Professional Documents
Culture Documents
Genetic Epilepsy Syndromes
Uploaded by
Anali Durán CorderoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Genetic Epilepsy Syndromes
Uploaded by
Anali Durán CorderoCopyright:
Available Formats
Genetic Epilepsy REVIEW ARTICLE
Syndromes CONTINUUM AUDIO
INTERVIEW AVAILABLE
ONLINE
By Kenneth A. Myers, MD, PhD, FRCPC, CSCN(EEG)
ABSTRACT
PURPOSE OF REVIEW: This article reviews the clinical features, typical EEG
findings, treatment, prognosis, and underlying molecular etiologies of the
more common genetic epilepsy syndromes. Genetic generalized epilepsy,
self-limited focal epilepsy of childhood, self-limited neonatal and infantile
epilepsy, select developmental and epileptic encephalopathies,
progressive myoclonus epilepsies, sleep-related hypermotor epilepsy,
photosensitive occipital lobe epilepsy, and focal epilepsy with auditory
features are discussed. Also reviewed are two familial epilepsy
syndromes: genetic epilepsy with febrile seizures plus and familial focal
epilepsy with variable foci. CITE AS:
CONTINUUM (MINNEAP MINN)
2022;28(2, EPILEPSY):339–362.
Recent years have seen considerable advances in our
RECENT FINDINGS:
understanding of the genetic factors underlying genetic epilepsy Address correspondence to
syndromes. New therapies are emerging for some of these conditions; in Dr Kenneth A. Myers, Montreal
Children's Hospital, 1001 Décarie
some cases, these precision medicine approaches may dramatically
Blvd, Montreal, Quebec,
improve the prognosis. H4A 3J1, Canada,
kenneth.myers@mcgill.ca.
SUMMARY: Many recognizable genetic epilepsy syndromes exist, the
RELATIONSHIP DISCLOSURE :
identification of which is a crucial skill for neurologists, particularly those Dr Myers has received personal
who work with children. Proper diagnosis of the electroclinical syndrome compensation in the range of
$500 to $4999 for serving as an
allows for appropriate treatment choices and counseling regarding academic writer with Springer
prognosis and possible comorbidities. Publishing Company. The
institution of Dr Myers has
received research support
from Dravet Canada, Fonds
de recherche du Québec,
INTRODUCTION Koolen-de Vries Syndrome
A
lthough epilepsy is an etiologically heterogeneous condition, the Foundation, The Liam
Foundation, and the Savoy
importance of genetic factors has been acknowledged for many Foundation.
decades.1 This is perhaps clearest in the case of generalized epilepsy,
where the risk in first-degree relatives is 5- to 10-fold greater than UNLABELED USE OF
PRODUCTS/INVESTIGATIONAL
the general population.2-4 In twin studies, the concordance rate is USE DISCLOSURE :
significantly higher for monozygotic compared with dizygotic twins.5-8 Epilepsy Dr Myers discusses the
unlabeled/investigational use of
inheritance can follow a Mendelian pattern (ie, autosomal dominant, autosomal
clobazam for the treatment of
recessive, or X-linked); however, in many cases the pattern appears more forms of epilepsy other than
complex, likely involving polygenic inheritance and epigenetic factors.1,9 Lennox-Gastaut syndrome and
quinidine for the treatment of
In many epilepsy syndromes, the underlying cause is known or assumed to be epilepsy due to KCNT1
genetic. These conditions include both self-limited (formerly termed benign) pathogenic variants.
phenotypes and more severe conditions, such as developmental and epileptic
encephalopathies. This article reviews the clinical and electrographic aspects of © 2022 American Academy
these syndromes, as well as what is known about the underlying molecular factors. of Neurology.
CONTINUUMJOURNAL.COM 339
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
GENETIC EPILEPSY SYNDROMES
GENETIC GENERALIZED EPILEPSIES
Also known as idiopathic generalized epilepsies, the genetic generalized epilepsy
syndromes comprise a group of disorders that share some common clinical and
electrophysiologic factors (TABLE 4-1). In the 2017 International League Against
Epilepsy (ILAE) epilepsy classification, genetic generalized epilepsy was described
as the more accurate nomenclature; however, idiopathic generalized epilepsy is
also considered acceptable.10 Overall, the genetic generalized epilepsy
syndromes are characterized by normal background activity and interictal
generalized epileptiform discharges on EEG; brain imaging is also almost always
TABLE 4-1 Genetic Generalized Epilepsy Syndromes
Typical
age of
onset, Seizure Brain Genetic
Syndrome years type(s) Treatment Prognosis EEG imaging causes
Childhood 4-10 Typical Ethosuximide or Majority have Normal Normal Complex
absence absences, valproic acid as spontaneous background; inheritance in
epilepsy rarely first-line remission, interictal vast majoritya;
generalized usually before generalized glucose
tonic-clonic or during spike-wave transporter
adolescence; fragments; type 1 (GLUT1)
minority evolve 3-Hz generalized deficiency
into juvenile spike-wave should be
myoclonic during considered if
epilepsy or absences onset is at
other syndrome <4 years or
other atypical
features are
present
Juvenile 12-18 Myoclonic Valproic acid Majority are Normal Normal Complex
myoclonic and usually first-line; controlled on background; inheritance in
epilepsy generalized in female medication, but interictal vast majoritya;
tonic-clonic; patients, other only a small generalized GABRA1 is rare
absences are options should be minority are spike-wave autosomal
less common considered first; able to wean off and polyspike- dominant
avoid of treatment wave cause
carbamazepine fragments;
and high-amplitude
oxcarbazepine spike-wave/
polyspike-
wave bursts
with myoclonic
seizures
CONTINUED ON PAGE 341
340 APRIL 2022
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
normal. Genetic testing is usually negative, as the vast majority of cases are
thought to occur through complex inheritance.11 The individual syndromes are
differentiated largely by seizure type(s), EEG findings, age of onset, and clinical
course (ie, likelihood of spontaneous remission).
Childhood Absence Epilepsy
Childhood absence epilepsy is a relatively common epilepsy syndrome, having an
estimated cumulative incidence of approximately 1 in 1000 people.12,13 Seizure
onset is typically between 4 and 10 years of age; children with onset before
CONTINUED FROM PAGE 340
Typical
age of
onset, Seizure Brain Genetic
Syndrome years type(s) Treatment Prognosis EEG imaging causes
Juvenile 12-18 Typical Many options Less than half Normal Normal Complex
absence absences are seizure free background; inheritance in
epilepsy and on medication; interictal vast majoritya
generalized usually require generalized
tonic-clonic lifelong spike-wave
treatment and polyspike-
wave
fragments; 4-
to 5-Hz
generalized
spike-wave
during
absences
Epilepsy 5-40 Generalized Many options Variable; Normal Normal Complex
with tonic-clonic Patients with background; inheritance in
generalized childhood- interictal vast majoritya
tonic-clonic onset have a generalized
seizures better spike-wave
alone prognosis fragments
Epilepsy 1-16 Eyelid Many options Drug resistance Normal Normal Complex
with eyelid myoclonia, in 80% background; 3- inheritance in
myoclonia absences, to 6-Hz vast majoritya;
generalized generalized pathogenic
tonic-clonic spike-wave/ variants in
polyspike- CHD2,
wave; fixation- SYNGAP1, and
off sensitivity KCNB1 can
produce
similar
phenotype
but usually
with more
severe
intellectual
disability
a
If the syndrome occurs in the context of a family with genetic epilepsy with febrile seizures plus, genetic testing should be considered.
CONTINUUMJOURNAL.COM 341
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
GENETIC EPILEPSY SYNDROMES
4 years of age can be considered to have early-onset absence epilepsy.14 For
reasons that are unclear, childhood absence epilepsy may have a higher incidence
in girls than boys.15
In childhood absence epilepsy, the defining seizure type is a typical absence
seizure, involving a sudden, brief loss of awareness (usually 4 to 30 seconds)
followed by an almost immediate return to baseline (ie, no significant postictal
state).16 Patients typically stare blankly and may have subtle automatisms, most
commonly oral.16 Typical absence seizures are often subtle, and children are
often having hundreds per day at the time of diagnosis. Affected children may be
misdiagnosed with attention deficit disorder or daydreaming before diagnosis.
Typical absence seizures can often be provoked by hyperventilation; asking the
patient to hyperventilate for at least 3 minutes provides a useful method to
evaluate seizure control in the clinic. During seizures, EEG shows an abrupt
onset of generalized rhythmic spike-wave discharges at approximately 3 Hz
(FIGURE 4-1).16 Interictal EEG often shows normal background activity with
generalized spike-wave fragments in up to 92% of patients.17
Initial treatment of childhood absence epilepsy is usually with either
ethosuximide or valproic acid; efficacy of the two agents is similar although
ethosuximide may be better tolerated overall.18 The long-term prognosis is good
with the majority of patients having spontaneous remission. In one study of
patients with childhood absence epilepsy, followed for at least 12 years, only 7%
still had seizures.19 Generalized tonic-clonic seizures occur in approximately 12%
of patients with childhood absence epilepsy, usually at least several years after
the onset of absences.20 This finding can signal an evolution of phenotype from
childhood absence epilepsy into a different epilepsy syndrome such as juvenile
myoclonic epilepsy (JME).
In the vast majority of patients with childhood absence epilepsy, brain
imaging is normal and the underlying genetic inheritance is thought to be
complex, so investigations beyond routine EEG are of little utility. However,
genetic testing should be considered in patients with atypical courses,
FIGURE 4-1
Typical absence seizure. EEG of a 12-second typical absence seizure in a 4-year-old girl
with childhood absence epilepsy. Three-Hz generalized spike wave is seen, with abrupt
onset and offset.
342 APRIL 2022
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
particularly early-onset absence epilepsy because 10% of these patients have KEY POINTS
pathogenic variants in SLC2A1, the gene encoding glucose transporter type 1
● Genetic epilepsy
(GLUT1).21 Children with GLUT1 deficiency may have other neurologic features, syndromes may follow
such as paroxysmal dyskinesias, and require different management, including Mendelian patterns or may
the ketogenic diet.22 Brain imaging should be considered in patients who are exhibit complex inheritance,
drug-resistant, as focal lesions can rarely mimic childhood absence epilepsy. likely related to both
polygenic and epigenetic
factors.
Juvenile Myoclonic Epilepsy
JME is another relatively common form of epilepsy, with a point prevalence in ● Overall, the genetic
generalized epilepsy
adults of approximately 0.4 in 1000.23 Age of onset is typically between 12 and syndromes are
18 years.24 The prototypic seizure type is myoclonic jerks that are most characterized by normal
prominent in the mornings, although patients may also experience generalized background activity and
tonic-clonic or absence seizures. Seizures are often provoked by sleep interictal generalized
epileptiform discharges on
deprivation, flashing lights, or alcohol intake.24 Avoiding these inciting factors is
EEG; brain imaging is also
often challenging for young people of normal intelligence and can limit quality of almost always normal.
life.25 Interictal EEG typically shows normal background activity with Genetic testing is usually
generalized 4- to 6-Hz spike-wave and polyspike-wave fragments.24 negative, as the vast
majority of cases are
Photosensitivity is often seen, and patients may have myoclonic seizures with
thought to occur through
high-amplitude spike-wave or polyspike-wave bursts (FIGURE 4-2).24 complex inheritance.
Valproic acid appears to have the greatest efficacy in controlling seizures in
JME; however, many clinicians avoid use in female patients because of the ● In childhood absence
teratogenic and neurodevelopmental risk to the fetus in pregnancy; other agents epilepsy, the defining
seizure type is a typical
such as levetiracetam or lamotrigine can be used instead.24,26,27 However, as well absence seizure, involving
as with other sodium channel antagonists such as carbamazepine and a sudden, brief loss of
oxcarbazepine, lamotrigine risks exacerbating myoclonic seizures and even awareness (usually 4 to
provoking myoclonic status epilepticus.26 Although the majority of patients with 30 seconds) followed by an
almost immediate return to
JME have seizures controlled with medication, the rate of long-term epilepsy baseline (ie, no significant
remission is very low; in one study, 80% of patients with JME who attempted postictal state). Patients
medication weaning had seizure recurrence.28 typically stare blankly and
may have subtle
automatisms, most
commonly oral.
● Typical absence seizures
can often be provoked by
hyperventilation; asking the
patient to hyperventilate for
at least 3 minutes provides a
useful method to evaluate
seizure control in the clinic.
During seizures, EEG shows
an abrupt onset of
generalized rhythmic spike-
wave discharges at
approximately 3 Hz.
FIGURE 4-2
Myoclonic seizure. EEG of a myoclonic seizure during 18-Hz photic stimulation in a 13-year-
old girl with juvenile myoclonic epilepsy. High-amplitude generalized polyspike-wave
discharges are seen, correlating with the patient’s clinical jerks.
