDermott
4. Corral L, Javierre CF, Ventura JL, Marcos P, MP, Kupersmith MJ, Wall M. CSF pressure,
Herrero JI, Manez R. Impact of non- papilledema grade, and response to acetazola-
neurological Complications in Severe Trau- mide in the Idiopathic Intracranial Hyperten-
matic Brain Injury Outcome. Crit Care 2012; sion Treatment Trial. J Neurol 2015;262:2271-
16:R44. 4.
5. Lee SU, Jeon JP, Lee H, Han JH, Seo M, 15. Sarkar S, Ghosh S, Ghosh SK, Collier A. Role
Byoun HS, et al. Optic Nerve Sheath Diameter of transcranial Doppler ultrasonography in
threshold by Ocular Ultrasonography for De- stroke. Postgrad Med J 2007;83:683-9.
tection of Increased Intracranial Pressure in 16. Gura M, Elmaci I, Sari R, Coskun N. Correla-
Korean Adults Patients with Brain Lesions. tion of Pulsatility Index with Intracranial Pres-
Medicine (Baltimore) 2016;95:e5061. sure in Traumatic Brain Injury. Turk Neuro-
6. Laksono BH. Transcranial Doppler Ultraso- surg 2011;21:210-5.
nography: Diagnosis dan Monitoring Non In- 17. Carney N, Totten AM, O’Reilly C, Ullman JS,
vasif pada Neuroanesthesia dan neurointensive Hawryluk GWJ, Bell MJ, et al. Guidelines for
Care. JNI 2017;6:124-31. the Management of Severe Traumatic Brain
7. Gao Y, Li Q, Wu C, Liu S, Zhang M. Diagnos- Injury, 4th edition. Neurosurgery 2016;0:1-10.
tic and Prognostic value of the Optic Nerve 18. Kirkman MA, Smith M. Supratentorial intra-
Sheath Diameter with respect to the intracrani- cerebral hemorrhage: A review of the underly-
al pressure and neurological outcome of pa- ing pathophysiology and its relevance for mul-
tients following hemicraniectomy. BMC Neu- timodality neuromonitoring in neurointensive
rol 2018;18:199. care. J Neurosurg Anesthesiol 2013;25:228-39.
8. Kelts EA. Traumatic brain injury and visual 19. Kimberley HH, Shah S, Marill K, Noble V.
dysfunction: a limited overview. NeuroReha- Correlation of optic nerve sheath diameter with
bilitation 2010;27:223-9. direct measurement of intracranial pressure.
9. Sandsmark DK, Kumar MA, Park S, Levine Acad Emer Med 2008;15:201-4.
JM. Multimodal monitoring in subarachnoid 20. Moretti R, Pizzi B, Cassini F, Vivaldi N. Reli-
hemorrhage. Stroke 2012;43:1440-5. ability of optic nerve ultrasound for the evalua-
10. Cremer OL. Does ICP monitoring make a dif- tion of patients with spontaneous intracranial
ference in neurocritical care? Eur J Anaesthe- hemorrhage. Neurocrit Care 2009;11:406-10.
siol Suppl 2008;42:87-93. 21. Geeraerts T, Merceron S, Benhamou D, Vigué
11. Kirkman MA, Smith M. Multi-modality Neu- B, Duranteau J. Noninvasive assessment of in-
rologic Monitoring. In: Cottrell JE, Patel P, ed- tracranial pressure using ocular sonography in
itors. Cottrell and Patel’s Neuroanesthesia. 6th neurocritical care patients. Intensive Care Med
ed. Edinburgh, Scotland: Elsevier; 2017. P. 2008;34:2062-7.
142-51. 22. Hansen HC, Helmke K. The subarachnoid
12. Alali AS, Fowler RA, Mainprize TG, Scales space surrounding the optic nerves. An ultra-
DC, Kiss A, de Mestral C, et al. Intracranial sound study of the optic nerve sheath. Surg
Pressure Monitoring in Severe Traumatic Radiol Anat 1996;18:323-8.
Brain Injury: Results from the American Col-
.
