Professional Documents
Culture Documents
Severity of Depression in Mothers of Children Suffering From Cerebral Palsy
Uploaded by
Dr Alamzeb JadoonOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Severity of Depression in Mothers of Children Suffering From Cerebral Palsy
Uploaded by
Dr Alamzeb JadoonCopyright:
Available Formats
DOI: https://doi.org/10.
53350/pjmhs2216818
ORIGINAL ARTICLE
Severity of Depression in Mothers of children suffering from Cerebral
Palsy
AYESHA GOHEIR1, ALAMZEB JADOON2, SYEDA SHAZMINA FAYYAZ3, NAZMA KIRAN4, NAVEED AKHTAR5, ZIA QAMAR6
1
Assistant Professor of Physiology, Rai Medical College, Sargodha, Pakistan
2
Assistant Professor of Physiology, Nowshera Medical College, Nowshera (K.P), Pakistan
3
House Officer, PAF Hospital, Sargodha, Pakistan
4
Associate Professor of Pathology, Rai Medical College, Sargodha, Pakistan
5
Professor of Anatomy, Rai Medical College, Sargodha, Pakistan.
6
Senior Registrar, Pulmonology Department, Ayub Teaching Hospital, Abbottabad.
Correspondence to Dr. Alamzeb Jadoon, Email: alamzebkhanjadoon@yahoo.com, Phone: 03008550585
ABSTRACT
Background: Cerebral palsy (CP) is the most common cause of motor disability in children with worldwide having incidence of 2
per 1000 live births. Children with CP have motor disability, decreased ability to walk, poor feeding and limited exposure to
sunlight. Malnutrition, behavior challenges and motor deficits in CP children are common causes of depression in their mothers.
Aim: The present study focused to estimate the severity of depression in mothers, looking after the children suffering from
severe CP and to compare their depression scoring with the scores of mothers having healthy children.
Methods: The cross-sectional comparative study included 21 mothers having children suffering from severe CP and 21 controls
(Mothers of normal children). Depression was calculated by the Beck Depression Inventory (BDI).
Results: A statistically significant difference was observed between the mean scores of BDI II between the two groups
Conclusion: Results revealed that mothers having CP children are more depressed than mothers having healthy children. It
imitates the importance of psychiatric, social and family support to mother along with the treatment of the child.
Keywords: CP, depression, BDI II.
INTRODUCTION The present study intended to explore the effects of CP on
maternal depression and to compare their scores with the healthy
Cerebral palsy (CP) is brain paralysis caused by the brain hypoxia controls. The results obtained highlighted the need of psychiatric
which affects body movements, balance and posture with support to improve the quality of life of child, parents, and family.
incidence of 2 per 1000 live births1 .Increased risk is associated The study also enlightened the need of proper antenatal checkups
with preterm delivery, congenital malformations, intrauterine and the deliveries to be conducted in a tertiary care hospital. The
infections, fetal growth retardation, multiple pregnancies, placental results obtained highlight the need for psychiatric support to the
abnormalities, prolonged labor and instrumental delivery. However, mothers along with the treatment of the child.
1-2% cases of CP are due to genetic abnormalities2. The disorders
of movement appear in early stages of life along with delayed
MATERIALS AND METHODS
milestones, diminished intellect and motor disability3.
Early diagnosis and intervention help to improve infant motor This was a Cross-sectional comparative study. The study was
and cognitive functions and protect from secondary complications4. approved by Ethical review board of the University of Health
In severe cases, CP can be detected soon after birth, but average Sciences Lahore and the Institutional review board (IRB) of
age of diagnosis is two years. For those with milder symptoms, a Children hospital / Institute of Child Health Lahore.
