Professional Documents
Culture Documents
Assessing Healthcare Accessibility Algorithms: A Comprehensive Investigation of Two-Step Floating Catchment Methodologies Family
Assessing Healthcare Accessibility Algorithms: A Comprehensive Investigation of Two-Step Floating Catchment Methodologies Family
Uploaded by
Alan Dino MoscosoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assessing Healthcare Accessibility Algorithms: A Comprehensive Investigation of Two-Step Floating Catchment Methodologies Family
Assessing Healthcare Accessibility Algorithms: A Comprehensive Investigation of Two-Step Floating Catchment Methodologies Family
Uploaded by
Alan Dino MoscosoCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/280531563
Assessing Healthcare Accessibility Algorithms: A Comprehensive Investigation
of Two-Step Floating Catchment Methodologies Family.
Conference Paper · January 2015
CITATIONS READS
20 1,442
3 authors, including:
Ace Vo Rahul Bhaskar
Loyola Marymount University Army Institute of Technology
23 PUBLICATIONS 120 CITATIONS 12 PUBLICATIONS 63 CITATIONS
SEE PROFILE SEE PROFILE
All content following this page was uploaded by Ace Vo on 05 September 2015.
The user has requested enhancement of the downloaded file.
Two-Step Floating Catchment Family Methodologies
Assessing Healthcare Accessibility
Algorithms: A Comprehensive Investigation
of Two-Step Floating Catchment
Methodologies Family
Full Paper
Au Vo Miloslava Plachkinova
Claremont Graduate University Claremont Graduate University
au.vo@cgu.edu miloslava.plachkinova@cgu.edu
Rahul Bhaskar
California State University, Fullerton
rbhaskar@fullerton.edu
Abstract
The Affordable Care Act (ACA) has altered the healthcare landscape in the US. ACA mandated US residents
to obtain health insurance. However, having insurance does not necessarily provide access to healthcare.
These legislation changes made it imperative for researchers to explore into more detail the problem of
healthcare accessibility. Recent advances in measuring healthcare accessibility have been fueled by a rapid
improvement of the Floating Catchment Area (FCA) methodologies. This current study summarizes the
abundance of existing knowledge on metrics of spatial accessibility and more specifically, the FCA family.
Organization of previous studies in a more comprehensive manner can assist both researchers and
practitioners who are struggling to identify which FCA methodology would best fit their needs. And finally,
the study provides a step-by-step analysis methodology, which is beneficial for decision makers when
considering solutions to the problem of physician shortage areas.
Keywords
Spatial Business Intelligence, Business Analytics, Knowledge Management, Big Data and Knowledge
Management
Introduction
Recent healthcare reforms in the US, especially the Affordable Care Act, have made it imperative for
professionals to provide better quality of care and reach out to a much larger population. In spite of the
ever-increasing amount of funds allocated to healthcare (17.9% of the nation’s GDP according to the World
Bank), population wellness and healthcare are still insufficient when compared with other countries. In
fact, the US healthcare system is ranked 37th in performance (Murray & Frenk, 2010) which demonstrates
that the state of US healthcare is not adequately meeting the needs of the population. Thus, there are
heeding calls to address the gap in providing better health services to a larger portion of the population.
This study explores the outreach of healthcare services and addresses the population’s overall access to
healthcare. A comprehensive investigation of different models for quantifying healthcare accessibility was
conducted. Consequently, the findings of this research can provide a better understanding of the challenges
associated with healthcare accessibility. There are a number of innovative approaches for assessing
healthcare accessibility. These methods compute an accessibility index within several geographical settings.
Collectively, they are known as the floating catchment area (FCA) methodologies “family”.
FCA methodologies are vector-based algorithms that utilize concepts in geography, econometrics, and
applied physics. The raster-based algorithm family is out of the scope of this study, as FCA is a more
Twenty-first Americas Conference on Information Systems, Puerto Rico, 2015 1
Two-Step Floating Catchment Family Methodologies
preferable method for measuring healthcare accessibility (Guagliardo 2004). Since the inception of the two-
step floating catchment method (2SFCA) (Luo and Wang 2003; Radke and Mu 2000), there are many
variations of the models, suggesting different ways of improvement. Given their immediate applicability in
accessing various accessibility metrics, the purpose of this study is to raise awareness in the healthcare
community regarding these methodologies. Consequently, the goals are to introduce the FCA
methodologies, suggesting a step-by-step approach when performing them, highlight their utility and
weaknesses, and provide future research directions.
To demonstrate the efficacy of the FCA methodologies family, we chose Los Angeles County, California as
the research setting because it represents a population as diverse as the US. It is expected that this analysis
can be utilized by researchers and practitioners to aid in the decision-making process of improving
healthcare accessibility and improving the quality of care in the US.
The current study contributes to existing knowledge in several aspects. First, it provides a comprehensive
literature review of the FCA methodologies family and it assesses the advantages and disadvantages of the
different methods. Second, it presents the processes associated with two FCA methodologies in a more
comprehensive manner and it describes the analysis methodology, enabling faster adoption and inviting
more robust improvement of the FCA methodologies family. Third, it points out publicly available resources
used in this research. And finally, its conclusion reflects on how the assessment of these methodologies can
inform other researchers in deciding which methodology to use and provides an overview of these
methodologies’ applicability to other disciplines.
Background
The increasing availability of geographic information systems (GIS) in health organizations, together with
the proliferation of spatially disaggregate data, has led to a number of studies that have been concerned
with developing measures of access to healthcare services (Higgs 2004). In order to summarize the existing
literature and propose a step-by-step method for measuring healthcare accessibility, the first need is to
understand what approaches have been suggested in prior studies and to conduct a comprehensive
investigation of these models. There is an abundance of accessibility research, predominantly focused on
the healthcare domain. Thus, the aim is to organize the work and offer a more comprehensive method for
exploring the relationship between geographic access, utilization, quality of care, and healthcare outcomes.
An examination of prior work and a critical evaluation of some of the most common accessibility measures
was conducted. Further, areas were identified where more research is needed to improve the process of
quantifying healthcare accessibility. More specifically, there was a focus on the FCA family of metrics, as it
employs principles from gravity-based models to incorporate supply, demand, and distance in their
characterization of the spatial accessibility of healthcare resources. Unlike traditional gravity models, the
FCA metrics provide an output in highly interpretable container-like units, e.g., physicians per person
(Delamater 2013) which are more easily understood by non-specialists. The following literature review
summarizes these studies and identifies gaps which can be addressed to improve the accuracy of the
healthcare accessibility index.
