Professional Documents
Culture Documents
Análisis Con Tira Reactiva de La Química de La Orina, Beneficios y Limitaciones de Los Ensayos Basados en Química Seca
Uploaded by
Antony Barzola GaldosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Análisis Con Tira Reactiva de La Química de La Orina, Beneficios y Limitaciones de Los Ensayos Basados en Química Seca
Uploaded by
Antony Barzola GaldosCopyright:
Available Formats
Postgraduate Medicine
ISSN: 0032-5481 (Print) 1941-9260 (Online) Journal homepage: https://www.tandfonline.com/loi/ipgm20
Dipstick analysis of urine chemistry: benefits and
limitations of dry chemistry-based assays
Varun Kavuru, Tommy Vu, Lampros Karageorge, Devasmita Choudhury,
Ryan Senger & John Robertson
To cite this article: Varun Kavuru, Tommy Vu, Lampros Karageorge, Devasmita Choudhury, Ryan
Senger & John Robertson (2019): Dipstick analysis of urine chemistry: benefits and limitations of
dry chemistry-based assays, Postgraduate Medicine, DOI: 10.1080/00325481.2019.1679540
To link to this article: https://doi.org/10.1080/00325481.2019.1679540
Accepted author version posted online: 14
Oct 2019.
Submit your article to this journal
View related articles
View Crossmark data
Full Terms & Conditions of access and use can be found at
https://www.tandfonline.com/action/journalInformation?journalCode=ipgm20
Publisher: Taylor & Francis & Informa UK Limited, trading as Taylor & Francis Group
Journal: Postgraduate Medicine
DOI: 10.1080/00325481.2019.1679540
Dipstick analysis of urine chemistry: benefits and limitations of dry chemistry-based assays
Varun Kavuru1, Tommy Vu2, Lampros Karageorge3, Devasmita Choudhury3, Ryan Senger2,
t
ip
John Robertson 3, 4 *
1
Virginia Tech Carilion School of Medicine, Roanoke, VA 24014
cr
2
Biological Systems Engineering, College of Engineering, Virginia Tech, Blacksburg, VA
us
24061
3
Salem Veterans Affairs Medical Center, Salem, VA 24153
an
4
Biomedical Engineering and Mechanics, College of Engineering, Virginia Tech, Blacksburg,
VA 24061
M
* Corresponding Author
Abstract
ed
Urinalysis is a commonly utilized laboratory test and analysis of urine has been studied and used
since ancient times. Urine contains a wide array of metabolites that can provide information
pt
regarding the current physiologic state of the body and clinical manifestations of disease. In this
ce
review, we discuss the mechanics of the dry chemistry component of the urine dipstick such as
the reaction principles underlying various assays and potential effects of collection and storage
Ac
on results. Additionally, we discuss the benefits and limitations of the urine dipstick as it pertains
to its use as a low cost tool in point-of-care settings and the reasoning for a lack of its use as a
broad screening tool.
Keywords: urinalysis, dipstick, dry chemistry, urine, assay principles
Disclosures: No potential conflict of interest reported by the authors.
Information Classification: General
Corresponding Author: Dr. John L. Robertson, 147 Kelly Hall, Virginia Tech, 325 Stanger St.,
Blacksburg, VA, 24061 E-mail: drbob@vt.edu Phone: 540-239-0169
Dipstick analysis of urine chemistry: benefits and limitations of dry chemistry-based assays
t
Varun Kavuru1, Tommy Vu2, Lampros Karageorge3, Devasmita Choudhury3, Ryan Senger2,
ip
John Robertson 3, 4
cr
1
Virginia Tech Carilion School of Medicine, Roanoke, VA 24014
2
Biological Systems Engineering, College of Engineering, Virginia Tech, Blacksburg, VA
us
24061 an
3
Salem Veterans Affairs Medical Center, Salem, VA 24153
4
Biomedical Engineering and Mechanics, College of Engineering, Virginia Tech, Blacksburg,
M
VA 24061
ed
Corresponding Author
Corresponding Author: Dr. John L. Robertson, 147 Kelly Hall, Virginia Tech, 325 Stanger St.,
pt
Blacksburg, VA, 24061 E-mail: drbob@vt.edu
ce
Ac
Information Classification: General
Abstract
Urinalysis is a commonly utilized laboratory test and analysis of urine has been studied and used
since ancient times. Urine contains a wide array of metabolites that can provide information
t
ip
regarding the current physiologic state of the body and clinical manifestations of disease. In this
review, we discuss the mechanics of the dry chemistry component of the urine dipstick such as
cr
the reaction principles underlying various assays and potential effects of collection and storage
us
on results. Additionally, we discuss the benefits and limitations of the urine dipstick as it pertains
to its use as a low cost tool in point-of-care settings and the reasoning for a lack of its use as a
an
broad screening tool.
Keywords: urinalysis, dipstick, dry chemistry, urine, assay principles
M
Introduction
ed
Urine is a biologically-active fluid that uniquely reflects a multitude of complex physiologic
activities of the kidneys, specifically, and the body, in general. Details of urine formation in
pt
health and disease are widely described in many physiology texts [1,2], and hundreds of review
ce
papers (not referenced here). Evaluation of urine composition is important because urine
formation reflects metabolism in health and disease. In this sense, urine can act as a monitor of
Ac
some aspects of the urinary tract.
The analysis of urine physical properties, chemical constituents, and suspended particulates
(cells, crystals, biological debris) has been an important medical diagnostic procedure for
thousands of years [3, 4]. Simple, inexpensive testing (visual observation of color and turbidity,
Information Classification: General
odor detection, refractometry for determination of specific gravity, dipstick analysis of
common/diagnostically important chemical constituents) can and is often done by physicians and
trained healthcare professionals in point-of-care (POC) settings (offices, hospitals). Microscopic
analysis of suspended particulates (“urine sediment”) is best done by those trained in urine
sediment analysis and typically occurs in the clinical laboratories. The evaluation of urine
t
ip
sediments is not discussed in this review.
cr
Results of visual characterization and dipstick testing (in samples that have been properly
us
collected [see below]) can be very helpful in triggering more rigorous patient evaluation. For
example, gross turbidity invariably indicates a need for sample centrifugation and sediment
an
evaluation. Intense, yellow-orange color and high urine specific gravity may be indicative of
dehydration, the presence of chromogenic drug metabolites (rifampin [Rifadin®],
M
phenazopyridine [Pyridium®], sulfasalazine [Azulfidine®], isoniazid [Nydrazid®]), vitamin and
dietary plant metabolites, and a number of other normal and abnormal states of health and
ed
disease.
pt
Therefore, an understanding of the value and limitations of dipstick evaluations of urine
ce
chemistry becomes important for timely patient care, in initiating further sensitive diagnostic
evaluation, and assessing the value of such tests for ‘routine screening’ to detect incipient
Ac
disease. The mechanics, value, and limitations of urine dipstick testing are the subjects of this
review.
Body
1. Urine sample collection, handling, storage
Information Classification: General
The quality of information derived from urinalysis is highly dependent on proper collection,
handling, and storage prior to analysis [5,6,7]. Urine is sterile when formed by healthy kidneys.
However contamination of urine occurs by microorganisms that inhabit the urinary tract and
external genitalia. Methods of urine collection include midstream clean-catch void,
catheterization of the bladder, and cystocentesis (suprapubic aspiration). Each method varies in
t
ip
degree of invasiveness and ease of collection. Midstream clean-catch void is the most common
method of urine collection [8]. While intended to minimize contamination without being
cr
invasive, some data suggests that midstream clean-catch samples do not necessarily decrease
us
contamination rates when compared with free catch (no cleaning, no midstream) in patients with
evidence of urinary tract disease [9]. A substantive body of literature however, suggests that
an
improvements in contamination rates are associated with specific portions of the midstream
clean-catch procedure such as spreading the labia or cleaning the perineum, and that this
M
improvement may be more pronounced in male patients performing midstream catch as opposed
to free catch [7]. Additionally, this apparent lack of improvement in contamination rates across
ed
some groups may be due to a lack of proper education and explanation to patients as to properly
perform the midstream clean-catch technique [10].
pt
ce
For purposes of chemical (dipstick) analysis, if uncontaminated urine samples are analyzed
within 1-4 hours, preservatives are usually not necessary. Virtually all clean -catch urine
Ac
specimens that are not preserved either chemically or with a range of cold temperatures will have
contaminant bacterial growth within 12-24 hours, rendering them unsuitable for dipstick or other
urinalysis [11,12]; however, the addition of some preservatives may affect chemical assays
Information Classification: General
(elaborated below) [13]. In more rare cases where urine cannot be analyzed immediately or for
the purposes of clinical research, it may be necessary to store samples for longer than 24 hours.