diagnosis may not be confirmed until the brain is fully developed at The study was conducted in Lahore, the provincial capital of
three to five years of age. The average age of diagnosis for a child Punjab, Pakistan. Subjects were recruited from the Children
with CP is 18 months5. Type of manifestation and extent of hospital, Lahore. A total of 42 mothers of middle class family, with
disability depends upon area of brain involved. The motor function age up to 40 years were included in this study. They were further
deficits limit the daily doings of life and may accompany cognitive, subdivided into two groups, 21 subjects having children suffering
speech, behavior, sensory impairments and behavioral difficulties from CP and 21 mothers having normal children were included
which can affect family functioning and over all wellbeing of child after written and informed consent. Gross Motor Functional
and family member6,7. Greater parental stress has been found to Classification System (GMFCS) level V was taken as severe CP in
be related with higher levels of behavioral problems in children8,9. children and diagnosed by doctor of the developmental pediatrics
A study carried out by using Self Report Questionnaires in department19,20. All pregnant or lactating mothers, using steroid
Bangladesh showed that the mothers of CP children are therapy, oral contraceptive pills or medication for depression,
susceptible to develop stress10. BDI-II used in our study is also a Widows and females with difficult relations with family and spouse
self-report 21 item questionnaire having 81% sensitivity and 92% and any other chronic medical condition were excluded based
specificity21,23. It is translated into multiple languages worldwide. In upon history and investigations. Sample size was calculated by
the current study Urdu version of the inventory was WHO calculator version 2.021, derived on basis of a previous
administered24,25.Mothers having a CP child are more prone to study15. The purposive sampling technique was used.
depression than the mothers having apparently healthy children11 . Well known self-report questionnaire with acceptable
Depression have negative impact on one’s feelings, views and psychometric properties were utilized after consultation with the
actions12,13. It is the frequently occurring psychopathology14. consultant psychiatrist. Depressive symptoms were assessed
Mothers with CP child are more predisposed to to depression. using BDI-II- U21,22. Data regarding the demographic profile of
Depression and anxiety was testified in 71% mothers with CP subjects, past medical or drug history and family history, was
children, compared to 33% in the control group11. Studies showed collected on carefully designed datasheets. History about antenatal
that mothers having CP children were high risk group for visits, duration of pregnancy, mode of delivery, the delayed cry of
depression and need psychiatric help15,16,17,18. the newborn, infections in neonate and family history of CP was
This study was conducted to calculate depression in mothers also taken to rule out the cause of CP. Questionnaire regarding
taking care of children. data and depression scoring was filled by the subjects or
------------------------------------------------------------------------------------ researcher under supervision of the psychologist.
Received on 11-03-2022 All the data was entered into Microsoft Excel data sheet and
Accepted on 29-07-2022 analyzed using the SPSS 25. Mean±S.D or median±interquartile
18 P J M H S Vol. 16, No. 08, August 2022
A. Goheir, A. Jadoon, S. S. Fayyaz et al
range was given for the quantitative variables. Frequencies and and positive correlation with GMFCS scores in the CP child.
percentages were given for qualitative variables. Graphs were Presence of CP child in a family is associated with maternal
presented for variables. Shapiro-Wilk test was applied to check the depression, musculoskeletal pain and negatively impacts the
normality of data. Mann-Whitney test was applied to compare BDI quality of life30,31. Increased psychological strain can be the
scores between the two groups. A p-value of ≤ 0.05 is taken as triggering factor for the development of depression among mothers
statistically significant. of CP children. Detailed history suggests that possible factors
causing stress in mothers included in our study could be because
RESULTS of disable child, behavioral problems or any other ailment
associated with the child, limited leisure time, improper sleep, lack
This study included 42 females divided equally into two groups. No of family support, the social or economic burden.
significant difference existed between the ages of mothers of both This study highlighted the need of psychological and social
groups (p= 0.103) help for the mother taking care of CP children and emphasized on
All the participants included in the study belonged to the the need for the provision of proper medical facilities to the mother
middle class. All had satisfactory relationship with their husband during pregnancy, during delivery and after birth.
and other people in the family. Among cases, only 2 children
reported CP in their first-degree relatives. Out of total 21 cases, CONCLUSION
13(61.9%) cases of CP reported prolonged labor and 8(38%)
children were delivered at home by a midwife (dai). Mothers taking care of CP children are more depressed as
Both groups were compared for the parameters included in compared to the mothers taking care of healthy children. Females
the study. The BDI scores for mothers taking care of children should have proper antenatal and post-natal visits to doctor for
suffering from CP were higher than in mothers taking care of evaluation and care of mother and newborn. Education of family
healthy children that was found significant (Mann Whitney U test, and society about the need for psychological help and need of
p=0.011) (Table 1). social and family support to the mother having CP child, is highly
All the mothers of CP children (group I) reported depression of recommended.
some severity, 17(80.95%) had minimal depression, 3(14.28%) Conflict of interest: Nil
had mild depression and 1(4.76%) had moderate depression.