Healthcare Accessibility
There are a number of definitions related to accessibility in the healthcare context. Some of them consider
the consumers’ willingness to enter the healthcare system, or the fit between the clients and the system
(Penchansky and Thomas 1981), or the influence of financial, informational, and behavior modalities which
go beyond the geographical access (Aday and Andersen 1974). Another study (Gulliford et al. 2002)
investigates the difference between “having access” to healthcare and “gaining access”, where the former is
related to the availability of services and the latter refers to whether individuals have the resources to
overcome financial, organizational and socio-cultural barriers in order to utilize that service. For the
purposes of this paper, the definitions proposed by Khan (1992), which are based on the interaction between
the individual and the healthcare system, are used. More specifically, the notion that accessibility is the
“availability of a service moderated by space, or the distance variable” (p. 275) is used and this information
is represented using travel time, road, or map distances as suggested by Higgs (2004). As mentioned earlier,
there are a number of barriers that patients need to overcome in addition to the physical distance to access
healthcare services. In the following sections these measures of accessibility are examined in more detail,
focusing in particular on the role of geographical factors.
Twenty-first Americas Conference on Information Systems, Puerto Rico, 2015 2
Two-Step Floating Catchment Family Methodologies
Spatial Decompositions
Measuring and predicting access to healthcare services is important for decision makers, so they can better
plan better the distribution of facilities and practitioners so that all individuals in the community have
access to them. This is especially important for underserved populations which often times have greater
needs but more limited access to social programs. One such method to delineate the service area of
providers delivering social services and to produce a probability metric that maps the equity of the program
of services for each household is suggested by Radke and Mu (2000).
The method they propose measures access to social services for each household and makes adjustments
among service providers to better accommodate under-served regions. Radke and Mu (2000) considered
the problem of location-allocation and decomposing service regions to predict access and generate equity.
Overall, their model computes the ratio of suppliers to residents within a service area centered at the
supplier’s location and sums up the ratios of residents living in areas where different providers overlap (Luo
and Wang 2003)(Luo and Wang 2003). Although the results support the creation of polygon-polygon
representations of the location-allocation substitution model, there is uncertainty in the application of the
model. For example, it relies to a great extent on the delineation of a service area defined for specific domain
and any modification would impact the empirical outcome of the model. Further, the model does not take
into consideration the regions not serviced by the original supply set. Thus, the proposed method for
measuring spatial decompositions does not offer the most accurate prediction of access to social programs.
Another approach for measuring spatial accessibility is by using the FCA methods. FCA has been used to
inform the US Department of Health and Human Service to designate the Health Professional Shortage
Areas (Luo 2014; Luo and Wang 2003). The following literature review summarizes prominent FCA
methodologies and identifies gaps which can be addressed to improve the accuracy of the healthcare
accessibility index.
Floating Catchment Area Methodologies Family Review
Since their inception, FCA methodologies have proliferated and increased in both sophistication and rigor.
However, the adoption of the methodologies remains fragmented. There are no uniform application
criteria. This review is intended to inform researchers and practitioners about different types of FCA
methodologies and provide a comprehensive summary of the advantages and disadvantages of each
method.
Two-Step Floating Catchment Area (2SFCA)
The FCA methodologies family started with the two-step floating catchment area method (2SFCA) proposed
by Luo and Wang (2003) . This method consists of two steps dealing with healthcare access; the first step
is concerned with the supply and the second step is concerned with the demand. The relationship between
supply and demand is underpinned by the gravity models, i.e. how both groups interact with each other.
Travel distance and drive time analysis form “catchments”, encompassing supply-to-demand and demand-
to-supply areas of effects. In short, the two-step floating catchment area method can be interpreted as
follows:
Step 1: Given a default 30-minute drive time (catchment) from a particular healthcare provider,
sum up the total population that the supplier can reach within that drive time, then compute a
provider-to-population ratio. In the case of an individual physician, the provider ratio is 1 to the
total population reached.
Step 2: Given a 30-minute drive time (catchment) from a particular population center, obtain the
previously computed provider-to-population ratio of each healthcare provider that is located within
that drive time. Compute the accessibility index by summing up all provider-to-population ratios.
Advantages:
The index created by the 2SFCA is easy to interpret, as opposed to its predecessor, the polygon-polygon
representation (Radke & Mu, 2000). By utilizing drive time analysis, 2SFCA embeds driving obstacles and
impedances, an improvement over buffer zones. The method also considers the interaction between supply
and demand.
Twenty-first Americas Conference on Information Systems, Puerto Rico, 2015 3
Two-Step Floating Catchment Family Methodologies
Disadvantages:
Even though 2SFCA is an innovative method, it has several limitations. First, 2SFCA assumes that all
providers and population centers that reside within the designated drive time are equal in access. In other
words, there is no difference between a 10-minute drive and a 25- minute drive. Additionally, the 2SFCA
does not perform well in rural areas, since the 30-minute catchment size does not capture sparse population
well (Haggerty et al. 2014; McGrail and Humphreys 2009). Furthermore, the 2SFCA is concerned with only
one source of transportation, i.e. personal vehicles. Obviously, an expansion to other modes of
transportation is needed.
Enhanced Two-Step Floating Catchment Area (E2SFCA) Method
To address some of the limitations of the two-step FCA, Luo and Qi (2009) present the enhanced Two-Step
Floating Catchment Area (E2SFCA) method. As the name suggests, the enhanced version is built upon
previous research and segregates different travel times. By assigning different weights associated with
different travel time zones, it accounts for distance decay. Travel preference is thought to be decreasing
while moving further away from the point of origin, hence the coinage of the term “distance decay”. The
E2SFCA can be interpreted as follows:
Step 1: Given three drive time zones (catchment) from a particular healthcare provider: 0-10, 10-
20, and 20-30 minutes, sum up the total population that the supplier can reach within each zone,
then compute a provider-to-population ratio. In the case of an individual physician, the provider
ratio is 1 to the total population reached for each zone.
Step 2: Given three drive time zones (catchment) from a particular population center: 0-10, 10-20,
and 20-30 minutes, obtain the previously computed provider-to-population ratio of each
healthcare provider that resides within each zone. Compute the accessibility index by summing up
all provider-to-population ratios.
