Professional Documents
Culture Documents
Clinical Chemistry - PITUITARY HORMONES TRANS
Uploaded by
Camella Beatrice Lujan ValleOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Chemistry - PITUITARY HORMONES TRANS
Uploaded by
Camella Beatrice Lujan ValleCopyright:
Available Formats
Trans by : nahaeminrmt
Introduction: Chapter 20 (Pituitary Hormones) Short feedback loop - pituitary (TSH) to the thymus
(Thyroxine)
Pituitary (Latin and Greek) - “spit mucus” Long feedback loop - hypothalamus to thymus
Brain is responsible for the signaling the pituitary to Ultrashort feedback loop - feedback loop between
secrete hormones that regulate other endocrine glands. pituitary and hypothalamus
Pituitary is also known as “master gland” or “hypophysis”
as it underneath the hypothalamus
Functions of Pituitary Gland: feedback loops, pulsatile
secretions, diurnal rhythms, and environmental or
external modification of its performance
Pituitary function can be detected between seventh and
ninth weeks of gestation
Anatomy of Pituitary Gland
The pituitary resides in the pocket of sella turcica
Three distinct parts of pituitary gland:
Anterior pituitary (adenohyophysis) Pulsatile Secretions
Intermediate lobe (pars intermedialis) - poorly e.g. Gonadotropin-Releasing Hormone
developed in humans and has little functional ↑ frequency of GnRH pulses = ↓ in the
capacity. gonadotrope secretory response
Posterior pituitary (neurophypophysis) ↓GnRH pulse frequency = ↑ LH pulse
Anterior Pituitary Cyclic Rhythms
Largest portion Diurnal rhythms
Originates from the Rathke’s pouch Zeitgeber (“time giver”) - the process of entraining
Enveloped by the sphenoid bone or synchronizing these external cues into the
It receives 80%-90% of its blood supply and many function of internal biologic clocks.
hypothalmic factors via the hypothalmic- e.g ACTH lowest secretion during 11PM to 3AM
hypophyseal portal system but at peak during 6AM-9AM; TSH more of a
Hormones produced: prolactin, GH, TSH, cortisol, nocturnal hormone than diurnal.
LH, FSH Hypothalmic Hormones
Posterior Pituitary
Arises from the diencephalon These hypophysiotrophic hormones are found
It is responsible for the storage and release of throughout the CNS and various other tissues (gut,
oxytocin and vasopressin pancreas, and other endocrine glands)
It is connected to the supraoptic and Hormone Structure Action
paraventricular hypothalmic nuclei TRH 3 Amino Acids Releases TSH
Paraventricular hypothalmic nuclei - where and prolactin
vasopressin and oxytocin are produced) GnRH 10 Amino Acids Releases LH and
FSH
Functio of Hypothalmic-Hypophyseal Unit CRH(corticotropin- 41 amino acids Releases ACTH
releasing hormone)
Open-loop Negative Feedback Mechanisms
Open means they are subjected to external Vasopressin (pituitary gland) Releases ACTH
modulation and generally influenced or modified GHRH 44 amino acids Releases GH
by higher neural input or other hormones Somatostatin 14 and 28 amino Inhibits GH and
e.g. hypothalmic-pituitary-thyroidal axis acids TSH release
It can be inhibited by adrenal steroids Dopamine 1 amino acid Inhibits
(glucocorticoids) and cytokines which are (prolactin prolactin
released during physiological stress inhibitory factor) release
hypothalamus will release TRH → thyrotrophs (TSH-producing Pituitary Tumors
cells) in the anterior pituitary will respond and release TSH → TSH
will stimulate thyroid to release thyroxine → thyroxine will be 20% of people harbor clinically silent pituitary
released in the blood → signals the hypothalamus and pituitary adenomas and findings are consistent with pituitary
to suppress their action tumors observed in 10%-30% normal individuals
undergoing MRI examinations.