Urine specimens kept at room temperature for greater than 4 hours show significant growth of
contaminating microorganisms [7]. Storing urine at cooler temperatures such as 4°C, -20°C, or -
t
ip
80°C can prevent degradation of the samples. Ideal temperature may vary depending upon the
cr
desired measurement. For example, osmolality of urine samples has been shown to be stable at
room temperature and 4°C for 4 and 5 days respectively but for >14 days at -20°C [14]. Even
us
cooler temperatures as low as -40°C and -80°C have been shown to be effective for preserving
albumin-to-creatinine ratios in urines samples for as long as up to 6 months both with and
an
without preservatives added [15]. Varying storage temperatures of urine samples affects urine
M
metabolomic profiles which can be seen with results on mass spectroscopy. Investigators note
variable decreases in the concentrations of branched chained amino acids (valine, leucine, for
ed
example)) and other metabolites (hexose H1, for example) attributable to the activity of enzyme
complexes over a variety of temperature settings (-80°C, -40°C, 4°C, 20°C) and multiple time
pt
points (0, 2, 8, 24 hours). This group recommended that urine be transported at temperatures at
least as low as -20°C to ensure integrity of samples and to prevent excessive cycles of freezing
ce
and thawing, which was also shown to affect the metabolomic profile [16].
Ac
Specimens not appropriately preserved can have particles lyse due to low osmolality, low
specific gravity, and higher pH. A variety of preservatives are used depending upon need. Boric
acid affects various reactions on a test strip and can also inhibit the growth of some bacteria. In
some cases, bacterial overgrowth may be undesirable and thus sodium azide may be used as for
Information Classification: General
prevention of this. Formaldehyde use lowers specimen pH and provides false positive results for
leukocyte esterase, peroxidase reaction, and the presence of urobilinogen. Mercury salts, on the
other hand, lead to false negative results for leukocyte esterase [5]. Chlorhexidine solutions can
be advantageous when urine is transported between healthcare services, but samples are best kept
at room temperature as decreased WBC counts and calcium oxalate can be found in samples kept
t
ip
on ice [17]. In summary, each preservative has specific situational uses but also comes with
particular disadvantages.
cr
2. Overview of dipstick analysis of urine chemical composition and assay principles
us
In practice, dipstick/dry chemistry analysis involves spotting urine onto different portions of a
dipstick, allowing a timed reaction to take place, and then comparing an associated color change
an
on the dipstick to a reference standard to determine a positive or negative result. The color
change is typically triggered by reaction of a chromogenic compound with another reaction
M
product produced by interaction of the sample and dipstick reagent. For example, heme (from
hemoglobin) and glucose are detected by reaction of these compounds with peroxidases
ed
incorporated in the dipstick and subsequent generation of a chromogen end-product that can be
pt
evaluated [18]. Other common chemical reactions include binding of the dye compounds,
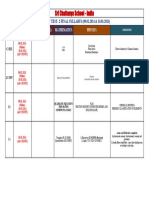
enzymatic, immunologic, and catalysis of oxidation-reduction reactions [19] (Table 1).
ce
Virtually all dipstick/dry chemistry analyses rely largely on colorimetry, with the intensity of
Ac
color change proportional to the concentration of the analyte being measured. The color is then
matched against a color reference chart to subjectively measure analyte concentration. These
manual/visual evaluations may be imprecise, depending on the visual acuity and color vision
fidelity of the observer.
Information Classification: General
Over the past 20 years, a variety of electronic technologies have significantly improved the
interpretation of color reaction products on dipsticks. Portable (handheld) dipstick readers have
become ubiquitous in primary care and hospital settings, as well as in the consumer market.
They are convenient, economical, and provide rapid, accurate results, depending on specimen
t
ip
handling, preservation, and quality. Such devices, based on electronics that convert photonic
energy [from colored reaction products) to electronic signals (CMOS – complementary metal
cr
oxide semiconductor devices), have reached a level of accuracy and precision that allows
us
generation of semi-quantitative/quantitative data. This type of technology is also present in
benchtop and larger laboratory automated systems that use dipstick/dry chemistry, such as the
an
Beckman Coulter IRICELL™,(Beckman Coulter Inc., Atlanta, GA), for example. . Automated
technologies increase specimen throughput, minimize specimen handling, reduce manual labor,
M
and speed delivery of results to patient records and clinical databases, but still employ the
fundamental dry chemistry technologies that evolved decades ago. These electronic
ed
technologies, and their use in dipstick interpretation, have been the subject of several excellent
papers and reviews; the interested reader is directed to them [20-25]. Recently, ‘lab on a chip’
pt
dipstick readers, that can be used with smartphone technology, have been described in the
ce
literature [26].
Ac
Dipstick/dry chemistry analysis can also provide useful information about other physical and
chemical properties of the urine sample. For osmolarity, a complexing agent in the dipstick will
release protons when in the presence of cations, which reacts with the dye indicator compound
bromthymol blue, producing a color change [18]. Sample pH can be determined within a range
Information Classification: General
of 5.0-8.5, although deviations can occur toward the ends of this range (<5.5 and >7.5). The
preferred and most accurate method to measure pH at those levels is use of a glass electrode [18].
Hemoglobin
Dipsticks can detect hemoglobin due to the heme moiety, which has pseudo-peroxidase activity
that catalyzes the reaction of peroxide and a chromogen molecule to produce a colored reaction
t
ip
product. The oxidation of a benzidine compound via reduction of a buffered organic peroxide
provides a positive result [27]. This test thus can detect hematuria, hemoglobinuria, or
cr
myoglobinuria, as all involve the heme moiety reaction [28].
us
Pseudo-peroxidases are hemoproteins that have active sites that can catalyze the H2O2 reduction
an
to water. Molecules that meet specific criteria can be considered to have peroxidase-like activity
and could theoretically trigger a false positive result. These criteria include: molecules that have
M
iron in the ferric form (Fe (III)), five coordination bonds and an H2O molecule on the distal side
of the heme molecule that is replaced with H2O2, and specific arrangements of amino acids
ed
(conserved histidine-arginine couple) [29]. There does not seem to be extensive documented
pt
evidence in the literature of porphyrin molecules or patients with porphyrias triggering ‘positive’
results for hematuria, however if a molecule in the pathway of hemoglobin synthesis were to
ce
meet the pseudoperoxidase criteria, then it could theoretically trigger a positive result.
Ac
False positive results for hematuria may be produced in instances of hemoglobinuria,
myoglobinuria, and from exogenous pseudo-peroxidases produced by contaminating bacteria
such as Lactobacillus species [27]. Strong reducing agents such as ascorbic acid can also cause
false-negative results [18]. In combination with a microscopic urinalysis for RBC count a
Information Classification: General
dipstick result for ‘blood’ (hematuria) can provide insight and guidance to whether a patient’s
macroscopically discolored urine may be the result of hematuria, hemoglobinuria,
myoglobinuria, pseudo-hematuria (drugs, dyes, etc.) [30].
Glucose
For glucose detection, it is the interaction of glucose with glucose oxidase that forms D-glucono-
t
ip
1,5-lactone and hydrogen peroxide. A peroxidase then catalyzes the reaction of hydrogen
peroxide with a reduced chromogen. Ascorbic acid (a reducing agent) and some bacteria may
cr
cause a false negative result, while oxidizing agents and hydrochloric acid can cause false
us
positive results [18].
Proteinuria
an
Dipsticks are commonly used to test for proteinuria. They can give a general estimate of the
amount of protein present in a sample. This is because the concentration of protein in a buffer
M
will cause a proportional change in pH. The dipstick method is most sensitive to albumin and
less sensitive to other proteins. The color of the dipstick can change from pale green, to green, to
ed
blue and offers an approximate quantification that is noted as 0 to plus-3 (+++) or plus-4 (++++)
depending upon the color [18].
pt
ce
In the absence of protein, the dipstick will remain yellow. Protein will disrupt the dye and buffer
on the dipstick and cause a green color to develop. Causes for a false positive result can include:
Ac
alkaline urine (pH > 7.5), overly length time of urine immersion, highly concentrated urine (less
hydrated states), gross hematuria, pus, semen, vaginal secretions, or some drugs such as
penicillin. False negative results can occur if the urine is extremely dilute such that the protein is
Information Classification: General
not adequately detected by the dipstick, or if the protein is significantly lower in molecular
weight (light chains) and other non-albumin proteins [31].