CONTINUUMJOURNAL.COM 343
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
GENETIC EPILEPSY SYNDROMES
For patients with JME, the diagnosis is clinical, and further investigations are
rarely indicated beyond routine EEG. Most clinicians would not perform genetic
testing, even though there may be some rare genes exhibiting Mendelian
inheritance, namely GABRA1.29 However, for patients who exhibit significant
developmental impairment, neuropsychiatric decline, or other atypical features,
alternative diagnoses, including progressive myoclonus epilepsy (discussed later
in this article), should be considered and investigated thoroughly.
Juvenile Absence Epilepsy
Juvenile absence epilepsy bears many similarities to JME, with one of the main
differentiating factors being the lack of myoclonic seizures.30 Typical absence
seizures are the most prominent seizure type; however, unlike in childhood
absence epilepsy, most patients with juvenile absence epilepsy have, at most, a
few seizures per day, and loss of awareness may be less complete.31 As well, the
ictal EEG during absences shows a faster rhythmic spike-wave signature of 4 to
5 Hz. Interictal EEG shows a normal background with generalized spike-wave
and polyspike-wave fragments. Roughly 50% to 80% of patients with juvenile
absence epilepsy will also experience generalized tonic-clonic seizures.30,31
The long-term prognosis may be slightly worse with juvenile absence epilepsy
than JME; in one study, only 39% of patients had been seizure free on
medications for at least 2 years, and 100% of patients who attempted medication
withdrawal had seizure relapse.28 As with JME, the diagnosis is primarily clinical,
and further investigations are not usually indicated if the patient is of normal
intelligence and has no atypical features.
Epilepsy with Generalized Tonic-Clonic Seizures Alone
As the name suggests, epilepsy with generalized tonic-clonic seizures alone is a
genetic generalized epilepsy in which generalized tonic-clonic seizures are the
only seizure type. Age of onset has been reported to vary from 5 to 41 years, but
some have argued that childhood-onset epilepsy with generalized tonic-clonic
seizures alone should be considered a distinct entity from patients who have
onset in adolescence or later.32,33 A subset of patients have seizures exclusively on
awakening, leading some to classify those patients separately from those with a
“random” seizure pattern.33
Interictal EEG typically shows a normal background with interictal
generalized spike-wave fragments.33 Valproic acid has classically been the first-
line therapy, with approximately two-thirds of patients becoming seizure free.33
Prognosis may be better overall in those with onset in childhood, with all
remaining seizure free after weaning of antiseizure medication in one study.32
As with the other genetic generalized epilepsy syndromes, genetic testing and
neuroimaging have limited utility, particularly if the patient has normal
intelligence.
Epilepsy With Eyelid Myoclonias
Epilepsy with eyelid myoclonias (also known as Jeavons syndrome) is a childhood-
onset genetic generalized epilepsy classically involving a triad of (1) characteristic
brief eye-fluttering seizures (eyelid myoclonia), (2) eye closure–induced seizures/
epileptiform abnormalities on EEG, and (3) photosensitivity.34,35 These eyelid
myoclonias usually occur hundreds of times per day and can often be triggered by
voluntary eye closure. Patients may also have other seizure types, the most
344 APRIL 2022
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
common being generalized tonic-clonic (70% to 75%) or typical absences (100% KEY POINTS
in one study).34,36 Age of seizure onset is variable, from 1 to 16 years.34,36
● Children with absence
Seizures are drug resistant in 80% of patients.36 Mild to moderate intellectual seizures starting before the
disability is reported in 23% to 35% of patients.34,36 Genetic testing is usually age of 4 years are
negative in patients with a classic phenotype. De novo pathogenic variants in considered to have early-
CHD2, SYNGAP1, and KCNB1 have been associated with epilepsy with eyelid onset absence epilepsy; 10%
of these patients have
myoclonia–like phenotypes; however, these patients usually have more severe glucose transporter type 1
cognitive impairment and sometimes have phenotypes more in keeping with (GLUT1) deficiency due to
developmental and epileptic encephalopathies.37-39 pathogenic SLC2A1 variants.
● Age of onset of juvenile
SELF-LIMITED FOCAL EPILEPSIES OF CHILDHOOD
myoclonic epilepsy is
The self-limited (formerly called benign) focal epilepsies of childhood are a group typically between 12 and 18
of sometimes overlapping epilepsy syndromes that share several common years. The prototypic
features (TABLE 4-2). The term benign was replaced by self-limited and seizure type is myoclonic
pharmacoresponsive in the 2017 ILAE epilepsy classification.10 Children with jerks that are most
prominent in the mornings,
self-limited focal epilepsies of childhood typically have normal or near-normal although patients may also
development and normal neuroimaging, and seizures usually spontaneously experience generalized
resolve before or during adolescence. tonic-clonic or absence
seizures. Seizures are often
provoked by sleep
Childhood Epilepsy With Centrotemporal Spikes deprivation, flashing lights,
Childhood epilepsy with centrotemporal spikes has previously been referred to or alcohol intake.
as benign epilepsy of childhood with centrotemporal spikes” and benign Rolandic
epilepsy. Children first present with seizures typically between 7 and 10 years of ● Interictal EEG of JME
typically shows normal
age (range, 1 to 14 years), often from sleep.40 The seizure symptomatology is
background activity with
focal aware or focal impaired awareness, involving prominent hemifacial jerking generalized 4- to 6-Hz
or dystonia, facial paresthesia, drooling, and mumbling, and occasionally spike-wave and polyspike-
progressing to bilateral tonic-clonic convulsions.40 EEG shows focal wave fragments.
monomorphic medium-high amplitude spikes and spike-wave discharges over
● Although the majority of
one or both centrotemporal regions, having a characteristic morphology and patients with JME have
horizontal dipole (FIGURE 4-3). The discharges may be sparse in wakefulness but seizures controlled with
are markedly potentiated in sleep. medication, the rate of long-
Seizures typically respond well to antiseizure medication; most agents would term epilepsy remission is
very low.
likely be effective, with carbamazepine and valproic acid being popular choices
in published studies.41 However, as many children will have only several ● Sodium channel inhibitors
seizures in their life, clinical practice varies as to whether to initiate treatment at should be avoided in
all. The overall practice tends to be to recommend antiseizure medication41; patients with juvenile
myoclonic epilepsy, if
however, it is reasonable to make this decision in consideration of several factors,
possible, as there is the
including the number of seizures the child has experienced, time interval potential to exacerbate
between seizures, seizure duration, whether seizures have progressed to bilateral myoclonic seizures.
tonic-clonic, and parent/caregiver preference.
Although originally termed a “benign” disorder, neuropsychological ● Juvenile absence epilepsy
bears many similarities to
evaluation of cohorts of children with childhood epilepsy with centrotemporal JME, with one of the main
spikes finds an elevated risk for mild developmental impairment, particularly differentiating factors being
involving language function.42-45 Childhood epilepsy with centrotemporal spikes the lack of myoclonic
is considered to be at the mild end of the epilepsy-aphasia spectrum of disorders, seizures.
which also includes atypical childhood epilepsy with centrotemporal spikes, ● The ictal EEG of juvenile
Landau-Kleffner syndrome, and epileptic encephalopathy with continuous spike absence epilepsy during
wave in sleep.46 For isolated, typical childhood epilepsy with centrotemporal absences shows a faster
spikes, genetic testing has little utility at this time, although this is not the case for rhythmic spike-wave
signature of 4 to 5 Hz.
other epilepsy aphasia spectrum disorders.47 Neuroimaging is not necessary for
CONTINUUMJOURNAL.COM 345
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
GENETIC EPILEPSY SYNDROMES
patients with typical presentations and well-controlled seizures, particularly if
the EEG shows independent bilateral epileptiform discharges; however, brain
MRI should be performed to rule out an intracranial lesion for any patients not
following the expected clinical course.
Atypical Childhood Epilepsy With Centrotemporal Spikes
The original clinical description of atypical childhood epilepsy with
centrotemporal spikes by Aicardi and Chevrie48 described patients with the same
TABLE 4-2 Self-Limited Focal Epilepsy Syndromes of Childhood
Typical
age of Brain Genetic
Syndrome onset, years Seizure type(s) Treatment Prognosis EEG imaging causes
Childhood 7-10 Focal aware May not need Majority have Normal Normal Complex
epilepsy with seizures/focal to initiate <10 seizures; background; inheritance
centrotemporal impaired medication; spontaneous interictal focal in vast
spikes awareness most agents remission spikes and majoritya
seizures, effective within 2-4 years spike-wave
hemifacial discharges
sensorimotor independently
(hemiface over right and/
clonic/ or left
dystonic, centrotemporal
drooling, regions,
vocalization, markedly
facial potentiated in
paresthesia); sleep
may have
focal-to-
bilateral tonic-
clonic seizures
Atypical 2-6 Focal aware Most agents May have Normal Normal Complex
childhood seizures/focal can be drug-resistant background; inheritance
epilepsy with impaired effective; seizures interictal focal in most;
centrotemporal awareness carbamazepine initially, but spikes and GRIN2A
spikes seizures (as in and spontaneous spike-wave pathogenic
childhood oxcarbazepine remission discharges variants in
epilepsy with can exacerbate usually occurs independently some
centrotemporal seizures by adolescence over right and/ patients;
spikes), negative or left single
myoclonus, centrotemporal reports of
atypical regions, de novo
absences markedly pathogenic/
potentiated in likely
sleep pathogenic
variants in
GRIN2B,
CAMK2A,
and
CACNG2
CONTINUED ON PAGE 347
346 APRIL 2022
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
focal seizures and EEG signature as childhood epilepsy with centrotemporal
spikes, but additional ictal symptomatologies, including atypical absences and
myoclonic or atonic seizures. With time, negative myoclonus has come to be
recognized as the classic feature of atypical childhood epilepsy with
centrotemporal spikes, and the presence of this or other seizure types should be
the primary consideration when considering the diagnosis of atypical childhood
epilepsy with centrotemporal spikes. Some authors have used the term atypical
childhood epilepsy with centrotemporal spikes to describe cases of typical childhood
CONTINUED FROM PAGE 346
Typical
age of Brain Genetic
Syndrome onset, years Seizure type(s) Treatment Prognosis EEG imaging causes
Panayiotopoulos 3-6 Focal aware May not need Few seizures Normal Normal Complex
syndrome seizures/focal to initiate (1/3 have background; inheritance
impaired medication; only one); interictal focal in vast
awareness most agents spontaneous spikes and majoritya
seizures with effective remission spike-wave
prominent within discharges
autonomic 2-4 years independently
features (eg, over right and/
vomiting, pallor) or left occipital
regions
Gastaut 7-10 Focal aware Most agents Seizures may Normal Normal Complex
syndrome seizures/focal can be be frequent; background inheritance
impaired effective majority have interictal focal in vast
awareness spontaneous spikes and majoritya
seizures with remission in spike-wave
visual 2-4 years discharges
hallucinations; independently
ictal blindness over right and/
and headache or left occipital
may occur regions;
fixation-off
sensitivity may
occur
a
If the syndrome occurs in the context of a family with genetic epilepsy with febrile seizures plus, genetic testing should be considered.
CONTINUUMJOURNAL.COM 347
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
GENETIC EPILEPSY SYNDROMES
KEY POINTS
● Roughly 50% to 80% of
patients with juvenile
absence epilepsy will also
experience generalized
tonic-clonic seizures.
● The seizure control
prognosis is poor in juvenile
absence epilepsy, with less
than half of patients seizure
free on medications after
2 years and nearly all having
seizure recurrence if
medication weaning is
attempted.