42 Crit Care Shock 2020 Vol. 23 No. 1
You might also like
- Gold Standards in Medical FieldDocument8 pagesGold Standards in Medical FieldJyothisankar Radhakrishnan100% (2)
- Jing Zhou, Jing Li, Tiantian Ye and Yanrong ZengDocument20 pagesJing Zhou, Jing Li, Tiantian Ye and Yanrong ZengNeelma MisraNo ratings yet
- ONSD measurement for monitoring ICPDocument11 pagesONSD measurement for monitoring ICPRony palwagunaNo ratings yet
- Research Article: Retinal Structural and Microvascular Alterations in Different Acute Ischemic Stroke SubtypesDocument10 pagesResearch Article: Retinal Structural and Microvascular Alterations in Different Acute Ischemic Stroke SubtypesKarina NathaniaNo ratings yet
- Transcranial Doppler Sonography Pulsatility Index (PI) Reflects Intracranial Pressure (ICP)Document7 pagesTranscranial Doppler Sonography Pulsatility Index (PI) Reflects Intracranial Pressure (ICP)Lulu LuwiiNo ratings yet
- Farhat Research ArticleDocument1 pageFarhat Research ArticleDr MS HarisNo ratings yet
- Measurement of optic nerve sheath diameter and optic nerve sheath diameter to eyeball transverse diameter (onsd/etd) ratio via ultrasonography in neurocritical patients and their correlation with intracranial pressure and functionaloutcome – a prospective observational studyDocument5 pagesMeasurement of optic nerve sheath diameter and optic nerve sheath diameter to eyeball transverse diameter (onsd/etd) ratio via ultrasonography in neurocritical patients and their correlation with intracranial pressure and functionaloutcome – a prospective observational studyBIOMEDSCIDIRECT PUBLICATIONSNo ratings yet
- GJHS 8 152Document6 pagesGJHS 8 152Ika PuspitaNo ratings yet
- Huang 2014Document16 pagesHuang 2014Kulsoom FatemaNo ratings yet
- Pocusj 08 16563Document5 pagesPocusj 08 16563andres ruizNo ratings yet
- Siriraj Stroke ScoreDocument3 pagesSiriraj Stroke ScoreHendy SetiawanNo ratings yet
- Brain Ultrasonography: Methodology, Basic and Advanced Principles and Clinical Applications. A Narrative ReviewDocument15 pagesBrain Ultrasonography: Methodology, Basic and Advanced Principles and Clinical Applications. A Narrative ReviewPablo Ezequiel SarmientoNo ratings yet
- 1 s2.0 S0929664617300487 MainDocument8 pages1 s2.0 S0929664617300487 MainSuryati HusinNo ratings yet
- DSADocument7 pagesDSANantini GopalNo ratings yet
- Gambaran Hasil Pemeriksaan CT Scan Kepala Pada PenDocument6 pagesGambaran Hasil Pemeriksaan CT Scan Kepala Pada PenhendridunantikoNo ratings yet
- Abstrak IsicamDocument22 pagesAbstrak IsicambgusjklNo ratings yet
- Pengaruh Mobilisasi Dini Terhadap Perubahan Tekanan Intra Kranial Pada Klien Post Trepanasi Di Instalasi Rawat Intensif RSD Dr. Soebandi JemberDocument9 pagesPengaruh Mobilisasi Dini Terhadap Perubahan Tekanan Intra Kranial Pada Klien Post Trepanasi Di Instalasi Rawat Intensif RSD Dr. Soebandi JemberRatriNo ratings yet
- Update On Multimodality MonitoDocument8 pagesUpdate On Multimodality MonitoConstanza Andrea Saldivia Blanco(RedSalud Magallanes)No ratings yet
- Result: There Were 94 Patients Enrolled: Chun-Min Wang Department of Neurology, National Cheng Kung University HospitalDocument23 pagesResult: There Were 94 Patients Enrolled: Chun-Min Wang Department of Neurology, National Cheng Kung University Hospital台灣中風醫誌100% (1)
- Relationship Between Increased Intracranial Pressure and Mastoid EffusionDocument9 pagesRelationship Between Increased Intracranial Pressure and Mastoid EffusionFebrian Parlangga MuisNo ratings yet
- JofIMAB 2019 25 2p2471 2475Document5 pagesJofIMAB 2019 25 2p2471 2475afriskha bulawanNo ratings yet
- Direct Accuracy Performance Comparison of Cerebral Oximeter Devices - AANA Journal CoursesDocument8 pagesDirect Accuracy Performance Comparison of Cerebral Oximeter Devices - AANA Journal CoursesRaluca LNo ratings yet
- Main 10Document11 pagesMain 10pokharelriwaj82No ratings yet
