Professional Documents
Culture Documents
Physical Examination of Urine
Uploaded by
Jannen Dela CruzOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Physical Examination of Urine
Uploaded by
Jannen Dela CruzCopyright:
Available Formats
PHYSICAL EXAMINATION OF
URINE
📌 reference discussion by miss Rolaine the Great <3 (use school email to access :>):
https://drive.google.com/file/d/1V-cxZbwJm9hycK5QX23dPAGWD6wgvKSx/view
https://drive.google.com/drive/u/0/folders/1a12uhG7PHPuZzGgeVIh5wlIjAEGbPu49
📌 pdf link:
https://drive.google.com/file/d/1Zlyd51V2vwPN1NhrHPqZiLOn9dAOKua0/view?
usp=sharing
physical examination serves as preliminary reporting of the state of our body
what are the 5 parameters of physical/gross/macroscopic examination of urine:
1. color
2. clarity
3. others: specific gravity, volume, odor
what are the 3 portion of parts of urinalysis?
1. physical examination (gross or macroscopic)
2. chemical examination
3. microscopic examination
COLOR
= timestamp: 3:45 =
the concentration of urine should be more correlated to osmolality rather than color
and specific gravity
what is the normal range of color of the urine? Pale to Dark yellow
PHYSICAL EXAMINATION OF URINE 1
also depends on physiologic and metabolic activities (e.g. what we eat, drink;
medications and diseases)
what are the three common pigments that can be seen in urine?
1. urochrome
2. urobilin
3. uroerythrin
Urochrome
this pigment causes yellow color urine specimen. Urochrome
when the kidney filters the plasma, the urochrome is also filtered and becomes part
of the filtrate and therefore excreted as urine which imparts a yellow color
this is also the major pigment of urine
urochrome is produced in what organ of the body? Liver
Urobilin
this pigment causes orange-brown pigment of urine. Urobilin
this is the by-product of the oxidation of the colorless pigment urobilinogen. Urobilin
urine has <4mg/dL or urobilinogen and are colorless
when urine is exposed to room temperature (standing for several minutes) it will be
oxidized by ordinary light (photooxidation) into the pigmented urobilin which
imparts the yellowish or orange-brown color of the urine
Uroerythrin
this pigment causes pink color of the urine specimen. Uroerythrin
it is attached to amorphous urates crystal giving a pink pigment
pink pigment uroerythrin can only be viewed if the specimen is refrigerated
crystals will form when refrigerated depending upon the pH of the urine:
After refrigeration (pH) Crystal formed
acidic amorphous urates (pink)
alkaline/basic amorphous phosphates (white)
PHYSICAL EXAMINATION OF URINE 2
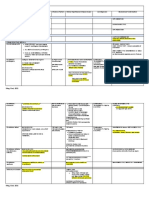
COLOR VARIATIONS
= timestamp: 10:23 =
list the variation of color of the urine:
light yellow
yellow
amber
brown
red
1. Dark yellow/Amber/Orange
dark yellow/amber/orange is caused by:
bilirubin
the heme ring is cleaved by the enzyme microsomal heme oxygenase to form
biliverdin (verde = “green”), which is then converted to the tetrapyrrole pigment
bilirubin by the cytosolic enzyme biliverdin reductase
reduced product of biliverdin
should not be exposed to light (coz light sensitive) and will decrease its value
polar to nonpolar bilirubin and inactive it then excreted into the bile, bacteria in
the large intestine reduces bilirubin into pigments which is excreted (urobilin
in urine, and stercobilinin feces)
other way to confirm the presence of bilirubin in urine is to perform “foam” or
“shake” test
shake the urine specimen inside the container if yellow large bubbles are
present then it is positive for bilirubin
confirmatory test: chemical examination (+), bilirubin crystals (+)
urobilin
biliverdin
this is the oxidized counterpart of the bilirubin
if yellow-green urine is present, it is (+) for biliverdin
PHYSICAL EXAMINATION OF URINE 3
phenazopyridine (pyridium) or azo-gantrisin (drug)
drug use for patients with UTI and are renal analgesic
others are: carotene, warfarin (coumadin), riboflavin, nitrofurantoin
2. Red/Pink/Brown
= timestamp: 21:35 =
the most common abnormal color of urine is. Red
