Professional Documents
Culture Documents
Arm and Leg Paresis As Outcome Predictors in Stroke Rehabilitation
Uploaded by
fernando_a_gonzalezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Arm and Leg Paresis As Outcome Predictors in Stroke Rehabilitation
Uploaded by
fernando_a_gonzalezCopyright:
Available Formats
Arm and leg paresis as outcome predictors in stroke rehabilitation.
T S Olsen
Stroke. 1990;21:247-251
doi: 10.1161/01.STR.21.2.247
Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1990 American Heart Association, Inc. All rights reserved.
Print ISSN: 0039-2499. Online ISSN: 1524-4628
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://stroke.ahajournals.org/content/21/2/247
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in
Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click Request
Permissions in the middle column of the Web page under Services. Further information about this process is
available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Stroke is online at:
http://stroke.ahajournals.org//subscriptions/
Downloaded from http://stroke.ahajournals.org/ by guest on March 13, 2014
247
Arm and Leg Paresis as Outcome Predictors
in Stroke Rehabilitation
Tom Skyh0j Olsen, MD
I used leg and arm paresis to predict outcome measured as extremity function in a prospective
study of 75 consecutive hemiplegic patients admitted to an inpatient stroke rehabilitation unit.
In each patient, extremity paresis was quantified according to the five-point scoring system
advised by the Medical Research Council, upper extremity function was quantified using the
Barthel Index subscore for feeding and dressing the upper body, and lower extremity function
was quantified according to a five-point scoring of the ability to walk. Improvement was
recorded for upper extremity function in 52% of the patients and for lower extremity function
in 89%. Best extremity function was reached a mean±SEM of 9±3 and 10±4 weeks after stroke
for the upper and lower extremities, respectively. In patients experiencing complete recovery,
this occurred a mean±SEM of 7±2 weeks (for both upper and lower extremities) after the
stroke. Only 8-11% of the patients with paresis scores of ^2 regained independent extremity
function after rehabilitation. Half of the patients with paresis scores of ^3 regained indepen-
dent extremity function after rehabilitation, while the other half were able to perform extremity
function with only minimal assistance. As predictors of extremity function, the Barthel Index
subscore was slightly better (r=0.64) than paresis score (r=0.58). However, because evaluation
of extremity paresis is easy, it appears to be useful as a preliminary predictor of outcome
following stroke. (Stroke 1990;21:247-251)
I mprovement of both upper and lower extremity
function is one of the major objectives of stroke
rehabilitation since extremity function greatly
affects the overall outcome. My investigation was
undertaken to study upper and lower extremity func-
was made up of 66 patients with unilateral upper
extremity paresis who on admission were unable to
feed themselves and/or to dress their upper body
independently; seven patients with lower extremity
paresis but no upper extremity paresis and two
tion after rehabilitation for stroke and the time to patients with unreliable scoring of upper extremity
reach maximum extremity function. Another purpose function were excluded. The second group was made
of my study was to predict outcome measured as up of 72 patients with unilateral lower extremity
extremity function on the basis of a simple bedside paresis who on admission were unable to walk inde-
evaluation on admission, that is, the degree of weak- pendently; three patients who had upper extremity
ness in the paretic arm and leg. paresis but no lower extremity paresis were excluded.
Subjects and Methods
Computed tomography or magnetic resonance imag-
ing was performed in all patients before referral to
This was a prospective study of consecutive rehabilitation.
patients admitted to an inpatient stroke rehabilita-
tion unit. I excluded patients who were admitted >60 On admission to the rehabilitation unit, all patients
days after their stroke, those who did not have had a full neurologic examination including evalua-
paresis, and those who had strokes involving both tion of proximal (hip and shoulder flexion) and distal
cerebral hemispheres. Seventy-five patients satisfied (ankle and finger flexion) leg and arm paresis scored
these criteria. From this population, I established according to the system advised by the Medical
two overlapping groups to test the effect of upper and Research Council (1: a trace of contraction, 2: active
lower extremity paresis independently. One group movement with gravity eliminated, 3: active move-
ment against gravity, 4: active movement against
From the Burke Rehabilitation Center, White Plains, New York. gravity and resistance, and 5: normal power).1
Supported by the Burke Foundation and the Burke Rehabilita- Upper extremity function was evaluated according
tion Center.
Address for correspondence: Tom Skyhej Olsen, MD, Depart-
to the Barthel Index2 using subscores for the patients'
ment of Neurology, Gentofte Hospital, University of Copenhagen, ability to prepare a tray and feed themselves (6: can
DK-2900 Hellerup, Denmark. feed self a meal placed within reach, can put on an
Received November 3, 1988; accepted August 21, 1989. assist device if used, can cut food, spread butter, and
Downloaded from http://stroke.ahajournals.org/ by guest on March 13, 2014
248 Stroke Vol 21, No 2, February 1990
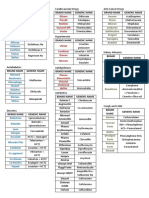
TABLE 1. Characteristics of 75 Stroke Patients contact guarding, minimal assistance, etc. Use of a
Patients with upper Patients with lower brace and a cane did not constitute assistance.
extremity paresis extremity paresis Overall stroke severity was assessed by determin-
Characteristic (n=66) (" = 72) ing the Barthel Index score of each patient on
Age (years) 68±10 67±11 admission.
