Professional Documents
Culture Documents
History
Uploaded by
Ahmed ExaminationOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
History
Uploaded by
Ahmed ExaminationCopyright:
Available Formats
History Taking
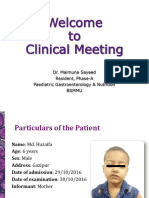
Patient Biodata:
1. Name(Triple):
2. Age: Years old
3. Sex(Gender): Male Famle Bisexual
4. Marital status: Single Married Widow Divorced
5. Religion: Muslim Christian Yazidian Sabian
6. Occupation(Job):
7. Residence(Address):
8. Date of admission: / /
9. Date of examination: / /
Chief Complaint and Its Duration:
(One or two no more!)
History of Present Illness(SOCRATES):
1. Site:
2. Onset: Sudden Gradual
3. Character(Nature): Aching Burning Stabbing Constricting Stitch
(Preferably using the patient’s own word description rather than offering suggestion)
4. Radiation:
5. Association phenomena:
6. Time (special time of pain occurrence or all the time):
7. Exacerbation and reliving factors:
8. Severity: Mild Moderate Severe
*In some cases like fever: don’t ask about site, character, radiation, exacerbation and reliving factors,
Instead: ask about treatment and response to it.
ابراهمي محمد سلطان:اعداد الطالب
Review of Other System:
Cardiovascular System(CVS):
Shortness of breath(Dyspnea):
1. Chest pain (usually center):
Shortness of breath when lying flat
2. Shortness of breath(Dyspnea):
(Orthopnea):
Sudden shortness of breath during
3. Awareness of heart beat(Palpitation):
sleep (PND Paroxysmal Nocturnal
4. Brief loss of consciousness (Syncope): Dyspnea):
5. Calf muscle pain(Claudication):
6. Peripheral swelling(Edema):
Respiratory System:
1. Chest pain (usually lateral):
2. Shortness of breath(Dyspnea):
3. Cough: Dry: Productive:
4. Sputum: Amount: Color:
5. Noisy breathing (Wheezing, Stridor):
6. Coughing of blood (Hemoptysis): Amount:
Gastrointestinal Track(GIT)
1. Appetite: loss (Anorexia): Good:
2. Weight: loss: Gain:
3. Swallowing: Good: Difficulty (Dysphagia or Odynophagia):
4. Abdominal pain:
5. Flatulence:
6. Indigestion (Dyspepsia):
7. Heartburn (burn sensation in the stomach or chest area):
8. Nausea:
9. Vomiting: Amount: Color:
10.Vomiting of blood (Hematemesis): Amount:
11.Bowel motion: Frequency: Amount: Color: Consistency:
12. Stool abnormality:
* From bowel motion we will know if it diarrhea or constipation.
Abnormal evacuation in general: 3 times per day(Diarrhea), less than 3 times per week(Constipation).
Genitourinary System (GUS):
1. Loin pain:
2. Difficulty of urination/pain passing urine (Dysuria):
3. Frequency and time, passing urine (at night Nocturia):
4. Quantity of urine: Normal: Polyuria: Oliguria: Anuria:
5. Color of urine (blood in urine (Hematuria)):
6. Sudden need to pass urine (Urgency):
7. Inability to prevent discharge of urine (urine Incontinence):
8. Dripping:
9. Ureteral discharge (Men): Amount: Color:
10. Vaginal discharge (Women): Amount: Color:
11. Vaginal bleeding: Amount:
12. Last menstrual period (consider pregnancy): Regular: Length:
Nervous System(CNS):
1. Headache:
2. Dizziness:
3. Sensation of unsteadiness (Vertigo):
4. Temporarily loss of consciousness (Faints):
5. Abnormal movement:
6. Altered feeling: Depression: Confusion: Anxious:
7. Weakness: Facial: Limb:
8. Abnormal sensation: Numbness: Tingling:
9. Visual disturbance:
10. Hearing problems (Deafness, Tinnitus):
11. Memory and concentration changes:
12.Sleep disorder:
Locomotor System:
1. Muscle: pain: Weakness: Contract:
2. Bone: pain:
3. Joint: pain: Swelling: v Stiffness:
Skin System: Rash: Ulcer: Sweating: Itch: Lumps:
Past Medical History:
1. Similar condition in the past:
2. History of endemic disease: T.B: Malaria:
3. History of common disease: DM.: HP: Rheumatic Fever:
Jaundice: Hypercholesterolemia: Angina: MI:
Asthma: Epilepsy: Stroke or TIA:
4. Previous admission to the hospital:
*If past disease present ask about:
When was it diagnosed?