red/pink/brown color of the urine is caused by:
intact RBCs
presence of this is termed as “hematuria” (hema=blood, uria=urine)
if urine is dark red and smoky, (+) hematuria
hemoglobin
presence of this is termed as “hemoglobinuria”
if urine is clear red can be both (+) for hemoglobinuria & myoglobinuria
if the plasma in the clear red urine is red then it is (+) for hemoglobinuria
myoglobin
very small protein and low molecular weight, and are easily excreted as urine
compare to hemoglobin
presence of this pigment is termed as “myoglobinuria”
if the plasma in the clear red urine is clear then it is (+) for myoglobinuria
others include:
porphyrins
if the patients have porphyria
port-wine color urine maybe observe
menstruation, beets, rifampin, phenolphthalein, phenosulphthalein,
phenindione, phenothiazines, senna, blackberries
3. Brown to Black
= timestamp: 27:50 =
PHYSICAL EXAMINATION OF URINE 4
brown to black color of the urine is caused by:
homogentisic acid
by product of tyrosine metabolism
melanin
others: levodopa, methyldopa, metronidazole, phenol derivatives
4. Blue to Green
= timestamp: 29:34 =
blue to green color of the urine is caused by bacterial infections and:
pseudomonas (proteus)
indicans
others: clorets, azure A, methocarbamol, methylene blue, amitriptyline,
catheterized patients
CLARITY
= timestamp: 31:26 =
it refers to the transparency or turbidity of the urine. Clarity
may be caused by pathologic states and nonpathological states
a normal freshly voided mid-stream clean catch urine specimen should be? Clear
it provides key to the microscopic examination results. Clarity
Reporting of Urine Clarity
= timestamp: 34:57 =
Clarity Term
no visible particulates,
Clear
transparent
few particulates, print easily
Hazy
seen through urine
many particulates, print
Cloudy
blurred through urine
PHYSICAL EXAMINATION OF URINE 5
Clarity Term
print cannot be seen
Turbid
through urine
may precipitate or be
Milky
clotted
To view color and clarity:
1. use a well mixed urine specimen
book: via swirling, miss: inversion (homogenously)
2. view through a clear container
e.g. test tube
3. view against a white background
newsprint can also be use
4. maintain adequate room lighting
should be place under a good light source NOT against
Non-Pathologic VS Pathologic Causes of Turbidity
Non-pathologic Pathologic
1. squamous epithelial cells
1. RBCs
(SECs)
2. mucus 2. WBCs
3. amorphous phosphates,
3. bacteria
carbonates, urates
4. semen, spermatozoa 4. yeast
5. non-squamous epithelial cells
5. fecal contamination
(NSECs)
6. radiographic contrast media 6. abnormal crystals
7. talcum powder 7. lymph fluids
8. vaginal creams 8. lipids
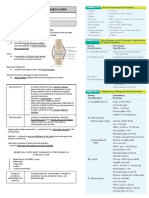
SPECIFIC GRAVITY
PHYSICAL EXAMINATION OF URINE 6
= timestamp: 41:29 =
it refers to the density of the solutions compared to the density of the distilled H2O
(1.00) at a similar temperature. Specific Gravity
what is the normal value of SG in the urine? 1.002-1.035 (with 24hr urine SG of 1.015-
1.025)
specific gravity provides key to urine _____. Concentration
but osmolality provides more key to urine concentration because SG is affected by
the number and size of the solution but ang osmolality is the number lang
SPECIFIC GRAVITY VARIATIONS
what are the specific gravity variations? Variations Specific Gravity
1. isosthenuria Isothenuria 1.010
2. hyposthenuria Hyposthenuria <1.010
Hypersthenuria >1.010
3. hypersthenuria
no problem if less than or greater than isosthenuria ang value of SG as long as the
analyte that contribute are not the abnormal analyte (e.g., protein, glucose, RBCs)
SPECIFIC GRAVITY METHODS
= timestamp:
Direct Indirect
1. Urinometer 1. Refractometry
2. Harmonic Oscillation
2. Reagent strip
Densitometry
the principles of direct methods in SG is based on. Density
the principles of refractometry method in SG is based on. Refractive index
the principles of reagent strips method in SG is based on. Polyelectrolyte change
Urinomety/Hydrometry
what are the disadvantage of urinometer?