Out of 21 mothers with normal children (control group), 19 REFERENCES
(90.4%) participants had minimal depression, 1(4.76%) had mild
depression and 1(4.76%) had moderate depression. 1. Odding E, Roebroeck ME, Stam HJ. The epidemiology of cerebral
palsy: incidence, impairments and risk factors. Disabil. Rehabil. 2006;
28(4):183-191.
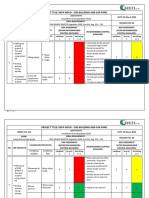
Table 1: Comparison of study parameters measured in cases and control
2. MacLennan AH, Thompson SC, Gecz, J. Cerebral palsy: causes,
groups by Mann Whitney U test
pathways, and the role of genetic variants. Am. J. Obstet. Gynecol.
Parameters Mothers with children Mothers having
2005; 213(6): 779-788.
suffering from CP(n=21) apparently healthy
3. Miller F, Bachrach SJ. Cerebral palsy: A complete guide for caregiving.
children(n=21)
2017; 3rd edition., Baltimore: JHU Press.
Mean±SD Mean±SD
4. Novak I, Morgan C, Adde L, Blackman J, Boyd RN, Brunstrom-
Median (IQR) Median (IQR) Hernandez J, Cioni G, Damiano D, Darrah J, Eliasson AC, De Vries
BDI score 7.57±5.33 4.62±5.12 LS. Early, accurate diagnosis and early intervention in cerebral palsy:
5 (4-12.5), 17 4 (1.5-5) advances in diagnosis and treatment. JAMA pediatr. 2017; 171(9):
P value 0.011 a* 897-907.
5. Byrne R, Noritz G, Maitre NL, Group NED. Implementation of early
DISCUSSION diagnosis and intervention guidelines for cerebral palsy in a high-risk
infant follow-up clinic. Pediatr. Neurol. 2017; 76: 66-71.
This study included 21 mothers with healthy children (control 6. Cadman D, Boyle M, Szatmari P, Offord DR. Chronic illness, disability,
group) and 21 mothers having children suffering from severe CP. and mental and social well-being: findings of the Ontario Child Health
The results revealed that the BDI scores were significantly higher Study. Pediatrics. 2017: 79(5): 805-813.
in mothers taking care of CP children as compared to the mothers 7. Majnemer A, Shevell M, Rosenbaum P, Law M, Poulin C.
Determinants of life quality in shcool-age children with cerebral palsy.
having apparently healthy children. A study reported similar results
J. Pediatr. 2007; 151(5): 470-475.
to our study, the higher BDI II scores and low quality of life was 8. Johnston C, Hessl D, Blasey C, Eliez S, Erba H, Dyer-Friedman J,
observed in mothers having CP children26. Previous studies Glaser B, Reiss AL. Factors associated with parenting stress in
reported significantly higher levels of BDI scores in mothers having mothers of children with fragile X syndrome. J. Dev. Behav. Pediatr.
CP children than the control group27,28. Mothers having CP children 2003; 24(4): 267-275.
are depressed and severity can be categorized as mild, moderate 9. Webster RI, Majnemer A, Platt RW, Shevell MI. Child health and
and severe29. parental stress in school-age children with a preschool diagnosis of
developmental delay. J Child Neurol. 2008; 23(1): 32-38.
Results of our study are consistent with the above-
10. Mobarak R, Khan NZ, Munir S, Zaman SS, McConachie H. Predictors
mentioned studies. Studies suggest that CP children's mothers of stress in mothers of children with cerebral palsy in Bangladesh. J
had a high prevalence of depression that had a negative impact on Pediatr. Psychol. 2000; 25(6): 427-433.
children quality of life16,17. 11. De Sousa A, Singhvi S. Depressive Symptoms In Mothers Of Children
Studies conducted earlier suggest that factors like increase With Cerebral Palsy. J Pak Psychiatr Soc. 2011; 8(1): 12-17.
in age of mother as well as child, poor spousal support, lack of 12. American Psychiatric Association . Diagnostic and statistical manual of
support from the family, unemployment and low education seemed mental disorders. 2013; Arlington: American Psychiatric Publishing.