FIGURE 4-3
● Epilepsy with generalized Centrotemporal spikes. EEG of interictal centrotemporal spikes in a 9-year-old boy
tonic-clonic seizures alone with childhood epilepsy with centrotemporal spikes. Independent monomorphic focal
is a genetic generalized spike-wave discharges are seen over both the right and left centrotemporal regions (arrows).
epilepsy in which
generalized tonic-clonic
seizures are the only seizure
epilepsy with centrotemporal spikes in which seizures are more frequent and
type.
difficult to control or in which neuropsychological dysfunction is more
● Epilepsy with eyelid profound49; however, these patients are better considered to have unusual forms
myoclonias is a childhood- of typical childhood epilepsy with centrotemporal spikes, rather than a separate
onset genetic generalized electroclinical syndrome.
epilepsy classically
involving a triad of (1)
Age of seizure onset tends to be earlier than childhood epilepsy with
characteristic brief eye- centrotemporal spikes, usually between 2 and 6 years.48,50 Although seizures are
fluttering seizures (eyelid more difficult to control, patients will still usually have spontaneous resolution
myoclonia), (2) eye closure– before or during adolescence.50 Most antiseizure medications can be used;
induced seizures/
epileptiform abnormalities
however, there is the potential for seizure exacerbation with carbamazepine and
on EEG, and (3) other sodium channel antagonists.51 The likelihood of significant cognitive
photosensitivity. dysfunction is much greater than in childhood epilepsy with centrotemporal
spikes, more than 50% in some studies.50 Inheritance is probably still complex in
the majority of cases; however, pathogenic variants in GRIN2A and several other
genes have been associated, so genetic testing should be considered, especially if
family history is consistent with autosomal dominant inheritance.52-54
Panayiotopoulos Syndrome
In Panayiotopoulos syndrome, seizure onset is usually between 3 and 6 years
of age (range, 1 to 14 years).55 Seizures may be focal aware or focal impaired
awareness, usually occurring from sleep, with the most notable feature being
prominent autonomic symptoms. Vomiting, pallor, flushing, mydriasis/miosis,
and temperature changes are among the autonomic signs that may be seen.55
Lateral head and eye deviation may occur late in seizures, and progression to
bilateral tonic-clonic seizures is possible.55 Seizures are often prolonged, lasting
more than 30 minutes in nearly 44% of patients.55 Interictal EEG shows focal
spikes and spike-wave discharges, which are often abundant, over one or both
occipital regions (CASE 4-1).55 Children have cognitive function in the normal
range; however, full-scale IQ is significantly lower than in controls.56,57
Patients with Panayiotopoulos syndrome have spontaneous remission by
adolescence and usually few seizures; approximately one-third of children will
348 APRIL 2022
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
A 4-year-old girl presented to the emergency department with a prolonged CASE 4-1
seizure. Over the past 3 months, she had four episodes of unexplained
vomiting. The events had occurred soon after falling asleep and had been
associated with pallor, sweating, and dilated pupils. The duration was
estimated at 1 to 2 minutes, after which she went back to sleep. During the
events, she maintained at least partial awareness. However, with the event
on the day of presentation, she developed right-eye deviation and became
unresponsive. The event continued for 25 minutes and was aborted when
emergency medical personnel administered midazolam. She had no fever,
infectious symptoms, or recent trauma.
Her background history was mostly unremarkable. She was born after an
uncomplicated pregnancy and delivery at term. She had no medical issues,
and her developmental milestones had all been normal. Her family history
was significant only for a first cousin with childhood epilepsy with
centrotemporal spikes. Her EEG showed normal background activity, but
abundant high-amplitude focal monomorphic spike-wave discharges were
seen over the left occipital region (FIGURE 4-4).
She was diagnosed with Panayiotopoulos syndrome, and her parents were
counseled regarding seizure safety precautions. The treating neurologist
elected not to order brain imaging or genetic testing. The patient was
prescribed daily clobazam, as well as home intranasal midazolam to be
administered by the parents for any seizure lasting longer than 5 minutes. She
did not have any further seizures and was weaned off clobazam 2 years later.
FIGURE 4-4
EEG of interictal epileptiform discharges in the patient in CASE 4-1 with Panayiotopoulos
syndrome. Abundant monomorphic focal spike-wave discharges are seen over the left
occipital region (arrows).
This case illustrates that neuroimaging may not be necessary if the clinical COMMENT
and EEG findings are classic for a self-limited focal epilepsy of childhood.
In this case, the girl avoided exposure to a general anesthetic, which would
have been necessary to perform a brain MRI given her young age.
CONTINUUMJOURNAL.COM 349
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
GENETIC EPILEPSY SYNDROMES
have only one event.55 Thus, as with childhood epilepsy with centrotemporal
spikes, it is reasonable to reserve treatment at the time of diagnosis and prescribe
medications only for those with frequent seizures. Inheritance is almost always
complex, so genetic testing is generally not indicated in isolated cases without a
relevant family history.
Gastaut Syndrome
Gastaut syndrome (not to be confused with Lennox-Gastaut syndrome) is an
occipital epilepsy syndrome with electrographic features essentially
indistinguishable from Panayiotopoulos syndrome, but it has a very different
clinical presentation. Seizure onset is slightly later on average, most commonly
7 to 10 years of age (range, 3 to 16 years).58 Patients have focal aware seizures,
although awareness may become impaired late in events. The symptomatology
mostly involves visual hallucinations usually lasting 1 to 3 minutes. These are
most typically elementary visual phenomena such as multicolored circles, but
about 10% of patients can have complex hallucinations, such as faces or figures.58
Ictal blindness lasting several minutes is also commonly reported. Patients may
also have headache during or after seizures.58 EEG shows focal occipital spikes
and spike-wave discharges as in Panayiotopoulos syndrome, and fixation-off
sensitivity (the appearance of epileptiform abnormalities with removal of visual
fixation, often by eye closure) often occurs.58
Diagnosis may be delayed as patients can be mistakenly thought to have either
migraines or a psychiatric condition. Unlike Panayiotopoulos syndrome, no clear
difference in IQ is seen when comparing children with Gastaut syndrome and
healthy controls.57 Seizures are usually sufficiently frequent that antiseizure
medication should be prescribed. Few data are available for long-term prognosis,
but the majority likely have spontaneous seizure resolution in 2 to 4 years.58
SELF-LIMITED FAMILIAL NEONATAL AND INFANTILE EPILEPSY
Spontaneously resolving seizures may occur in the first 1 to 2 years of life. The
two most common syndromes fitting this description are self-limited neonatal
epilepsy and self-limited infantile epilepsy.
Self-Limited Neonatal Epilepsy
In self-limited familial neonatal epilepsy, seizures begin in the neonatal period,
usually on the second or third day of life.59,60 Seizures may involve any or all of
tonic posturing, apnea, vocalization, eye deviation, change in skin color, and
unilateral or bilateral clonic movements.59 Duration is typically brief, usually less
than 30 seconds.59 EEG is usually normal in the interictal period, although
focal interictal epileptiform abnormalities are reported in 25% of patients.59,61
Affected children have spontaneous resolution of seizures, occurring by 6 weeks
in two-thirds of cases and by 6 months in 94% of cases.59,61 Neurologic
examination is normal, as is development. If present, family history is consistent
with autosomal dominant inheritance. Genetic testing identifies a cause in more
than 90% of familial cases; the most common cause is pathogenic variants in
KCNQ2, but KCNQ3 and SCN2A are also associated.61
Self-Limited Infantile Epilepsy
Self-limited infantile epilepsy is usually defined as seizures occurring in
otherwise healthy and typically developing children, usually between the ages of
350 APRIL 2022
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
3 and 20 months.62 Family history is often positive, following an autosomal KEY POINTS
dominant pattern. In some familial cases, patients may have younger onset, and
● Children with childhood
an overlap syndrome termed self-limited familial neonatal-infantile seizures has epilepsy with centrotemporal
been proposed in the past.63 Patients have focal impaired awareness seizure, spikes first present with
often with hemiclonic movements, head and eye deviation, or facial/limb seizures typically between 7
automatisms. Seizures usually occur in clusters of up to 8 to 10 per day over 1 to and 10 years of age (range, 1 to
14 years), often from sleep.
3 days.62 Interictal EEG is usually normal, as is brain MRI.62
The seizure symptomatology
In familial cases, PRRT2 pathogenic variants are identified in more than 80% is focal aware or focal
of patients.64,65 Other associated genes include SCN2A, KCNQ2, and KCNQ3, impaired awareness, involving
although these are often the earlier-onset self-limited familial neonatal-infantile prominent hemifacial jerking
or dystonia, facial
seizure phenotype.63,66 Despite the self-limited course, patients are usually
paresthesia, drooling, and
treated with antiseizure medication because of the high seizure frequency during mumbling, and occasionally
clusters; most antiseizure agents should be effective.62 Seizures usually resolve progressing to bilateral tonic-
within 1 year of onset. clonic convulsions. EEG
shows focal monomorphic
medium-high amplitude
DEVELOPMENTAL AND EPILEPTIC ENCEPHALOPATHIES spikes and spike-wave
The 2017 ILAE epilepsy classification introduced the term developmental and discharges over one or both
epileptic encephalopathy to describe patients who have both epilepsy and centrotemporal regions,
developmental impairment, in whom the epileptic activity contributes to the having a characteristic
morphology and horizontal
degree of developmental impairment.10 In most cases, patients with dipole.
developmental and epileptic encephalopathy will have experienced
developmental regression at some point, often at the time of seizure onset or ● Decisions on whether to
worsening. Although many developmental and epileptic encephalopathies are initiate antiseizure
medication in childhood
genetic, most of the developmental and epileptic encephalopathy syndromes
epilepsy with
may occur as a result of other factors, including after brain injury early in life. centrotemporal spikes
Here, only the developmental and epileptic encephalopathy syndromes that should be made on a child-
occur solely due to genetic factors are discussed. Other developmental and by-child basis, taking into
consideration frequency
epileptic encephalopathies that are more etiologically heterogeneous such as
and duration of seizures, if
West syndrome and Lennox-Gastaut syndrome are discussed elsewhere; refer to seizures have progressed to
the articles “Evaluation of First Seizure and Newly Diagnosed Epilepsy” by bilateral tonic-clonic, as
Elaine Wirrell, MD, FRCP(C), FAAN,67 and “Seizures and Epilepsy in well as parent/caregiver
Childhood” by Maria Gogou, MD, PhD, and Judith Helen Cross, MBChB, PhD,68 concerns.
in this issue of Continuum. Also, many genes may produce a nonspecific ● In Panayiotopoulos
developmental and epileptic encephalopathy phenotype, but they are also not syndrome, seizure onset is
discussed here. usually between 3 and
6 years of age (range, 1 to
14 years). Seizures may be
Dravet Syndrome focal aware or focal
Dravet syndrome (previously known as severe myoclonic epilepsy of infancy) first impaired awareness, usually
presents around 6 months of age, usually with febrile seizures that are often occurring from sleep, with
hemiclonic and prolonged.69 Patients subsequently develop afebrile seizure types the most notable feature
being prominent autonomic
that most commonly include any or all of generalized tonic-clonic, focal impaired
symptoms. Vomiting, pallor,
awareness, atypical absences, and myoclonic seizures.69 Seizures are almost flushing, mydriasis/miosis,
always drug resistant, with the most effective treatments being clobazam, and temperature changes
valproic acid, topiramate, and stiripentol.69,70 More recent data support the use are among the autonomic
signs that may be seen.
of cannabidiol and fenfluramine.71,72 EEG is initially normal but eventually
Lateral head and eye
shows generalized or multifocal epileptiform abnormalities and background deviation may occur late in
slowing.69 Brain imaging is typically normal. seizures, and progression to
The underlying cause in 80% to 90% of cases of Dravet syndrome is a bilateral tonic-clonic
pathogenic variant in SCN1A; however, it is crucial to remember that other seizures is possible.
epilepsy phenotypes may be associated with SCN1A.73,74 Dravet syndrome is a
CONTINUUMJOURNAL.COM 351
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
GENETIC EPILEPSY SYNDROMES
clinical diagnosis and is not made by a positive SCN1A result. Development is
initially normal, with regression or plateau most commonly occurring in the
second year of life.69 The long-term developmental prognosis is highly variable;
all patients have some degree of intellectual disability, but this can range from
mild to profound. Dravet syndrome has a high rate of early mortality. The rate of
sudden unexpected death in epilepsy (SUDEP) is much higher than in other
forms of epilepsy, but individuals can also die by drowning or as a result of
massive cerebral edema developing after prolonged seizures.75,76
Myoclonic-Atonic Epilepsy
Myoclonic-atonic epilepsy (previously known as epilepsy with myoclonic-astatic
seizures and Doose syndrome) is considered a developmental and epileptic
encephalopathy, although the developmental course can be quite variable.77
Patients initially present with afebrile seizures and are between 1 and 6 years of
age, although a minority of patients have a preceding history of febrile
seizures.77,78 Myoclonic-atonic seizures are essential for diagnosis, although
patients may also have myoclonic, atonic, atypical absence, tonic, and
generalized tonic-clonic seizures.77,78 Nonconvulsive status epilepticus occurs in
a minority of patients.77,78 Many patients experience a “stormy phase” during
which the frequency of seizures is increased, development may deteriorate, and
EEG may show background slowing.77,78 Family history may be positive for
febrile seizures or other genetic epilepsy with febrile seizures plus (GEFS+)
phenotypes (discussed later in this article).
Genetic testing is negative in the majority of patients with myoclonic-atonic
epilepsy, and inheritance is probably complex in most. Even in monogenic cases,
the syndrome appears to be highly genetically heterogeneous, with pathogenic
variants in many genes reported to be causative. Some of the more commonly
reported include SLC6A1, SCN1A, and SLC2A1 (the gene for GLUT1 deficiency,
discussed earlier).79-82 Valproic acid and clobazam are the most commonly used
first-line antiseizure medications, but the ketogenic diet should be considered
early if patients do not respond to initial medical therapy.77,78 Seizures remit in at
least half of patients, generally within 5 years of onset.77,78 Of those with
complete remission, more than half are developmentally normal; the remainder
of patients typically have mild to moderate developmental impairment.77
Epilepsy of Infancy With Migrating Focal Seizures
Epilepsy of infancy with migrating focal seizures has a very characteristic seizure
symptomatology involving focal seizures with interhemispheric migration that
can be diagnosed either by clinical observation or EEG or both (FIGURE 4-5).
