Professional Documents
Culture Documents
Hypertension and Lipids - Lothian Hypertriglyceridaemia Guideline. May 2019
Uploaded by
J WongCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hypertension and Lipids - Lothian Hypertriglyceridaemia Guideline. May 2019
Uploaded by
J WongCopyright:
Available Formats
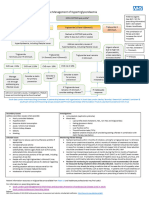
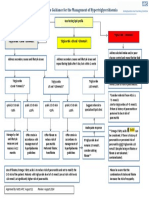
NHS Lothian Primary Care Summary Guidance for the Investigation & Management of
Hypertriglyceridaemia November 2017
A Guide to Best Practice in Lothian revised in line with 2016 updated NICE Guidelines
Dr T Caparrotta, Dr S Jenks, Dr I MacIntyre, Dr J Malo, Prof S Maxwell, Dr E Morrison, Dr P Rae and Prof DJ Webb
Triglycerides (TG) (mmol/L) Raised TG
▪ Routinely measured as part of a full lipid profile to e.g. >5mmol/L on a random sample
enable LDL calculation.
▪ TG testing in isolation is rarely indicated.
▪ Can be elevated on a non-fasting sample due to Repeat fasting lipid profile
the presence of dietary TG, consider fasting to confirm in 1-2 weeks
sample.
▪ Very high TG levels e.g. >10mmol/L are
associated with pancreatitis; increased morbidity
and mortality independent of CVD risk. If fasting TG raised at >2.5
▪ High TG are most commonly due to secondary
causes e.g. poorly controlled diabetes mellitus, ▪ Assess & treat secondary
alcohol excess or medications. causes†
▪ The relationship between TG and cardiovascular
▪ Give lifestyle & dietary advice*
risk is unclear. Overall it is felt that raised TG still
confer a small degree of additional risk. ▪ Repeat fasting lipid profile after
above interventions
Clinical assessment
Check BP, measure weight/BMI,
TG 2.5 – 4.49 TG 4.5 – 10 TG >10
smoking status & alcohol intake
▪ Continue to treat ▪ Treat with a statin if at ▪ Refer to
Examine for any skin changes secondary care
suggestive of a primary any secondary significant
causes cardiovascular risk ▪ Optimise any
hyperlipidaemia
▪ Reinforce (based on usual criteria) secondary causes
Check TFTs, fasting blood glucose ▪ Consider
(click here for more information on lifestyle advice ▪ If treatment is not
▪ Regular TG started repeat TG starting a fibrate
the diagnostic work-up for
diabetes), renal function, liver monitoring not in 1 month to confirm if not contra-
function, MCV and GGT required TG remain <10 indicated
† Consider any relevant secondary
causes e.g. review medications
Further tests as appropriate e.g. During treatment
pregnancy test, urinalysis to check ▪ Repeat fasting lipid profile & ALT in 8 weeks
for proteinuria ▪ No specific treatment target exists for TG at present
† ▪ In this group the main treatment aim is to transform a
Secondary causes of raised TG
highly atherogenic lipid profile with moderately raised
Alcohol excess Hypothyroidism
TG, high LDL and low HDL into a less atherogenic
Nephrotic syndrome/ Immunoglobulin one
renal disease excess ▪ If TG remain > 5 on statin treatment and the patient is
Drugs (including Bulimia at high cardiovascular risk we recommend specialist
thiazides, non- Pregnancy advice is obtained(preferably via e-mail)
cardioselective beta
Obesity
blockers, oestrogens,
Insulin resistance
tamoxifen, Seek specialist advice
Diabetes
corticosteroids)
Metabolic syndrome ▪ If TG >10
▪ TG 5–10 in a high cardiovascular risk patient
* Lifestyle advice not responding to statin treatment
Weight loss, if appropriate ▪ Suspected familial hyperlipidaemia
▪ Patients with significant hyperlipidaemia that is
Reduce or abstain from alcohol
proving difficult to manage in primary care
Dietary modification: ▪ Refer urgently to secondary care those with TG >20