These tumors account for 91% of the lesions removed Effector)
from carefully selected patients who have undergone
transphenoidal surgery. Growth Hormone
Pituitary tumors:
1. Prolactin-secreting pituitary tumors - most common Also called as “somatotropin”
2. Non-functioning or null cell tumors Kapag walang GH, pero present yung ibang hormones
3. Tumors that secrete GH, gonadotropins, ACTH, or TSH (T4, adrenal steroids, and gonadal steroids) wala pa ring
Atypical Pituitary Tumors growth unless nag-administer ng GH. Kung may GH pero
Most of these tumors are macroadenomas (>1 cm wala naman yung ibang hormones, wala pa ring growth.
in diameter) and show invasion into surrounding In short, kailangan maayos talaga yung pituitary gland.
structures like the cavernous sinuses DIRECT EFFECTOR (Multiple)
MIB-1 is a monoclonal antibody that is used to It is structurally related to prolcatin and human
detect the Ki-67 antigen, a marker of cell placental lactogen
proliferation A single peptide with two intramolecular disulfide
A high “proliferation index” suggests higher bridges
degree of atypia It takes complete functioning of the pituitary to
Tumors that have an MIB-1 proliferative index establish conditions ripe for the growth of the individual
greater that 3%, excessive p53 immunoreactivity, Adequate nutrition, normal levels of insulin, and
and increased mitotic activity overall good health
Physiologic Enlargement of Pituitary Gland Somatotrophs - pituitary cells that produce GH;
Pregnancy - It is due to lactotroph hyperplasia composed the 1/3 of the normal weight of pituitary
Puberty Pulse secretion
Long-standing primary thyroidal failure - Average interpulse interval - 2 to 3 hrs
thyrotroph and lactotroph hyperplasia Peak secretion happen on the onset of sleep
Long-standing primary gonadal failure - Ghrelin - An enteric hormone that plays important roles
gonadotrph hyperplasia in nutrient sensing, appetite and in glucose regulation; a
potent stimulator of GH
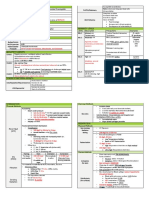
Anterior Pituitary Hormones
More complex Hypothalmic GHRH → Pituitary Gland will release GH →
Either tropic or direct effector Secretion of GH will be inhibited by somatostatin
Tropic - the effect is specific for another endocrine
gland Actions of GH
TSH - regulate thyroid function (it is directed Amphibolic Hormone - directly influences anabolic
to the thyroid gland) and catabolic process
LH - directs testosterone (Leydig Cells) and CATABOLIC - Breakdown
ovulation ANABOLIC - Build
FSH - folliculogenesis and spermatogenesis GH allows an individual to effectively transition
ACTH - regulates adrenal steroidogenesis from a fed state to a fasting state without
Direct Effector - act directly on peripheral tissue experiencing a shortage of substrates required for
Growth Hormone - it affects numerous normal intracellular oxidation.
tissues and also stimulates the liver to GH antagonizes the effect of insulin on glucose
produce growth factors metabolism, promotes hepatic gluconeogenesis,
Prolactin - direct effector of breasts and stimulates lipolysis
Enhanced lipolysis (Catabolic) → oxidative substrate for peripheral tissue
Pituitary Target Structure Feedback (skeletal muscle)
Hormon Gland Hormone Hepatic gluconeogenesis (Anabolic) → conserves glucose for the CNS
e
LH Gonad Dimeric Sex steroids *GH deficiency in children may be accompanied with
(Tropic) glycoprotein (Estradiol/Testost hypoglycemia
erone) *Adult hypoglycemia may occur if both GH and ACTH are
FSH Gonad Dimeric Inhibin deficient
(Tropic) glycoprotein Other anabolic effects of GH
TSH Thyroid Dimeric Thyroid Protein synthesis in skeletal muscle and other
(Tropic) glycoprotein Hormones (T4/T3) tissues → positive nitrogen balance and
ACTH Adrenal Single peptide Cortisol phosphate retention
(Tropic) derived from Indirect effects of GH
POMC Mediated by factors that were initially called,
GH Multiple Single Peptide IGF-I somatomedins now called Insulin-like Growth
(Direct Factor (IGF) due to its homology to proinsulin