While glomerular disease is more common, tubular pathology can also result in proteinuria. This
occurs when proteins, of lower molecular weight, are unable to be reabsorbed from the filtrate
t
ip
due to a tubulointerstitial pathological process. This proteinuria is generally less than 2 grams in
24 hours and may result in a false negative dipstick result [31].
cr
Protein light chains such as Bence-Jones proteins (kappa and lambda light chains) are not
us
detected by dipstick and require additional testing. If there is suspicion for these smaller protein
chains, a sulfosalicylic acid test may be performed, however the definitive test for monoclonal
an
light chains would be electrophoresis [32,33].
Leukocytes – Esterase Activity
M
Dipsticks can provide insight into the presence of leukocytes in urine by means of indoxyl
esterase activity. This enzyme is released in the lysis of neutrophils and macrophages. Samples
ed
that have an alkaline pH or low densities due to the favored lysis of leukocytes in those
pt
environments will result in false positives, while conversely, high-density samples will decrease
sensitivity to leukocytes. High levels of glucose and protein, as well as some drugs (e.g.
ce
tetracyclines) can provide false negative results for leukocytes. Leukocytes will lyse and release
indoxyl esterase, which will catalyze reactions involving indoxyl or pyrrole carbonic acid esters,
Ac
and result in a product that interacts with a diazonium salt to produce color [34].
Nitrites
Dipstick tests for nitrites can be used as a proxy test for some Gram-negative bacteria that utilize
the nitrate reductase to reduce nitrates into nitrites. In order for this test to detect nitrites, there
Information Classification: General
first must be sufficient nitrates, typically from a vegetable-rich diet. The nitrites first react with
p-arsanilic acid on the dipstick to create a diazonium compound which then couples with a
quinolone compound on the dipstick to produce a pink color [34].
Ketones
The dipstick test to detect ketones such acetoacetate and acetone, involves their reaction with
t
ip
nitroprusside or nitroferricyanide and glycine [28]. Most test strips will detect acetoacetate,
which is the first ketone body created from acetyl-CoA, and some brands will detect acetone,
cr
however none detect beta-hydroxybutyric acid [34]. Ketostix® reagent strips (Siemens
us
Healthcare Diagnostics Inc./Bayer Diagnostics, Tarrytown, NY) were first demonstrated to be
more effective than test tube methods of ketone detection in 1958 [35]. Most modern test strips
an
will detect acetoacetate, which is the first ketone body created from acetyl-CoA, and some
brands will detect acetone, however none detect beta-hydroxybutyric acid [34]. Beta-
M
hydroxybutyric acid is the predominant ketone body present and is best tested with its own assay
using capillary blood [36]. Due to the predominance of beta-hydroxybutyric acid, the
ed
nitroprusside test may be weakly positive in some cases of increased ketones such as alcoholic
ketoacidosis [37]. In diabetic ketosis and ketoacidosis, capillary blood ketone testing was found
pt
to have fewer false positive and negative results than dipstick urine ketone testing [38].
ce
Bilirubin and Urobilinogen
Only bilirubin that is conjugated with glucuronic acid can pass through the glomerulus. Bilirubin
Ac
is also converted by bacterial enzymes into urobilinogen in the intestines, which can then be
oxidized into urobilin, which has a brown-pigmented color. These compounds can be present in
the urine. Bilirubin is normally not present in urine in any significant quantity, however
urobilinogen can be present normally. [34].
Information Classification: General
Many dipsticks that screen for bilirubin make use of a coupling reaction that occurs in the
presence of acid between bilirubin and a diazonium salt, however the specific salt used and
resulting color can vary between manufacturers. These sticks are ready after 30-60 seconds and
the typical resulting colors range from shades of tan to purple. Common diazonium salt
t
ip
indicators used by different dipsticks include: 2,6-dichlorobenzene-diazoniuim-tetrafluoroborate
in the Chemistrip® (Hoffmann-LaRoche Ltd., Basel, Switzerland)) and 2,4-dichloroanaline
cr
diazonium salt (Siemens Healthcare Diagnostics, Tarrytown, NY) [34].
us
an
For urobilinogen dipstick screening, the Ehrlich aldehyde reaction is utilized. In this reaction, an
aldehyde (p-dimethylaminobenzaldehyde) or diazonium salt compound is used in an acid
M
condition to react with urobilinogen to produce a red or pink colored azo dye product. The
dipstick is read after 30-60 seconds [34]. Urobilinogen may be elevated in situations of increased
ed
hemolysis and hepatocellular disease. It may also be decreased with antibiotic use due to a
change in the microbiota [28]. Since a positive result on this test may be normal, the screening of
pt
bilirubin is more useful for the early detection of pathology than urobilinogen.
ce
3. Benefits - why are dipsticks used?
Urine dipsticks are widely used for a number of reasons. As depicted above in the section on
Ac
assay principles, dipsticks can be used to test for a variety of factors that can help with clinical
decision-making and trigger further testing or investigation. Urine dipsticks are well poised to be
used in point-of-care settings due to their ease of use. This type of testing, as opposed to
traditional central laboratory testing has some advantages.
Information Classification: General
Point-of-care testing (POCT) can improve efficiency and metrics in primary care clinics by
allowing for faster communication with patients prior to them leaving the clinic, as well as
saving costs on more expensive tests that may not be necessary [39]. While initially more
expensive than central laboratory testing, POCT can reduce costs over time by reducing turn
around time, and reducing patient time spent in the emergency department (ED) or hospital
t
ip
depending upon the situation [40]. Use of a point-of-care comprehensive metabolic panel has
been shown to reduce ED length of stay in patients either admitted to the hospital or discharged
cr
to home as compared to central laboratory testing [41].
us
POCT urine analyzers can be used to read the results of dipstick dry chemistry, which can appear
an
very shortly after exposure to urine, with accuracy comparable to or exceeding visual analysis
[42]. This automation can further improve the efficiency of point-of-care urinalysis. Automated
M
dipstick tools have been shown to be sensitive for diagnosing urinary tract infection (UTI) and
can provide further justification to move forward with urine culture, although flow cytometry
ed
may provide even better predictions [43]. As stated in the section on assay principles, a standard
urine dipstick can be used to assess for a variety of enzymes and the presence of particles.
pt
Further, regardless of automation, dipsticks themselves are relatively straightforward to use in
ce
the clinic and can be utilized in settings with fewer resources and technology [18]. Automated
dipstick analysis has been combined with flow cytometry to construct devices that can cross-
Ac
check for discrepancies between tests, thus reducing the turnaround time necessary to check
samples manually in which results may be incorrect [44]. As noted previously, there is robust
literature describing the benefits accrued from both handheld and automated systems that use
electronic technologies to interpret chemical reactions on dipsticks.
Information Classification: General
Economically, urine dipsticks are among some of the most affordable and least expensive
laboratory tests available. The cost to a primary care clinic of running a test including specimen
collection, processing, labor costs, personal protective equipment (gloves), and the physical
dipstick itself can be estimated to total $3.05 [45]. The retail price of a packet of 100 Chemstrip
t
ip
9® dipsticks costs $57.45 at the time of this writing, amounting to less than $0.60 per stick [46].
The estimated cost of the automated urinalysis test at the Veterans Affairs Medical Center in
cr
Salem, VA, including cost of labor for technicians, phlebotomy and bundled cost of a
us
microscopic analysis, is less than $5.00. Average combined time for collection and analysis is
approximately 6 minutes (April 2019 email from S.T. Stoneman, Laboratory Information
an
Manager, MT to Varun Kavuru [VA urine dipstick cost]; unreferenced).
M
Dipsticks themselves are fairly inexpensive tests, but a positive result for proteinuria will result
in further confirmatory, quantitative testing such as a 24-hour urine collection or albumin-to-
ed
creatinine ratio (ACR ratio) [31]. The National Kidney Foundation also supports the use of ACR
ratio or albumin-specific dipsticks after a positive dipstick for proteinuria in its information for
pt
patients [47]. In addition to the above quantitative tests, a positive proteinuria dipstick result can
ce
trigger further microscopic analysis of urine sediment which may provide further findings of
casts that can provide further insight into a pathologic process [31]. In the cases of false
Ac
positives, this will result in more cost as tests are ordered with no true need to calculate protein
loss, however a negative screening dipstick result would not trigger the further more expensive
testing and provides a quick less expensive POC option for testing.
5. Limitations – why shouldn’t dipsticks be used
Information Classification: General
As noted, dipstick/dry chemistry tests can be useful POC screening tests to trigger more
definitive diagnostic evaluation, but are not useful for providing a definitive diagnosis alone.