▪ reduce total calorie intake by minimizing
not caused by alcohol or poor glycaemic control
intake of fats and carbohydrate
▪ increase intake of fish, especially oily fish
Clinic Specialist advice contact details
Smoking cessation (smoking independently
Lipid Clinic, RIE RIE.LipidClinicAdvice@luht.scot.nhs.uk
increases TG levels)
CVD risk clinic, WGH WGH.CardiovascRiskAdvice@luht.scot.nhs.uk
Increase physical activity Lipid clinic, SJH Tel: 01506 523 841
Version: 2, Approved: ADTC ‘17, Review date: 11/20 Lothian lipid guidelines here
You might also like
- This Study Resource Was: FNP I Final Review Powerpoint QuestionsDocument5 pagesThis Study Resource Was: FNP I Final Review Powerpoint QuestionsMartin HusseinNo ratings yet
- Hi Per Colesterol Emi ADocument38 pagesHi Per Colesterol Emi AFernando ArancibiaNo ratings yet
- Dyslipidemia: Established FactsDocument2 pagesDyslipidemia: Established FactsmeilunlyNo ratings yet
- Dyslipedemia ShortDocument5 pagesDyslipedemia Shortذوالفقار أحمدNo ratings yet
- Type 2 DMDocument19 pagesType 2 DMhussain AltaherNo ratings yet
- "Dyslipidemia" : Dyslipidemia Caused by Excessive Hepatic Secretion of VLDLDocument5 pages"Dyslipidemia" : Dyslipidemia Caused by Excessive Hepatic Secretion of VLDLDANEKKA TANNo ratings yet
- Atorvastatin Calcium Drug Study WWW RNpedia ComDocument3 pagesAtorvastatin Calcium Drug Study WWW RNpedia ComSha AbdulaNo ratings yet
- Dyslipidemia Malaysian CPG 2011Document23 pagesDyslipidemia Malaysian CPG 2011aideeh3110No ratings yet
- HyperlipidemiaDocument17 pagesHyperlipidemiabent alfay7a2No ratings yet
- Dyslipidemia 2023Document39 pagesDyslipidemia 2023medt80No ratings yet
- Treatment Protocol For Type-II Diabetes MellitusDocument7 pagesTreatment Protocol For Type-II Diabetes MellitusSOUMIK MANDALNo ratings yet
- How To Approach A Case of Dyslipidemia Y2!30!31Document10 pagesHow To Approach A Case of Dyslipidemia Y2!30!31MaisaraNo ratings yet
- LIPIDS Guidance For The Management of Hypertriglyceridaemia July 2018Document2 pagesLIPIDS Guidance For The Management of Hypertriglyceridaemia July 2018siti munajaliahNo ratings yet
- Treatment of Lipid Disorders-SchubartDocument76 pagesTreatment of Lipid Disorders-SchubartOliver OwuorNo ratings yet
- Management of HyperlipidemiaDocument39 pagesManagement of HyperlipidemiaRajgopal100% (2)
- TPN and Pregnancy: Related To Hyperemesis GravidarumDocument37 pagesTPN and Pregnancy: Related To Hyperemesis Gravidarumapi-319236078No ratings yet
- HypercholesterolemiaDocument7 pagesHypercholesterolemiaRiskullah MakmurNo ratings yet
- CPT CC5Document103 pagesCPT CC5KAYLLIEN DURANNo ratings yet
- Lecture 7 Diabetes Mellitus 2021Document39 pagesLecture 7 Diabetes Mellitus 2021Ahmed ShakerNo ratings yet
- ENDO - Metabolic SyndromeDocument3 pagesENDO - Metabolic SyndromeHajime NakaegawaNo ratings yet
- DRUGSTUDY AtorvastatinDocument2 pagesDRUGSTUDY AtorvastatinMicaela Andrea CieloNo ratings yet
- Diabetes Mellitus 2021Document61 pagesDiabetes Mellitus 2021Andarge ImperialNo ratings yet
- Bpjs Case Study DiabetesDocument33 pagesBpjs Case Study DiabetesAdhi TjahyadiNo ratings yet
- Approach To Management of NCDDocument54 pagesApproach To Management of NCDrohil jainNo ratings yet
- DyslipidemiaDocument11 pagesDyslipidemiaDr-Mohammed ElsawyNo ratings yet
- 2nd Case Session ToT CPG HPTDocument127 pages2nd Case Session ToT CPG HPThakimahsNo ratings yet
- Origin and Therapy For Hypertriglyceridaemia in Type 2 DiabetesDocument12 pagesOrigin and Therapy For Hypertriglyceridaemia in Type 2 DiabetesArturo Sànchez DìazNo ratings yet