Advantages:
This enhancement is another special case of the gravity model discussed above. Luo and Qi (2009)
discovered that the E2SFCA reveals a spatial accessibility pattern that is more consistent with intuition and
delineates even more precisely spatially explicit health professional shortage areas. The advantage of
E2SFCA is that it considers distance decay in both steps, mimicking travel preferences between close and
far destinations.
Disadvantages:
The weights between different travel time zones are not properly addressed in E2FCA. By providing a set of
Gaussian weights for each time zone, the authors composed an initial weights composition. Gaussian
weights were derived from a normality assumption of the data. In other words, for each time zone,
population’s and providers’ distribution lie along the bell curve distribution. The smaller distance between
providers and population centers is, the smaller the statistical variance would be. This variance then inform
the data distribution percentage, which in turn inform the Gaussian weights. However, the article does not
explain why the weights were chosen. Nevertheless, the study called for future research with applying
different sets of weights. Despite these shortcomings, E2FSCA is the most preferred method of the family.
Various Improvements to 2FSCA and E2SFCA
The advent of 2SFCA and E2SFCA has enabled the need for extending the efficacy of the FCA methodologies
family. Improvements upon both methods come from many different aspects. Below is a brief discussion of
the most notable improvements.
Optimized 2SFCA (Ngui and Apparicio 2011): The focal improvement of the Optimized 2SFCA is
weighted calculation of travel times. By using the Canadian Health Survey in 2005, the authors
calculated demand by considering the proportion of medical users. In addition, in contrast with
using individual physicians, the method utilized aggregated physician counts in the associated
medical clinics. However, the method is only accurate for small distances, which are lower than
500 meters (approximately 550 yards).
Twenty-first Americas Conference on Information Systems, Puerto Rico, 2015 4
Two-Step Floating Catchment Family Methodologies
Kernel Density 2SFCA (Dai and Wang 2011; Polzin et al. 2014): Using kernel density
(Epanechnikov function) as a catalyst to improve 2SFCA, the method transformed the discrete and
stepwise accessibility distance decay in E2SFCA into a continuous and step-less distance decay. The
improvement of the Kernel Density 2SFCA also introduced a health needs index and a commuting
index by ways of considering principle component analysis on various demographics and
socioeconomic variables. The indices were borrowed and condensed from (Wang and Luo 2005)
applying the US notion of Health Professionals Shortage Areas to Portugal.
Variable Catchment size for 2SFCA (Luo and Whippo 2012; McGrail and Humphreys 2014): This
method proposed a flow diagram in determining the catchment size between supply and demand.
The flow diagram depicted a decision process to increase the catchment size in small increments
until a predetermined base population and a provider-to-population ratio is reached. The added
two steps of calculating the catchment sizes precede the E2SFCA steps. A further exploration of
robust catchment size determination has also been proposed in the study.
Three-step FCA (Wan et al. 2012): The three-step FCA was designed to compensate for the
overestimation in the demand. The method accounts for surrounding supply sites as competition
by computing a selection weight. The selection weight was implemented into both catchment
calculations.
Modified 2SFCA (Delamater 2013): Modified 2SFCA addresses the inherent underestimation and
overestimation in three-step FCA (Delamater, 2013). Modified 2SFCA employs both relative and
absolute distance between supply and demand in a pairwise mechanism. This builds upon the
three-step FCA method and provides a compensation for the suboptimal supplier distribution.
Multi-transportation mode 2SFCA (Mao and Nekorchuk 2013): This variation of the E2SFCA
utilizes different types of transportation as weights. It assigns a weight for each mode of
transportation in the calculation of the provider-to-population ratio and the spatial accessibility
index.
Huff model-based 2SFCA (Luo 2014): The Huff Model is a probabilistic gravity model that was
designed to predict consumer behavior within competing retail locations (Huff 1963; Huff 1964).
Essentially, the Huff Model provides a probability value for a particular demand area in relation to
a particular supply location. The probability calculation adjusts for population demand, and is
integrated into both catchments.
Commuter-based 2SFCA (Fransen et al. 2015): Focusing on bidirectional travel, the commuter-
based 2SCFA considers the routine trip observed in frequent travel to and from a supply location.
Commuter-based 2SFCA is an extension of the family to a different domain, i.e. daycare center
access. Though commuting behavior does not coincide with healthcare visits in patient scenarios,
it should be taken into consideration for the current study.
Proposed Solution
The myriad methods in the FCA family that have proliferated in recent years have not paved the way for a
better assessment or more accurate measures of healthcare accessibility. Rather, it has actually hampered
the robustness of the newly developed FCA methods. FCA is an inherent transdisciplinary method
(utilization of econometrics, applied physics, and geography in the public health domain), and as such, it
proposes that an analysis methodology can constructed to facilitate and permeate future FCA research.
The proposed methodology is designed to encourage the use of GIS. First, the two FCA methods, viz. the
original 2SFCA and ESFCA, are reexamined to provide the overall narration as well as the mathematical
notation. These two techniques were chosen as they encompass the majority of steps required for
subsequent FCA methods. Second, a brief description of the most common GIS datatypes is provided. Each
datatype bears a pseudo symbol to help non-specialists following the analysis from obtaining the data to
displaying the results.
Twenty-first Americas Conference on Information Systems, Puerto Rico, 2015 5
Two-Step Floating Catchment Family Methodologies
2SFCA and E2SFCA
Two-Step Floating Catchment Area Enhanced Two-Step Floating
(Luo and Wang 2003) Catchment Area (Luo and Qi 2009)
Overview Generate a 30-minute drive time zone Generate three drive time zones, 0-10, 10-
(catchment) with respect to the provider 20, and 20-30 minutes with respect to the
site. provider site. Assign Gaussian weights for
each zone (1.00; 0.42; 0.03) (Luo 2011)
Compute the provider-to-population ratio
at each provider location. Compute the provider-to-population ratio
at each provider location with the assigned
Generate another 30-minute drive time
weights.
catchment with respect to the population
site. Compute the spatial accessibility Generate three drive time catchments
index for each population site. similar to that of the provider. Compute
the spatial accessibility index for each
population site with the assigned weights.