13. Lipinski J, Crothers LM. eds. Bullying in the workplace: Causes,
to aggravate depression in these mothers. However, having
symptoms, and remedies. 2013; New York: Routledge.
another child with normal health and development, good family 14. Schraedley PK. Intergenerational transmission of psychopathology:
support and living in joint families served as protective factors. Psychosocial difficulties among daughters of depressed mothers.
Presence of associated problems like epilepsy in the child, low 2003; Sandford: Stanford University.
intelligence, the severity of paralysis, motor disabilities, feeding 15. Altindag Ö, Işcan A, Akcan S, Koksal S, Erçin , Ege L. Anxiety and
issues and behavioral problems along with poor toilet training Depression Levels in Mothers of Children with Cerebral Palsy. Turk J
worsened the depression scores in mothers looking after the Ph Med Rehab/Turkiye Fiziksel Tip ve Rehabilitasyon Dergisi. 2007;
53(1): 22-24.
children suffering from CP17. Similarly, higher BDI scores were
16. TÜRKOĞLU S, Bilgic A, TÜRKOĞLU G, YILMAZ S. Impact of
observed by Altindag and his fellows15. symptoms of maternal anxiety and depression on quality of life of
Physical disability in the child negatively affects the life of the children with cerebral palsy. Nöro Psikiyatri Arş. 2016; 53(1): 49-54.
mother. Literature showed that maternal depression levels have a 17. Soliman RH, Altwairqi RG, Alshamrani NA, Al-Zahrani AA, Al-Towairqi
negative correlation with functional independence measurement RM, Al-Habashi AH. Relationship between quality of life of children
P J M H S Vol. 16, No. 08, August 2022 19
Depression in Mothers
with cerebral palsy and their mothers' depression and anxiety. Saudi J 25. Fatima B, Khaliq SA, Gul A, Mubeen SM. Depression Among Islamic
Health Sci. 2019; 8(1): 1-5. Seminaries Students: A Cross Sectional Survey. RADS J Pharm
18. Gull M. Level of depression among mothers of differently abled Pharm Sci. 2018; 6(4): 236-240.
children in Kashmir. ZENITH Int J Multidiscip Res.2019; 9(3): 29-36. 26. Sajedi F, Alizad V, Malekkhosravi G, Karimlou M, Vameghi R.
19. Palisano RJ. GMFCS-E & R Gross Motor Function Classification Depression in mothers of children with cerebral palsy and its relation to
System: Expanded and Revised. Canchild centre for childhood severity and type of cerebral palsy. Acta Med Iran. 2010;48(4):250-
disability research;2007. 254.
20. Stucky KJ, Kirkwood MW, Donders J. editors. Clinical 27. Begum, Desai O. A Comparative Study To Evaluate Psychological
Neuropsychology study guide and board review. Oxford University Status Of Mothers Of Children With Cerebral Palsy And Mothers Of
Press; 2014. Normal Children. IJOT. 2010; 42(2): 3-9.
21. Beck A, Steer R, Brown G. Beck Depression Inventory-II (BDI-II) for 28. Ones K, Yilmaz E, Cetinkaya B, Caglar N. Assessment of the quality of
Beck Depression Inventory-II ;1993. Available onine at: http://www. life of mothers of children with cerebral palsy (primary caregivers).
jvrcatalogue. com/wp-content/uploads/2010/09/Beck-Depression- Neurorehab Neural Repair. 2005;19(3): 232-237.
Inventory. 29. Diwan S, Chovatiya H, Diwan J. Depression and quality of life in
22. Fatima B, Khaliq SA, Gul A, Mubeen SM. Depression Among Islamic mothers of children with cerebral palsy. NJIRM. 2011; 2(4):11-13.
Seminaries Students: A Cross Sectional Survey. RADS JPPS 2018; 30. Kaya K, Unsal-Delialioglu S, Ordu-Gokkaya NK, Ozisler Z, Ergun N,
6(4):236-240. Ozel S, Ucan H. Musculo-skeletal pain, quality of life and depression in
23. Dozois DJ, Covin R. The Beck depression inventory-II (BDI-II), Beck mothers of children with cerebral palsy. Disabil. Rehabil. 2010;
hopelessness scale (BHS), and Beck scale for suicide ideation (BSS). 32(20):1666-1672.