- Genetic Disorders Causing Hypertriglyceridemia in Children and AdolescentsDocument32 pagesGenetic Disorders Causing Hypertriglyceridemia in Children and AdolescentsThanasis PapatheodorouNo ratings yet
- AtorvastatinDocument2 pagesAtorvastatinMichael Kuzbyt100% (4)
- Diabetes FNP IIDocument9 pagesDiabetes FNP IImilkah mwauraNo ratings yet
- Diabetes Mellitus: (DM)Document84 pagesDiabetes Mellitus: (DM)Andika HNo ratings yet
- Diabetes Yale CurriculumDocument20 pagesDiabetes Yale CurriculumAbid JamilNo ratings yet
- CPG DyslipidemiaDocument26 pagesCPG DyslipidemiaRenzy SalumbreNo ratings yet
- Dyslipidemia: Dr. Sohail AhmadDocument36 pagesDyslipidemia: Dr. Sohail AhmadChong Zhi LinNo ratings yet
- Final Presentation-2Document12 pagesFinal Presentation-2api-652480224No ratings yet
- Screening and Management of DyslipidemiaDocument16 pagesScreening and Management of DyslipidemiaSakina GhaziNo ratings yet
- Hyperlipidemia: Revised: October 4, 2019Document7 pagesHyperlipidemia: Revised: October 4, 2019HannaNo ratings yet
- Case Study DM & CKDDocument22 pagesCase Study DM & CKDNavina PurushotmananNo ratings yet
- Management of Dyslipidemia and The Prevention of Cardiovascular DiseaseDocument2 pagesManagement of Dyslipidemia and The Prevention of Cardiovascular DiseaseBenny TrisaktyariNo ratings yet
- Atorvastatin Drugs StudyDocument3 pagesAtorvastatin Drugs StudyRodolfo CampoNo ratings yet
- Updated For Diabetes Mellitus: Krairat Komdee, MD. Department of Internal Medicine Phayao HospitalDocument47 pagesUpdated For Diabetes Mellitus: Krairat Komdee, MD. Department of Internal Medicine Phayao HospitalKrairat KomdeeNo ratings yet
- CPT Group 5 Section DDocument83 pagesCPT Group 5 Section DLinus WerkeNo ratings yet
- Diabetes MellitusDocument32 pagesDiabetes Mellitusanfalalamin9915No ratings yet
- 6.2 Diabetes MellitusDocument53 pages6.2 Diabetes MellitusMohammad AlrefaiNo ratings yet
- UNSW Medicine GP Management Vivas: Lawson Ung UNSW VI 2015Document41 pagesUNSW Medicine GP Management Vivas: Lawson Ung UNSW VI 2015hernandez2812No ratings yet
- Thiazolidinediones (NCBI) : Go ToDocument5 pagesThiazolidinediones (NCBI) : Go ToPatrick CommettantNo ratings yet
- Hyprlipdemia 2020 4th EditionDocument24 pagesHyprlipdemia 2020 4th EditionLillian KrazemNo ratings yet
- Common ConditionsDocument64 pagesCommon Conditionsch wNo ratings yet
- Oral Diabetes Mellitus MedicationsDocument43 pagesOral Diabetes Mellitus MedicationsSanjeev Harry BudhooramNo ratings yet
- LC HyperlipidemiaDocument11 pagesLC Hyperlipidemiaabdul basithNo ratings yet
- Hypolipidemic AgentsDocument39 pagesHypolipidemic AgentsAC ACNo ratings yet
- Caso Clínico de DislipidemiaDocument3 pagesCaso Clínico de DislipidemiaCamiiliita Fernández La TorreNo ratings yet
- Diabetes Mellitus: Supervisor: DR ShaleenaDocument80 pagesDiabetes Mellitus: Supervisor: DR ShaleenaMuhamad HilmiNo ratings yet
- Lipid ManagementDocument2 pagesLipid ManagementMedicina FamiliarNo ratings yet
- Pcos GP Tool 2dec2013Document6 pagesPcos GP Tool 2dec2013Maram AbdullahNo ratings yet
- Cardiovascular DiseasesDocument8 pagesCardiovascular DiseasesRebecca MarshallNo ratings yet
- Kuliah Dislipidemia Dan ObesitasDocument50 pagesKuliah Dislipidemia Dan ObesitasiikNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- G6PD - Indiana Hemophilia & Thrombosis CenterDocument5 pagesG6PD - Indiana Hemophilia & Thrombosis CenterJ WongNo ratings yet
- Diabetes Type 2 Treatment AlgorithmDocument25 pagesDiabetes Type 2 Treatment AlgorithmJ Wong100% (1)
- Best Tests Oct2012 Glandular Pages 10-17Document8 pagesBest Tests Oct2012 Glandular Pages 10-17J WongNo ratings yet
- Bpac CRP Esr Reminder WVDocument2 pagesBpac CRP Esr Reminder WVJ WongNo ratings yet