PHYSICAL EXAMINATION OF URINE 7
less accurate
uses large volume of urine (10-15mL)
temperature sensitive
sensitive to the presence of protein and glucose
other characteristics:
should be calibrated (20 deg. Celsius using distilled H20 with a SG of 1.00)
temperature, protein, and glucose correction must be performed
Refractrometry
= timestamp: 9:15 =
it uses refractive index. Refractometer
what are some advantages of refractometer?
uses small volume of urine (1-2gtts or drops)
not temperature sensitive (means NO need for temperature correction)
other characteristics:
should be calibrated (15-38 deg. Celsius using distilled H20 with a SG of 1.00)
calibrators used with normal value/result:
distilled H2O
3% NaC (1.015)
5% NaCl (1.022 +/-0.001)
9% Sucrose (1.034 +/-0.001)
PHYSICAL EXAMINATION OF URINE 8
TEMPERATURE & SOLUTE CORRECTIONS
(SG)
= timestamp: 11:45 =
PHYSICAL EXAMINATION OF URINE 9
EXAMPLES:
A. TEMPERATURE
A.1
if u take out urine sample from the ref nya 17 deg. Celsius (which is BELOW 20 deg.
Celsius) iyang temperature and your reading was 1.020, then your final SG will be 1.019
(1.020-0.001=1.019) after temperature correction
for every 3 deg. centigrade BELOW 20 deg. centigrade diha raka mag substract
og 0.001 (18-19 deg. centigrade is not included daw)
A.2
if u take out urine sample from the ref nya 23 deg. Celsius (which is ABOVE 20 deg.
Celsius) iyang temperature and your reading was 1.020, then your final SG will be 1.021
(1.020+0.001=1.021) after temperature correction
for every 3 deg. centigrade ABOVE 20 deg. centigrade diha raka mag add og 0.001
(21-22 deg. centigrade is not included daw)
GLUCOSE & PROTEIN
if the urine specimen has has the presence of both 1g/dL of glucose and protein then
you subtract it with 0.007 (0.004 from glucose + 0.003 from protein=0.007)
VOLUME
= timestamp: 18:37 =
this provides key to the body’s state of hydration. Volume
but it’s not routinely performed during microscopic examination
what is the normal volume of the urine?
24-hr urine: 600-2000mL
night urine: <400mL
Volume Variations
what is the urine volume when you experience oliguria. <400mL/day
PHYSICAL EXAMINATION OF URINE 10
what is the urine volume when you have diabetes mellitus and insipidus or you
experience polyuria. >2,500mL/day
what is the urine volume when you experience anuria. <100mL/day for 2-3
consecutive days
what is the urine volume when you experience nocturia. >500mL@night (SG: <1.018)
Table 1.0 : Summary of Volume Variations
Variations Volume
Oliguria <400mL/day
Polyuria >2,500mL/day
Anuria <100mL/day for 2-3 days
Nocturia >500mL@night (SG: <1.018)
Urine Volume (DM vs. DI)
= timestamp: 20:49 =
these diseases are usually associated with increased volume of urine or polyuria.