Seizure onset ranges from the first day of life to 6 months; in addition to the
migrating focal seizures, children may have epileptic spasms or tonic seizures, as
well.83 Interictal EEG may show focal/multifocal epileptiform discharges,
hypsarhythmia, or burst suppression.83 Although most patients have severe to
profound intellectual disability, milder phenotypes involving even normal
development can rarely occur.83
Genetic testing will be positive in the majority, although the condition is quite
genetically heterogeneous. Pathogenic variants in KCNT1 account for
approximately one-quarter of cases, followed by SCN2A in about 7%; however,
many other genes are associated, as well.83 Mortality is high, with at least one-
third of patients dying during childhood.83 Optimal treatment may depend on
352 APRIL 2022
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
● Status epilepticus is
common in Panayiotopoulos
syndrome, with nearly half
of patients having seizures
lasting longer than
30 minutes.
● Interictal EEG in patients
with Panayiotopoulos
syndrome shows focal
spikes and spike-wave
discharges, which are often
abundant, over one or both
occipital regions.
● Patients with Gastaut
syndrome have focal aware
FIGURE 4-5 seizures, although
Migrating focal seizure. EEG demonstrating migrating focal seizure in an 8-day-old girl with awareness may become
epilepsy of infancy with migrating focal seizures. The seizure starts in the right frontal region impaired late in events. The
and then migrates to the left frontal region. Note that the time scale is compressed. symptomatology mostly
involves visual
hallucinations usually lasting
the underlying genetic cause; those with SCN2A variants presenting before 1 to 3 minutes. These are
3 months of age will typically respond very well to sodium channel antagonists most typically elementary
visual phenomena such as
(eg, carbamazepine, oxcarbazepine, and lacosamide).84-86 Patients with KCNT1 multicolored circles, but
pathogenic variants may respond to quinidine; however, this is not universal, about 10% of patients can
and children should be carefully monitored for cardiac arrhythmias when the have complex
medication is initiated.87-90 hallucinations, such as faces
or figures. Ictal blindness
lasting several minutes is
PROGRESSIVE MYOCLONUS EPILEPSIES also commonly reported.
The progressive myoclonus epilepsies are a clinically and genetically
● EEG in patients with
heterogeneous group of disorders that share the common features of myoclonic Gastaut syndrome shows
seizures and progressive neurologic decline.91 Age of onset is typically in focal occipital spikes and
childhood or adolescence, and patients may have additional seizure types spike-wave discharges as in
including focal, atypical absence, atonic, and generalized tonic-clonic. Panayiotopoulos syndrome,
and fixation-off sensitivity
Photosensitive seizures, which may be noted on EEG, are a common feature in (the appearance of
several of the forms.91 epileptiform abnormalities
Depending on the underlying cause, patients may have other neurologic with removal of visual
features, including ataxia, dysarthria, vision loss, hearing loss, neuropathy, and fixation, often by eye
closure) often occurs.
myopathy. Historically, ophthalmologic examination (to identify cherry-red
spot) and skin biopsy were universally indicated as part of the diagnostic ● Children with Gastaut
workup; however, a gene panel is now often sufficient to determine the syndrome may be
molecular cause. In most cases, the underlying genetic cause occurs via misdiagnosed with migraines
or psychiatric disorders as
autosomal recessive inheritance; however, mitochondrial and autosomal
they present with visual
dominant forms exist.91,92 TABLE 4-3 summarizes the more studied forms of hallucinations, sometimes
genetic progressive myoclonus epilepsies. with associated headache.
SLEEP-RELATED HYPERMOTOR EPILEPSY
Sleep-related hypermotor epilepsy (previously known as nocturnal frontal lobe
epilepsy) is a form of focal epilepsy involving seizures that usually occur
exclusively from sleep. Seizures usually arise from the frontal lobe; however,
CONTINUUMJOURNAL.COM 353
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
GENETIC EPILEPSY SYNDROMES
TABLE 4-3 Progressive Myoclonus Epilepsy
Other seizure
types that may Additional features
Disease Gene(s) Inheritance Age of onset occur that may be seen Prognosis
Lafora body EPM2A, Autosomal 14-16 years Generalized Dysarthria, ataxia, Death usually
disease NHLRC1 recessive (range, tonic-clonic, spasticity within
8-19 years) atypical 10 years of
absences, onset
atonic, focal
impaired
awareness
seizure
(transient
blindness or
visual
hallucinations)
Unverricht- CSTB Autosomal 6-15 years Generalized Ataxia Life
Lundborg recessive tonic-clonic expectancy
disease decreased,
but patients
usually live to
at least
40 years
Myoclonic MT-TK in Mitochondrial Childhood to Atonic, focal Myopathy, migrainous Variable
epilepsy with >90%; adulthood clonic, headaches, hearing
ragged red others: generalized loss, peripheral
fibers (MERRF) MT-TF, tonic-clonic, neuropathy, psychiatric
MT-TH, myoclonic- illness
MT-TI, atonic,
MT-TL1, absences,
MT-TP, myoclonic-
MT-TS1, absences
MT-TS2
Neuronal PPT1, TPP1, Autosomal Variable Generalized Retinopathy (may have Variable
ceroid DNAJC5, recessive tonic-clonic, cherry-red spot), vision
lipofuscinoses MFSD8, (rarely focal impaired loss, ataxia
CTSD, autosomal awareness
GRN, dominant) seizure
ATP13A2,
CTSF,
KCTD7
CONTINUED ON PAGE 355
354 APRIL 2022
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
CONTINUED FROM PAGE 354
Other seizure
types that may Additional features
Disease Gene(s) Inheritance Age of onset occur that may be seen Prognosis
Action SCARB2 Autosomal Late Generalized Tremor, peripheral Variable
myoclonus- recessive adolescence clonic-tonic- neuropathy, dysarthria,
renal failure to adulthood clonic ataxia, sensorineural
syndrome hearing loss,
proteinuria/nephrotic
syndrome/renal failure
Myoclonus KCNC1 Autosomal 3-15 years Generalized Ataxia, clinical Mild
epilepsy and dominant tonic-clonic improvement with fever cognitive
ataxia due to decline in
potassium 50%
mutation
Sialidosis type I NEU1 Autosomal Infancy to Focal, bilateral Retinopathy (cherry-red Variable
and type II recessive third decade tonic-clonic spot), vision loss, ataxia,
of life coarse features,
hepatosplenomegaly,
dysostosis multiplex,
hearing loss, hernias
Gaucher GBA Autosomal Childhood to Generalized Ophthalmoplegia, Death often
disease, type III recessive adolescence tonic-clonic ataxia, spasticity, within
neuronopathic dementia, growth several years
retardation, delayed of onset
puberty,
hepatosplenomegaly,
bone abnormalities
Dentatorubral- ATN1 Autosomal <12 months to Generalized Ataxia Progressive
pallidoluysian dominant 19 years tonic-clonic, decline
atrophy (CAG repeat tonic, atonic,
expansion) clonic
North Sea GOSR2 Autosomal 2-8 years Generalized Ataxia (precedes Cognitive
progressive recessive tonic-clonic, myoclonus), dysarthria, function
myoclonus absences areflexia, scoliosis relatively
epilepsy spared;
assistance
required with
activities of
daily living
CONTINUUMJOURNAL.COM 355
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
GENETIC EPILEPSY SYNDROMES
extrafrontal onset with spread to the frontal regions can produce the same
phenotype.93 The seizure symptomatology typically involves hypermotor
behaviors such as violent thrashing and writhing, often with vocalization and
emotional facial expression.93 Tonic and dystonic features are often seen, as well.
Seizures are usually frequent, often occurring several times per night. A clear
ictal rhythm is rarely seen on EEG, which may show only artifacts from muscle
and movement.93 Interictal EEG is usually normal, and the clinical presentation
can be easily confused with parasomnias or nonepileptic seizures, so inpatient
video-EEG recording is often essential to confirming the diagnosis. Treatment
with most standard antiseizure medications is appropriate, although patients are
often drug resistant.
A family history suggestive of autosomal dominant inheritance is present in
some patients with sleep-related hypermotor epilepsy. Pathogenic variants in
acetylcholine receptor subunit genes (CHRNA4, CHRNB2, CHRNA2) are
the most common identified causes of autosomal dominant sleep-related
hypermotor epilepsy.94-96 Pathogenic variants in KCNT1 can also produce
autosomal dominant sleep-related hypermotor epilepsy, but these are often de
novo, and patients usually have more severe comorbid neuropsychiatric
disturbance.97 Lastly, some evidence has been shown that pathogenic variants
in CRH are causative in some families.98
Pathogenic variants in mammalian target of rapamycin (mTOR) regulatory
genes (ie, DEPDC5, NPRL2, NPRL3) may also cause sleep-related hypermotor
epilepsy; however, these families more commonly have familial focal epilepsy
with variable foci (discussed later in this article) in which a variety of phenotypes
that may or may not include sleep-related hypermotor epilepsy are seen. For
patients in this group who are drug resistant or those with negative genetic
testing, a thorough workup should be undertaken to investigate if they have a
surgically remediable lesion such as a focal cortical dysplasia.
PHOTOSENSITIVE OCCIPITAL LOBE EPILEPSY
Photosensitive occipital lobe epilepsy (formerly known as idiopathic
photosensitive occipital epilepsy) is an epilepsy syndrome in which photosensitivity
is a hallmark feature. The classic seizures involve simple, colorful visual auras
that often progress to conscious tonic lateral head and eye version.99 Seizure
onset can be from childhood to adolescence (range, 5 to 17 years of age).99 EEG
shows occipital spikes or spike wave, although centrotemporal spikes may also
occur.99 Intelligence is usually in the normal range. The clinical features of
photosensitive occipital lobe epilepsy may overlap with other epilepsy
syndromes, including JME, epilepsy with eyelid myoclonias, and Gastaut
syndrome.99-101 Presently, no genes are clearly associated with the classical
phenotype, and inheritance is presumed to be complex in most cases.
FOCAL EPILEPSY WITH AUDITORY FEATURES
Epilepsy with auditory features is an epilepsy syndrome characterized by focal
aware seizures localized to the lateral temporal region. Patients experience
seizures involving simple or complex auditory hallucinations, and 86% of
patients have focal-to-bilateral tonic-clonic seizures.102 Patients may report that
loud sounds or noise can provoke seizures. Some patients may also experience an
aura of receptive or global aphasia. Seizure onset is usually in adolescence, but a
range from 0.5 to 57 years has been reported.102 At least one-third of patients are
356 APRIL 2022
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
drug resistant, and although seizures can eventually remit, this may not occur KEY POINTS
until decades after onset.102 Intelligence is usually normal. Interictal EEG is
● In self-limited familial
normal in two-thirds of patients, and ictal EEG may not show abnormalities with neonatal epilepsy, seizures
the auditory phenomena alone.102 The differential diagnosis includes migraine begin in the neonatal period,
variants and psychiatric disorders, so inpatient video-EEG monitoring may be usually on the second or
necessary to confirm the diagnosis. third day of life. Seizures
may involve any or all of
Family history may suggest autosomal dominant inheritance, although genetic
tonic posturing, apnea,
testing is positive in only 5% and 15% of sporadic and familial cases, vocalization, eye deviation,
respectively.103 Pathogenic variants in LGI1, RELN, MICAL1, SCN1A, and change in skin color, and
DEPDC5 have all been associated.104-108 unilateral or bilateral clonic
movements. Duration is
typically brief, usually less
FAMILIAL SYNDROMES WITH VARIABLE PHENOTYPES than 30 seconds.
When obtaining a family history, it is not uncommon to identify other
individuals who may have experienced seizures, but with apparently different ● Affected children with
phenotypes from the proband the neurologist is seeing. This history may still be self-limited neonatal
epilepsy have spontaneous
very relevant because in two main familial epilepsy syndromes affected family resolution of seizures,
members may have a range of epilepsy syndromic phenotypes. occurring by 6 weeks in two-
thirds of cases and by
Genetic Epilepsy With Febrile Seizures Plus 6 months in 94% of cases.