While a single, dipstick/dry chemistry measurement of a suitable urine specimen at a single time
point may provide temporally useful information, the results are not intended to be diagnostic.
Dipstick/dry chemistry testing is not generally accepted as a means to screen large populations
t
ip
for the presence/absence of disease (see below).
cr
The limitations of such dipstick/dry chemistry tests (whether at a POC or in an automated
us
laboratory setting) are well-known and include:
• They may be inaccurate in quantifying important indicators of disease including glucose,
an
protein, albumin, hemoglobin (see examples and discussion, below), although recent
advances in the analysis of dipstick reactions (colors) with electronic technology can
M
produce semi-quantitative/quantitative data for further interpretation,
• Their use in determining the presence/absence of common conditions such as urinary
ed
tract infections may be problematic and is considered debatable, (especially in urgent
pt
POC settings) [48,10,49-54],
• They are not diagnostic for any particular disease and may only provide a simple,
ce
suggestive result for a variety of simple or more complex pathologies,
• Interfering compounds, including therapeutic drugs, vitamins/supplements, chemical
Ac
preservatives and detergents (used during sample collection) may invalidate test results,
• Values obtained by dipstick/dry chemistry measurement need to be interpreted in the
context of urine concentration, measured as urine specific gravity, and time of sample
collection [55],
Information Classification: General
• Values obtained by dipstick/dry chemistry measurements need to be interpreted in the
context of urine pH, since dipstick chemical reactions may be suboptimal at the extremes
of urine pH,
• Re-testing of individual samples (i.e., repeated dipstick tests on the same sample) is
rarely done,
t
ip
• Proximately timed, serial samples from the same individual are rarely tested,
cr
• False positive test results clearly may mislead and channel diagnostic thinking among
healthcare providers, and may create needless anxiety for patients,
us
• False negative results may discourage further diagnostic evaluation,
• POC interpretation (visual inspection) is subjective, based on color vision acuity of the
an
observer, lighting conditions, and correct timing of test interpretation (at the chemical
M
reaction maximum), and,
• The use of dipstick/dry chemistry test strips that are nearing expiration or which have
ed
been improperly stored is problematic due to the possibility of false positives.
pt
Two examples illustrate some of these limitations.
Both macroscopic and microscopic hematuria can be detected with dipstick/dry chemistry
ce
testing. There is a multitude of common and uncommon causes of hematuria, including urinary
tract infection, normal menstruation, abnormal menstruation, urinary tract calculi,
Ac
glomerulonephritis, pyelonephritis, and genitourinary tract neoplasms, to name a few. Clearly,
the dipstick test was not designed to and cannot differentiate among these and many other
causes.
Information Classification: General
Dipstick testing is rarely needed or used when macroscopic hematuria is seen. When
accompanied by pain, urinary tract infection or the presence of calculi are common, suspected
etiologies. When pain is not present, there is suspicion of primary glomerular disease or the
presence of urinary tract neoplasia. Further diagnostics may follow such as urine microscopy
and cytology followed by referral to a urologist if no clear etiology is determined. This may lead
t
ip
to further more testing such as CT intravenous pyelogram and cystoscopy [56]. In the setting of
macroscopic hematuria in the ED, use of dipsticks may still provide utility in evaluating the
cr
presence of infection as a possibly cause and can be consider part of the workup [57].
us
However, the detection of asymptomatic microscopic hematuria in routine urinalysis specimens
an
is common (seen in up to 18% of specimens) with dipstick testing [58,59]. Given a positive test
result, the patient and physician must then decide how to proceed, including 1) whether or not to
M
repeat the urinalysis, including urinary cytology, and/or 2) pursue diagnostic imaging, and/or 3)
consider cystoscopy for occult lesions (such as bladder cancer). The diagnostic path to be
ed
followed has been the subject of considerable debate [60,61]. In a recent study, Matulewicz and
co-workers considered the use of dipsticks to detect microhematuria a useful diagnostic
pt
procedure for detection of bladder cancer [62], however, there is no widely accepted algorithm
ce
that is followed when “dipstick hematuria” is found in routine screening urinalyses [63-65].
The presence of protein in urine is a significant indicator for further diagnostic evaluation, if
Ac
incidental specimen contamination is ruled out (i.e, from secretions and cells in free-catch
specimens). While protein in urine may indicate renal disease, it is difficult to discern early
stages of disease (i.e., before albumin appears in urine), and free-catch specimens may be
Information Classification: General
contaminated with proteins and secretions from other tissues in the urinary and genital tracts
[66].
In the past, regular measurement of urine glucose (for the purposes of adjusting insulin dosage)
allowed incidental measurement of urine protein. With the widespread acceptance of blood
t
ip
glucose monitoring for management of diabetes, routine collection of urine from diabetics has
decreased. It is, however, well-established that the development of microalbuminuria (defined
cr
here as the presense of small amounts of albumin in urine) is a harbinger of renal dysfunction in
us
diabetes mellitus, and that regular screening of the urine of diabetics for the presence of albumin
is both necessary and standard-of-care [67,68].
an
It is apparent that an economical, home-based test (i.e., dipstick/dry chemistry assay) could be
M
useful in early detection of diabetes-associated renal dysfunction. In a home-testing based
study of a cohort of patients with type 2 diabetes, Nagrebetsky and coworkers found that
ed
dipstick-based testing did not reliably detect microalbuminuria, compared to laboratory-based
testing of urine albumin-creatinine ratio [69]. Using systematic literature review and data meta-
pt
analysis, Wu and coworkers found that laboratory-based testing of urinary albumin concentration
ce
and albumin-creatinine ratio, although more expensive and less convenient than dipsticks, were
more reliably sensitive and specific tests for diabetes-associated microalbuminuria [70].
Ac
Zeller et al. conducted a study in which they assessed the diagnostic accuracy of transferrinuria
and an albumin-specific dipstick for detecting microalbuminuria in hypertensive non-diabetic
patients. These albumin-specific dipsticks such as Micral® (Hoffmann-LaRoche Ltd., Basel,
Information Classification: General
Switzerland) strips were found to be less sensitive and specific than transferrin-to-creatinine
ratios. The authors noted that prior studies of this type of dipstick had largely been done in
diabetic patients. They found the test to have more false positives than false negatives, but
deemed this acceptable for the screening purposes of the test. They found the negative predictive
value of the albumin-specific dipsticks to be high (92%) and concluded that the test provides a
t
ip
simple, useful, and cost-effective method of screening for microalbuminuria in hypertensive
patients in a primary care setting [71].
cr
us
The presence of albumin (and other proteins) in urine is an accepted indicator of the presence
and severity of chronic kidney disease (CKD) and regular monitoring of the urine of patients in
an
early stages of CKD may be quite useful in detecting responses to medical/lifestyle management,
as well as detecting progression of disease. Although economical and convenient (see above),
M
dipstick/dry chemistry testing for the presence of protein is unlikely to be either sufficiently
sensitive or specific in management of CKD. Abnormalities in the composition of urine
ed
sediments (hematuria, pyuria, casts, and other changes) also are considered potential indicators
of CKD and may be of greater value than single spot measurements of urine proteins with
pt
dipstick assays. Other molecular indicators of CKD, including the presence of complex
ce
metabolic by-products collectively termed “uremic solutes,” are not measured routinely in serum
or urine, either by dipstick/dry chemistry assays or standard laboratory automated urinalysis, but
Ac
may become important diagnostic biomarkers, since they are important in the pathogenesis/
progression of CKD and systemic co-morbidities such as cardiovascular disease [72].
Information Classification: General
A 2014 systemic review of guidelines for the use of urinary dipsticks for screening across 67
organizations in 9 countries found a lack of agreement in guidance amongst organizations for the
use of dipsticks for screening for some assays. Regarding screening for hemoglobin with
dipsticks, UK organizations of nephrology, urology, and the UK National screening committee
recommended against screening while some organizations made no comment or
t
ip
recommendation. Regarding screenings for leukocyte esterase and nitrites, all organizations
recommended against screening asymptomatic non-pregnant patients. Additionally, regarding
cr
screening for proteinuria, the UK National Screening Committee and Canadian Society of
us
Nephrology recommended against screening with dipsticks. The National Kidney Foundation
K/DOQI guideline recommends screening patients at high risk for CKD but recommended the
an
use of albumin-creatinine ratios or albumin-specific dipsticks. Overall this study found a lack of
clear consensus amongst guidelines across multiple organizations and countries for the use of
M
dipsticks for screening purposes [73].
ed
Conclusion
In summary, urine dipstick dry chemistry is easy to use, inexpensive, and has the ability to assess
pt
a variety of assay principles in a short period of time, making it ideal for a POCT setting. It is
ce
critical that careful attention is paid to the storage conditions of urine samples that are stored for
longer than two hours. The use of preservatives and cold temperature ranging from -80C to 4C
Ac
can extend the shelf life of urine and prevent the overgrowth of microorganisms, breakdown of
metabolites, and subsequent test results on a dry chemistry dipstick. However, one must note that
no one preservative substance is capable of perfectly preserving urine samples and without affect
on sample composition.