Sex Statistical analysis was performed using linear
Females 33 33
regression analysis and the Mann-Whitney test.
Males 33 39 Results
Side affected
Patient characteristics are listed in Table 1. Leg
Left 30 39
and arm paresis score on admission correlated signif-
Right 36 33 icantly with extremity function score on discharge
Stroke mechanism (proximal upper extremity: /-=0.58, proximal lower
Hematoma 3 4 extremity: r=0.53, distal upper extremity: r=0.55,
Infarct 63 68 distal lower extremity: r=0.54;/?<0.01). Proximal and
Admission after stroke distal paresis scores were found to be equally good in
(weeks) 4±2 4±2 predicting outcome measured as function score. Only
Length of stay (weeks) 9±3 9±3 the relations between proximal paresis scores and
Data are mean±SEM or number. outcome are given below.
On admission, 40 patients had upper extremity
paresis scores of 22 (Table 2). Three (8%) regained
use salt/pepper; 4: some help required, but can feed independence in both upper extremity functions
self once food is cut up; and 0: unable to feed self) (scored 11 on discharge), and nine (23%) regained
and to dress their upper body (5: able to put on, independence in at least one function (scored 9 or 11
fasten, and remove clothing; 3: needs help, but able on discharge). Eleven (42%) of the 26 patients with
to do at least half the work; and 0: performance upper extremity paresis scores of ^3 regained inde-
worse than described). The sum of the two Barthel pendence in both upper extremity functions, and 21
Index subscores was considered to be a measure of (81%) regained independence in at least one function.
upper extremity function. Patients who scored 11 On admission, 38 patients had lower extremity pare-
were independent in both upper extremity functions. sis scores of ^2 (Table 3). Four (11%) regained the
Those who scored 9 were independent in one func- ability to walk independently (scored 5 on discharge),
tion and needed only minimal assistance with the and 19 (50%) became able to walk >150 feet with
other. Patients who scored 7 and 3 or 4 needed assistance (scored 4 on discharge). Of the 34 patients
assistance in performing both functions. Patients who had paresis scores of ^ 3 , independent walking was
with the lowest possible function score, 0, needed regained by 19 (56%) and all 34 became able to walk
maximal help of another individual in performing > 150 feet with assistance or independently.
both upper extremity functions. Function thus refers The Barthel Index score on admission correlated
to both extremities, the paretic as well as the non- significantly with function score on discharge (upper
paretic one, while motor impairment refers to the extremity: r=0.64, lower extremity: r=0.65;/?<0.01).
paretic extremity only. Among the 28 patients with Barthel Index scores of
Lower extremity function was evaluated by scoring <40, only one (4%) regained independence in both
the patients' ability to walk (1: nonambulatory, 2: can upper extremity functions, and only six (21%)
walk <50 feet with assistance, 3: can walk 50-150 regained independence in at least one function
feet with assistance, 4: can walk >150 feet with (Table 4). Independence in both upper extremity
assistance, and 5: can walk independently). Patients functions was regained by 13 (34%) of the 38 patients
were said to require assistance when they needed the who had Barthel Index scores of £40, and 24 (63%)
presence of another individual for safety such as regained independence in at least one function.
TABLE 2. Proximal Upper Extremity Paresis on Admission and Upper Extremity Functional Outcome in 66 Stroke Patients
Paresis score Function score on discharge TotaJ
on admission 0 3,4 7 9 11 n %
0 5 8 10 4 2 29 44
1 0 3 2 2 0 7 10
2 0 1 2 0 1 4 6
3 0 1 3 3 4 11 17
4 0 1 0 7 7 15 23
Total 5 (8%) 14 (21%) 17 (26%) 16 (24%) 14 (21%) 66 100
Paresis scored by Medical Research Council system; function scored by Barthel Index subscores.
Downloaded from http://stroke.ahajournals.org/ by guest on March 13, 2014
Olsen Outcome Predictors in Stroke Rehabilitation 249
TABLE 3. Proximal Lower Extremity Paresis on Admission and Lower Extremity Functional Outcome in 72 Stroke Patients
Function score on discharge Total
Paresis score
on admission 1 2 3 4 5 n %
0 1 1 2 4 1 9 12
1 2 1 1 6 2 12 16
2 0 1 6 9 1 17 24
3 0 0 0 10 7 17 24
4 0 0 0 5 12 17 24
Total 3 (4%) 3 (4%) 9 (13%) 34 (47%) 23 (32%) 72 100
Paresis scored by Medical Research Council system; function scored by ability to walk.
