Professional Documents
Culture Documents
Case Study
Uploaded by
rum cueszhOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Study
Uploaded by
rum cueszhCopyright:
Available Formats
I.
INTRODUCTION
II. DESCRIPTION OF CLIENT’S DIAGNOSES AND ASSESSMENT HISTORY
a) Client’s personal and demographic data and lifestyle factors:
Age:
Sex:
Birthday:
Address:
Role:
Religion:
Weight:
Height:
b) Client’s chief complaint:
c) History of the present illness:
d) Past Medical History:
e) Review of Systems:
Constitutional symptoms:
Blood pressure:
Respiratory rate:
Pulse rate:
Temperature:
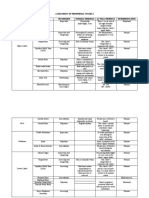
f) Gordon’s 11 Functional Health Patterns
g) Physical Assessment and other Vital Assessment
I. General Survey and Vital Signs
Date:
Time:
VITAL SIGNS MEASUREMENTS
Blood Pressure: Age:
Temperature: Weight:
Pulse Rate: Height:
Respiratory Rate: BMI:
Oxygen Saturation:
GCS
Eye-opening =
Verbal Response =
Best Motor Response =
You might also like
- Medical CertificateDocument1 pageMedical Certificatepaul vinothNo ratings yet
- First Aid ReportDocument2 pagesFirst Aid ReportOezm-mhan JocamerzNo ratings yet
- Medical Fitness For OfficersDocument1 pageMedical Fitness For OfficersApoorv TripathiNo ratings yet
- Confidential Medical ReportDocument1 pageConfidential Medical Reportariyogamd9No ratings yet
- Cardio ChaDocument6 pagesCardio ChaKhim BalcitaNo ratings yet
- Health and WellnessDocument21 pagesHealth and WellnessRahul KapooorNo ratings yet
- Baseline Health Monitoring Data Sheet SampleDocument1 pageBaseline Health Monitoring Data Sheet SampleStewart CredoNo ratings yet
- Medical Checkup FormatDocument2 pagesMedical Checkup FormatLinson Johnson71% (14)
- Week 1: Item PointsDocument112 pagesWeek 1: Item PointsAngel Lynn YlayaNo ratings yet
- First Page PDF - 2Document1 pageFirst Page PDF - 2aftab khanNo ratings yet
- Rigonan, Alexander John Hendrix III S. PFT FormDocument2 pagesRigonan, Alexander John Hendrix III S. PFT FormALEXANDER JOHN HENDRIX III RIGONANNo ratings yet
- Antenatalassessment 20 200302040026Document7 pagesAntenatalassessment 20 200302040026Anitha SnowhiteNo ratings yet
- College of Allied Health Sciences Nursing Department: Rizal Street, Iloilo CityDocument9 pagesCollege of Allied Health Sciences Nursing Department: Rizal Street, Iloilo CityArianne Nicole PinuelaNo ratings yet
- Physio Respiratory Ax TemplateDocument7 pagesPhysio Respiratory Ax TemplateHussain LaftaNo ratings yet
- DPN Icu PDFDocument1 pageDPN Icu PDFharoonNo ratings yet
- PFC - General PhysicianDocument2 pagesPFC - General PhysicianIMTEYAZ mallickNo ratings yet
- HA Finals TemplateDocument7 pagesHA Finals TemplateWilfredo V. BelloNo ratings yet
- Pa Tool MihpDocument23 pagesPa Tool MihpNassif M. BangcolaNo ratings yet
- First Page PDFDocument1 pageFirst Page PDFdheerajjakhranaNo ratings yet
- Celiac Disease Symptoms in Athletes: Prevalence Indicators of Perceived Quality of LifeDocument10 pagesCeliac Disease Symptoms in Athletes: Prevalence Indicators of Perceived Quality of LifenutrijudemetrioNo ratings yet
- Fitness Assessment FormDocument4 pagesFitness Assessment FormKimberly LectanaNo ratings yet
- Obstetric Form EditableDocument4 pagesObstetric Form EditableJhannyt Jyn BasaloNo ratings yet
- Taller People Should Have Higher BMI's and Blood Pressure Measurements As Their NormalDocument2 pagesTaller People Should Have Higher BMI's and Blood Pressure Measurements As Their Normalwisam salehNo ratings yet
- Obesity Health Assessment FormDocument5 pagesObesity Health Assessment FormMansi DarjiNo ratings yet
- HT SampleDocument4 pagesHT SampleElla YuNo ratings yet
- Physical Fitness Certificate Employee Full Name: RBEI-BOSCH Medical Professional RecommendationsDocument2 pagesPhysical Fitness Certificate Employee Full Name: RBEI-BOSCH Medical Professional RecommendationsBeuny MathewsNo ratings yet
- Digital Healthcare Kiosk With Analyser 1Document7 pagesDigital Healthcare Kiosk With Analyser 1happyboneshealthcarehbhNo ratings yet
- Case ClosedDocument10 pagesCase ClosedIvel Kram DunoNo ratings yet
- Antenatal Assessment PDFDocument7 pagesAntenatal Assessment PDFVikiNo ratings yet
- Case Record FormDocument5 pagesCase Record FormMontu ChakmaNo ratings yet
- Care Plan Client ProfileDocument13 pagesCare Plan Client ProfileVaishali SinghNo ratings yet
- Biodata of The PatientDocument8 pagesBiodata of The PatientRuchika KaushalNo ratings yet