Information Classification: General
Urine dry chemistry is capable of assessing a wide array of assays such as pH, osmolality,
hemoglobin/myoglobin/hematuria, leukocyte esterase, glucose, proteinuria, nitrites, ketones, and
bilirubin. These findings can then provide a basis for further testing based upon clinical
suspicion. Examples include UTIs, diabetes mellitus (as well as diabetic ketoacidosis),
glomerular damage, metabolic defects, and even hepatic dysfunction.
t
ip
Other benefits of dipsticks include their ability to be automated to reduce human error and labor
cr
as well as their ability to be utilized in a point-of-care setting. The simple and fast nature of the
us
test, dripping urine onto the test strip, or dipping the test strip into a urine sample and allowing
the relevant reaction to occur lends itself able to be done very close to the patient’s bedside.
an
These factors allow for the potential for the test result to be returned to the patient very early and
may prevent the need for a second visit. In an emergent care setting, it can allow for faster
M
discharge or admission and facilitate decision making between provider and patient.
ed
Despite its advantages, dipstick dry chemistry presents a number of limitations to its use as a
broad screening tool. Dipstick dry chemistry alone is often not sufficient for decisions regarding
pt
clinical management and often prompt or discourage further testing, depending upon dry
ce
chemistry results. Limitations include a lack of quantifiable results, subject to false positives and
negatives due to various confounding factors in the patients diet or contamination of sample, and
Ac
dipstick interpretation variability. Another example of the limitation of dipsticks is the lack of a
widely accepted diagnostic algorithm for asymptomatic hematuria. Furthermore dipsticks have
not been shown to exhibit sufficient sensitivity for albumin in a routine home testing setting and
other markers such as albumin-to-creatinine ratio have been shown to be more effective for the
Information Classification: General
detection of diabetes associated microalbuminuria. In conclusion, despite the benefits of their
ease of use, low economic cost, and wide assay, urine dipsticks face a number of limitations in
their use as broad screening tools.
Disclosures:
t
ip
The contents of the paper and the opinions expressed within are those of the authors, and it was the
decision of the authors to submit the manuscript for publication.
cr
No potential conflict of interest reported by the authors.
us
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
an
References
[1] Pitts RF. Physiology of the Kidney and Body Fluids: An Introductory Text. 3rd revised ed.
M
Chicago: Year Book Medical Publishers; 1974.
ed
[2] Hall JE. Guyton and Hall Textbook of Medical Physiology. 13th ed. Philadelphia, PA:
Elsevier; 2016.
pt
[3] Haber MH. Pisse prophecy: a brief history of urinalysis. Clin. Lab. Med. 1988;8:415–430.
ce
[4] Echeverry G, Hortin GL, Rai AJ. Introduction to urinalysis: historical perspectives and
clinical application. Methods Mol. Biol. 2010;641:1–12.
Ac
[5] Delanghe JR, Speeckaert MM. Preanalytics in urinalysis. Clin. Biochem. 2016;49:1346–
1350.
[6] Dolscheid-Pommerich RC, Klarmann-Schulz U, Conrad R, et al. Evaluation of the
Information Classification: General
appropriate time period between sampling and analyzing for automated urinalysis.
Biochem Med (Zagreb). 2016;26:82–89.
[7] LaRocco MT, Franek J, Leibach EK, et al. Effectiveness of preanalytic practices on
contamination and diagnostic accuracy of urine cultures: a laboratory medicine best
t
practices systematic review and meta-analysis. Clin. Microbiol. Rev. 2016;29:105–147.
ip
[8] Wilson ML, Gaido L. Laboratory diagnosis of urinary tract infections in adult patients.
cr
Clin. Infect. Dis. 2004;38:1150–1158.
us
[9] Lifshitz E, Kramer L. Outpatient urine culture: Does collection technique matter? Arch.
an
Intern. Med. 2000;160:2537–2540.
[10] Frazee BW, Frausto K, Cisse B, et al. Urine collection in the emergency department: What
M
really happens in there? West. J. Emerg. Med. 2012;13:401–405.
ed
[11] Huttaus, H, Martinez, G, Coogan, H, Vu, T, Agnor, B, Donaghy, T, Zhang, S, Senger, R,
Robertson, J. Stability of Raman chemical signature of urine following microfiltration. In
pt
preparation,2019;
ce
[12] Senger, RS, Du, P, De la Torre Campos, D, Carswell, W, Webster, K, Sullivan, M, Gong,
J, Robertson, J. Assessment of urine specimen storage conditions using Raman
Ac
Chemometric Urinalysis™ (Rametrix™). Submitted, Peer J. 2019;
[13] Delanghe J, Speeckaert M. Preanalytical requirements of urinalysis. Biochemia Medica.
2014;89–104.
[14] Sureda-Vives M, Morell-Garcia D, Rubio-Alaejos A, et al. Stability of serum, plasma and
Information Classification: General
urine osmolality in different storage conditions: Relevance of temperature and
centrifugation. Clin. Biochem. 2017;50:772–776.
[15] Herrington W, Illingworth N, Staplin N, et al. Effect of processing delay and storage
conditions on Urine albumin-to-creatinine ratio. Clin J Am Soc Nephrol. 2016;11:1794–
t
1801.
ip
[16] Rotter M, Brandmaier S, Prehn C, et al. Stability of targeted metabolite profiles of urine
cr
samples under different storage conditions. Metabolomics. 2017;13:4.
us
[17] Ercan M, Akbulut ED, Abuşoğlu S, et al. Stability of urine specimens stored with and
an
without preservatives at room temperature and on ice prior to urinalysis. Clin. Biochem.
2015;48:919–922.
M
[18] Fogazzi GB, Verdesca S, Garigali G. Urinalysis: Core Curriculum 2008. Am. J. Kidney
Dis. 2008;51:1052–1067.
ed
[19] Pugia MJ. Technology behind diagnostic reagent strips. Lab Med. 2000;31:92–96.
pt
[20] Penders J, Fiers T, Delanghe JR. Quantitative evaluation of urinalysis test strips.
ce
Clin. Chem. 2002;48:2236–2241.
[21] Decavele A-SC, Fiers T, Penders J, et al. A sensitive quantitative test strip based
Ac
point-of-care albuminuria screening assay. Clin. Chem. Lab. Med. 2012;50:673
678.
[22] Delanghe JR, Himpe J, De Cock N, et al. Sensitive albuminuria analysis using dye
binding based test strips. Clin. Chim. Acta. 2017;471:107–112.
[23] Oyaert MN, Himpe J, Speeckaert MM, et al. Quantitative urine test strip reading for
Information Classification: General
leukocyte esterase and hemoglobin peroxidase. Clin. Chem. Lab. Med. 2018;56:1126–
1132.
[24] Salinas M, López-Garrigós M, Flores E, et al. Urinary albumin strip assay as a
screening test to replace quantitative technology in certain conditions. Clin. Chem. Lab.
Med. 2018;57:204–209.
t
ip
[25] Oyaert M, Delanghe J. Progress in Automated Urinalysis. Ann Lab Med.
2019;39:15–22.
cr
[26] Smith GT, Dwork N, Khan SA, et al. Robust dipstick urinalysis using a low-cost,
us
micro-volume slipping manifold and mobile phone platform. Lab Chip. 2016;16:2069–
2078.
an
[27] Pirkle JL, Palavecino EL, Freedman BI. Lactobacillus species can cause a false-positive
test for hematuria on dipstick urinalysis. Am. J. Med. 2013;126:e3-4.
M
[28] Simerville JA, Maxted WC, Pahira JJ. Urinalysis: A comprehensive review. Am. Fam.
ed
Physician. 2005;71:1153–1162.
[29] Vlasova II. Peroxidase Activity of Human Hemoproteins: Keeping the Fire under
pt
Control. Molecules. 2018;23.
ce
[30] Veerreddy P. Hemoglobinuria Misidentified as Hematuria: Review of Discolored
Urine and Paroxysmal Nocturnal Hemoglobinuria. Clin Med Insights Blood Disord.