diabetes insipidus
diabetes mellitus
Diabetes Insipidus
what is the main problem in diabetes insipidus? ADH is either absent or released in
decreased amount
maybe caused by tumors in brain especially compressing the pituitary gland
(remember that ADH is produced by pituitary gland)
water retention is dysfunctional
specific gravity is low compare to diabetes melllitus
what are the signs and symptoms of diabetes insipidus?
excessive urination (polyuria)
excessive thirst
elevated serum sodium
PHYSICAL EXAMINATION OF URINE 11
increased dehydration
Diabetes Mellitus
what is the main problem in diabetes mellitus? Insulin
such as when your pancreas is not producing insulin or are resistant to insulin
production (e.g. obese) which causes increased glucose value (which is highly
osmotic) and are prone to dehydration
specific gravity is high compare to diabetes insipidus due to the presence of
glucose
what are the signs and symptoms of diabetes mellitus?
excessive urination (polyuria)
excessive thirst
weight loss and fatigue
elevated blood glucose
ODOR
= timestamp: 25:13 =
not routinely performed same as specific gravity and volume. Odor
what is the normal odor of a fresh urine? faintly Aromatic
what is the normal odor of an old urine? Ammoniacal
what are some factors that contribute to the urine odor? Food & Metabolic disorders
Odor Variations
PHYSICAL EXAMINATION OF URINE 12
PHYSICAL EXAMINATION OF URINE 13
You might also like
- Liver Function TestDocument9 pagesLiver Function TestFarah Krisna Sadavao AndangNo ratings yet
- Staphylococcus Streptococcus: Propertie S Morpholo Gy Culture & Biochemi Cal ReactionsDocument3 pagesStaphylococcus Streptococcus: Propertie S Morpholo Gy Culture & Biochemi Cal ReactionsmadhuNo ratings yet
- Chapter 22Document13 pagesChapter 22Ivy Jan OcateNo ratings yet
- Streak Plate Method - Principle, Types, Methods, UsesDocument20 pagesStreak Plate Method - Principle, Types, Methods, UsesHerda CahyaningrumNo ratings yet
- Laboratory 9 Digestive SystemDocument8 pagesLaboratory 9 Digestive SystemClyde Alec (Clydealec)No ratings yet
- MLS 422 Diagnostic MicrobiologyDocument50 pagesMLS 422 Diagnostic MicrobiologyMayowa OgunmolaNo ratings yet
- AUBF Synovial FluidDocument6 pagesAUBF Synovial FluidRichelyn Grace B. VenusNo ratings yet
- Renal Function and The Significance of Non-Protein Nitrogen CompoundsDocument12 pagesRenal Function and The Significance of Non-Protein Nitrogen CompoundsSrujana BudheNo ratings yet
- Anaerobes: Gram Positive CocciDocument4 pagesAnaerobes: Gram Positive CocciCindy Mae Flores UtlegNo ratings yet
- Enterobacteriaceace Part 1Document48 pagesEnterobacteriaceace Part 1Krenz CatiboNo ratings yet
- Virus PDFDocument60 pagesVirus PDFrenz bartolomeNo ratings yet
- Chapter 8 Biochemical Tests in MicrobiologyDocument33 pagesChapter 8 Biochemical Tests in Microbiologyits james de guzmanNo ratings yet
- HEMA-1 Up To PG 30.-1-31Document31 pagesHEMA-1 Up To PG 30.-1-31Angela ReyesNo ratings yet
- 5 - Microscopic Examination of UrineDocument19 pages5 - Microscopic Examination of UrineKunware TropaNo ratings yet
- Micro para by Kiara (Nov 29)Document7 pagesMicro para by Kiara (Nov 29)PojangNo ratings yet