Table 5 shows that among 28 patients with Barthel Discussion
Index scores of <40, only one (4%) regained the Functional outcome in this series was less favor-
ability to walk independently, while 14 (50%) were able than that reported for the average stroke pop-
able to walk > 150 feet with assistance after rehabil- ulation since no more than 21% and 32% regained
itation. Of the 44 patients with Barthel Index scores independent upper and lower extremity function,
of ^40, 22 (50%) regained independent walking and respectively. In unselected patients with stroke,
42 (95%) were able to walk >150 feet with assistance approximately 70% are able to feed and dress them-
or independently after rehabilitation. All four selves independently and >80%3"5 are able to walk
patients with Barthel Index scores of ^80 were able independently 6 months after the event.5 Wade et al6
to walk independently after rehabilitation. assessed lower extremity weakness 3-4 weeks after a
Table 6 shows the time to maximum extremity stroke in 196 unselected patients and found that 86%
function score in the patients who recovered. Upper had either no or only mild weakness. In my study, this
extremity function improved during rehabilitation in occurred in approximately 24% (paresis score of 4),
34 patients (52%), while lower extremity function which indicates that these patients were recruited
improved in 60 patients (89%). The patients who from those with more severe strokes, usually 20% of
improved were discharged a mean±SEM of 2±1 the stroke population.
weeks after they had reached their maximum extrem- Arm and leg paresis are easy to determine and
ity function score. Maximum score was reached 9±3 appear to be useful predictors of functional outcome.
(for the upper extremity) and 10±4 (for the lower Severe extremity paresis (Medical Research Council
extremity) weeks after the stroke; 95% of the patients scores of ^2 on admission) predicts a bad outcome.
had achieved their best extremity function within 14 Neither independent upper extremity function nor
weeks after their stroke. Patients who recovered com- independent walking should be expected by patients
pletely (achieved independent extremity function) did with paresis of that degree. Only 8% and 11% of my
so 7±2 weeks after the stroke, while patients who patients with paresis scores of £2 on admission per-
recovered only incompletely reached best extremity formed upper extremity functions and walked inde-
function 10±3 (for the upper extremity) and 10±4 pendently after rehabilitation. Approximately 40%
(for the lower extremity) after the stroke. This differ- were not able to walk 150 feet, even with assistance,
ence in time to maximum score is significant (p>0.03 and upper extremity function outcome was even
andp<0.002, respectively, by the Mann-Whitney test). worse; >75% of the patients with paresis scores of ^2
There was no significant difference between patients on admission still needed significant assistance with
with paresis scores of ^2 and those with scores of ^3 upper extremity function after rehabilitation.
in the time to maximum extremity function score Mild extremity paresis (Medical Research Council
scores of ^3 on admission) predicts a relatively good
(/?>0.05 by the Mann-Whitney test).
functional outcome. About half of these patients
TABLE 4. Overall Stroke Severity on Admission and Upper Extremity Functional Outcome in 66 Stroke Patients
Function score on discharge Total
Severity score
on admission 0 3,4 5-8 9 11 n %
0-19 3 2 2 0 0 7 11
20-39 2 9 4 5 1 21 32
40-59 0 3 7 7 4 21 32
60-79 0 0 4 4 8 16 24
80-100 0 0 0 0 1 1 1
Total 5 (8%) 14 (21%) 17 (26%) 16 (24%) 14 (21%) 66 100
Severity scored by Barthel Index; function scored by Barthel Index subscores.
Downloaded from http://stroke.ahajournals.org/ by guest on March 13, 2014
250 Stroke Vol 21, No 2, February 1990
TABLE 5. Overall Stroke Severity on Admission and Lower Extremity Functional Ontcome In 72 Stroke Patients
Function score on discharge Total
Severity score
on admission 1 2 3 4 5 n %
0-19 2 0 4 2 0 8 11
20-39 1 3 3 12 1 20 28
40-59 0 0 2 16 8 26 36
60-79 0 0 0 4 10 14 19
80-100 0 0 0 0 4 4 6
Total 3 (4%) 3 (4%) 9 (13%) 34 (47%) 23 (32%) 72 100
Severity scored by Barthel Index; function scored by ability to walk.
regained independent extremity function. After reha- stroke patients with hemiplegia, Newman19 found
bilitation, all were able to walk >150 feet with that little recovery took place later than 14 weeks
assistance or independently and 80% were either after the stroke and that the average interval from
independent or needed only minor assistance with stroke onset to 80% of final recovery was 6 weeks.