GEFS+ (previously known as generalized epilepsy with febrile seizures plus) is a
● Self-limited infantile
familial syndrome in which autosomal dominant or complex inheritance patterns epilepsy is usually defined
are most commonly seen.109,110 The most frequent epilepsy phenotypes are as seizures occurring in
febrile seizures and febrile seizures plus111; the latter refers to patients with otherwise healthy and
typically developing
febrile and afebrile generalized tonic-clonic seizures or in whom febrile seizures
children, usually between
continue outside the usual age range (ie, after 6 years).109 However, many other the ages of 3 and 20 months.
epilepsy phenotypes may occur within families, most commonly including
genetic generalized epilepsies, focal epilepsy without preceding febrile seizures, ● Patients with self-limited
and the developmental and epileptic encephalopathies, Dravet syndrome, and infantile epilepsy have focal
impaired awareness seizure,
myoclonic-atonic epilepsy.111 often with hemiclonic
A family with GEFS+ has been defined as having two or more individuals with movements, head and eye
a GEFS+ spectrum phenotype, at least one of which is febrile seizures plus, or, if deviation, or facial/limb
no individuals have febrile seizures plus, at least three individuals have other automatisms. Seizures
usually occur in clusters of
classic GEFS+ phenotypes (eg, febrile seizures or myoclonic-atonic epilepsy).111 up to 8 to 10 per day over 1 to
An example pedigree is shown in FIGURE 4-6A. Notably, a family in which the only 3 days.
phenotype seen is febrile seizures would not be considered GEFS+ but instead
classified as familial febrile seizures.111 Although complex inheritance likely ● Dravet syndrome first
presents around 6 months of
accounts for the majority of families with GEFS+, a monogenic cause (usually
age, usually with febrile
autosomal dominant) is identified in up to one-third.111 The most commonly seizures that are often
associated genes are SCN1A, SCN1B, SCN2A, SCN9A, GABRG2, and STX1B.111 hemiclonic and prolonged.
Patients subsequently
Familial Focal Epilepsy With Variable Foci develop afebrile seizure
types that most commonly
Familial focal epilepsy with variable foci is an autosomal dominant familial include any or all of
syndrome in which all affected members have focal epilepsy but with different generalized tonic-clonic,
seizure types.112 For example, a woman with temporal lobe epilepsy might give focal impaired awareness,
birth to two children, one of whom has sleep-related hypermotor epilepsy and atypical absences, and
myoclonic seizures.
the other occipital epilepsy. An example pedigree is shown in FIGURE 4-6B.
Affected patients may have normal brain MRI or may show signs of
malformations, namely focal cortical dysplasia.
The underlying genetics have thus far all involved genes related to the mTOR
pathway. Pathogenic variants in DEPDC5, NPRL2, and NPRL3 have all been
CONTINUUMJOURNAL.COM 357
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
GENETIC EPILEPSY SYNDROMES
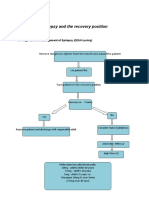
FIGURE 4-6
Pedigrees for familial epilepsy syndromes. Example pedigrees for genetic epilepsy with
febrile seizures plus (A) and familial focal epilepsy with variable foci (B).
CAE = childhood absence epilepsy; FS = febrile seizures; FS + = febrile seizures plus; MAE = myoclonic-
atonic epilepsy; SHE = sleep-related hypermotor epilepsy; TLE = temporal lobe epilepsy.
associated.113-115 These genes encode subunits of the GATOR1 complex, an
inhibitor of mTOR.116
CONCLUSION
Many genetic epilepsy syndromes have been identified for individuals, as well as
two main familial syndromes. A neurologist’s ability to recognize these
syndromes is crucial to allow for appropriate investigation, including the need
for neuroimaging and molecular genetic testing. Regarding the latter, the yield of
genetic testing will be much higher in certain syndromes (eg, severe early-onset
developmental and epileptic encephalopathies such as Dravet syndrome)
compared with others (eg, self-limited focal epilepsy of childhood and genetic
generalized epilepsy). Accurate identification of genetic epilepsy syndromes also
allows for proper counseling of patients and their families regarding prognosis
and risk for comorbidities such as developmental impairment and SUDEP.
REFERENCES
1 Lennox WG. The genetics of epilepsy. Am J 4 Peljto AL, Barker-Cummings C, Vasoli VM, et al.
Psychiatry 1947;103(4):457-462. doi:10.1176/ Familial risk of epilepsy: a population-based
ajp.103.4.457 study. Brain 2014;137(pt 3):795-805. doi:10.1093/
brain/awt368
2 Hemminki K, Li X, Johansson SE, et al. Familial risks
for epilepsy among siblings based on 5 Berkovic SF, Howell RA, Hay DA, Hopper JL.
hospitalizations in Sweden. Neuroepidemiology Epilepsies in twins: genetics of the major
2006;27(2):67-73. doi:10.1159/000094976 epilepsy syndromes. Ann Neurol 1998;43(4):
435-445. doi:10.1002/ana.410430405
3 Annegers JF, Hauser WA, Anderson VE, Kurland
LT. The risks of seizure disorders among relatives 6 Vadlamudi L, Milne RL, Lawrence K, et al.
of patients with childhood onset epilepsy. Genetics of epilepsy: the testimony of twins in
Neurology 1982;32(2):174-179. doi:10.1212/ the molecular era. Neurology 2014;83(12):
wnl.32.2.174 1042-1048. doi:10.1212/WNL.0000000000000790
358 APRIL 2022
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
7 Kjeldsen MJ, Kyvik KO, Christensen K, Friis ML. 21 Suls A, Mullen SA, Weber YG, et al. Early-onset KEY POINTS
Genetic and environmental factors in epilepsy: absence epilepsy caused by mutations in the
a population-based study of 11900 Danish twin glucose transporter GLUT1. Ann Neurol 2009;
pairs. Epilepsy Res 2001;44(2-3):167-178. 66(3):415-419. doi:10.1002/ana.21724
● Early mortality risk is high
doi:10.1016/s0920-1211(01)00196-6 in Dravet syndrome, with
22 Wang D, Pascual JM, De Vivo D, Glucose death most commonly
8 Kjeldsen MJ, Corey LA, Solaas MH, et al. Genetic transporter type 1 deficiency syndrome. In: Adam occurring due to sudden
factors in seizures: a population-based study of MP, Ardinger HH, Pagon RA, et al, editors.
unexpected death in
47,626 US, Norwegian and Danish twin pairs. Twin GeneReviews. University of Washington,
Res Hum Genet 2005;8(2):138-147. doi:10.1375/ Seattle, 1993.
epilepsy (SUDEP), drowning,
1832427053738836 or massive cerebral edema
23 Gesche J, Christensen J, Hjalgrim H, et al. following prolonged
9 Klassen T, Davis C, Goldman A, et al. Exome Epidemiology and outcome of idiopathic seizures.
sequencing of ion channel genes reveals generalized epilepsy in adults. Eur J Neurol 2020;
complex profiles confounding personal risk 27(4):676-684. doi:10.1111/ene.14142
assessment in epilepsy. Cell 2011;145(7): ● Myoclonic-atonic
24 Kasteleijn-Nolst Trenite DGA, Schmitz B, Janz D, epilepsy is considered a
1036-1048. doi:10.1016/j.cell.2011.05.025
et al. Consensus on diagnosis and management developmental and
10 Scheffer IE, Berkovic S, Capovilla G, et al. ILAE of JME: from founder's observations to current
epileptic encephalopathy,
classification of the epilepsies: position paper of trends. Epilepsy Behav 2013;28(suppl 1):S87-S90.
although the developmental
the ILAE Commission for Classification and doi:10.1016/j.yebeh.2012.11.051
Terminology. Epilepsia 2017;58(4):512-521. course can be quite variable.
25 Leahy T, Hennessy MJ, Counihan TJ. The
doi:10.1111/epi.13709
“Cinderella Syndrome”: a narrative study of ● Epilepsy of infancy with
11 Mullen SA, Berkovic SF; ILAE Genetics social curfews and lifestyle restrictions in
migrating focal seizures has
Commission. Genetic generalized epilepsies. juvenile myoclonic epilepsy. Epilepsy Behav
Epilepsia 2018;59(6):1148-1153. doi:10.1111/epi.14042 2018;78:104-108. doi:10.1016/j.yebeh.2017.10.024
a very characteristic seizure
symptomatology involving
12 Olsson I. Epidemiology of absence epilepsy. I. 26 Crespel A, Gelisse P, Reed RC, et al. Management focal seizures with
Concept and incidence. Acta Paediatr Scand of juvenile myoclonic epilepsy. Epilepsy Behav interhemispheric migration
1988;77(6):860-866. doi:10.1111/j.1651-2227.1988. 2013;28(suppl 1):S81-S86. doi:10.1016/
that can be diagnosed either
tb10769.x j.yebeh.2013.01.001
by clinical observation or
13 Juul-Jensen P, Foldspang A. Natural history of 27 Silvennoinen K, de Lange N, Zagaglia S, et al. EEG or both.
epileptic seizures. Epilepsia 1983;24(3):297-312. Comparative effectiveness of antiepileptic
doi:10.1111/j.1528-1157.1983.tb04893.x drugs in juvenile myoclonic epilepsy. Epilepsia
● The progressive
Open 2019;4(3):420-430. doi:10.1002/epi4.12349
14 Guerrini R, Sanchez-Carpintero R, Deonna T, et al. myoclonus epilepsies are a
Early-onset absence epilepsy and paroxysmal 28 Healy L, Moran M, Singhal S, et al. Relapse after clinically and genetically
dyskinesia. Epilepsia 2002;43(10):1224-1229. treatment withdrawal of antiepileptic drugs for heterogeneous group of
doi:10.1046/j.1528-1157.2002.13802.x juvenile absence epilepsy and juvenile myoclonic disorders that share the
epilepsy. Seizure 2018;59:116-122. doi:10.1016/j.
15 Waaler PE, Blom BH, Skeidsvoll H, Mykletun A. common features of
seizure.2018.05.015
Prevalence, classification, and severity of myoclonic seizures and
epilepsy in children in western Norway. Epilepsia 29 Cossette P, Liu L, Brisebois K, et al. Mutation of progressive neurologic
2000;41(7):802-810. doi:10.1111/j.1528-1157.2000. GABRA1 in an autosomal dominant form of decline. Age of onset is
tb00246.x juvenile myoclonic epilepsy. Nat Genet 2002; typically in childhood or
31(2):184-189. doi:10.1038/ng885
16 Sadleir LG, Farrell K, Smith S, et al. Electroclinical adolescence, and patients
features of absence seizures in childhood 30 Tovia E, Goldberg-Stern H, Shahar E, Kramer U. may have additional seizure
absence epilepsy. Neurology 2006;67(3):413-418. Outcome of children with juvenile absence types including focal,
doi:10.1212/01.wnl.0000228257.60184.82 epilepsy. J Child Neurol 2006;21(9):766-768. atypical absence, atonic,
doi:10.1177/08830738060210092101 and generalized tonic-
17 Matricardi S, Verrotti A, Chiarelli F, et al. Current
advances in childhood absence epilepsy. 31 Guerrini R, Marini C, Barba C. Generalized clonic.
Pediatr Neurol 2014;50(3):205-212. doi:10.1016/ epilepsies. Handb Clin Neurol 2019;161:3-15.
j.pediatrneurol.2013.10.009 doi:10.1016/B978-0-444-64142-7.00038-2 ● Sleep-related
18 Glauser TA, Cnaan A, Shinnar S, et al. 32 Caraballo R, Silva S, Beltran L, et al. Childhood- hypermotor epilepsy is a
Ethosuximide, valproic acid, and lamotrigine in only epilepsy with generalized tonic-clonic form of focal epilepsy
childhood absence epilepsy. N Engl J Med 2010; seizures: a well-defined epileptic syndrome. involving seizures that
362(9):790-799. doi:10.1056/NEJMoa0902014 Epilepsy Res 2019;153:28-33. doi:10.1016/j. usually occur exclusively
eplepsyres.2019.03.017 from sleep. Seizures usually
19 Callenbach PMC, Bouma PAD, Geerts AT, et al.
Long-term outcome of childhood absence 33 Unterberger I, Trinka E, Luef G, Bauer G. arise from the frontal lobe;
epilepsy: Dutch Study of Epilepsy in Childhood. Idiopathic generalized epilepsies with pure grand however, extrafrontal onset
Epilepsy Res 2009;83(2-3):249-256. doi:10.1016/ mal: clinical data and genetics. Epilepsy Res 2001; with spread to the frontal
j.eplepsyres.2008.11.011 44(1):19-25. doi:10.1016/s0920-1211(00)00210-2 regions can produce the
20 Shinnar S, Cnaan A, Hu F, et al. Long-term 34 Nilo A, Crespel A, Genton P, et al. Epilepsy with same phenotype.
outcomes of generalized tonic-clonic seizures in eyelid myoclonias (Jeavons syndrome): an
a childhood absence epilepsy trial. Neurology electro-clinical study of 40 patients from
2015;85(13):1108-1114. doi:10.1212/WNL. childhood to adulthood. Seizure 2021;87:30-38.