How has it been treated?
Past Surgical History:
1. History of any operation or injury:
Operation: Date: / / Type: Any complication:
2. History of trauma: head: Chest: Abdomen:
Drug History:
Name: Dose: Duration: Mode of Use:
1.
2.
3.
Drug allergy (Especially Penicillin, Methoprime, Sulfa group):
Family History:
1. Similar condition in the family:
2. Family history of common disease:
3. Premature death of member of the family: Age: Cause:
Social History:
A) Personal History: Single: Married: No. of Children:
Occupation: Hobbies: Habit: Alcohol:
Smoke: Light: Heavy: {Less than 20 Cigarette Light Smoker, >20 heavy}
B) Social History:
Economic status: Good: Mild: Moderate:
House: Type: Size: Owned: Rented:
Animal in the house: Travel aboard:
You might also like
- Red Wolf Disease (Systemic Lupus Erythematosus), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandRed Wolf Disease (Systemic Lupus Erythematosus), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Positive Options for Antiphospholipid Syndrome (APS): Self-Help and TreatmentFrom EverandPositive Options for Antiphospholipid Syndrome (APS): Self-Help and TreatmentRating: 3.5 out of 5 stars3.5/5 (2)
- History Taking List Origin Copy 2Document7 pagesHistory Taking List Origin Copy 2Sudhakaŕ KolluNo ratings yet
- HX Taking Sheet - Rami AlkayalDocument14 pagesHX Taking Sheet - Rami Alkayalsajad abasewNo ratings yet
- FormatDocument3 pagesFormatwarnerNo ratings yet
- General HistoryDocument16 pagesGeneral HistoryjjNo ratings yet
- CR DR - Dedi Hidropneumothorax Ec TB ParuDocument38 pagesCR DR - Dedi Hidropneumothorax Ec TB ParuBunga Listia ParamitaNo ratings yet
- GITDocument4 pagesGITDarawan MirzaNo ratings yet
- GUTDocument4 pagesGUTDarawan MirzaNo ratings yet
- Hematology CasesDocument10 pagesHematology Casesuyes100% (1)
- History and Examinatoin of The Resp. SystemDocument37 pagesHistory and Examinatoin of The Resp. Systemmawada abdallaNo ratings yet
- History TakingDocument9 pagesHistory Takingmahmoud selimNo ratings yet
- Nursing Assessment New 1Document10 pagesNursing Assessment New 1smithapsNo ratings yet
- OSCE Medicine by DR BilanDocument77 pagesOSCE Medicine by DR BilanBukhaari MohamedNo ratings yet
- Obs&GYN 1Document5 pagesObs&GYN 1AbedelrahmanShekhAhmadNo ratings yet
- IM Guide OnlyDocument14 pagesIM Guide OnlyMicah Ley OlposNo ratings yet
- Proforma For Chronic CaseDocument9 pagesProforma For Chronic CaseClangames 4No ratings yet
- 2011 09 Medical HistoryDocument52 pages2011 09 Medical HistoryGurpreet CharaNo ratings yet
- Surgery: Dr. Ebtisam Lec: - 1-1-Oct-06Document4 pagesSurgery: Dr. Ebtisam Lec: - 1-1-Oct-06api-3829364No ratings yet
- I. Vital Information: W La Paz, Iloilo CityDocument7 pagesI. Vital Information: W La Paz, Iloilo CityelleNo ratings yet
- Sheet Abeer PDFDocument96 pagesSheet Abeer PDFFate ChanNo ratings yet
- Internal All PracticalDocument60 pagesInternal All PracticalearNo ratings yet
- History Taking in Medicine by DR Ibtisam Salah 2017Document58 pagesHistory Taking in Medicine by DR Ibtisam Salah 2017abdi adamNo ratings yet
- Clinical Social Case Study Proforma: Coronary Artery DiseaseDocument34 pagesClinical Social Case Study Proforma: Coronary Artery DiseaseRiya SweetsolitudeNo ratings yet
- Case Study FormatDocument15 pagesCase Study FormatLavie GangwarNo ratings yet
- History Taking HandbookDocument2 pagesHistory Taking Handbookyouservezeropurpose113No ratings yet
- 429 History Taking and Physical Examination Booklet 2nd Edition 2013Document152 pages429 History Taking and Physical Examination Booklet 2nd Edition 2013Aloah122346100% (2)