Comprehensive handbook of psychological assessment. 2004; 2: 31. Unsal-Delialioglu S, Kaya K, Ozel S, Gorgulu G. Depression in
pp.50-69. mothers of children with cerebral palsy and related factors in Turkey: a
24. Fahim M. Frequency of Depression in Mothers of Learning-Disabled controlled study. Int J Rehabil Res. 2009 ;32(3): 199-204.
Children. J Islamabad Med Dent College. 2017; 6(2): 113-116.
20 P J M H S Vol. 16, No. 08, August 2022
You might also like
- Agesta Sacred Codes ListDocument22 pagesAgesta Sacred Codes Listmimigogo92% (12)
- Hirarc LiftingDocument1 pageHirarc LiftingAmir Syahir75% (4)
- Time in Psychoanalysis: Some Contradictory AspectsDocument185 pagesTime in Psychoanalysis: Some Contradictory AspectsDrustvo Mrtvih Slikara100% (1)
- Blood Physiology Gutyon 14th Edition Chapter 35 ImmunityDocument27 pagesBlood Physiology Gutyon 14th Edition Chapter 35 ImmunityDr Alamzeb JadoonNo ratings yet
- CDM Smith Study - Eastern Pender Water System ImprovementsDocument138 pagesCDM Smith Study - Eastern Pender Water System ImprovementsMark DarroughNo ratings yet
- YANG SHENG 2011 October B PDFDocument70 pagesYANG SHENG 2011 October B PDFSasa PuiuNo ratings yet
- MantelDocument13 pagesManteljacopo pruccoliNo ratings yet
- Research PaperDocument4 pagesResearch PaperMridula DasNo ratings yet
- 10 1016@j Jaac 2018 06 010 PDFDocument2 pages10 1016@j Jaac 2018 06 010 PDFRaúl AñariNo ratings yet
- Epilepsy and BehaviorDocument8 pagesEpilepsy and Behaviorviviana84No ratings yet
- ACEsADHDmanuscriptAcademicPediatrics2017May JuneDocument6 pagesACEsADHDmanuscriptAcademicPediatrics2017May JuneDanya KatsNo ratings yet
- Developmental Correlates Persistent Snoring in Preschool Children: Predictors and Behavioral andDocument10 pagesDevelopmental Correlates Persistent Snoring in Preschool Children: Predictors and Behavioral andsambalikadzilla6052No ratings yet
- Aindev 2012 12 004Document10 pagesAindev 2012 12 004Gisele Elise MeninNo ratings yet
- E541 FullDocument9 pagesE541 FullAlba VilaNo ratings yet
- Parental Stress in Patients With Schizophrenia Spectrum DisorderDocument11 pagesParental Stress in Patients With Schizophrenia Spectrum DisorderNur IlyaniNo ratings yet
- Guerro-Prado Et Al, 2015. Evolution of Stress in Families of Children With PHDADocument8 pagesGuerro-Prado Et Al, 2015. Evolution of Stress in Families of Children With PHDAHannahNo ratings yet
- Assessment of Mothers Care Toward Their Children Having PhenylketonuriaDocument14 pagesAssessment of Mothers Care Toward Their Children Having Phenylketonuriaأميرة خليلNo ratings yet
- Cognitive-Electrophysiological IndicesDocument9 pagesCognitive-Electrophysiological IndicesbhasiNo ratings yet
- Obsos 1 PDFDocument8 pagesObsos 1 PDFyosevangelika hutabaratNo ratings yet
- 5938 20021 3 PBDocument9 pages5938 20021 3 PBbiswaspritha.18No ratings yet
- PPD Porposal Draft AssignmentDocument4 pagesPPD Porposal Draft AssignmentRayan JaafeerNo ratings yet
- BR J Psychiatry - Artigo 1Document8 pagesBR J Psychiatry - Artigo 1Victoria AlmeidaNo ratings yet
- Faktor Resiko DPP 2020Document13 pagesFaktor Resiko DPP 2020sipen poltekkesbdgNo ratings yet
- Cognitive Behavioral TherapyDocument14 pagesCognitive Behavioral TherapyLunaFiaNo ratings yet
- Functional Consequences of Attention-De Ficit Hyperactivity Disorder On Children and Their FamiliesDocument15 pagesFunctional Consequences of Attention-De Ficit Hyperactivity Disorder On Children and Their FamiliesAlba VilaNo ratings yet