- J of Clinical Hypertension - 2020 - Candan - The Relationship Between Nocturnal Blood Pressure Drop and Body CompositionDocument7 pagesJ of Clinical Hypertension - 2020 - Candan - The Relationship Between Nocturnal Blood Pressure Drop and Body Compositionanthony.teggNo ratings yet
- Form 86Document8 pagesForm 86Hanna Jane BayarcalNo ratings yet
- Form Pemeriksanaan FTDocument4 pagesForm Pemeriksanaan FTNurul Misna LestariNo ratings yet
- PhysicalFitness CertificateDocument2 pagesPhysicalFitness Certificatesoyamsidh dasNo ratings yet
- HXPEDocument2 pagesHXPEPaulaSarahNo ratings yet
- The Role of Healthy Lifestyles in Healthy AgingDocument3 pagesThe Role of Healthy Lifestyles in Healthy AgingDESMOND EZIEKENo ratings yet
- Wellness Expo 2021Document6 pagesWellness Expo 2021Doctora MaryNo ratings yet
- Rossi 2012Document12 pagesRossi 2012Neha RauhilaNo ratings yet
- Medical Record & SheetDocument9 pagesMedical Record & SheetTawfek RedaNo ratings yet
- Relationship Between Obesity, Physical Activity, Sleeping Hours and Red Blood Cell Parameters in Adult Sudanese PopulationDocument6 pagesRelationship Between Obesity, Physical Activity, Sleeping Hours and Red Blood Cell Parameters in Adult Sudanese Populationyuuki asunaNo ratings yet
- Statement of The ProblemDocument13 pagesStatement of The ProblemDaniel LeoNo ratings yet
- ICU Initial Assessment SheetDocument2 pagesICU Initial Assessment SheetNac OsceNo ratings yet
- Teachers' Health Examination Card (CS Form 86)Document2 pagesTeachers' Health Examination Card (CS Form 86)MelynJoyObiSoAuman100% (1)
- Postnatalassessment 190419153322Document3 pagesPostnatalassessment 190419153322megha30kashyap09No ratings yet
- The Fundamental of Anti-Aging Medicine: Wimpie PangkahilaDocument44 pagesThe Fundamental of Anti-Aging Medicine: Wimpie PangkahilajujuNo ratings yet
- SEMPRO Bismillah PDFDocument15 pagesSEMPRO Bismillah PDFAlisantoniNo ratings yet
- Case StudyDocument31 pagesCase StudySubhalaxmi SahuNo ratings yet
- Social Determinants of Health and Well-Being Among Young PeopleDocument28 pagesSocial Determinants of Health and Well-Being Among Young Peoplealex kNo ratings yet
- Case Presentation FormatDocument11 pagesCase Presentation FormatSweetzel MoratallaNo ratings yet
- Postnatal Examination and CareDocument5 pagesPostnatal Examination and CareAnusha VergheseNo ratings yet
- West Visayas State University: College of NursingDocument12 pagesWest Visayas State University: College of NursingelleNo ratings yet
- CPG IP Pneumonia-AdultDocument15 pagesCPG IP Pneumonia-Adultkarthi keyanNo ratings yet
- CS Form 86 ExternalDocument2 pagesCS Form 86 ExternalJessah Chris Eve Valle100% (1)
- Lectorial 3 Conceptual ModellingDocument27 pagesLectorial 3 Conceptual ModellingNoor PervezNo ratings yet
- General HistoryDocument16 pagesGeneral HistoryjjNo ratings yet
- Pediatric History and Physical Exam TemplateDocument4 pagesPediatric History and Physical Exam TemplateJay Pee Tumaliuan Tumanguil0% (2)
- Physical Assessment Measurements Measurements Norms Findings Interpretation Deviation From NormalDocument30 pagesPhysical Assessment Measurements Measurements Norms Findings Interpretation Deviation From NormalAbie Jewel Joy RoqueNo ratings yet
- Teaching Exercise to Children: A Complete Guide to Theory and PracticeFrom EverandTeaching Exercise to Children: A Complete Guide to Theory and PracticeRating: 5 out of 5 stars5/5 (1)
- NCM 100 - Theoritical Foundation of NursingDocument11 pagesNCM 100 - Theoritical Foundation of Nursingrum cueszhNo ratings yet
- UTS Quarantivity103Document4 pagesUTS Quarantivity103rum cueszhNo ratings yet
- Ped 101Document3 pagesPed 101rum cueszhNo ratings yet
- MICROPARALABDocument13 pagesMICROPARALABrum cueszhNo ratings yet
- NSTPDocument7 pagesNSTPrum cueszhNo ratings yet
- AnsDocument1 pageAnsrum cueszhNo ratings yet
- Matters: ElectionDocument1 pageMatters: Electionrum cueszhNo ratings yet
- Enrolled SubjectsDocument2 pagesEnrolled Subjectsrum cueszhNo ratings yet
- H.A PeriDocument5 pagesH.A Perirum cueszhNo ratings yet
- HNRDADocument3 pagesHNRDArum cueszhNo ratings yet
- LFD Iv PrimingDocument1 pageLFD Iv Primingrum cueszhNo ratings yet
- WEEK 3 Laboratory Activity 1 (STUDENT'S COPY)Document8 pagesWEEK 3 Laboratory Activity 1 (STUDENT'S COPY)rum cueszhNo ratings yet
- Human FlourishingDocument23 pagesHuman Flourishingrum cueszhNo ratings yet
- Laboratory Activity 1 On Integumentary System (STUDENT'S COPY)Document6 pagesLaboratory Activity 1 On Integumentary System (STUDENT'S COPY)rum cueszhNo ratings yet
- The Integumentary System (STUDENT'S COPY)Document8 pagesThe Integumentary System (STUDENT'S COPY)rum cueszhNo ratings yet