Step 1 Calculate provider-to-population ratio 𝑅𝑗 Calculate provider-to-population ratio 𝑅𝑗
at each provider location 𝑗 : at each provider location 𝑗 :
𝑆𝑗 𝑆𝑗
𝑅𝑗 = 𝑅𝑗 =
∑𝑘 ∈{𝐷𝑖𝑠𝑡𝑎𝑛𝑐𝑒(𝑘,𝑗)≤𝑑0 } 𝑃𝑘 ∑3𝑟=1 ∑𝑘 ∈{𝐷𝑖𝑠𝑡𝑎𝑛𝑐𝑒(𝑘,𝑗)≤𝑑0 } 𝑃𝑘 𝑊𝑟
Step 2 Calculate the spatial accessibility index 𝐴𝐹𝑖 Calculate the spatial accessibility index 𝐴𝐹𝑖
for each population site 𝑖 : for each population site 𝑖 :
3
𝐴𝐹𝑖 = ∑ 𝑅𝑗
𝐴𝐹𝑖 = ∑ ∑ 𝑅𝑗 𝑊𝑟
𝑗 ∈{𝐷𝑖𝑠𝑡𝑎𝑛𝑐𝑒(𝑖,𝑗)≤𝑑0 }
𝑟=1 𝑗 ∈{𝐷𝑖𝑠𝑡𝑎𝑛𝑐𝑒(𝑖,𝑗)≤𝑑0 }
Mathematical 𝑆𝑗 : medical capacity at each provider 𝑗 𝑆𝑗 : medical capacity at each provider 𝑗
Notation
Explained 𝑅𝑗 : provider-to-population ratio 𝑅𝑗 : provider-to-population ratio
𝑃𝑘 : population site 𝑘 𝑃𝑘 : population site 𝑘
𝑑0 : travel threshold 𝑑0 : travel threshold
𝐷𝑖𝑠𝑡𝑎𝑛𝑐𝑒(𝑘, 𝑗): travel time between 𝑘 and 𝐷𝑖𝑠𝑡𝑎𝑛𝑐𝑒(𝑘, 𝑗): travel time between 𝑘 and 𝑗
𝑗
𝐴𝐹𝑖 : Spatial accessibility index of each
𝐴𝐹𝑖: Spatial accessibility index of each population site 𝑗
population site 𝑗
𝐷𝑖𝑠𝑡𝑎𝑛𝑐𝑒(𝑖, 𝑗): travel time between 𝑖 and 𝑗
𝐷𝑖𝑠𝑡𝑎𝑛𝑐𝑒(𝑖, 𝑗): travel time between 𝑖 and 𝑗
𝑊𝑟 : Gaussian weight for each zone (1:00 ;
0.42 ; 0.03)
Twenty-first Americas Conference on Information Systems, Puerto Rico, 2015 6
Two-Step Floating Catchment Family Methodologies
GIS Datatypes Description
Overall, there are four different datatypes. They are depicted as follows:
Type Symbol used Description Example
Tabular (t) Generic datatype in table and row format Census data
Point (p) A single location on the map Physician location
Line (l) A vector from point A to point B A road
Polygon (g) An enclosed shape on the map A Census tract
Analysis Methodology
We conducted an analysis comparing these two methods. This was performed on an Intel Xeon 2.1 GHz
chipset on a Windows 8.1 PC with 16 GB RAM. We used Esri’s ArcGIS Desktop 10.2.2 with the Network
Analyst Extension. The overall computer processing time for 2SFCA was about six hours and the E2SFCA
was about ten hours. Following are the steps we performed.
1. Obtain Census Data (t)
The appropriate population Census data (t) was obtained for the study site - Los Angeles County, California.
The 2010 Census total population data was obtained at two levels: Census tracts and block groups
(http://factfinder.census.gov/).
2. Obtain TIGER Shapefiles (g)
TIGER Shapefiles (g) (https://www.census.gov/geo/maps-data/data/tiger-line.html) contain geographic
boundaries of the US. The Census tracts and block groups (t), filtered for Los Angeles County, were joined
with the corresponding TIGER Shapefiles (g). We cleaned the data by removing all non-alphanumeric
characters and incorrect geographical joins.
3. Obtain and Geocode Physician Data (p) (http://www.cms.gov/Research-Statistics-Data-and-
Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Physician-and-Other-
Supplier.html)
This 2012 Center for Medicare and Medicaid Services (CMS) dataset provides addresses of all physicians
who claim Medicare payments. After limiting the data to only Los Angeles County and including only
physicians who practice “Emergency Medicine, General Practice, and Family Practice”, there were a total
of 2,669 physicians. Then we geocoded the addresses. Geocoding involves taking an address and providing
the corresponding longitude and latitude coordinates.
4. Obtain the road network datasets
We obtained road network datasets (l) from ESRI Streetmap Premium Services.
5. Calculate population-weighted centroids (Luo and Wang 2003)
We transformed the Census block shapefile (g) to obtain the longitude and latitude of the centroid (p). We
used the information to calculate the population-weighted centroid of the Census tract. The calculation is
as follows:
𝑁 𝑁
∑𝑖=1
𝑏
𝑃𝑖 𝑥𝑖 ∑𝑖=1
𝑏
𝑃𝑖 𝑦𝑖
𝐿𝑜𝑛𝑔𝑖𝑡𝑢𝑑𝑒 𝑥𝑡 = 𝑁 𝐿𝑎𝑡𝑖𝑡𝑢𝑑𝑒 𝑦𝑡 = 𝑁
∑𝑖=1
𝑏
𝑃𝑖 ∑𝑖=1
𝑏
𝑃𝑖
Where 𝑖 is the Census block inside a particular Census tract; 𝑃𝑖 is the population of each Census block; 𝑥𝑖
and 𝑦𝑖 is the longitude and latitude of each Census block, respectively. The calculation derives the
longitude,𝑥𝑡 , and latitude, 𝑦𝑡 , of the Census tract (t). These longitude and latitude coordinates are designed
to compensate for the difference in population concentration in each Census tract. This calculation omits
non-residential Census tracts such as airfield and military bases. Including such tracts is interesting and
Twenty-first Americas Conference on Information Systems, Puerto Rico, 2015 7
Two-Step Floating Catchment Family Methodologies
worthy of discussion in regards to healthcare access, most notably in emergency medicine. However, we
excluded these tracts in the current analysis.
6. Allot the first catchment area (g)
The first catchment area was performed by using ArcGIS’s Network Analyst tool. The drive time analysis
was done in the Service Area option utilizing Dijkstra’s algorithm. The geocoded physician data (p)
mentioned above was used to perform the analysis with a 30-minute drive time for 2SFCA and discrete
rings of 0-10, 10-20, and 20-30 minute drive time for E2SFCA.