- Carbohydrates Trace Elements VitaminsDocument31 pagesCarbohydrates Trace Elements VitaminsSophia Gail ChingNo ratings yet
- Enterobacteriaceae: Click To Edit Master Subtitle StyleDocument49 pagesEnterobacteriaceae: Click To Edit Master Subtitle StyleAljon AniesNo ratings yet
- ArsenicDocument15 pagesArsenicIsabela PavălNo ratings yet
- (Compre - 3itransteam) Mt6320 - Bacte Lec Unit 1.1-11Document244 pages(Compre - 3itransteam) Mt6320 - Bacte Lec Unit 1.1-11Ylia MastarsNo ratings yet
- Aubf - Chapter 4Document6 pagesAubf - Chapter 4Kristin SoquilloNo ratings yet
- Aubf ReviewerDocument30 pagesAubf ReviewerPoly EstherNo ratings yet
- HEMA 1 LAB - WatermarkDocument133 pagesHEMA 1 LAB - WatermarkDavid WolfyNo ratings yet
- Parasitology Notes: Phasmids: Species Infective Stage Diagnostic Stage Pathology/Notes Diagnosis TreatmentDocument4 pagesParasitology Notes: Phasmids: Species Infective Stage Diagnostic Stage Pathology/Notes Diagnosis TreatmentOrhan AsdfghjklNo ratings yet
- Lesson 1: Pre-Analytical Factors and Gross Description: Histopathologic and Cytologic Techniques - LectureDocument28 pagesLesson 1: Pre-Analytical Factors and Gross Description: Histopathologic and Cytologic Techniques - Lecturechristian Jay HorseradaNo ratings yet
- 1 SEMR421 Bacteriology Part 1Document10 pages1 SEMR421 Bacteriology Part 1Micah Daniel TapiaNo ratings yet
- HEMATOLOGYDocument28 pagesHEMATOLOGYRyan PedregosaNo ratings yet
- 1 Hemoglobinopathies BookDocument26 pages1 Hemoglobinopathies BookRhoda Lom-ocNo ratings yet
- Strasinger AUBFDocument44 pagesStrasinger AUBFangela tanteoNo ratings yet
- Family EnterobacteriaceaeDocument19 pagesFamily EnterobacteriaceaeJisanieNo ratings yet
- Bacteriology HandoutDocument30 pagesBacteriology HandoutMoonyeen Jann Casera BalicNo ratings yet
- Recombinant Protein Production EbookDocument27 pagesRecombinant Protein Production Ebookeva nursyifaNo ratings yet
- Compre MolbioDocument93 pagesCompre MolbioDeniebev'z OrillosNo ratings yet
- Fixation ImpregnationDocument18 pagesFixation ImpregnationKarla Mae Tolelis - BurlatNo ratings yet
- Introductory Mycology: Laboratory Manual ForDocument206 pagesIntroductory Mycology: Laboratory Manual ForSekste MaludaNo ratings yet
- Buffer Solution - Acidic and Basic Buffers, Preparations, Examples PDFDocument5 pagesBuffer Solution - Acidic and Basic Buffers, Preparations, Examples PDFSakshi DevalekarNo ratings yet
- Vibrio, Campylobacter, and HelicobacterDocument7 pagesVibrio, Campylobacter, and HelicobacterRach ReyesNo ratings yet
- Cb1 - Specimen Handling, Transport and ProcessingDocument7 pagesCb1 - Specimen Handling, Transport and ProcessingAngelic AngelesNo ratings yet
- HematologyDocument37 pagesHematologykurt Allen MacarilayNo ratings yet
- CM All Compiled NotesDocument100 pagesCM All Compiled NotesKatrina Mae PatalinghugNo ratings yet
- Current Concepts of Enzyme Histochemistry in Modern PathologyDocument11 pagesCurrent Concepts of Enzyme Histochemistry in Modern PathologyRosa AquinoNo ratings yet
- Clinical Chemistry 2: Shift Unit 2: EnzymologyDocument54 pagesClinical Chemistry 2: Shift Unit 2: EnzymologyDericNo ratings yet
- Clinical MicrosDocument30 pagesClinical MicrosRyan PedregosaNo ratings yet