upper extremity functions. Prescott et al20 studied 100 patients with moderate-
Extensive work using the Barthel Index as a pre- severe strokes from 4 weeks after the stroke until
dictor of outcome has demonstrated a close relation discharge; 89% had reached their best functional
between the score on this index (i.e., overall func- outcome ^16 weeks after their stroke. Wade et al17
tion) at admission and outcome.3'5-14 The Barthel studied arm function in 92 patients over 2 years
Index cannot be established at the bedside on admis- following their stroke; statistically significant improve-
sion since it requires observation of the patient over ment was seen only during the first 3 months. In 135
several days. The Barthel Index seems to be slightly stroke patients studied by Andrews et al,18 maximum
better than extremity paresis in delineating those improvement for walking was reached within 8 weeks
patients who will be unable to perform upper extrem- after the stroke in 88% of the patients. These find-
ity functions or to walk independently after rehabil- ings are in accord with my findings. Best upper and
itation. In accordance with the findings of Granger et lower extremity function was obtained on average 9
a],9 in my study such functionally impaired patients and 10 weeks, respectively, after the stroke, and 95%
comprised only 4% of those with Barthel Index of the patients had reached their best upper and
scores of <40 compared with 8-11% of those with lower extremity function within 13 and 14 weeks,
Medical Research Council paresis scores of <2. The respectively.
Barthel Index is also better in predicting walking Stroke severity affects the time required to obtain
outcome in "high-level" patients (those with a Bar- maximal recovery. Length of stay in a rehabilitation
thel Index score of >80). unit is directly related to the severity of paresis on
Improvement may occur as long as 6-12 months admission.21-22 Patients with a low Barthel Index
after a stroke,31'-18 but the majority of functional score on admission recover more slowly than patients
recovery occurs within the first 3 months. Studying 39 with a high score.3 In my study, complete recovery of
TABLE 6. Time to Obtain Best Extremity Function in Stroke Patients Who Improved During Rehabilitation
Time (weeks) Best function reached
by 95% of patients Stroke-discharge interval
n Mean±SEM Range (weeks) (mean±SEM weeks)
upper extremity (/v=66)
Best function 34 9±3 5-16 13 11+4
All patients
Paresis score <,2 17 9±3 5-16 13 13±4
Paresis score S3 17 8±2 5-11 10 10±3
Incomplete recovery 21 10±3 5-16 13 13±3
Complete recovery 13 7±2* 5-10 10 9±3
Lower extremity (N=12)
Best function 60 10±4 4-27 14 12±5
All patients
Paresis score s 2 33 10±4 4-27 14 13±5
Paresis score &3 27 9±3 5-20 13 12±4
Incomplete recovery 37 10±4 4-27 18 14±5
Complete recovery 23 7±2t 5-11 10 10±3
*tp<0.03, 0.002, respectively, different from incomplete recovery by Mann-Whitney test.
Downloaded from http://stroke.ahajournals.org/ by guest on March 13, 2014
Olsen Outcome Predictors in Stroke Rehabilitation 251
extremity function was achieved on average 7 weeks 7. Granger CV, Greer DS, Liset E, Coulombe J, O'Brien E:
after the stroke, whereas recovery progressed for an Measurement of outcomes of care for stroke patients. Stroke
1975;6:34-41
average of 10 weeks in patients who achieved only 8. Granger CV, Sherwood CC, Greer DS: Functional status
incomplete recovery. measures in a comprehensive stroke care program. Arch Phys
Med Rehabil 1977;58:555-560
Andrews et al18 showed that approximately one 9. Granger CV, Dewis LS, Peters NC, Sherwood CC, Barrett JE:
third of moderately or severely disabled stroke Stroke rehabilitation: Analysis of repeated Barthel Index
patients had improvement of their walking between 3 measures. Arch Phys Med Rehabil 1979;60:14-17
10. Granger CV, Albrecht GL, Hamilton BB: Outcome of com-
and 6 months after their stroke. In my study, the prehensive medical rehabilitation: Measurement by PULSES
patients were discharged an average of 2 weeks after profile and the Barthel Index. Arch Phys Med Rehabil 1979;
maximum improvement was achieved. Although the 60:145-154
majority of the patients thus seemed to have reached 11. Hertanu JS, Demoupoulos JT, Yang WC, Calhoun WF,
Fenigstein HA: Stroke rehabilitation: Correlation and prog-
their best possible outcome on discharge, some nostic value of computerized tomography and sequential func-
patients may continue to improve. However, the tional assessments. Arch Phys Med Rehabil 1974;65:505-508
process of recovery may be so slow in these patients 12. Wade DT, Skilbeck CE, Hewer RL: Predicting ADL score at
6 months after an acute stroke. Arch Phys Med Rehabil
that recordable improvement of function requires >2 1986;64:24-28
weeks of observation during inpatient rehabilitation. 13. Gresham GE, Phillips TF, Labi MLC: ADL status in stroke:
Relative merits of three standard indexes. Arch Phys Med
Rehabil 1980;61:355-358
Acknowledgments 14. DeJong G, Branch L: Predicting the stroke patients ability to
live independently. Stroke 1982; 13:648-655
Thanks to Dr. Fletcher H. McDowell and Dr. 15. Hier DB, Mondlock J, Caplan LR: Recovery of behavioural
Michael J. Reding for invaluable advice during prep- abnormalities after right hemisphere stroke. Neurology 1983;
33:345-350
aration of the manuscript. 16. Bard G, Hirschberg GG: Recovery of voluntary motion in