7. Calculate the provider-to-population ratio
A spatial join linked the first catchment (g) and the population-weighed centroids of the Census tracts (p)
which resided within the catchment. This procedure aggregated the total population of all joined Census
tracts within the catchment. For E2SFCA, the total population was multiplied with the weights: 1.00, 0.2,
and 0.03 with respect to 0-10, 10-20, and 20-30 catchments. These catchments (g) were then joined with
the physician data (p). For 2SFCA, since each physician was the sole healthcare provider at his or her
location, the provider-to-population ratio calculation was equal to the reciprocal of total population. For
E2SFCA, the provider-to-population ratio was equal to the summation of the weighed total population.
8. Allot the second catchment area (g)
Similar to the first catchment, the second catchment (g) analysis was performed using Network Analyst. It
is notable that the population-weighed centroids (p) may or may not reside on an optimal location alongside
the road data (l). There are three ways to account for this shortcoming: (1) increase the location tolerance;
(2) manually move centroids; or (3) create a new road that connects to the centroid (l). The current analysis
doubled the tolerance and utilized the second option.
9. Calculate spatial accessibility index
We performed another spatial join to link each catchment (g) with each physician location (p). For 2SFCA,
we summed all provider-to-population ratios to compute the spatial accessibility index. For E2SFCA, the
provider-to-population ratios of physicians who reside in different travel zones were multiplied by the
appropriate weights (similar to step 7). Then, the total weighted provider-to-population ratios resulted in a
spatial accessibility index. The catchments (g), which contained this information, were joined with the
Census tract (g).
10. Display 2SFCA on a map.
Each Census tract (g) should contain a spatial accessibility index. A choropleth map was produced by using
color-coded quintiles with the Jenks natural breaks method, where the lighter the color, the lower the health
accessibility index.
Twenty-first Americas Conference on Information Systems, Puerto Rico, 2015 8
Two-Step Floating Catchment Family Methodologies
Figure 1. Los Angeles County 2SFCA
Figure 2. Los Angeles County E2SFCA
Figure 1 and Figure 2 offer different healthcare accessibility indices. The E2SFCA displays certain pockets
that have high accessibility index while the 2SFCA presents a centrality of healthcare accessibility. The
E2SFCA provides more subtle accessibility because of drive time zone differentiation. This improvement is
imperative for decision makers concerned with total population healthcare accessibility index.
Twenty-first Americas Conference on Information Systems, Puerto Rico, 2015 9
Two-Step Floating Catchment Family Methodologies
Furthermore, the analysis methodology offers a solid foundation for conducting FCA methodology family
research. Other FCA methods mentioned above can be applied by modifying some of the steps in this
analysis.
Practical Implications
The current paper not only contributes to research, but also it provides important implications for practice.
First, the study offers decision makers a comprehensive summary of existing methods for measuring
healthcare accessibility. This information can be of critical significance when assessing physician shortage
areas. These areas would have higher priority for decision makers when considering building new facilities
or offering incentives for relocating. In addition, the current study organizes existing knowledge on
healthcare accessibility by providing a corpus of the FCA methodology family.
Second, we offer an easy to follow analysis methodology, encouraging replication and improvement. This
methodology contains detailed instructions and explanations which are accessible to a much broader
audience compared to prior studies. Our study can be used as a guideline by both researchers and
practitioners who are interested in pursuing further research on healthcare accessibility.
Discussion and Limitations
The guidelines provided for measuring accessibility may also be extended to other domains beyond
healthcare. We hope that others would consider the FCA methodology family and employ it in a variety of
disciplines such as education, finance, or public administration.
The current study does not come without limitations. First, we used only physician data. Including hospital
data in the analysis would be more informative. Hospitals can provide unequivocal healthcare services
compared individual physicians. However, in order to be consistent with prior studies, only physician data
was used.
The second limitation of this study is the generalizability of the results. We used only data from Los Angeles
County. However, the County is the most populous and diverse in the US according to the 2010 US Census
(http://quickfacts.census.gov/qfd/states/06/06037.html), it could be considered representative of the
total population. On the other hand, we used a small dataset to evaluate the utility of the FCA
methodologies. Other researchers are encouraged to build upon our findings on a larger scale.
And finally, this study is subjected to the edge effect. This problem occurs when administrative boundaries
define spatial data. In the case of an urbanized area such as Los Angeles, the edge effect is unavoidable.
Thus, the patterns of patient-physician interaction along the borders of the bounded region are likely to be
ignored or distorted. This phenomenon may have some effect on the measured healthcare accessibility.
Conclusion
The current study makes several important contributions to spatial business intelligence. First, it
summarizes the abundance of existing knowledge on metrics of spatial accessibility and more specifically,
the FCA family. It employs principles from gravity-based models to incorporate supply, demand, and
distance in their characterization of the spatial accessibility of healthcare resources.
Second, this research organizes previous studies in a comprehensive manner. Such a structured literature
review can assist both researchers and practitioners who are struggling to identify which FCA methodology
would best fit their needs.
And finally, the study provides a step-by-step analysis methodology, which can be immensely beneficial for
decision makers when considering solutions to the problem of physician shortage areas. The proposed
methodology is based on prior literature and it builds upon the strengths of current studies while at the
same time addressing their weaknesses and limitations.
In conclusion, measuring healthcare accessibility is of growing importance to the US government and it is
vital for researchers and practitioners to use reliable datasets and be consistent in their analyses. Thus, the
current study provides valuable aids for them to extend this work and measure healthcare accessibility in
Twenty-first Americas Conference on Information Systems, Puerto Rico, 2015 10
Two-Step Floating Catchment Family Methodologies
other counties and states. This would also have a positive effect on healthcare services and would provide
more useful resources for managers when making decisions regarding new facilities.
References
Aday, L.A., and Andersen, R. 1974. "A Framework for the Study of Access to Medical Care," Health services
research (9:3), p. 208.
Dai, D., and Wang, F. 2011. "Geographic Disparities in Accessibility to Food Stores in Southwest
Mississippi," Environment and Planning-Part B (38:4), p. 659.
Delamater, P.L. 2013. "Spatial Accessibility in Suboptimally Configured Health Care Systems: A Modified
Two-Step Floating Catchment Area (M2sfca) Metric," Health & place (24), pp. 30-43.