Ac
2013;6:7–17.
[31] Carroll MF, Temte JL. Proteinuria in Adults: A Diagnostic Approach. AFP.
2000;62:1333–1340.
[32] Ramakrishnan N, Jialal I. Bence-Jones Protein. StatPearls [Internet]. Treasure Island
Information Classification: General
(FL): StatPearls Publishing; 2019 [cited 2019 Sep 29]. Available from:
http://www.ncbi.nlm.nih.gov/books/NBK541035/.
[33] Fine LG, Salehmoghaddam S. Proteinuria. In: Walker HK, Hall WD, Hurst JW,
editors. Clinical Methods: The History, Physical, and Laboratory Examinations [Internet].
3rd ed. Boston: Butterworths; 1990 [cited 2019 Sep 29]. Available from:
t
ip
http://www.ncbi.nlm.nih.gov/books/NBK705/.
[34] Mundt LA, Graff L, Shanahan K. Graff’s Textbook of Routine Urinalysis and Body
cr
Fluids. 2nd ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health;
us
2011.
an
[35] Chertack MM, Sherrick JC. Evaluation of a nitroprusside dip test for ketone bodies. J.
Am. Med. Assoc. 1958;167:1621–1624.
M
[36] Taboulet P, Haas L, Porcher R, et al. Urinary acetoacetate or capillary beta
hydroxybutyrate for the diagnosis of ketoacidosis in the Emergency Department setting.
ed
Eur J Emerg Med. 2004;11:251–258.
[37] Howard RD, Bokhari SRA. Alcoholic Ketoacidosis (AKA). StatPearls [Internet].
pt
Treasure Island (FL): StatPearls Publishing; 2019 [cited 2019 Sep 29]. Available from:
ce
http://www.ncbi.nlm.nih.gov/books/NBK430922/.
[38] Bektas F, Eray O, Sari R, et al. Point of care blood ketone testing of diabetic patients
Ac
in the emergency department. Endocr. Res. 2004;30:395–402.
[39] Lewandrowski E-L, Yeh S, Baron J, et al. Implementation of point-of-care testing in a
general internal medicine practice: A confirmation study. Clin. Chim. Acta. 2017;473:71–
74.
Information Classification: General
[40] Abel G. Current status and future prospects of point-of-care testing around the globe.
Expert Rev. Mol. Diagn. 2015;15:853–855.
[41] Jang JY, Shin SD, Lee EJ, et al. Use of a comprehensive metabolic panel point-of-care test
to reduce length of stay in the emergency department: a randomized controlled trial. Ann.
t
Emerg. Med. 2013;61:145–151.
ip
[42] van Delft S, Goedhart A, Spigt M, et al. Prospective, observational study comparing
cr
automated and visual point-of-care urinalysis in general practice. BMJ Open.
us
2016;6:e011230.
an
[43] Yusuf E, Van Herendael B, van Schaeren J. Performance of urinalysis tests and their
ability in predicting results of urine cultures: a comparison between automated test strip
M
analyser and flow cytometry in various subpopulations and types of samples. J. Clin.
Pathol. 2017;70:631–636.
ed
[44] Susianti H. Auto-Identification of discrepancies between urine test strip and sediment
results using Cross Check Function on fully automated urine analyzer. Intern.Clin. Path. J.
pt
[Internet]. 2015 [cited 2019 Mar 21];1. Available from:
ce
http://medcraveonline.com/ICPJL/ICPJL-01-00020.php.
[45] Sekhar DL, Wang L, Hollenbeak CS, et al. A cost-effectiveness analysis of screening
Ac
urine dipsticks in well-child care. Pediatrics. 2010;125:660–663.
[46] Chemstrip 9® strips use for glucose and ketones - 100 each [Internet]. Walmart.com.
[cited 2019 Apr 20]. Available from: /ip/Chemstrip-9®-Strips-Use-For-Glucose-And-
Ketones-100-Ea/47770344.
Information Classification: General
[47] Tests to Measure Kidney Function, Damage and Detect Abnormalities [Internet].
National Kidney Foundation. 2016 [cited 2019 Oct 5]. Available from:
https://www.kidney.org/atoz/content/kidneytests.
[48] Devillé WLJM, Yzermans JC, van Duijn NP, et al. The urine dipstick test useful to rule
out infections. A meta-analysis of the accuracy. BMC Urol. 2004;4:4.
t
ip
[49] Hooton TM, Roberts PL, Cox ME, et al. Voided midstream urine culture and acute cystitis
cr
in premenopausal women. N. Engl. J. Med. 2013;369:1883–1891.
us
[50] Huysal K, Budak YU, Karaca AU, et al. Diagnostic accuracy of UriSed® automated urine
microscopic sediment analyzer and dipstick parameters in predicting urine culture test
an
results. Biochem. Med. (Zagreb). 2013;23:211–217.
M
[51] Glissmeyer EW, Korgenski EK, Wilkes J, et al. Dipstick screening for urinary tract
infection in febrile infants. Pediatrics. 2014;133:e1121-1127.
ed
[52] Pallin DJ, Ronan C, Montazeri K, et al. Urinalysis in acute care of adults: pitfalls in testing
and interpreting results. Open Forum Infect. Dis. 2014;1:ofu019.
pt
[53] Frazee BW, Enriquez K, Ng V, et al. Abnormal urinalysis results are common, regardless
ce
of specimen collection technique, in women without urinary tract infections. J. Emerg.
Med. 2015;48:706–711.
Ac
[54] Ginting F, Sugianli AK, Kusumawati RL, et al. Predictive value of the urinary dipstick test
in the management of patients with urinary tract infection-associated symptoms in primary
care in Indonesia: A cross-sectional study. BMJ Open. 2018;8:e023051.
Information Classification: General
[55] Witte EC, Lambers Heerspink HJ, de Zeeuw D, et al. First morning voids are more
reliable than spot urine samples to assess microalbuminuria. J. Am. Soc. Nephrol.
2009;20:436–443.
[56] Yeoh M, Lai NK, Anderson D, et al. Macroscopic haematuria--a urological
t
approach. Aust Fam Physician. 2013;42:123–126.
ip
[57] Hicks D, Li C. Management of macroscopic haematuria in the emergency
cr
department. Emerg Med J. 2007;24:385–390.
[58] Mohr DN, Offord KP, Owen RA, et al. Asymptomatic microhematuria and urologic
us
disease. A population-based study. JAMA. 1986;256:224–229.
an
[59] Woolhandler S, Pels RJ, Bor DH, et al. Dipstick urinalysis screening of asymptomatic
adults for urinary tract disorders. I. Hematuria and proteinuria. JAMA. 1989;262:1214–
M
1219.
ed
[60] Nielsen M, Qaseem A, High Value Care Task Force of the American College of
Physicians. Hematuria as a marker of occult urinary tract cancer: Advice for high-value
pt
care from the American College of Physicians. Ann. Intern. Med. 2016;164:488–497.
ce
[61] Brown DD, Reidy KJ. Approach to the child with hematuria. Pediatr. Clin. North Am.
2019;66:15–30.
Ac
[62] Matulewicz RS, DeLancey JO, Pavey E, et al. Dipstick urinalysis as a test for
microhematuria and occult bladder cancer. Bladder Cancer. 2017;3:45–49.
[63] Kazi SN, Benz RL. Work-up of hematuria. Prim. Care. 2014;41:737–748.
Information Classification: General
[64] Bolenz C, Schröppel B, Eisenhardt A, et al. The investigation of hematuria. Dtsch.
Arztebl. Int. 2018;115:801–807.
[65] Brown RS. Hematuria as a marker of occult urinary tract cancer. Ann. Intern. Med..
2016;165:601.
t
ip
[66] Lambers Heerspink HJ, Gansevoort RT, Brenner BM, et al. Comparison of different
measures of urinary protein excretion for prediction of renal events. J. Am. Soc. Nephrol.
cr
2010;21:1355–1360.
us
[67] Ruggenenti P, Perna A, Ganeva M, et al. Impact of blood pressure control and
an
angiotensin-converting enzyme inhibitor therapy on new-onset microalbuminuria in type 2
diabetes: a post hoc analysis of the BENEDICT trial. J. Am. Soc. Nephrol. 2006;17:3472–
M
3481.