upper extremity following hemiplegia. Arch Phys Med Rehabil
References 1965;46:567-572
17. Wade DT, Hewer RL, Wood VA, Skilbeck CE, Ismail HM:
1. Medical Research Council: Aids to the Examination of the The hemiplegic arm after stroke: Measurement and recovery.
Peripheral Nervous System. London, Her Majesty's Stationary J Neurol Neurosurg Psychiatry 1983;46:521-524
Office, 1976 18. Andrews K, Brocklehurst JC, Richards B, Laycock PJ: The
2. Mahoney F, Barthel D: Functional evaluation: The Barthel rate of recovery from stroke —And its measurement. Int
Index. Md Med J 1965;2:61-65 Rehabil Med 1981;3:155-161
19. Newman M: The process of recovery after hemiplegia. Stroke
3. Skillbeck CE, Wade DT, Hewer RL, Wood VA: Recovery 1972;3:702-710
after stroke. J Neurol Neurosurg Psychiatry 1983;46:5-8 20. Prescott RJ, Garraway WM, Akhtar AJ: Predicting functional
4. Strand T, Asplund K, Eriksson S, Hagg E, Lithner F, Wester outcome following acute stroke using a standard clinical
PO: A non-intensive stroke unit reduces functional disability examination. Stroke 1982;13:641-647
and the need for long term hospitalization. Stroke 1985; 21. Feigenson JS, McDowell FH, Meese P, McCarthy ML, Green-
16:29-34 berg SD: Factors influencing outcome and length of stay in a
5. Wade DT, Hewer RL: Functional abilities after stroke: Mea- stroke rehabilitation unit. Part 1. Analysis of 248 unscreened
surement, natural history and prognosis. J Neurol Neurosurg patients —Medical and functional prognostic indicators. Stroke
Psychiatry 1987;50:177-182 1977;8:651-656
22. Smith DL, Akhtar AJ, Garraway WM: Motor function after
6. Wade DT, Hewer RL, Skillbeck CE, David RM: Stroke. A stroke. Age Ageing 1985;14:46-48
Critical Approach to Diagnosis, Treatment and Management.
Chicago, Yearbook Medical Publishers, Inc, 1985 KEYWORDS • cerebrovasculardisorders • paresis • rehabilitation
Downloaded from http://stroke.ahajournals.org/ by guest on March 13, 2014
You might also like
- Bobath en Prevenciòn de Subuxacion de Hombro Despues de ECVDocument10 pagesBobath en Prevenciòn de Subuxacion de Hombro Despues de ECVLuisa SánchezNo ratings yet
- Faghri 1994Document7 pagesFaghri 1994Leticia PereiraNo ratings yet
- Trunk Impairment ScaleDocument11 pagesTrunk Impairment ScaleRavneet singhNo ratings yet
- Trunk Impairment Scale PDFDocument10 pagesTrunk Impairment Scale PDFPatricio Eduardo Barría AburtoNo ratings yet
- propiocepcion hombro post cirugiaDocument6 pagespropiocepcion hombro post cirugiamarcelogascon.oNo ratings yet
- E706 FullDocument17 pagesE706 FullDana DumitruNo ratings yet
- Lumbar Microdiscectomy With Spinal AnesthesiaDocument9 pagesLumbar Microdiscectomy With Spinal AnesthesiaRicardoNo ratings yet
- Stroke 32Document8 pagesStroke 32pokharelriwaj82No ratings yet
- Belardi Nell I 1999Document11 pagesBelardi Nell I 1999LidiyahNo ratings yet
- Trunk Impairment ScaleDocument11 pagesTrunk Impairment Scale林良駿No ratings yet
- Diagnostic Accuracy of Clinical Tests for Shoulder ImpingementDocument5 pagesDiagnostic Accuracy of Clinical Tests for Shoulder ImpingementAnanth NagarajNo ratings yet
- John E. Brown, Jason O. Jaeger, Todd A. Polatis, Alexander J. Peters, Paul A. Oakley, Deed E. HarrisonDocument11 pagesJohn E. Brown, Jason O. Jaeger, Todd A. Polatis, Alexander J. Peters, Paul A. Oakley, Deed E. HarrisonJose JiménezNo ratings yet
- The Immediate Effects of Lumbar Rotational Mobilization On Trunk Control and Gait Parameter in Patients With StrokeDocument7 pagesThe Immediate Effects of Lumbar Rotational Mobilization On Trunk Control and Gait Parameter in Patients With Stroke林良駿No ratings yet
- EMG en UCI - Club de Revista PDFDocument6 pagesEMG en UCI - Club de Revista PDFJOSE JULIAN BERNAL SANCHEZNo ratings yet
- Artrosis glenohumeral despues de artroscopia Bankart repair a long-term follow-up of 13 yearsDocument6 pagesArtrosis glenohumeral despues de artroscopia Bankart repair a long-term follow-up of 13 yearsmarcelogascon.oNo ratings yet