- Blood Glucose Control Pathway in Type 2 Diabetes Apr 2013Document2 pagesBlood Glucose Control Pathway in Type 2 Diabetes Apr 2013J WongNo ratings yet
- Travel Medicine - NHG PharmacyDocument2 pagesTravel Medicine - NHG PharmacyJ WongNo ratings yet
- TGlipids NHSguidleiensDocument1 pageTGlipids NHSguidleiensJ WongNo ratings yet
- Antiplatelet Guidance March 2014 Amended December 2014 2.1Document4 pagesAntiplatelet Guidance March 2014 Amended December 2014 2.1J WongNo ratings yet
- Edc Contractors Basic Safety Training: "New Normal" EditionDocument8 pagesEdc Contractors Basic Safety Training: "New Normal" EditionCharles Rommel TadoNo ratings yet
- Minor Losses ExperimentDocument4 pagesMinor Losses ExperimentRaj GuptaNo ratings yet
- BJ SurfactantsDocument2 pagesBJ SurfactantsAquiles Carrera100% (2)
- Astm D6321-98-2004Document3 pagesAstm D6321-98-2004Thyagu LingamurthyNo ratings yet
- Hydrostatics-Assignment 3: MPI td9Document2 pagesHydrostatics-Assignment 3: MPI td9whoeverNo ratings yet
- EPA Process Design Manual For Carbon AdsorptionDocument211 pagesEPA Process Design Manual For Carbon AdsorptionchongchoifattNo ratings yet
- Truss Design GuidDocument3 pagesTruss Design GuidRafi HasanNo ratings yet
- Post Graduate Diploma in Psychological CounselingDocument1 pagePost Graduate Diploma in Psychological CounselingAvalokiteswari KurupNo ratings yet
- Chapter 8 - Nervous ReviewerDocument18 pagesChapter 8 - Nervous Reviewerchristian anchetaNo ratings yet
- Lover Album LyricsDocument34 pagesLover Album LyricsMichael PlanasNo ratings yet
- AlasDocument3 pagesAlasdara HinariNo ratings yet
- Op Amp AssignmentDocument10 pagesOp Amp AssignmentJuan-Wian CoetzerNo ratings yet
- FF - Fire Extinguisher LayoutDocument1 pageFF - Fire Extinguisher LayoutRanielNo ratings yet
- Unit 1Document175 pagesUnit 1Karthikeya SharmaNo ratings yet
- JC 1010Document19 pagesJC 1010mcsmiley11No ratings yet
- Distribution System ReliabilityDocument8 pagesDistribution System Reliabilityabera alemayehuNo ratings yet
- Project Sanjay YadavDocument51 pagesProject Sanjay YadavriyacomputerNo ratings yet
- OpenSeesPL 5ICEEDocument6 pagesOpenSeesPL 5ICEEDaniel Hernandez AtencioNo ratings yet
- Raw Material Chemical AnalysisDocument41 pagesRaw Material Chemical AnalysisVinod Kumar VermaNo ratings yet
- Elementary Statistics A Step by Step Approach 9th Edition Bluman Solutions ManualDocument23 pagesElementary Statistics A Step by Step Approach 9th Edition Bluman Solutions Manuala305894328100% (3)
- SURELAM-380,540II (User Manual)Document25 pagesSURELAM-380,540II (User Manual)kamran.sefyaliyevNo ratings yet
- Designing New Vanillin Schiff Bases and Their Antibacterial StudiesDocument4 pagesDesigning New Vanillin Schiff Bases and Their Antibacterial StudiesAvinash PurohitNo ratings yet
- User'S Design Requirements For Single Chamber Pressure VesselsDocument8 pagesUser'S Design Requirements For Single Chamber Pressure VesselspjsanchezmNo ratings yet
- PPG 2020Document131 pagesPPG 2020Syed Rohail AhmedNo ratings yet
- Calculus II: Prepared By: Cathleen HoboDocument19 pagesCalculus II: Prepared By: Cathleen HoboEspinosa Teves FernanNo ratings yet
- 00capítulo - The Routledge Handbook of Henri Lefebvre, The City and Urban SocietyDocument12 pages00capítulo - The Routledge Handbook of Henri Lefebvre, The City and Urban SocietyJeronimoNo ratings yet
- Features and Highlights - : CapableDocument2 pagesFeatures and Highlights - : CapableaarianNo ratings yet
- Opti-Cal TPS1200 Terminal Mode QuickguideDocument4 pagesOpti-Cal TPS1200 Terminal Mode QuickguideClaudiu OvidiuNo ratings yet
- Animal Cells PDFDocument4 pagesAnimal Cells PDFFalah HabibNo ratings yet