- History and Physical ExamDocument5 pagesHistory and Physical ExamAnastasia TjanNo ratings yet
- Decachords by A G ClarkeDocument83 pagesDecachords by A G Clarkesunnyjamiel100% (1)
- 5-History Taking and Neurological ExaminationDocument114 pages5-History Taking and Neurological ExaminationLolla SinwarNo ratings yet
- Care Plan FormatDocument14 pagesCare Plan FormatAndalNo ratings yet
- Case Report Session (CRS)Document9 pagesCase Report Session (CRS)revininNo ratings yet
- History Hassan Karar LongDocument125 pagesHistory Hassan Karar LongHamidHassanNo ratings yet
- اسنان باطنة Clinical FinalDocument40 pagesاسنان باطنة Clinical FinalShady AnwarNo ratings yet
- Sheet of CardiologyDocument5 pagesSheet of Cardiologyatef51664No ratings yet
- CVS System: Bader Al-Mukhtar - RCSI - SCDocument8 pagesCVS System: Bader Al-Mukhtar - RCSI - SCmuhammadridhwanNo ratings yet
- Electronic Health Record (EHR) of Click Health Services Care Receiver (CR)Document10 pagesElectronic Health Record (EHR) of Click Health Services Care Receiver (CR)Himel Baidya HimuNo ratings yet
- Electronic Health Record (EHR) of Click Health Services Care Receiver (CR)Document10 pagesElectronic Health Record (EHR) of Click Health Services Care Receiver (CR)Himel Baidya HimuNo ratings yet
- Clinical History: I. AnamnesiaDocument6 pagesClinical History: I. AnamnesiaJosé GuarnizoNo ratings yet
- Cardiac System AssessmentDocument14 pagesCardiac System AssessmentValarmathi100% (1)
- PPGMedical History FormDocument2 pagesPPGMedical History Formmb344617No ratings yet
- 1 كتب دكتور علام باطنه General & Cardio.whiteKnightLoveDocument111 pages1 كتب دكتور علام باطنه General & Cardio.whiteKnightLoveNour ShăbanNo ratings yet
- Case Study MM-2Document40 pagesCase Study MM-2Aya Sayed100% (1)
- New Chronic FormatDocument6 pagesNew Chronic FormatSamrath DhirNo ratings yet
- Preskas BedahDocument23 pagesPreskas BedahAlimuslimahNo ratings yet
- Easy Way To History Taking and Physical ExaminationDocument279 pagesEasy Way To History Taking and Physical ExaminationAbdirahiim Ahmed100% (6)
- Clinicalmeetingoriginal 161117192705Document50 pagesClinicalmeetingoriginal 1611171927057dbnf4stjyNo ratings yet
- History TakingDocument4 pagesHistory TakingChristopher WuNo ratings yet
- CVS Nac-Osce BlocksDocument35 pagesCVS Nac-Osce BlocksRoop SinghNo ratings yet
- Establish Initial Rapport: History TakingDocument7 pagesEstablish Initial Rapport: History TakingasdfsNo ratings yet
- History Taking: DR Anwar H. SiddiquiDocument26 pagesHistory Taking: DR Anwar H. SiddiquiAssad mustafNo ratings yet
- Nursing Process - AdultDocument7 pagesNursing Process - Adultjoannamae molagaNo ratings yet
- Diagnostico Chines (Inglês)Document40 pagesDiagnostico Chines (Inglês)Sónia Oliveira100% (1)
- OSCE EverythingDocument24 pagesOSCE EverythingkendymillNo ratings yet
- Advance Adult Care Nursing Case StudyDocument12 pagesAdvance Adult Care Nursing Case StudySima SaeedNo ratings yet
- History and Examinatoin of The Cardiovascular SystemDocument47 pagesHistory and Examinatoin of The Cardiovascular Systemmawada abdallaNo ratings yet
- Gynaecology Clerking NoteDocument10 pagesGynaecology Clerking NoteHarithx97No ratings yet
- OSCE Paeds Master Sheet Rachel AlbertDocument26 pagesOSCE Paeds Master Sheet Rachel AlbertVahni SamarooNo ratings yet
- Basic of Clinical Examination For OSCEDocument109 pagesBasic of Clinical Examination For OSCEkhairul amilin83% (6)
- Fibromyalgia: Living a Life of Blessing and HopeFrom EverandFibromyalgia: Living a Life of Blessing and HopeRating: 4.5 out of 5 stars4.5/5 (3)