- Epidural Spinal Cord Stimulation Facilitates Immediate RestorationDocument11 pagesEpidural Spinal Cord Stimulation Facilitates Immediate RestorationnorazmiNo ratings yet
- Ravichandran Et Al 2019 Systematic Review On Effectiveness of ShoulderDocument11 pagesRavichandran Et Al 2019 Systematic Review On Effectiveness of ShoulderCynthia RodriguesNo ratings yet
- Task Oriented Improves Strength - Stroke PatientsDocument7 pagesTask Oriented Improves Strength - Stroke PatientsPedro FonsecaNo ratings yet
- Treatment of Bankart Lesions in Traumatic Anterior Instability of The ShoulderDocument9 pagesTreatment of Bankart Lesions in Traumatic Anterior Instability of The ShoulderphantomkatalynNo ratings yet
- SEGUIMIENTO A 5 AÑOS PTGH REVERSADocument7 pagesSEGUIMIENTO A 5 AÑOS PTGH REVERSAmarcelogascon.oNo ratings yet
- indice motorDocument4 pagesindice motormanu122114No ratings yet
- A Blinded, Randomized, Controlled Trial Assessing Conservative Management Strategie - 20170730120051Document8 pagesA Blinded, Randomized, Controlled Trial Assessing Conservative Management Strategie - 20170730120051sebafigueroa94No ratings yet
- Role of exercises in neurogenic thoracic outlet syndromeDocument4 pagesRole of exercises in neurogenic thoracic outlet syndromeGeraldine Alvarez ANo ratings yet
- Controlled Study of Neuroprosthetic Functional Electrical Stimulation in Sub-Acute Post-Stroke RehabilitationDocument5 pagesControlled Study of Neuroprosthetic Functional Electrical Stimulation in Sub-Acute Post-Stroke RehabilitationAiry MercadoNo ratings yet
- Recovery of Over-Ground Walking After Chronic Motor Complete Spinal Cord InjuryDocument7 pagesRecovery of Over-Ground Walking After Chronic Motor Complete Spinal Cord Injuryrich sitaNo ratings yet
- The Effect of Physical Training in Chronic Heart FailureDocument5 pagesThe Effect of Physical Training in Chronic Heart FailureDitaris GINo ratings yet
- Jurnal KardiovaskularDocument6 pagesJurnal Kardiovaskularrizk86No ratings yet
- Clinical Tests in Shoulder Examination - How To Perform ThemDocument7 pagesClinical Tests in Shoulder Examination - How To Perform ThemkabshielNo ratings yet
- ISPR8-1352: Posters (First Part) / Annals of Physical and Rehabilitation Medicine 61S (2018) E103-E308 E219Document1 pageISPR8-1352: Posters (First Part) / Annals of Physical and Rehabilitation Medicine 61S (2018) E103-E308 E219Amal VRNo ratings yet
- Lower HemiplegicDocument8 pagesLower HemiplegicdindasaviraNo ratings yet
- Fusion Rates and SF-36 Outcomes After Multilevel Laminectomy and Noninstrumented Lumbar Fusions in A Predominantly Geriatric PopulationDocument6 pagesFusion Rates and SF-36 Outcomes After Multilevel Laminectomy and Noninstrumented Lumbar Fusions in A Predominantly Geriatric PopulationMaria Daniela Jiménez AguilarNo ratings yet
- Myer 2013 A Users Guide To Performance of The Best Shoulder Physical Examination TestsDocument7 pagesMyer 2013 A Users Guide To Performance of The Best Shoulder Physical Examination TestsFabiano LacerdaNo ratings yet
- 115 Full-DikonversiDocument6 pages115 Full-DikonversiAnggelia jopa sariNo ratings yet
- Validity of The Lateral Gliding Test As Tool ForDocument7 pagesValidity of The Lateral Gliding Test As Tool ForFelippe GuarigliaNo ratings yet
- Jarbo OJSM Lever TestDocument7 pagesJarbo OJSM Lever Testashlyn granthamNo ratings yet
- Primary Total Shoulder Arthroplasty Performed Entirely Thru The Rotator Interval - Technique and Minimum Two-Year OutcomesDocument10 pagesPrimary Total Shoulder Arthroplasty Performed Entirely Thru The Rotator Interval - Technique and Minimum Two-Year OutcomesmotohumeresNo ratings yet
- Electrical Stimulation of Wrist Extensors in Poststroke HemiplegiaDocument7 pagesElectrical Stimulation of Wrist Extensors in Poststroke HemiplegiabastianusjuatmadjaNo ratings yet
- Cat 2Document5 pagesCat 2Edgardo BivimasNo ratings yet
- Posterior Fixation of APC-2 Pelvic Ring Injuries PDFDocument8 pagesPosterior Fixation of APC-2 Pelvic Ring Injuries PDFgevowo3277No ratings yet