0000000000001971 doi:10.1016/j.seizure.2021.02.028
CONTINUUMJOURNAL.COM 359
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
GENETIC EPILEPSY SYNDROMES
35 Jeavons PM. Nosological problems of myoclonic 48 Aicardi J, Chevrie JJ. Atypical benign partial
epilepsies in childhood and adolescence. epilepsy of childhood. Dev Med Child Neurol
Dev Med Child Neurol 1977;19(1):3-8. doi:10.1111/ 1982;24(3):281-292. doi:10.1111/j.1469-8749.1982.
j.1469-8749.1977.tb08014.x tb13620.x
36 Smith KM, Youssef PE, Wirrell EC, et al. Jeavons 49 Parisi P, Paolino MC, Raucci U, et al. “Atypical
syndrome: clinical features and response to forms” of benign epilepsy with centrotemporal
treatment. Pediatr Neurol 2018;86:46-51. spikes (BECTS): how to diagnose and guide these
doi:10.1016/j.pediatrneurol.2018.06.001 children. A practical/scientific approach.
Epilepsy Behav 2017;75:165-169. doi:10.1016/
37 Marini C, Romoli M, Parrini E, et al. Clinical
j.yebeh.2017.08.001
features and outcome of 6 new patients carrying
de novo KCNB1 gene mutations. Neurol Genet 50 Hahn A. Atypical benign partial epilepsy/
2017;3(6):e206. doi:10.1212/ pseudo-Lennox syndrome. Epileptic Disord
NXG.0000000000000206 2000;2(suppl 1):S11-S17.
38 Vlaskamp DRM, Shaw BJ, Burgess R, et al. 51 Yang Z, Liu X, Qin J, et al. A study on epileptic
SYNGAP1 encephalopathy: a distinctive negative myoclonus in atypical benign partial
generalized developmental and epileptic epilepsy of childhood. Brain Dev 2009;31(4):
encephalopathy. Neurology 2019;92(2):e96-e107. 274-281. doi:10.1016/j.braindev.2008.04.004
doi:10.1212/WNL.0000000000006729
52 Carvill GL, Regan BM, Yendle SC, et al. GRIN2A
39 Thomas RH, Zhang LM, Carvill GL, et al. CHD2 mutations cause epilepsy-aphasia spectrum
myoclonic encephalopathy is frequently disorders. Nat Genet 2013;45(9):1073-1076.
associated with self-induced seizures. doi:10.1038/ng.2727
Neurology 2015;84(9):951-958. doi:10.1212/WNL.
53 Lemke JR, Lal D, Reinthaler EM, et al. Mutations in
0000000000001305
GRIN2A cause idiopathic focal epilepsy with
40 Dalla Bernardina B, Sgro V, Fejerman N. Epilepsy rolandic spikes. Nat Genet 2013;45(9):1067-1072.
with centro-temporal spikes and related doi:10.1038/ng.2728
syndromes. In: Roger J, Bureau M, Dravet C, et al,
54 Rudolf G, de Bellescize J, de Saint Martin A, et al.
editors. Epileptic syndromes in infancy,
Exome sequencing in 57 patients with self-
childhood and adolescence. John Libbey
limited focal epilepsies of childhood with typical
Eurotex Ltd, 2005:203-225.
or atypical presentations suggests novel
41 Hughes JR. Benign epilepsy of childhood with candidate genes. Eur J Paediatr Neurol 2020;27:
centrotemporal spikes (BECTS): to treat or not to 104-110. doi:10.1016/j.ejpn.2020.05.003
treat, that is the question. Epilepsy Behav 2010;
55 Ferrie C, Caraballo R, Covanis A, et al.
19(3):197-203. doi:10.1016/j.yebeh.2010.07.018
Panayiotopoulos syndrome: a consensus view.
42 Ebus SCM, Overvliet GM, Arends JBAM, Dev Med Child Neurol 2006;48(3):236-240.
Aldenkamp AP. Reading performance in children doi:10.1017/S0012162206000508
with rolandic epilepsy correlates with nocturnal
56 Fonseca Wald ELA, Debeij-Van Hall MHJA, De
epileptiform activity, but not with epileptiform
Jong E, et al. Neurocognitive and behavioural
activity while awake. Epilepsy Behav 2011;22(33):
profile in Panayiotopoulos syndrome. Dev Med
518-522. doi:10.1016/j.yebeh.2011.08.008
Child Neurol 2020;62(8):985-992. doi:10.1111/
43 Northcott E, Connolly AM, Berroya A, et al. The dmcn.14417
neuropsychological and language profile of
57 Akca Kalem S, Elmali AD, Demirbilek V, et al.
children with benign rolandic epilepsy. Epilepsia
Panayiotopoulos syndrome and Gastaut
2005;46(6):924-930. doi:10.1111/j.1528-1167.
syndrome are distinct entities in terms of
2005.62304.x
neuropsychological findings. Epilepsy Behav
44 Piccinelli P, Borgatti R, Aldini A, et al. Academic 2019;99:106447. doi:10.1016/j.yebeh.2019.106447
performance in children with rolandic epilepsy.
58 Caraballo R, Koutroumanidis M, Panayiotopoulos
Dev Med Child Neurol 2008;50(5):353-356. doi:
CP, et al. Idiopathic childhood occipital epilepsy
10.1111/j.1469-8749.2007.02040.x
of Gastaut: a review and differentiation from
45 Staden U, Isaacs E, Boyd SG, et al. Language migraine and other epilepsies. J Child Neurol
dysfunction in children with Rolandic epilepsy. 2009;24(12):1536-1542. doi:10.1177/
Neuropediatrics 1998;29(5):242-248. doi:10.1055/ 0883073809332395
s-2007-973569
59 Ronen GM, Rosales TO, Connolly M, et al. Seizure
46 Vears DF, Tsai MH, Sadleir LG, et al. Clinical characteristics in chromosome 20 benign familial
genetic studies in benign childhood epilepsy neonatal convulsions. Neurology 1993;43(7):
with centrotemporal spikes. Epilepsia 2012;53(2): 1355-1360. doi:10.1212/wnl.43.7.1355
319-324. doi:10.1111/j.1528-1167.2011.03368.x
60 Pettit RE, Fenichel GM. Benign familial neonatal
47 Bobbili DR, Lal D, May P, et al. Exome-wide seizures. Arch Neurol 1980;37(1):47-48.
analysis of mutational burden in patients with doi:10.1001/archneur.1980.00500500077012
typical and atypical Rolandic epilepsy. Eur J Hum
Genet 2018;26(2):258-264. doi:10.1038/
s41431-017-0034-x
360 APRIL 2022
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
61 Grinton BE, Heron SE, Pelekanos JT, et al. Familial 76 Cooper MS, McIntosh A, Crompton DE, et al. KEY POINTS
neonatal seizures in 36 families: clinical and Mortality in Dravet syndrome. Epilepsy Res 2016;
genetic features correlate with outcome. 128:43-47. doi:10.1016/j.eplepsyres.2016.10.006
Epilepsia 2015;56(7):1071-1080. doi:10.1111/epi.13020
● The seizure
77 Joshi C, Nickels K, Demarest S, et al. Results of an symptomatology in sleep-
62 Vigevano F. Benign familial infantile seizures. international Delphi consensus in epilepsy with related hypermotor epilepsy
Brain Dev 2005;27(3):172-177. doi:10.1016/j. myoclonic atonic seizures/Doose syndrome. typically involves
braindev.2003.12.012 Seizure 2021;85:12-18. doi:10.1016/j.seizure.2020.11.017
hypermotor behaviors such
63 Heron SE, Crossland KM, Andermann E, et al. 78 Nickels K, Kossoff EH, Eschbach K, Joshi C. as violent thrashing and
Sodium-channel defects in benign familial Epilepsy with myoclonic-atonic seizures (Doose writhing, often with
neonatal-infantile seizures. Lancet 2002; syndrome): clarification of diagnosis and vocalization and emotional
360(9336):851-852. doi:10.1016/S0140-6736(02) treatment options through a large retrospective facial expression.
09968-3 multicenter cohort. Epilepsia 2021;62(1):120-127.
doi:10.1111/epi.16752
64 Heron SE, Grinton BE, Kivity S, et al. PRRT2 ● In photosensitive
mutations cause benign familial infantile epilepsy 79 Tang S, Addis L, Smith A, et al. Phenotypic and occipital lobe epilepsy, the
and infantile convulsions with choreoathetosis genetic spectrum of epilepsy with myoclonic classic seizure
syndrome. Am J Hum Genet 2012;90(1):152-160. atonic seizures. Epilepsia 2020;61(5):995-1007.
symptomatology is of a
doi:10.1016/j.ajhg.2011.12.003 doi:10.1111/epi.16508
colorful visual aura that may
65 Ono S, Yoshiura K, Kinoshita A, et al. Mutations in 80 Carvill GL, McMahon JM, Schneider A, et al. evolve into lateral head and
PRRT2 responsible for paroxysmal kinesigenic Mutations in the GABA transporter SLC6A1 cause eye version; the patient may
dyskinesias also cause benign familial infantile epilepsy with myoclonic-atonic seizures. Am J maintain awareness
convulsions. J Hum Genet 2012;57(5):338-341. Hum Genet 2015;96(5):808-815. doi:10.1016/j.ajhg.
throughout.
doi:10.1038/jhg.2012.23 2015.02.016
66 Zara F, Specchio N, Striano P, et al. Genetic 81 Routier L, Verny F, Barcia G, et al. Exome ● Epilepsy with auditory
testing in benign familial epilepsies of the first sequencing findings in 27 patients with features is an epilepsy
year of life: clinical and diagnostic significance. myoclonic-atonic epilepsy: is there a major syndrome characterized by
Epilepsia 2013;54(3):425-436. doi:10.1111/epi.12089 genetic factor? Clin Genet 2019;96(3):254-260.
focal aware seizures
doi:10.1111/cge.13581
67 Wirrell E. The evaluation of first seizure and newly localized to the lateral
diagnosed epilepsy. Continuum (Minneap Minn) 82 Hinokuma N, Nakashima M, Asai H, et al. Clinical temporal region. Patients
2022;28(2, Epilepsy):230-260. and genetic characteristics of patients with experience seizures
Doose syndrome. Epilepsia Open 2020;5(3): involving simple or complex
68 Gogou M, Cross JH. Seizures and epilepsy in
442-450. doi:10.1002/epi4.12417
childhood. Continuum (Minneap Minn) 2022; auditory hallucinations, and
28(2, Epilepsy):428-456. 83 Burgess R, Wang S, McTague A, et al. The genetic 86% of patients have focal-
landscape of epilepsy of infancy with migrating to-bilateral tonic-clonic
69 Dravet C. The core Dravet syndrome phenotype.
focal seizures. Ann Neurol 2019;86(6):821-831. doi: seizures.
Epilepsia 2011;52(suppl 2):3-9. doi:10.1111/j.1528-
10.1002/ana.25619
1167.2011.02994.x
84 Foster LA, Johnson MR, MacDonald JT, et al. ● Genetic epilepsy with
70 Chiron C, Dulac O. The pharmacologic treatment
Infantile epileptic encephalopathy associated febrile seizures plus is a
of Dravet syndrome. Epilepsia 2011;52(suppl 2):
with SCN2A mutation responsive to oral familial syndrome in which
72-75. doi:10.1111/j.1528-1167.2011.03007.x
mexiletine. Pediatr Neurol 2017;66:108-111. members of the same family
71 Devinsky O, Cross JH, Laux L, et al. Trial of doi:10.1016/j.pediatrneurol.2016.10.008
have different phenotypes,
cannabidiol for drug-resistant seizures in the
85 Flor-Hirsch H, Heyman E, Livneh A, et al. the most common being
Dravet syndrome. N Engl J Med 2017;376:
Lacosamide for SCN2A-related intractable febrile seizures and febrile
2011-2020. doi:10.1056/NEJMoa1611618
neonatal and infantile seizures. Epileptic Disord seizures plus (febrile
72 Lagae L, Sullivan J, Knupp K, et al. Fenfluramine 2018;20(5):440-446. doi:10.1684/epd.2018.1001 seizures outside the usual
hydrochloride for the treatment of seizures in age range or bilateral tonic-
86 Wolff M, Johannesen KM, Hedrich UBS, et al.
Dravet syndrome: a randomised, double-blind,
Genetic and phenotypic heterogeneity suggest clonic seizures occurring
placebo-controlled trial. Lancet 2019;394(10216):
therapeutic implications in SCN2A-related with and without fever).
2243-2254. doi:10.1016/S0140-6736(19)32500-0
disorders. Brain 2017;140(5):1316-1336. doi:10.1093/
73 De Jonghe P. Molecular genetics of Dravet brain/awx054
syndrome. Dev Med Child Neurol 2011;
87 Milligan CJ, Li M, Gazina EV, et al. KCNT1 gain of
53(suppl 2):7-10. doi:10.1111/j.1469-
function in 2 epilepsy phenotypes is reversed by
8749.2011.03965.x
quinidine. Ann Neurol 2014;75(4):581-590.