Fransen, K., Neutens, T., De Maeyer, P., and Deruyter, G. 2015. "A Commuter-Based Two-Step Floating
Catchment Area Method for Measuring Spatial Accessibility of Daycare Centers," Health & place (32),
pp. 65-73.
Guagliardo, M.F. 2004. "Spatial Accessibility of Primary Care: Concepts, Methods and Challenges,"
International journal of health geographics (3:1), p. 3.
Gulliford, M., Figueroa-Munoz, J., Morgan, M., Hughes, D., Gibson, B., Beech, R., and Hudson, M. 2002.
"What Does' Access to Health Care'mean?," Journal of health services research & policy (7:3), pp. 186-
188.
Haggerty, J.L., Roberge, D., Lévesque, J.-F., Gauthier, J., and Loignon, C. 2014. "An Exploration of Rural–
Urban Differences in Healthcare-Seeking Trajectories: Implications for Measures of Accessibility,"
Health & place (28), pp. 92-98.
Higgs, G. 2004. "A Literature Review of the Use of Gis-Based Measures of Access to Health Care Services,"
Health Services and Outcomes Research Methodology (5:2), pp. 119-139.
Huff, D.L. 1963. "A Probabilistic Analysis of Shopping Center Trade Areas," Land economics), pp. 81-90.
Huff, D.L. 1964. "Defining and Estimating a Trading Area," The Journal of Marketing), pp. 34-38.
Khan, A.A. 1992. "An Integrated Approach to Measuring Potential Spatial Access to Health Care Services,"
Socio-Economic Planning Sciences (26:4), pp. 275-287.
Luo, J. 2014. "Integrating the Huff Model and Floating Catchment Area Methods to Analyze Spatial Access
to Healthcare Services," Transactions in GIS (18:3), pp. 436-448.
Luo, W. 2011. "Erratum to “Luo and Qi, 2009, an Enhanced Two-Step Floating Catchment Area (E2sfca)
Method for Measuring Spatial Accessibility to Primary Care Physicians”[Health and Place 15 (2009)
1100–1107]," Health & Place (17:1), p. 394.
Luo, W., and Qi, Y. 2009. "An Enhanced Two-Step Floating Catchment Area (E2sfca) Method for Measuring
Spatial Accessibility to Primary Care Physicians," Health & place (15:4), pp. 1100-1107.
Luo, W., and Wang, F. 2003. "Measures of Spatial Accessibility to Health Care in a Gis Environment:
Synthesis and a Case Study in the Chicago Region," Environment and Planning B Planning and
Design:30), pp. 865-884.
Luo, W., and Whippo, T. 2012. "Variable Catchment Sizes for the Two-Step Floating Catchment Area (2sfca)
Method," Health & place (18:4), pp. 789-795.
Mao, L., and Nekorchuk, D. 2013. "Measuring Spatial Accessibility to Healthcare for Populations with
Multiple Transportation Modes," Health & place (24), pp. 115-122.
McGrail, M.R., and Humphreys, J.S. 2009. "The Index of Rural Access: An Innovative Integrated Approach
for Measuring Primary Care Access," BMC Health Services Research (9:1), p. 124.
McGrail, M.R., and Humphreys, J.S. 2014. "Measuring Spatial Accessibility to Primary Health Care
Services: Utilising Dynamic Catchment Sizes," Applied Geography (54), pp. 182-188.
Ngui, A.N., and Apparicio, P. 2011. "Optimizing the Two-Step Floating Catchment Area Method for
Measuring Spatial Accessibility to Medical Clinics in Montreal," BMC health services research (11:1),
p. 166.
Penchansky, R., and Thomas, J.W. 1981. "The Concept of Access: Definition and Relationship to Consumer
Satisfaction," Medical care (19:2), pp. 127-140.
Polzin, P., Borges, J., and Coelho, A. 2014. "An Extended Kernel Density Two-Step Floating Catchment Area
Method to Analyze Access to Health Care," Environment and Planning B: Planning and Design (41:4),
pp. 717-735.
Radke, J., and Mu, L. 2000. "Spatial Decompositions, Modeling and Mapping Service Regions to Predict
Access to Social Programs," Geographic Information Sciences (6:2), pp. 105-112.
Twenty-first Americas Conference on Information Systems, Puerto Rico, 2015 11
Two-Step Floating Catchment Family Methodologies
Wan, N., Zou, B., and Sternberg, T. 2012. "A Three-Step Floating Catchment Area Method for Analyzing
Spatial Access to Health Services," International Journal of Geographical Information Science (26:6),
pp. 1073-1089.
Wang, F., and Luo, W. 2005. "Assessing Spatial and Nonspatial Factors for Healthcare Access: Towards an
Integrated Approach to Defining Health Professional Shortage Areas," Health & place (11:2), pp. 131-
146.