- MaternalPsychopathologyAndOffs SINDocument10 pagesMaternalPsychopathologyAndOffs SINEsmeraldaNo ratings yet
- Jurnal Dukungan SosialDocument4 pagesJurnal Dukungan SosialDevita HandayaniNo ratings yet
- Shuang 2021Document7 pagesShuang 2021Raul Morales VillegasNo ratings yet
- Neurodevelopmental Outcomes of Preterm Infants: A Recent Literature ReviewDocument6 pagesNeurodevelopmental Outcomes of Preterm Infants: A Recent Literature ReviewJyotirmayeeNo ratings yet
- Factors Affecting The Quality of Life in Childhood Epilepsy in ChinaDocument7 pagesFactors Affecting The Quality of Life in Childhood Epilepsy in ChinavicraadhityaNo ratings yet
- 1 s2.0 S0003999313002864 MainDocument8 pages1 s2.0 S0003999313002864 MainKiki PuchiNo ratings yet
- Are Siblings of Children With Autism More Prone ToDocument18 pagesAre Siblings of Children With Autism More Prone ToAdina CipariuNo ratings yet
- IndianJContNsgEdn17169-1808062 050120Document6 pagesIndianJContNsgEdn17169-1808062 050120rmconvidhya sri2015No ratings yet
- Association of Use of Different Type of Manual Therapy Approach With Upper Extremity Pain in Manual Therapists of LahoreDocument9 pagesAssociation of Use of Different Type of Manual Therapy Approach With Upper Extremity Pain in Manual Therapists of LahoreInternational Health ReviewNo ratings yet
- 2019 Article 1336Document6 pages2019 Article 1336Eduardo LimaNo ratings yet
- Protective Factors For Child Development at Age 2 in The Presence of Poor Maternal Mental Health: Results From The All Our Babies (AOB) Pregnancy CohortDocument8 pagesProtective Factors For Child Development at Age 2 in The Presence of Poor Maternal Mental Health: Results From The All Our Babies (AOB) Pregnancy CohortAndikNo ratings yet
- J CHC 2019 08 017Document20 pagesJ CHC 2019 08 017Luis MiguelNo ratings yet
- Anxiety and Depression Among Parents of Children With Intellectual Disability in PakistanDocument6 pagesAnxiety and Depression Among Parents of Children With Intellectual Disability in PakistanRiris KurnialatriNo ratings yet
- Effect of Preterm Infant Massage by The Mother On The Mood of Mothers Having Preterm InfantsDocument10 pagesEffect of Preterm Infant Massage by The Mother On The Mood of Mothers Having Preterm InfantsopanocayNo ratings yet
- Prevalence of Postpartum Depression Among Mothers Who DeliveredDocument7 pagesPrevalence of Postpartum Depression Among Mothers Who Deliveredroven desuNo ratings yet
- Sobrecarga CuidadoresDocument6 pagesSobrecarga CuidadoresMARIA FRANCISCA VERGARA AGUILARNo ratings yet
- Preoperativeanxiety Management, Emergence Delirium, Andpostoperative BehaviorDocument23 pagesPreoperativeanxiety Management, Emergence Delirium, Andpostoperative BehaviorVania CasaresNo ratings yet
- MIsmatch JCPP For Preprint 30.9.2017Document28 pagesMIsmatch JCPP For Preprint 30.9.2017BRIGITA CHRISTI PETRA KARINA FEBITASARI 1No ratings yet
- EBP Practice 2 - N - HiscockInfantSleep08 - 2016Document9 pagesEBP Practice 2 - N - HiscockInfantSleep08 - 2016Sitti Rosdiana YahyaNo ratings yet
- 2018 - Adhd e VLBWDocument18 pages2018 - Adhd e VLBWdeborahpreitiNo ratings yet
- Asociacioìn Entre SOP y TDAHDocument10 pagesAsociacioìn Entre SOP y TDAHalondraNo ratings yet
- SDocument10 pagesSDewi PrasetiaNo ratings yet
- Neurosci 09 02 015Document11 pagesNeurosci 09 02 015Divya JoshiNo ratings yet