[68] Jun M, Ohkuma T, Zoungas S, et al. Changes in albuminuria and the risk of major clinical
ed
outcomes in diabetes: Results from ADVANCE-ON. Diabetes Care. 2018;41:163–170.
pt
[69] Nagrebetsky A, Jin J, Stevens R, et al. Diagnostic accuracy of urine dipstick testing in
screening for microalbuminuria in type 2 diabetes: a cohort study in primary care. Fam.
ce
Pract. 2013;30:142–152.
Ac
[70] Wu H-Y, Peng Y-S, Chiang C-K, et al. Diagnostic performance of random urine samples
using albumin concentration vs ratio of albumin to creatinine for microalbuminuria
screening in patients with diabetes mellitus: a systematic review and meta-analysis.
JAMA. Intern. Med. 2014;174:1108–1115.
Information Classification: General
[71] Zeller A, Haehner T, Battegay E, et al. Diagnostic significance of transferrinuria and
albumin-specific dipstick testing in primary care patients with elevated office blood
pressure. J Hum Hypertens. 2005;19:205–209.
[72] Ito S, Yoshida M. Protein-bound uremic toxins: new culprits of cardiovascular events in
chronic kidney disease patients. Toxins (Basel). 2014;6:665–678.
t
ip
[73] Krogsbøll LT. Guidelines for screening with urinary dipsticks differ substantially—a
cr
systematic review. Dan Med J. 2014;61:A4781.
us
an
M
ed
pt
ce
Ac
Information Classification: General
Table 1
t
ip
cr
us
an
M
ed
pt
ce
Ac
Informattion Classifica
ation: Generall
You might also like
- Proteins in Biology and MedicineFrom EverandProteins in Biology and MedicineRalph BradshawNo ratings yet
- Metabolomics Review 2014Document24 pagesMetabolomics Review 2014JessicaNo ratings yet
- Ha NNNNNDocument17 pagesHa NNNNNmr samoNo ratings yet
- Systematic Review and Meta-Analysis of Methods of Diagnostic Assessment For Urinary IncontinenceDocument10 pagesSystematic Review and Meta-Analysis of Methods of Diagnostic Assessment For Urinary Incontinence9661jackNo ratings yet
- Article - 1517381877 3Document14 pagesArticle - 1517381877 3Jeena RajNo ratings yet
- Prinsip Pemeriksaan Urin Rutin - 1Document6 pagesPrinsip Pemeriksaan Urin Rutin - 1AdnanNo ratings yet
- Friction Anisotropy Driven Domain Imaging On Exfoliated Monolayer GrapheneDocument5 pagesFriction Anisotropy Driven Domain Imaging On Exfoliated Monolayer GrapheneanggieNo ratings yet
- Kostelnik JAm Coll Nutr 2020 Urine ColorreviewDocument10 pagesKostelnik JAm Coll Nutr 2020 Urine ColorreviewNicole TenenbaumNo ratings yet
- Pharmacology of Selective Androgen Receptor ModulatorsDocument203 pagesPharmacology of Selective Androgen Receptor ModulatorsJoao RobaloNo ratings yet
- Male Lower Urinary Tract Symptoms & Benign Prostatic HyperplasiaDocument106 pagesMale Lower Urinary Tract Symptoms & Benign Prostatic HyperplasiaZICO0% (1)
- 2017 - CHEN - Etal - Raman Spectroscopy in Quality Control of Chinese Herbal Medicine - Chinese - Herbal - MedicineDocument9 pages2017 - CHEN - Etal - Raman Spectroscopy in Quality Control of Chinese Herbal Medicine - Chinese - Herbal - MedicinescribdNo ratings yet
- Journal of BTDocument19 pagesJournal of BTMr. BamsNo ratings yet
- Yakymenkoetal 2015Document17 pagesYakymenkoetal 2015Jake StoneNo ratings yet
- Chemical and Functional Genomic Approaches to Stem Cell Biology and Regenerative MedicineFrom EverandChemical and Functional Genomic Approaches to Stem Cell Biology and Regenerative MedicineNo ratings yet
- Chen 2013Document16 pagesChen 2013Alexandru ArcireNo ratings yet
- (Subcellular Biochemistry 73) Baoxue Yang, Jeff M. Sands (Eds.) - Urea Transporters-Springer Netherlands (2014)Document267 pages(Subcellular Biochemistry 73) Baoxue Yang, Jeff M. Sands (Eds.) - Urea Transporters-Springer Netherlands (2014)Alejandro Rojas GómezNo ratings yet
- Final Project DipangkarDocument27 pagesFinal Project DipangkarDIPANGKAR DUWARAHNo ratings yet
- Abhay Satoskar, Ravi Durvasula (Eds.) - Pathogenesis of Leishmaniasis - New Developments in Research-Springer-Verlag New York (2014)Document98 pagesAbhay Satoskar, Ravi Durvasula (Eds.) - Pathogenesis of Leishmaniasis - New Developments in Research-Springer-Verlag New York (2014)Abigail Roman SusayaNo ratings yet
- 1 s2.0 S0039914020310092 MainDocument20 pages1 s2.0 S0039914020310092 MainBen DresimNo ratings yet
- Methods in Enzymology Chromatin and Chromatin Remodeling EnzymesDocument475 pagesMethods in Enzymology Chromatin and Chromatin Remodeling EnzymesDiego Mauricio Gomez CuevasNo ratings yet
- Acm 2010 0572 PDFDocument6 pagesAcm 2010 0572 PDFRiley RilanNo ratings yet
- Acm 2010 0572 PDFDocument6 pagesAcm 2010 0572 PDFRiley RilanNo ratings yet
- 03 Na CB GuidelinesDocument152 pages03 Na CB GuidelinesPutri Zahra ArdiyanitaNo ratings yet
- Yeast As A Tool in Cancer Research 2007Document441 pagesYeast As A Tool in Cancer Research 2007Doorsea100% (1)
- Fraga 2014 BBA Total Antioxidant CapacityDocument4 pagesFraga 2014 BBA Total Antioxidant CapacityIgnacio PaviaNo ratings yet
- Baro Cycle RDocument24 pagesBaro Cycle RMousochist Yuanyang IINo ratings yet
- Powerpoint PresentationDocument16 pagesPowerpoint PresentationInga Budadoy NaudadongNo ratings yet
- Electrochemical Biosensors For Point-Of-Care Medical DiagnosticsDocument130 pagesElectrochemical Biosensors For Point-Of-Care Medical DiagnosticsJoão CostaNo ratings yet
- Laboratory Manager or AdministrationDocument4 pagesLaboratory Manager or Administrationapi-121327593No ratings yet
- Article StandardsandGuidelinesACMGDocument21 pagesArticle StandardsandGuidelinesACMGJuan Nezaret Baez LujanNo ratings yet
- Antibio AbstractDocument2 pagesAntibio Abstractvaidyam78No ratings yet
- Concise Biostatistics ManualDocument85 pagesConcise Biostatistics ManualMANASA AswathNo ratings yet
- CRISPR. Biology and Applications (Wiley, 2022)Document293 pagesCRISPR. Biology and Applications (Wiley, 2022)ntqhppnddpNo ratings yet
- Mode of Action PAADocument13 pagesMode of Action PAAAsa Étudier La-DienNo ratings yet
- Hair Analysis As A Biomonitor For Toxicology, Disease and Health StatusDocument26 pagesHair Analysis As A Biomonitor For Toxicology, Disease and Health StatusF WoyenNo ratings yet
- Chow Et Al 2023 Ispd Catheter Related Infection Recommendations 2023 UpdateDocument19 pagesChow Et Al 2023 Ispd Catheter Related Infection Recommendations 2023 UpdateMaria Eduarda CardosoNo ratings yet
- Article WJPR 1420104595Document15 pagesArticle WJPR 1420104595Vansh AggarwalNo ratings yet
- Analysis of Serum Immunoglobulins Using Fourier Transform Infrared Spectral MeasurementsDocument8 pagesAnalysis of Serum Immunoglobulins Using Fourier Transform Infrared Spectral MeasurementsHannaNo ratings yet
- JCM 13 00850Document10 pagesJCM 13 00850M Tapia CcNo ratings yet
- Journal ReviewDocument4 pagesJournal ReviewAndresurya PradanaNo ratings yet
- Ice ContaminationDocument52 pagesIce ContaminationKemasAlkindyNo ratings yet
- Jurnal ToxicDocument47 pagesJurnal ToxicMuh ImranNo ratings yet
- Shaker (2013) Manual of Diagnostic and Therapeutic Techniques For Disorders of DeglutitionDocument412 pagesShaker (2013) Manual of Diagnostic and Therapeutic Techniques For Disorders of DeglutitionVale GonzálezNo ratings yet