- Sensorimotor Control Deficiency in Recurrent Anterior Shoulder Instability Assessed With A Stabilometric Force PlatformDocument6 pagesSensorimotor Control Deficiency in Recurrent Anterior Shoulder Instability Assessed With A Stabilometric Force PlatformA ANo ratings yet
- PicadoDocument3 pagesPicadoGrigori ChulakiNo ratings yet
- Barker 2008Document9 pagesBarker 2008AkinniyiOmobolanleNo ratings yet
- Diagnostic Values of Tests For Acromioclavicular Joint PainDocument6 pagesDiagnostic Values of Tests For Acromioclavicular Joint Painarum_negariNo ratings yet
- Brunnstrom2010 BraininjuryDocument8 pagesBrunnstrom2010 BraininjuryAndreaNo ratings yet
- Non-Operative Treatment of Subacromial Impingement Syndrome PDFDocument6 pagesNon-Operative Treatment of Subacromial Impingement Syndrome PDFAnonymous 8viyyVNo ratings yet
- Which Treatment Approach Is Better For Hemiplegic Shoulder Pain in Stroke PatientsDocument10 pagesWhich Treatment Approach Is Better For Hemiplegic Shoulder Pain in Stroke PatientsDiego Pinto PatroniNo ratings yet
- 2015 Schmitz FOCUSED AND RADIAL Shockwave For Musculoskeletal, More SmilaritiesDocument2 pages2015 Schmitz FOCUSED AND RADIAL Shockwave For Musculoskeletal, More SmilaritieskangmasNo ratings yet
- Beaulieu J. Y. 2006 Cerebral Plasticity in Crossed C7 Grafts of The Brachial Plexus An fMRI StudyDocument8 pagesBeaulieu J. Y. 2006 Cerebral Plasticity in Crossed C7 Grafts of The Brachial Plexus An fMRI StudyTatiane SantosNo ratings yet
- Mazzoleni 2015Document6 pagesMazzoleni 2015juanNo ratings yet
- Pandian Et Al 2013 Shoulder Taping Reduces Injury and Pain in StrokeDocument6 pagesPandian Et Al 2013 Shoulder Taping Reduces Injury and Pain in StrokeCynthia RodriguesNo ratings yet
- Prevention of Intractable Partial Seizures by Intermittent Vagal Stimulation in Humans: Preliminary ResultsDocument4 pagesPrevention of Intractable Partial Seizures by Intermittent Vagal Stimulation in Humans: Preliminary ResultsZeptalanNo ratings yet
- Echo 2Document16 pagesEcho 2Indera VyasNo ratings yet
- A Test Battery To Measure The Recovery of Voluntary Movement Control Following StrokeDocument4 pagesA Test Battery To Measure The Recovery of Voluntary Movement Control Following StrokeAashish G. ShresthaNo ratings yet
- Comparison of Ultrasound and Extracorporeal Shock Wave Therapy in Lateral EpicondylosisDocument6 pagesComparison of Ultrasound and Extracorporeal Shock Wave Therapy in Lateral EpicondylosisWilliam ChienNo ratings yet
- Physical Examination Tests For Hip Dysfunction and Injury: March 2015Document8 pagesPhysical Examination Tests For Hip Dysfunction and Injury: March 2015wladjaNo ratings yet
- Distribution of Muscle Strength Impairm e N T SDocument9 pagesDistribution of Muscle Strength Impairm e N T SPedro FonsecaNo ratings yet
- Effects of Kinesio Taping For Stroke Patients WithDocument8 pagesEffects of Kinesio Taping For Stroke Patients WithBias HerkawentarNo ratings yet
- Smith 2013 SMIIDocument9 pagesSmith 2013 SMIIGryseldaGryGryNo ratings yet
- Current Techniques in Canine and Feline NeurosurgeryFrom EverandCurrent Techniques in Canine and Feline NeurosurgeryAndy ShoresNo ratings yet
- Ammar Al Chalabi 2015 InstructivoDocument33 pagesAmmar Al Chalabi 2015 Instructivofernando_a_gonzalezNo ratings yet
- An EQ-5D-5L Value Set Based On Uruguayan Population PreferencesDocument20 pagesAn EQ-5D-5L Value Set Based On Uruguayan Population Preferencesfernando_a_gonzalezNo ratings yet
- An 2016Document10 pagesAn 2016fernando_a_gonzalezNo ratings yet
- Olsson 2005Document6 pagesOlsson 2005fernando_a_gonzalezNo ratings yet
- Fall Prevention Therapies For IndividualDocument22 pagesFall Prevention Therapies For Individualfernando_a_gonzalezNo ratings yet
- 651 FullDocument5 pages651 Fullfernando_a_gonzalezNo ratings yet
- The Mobility Scale For Acute Stroke Patients: Concurrent ValidityDocument7 pagesThe Mobility Scale For Acute Stroke Patients: Concurrent Validityfernando_a_gonzalezNo ratings yet
- Nine Hole Peg Test InstructionsDocument3 pagesNine Hole Peg Test InstructionsjermaineNo ratings yet
- OSHA Form 300 SummaryDocument3 pagesOSHA Form 300 SummaryMashur Al JunaibiNo ratings yet