74 Sadleir LG, Mountier EI, Gill D, et al. Not all SCN1A doi:10.1002/ana.24128
epileptic encephalopathies are Dravet
88 Mikati MA, Jiang YH, Carboni M, et al. Quinidine in
syndrome: early profound Thr226Met
the treatment of KCNT1-positive epilepsies.
phenotype. Neurology 2017;89(10):1035-1042.
Ann Neurol 2015;78(6):995-999. doi:10.1002/
doi:10.1212/WNL.0000000000004331
ana.24520
75 Myers KA, McMahon JM, Mandelstam SA, et al.
89 Borlot F, Abushama A, Morrison-Levy N, et al.
Fatal cerebral edema with status epilepticus in
KCNT1-related epilepsy: an international
children with Dravet syndrome: report of 5
multicenter cohort of 27 pediatric cases.
cases. Pediatrics 2017;139(4):e20161933. doi:
Epilepsia 2020;61(4):679-692. doi:10.1111/epi.16480
10.1542/peds.2016-1933
CONTINUUMJOURNAL.COM 361
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
GENETIC EPILEPSY SYNDROMES
90 Mullen SA, Carney PW, Roten A, et al. Precision 103 Bisulli F, Rinaldi C, Pippucci T, et al. Epilepsy with
therapy for epilepsy due to KCNT1 mutations: a auditory features: contribution of known genes
randomized trial of oral quinidine. Neurology in 112 patients. Seizure 2021;85:115-118. doi:
2018;90(1):e67-e72. doi:10.1212/ 10.1016/j.seizure.2020.12.015
WNL.0000000000004769
104 Kalachikov S, Evgrafov O, Ross B, et al. Mutations
91 Kälviäinen R. Progressive myoclonus epilepsies. in LGI1 cause autosomal-dominant partial
Semin Neurol 2015;35(3):293-299. doi:10.1055/ epilepsy with auditory features. Nat Genet 2002;
s-0035-1552620 30(3):335-341. doi:10.1038/ng832
92 Muona M, Berkovic SF, Dibbens LM, et al. A 105 Morante-Redolat JM, Gorostidi-Pagola A,
recurrent de novo mutation in KCNC1 causes Piquer-Sirerol S, et al. Mutations in the LGI1/
progressive myoclonus epilepsy. Nat Genet 2015; epitempin gene on 10q24 cause autosomal
47(1):39-46. doi:10.1038/ng.3144 dominant lateral temporal epilepsy. Hum Mol
Genet 2002;11(9):1119-1128. doi:10.1093/hmg/11.9.1119
93 Tinuper P, Bisulli F, Cross JH, et al. Definition and
diagnostic criteria of sleep-related hypermotor 106 Dazzo E, Fanciulli M, Serioli E, et al. Heterozygous
epilepsy. Neurology 2016;86(19):1834-1842. reelin mutations cause autosomal-dominant
doi:10.1212/WNL.0000000000002666 lateral temporal epilepsy. Am J Hum Genet 2015;
96(6):992-1000. doi:10.1016/j.ajhg.2015.04.020
94 Steinlein OK, Mulley JC, Propping P, et al. A
missense mutation in the neuronal nicotinic 107 Dazzo E, Rehberg K, Michelucci R, et al.
acetylcholine receptor alpha 4 subunit is Mutations in MICAL-1cause autosomal-
associated with autosomal dominant nocturnal dominant lateral temporal epilepsy. Ann Neurol
frontal lobe epilepsy. Nat Genet 1995;11(2): 2018;83(3):483-493. doi:10.1002/ana.25167
201-203. doi:10.1038/ng1095-201
108 Bisulli F, Licchetta L, Baldassari S, et al. SCN1A
95 Phillips HA, Favre I, Kirkpatrick M, et al. CHRNB2 is mutations in focal epilepsy with auditory
the second acetylcholine receptor subunit features: widening the spectrum of GEFS plus.
associated with autosomal dominant nocturnal Epileptic Disord 2019;21(2):185-191. doi:10.1684/
frontal lobe epilepsy. Am J Hum Genet 2001;68(1): epd.2019.1046
225-231. doi:10.1086/316946
109 Myers KA, Scheffer IE, Berkovic SF, et al. Genetic
96 Aridon P, Marini C, Di Resta C, et al. Increased literacy series: genetic epilepsy with febrile
sensitivity of the neuronal nicotinic receptor α2 seizures plus. Epileptic Disord 2018;20(4):
subunit causes familial epilepsy with nocturnal 232-238. doi:10.1684/epd.2018.0985
wandering and ictal fear. Am J Hum Genet 2006;
110 Scheffer IE, Berkovic SF. Generalized epilepsy
79(2):342-350. doi:10.1086/506459
with febrile seizures plus. A genetic disorder
97 Heron SE, Smith KR, Bahlo M, et al. Missense with heterogeneous clinical phenotypes. Brain
mutations in the sodium-gated potassium 1997;120(pt 3):479-490. doi:10.1093/brain/120.3.479
channel gene KCNT1 cause severe autosomal
111 Zhang YH, Burgess R, Malone JP, et al. Genetic
dominant nocturnal frontal lobe epilepsy.
epilepsy with febrile seizures plus: refining the
Nat Genet 2012;44(11):1188-1190.
spectrum. Neurology 2017;89(12):1210-1219.
doi:10.1038/ng.2440
doi:10.1212/WNL.0000000000004384
98 Combi R, Dalprà L, Ferini-Strambi L, Tenchini ML.
112 Scheffer IE, Phillips HA, O'Brien CE, et al. Familial
Frontal lobe epilepsy and mutations of the
partial epilepsy with variable foci: a new partial
corticotropin-releasing hormone gene.
epilepsy syndrome with suggestion of linkage to
Ann Neurol 2005;58(6):899-904.
chromosome 2. Ann Neurol 1998;44(6):890-899.
doi:10.1002/ana.20660
doi:10.1002/ana.410440607
99 Guerrini R, Dravet C, Genton P, et al. Idiopathic
113 Dibbens LM, de Vries B, Donatello S, et al.
photosensitive occipital lobe epilepsy. Epilepsia
Mutations in DEPDC5 cause familial focal
1995;36(9):883-891. doi:10.1111/j.1528-1157.1995.
epilepsy with variable foci. Nat Genet 2013;45(5):
tb01631.x
546-551. doi:10.1038/ng.2599
100 Taylor I, Marini C, Johnson MR, et al. Juvenile
114 Ricos MG, Hodgson BL, Pippucci T, et al.
myoclonic epilepsy and idiopathic
Mutations in the mammalian target of rapamycin
photosensitive occipital lobe epilepsy: is there
pathway regulators NPRL2 and NPRL3 cause
overlap? Brain 2004;127(pt 8):1878-1886.
focal epilepsy. Ann Neurol 2016;79(1):120-131.
doi:10.1093/brain/awh211
doi:10.1002/ana.24547
101 Xue J, Gong P, Yang H, et al. Genetic (idiopathic)
115 Weckhuysen S, Marsan E, Lambrecq V, et al.
epilepsy with photosensitive seizures includes
Involvement of GATOR complex genes in familial
features of both focal and generalized seizures.
focal epilepsies and focal cortical dysplasia.
Sci Rep 2018;8:6254. doi:10.1038/s41598-018-
Epilepsia 2016;57(6):994-1003. doi:10.1111/epi.13391
24644-0
116 Bar-Peled L, Chantranupong L, Cherniack AD,
102 Bisulli F, Menghi V, Vignatelli L, et al. Epilepsy with
et al. A tumor suppressor complex with GAP
auditory features: long-term outcome and
activity for the Rag GTPases that signal amino
predictors of terminal remission. Epilepsia 2018;
acid sufficiency to mTORC1. Science 2013;
59(4):834-843. doi:10.1111/epi.14033
340(6136):1100-1106. doi:10.1126/science.1232044
362 APRIL 2022
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
You might also like
- Electroencephalogram (EEG) : Presented by Vajarala AshikhDocument34 pagesElectroencephalogram (EEG) : Presented by Vajarala Ashikhzohaib100% (1)
- Epilepsy Syndromes inDocument24 pagesEpilepsy Syndromes inEdwin AlvarezNo ratings yet
- The Aetiologies of Epilepsy 2021Document16 pagesThe Aetiologies of Epilepsy 2021Ichrak GhachemNo ratings yet
- Psychiatric and Behavioral Aspects of Epilepsy: Nigel C. Jones Andres M. Kanner EditorsDocument352 pagesPsychiatric and Behavioral Aspects of Epilepsy: Nigel C. Jones Andres M. Kanner EditorsDAVID100% (1)
- OET Speaking Role PlayDocument2 pagesOET Speaking Role Playsyed100% (1)
- Epilepsy - Definition, Classification, Pathophysiology, and EpidemiologyDocument7 pagesEpilepsy - Definition, Classification, Pathophysiology, and EpidemiologyMartín FleiNo ratings yet
- 02 Normal ''Suspicious'' EEGDocument10 pages02 Normal ''Suspicious'' EEGasNo ratings yet
- Infantile, Childhood, and Adolescent Epilepsies.9Document34 pagesInfantile, Childhood, and Adolescent Epilepsies.9Silviana IlieNo ratings yet
- Cluster Headache and Other Trigeminal Autonomic CephalalgiasDocument19 pagesCluster Headache and Other Trigeminal Autonomic CephalalgiasBryan100% (1)
- Adult epilepsy: diagnosis, treatment and managementDocument14 pagesAdult epilepsy: diagnosis, treatment and managementfikaNo ratings yet
- NIH Stroke Scale - Score (NIHSS) - MDCalc PDFDocument7 pagesNIH Stroke Scale - Score (NIHSS) - MDCalc PDFNovia SaragihNo ratings yet
- Adult Focal EpilepsyDocument22 pagesAdult Focal EpilepsyzhoujNo ratings yet
- Bianda Axanditya 22010110130181 Bab2ktiDocument10 pagesBianda Axanditya 22010110130181 Bab2ktimeiutaNo ratings yet
- NEUROLOGY SYMPOSIUMDocument6 pagesNEUROLOGY SYMPOSIUMSantiago Chávez BolañosNo ratings yet
- EtiologyEpilepsy2011ExpertRevNeur (Recovered)Document17 pagesEtiologyEpilepsy2011ExpertRevNeur (Recovered)ArwatiKilwowD'ctzGreenNo ratings yet
- NEUROLOGY2016771188Document7 pagesNEUROLOGY2016771188csuheena.chamandNo ratings yet
- Epilepsia - 2022 - Zuberi - ILAE Classification and Definition of Epilepsy Syndromes With Onset in Neonates and InfantsDocument49 pagesEpilepsia - 2022 - Zuberi - ILAE Classification and Definition of Epilepsy Syndromes With Onset in Neonates and InfantsAndres Rojas JerezNo ratings yet
- Summary Proceedings From The Neurology Group On Neonatal SeizuresDocument7 pagesSummary Proceedings From The Neurology Group On Neonatal SeizuresTran Trang AnhNo ratings yet
- Antibody Mediated Autoimmune Encephalitis in ChildhoodDocument11 pagesAntibody Mediated Autoimmune Encephalitis in ChildhoodTessa CruzNo ratings yet
- Encef Peds PDFDocument11 pagesEncef Peds PDFNicolas TovarNo ratings yet
- Epilepsy in AdultsDocument13 pagesEpilepsy in AdultsHellen SantosNo ratings yet
- The_Continued_Evolution_of_Epilepsy.8Document2 pagesThe_Continued_Evolution_of_Epilepsy.8mhd.mamdohNo ratings yet
- Encefalopatia Neonatal PDFDocument13 pagesEncefalopatia Neonatal PDFVanessa RomeroNo ratings yet
- Encephalopathy in Children: An Approach To Assessment and ManagementDocument8 pagesEncephalopathy in Children: An Approach To Assessment and ManagementLiaw Siew Ching 廖秀清No ratings yet
- SUPPORTINGDocument13 pagesSUPPORTINGambiit25No ratings yet
- Epilepsia - 2022 - Specchio - International League Against Epilepsy Classification and Definition of Epilepsy SyndromesDocument45 pagesEpilepsia - 2022 - Specchio - International League Against Epilepsy Classification and Definition of Epilepsy SyndromesIngrid RivadeneiraNo ratings yet
- Epilepsia en AdultosDocument13 pagesEpilepsia en AdultosMarcoNo ratings yet
- Epd 319675 48984 The Aetiologies of Epilepsy ADocument16 pagesEpd 319675 48984 The Aetiologies of Epilepsy Abilal hadiNo ratings yet
- Epilepsy in Adults - Lancet 2019Document13 pagesEpilepsy in Adults - Lancet 2019samNo ratings yet
- Neonatal Seizures: Incidence, Etiologies, Clinical Features and EEG Findings in The Neonatal Intensive Care UnitDocument5 pagesNeonatal Seizures: Incidence, Etiologies, Clinical Features and EEG Findings in The Neonatal Intensive Care UnitDoraemon BiruNo ratings yet
- neonatal_seizures__etiologies,_clinical.52_2Document7 pagesneonatal_seizures__etiologies,_clinical.52_2noya.olshop1No ratings yet
- Thijs 2019Document13 pagesThijs 2019Priska CrisnandaNo ratings yet