- A Study On Serum Sodium and Potassium in Newly Diagnosed Primary HypertensionDocument6 pagesA Study On Serum Sodium and Potassium in Newly Diagnosed Primary HypertensionIJAR JOURNALNo ratings yet
- Lab Tech Ques Set 1Document7 pagesLab Tech Ques Set 1Radha ThangamNo ratings yet
- Clinical Microscopy ExamsDocument36 pagesClinical Microscopy ExamsVanessa May BlancioNo ratings yet
- Blood and Blood ComponentsDocument51 pagesBlood and Blood ComponentsJeevitha VanithaNo ratings yet
- Biological Safety ManualDocument193 pagesBiological Safety ManualJoshua WelchNo ratings yet
- International Journal of PharmaceuticsDocument6 pagesInternational Journal of PharmaceuticsSjis11362No ratings yet
- To In-Vitro Antispasmodic Activity of Aqueous Leaves Extract of Coriandrum Sativum (C. Sativum) Linn. On Chicken IleumDocument5 pagesTo In-Vitro Antispasmodic Activity of Aqueous Leaves Extract of Coriandrum Sativum (C. Sativum) Linn. On Chicken IleumInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Neisse RiaDocument49 pagesNeisse RiaSubhada GosaviNo ratings yet
- List of Funding AgenciesDocument1 pageList of Funding AgenciesShamia Sathish100% (1)
- Aubf Lec Reviewer MidtermDocument129 pagesAubf Lec Reviewer MidtermTrangia, SharmaineNo ratings yet
- Lesson 10Document66 pagesLesson 10Angel joyce ValenciaNo ratings yet
- MYCODocument59 pagesMYCOAngela ReyesNo ratings yet
- Enterobacteriaceae Rev 2013Document46 pagesEnterobacteriaceae Rev 2013MOCHILNo ratings yet
- Flora of Jizan Region: Final ReportDocument545 pagesFlora of Jizan Region: Final ReportDoctorQariNo ratings yet
- cc1 LecDocument18 pagescc1 LecRayvince LopezNo ratings yet
- Parasitology SAQs With AnswersDocument14 pagesParasitology SAQs With AnswersGeorge Makori100% (1)
- Analysis of Urine and Other Body FluidsDocument9 pagesAnalysis of Urine and Other Body FluidsPajarillaga Franz Erick QuintoNo ratings yet
- Physical Examination of Urine SummaryDocument3 pagesPhysical Examination of Urine SummaryBiancake Sta. AnaNo ratings yet
- Kelas ChondrichtyesDocument15 pagesKelas ChondrichtyesanitagustinawatiNo ratings yet
- Ecological Quality RatioDocument24 pagesEcological Quality RatiofoocheehungNo ratings yet
- Azure Machine Learning StudioDocument17 pagesAzure Machine Learning StudioNurain IsmailNo ratings yet
- Test7 PointersDocument16 pagesTest7 PointersPratibha DwivediNo ratings yet
- Asaali - Project Estimation - Ce155p-2 - A73Document7 pagesAsaali - Project Estimation - Ce155p-2 - A73Kandhalvi AsaaliNo ratings yet
- Solar Charge Controller: Solar Car Solar Home Solar Backpack Solar Boat Solar Street Light Solar Power GeneratorDocument4 pagesSolar Charge Controller: Solar Car Solar Home Solar Backpack Solar Boat Solar Street Light Solar Power Generatorluis fernandoNo ratings yet
- Petersen Coils Basic 20principle and ApplicationDocument3 pagesPetersen Coils Basic 20principle and ApplicationasotozuazuaNo ratings yet
- Carinthia Katalog DownloadDocument16 pagesCarinthia Katalog DownloadOperator_010100% (2)
- Karl MarxDocument4 pagesKarl Marxeirvine noah isidroNo ratings yet
- RD Sharma Class8 SolutionsDocument2 pagesRD Sharma Class8 Solutionsncertsoluitons100% (2)