- Post Partum DepressionDocument9 pagesPost Partum DepressionNaufal BinseffNo ratings yet
- Jacka. Maternal and Early Postnatal Nutrition and Mental Health of Offspring by Age 5 Years A Prospective Cohort Study Jacka 2013Document10 pagesJacka. Maternal and Early Postnatal Nutrition and Mental Health of Offspring by Age 5 Years A Prospective Cohort Study Jacka 2013sarbu_mirelaNo ratings yet
- Journal Adhi DR Rini Behavioral Problems in Children With Epilepsy (Autosaved)Document33 pagesJournal Adhi DR Rini Behavioral Problems in Children With Epilepsy (Autosaved)Utomo SiswoNo ratings yet
- E113 FullDocument8 pagesE113 FullMirza RisqaNo ratings yet
- Abstrak BipolarDocument1 pageAbstrak BipolarendahNo ratings yet
- Mental Health of Parents and Preschool-Aged Children During The COVID-19 Pandemic The Mediating Role of Harsh Parenting and Child Sleep DisturbancesDocument9 pagesMental Health of Parents and Preschool-Aged Children During The COVID-19 Pandemic The Mediating Role of Harsh Parenting and Child Sleep DisturbancesToth Fanni-BarbaraNo ratings yet
- Biomedical Journal: SciencedirectDocument8 pagesBiomedical Journal: SciencedirectCarlosToledoNo ratings yet
- Journal 11Document5 pagesJournal 11Francis GecobeNo ratings yet
- Mental Health Problems in A School Setting in Children and AdolescentsDocument9 pagesMental Health Problems in A School Setting in Children and AdolescentsRezky PutriNo ratings yet
- Hartbert Et Al., 2012Document6 pagesHartbert Et Al., 2012Isabel BelisaNo ratings yet
- Relationship Between The Baby Blues and PostpartumDocument5 pagesRelationship Between The Baby Blues and PostpartumTanu BhatiaNo ratings yet
- Group 7 Written ReportDocument4 pagesGroup 7 Written ReportMaryrose SanchezNo ratings yet
- Infant Mental Health Journal - 2020 - Salomonsson - Short Term Psychodynamic Infant Parent Interventions at Child HealthDocument15 pagesInfant Mental Health Journal - 2020 - Salomonsson - Short Term Psychodynamic Infant Parent Interventions at Child HealthArif Erdem KöroğluNo ratings yet
- Medical Comorbidities in Children and AdolescentsDocument12 pagesMedical Comorbidities in Children and AdolescentsSalud-psicología-psiquiatria DocenciaNo ratings yet
- Breastfeeding and Parafunctional Oral Habits in Children With and Without Attention-Deficit/Hyperactivity DisorderDocument7 pagesBreastfeeding and Parafunctional Oral Habits in Children With and Without Attention-Deficit/Hyperactivity DisorderCloudcynaraaNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument10 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- A Clinical Pathway To Standardize Care of Children With Delirium in Pediatric Inpatient Settings-2019Document10 pagesA Clinical Pathway To Standardize Care of Children With Delirium in Pediatric Inpatient Settings-2019Juan ParedesNo ratings yet
- BLOOD Physiology Guyton 14th Edition Chapter 33Document57 pagesBLOOD Physiology Guyton 14th Edition Chapter 33Dr Alamzeb Jadoon100% (1)
- Risk Assessment of Hepatitis B Patients of Northern Areas of Pakistan: A Case Control StudyDocument3 pagesRisk Assessment of Hepatitis B Patients of Northern Areas of Pakistan: A Case Control StudyDr Alamzeb JadoonNo ratings yet
- Attitude of StudentsDocument9 pagesAttitude of StudentsDr Alamzeb JadoonNo ratings yet
- Uric AcidDocument5 pagesUric AcidDr Alamzeb JadoonNo ratings yet