- Survival Guide 08Document172 pagesSurvival Guide 08Kavirm35No ratings yet
- Directory Update July. 2012Document208 pagesDirectory Update July. 2012Raj KamalNo ratings yet
- Septic ShockDocument11 pagesSeptic ShockJonna Mae Agcaoili SalameroNo ratings yet
- Bleeding GumsDocument1 pageBleeding GumsalyssaNo ratings yet
- Case Study Tonsil It IsDocument16 pagesCase Study Tonsil It IsMuhammad FarhanNo ratings yet
- Care of Mother, Child, and Adolescent: Prepared by Donna Belle Sumugat RN ManDocument26 pagesCare of Mother, Child, and Adolescent: Prepared by Donna Belle Sumugat RN ManLaurence Docog100% (1)
- How To Remove Blackheads in Hindi: Jaane Asan TarekeDocument7 pagesHow To Remove Blackheads in Hindi: Jaane Asan TarekecshradhhaNo ratings yet
- Iloilo Doctors' Hospital, Inc. Department of Internal MedicineDocument10 pagesIloilo Doctors' Hospital, Inc. Department of Internal MedicineAllison Eunice ServandoNo ratings yet
- Graston TechniqueDocument8 pagesGraston TechniqueSvetlana PolyakovaNo ratings yet
- Ministry of Health and Family Welfare Pregnancy GuidelinesDocument173 pagesMinistry of Health and Family Welfare Pregnancy GuidelinesKhushi GuptaNo ratings yet
- Thesis AsthmaDocument8 pagesThesis Asthmacjzarbkef100% (2)
- Auditory Verbal Hallucinations in Patients With Borderline Personality Disorder Are Similar To Those in SchizophreniaDocument7 pagesAuditory Verbal Hallucinations in Patients With Borderline Personality Disorder Are Similar To Those in SchizophrenializardocdNo ratings yet
- Ede QDocument5 pagesEde Qapi-286166842No ratings yet
- Clippers and Its MimicsDocument12 pagesClippers and Its Mimicsveerraju tvNo ratings yet
- Post Anesthesia Care UnitDocument19 pagesPost Anesthesia Care UnitRizqidio LarisoNo ratings yet
- LicenseSPC PA0002-009-002 16122008220131Document5 pagesLicenseSPC PA0002-009-002 16122008220131abdelaziz_ismail685662No ratings yet
- Finding The Future of Care Provision The Role of Smart HospitalDocument10 pagesFinding The Future of Care Provision The Role of Smart HospitalDian Putri SusantiNo ratings yet
- 1 Lecture 1Document75 pages1 Lecture 1Hoven MacasinagNo ratings yet
- An Excerpt From "Teeth" by Mary OttoDocument6 pagesAn Excerpt From "Teeth" by Mary OttoOnPointRadio0% (1)
- Dyspepsia: Group 3ADocument14 pagesDyspepsia: Group 3AAradhanaRamchandaniNo ratings yet
- Men's Health History: Personal InformationDocument5 pagesMen's Health History: Personal InformationBob DomkuskiNo ratings yet
- Cardianix Mission Vision SlogansDocument3 pagesCardianix Mission Vision SlogansArsal KhanNo ratings yet
- Types of Myocardial InfarctionDocument4 pagesTypes of Myocardial InfarctionntnquynhproNo ratings yet
- 2018.5.15 Insite Colo ContentDocument21 pages2018.5.15 Insite Colo ContentKatrinaBennettNo ratings yet
- Management of CholeraDocument69 pagesManagement of CholeraNatalia LawrenceNo ratings yet
- Research Proposal SampleDocument4 pagesResearch Proposal SampleClaire marionette LlamasNo ratings yet
- History of StatinsDocument32 pagesHistory of StatinsCelia Nieto Romero0% (1)
- Jcthe Role of Abutment-Attachment Selection in Resolving Inadequate Interarch Distance: A Clinical ReportdDocument7 pagesJcthe Role of Abutment-Attachment Selection in Resolving Inadequate Interarch Distance: A Clinical ReportdSyed Noorani100% (1)
- Bariño, Patricia Jamin: Online Grades InquiryDocument1 pageBariño, Patricia Jamin: Online Grades InquirySamiracomputerstation Kuya MarvsNo ratings yet
- Rheumatology: With Kartik Rangaraj MDDocument39 pagesRheumatology: With Kartik Rangaraj MDNailahRahmahNo ratings yet