- Diagnostic LabDocument74 pagesDiagnostic LabVishnu Goenka0% (1)
- Digital Healthcare Data - Electronic Medical Records for Improved Patient OutcomesDocument18 pagesDigital Healthcare Data - Electronic Medical Records for Improved Patient Outcomesbpk riNo ratings yet
- Progress of Molecular Targeted Therapies For ProstatecancersDocument13 pagesProgress of Molecular Targeted Therapies For ProstatecancersNenad MladenovicNo ratings yet
- Drug StudyDocument4 pagesDrug Studyshiela marie cortezNo ratings yet
- Dispensing DrugsDocument1 pageDispensing DrugsIan CalalangNo ratings yet
- BJOG - 2024 - Nelson Piercy - The Management of Nausea and Vomiting in Pregnancy and Hyperemesis Gravidarum Green TopDocument30 pagesBJOG - 2024 - Nelson Piercy - The Management of Nausea and Vomiting in Pregnancy and Hyperemesis Gravidarum Green TopNilaaharan RobinsonNo ratings yet
- Dr. Richard Teo Gave Inspiring SpeechDocument6 pagesDr. Richard Teo Gave Inspiring Speechpeli1974No ratings yet
- CardiovascularDocument3 pagesCardiovascularNicomille T. CaligingNo ratings yet
- LinesDocument1 pageLinesEmily PeschongNo ratings yet
- Drug Study - FurosemideDocument2 pagesDrug Study - FurosemideryanNo ratings yet
- Congestive Heart Failure 1 Concept Map !Document1 pageCongestive Heart Failure 1 Concept Map !Franklin A. Salaum IIINo ratings yet
- COVID 19 Prevention Strategies for Healthcare WorkersDocument31 pagesCOVID 19 Prevention Strategies for Healthcare WorkersPuteriNo ratings yet
- Design and Characterization of Bilayer Tablet of Rifampicin and Isoniazid For Tuberculosis TherapyDocument5 pagesDesign and Characterization of Bilayer Tablet of Rifampicin and Isoniazid For Tuberculosis TherapyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Métodos de Reabilitação para Redução Da Subluxação Do Ombro Na Hemiparesia pós-AVC Uma Revisão SistemátDocument15 pagesMétodos de Reabilitação para Redução Da Subluxação Do Ombro Na Hemiparesia pós-AVC Uma Revisão SistemátMatheus AlmeidaNo ratings yet
- Association Between Mir Let-7g Gene Expression and The Risk of Cervical Cancer in Human Papilloma Virus-Infected PatientsDocument8 pagesAssociation Between Mir Let-7g Gene Expression and The Risk of Cervical Cancer in Human Papilloma Virus-Infected PatientsGICELANo ratings yet
- University of Northern PhilippinesDocument7 pagesUniversity of Northern PhilippinesRc Peralta Adora100% (1)
- IB QUESTIONS From PAST PAPERSDocument9 pagesIB QUESTIONS From PAST PAPERSJohn Osborne100% (2)
- Effects of Child Abuse on Mental Health, Behavior, and DevelopmentDocument4 pagesEffects of Child Abuse on Mental Health, Behavior, and Developmentlotusrai100% (2)
- Presentation 1Document13 pagesPresentation 1RatulNo ratings yet
- Test-4 Angina Pectoris Text ADocument11 pagesTest-4 Angina Pectoris Text ANaveen Abraham100% (2)
- Resume Format For Doctors PDFDocument3 pagesResume Format For Doctors PDFANIL PATELNo ratings yet
- Horowitz Taylor A Method of Tapering SSRI Treatment To Mitigate Withdrawal SymptomsDocument17 pagesHorowitz Taylor A Method of Tapering SSRI Treatment To Mitigate Withdrawal SymptomsDonaNo ratings yet
- Pregnancy Heart Disease v28 WebDocument1 pagePregnancy Heart Disease v28 WebMishka LaldaparsadNo ratings yet
- Svengali in Arizona - TIME 10-22-1973Document2 pagesSvengali in Arizona - TIME 10-22-1973tonyleontNo ratings yet
- Emergency Surgery for Ruptured Ectopic PregnancyDocument4 pagesEmergency Surgery for Ruptured Ectopic PregnancySam MataNo ratings yet
- Basic Airway Management in AdultsDocument7 pagesBasic Airway Management in AdultsBereket temesgenNo ratings yet
- Navi Cure - Customer Information Sheet: Product Name What Am I Covered ForDocument12 pagesNavi Cure - Customer Information Sheet: Product Name What Am I Covered ForsandeepfoxNo ratings yet
- Rehabilitasi Pasca CABGDocument23 pagesRehabilitasi Pasca CABGPaulina WowilingNo ratings yet
- WSH Guidelines Statutory Medical Examinations 2013Document210 pagesWSH Guidelines Statutory Medical Examinations 2013OnaFajardoNo ratings yet