- Undesirable Body Mass Index Profiles in Young Adults: No One Is Immune To Obesity Epidemic in PakistanDocument5 pagesUndesirable Body Mass Index Profiles in Young Adults: No One Is Immune To Obesity Epidemic in PakistanDr Alamzeb JadoonNo ratings yet
- ResistinDocument3 pagesResistinDr Alamzeb JadoonNo ratings yet
- Blending Old and New Teaching MethodsDocument4 pagesBlending Old and New Teaching MethodsDr Alamzeb JadoonNo ratings yet
- Assign Chem in EverydayLife 16Document1 pageAssign Chem in EverydayLife 16Shubham AsthanaNo ratings yet
- JHA-H011 Scrubbing and Mopping FloorsDocument2 pagesJHA-H011 Scrubbing and Mopping Floorstjeng syuwenNo ratings yet
- Memorize BiologyDocument79 pagesMemorize BiologyprthrNo ratings yet
- Fneur 13 871187Document7 pagesFneur 13 871187Yery AparicioNo ratings yet
- A Rare Presentation of Tibial Eminence Avulsion Fracture in AdultDocument4 pagesA Rare Presentation of Tibial Eminence Avulsion Fracture in AdultIJAERS JOURNALNo ratings yet
- Diabetes Care.: Daftar PustakaDocument3 pagesDiabetes Care.: Daftar PustakaariNo ratings yet
- TM HDMF June 2019Document620 pagesTM HDMF June 2019Wendelle Mayo DomingcilNo ratings yet
- Adult Friends Diaper (Thought Process)Document2 pagesAdult Friends Diaper (Thought Process)Rohan HiremathNo ratings yet
- Non-Invasive Methods of Penile Lengthening: Fact or Fiction?Document5 pagesNon-Invasive Methods of Penile Lengthening: Fact or Fiction?BJ VeuxNo ratings yet
- Insanity Workout DVDDocument2 pagesInsanity Workout DVDshopzillahouse001No ratings yet
- Ficha Tecnica E803Document2 pagesFicha Tecnica E803Zenen AlarconNo ratings yet
- Hemodynamic Disorders: (Disorders of Blood Flow)Document25 pagesHemodynamic Disorders: (Disorders of Blood Flow)EZHIL N100% (1)
- Sleeping Pattern Among Students ReportDocument15 pagesSleeping Pattern Among Students ReportHazwani RahmanNo ratings yet
- X-Ray GeneratorDocument6 pagesX-Ray GeneratorDidimo Antonio Paez ClavijoNo ratings yet
- Biologic Agents To Optimize Outcomes Following ACL Repair and Reconstruction A Systematic Review of Clinical EvidenceDocument38 pagesBiologic Agents To Optimize Outcomes Following ACL Repair and Reconstruction A Systematic Review of Clinical EvidenceyasimNo ratings yet
- 013 HIRARC Installation of Hoisting BeamDocument8 pages013 HIRARC Installation of Hoisting Beambdiey100% (1)
- 2010 Integrated Updated Circulation ACLS Tachycardia AlgorithmDocument1 page2010 Integrated Updated Circulation ACLS Tachycardia AlgorithmRyggie ComelonNo ratings yet
- Medic Shoes - Clinic Report - 25/10/2020Document49 pagesMedic Shoes - Clinic Report - 25/10/2020יפה גולןNo ratings yet
- Kel 4 - BioethicsDocument22 pagesKel 4 - BioethicsLyana BerlyNo ratings yet
- RAGHU Final ProjectDocument50 pagesRAGHU Final ProjectPrakashNo ratings yet
- Loyola Public School, Loyola Nagar, Guntur - 522005 Promotion From Class VIII To IXDocument1 pageLoyola Public School, Loyola Nagar, Guntur - 522005 Promotion From Class VIII To IXDevi KalyanNo ratings yet
- SOP For Training of Employees - Pharmaceutical GuidelinesDocument14 pagesSOP For Training of Employees - Pharmaceutical GuidelinesAli50% (2)
- DR Axe 5 Essential Oils Proven Bymedical Science PDFDocument7 pagesDR Axe 5 Essential Oils Proven Bymedical Science PDFDubravka Duda100% (1)
- NUTRITIONAL MANAGEMENT OF OBESITY & TYPE 2 DIABETES EspenDocument34 pagesNUTRITIONAL MANAGEMENT OF OBESITY & TYPE 2 DIABETES EspenMarcelo Murillo0% (1)
- GE Discovery VCT BrochureDocument11 pagesGE Discovery VCT Brochurerabbani.moNo ratings yet