- Head Position in Acute Stroke Trial Statistical Analysis PlanDocument5 pagesHead Position in Acute Stroke Trial Statistical Analysis PlanNurul AzmiyahNo ratings yet
- Near Infrared Spectroscopy As A Predictor For Shunt Requirement During Carotid EndarterectomyDocument9 pagesNear Infrared Spectroscopy As A Predictor For Shunt Requirement During Carotid EndarterectomyAmira DayoubNo ratings yet
- UOCTDocument8 pagesUOCTUlquiorra SchifferNo ratings yet
- Brain SPECT in Neurology and PsychiatryDocument13 pagesBrain SPECT in Neurology and PsychiatryCarol ArtigasNo ratings yet
- USG Nervo Optico e TC CrânioDocument5 pagesUSG Nervo Optico e TC CrânioVictor CiriloNo ratings yet
- NERVIO OPTICO HIPERTENSIOM CRANEAL 2021Document5 pagesNERVIO OPTICO HIPERTENSIOM CRANEAL 2021Andrea GutierrezNo ratings yet
- MonitoreoicpnoinvasivoDocument7 pagesMonitoreoicpnoinvasivoCristianMP96No ratings yet
- 1726-Article Text-23983-2-10-20220330Document6 pages1726-Article Text-23983-2-10-20220330CL X-RAY IMAGESNo ratings yet
- Comparison of Neurological Clinical Manifestation in Patients With Hemorrhagic and Ischemic StrokeDocument5 pagesComparison of Neurological Clinical Manifestation in Patients With Hemorrhagic and Ischemic StrokeDessy FarwasNo ratings yet
- 8.V2 (4) 310 319Document10 pages8.V2 (4) 310 319台灣中風醫誌No ratings yet
- 24Document2 pages24Audhrey BNo ratings yet
- TADocument7 pagesTAAngela Villanueva SocolaNo ratings yet
- Chen 2021Document7 pagesChen 2021Felipe GonzálezNo ratings yet
- Jurnal 20Document7 pagesJurnal 20Zella ZakyaNo ratings yet
- Magnetic Resonance Imaging: Jun Chen, Bin Zhao, Chunqing Bu, Guohua XieDocument7 pagesMagnetic Resonance Imaging: Jun Chen, Bin Zhao, Chunqing Bu, Guohua XieMabel MerinNo ratings yet
- Newer Trends in StrokeDocument26 pagesNewer Trends in StrokejoemamrocksusNo ratings yet
- Diagnosis of Idiopathic Normal Pressure Hydrocephalus Is Supported by MRI-based Scheme: A Prospective Cohort StudyDocument11 pagesDiagnosis of Idiopathic Normal Pressure Hydrocephalus Is Supported by MRI-based Scheme: A Prospective Cohort StudyDini NanamiNo ratings yet
- NeuroDocument6 pagesNeuroAkhdan AufaNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument11 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Review Article Imaging Assessment of Acute Ischaemic Stroke: A Review of Radiological MethodsDocument26 pagesReview Article Imaging Assessment of Acute Ischaemic Stroke: A Review of Radiological MethodsImanuel CristiantoNo ratings yet
- Content ServerDocument8 pagesContent ServerG. Araya MoraNo ratings yet
- Koziarz 2019Document11 pagesKoziarz 2019Thiago DiasNo ratings yet
- 2018 Book CerebralIschemicReperfusionInjDocument269 pages2018 Book CerebralIschemicReperfusionInjVictor M TorresNo ratings yet
- Ich - Inducido Por DrogasDocument14 pagesIch - Inducido Por DrogasMarceloAndresCastañedaDuarteNo ratings yet
- CME Article January 2017 PDFDocument7 pagesCME Article January 2017 PDFsheila dewantyNo ratings yet
- Continuous Determination of Optimal Cerebral Perfusion Pressure in Traumatic Brain InjuryDocument8 pagesContinuous Determination of Optimal Cerebral Perfusion Pressure in Traumatic Brain InjurydrdivyapukNo ratings yet
- TMP E094Document7 pagesTMP E094FrontiersNo ratings yet
- Puerta Balon y Mortalidad Circunfleja AngioplastiaDocument7 pagesPuerta Balon y Mortalidad Circunfleja Angioplastiamichael.medpaNo ratings yet
- Tomasello ContourDocument11 pagesTomasello ContourangelNo ratings yet
- Can Transient BP High Risk Cerebral InfarctsDocument9 pagesCan Transient BP High Risk Cerebral InfarctsshofidhiaaaNo ratings yet
- Jurnal 16Document3 pagesJurnal 16Zella ZakyaNo ratings yet
- Dessens, F.M Et Al. 2020Document8 pagesDessens, F.M Et Al. 2020widyadariNo ratings yet
- Journal ReadingDocument53 pagesJournal ReadingRhadezahara PatrisaNo ratings yet
- Carotid UltrasoundDocument9 pagesCarotid UltrasoundLora LefterovaNo ratings yet