- ContempoDocument4 pagesContempoPrincess Jonette YumulNo ratings yet
- Optical Scattering of Gold NanosphereDocument24 pagesOptical Scattering of Gold NanosphereParas KumarNo ratings yet
- Asme b16-25Document22 pagesAsme b16-25JamesNo ratings yet
- Us Navy To Evaluate Anti Submarine Warfare Training SystemDocument2 pagesUs Navy To Evaluate Anti Submarine Warfare Training SystemVictor PileggiNo ratings yet
- 08 - 2061 USTR 2222a (1) Supor EKVDocument24 pages08 - 2061 USTR 2222a (1) Supor EKVHassan Houdoud0% (1)
- Stopping by Woods On A Snowy EveningDocument9 pagesStopping by Woods On A Snowy EveningJulia Garces100% (2)
- Addtional List Dissertation 040117Document6 pagesAddtional List Dissertation 040117Sagar Kansara100% (2)
- Ecall Vs NG EcallDocument6 pagesEcall Vs NG EcallTrần Văn DũngNo ratings yet
- Manual of Sensorless Brushless Motor Speed Controller: Pentium SeriesDocument4 pagesManual of Sensorless Brushless Motor Speed Controller: Pentium Seriesfosavo5839No ratings yet
- The 10 Most Famousfilipino Artists and Their MasterworksDocument3 pagesThe 10 Most Famousfilipino Artists and Their MasterworksGina MagtibayNo ratings yet
- Chapter 7: Protein Function Part I: Myoglobin and HemoglobinDocument27 pagesChapter 7: Protein Function Part I: Myoglobin and HemoglobineliNo ratings yet
- Dairy Products Theory XIIDocument152 pagesDairy Products Theory XIIDskNo ratings yet
- Asteroids Prospective EnergyDocument710 pagesAsteroids Prospective EnergySlavica Otovic100% (1)
- Earth Science Essential Learning Competencies 2020Document5 pagesEarth Science Essential Learning Competencies 2020Charry CervantesNo ratings yet
- Minimalist KWL Graphic OrganizerDocument2 pagesMinimalist KWL Graphic OrganizerIrish Nicole AlanoNo ratings yet
- Crma Unit 1 Crma RolesDocument34 pagesCrma Unit 1 Crma Rolesumop3plsdn0% (1)
- 1F-Korean-Nami Mun - Miles From NowhereDocument4 pages1F-Korean-Nami Mun - Miles From NowhereNeil PatelNo ratings yet
- Manual GA 55 VSD Atlas CompresorDocument114 pagesManual GA 55 VSD Atlas Compresormondaxa_mme50% (4)
- The Spirit Controlled Life Ebook PDF 1Document184 pagesThe Spirit Controlled Life Ebook PDF 1Okesola AbayomiNo ratings yet
- Child DevelopmentDocument15 pagesChild Development4AndreeaNo ratings yet
- Organic Chemistry for Schools: Advanced Level and Senior High SchoolFrom EverandOrganic Chemistry for Schools: Advanced Level and Senior High SchoolNo ratings yet
- Periodic Tales: A Cultural History of the Elements, from Arsenic to ZincFrom EverandPeriodic Tales: A Cultural History of the Elements, from Arsenic to ZincRating: 3.5 out of 5 stars3.5/5 (137)
- The Disappearing Spoon: And Other True Tales of Madness, Love, and the History of the World from the Periodic Table of the ElementsFrom EverandThe Disappearing Spoon: And Other True Tales of Madness, Love, and the History of the World from the Periodic Table of the ElementsRating: 4 out of 5 stars4/5 (146)
- Is That a Fact?: Frauds, Quacks, and the Real Science of Everyday LifeFrom EverandIs That a Fact?: Frauds, Quacks, and the Real Science of Everyday LifeRating: 5 out of 5 stars5/5 (4)