Twenty-first Americas Conference on Information Systems, Puerto Rico, 2015 12
View publication stats
You might also like
- 2022 Camping ReportDocument14 pages2022 Camping ReportIshaNo ratings yet
- TensionersDocument20 pagesTensionersSuresh KumarNo ratings yet
- Big Data Analytics in Healthcare - Promise and PotentialDocument10 pagesBig Data Analytics in Healthcare - Promise and PotentialMohd Otibi100% (1)
- IT Code 402 Notes: CBSE Class 10Document6 pagesIT Code 402 Notes: CBSE Class 10Ritu Aryan0% (1)
- CYPECAD - User's Manual PDFDocument141 pagesCYPECAD - User's Manual PDFBelak1No ratings yet
- SQL HandbookDocument26 pagesSQL HandbookkjhlkNo ratings yet
- Writing The Proposal For A Qualitative Research Methodology ProjectDocument41 pagesWriting The Proposal For A Qualitative Research Methodology Projectrcaba100% (1)
- Data for Nurses: Understanding and Using Data to Optimize Care Delivery in Hospitals and Health SystemsFrom EverandData for Nurses: Understanding and Using Data to Optimize Care Delivery in Hospitals and Health SystemsMolly McNettNo ratings yet
- Assignment 5Document4 pagesAssignment 5WaqasNo ratings yet
- Assessing Needs-Based Supply of Physicians - A Criteria-Led Methodological Review of International Studies in High-Resource SettingsDocument19 pagesAssessing Needs-Based Supply of Physicians - A Criteria-Led Methodological Review of International Studies in High-Resource SettingsPatri BarberNo ratings yet
- s12913 023 09612 3Document15 pagess12913 023 09612 3imidazolaNo ratings yet
- 2004 Beyond RCT - AjphDocument6 pages2004 Beyond RCT - AjphSamuel Andrés AriasNo ratings yet
- A Qualitative Study of Perspectives On The AcceptaDocument11 pagesA Qualitative Study of Perspectives On The Acceptapg8.adoboNo ratings yet
- SSRN Id4302002Document37 pagesSSRN Id4302002Simon fishNo ratings yet
- PublicDocument12 pagesPublicJayapriya jayaramanNo ratings yet
- Applications of Business Analytics in HealthcareDocument13 pagesApplications of Business Analytics in Healthcareshahul kNo ratings yet
- Experiences of Hospital Care For People With Multiple Long-Term Conditions: A Scoping Review of Qualitative ResearchDocument23 pagesExperiences of Hospital Care For People With Multiple Long-Term Conditions: A Scoping Review of Qualitative ResearchBulat StalnoffNo ratings yet
- Lyles Et Al 2020 Using Electronic Health Record Portals To Improve Patient Engagement Research Priorities and BestDocument15 pagesLyles Et Al 2020 Using Electronic Health Record Portals To Improve Patient Engagement Research Priorities and Besttylermichael912No ratings yet
- The Transdiagnostic Intervention For Sleep and CirDocument16 pagesThe Transdiagnostic Intervention For Sleep and CirSimonia CoutinhoNo ratings yet
- The Concept of Access: Definition and Relationship To Consumer SatisfactionDocument15 pagesThe Concept of Access: Definition and Relationship To Consumer SatisfactionTate SimbaNo ratings yet
- Literature Review BMJDocument8 pagesLiterature Review BMJc5qwqy8v100% (1)
- How Can Clinical Epidemiology Better Support Evidence-Based Guidelines and Policies in Low-Income CountriesDocument3 pagesHow Can Clinical Epidemiology Better Support Evidence-Based Guidelines and Policies in Low-Income CountriesEko Wahyu AgustinNo ratings yet
- Articulos 12022Document13 pagesArticulos 12022john jeanfranco melendres velascoNo ratings yet
- Large Language Models For Generating Medical Examinations Systematic reviewBMC Medical EducationDocument11 pagesLarge Language Models For Generating Medical Examinations Systematic reviewBMC Medical Educationalbertus tuhuNo ratings yet
- Interventions To Drive Uptake of VoluntaDocument6 pagesInterventions To Drive Uptake of VoluntaMalkit SinghNo ratings yet
- Times Series and Risk Adjusted Control ChartsDocument2 pagesTimes Series and Risk Adjusted Control Chartselo ochoa coronaNo ratings yet
- Decision Support System Literature ReviewDocument6 pagesDecision Support System Literature Reviewc5j2ksrg100% (1)
- 2020 - Quality and Women's Satisfaction With Referral System Systematic ReviewDocument16 pages2020 - Quality and Women's Satisfaction With Referral System Systematic ReviewTaklu Marama M. BaatiiNo ratings yet
- Peer Review - COMPLETE - EDITEDDocument4 pagesPeer Review - COMPLETE - EDITEDDavid KaranuNo ratings yet
- Lizarondo 2014 PerformanceEvalDocument13 pagesLizarondo 2014 PerformanceEvalKamila AmmarNo ratings yet
- qt5j15k0nf NosplashDocument2 pagesqt5j15k0nf NosplashsinayaphetNo ratings yet
- Literature Review On HmisDocument7 pagesLiterature Review On Hmisea219sww100% (1)
- Navigation Programs To Support Community-Dwelling Individuals With Life-Limiting Illness: Determinants of ImplementationDocument11 pagesNavigation Programs To Support Community-Dwelling Individuals With Life-Limiting Illness: Determinants of ImplementationarysiaNo ratings yet
- Privett and Gonsalvez (2014) The Top Ten Global Health Supply Chain Issues - Perspectives From The Field (ORHC)Document6 pagesPrivett and Gonsalvez (2014) The Top Ten Global Health Supply Chain Issues - Perspectives From The Field (ORHC)Damonda PradiptaNo ratings yet
- Healthcare Logistics and Supply Chain Issues and Future ChallengesDocument4 pagesHealthcare Logistics and Supply Chain Issues and Future Challengespallavi mehraNo ratings yet
- Applications of Business Analytics in Healthcare: SciencedirectDocument12 pagesApplications of Business Analytics in Healthcare: SciencedirectSujay ShahNo ratings yet
- The Impact of Hospital Accreditation On The QualitDocument13 pagesThe Impact of Hospital Accreditation On The QualitRai Riska Resty WasitaNo ratings yet
- 2008a Sanhueza Leiva BalakrishnanDocument27 pages2008a Sanhueza Leiva BalakrishnanMych BogdanNo ratings yet
- The Impact of Hospital Accreditation On The Quality of Healthcare A Systematic Literature ReviewDocument12 pagesThe Impact of Hospital Accreditation On The Quality of Healthcare A Systematic Literature Reviewners edisapNo ratings yet
- Classification and Regression Tree Analy PDFDocument10 pagesClassification and Regression Tree Analy PDFEduard MacoveiNo ratings yet
- s12913 022 08783 9Document23 pagess12913 022 08783 9Shuai ShaoNo ratings yet
- Lectura en InglésDocument8 pagesLectura en InglésReev KatsNo ratings yet