- Seizures in Children - Pediatric in Review 2020Document29 pagesSeizures in Children - Pediatric in Review 2020Apple B RaiwaaNo ratings yet
- Evaluation of First Seizure and Newly Diagnosed.4Document31 pagesEvaluation of First Seizure and Newly Diagnosed.4veerraju tvNo ratings yet
- Investigating The Child With Intellectual Disability: Review ArticleDocument5 pagesInvestigating The Child With Intellectual Disability: Review ArticleCristinaNo ratings yet
- Genetic Myelopathies.8Document14 pagesGenetic Myelopathies.8Mayra AldecoaNo ratings yet
- E939 FullDocument8 pagesE939 FullSalvia MeiraniNo ratings yet
- Idiopathic Generalised Epilepsies: January 2010Document7 pagesIdiopathic Generalised Epilepsies: January 2010PryslalalaNo ratings yet
- Seminar: Kaj Blennow, Mony J de Leon, Henrik ZetterbergDocument17 pagesSeminar: Kaj Blennow, Mony J de Leon, Henrik ZetterbergDanni XNo ratings yet
- British Medical JournalDocument2 pagesBritish Medical Journalpatricia roseNo ratings yet
- Psychogenic Non-Epileptic Seizures: Indian Pediatrics November 2004Document4 pagesPsychogenic Non-Epileptic Seizures: Indian Pediatrics November 2004Nico NicoNo ratings yet
- Familial Congenital Facial Synkinesis Due To 12q Duplication: A Case Report and Literature ReviewDocument7 pagesFamilial Congenital Facial Synkinesis Due To 12q Duplication: A Case Report and Literature ReviewherdhikaNo ratings yet
- Diagnosing Idiopathic Generalized EpilepsiesDocument22 pagesDiagnosing Idiopathic Generalized EpilepsiesDavid De Luna MartínezNo ratings yet
- Estatus Epileptico de Nuevo Inicio (NORSE)Document8 pagesEstatus Epileptico de Nuevo Inicio (NORSE)juanutNo ratings yet
- Seizures in Children JULIO 2020Document29 pagesSeizures in Children JULIO 2020Elizabeth HendersonNo ratings yet
- Approach To MacrocephalyDocument15 pagesApproach To MacrocephalywarunkumarNo ratings yet
- FIRES-Pathophysiology, Therapeutical Approach, and Outcome: in This ArticleDocument10 pagesFIRES-Pathophysiology, Therapeutical Approach, and Outcome: in This ArticleMohinish SNo ratings yet
- Epileptic Encephalopathies SYNGAP1Document7 pagesEpileptic Encephalopathies SYNGAP1Saya OtonashiNo ratings yet
- Aroxysmal Isorders: Approach To Paroxysmal DisordersDocument46 pagesAroxysmal Isorders: Approach To Paroxysmal DisordersblwNo ratings yet
- Epilepsia focalDocument17 pagesEpilepsia focalVíctor CalzadaNo ratings yet
- 2023-Focal epilepsies-Update on diagnosis and classificationDocument17 pages2023-Focal epilepsies-Update on diagnosis and classificationdavid.najera.lunaNo ratings yet
- Epilepsia - 2023 - Ng - Mechanisms of infantile epileptic spasms syndrome What have we learned from animal modelsDocument15 pagesEpilepsia - 2023 - Ng - Mechanisms of infantile epileptic spasms syndrome What have we learned from animal modelsilonaskorinNo ratings yet
- Epilepsy Syndromes IntroductionDocument3 pagesEpilepsy Syndromes Introductionvincent obungaNo ratings yet
- Epileptic Disorders - 2023 - Nascimento - Focal Epilepsies Update On Diagnosis and ClassificationDocument17 pagesEpileptic Disorders - 2023 - Nascimento - Focal Epilepsies Update On Diagnosis and ClassificationIvan MihailovicNo ratings yet
- Pi Is 1474442205702477Document14 pagesPi Is 1474442205702477Andi Karwana CiptaNo ratings yet
- A Review of Diagnostic Techniques in The Differential Diagnosis of Epileptic and Nonepileptic SeizuresDocument34 pagesA Review of Diagnostic Techniques in The Differential Diagnosis of Epileptic and Nonepileptic Seizurestayfan1No ratings yet
- Hypoxic-Ischemic Encephalopathy A Review For The ClinicianDocument7 pagesHypoxic-Ischemic Encephalopathy A Review For The ClinicianNorita Ruiz PalaciosNo ratings yet
- Epilepsysurgeryinchildren: Luis E. Bello-Espinosa,, Greg OlavarriaDocument12 pagesEpilepsysurgeryinchildren: Luis E. Bello-Espinosa,, Greg OlavarriaAzizah HalidNo ratings yet
- lukmanji2019 الصرعDocument11 pageslukmanji2019 الصرعkhadidja BOUTOUILNo ratings yet
- Approach To Refractory Childhood SeizuresDocument10 pagesApproach To Refractory Childhood SeizureskholisahnasutionNo ratings yet
- Cerebral Palsy: An Overview of Epidemiology, Pathophysiology and InterventionsDocument12 pagesCerebral Palsy: An Overview of Epidemiology, Pathophysiology and InterventionsMATERIAL24No ratings yet
- Epilepsia - 2022 - Hirsch - ILAE Definition of The Idiopathic Generalized Epilepsy Syndromes Position Statement by TheDocument25 pagesEpilepsia - 2022 - Hirsch - ILAE Definition of The Idiopathic Generalized Epilepsy Syndromes Position Statement by TheIngrid RivadeneiraNo ratings yet
- Controversies in Neuro-Ophthalmic Management: An Evidence and Case-Based AppraisalFrom EverandControversies in Neuro-Ophthalmic Management: An Evidence and Case-Based AppraisalAmanda D. HendersonNo ratings yet
- Neuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesFrom EverandNeuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesAmanda L. PiquetNo ratings yet
- Pediatric Immunology: A Case-Based Collection with MCQs, Volume 2From EverandPediatric Immunology: A Case-Based Collection with MCQs, Volume 2No ratings yet
- Surgical Therapies For Parkinson DiseaseDocument13 pagesSurgical Therapies For Parkinson DiseaseAnali Durán CorderoNo ratings yet
- Effect of Torsemide Vs Furosemide After Discharge On All Cause Mortality in Patients Hospitalized With Heart Failure - The TRANSFORM HF Randomized Clinical TrialDocument10 pagesEffect of Torsemide Vs Furosemide After Discharge On All Cause Mortality in Patients Hospitalized With Heart Failure - The TRANSFORM HF Randomized Clinical TrialAnali Durán CorderoNo ratings yet
- Operational New IILAE Classification of EpilepsyDocument9 pagesOperational New IILAE Classification of EpilepsyJonnyNo ratings yet
- Impact of Sacubitril - Valsartan Compared With Ramipril On Cardiac Structure and Function After Acute Myocardial Infarction - The PARADISE-MI Echocardiographic SubstudyDocument15 pagesImpact of Sacubitril - Valsartan Compared With Ramipril On Cardiac Structure and Function After Acute Myocardial Infarction - The PARADISE-MI Echocardiographic SubstudyAnali Durán CorderoNo ratings yet
- Multiple Sclerosis International Federation Guideline Methodology For Off-Label Treatments For Multiple SclerosisDocument6 pagesMultiple Sclerosis International Federation Guideline Methodology For Off-Label Treatments For Multiple SclerosisAnali Durán CorderoNo ratings yet
- Movement Disorders - 2022 - Deuschl - European Academy of Neurology Movement Disorder Society European Section Guideline OnDocument15 pagesMovement Disorders - 2022 - Deuschl - European Academy of Neurology Movement Disorder Society European Section Guideline OnAnali Durán CorderoNo ratings yet
- Seizures and Epilepsy in Patients With Ischaemic StrokeDocument17 pagesSeizures and Epilepsy in Patients With Ischaemic StrokeAnali Durán CorderoNo ratings yet
- Farmacoterapia en ObesidadDocument29 pagesFarmacoterapia en ObesidadAnali Durán CorderoNo ratings yet
- Easo 2015 Adult Obesity GuidelinesDocument24 pagesEaso 2015 Adult Obesity GuidelinesDana MuresanNo ratings yet
- Epidemiology of Traumatic Brain Injury-Associated Epilepsy in WesternDocument7 pagesEpidemiology of Traumatic Brain Injury-Associated Epilepsy in Westernhermalina sabruNo ratings yet
- Rekapitulasi Lap Pasien Gangguan Jiwa Bulan Januari 21Document2 pagesRekapitulasi Lap Pasien Gangguan Jiwa Bulan Januari 21Photo Repair ProjectNo ratings yet
- Three - Drug Combination ofDocument5 pagesThree - Drug Combination ofNaji Z. ArandiNo ratings yet
- Sindrome de WestDocument8 pagesSindrome de Westmaria laura ramirezNo ratings yet
- EpilepsyDocument11 pagesEpilepsyStella WatkinsNo ratings yet
- Blanke Et Al., 2004 OOB of Neurological OriginDocument16 pagesBlanke Et Al., 2004 OOB of Neurological OriginMarkNo ratings yet
- Epilepsia - 2023 - Carroll - A Core Outcome Set For Childhood Epilepsy Treated With Ketogenic Diet Therapy CORE KDT StudyDocument18 pagesEpilepsia - 2023 - Carroll - A Core Outcome Set For Childhood Epilepsy Treated With Ketogenic Diet Therapy CORE KDT Studysandra villeccoNo ratings yet
- Seizure First AidDocument1 pageSeizure First Aidabed aushNo ratings yet
- Epilepsy Recovery Period - Second YrDocument3 pagesEpilepsy Recovery Period - Second YrBrian MaloneyNo ratings yet
- Dravet SyndromeDocument61 pagesDravet SyndromeSnezana MihajlovicNo ratings yet
- Absence Seizures Involve BriefDocument4 pagesAbsence Seizures Involve BriefsakuraleeshaoranNo ratings yet
- How To Code Epilesy and SeizuresDocument2 pagesHow To Code Epilesy and Seizuresjoseline kenmoeNo ratings yet
- Psychogenic Non-Epileptic Seizures: ArticleDocument3 pagesPsychogenic Non-Epileptic Seizures: ArticleNico NicoNo ratings yet
- CV Rima Mayuresh Chaudhari NeurologistDocument8 pagesCV Rima Mayuresh Chaudhari Neurologistmeenakshi.r.agrawalNo ratings yet
- American Clinical Neurophysiology Society.5Document5 pagesAmerican Clinical Neurophysiology Society.5ShanaHNo ratings yet
- EEG - Basic Principles and Application in EpilepsyDocument19 pagesEEG - Basic Principles and Application in Epilepsyemilio9fernandez9gatNo ratings yet
- Epilepsy & BehaviorDocument4 pagesEpilepsy & BehaviorMIKS DARKNo ratings yet
- Evaluation of Sleep Disturbances in Children With Epilepsy A Questionnaire BasedDocument4 pagesEvaluation of Sleep Disturbances in Children With Epilepsy A Questionnaire BasednoiNo ratings yet
- Project Report On EEG MachineDocument26 pagesProject Report On EEG Machineneetubansal60% (5)
- Tongue Injury Healing in Epileptic Teen: Case ReportDocument12 pagesTongue Injury Healing in Epileptic Teen: Case ReportJoão EduardoNo ratings yet
- The Art of Lying - How the Brain Lies and Detects DeceptionDocument2 pagesThe Art of Lying - How the Brain Lies and Detects DeceptionCrischelle PascuaNo ratings yet
- Factors Affecting The Mini-Mental State Examination (MMSE) Score in The Epilepsy Patients in Aceh, IndonesiaDocument4 pagesFactors Affecting The Mini-Mental State Examination (MMSE) Score in The Epilepsy Patients in Aceh, IndonesiaRauzah MunziahNo ratings yet
- Mayfield: Product DescriptionDocument2 pagesMayfield: Product DescriptionGiapril DoniNo ratings yet
- MCQ Samples - Docx Pedia 473Document2 pagesMCQ Samples - Docx Pedia 473walaa mousaNo ratings yet
- Jurnal Efficacy and Tolerability of Adjunctive Lacosamide in Pediatric Patients With Focal SeizuresDocument15 pagesJurnal Efficacy and Tolerability of Adjunctive Lacosamide in Pediatric Patients With Focal SeizuresAnida HasnaNo ratings yet