- Monkeys, Myths, and Molecules: Separating Fact from Fiction, and the Science of Everyday LifeFrom EverandMonkeys, Myths, and Molecules: Separating Fact from Fiction, and the Science of Everyday LifeRating: 4 out of 5 stars4/5 (1)
- The Regenerative Grower's Guide to Garden Amendments: Using Locally Sourced Materials to Make Mineral and Biological Extracts and FermentsFrom EverandThe Regenerative Grower's Guide to Garden Amendments: Using Locally Sourced Materials to Make Mineral and Biological Extracts and FermentsRating: 5 out of 5 stars5/5 (3)
- The Elements We Live By: How Iron Helps Us Breathe, Potassium Lets Us See, and Other Surprising Superpowers of the Periodic TableFrom EverandThe Elements We Live By: How Iron Helps Us Breathe, Potassium Lets Us See, and Other Surprising Superpowers of the Periodic TableRating: 3.5 out of 5 stars3.5/5 (22)
- The Periodic Table: A Very Short IntroductionFrom EverandThe Periodic Table: A Very Short IntroductionRating: 4.5 out of 5 stars4.5/5 (3)
- The Nature of Drugs Vol. 1: History, Pharmacology, and Social ImpactFrom EverandThe Nature of Drugs Vol. 1: History, Pharmacology, and Social ImpactRating: 5 out of 5 stars5/5 (5)
- Chemistry for Breakfast: The Amazing Science of Everyday LifeFrom EverandChemistry for Breakfast: The Amazing Science of Everyday LifeRating: 4.5 out of 5 stars4.5/5 (90)
- Handbook of Formulating Dermal Applications: A Definitive Practical GuideFrom EverandHandbook of Formulating Dermal Applications: A Definitive Practical GuideNo ratings yet
- A Perfect Red: Empire, Espionage, and the Quest for the Color of DesireFrom EverandA Perfect Red: Empire, Espionage, and the Quest for the Color of DesireRating: 4 out of 5 stars4/5 (129)
- Water-Based Paint Formulations, Vol. 3From EverandWater-Based Paint Formulations, Vol. 3Rating: 4.5 out of 5 stars4.5/5 (6)
- Essential Oil Chemistry Formulating Essential Oil Blends that Heal - Aldehyde - Ketone - Lactone: Healing with Essential OilFrom EverandEssential Oil Chemistry Formulating Essential Oil Blends that Heal - Aldehyde - Ketone - Lactone: Healing with Essential OilRating: 5 out of 5 stars5/5 (1)
- Bioplastics: A Home Inventors HandbookFrom EverandBioplastics: A Home Inventors HandbookRating: 4 out of 5 stars4/5 (2)
- Chemistry: a QuickStudy Laminated Reference GuideFrom EverandChemistry: a QuickStudy Laminated Reference GuideRating: 5 out of 5 stars5/5 (1)
- Formulating, Packaging, and Marketing of Natural Cosmetic ProductsFrom EverandFormulating, Packaging, and Marketing of Natural Cosmetic ProductsNo ratings yet
- Guidelines for Integrating Process Safety into Engineering ProjectsFrom EverandGuidelines for Integrating Process Safety into Engineering ProjectsNo ratings yet
- The Periodic Table of Elements - Alkali Metals, Alkaline Earth Metals and Transition Metals | Children's Chemistry BookFrom EverandThe Periodic Table of Elements - Alkali Metals, Alkaline Earth Metals and Transition Metals | Children's Chemistry BookNo ratings yet
- The Periodic Table of Elements - Post-Transition Metals, Metalloids and Nonmetals | Children's Chemistry BookFrom EverandThe Periodic Table of Elements - Post-Transition Metals, Metalloids and Nonmetals | Children's Chemistry BookNo ratings yet