- Clinical Study and Management of UrolithiasisDocument11 pagesClinical Study and Management of UrolithiasisLusi RustinaNo ratings yet
- Effects of Gastrectomy or Colectomy On Liver Metabolism and Liver Morphology in An Experimental Rat ModelDocument9 pagesEffects of Gastrectomy or Colectomy On Liver Metabolism and Liver Morphology in An Experimental Rat ModelNishi RuciNo ratings yet
- Corticosteroid Injections For Symptomatic Treatment of Osteoarthritis of The Knee A Pilot Blinded Randomized TrialDocument7 pagesCorticosteroid Injections For Symptomatic Treatment of Osteoarthritis of The Knee A Pilot Blinded Randomized TrialkiranNo ratings yet
- Test Bank For Tietz Fundamentals of Clinical Chemistry and Molecular Diagnostics 7th Edition by BurtisDocument35 pagesTest Bank For Tietz Fundamentals of Clinical Chemistry and Molecular Diagnostics 7th Edition by Burtiscereus.kailc39cf97% (38)
- Effects of Dietary Supplementation at Nile Tilapia With Thymus Vulgaris, Trigonela Foenum Graecum and Azadirachta Indica On Welfare StatusDocument9 pagesEffects of Dietary Supplementation at Nile Tilapia With Thymus Vulgaris, Trigonela Foenum Graecum and Azadirachta Indica On Welfare StatusJosue GarciaNo ratings yet
- s42759148 Final ThesisDocument177 pagess42759148 Final Thesisnguyen baoNo ratings yet
- Cancer VejigaDocument10 pagesCancer VejigaMELANY MIRELLA FLORES RODRIGUEZNo ratings yet
- Atp As A Marker For Surface Contamination of Biological Origin in Schools and As A Potential Approach To The Measurement of Cleaning EffectivenessDocument12 pagesAtp As A Marker For Surface Contamination of Biological Origin in Schools and As A Potential Approach To The Measurement of Cleaning EffectivenessOSCAR DE JESUS FLORESNo ratings yet
- Pone D 24 09157Document27 pagesPone D 24 09157Wilson Adrian WijayaNo ratings yet
- Myocardial Preservation and Cellular AdaptationFrom EverandMyocardial Preservation and Cellular AdaptationRating: 5 out of 5 stars5/5 (1)
- Literature Review On Bacteriological Analysis of Well WaterDocument9 pagesLiterature Review On Bacteriological Analysis of Well Waterbav1dik0jal3No ratings yet
- Key Questions in Clinical Farm Animal Medicine, Volume 2: Types, Causes and Treatments of Infectious DiseaseFrom EverandKey Questions in Clinical Farm Animal Medicine, Volume 2: Types, Causes and Treatments of Infectious DiseaseTanmoy RanaNo ratings yet
- The Role of Membranes in Metabolic RegulationFrom EverandThe Role of Membranes in Metabolic RegulationMyron MehlmanNo ratings yet
- 2017 ACR Appropriateness Criteria Renal TrasplantDocument10 pages2017 ACR Appropriateness Criteria Renal TrasplantLiliana TorresNo ratings yet
- Clinical Applications of Capillary Electrophoresis: Methods and ProtocolsDocument270 pagesClinical Applications of Capillary Electrophoresis: Methods and ProtocolshesicosNo ratings yet
- Full Download Test Bank For Tietz Fundamentals of Clinical Chemistry and Molecular Diagnostics 7th Edition by Burtis PDF Full ChapterDocument35 pagesFull Download Test Bank For Tietz Fundamentals of Clinical Chemistry and Molecular Diagnostics 7th Edition by Burtis PDF Full Chapterseesaw.insearchd8k4100% (23)
- Como Usar ... Tiras Reactivas de OrinaDocument8 pagesComo Usar ... Tiras Reactivas de OrinaAntony Barzola GaldosNo ratings yet
- Actinobaculum Schaalii 2Document5 pagesActinobaculum Schaalii 2Antony Barzola GaldosNo ratings yet
- Beneficios de La Tincion Gram DirectaDocument7 pagesBeneficios de La Tincion Gram DirectaAntony Barzola GaldosNo ratings yet
- Microbiology Identification PDFDocument31 pagesMicrobiology Identification PDFAntony Barzola GaldosNo ratings yet
- Org. Synth. 2005, 81, 33-41 (Fer Discussion)Document15 pagesOrg. Synth. 2005, 81, 33-41 (Fer Discussion)ludoNo ratings yet
- AITS 2019 25 Papers WITH ANS 458pgDocument458 pagesAITS 2019 25 Papers WITH ANS 458pgSahil chetry100% (1)
- Brazing, Soldering, Adhesive, Bonding & Mechanical Fastening ProcessDocument23 pagesBrazing, Soldering, Adhesive, Bonding & Mechanical Fastening ProcessAd Man GeTigNo ratings yet
- Modified Rosin Ester PreparationDocument17 pagesModified Rosin Ester PreparationRian Pratama AkbaNo ratings yet
- Ver.2014 1 MagCore SUPER PLUS Service ManualDocument72 pagesVer.2014 1 MagCore SUPER PLUS Service Manualمحمد سامىNo ratings yet
- Physical and Chemical ChangesDocument7 pagesPhysical and Chemical ChangesSarika AhujaNo ratings yet
- Mean Median Mode RangeDocument2 pagesMean Median Mode RangeShin WonHoNo ratings yet
- US2789119Document3 pagesUS2789119Feride Elif ErtürkNo ratings yet
- Zoeller. Eastman Chemical Company Acetic Anhydride ProcessDocument19 pagesZoeller. Eastman Chemical Company Acetic Anhydride ProcessJohn Patrick DagleNo ratings yet
- Chemistry June 2021 MSDocument14 pagesChemistry June 2021 MSΒασιλεία ΕυαγγέλουNo ratings yet
- 7182 PDFDocument5 pages7182 PDFAslam SheriffNo ratings yet
- Anacardium Occidentale 5Document7 pagesAnacardium Occidentale 5Jesus Llorente MendozaNo ratings yet
- Archive Test Series JEE (Main) 2024Document2 pagesArchive Test Series JEE (Main) 2024aakaastyagiNo ratings yet
- AINOMICRODocument13 pagesAINOMICROLast Juan StandingNo ratings yet
- Coordination Compounds Theory Sheet-244 PDFDocument36 pagesCoordination Compounds Theory Sheet-244 PDFJatin SinglaNo ratings yet
- Molecular Basis of Inheritance TranscriptionDocument2 pagesMolecular Basis of Inheritance TranscriptionsoundharyaNo ratings yet
- Ipl Part Test - 2 Final Syllabus (09.01.2024 0 10.01.2024)Document1 pageIpl Part Test - 2 Final Syllabus (09.01.2024 0 10.01.2024)murali.trichyNo ratings yet
- Databook Aw HT 0404 0604Document28 pagesDatabook Aw HT 0404 0604tachetacheNo ratings yet
- Biological Magnetic Resonance V 2Document360 pagesBiological Magnetic Resonance V 2pauloNo ratings yet
- Prepared & Presented by Technical Service - PT. HEMPEL IndonesiaDocument32 pagesPrepared & Presented by Technical Service - PT. HEMPEL IndonesiavvpvarunNo ratings yet
- Reaction Quotient: Trial 1 Trial 2Document14 pagesReaction Quotient: Trial 1 Trial 2criselda macabuhayNo ratings yet
- AP Chemistry Laboratory Manual Mr. Davis Auburn Riverside HSDocument86 pagesAP Chemistry Laboratory Manual Mr. Davis Auburn Riverside HSstrivedi23No ratings yet
- Carbon NanomaterialDocument4 pagesCarbon NanomaterialAshish Dev (B21MT009)No ratings yet
- 2013 02 DNT 044 LIDA RodDocument2 pages2013 02 DNT 044 LIDA RodKeny AnchanteNo ratings yet
- 2a - Titrations For 2014Document3 pages2a - Titrations For 2014Lutendo Assurance MadzivhaaNo ratings yet
- Biomolecules ScriptDocument2 pagesBiomolecules ScriptGladz GladzNo ratings yet
- SikaWrap 231 C PDS PDFDocument4 pagesSikaWrap 231 C PDS PDFMohit KohliNo ratings yet
- Draft Resti..Document63 pagesDraft Resti..Leni LismayantiNo ratings yet
- CO2 Handbook IIARDocument190 pagesCO2 Handbook IIAROnofreHalberNo ratings yet
- Science 7 2.1 Pure SubstancesDocument17 pagesScience 7 2.1 Pure SubstancesaiceNo ratings yet