- Hrm&a Group AssignmentDocument8 pagesHrm&a Group AssignmentDivya ParmarNo ratings yet
- Maya Semrau - Service User and Caregiver Involvement in Mental Health System Strengthening in Low - and Middle-Income Countries Systematic ReviewDocument18 pagesMaya Semrau - Service User and Caregiver Involvement in Mental Health System Strengthening in Low - and Middle-Income Countries Systematic ReviewsukmarahastriNo ratings yet
- Nurses' Utilization and Perception of The Community/Public Health Nursing CredentialDocument6 pagesNurses' Utilization and Perception of The Community/Public Health Nursing CredentialViolin Irene NinefNo ratings yet
- Electronic Med Rec AOMDocument25 pagesElectronic Med Rec AOMfatiisaadatNo ratings yet
- How Do Health Systems Improve Patient Flow When Services Are Misaligned With Population Needs? A Qualitative StudyDocument11 pagesHow Do Health Systems Improve Patient Flow When Services Are Misaligned With Population Needs? A Qualitative StudySara Adi KreindlerNo ratings yet
- Geostatistical Linkage of National Demographic and Health Survey Data: A Case Study of TanzaniaDocument14 pagesGeostatistical Linkage of National Demographic and Health Survey Data: A Case Study of Tanzaniaobaidur.slghnNo ratings yet
- Running Head: Health Information Technology 1Document12 pagesRunning Head: Health Information Technology 1api-469824583No ratings yet
- Investigating Discrete Event Simulation Method To Assess The Effectiveness of Wearable Health Monitoring Devices 2014 Procedia Economics and FinanceDocument19 pagesInvestigating Discrete Event Simulation Method To Assess The Effectiveness of Wearable Health Monitoring Devices 2014 Procedia Economics and FinanceRupaliNo ratings yet
- 01 Kruse 2016Document7 pages01 Kruse 2016Claudio PinuerNo ratings yet
- Guidance To Best Tools and Practices ForDocument33 pagesGuidance To Best Tools and Practices Forcvdk8dc8sbNo ratings yet
- 2023 Article 6059Document12 pages2023 Article 6059Chloe BujuoirNo ratings yet
- Literature Review On Clinical Decision Support System Reducing Medical ErrorDocument7 pagesLiterature Review On Clinical Decision Support System Reducing Medical Errorgvzwyd4nNo ratings yet
- Systematic Quantitative Literature Review MethodDocument7 pagesSystematic Quantitative Literature Review Methodc5qdk8jnNo ratings yet
- Performing A Literature Review BMJDocument8 pagesPerforming A Literature Review BMJfvgrsm8r100% (1)
- Capturing Patients Needs in CaDocument18 pagesCapturing Patients Needs in CaAnissa ResianaNo ratings yet
- Trachoma Survey Methods A Literature ReviewDocument5 pagesTrachoma Survey Methods A Literature Reviewiiaxjkwgf100% (1)
- Literature Review of Decision Support SystemDocument11 pagesLiterature Review of Decision Support Systemafmzmqwdglhzex100% (1)
- 10.1108@jhom 06 2018 0176Document19 pages10.1108@jhom 06 2018 0176Karenziitah Katiuska Sosa RamirezNo ratings yet
- Symposium: Challenges in Targeting Nutrition Programs: Discussion: Targeting Is Making Trade-OffsDocument4 pagesSymposium: Challenges in Targeting Nutrition Programs: Discussion: Targeting Is Making Trade-OffsMukhlidahHanunSiregarNo ratings yet
- Assignment 3Document6 pagesAssignment 3WaqasNo ratings yet
- Literature Review Developing Competencies For Health Promotion Deliverable 3bDocument10 pagesLiterature Review Developing Competencies For Health Promotion Deliverable 3bxfeivdsifNo ratings yet
- 53Document10 pages53Steve GannabanNo ratings yet
- Osteoarthritis Physical Activity Care Pathway (OA-PCP) : Results of A Feasibility TrialDocument11 pagesOsteoarthritis Physical Activity Care Pathway (OA-PCP) : Results of A Feasibility TrialrahmarahmatNo ratings yet
- 4.3.3.4 Packet Tracer - Configuring VPN Tunnel ModeDocument3 pages4.3.3.4 Packet Tracer - Configuring VPN Tunnel ModeFahadNo ratings yet
- Revision Status History For F-70H Compressor - 04-23-15Document3 pagesRevision Status History For F-70H Compressor - 04-23-15Daniel Martinez CollazoNo ratings yet
- TRS SMCDocument8 pagesTRS SMCSeverino NetoNo ratings yet
- MongoDB Update RemoveDocument6 pagesMongoDB Update RemovePreeti SinghNo ratings yet
- The Student Manage Their Time Using TechnologyDocument2 pagesThe Student Manage Their Time Using TechnologyJed Andrei RubioNo ratings yet
- s11423 018 9598 6 PDFDocument17 pagess11423 018 9598 6 PDFJoy PascoNo ratings yet
- Er DiagramDocument3 pagesEr Diagramرهيب صادق النظيفNo ratings yet
- 1st AssignmentDocument3 pages1st AssignmentM10r SidhuNo ratings yet
- Drivability GuideDocument144 pagesDrivability GuideSuciu Florin100% (1)
- Samsung A330Document48 pagesSamsung A330cipcozianu_297765774No ratings yet
- Led Performance Highbay 150 W 6500 K Gen2: Product DatasheetDocument3 pagesLed Performance Highbay 150 W 6500 K Gen2: Product DatasheetTerry wei shengNo ratings yet
- 1. pH计 pH Meters 24.3.6Document27 pages1. pH计 pH Meters 24.3.6Valentine MalamaNo ratings yet
- Placement Code of Conduct PDFDocument13 pagesPlacement Code of Conduct PDFEdwinNo ratings yet
- Decidability & Rice's Theorem: Arjun Suresh For GATE Overflow Helped by Subarna and SukanyaDocument47 pagesDecidability & Rice's Theorem: Arjun Suresh For GATE Overflow Helped by Subarna and SukanyaAbhishek JainNo ratings yet
- CYNOSUREDocument49 pagesCYNOSUREMadge FordNo ratings yet
- AEPC Annual Report 2019-20Document100 pagesAEPC Annual Report 2019-20Parvez khanNo ratings yet
- Pool Control Prof IDocument2 pagesPool Control Prof IskromenNo ratings yet
- Abb Utilities GMBH: ApplicationDocument2 pagesAbb Utilities GMBH: Applicationantlsm733No ratings yet
- English For Career DevelopmentDocument5 pagesEnglish For Career DevelopmentJuan Daniel Vargas PerdomoNo ratings yet
- Tenant Management: Signup-Login Upload Property Details My AccountDocument14 pagesTenant Management: Signup-Login Upload Property Details My AccountANIRUDDH MAKWANANo ratings yet
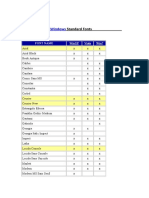
- Microsoft Windows Standard FontsDocument2 pagesMicrosoft Windows Standard FontscrosupermanNo ratings yet
- CHUANGYI CatalogueDocument13 pagesCHUANGYI CataloguebereketNo ratings yet
- CFD Project - Jan 2022Document2 pagesCFD Project - Jan 2022Aqil ZainieNo ratings yet
- Electronics Coaching Notes 5Document6 pagesElectronics Coaching Notes 5Jojo TakatoNo ratings yet