- Ultrasound Non-Invasive Measurement of Intracranial Pressure in Neurointensive Care: A Prospective Observational StudyDocument16 pagesUltrasound Non-Invasive Measurement of Intracranial Pressure in Neurointensive Care: A Prospective Observational StudyRonald GoyesNo ratings yet
- Tayal 2007Document7 pagesTayal 2007Candra YogiswaraNo ratings yet
- Ischemic Core and Hypoperfusion Volumes Predict Infarct Size in Swift PrimeDocument14 pagesIschemic Core and Hypoperfusion Volumes Predict Infarct Size in Swift PrimePutri YingNo ratings yet
- Anesthesiology GuideDocument4 pagesAnesthesiology GuideGeorge Wang100% (1)
- p214 PDFDocument3 pagesp214 PDFNinaNo ratings yet
- Methadone Hydro ChlorideDocument4 pagesMethadone Hydro Chlorideapi-3797941100% (1)
- MCQ On Bleeding in Early Pregnancy: DR Manal Behery Zagazig University 2013Document36 pagesMCQ On Bleeding in Early Pregnancy: DR Manal Behery Zagazig University 2013joseph0% (1)
- DacryocystorhinostomyDocument3 pagesDacryocystorhinostomyNarla SusheelNo ratings yet
- Acoustic Voice Quality IndexDocument3 pagesAcoustic Voice Quality IndexjessicadanleyuarkNo ratings yet
- MICROPARA LEC Chapter 14 ReviewerDocument11 pagesMICROPARA LEC Chapter 14 ReviewerRen “Shel” ManaloNo ratings yet
- Hydrogen Iodide Chemical Properties Uses EffectsDocument3 pagesHydrogen Iodide Chemical Properties Uses EffectsJohn KellyNo ratings yet
- Surat Dental 181Document15 pagesSurat Dental 181deva nesanNo ratings yet
- Bloodborne Pathogens PPT v-03!01!17Document44 pagesBloodborne Pathogens PPT v-03!01!17kunalphalswal0005No ratings yet
- Physical Fitness & Longevity TestsDocument17 pagesPhysical Fitness & Longevity TestsmrludiNo ratings yet
- Toxicological and Pharmacokinetic Properties of Sucralose 6 Acetate and Its Parent Sucralose in Vitro Screening AssaysDocument36 pagesToxicological and Pharmacokinetic Properties of Sucralose 6 Acetate and Its Parent Sucralose in Vitro Screening AssayswipiriNo ratings yet
- Increased Intracranial Pressure NCLEX ReviewDocument8 pagesIncreased Intracranial Pressure NCLEX ReviewAnia JuanNo ratings yet
- Comprehensive Cleft CareDocument9 pagesComprehensive Cleft CareEvgeniya KocherginaNo ratings yet
- Ipcr Accomplishment June To Dec 2020Document3 pagesIpcr Accomplishment June To Dec 2020edwardraymond holl0% (1)
- COMPARING URINARY RETENTIONDocument7 pagesCOMPARING URINARY RETENTIONKomang DeaNo ratings yet
- Provision of Heel Cast For Treatment of Heel Ulcers December 2016 NWCEG GuidelineDocument39 pagesProvision of Heel Cast For Treatment of Heel Ulcers December 2016 NWCEG GuidelineneilNo ratings yet
- 2010 Catalog USDocument47 pages2010 Catalog USengequinNo ratings yet
- Kimia Farma Per 30 September ZRMM076Document271 pagesKimia Farma Per 30 September ZRMM076SriyatiNo ratings yet
- Nursing Impact On Maternal and Infant Mortality in The United States.Document7 pagesNursing Impact On Maternal and Infant Mortality in The United States.boniface mogisoNo ratings yet
- NCP - Ineffective Breathing PatternDocument4 pagesNCP - Ineffective Breathing PatternPRINCESS KOBAYASHINo ratings yet
- Turkey Position PaperDocument3 pagesTurkey Position PaperBill GatesNo ratings yet
- Defibrillator: DR Sumanth ReddyDocument39 pagesDefibrillator: DR Sumanth Reddyrohith100% (1)
- Assessing Community Health ProblemsDocument5 pagesAssessing Community Health ProblemsMARC JOSHUA SARANILLONo ratings yet
- Radiotherapy and Oncology: Karen Wong, Geoff P. Delaney, Michael B. BartonDocument5 pagesRadiotherapy and Oncology: Karen Wong, Geoff P. Delaney, Michael B. BartonFrançois IdjiwoleNo ratings yet
- AMEBIASISDocument19 pagesAMEBIASISDika Herza Pratama100% (1)
- Paramedian Forehead Flap Nasal Reconstruction Surgical TechniqueDocument10 pagesParamedian Forehead Flap Nasal Reconstruction Surgical Techniquetegegnegenet2No ratings yet
- Complete Small Med Surgery 2Document65 pagesComplete Small Med Surgery 2MelanieNo ratings yet
- Untitled 5 PDFDocument6 pagesUntitled 5 PDFDeepak saxenaNo ratings yet