Effector) IGF-I: Major growth factor induced by GH; it
Prolactin Breast Single Peptide Unknown has distinct cell surface receptors that are
(Direct distinct from insulin
Produced in the liver when stimulated GH-producing tumors occurs before
by GH epiphyseal closure
IGF-I receptors can be activated by Growth in impressive height
hyperinsulinemia Classical symptoms include:
IGF-II: supraphysiologic levels could cause Insidious, features of bony and soft tissue
hypoglycemia overgrowth
IGF Binding Protein 3 (IGFBP-3) - it could Progressive enlargment of the hands and feet
inhibit neoplastic proliferation Growth of facial bones (mandible and skull)
Significant teeth gaps (severe cases)
P53 tumor supressor gene → upregulate active IGFBP-3 secretion Diffuse (puberty) overgrowth of the ends of
→ inhibits IGF-I signaled mutagenesis → inhibition of neoplastic
the long bones
cell proliferation
Spine can produce debilitating form of
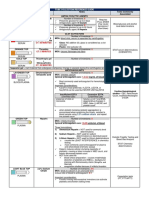
Other Modifiers of Growth Hormone arthritis
Stimulate Growth Hormone Inhibit Growth Hormone Glucose intolerance or overt diabetes can
Secretion Secretion occur
Sleep Glucose loading Hypertension
Exercise β-antagonists (e.g., Accelerated atherosclerosis
epinephrine) Proximal muscle weakness due to acquired
Physiologic Stress α-Blockers (e.g., myopathy (may be seen late in illness)
phentolamine) Sleep apnea
Amino Acids (e.g., arginine) Emotional/Psychogenic Organomegaly esp. Thyromegaly
Stress (hyperthyroidism is exceedingly rare unless
Hypoglycemia Nutritional deficiencies the tumor cosecretes TSH)
Sex Steroids Insulin deficiency Hypermetabolic condition → excessive
α-Agonists (e.g., Thyroxine deficieny sweating or heat intolerance
norepinephrine) Symptoms of acromegaly manifest GRADUALLY
β-Blockers (e.g., propanolol) Patients may complain about local effects of
the tumor (headache or visual complaints) or
symptoms related to hypopituitarism
Testing of GH
Acromegaly if left untreated will lead to
Rarely diagnostic
Shortened life-span
Possible Laboratory Results
Increase risk for heart disease (combination
Disease Associated Characteristics
of hypertension, coronary artery disease, and
Hepatoma associated with ↑ of IGF-I
diabetes/insulin resistance
Patients with active has ↑ level of IGGBP-3 Development of cancer
acromegaly Cosecretion of prolactin can be seen up to 40% of
Inadequate production of GH ↓ IGF-I patients with acromegaly; few cases TSH-GH
Poorly controlled diabetes ↓ IGF levels secreting tumors have also been reported
Oral Glucose Testing (100g glucose load) Laboratory Diagnosis of GH
GH levels are undetectable in normal ↑ levels of GH do not suppress normally with
individuals glucose loading (definitive test)
Patients with acromegaly - ↑GH Some patients have normal level of GH
Insulin-induced hypoglycemia - once a gold Elevated levels of IGF-I are helpful
standard for testing patients with GH deficiency Treatment of Acromegaly
Combination infusion of GHRH and amino acid l- Goal: tumor ablation with continued function
arginine or infusion of l-arginine coupled with oral of the remainder pituitary
l-DOPA Transphenoidal adenomectomy - procedure
GH level up to 3-5 ng/mL - unlikely that the of choice
patient is GH deficient External beam or Focused irradiation - for
*provocative GH levels is not necessary for px with low IGF-1 patients with extremely large tumors and may
levels, or with panhypotuitarism invade local structures
GH decline may take several years
Acromegaly Temporary suppression of GH:
It results from pathologic or autonomous GH SS analogs - octreotide, pasireotide, and
excess or in majority, pituitary tumor lanreotide
Pituitary tumor due to ectopic production of Dopaminergic agonists - cabergoline
GHRH or GH (rare) and bromocriptine
Familial Acromegaly - mutations in the aryl- GH Receptor Antagonists - pegvisomant
hydrocarbon-interacting protein gene (AIP)
Sporadic (irregular) cases - due to polymorphisms GH Deficiency
in the SS receptor type 5 gene Children - genetic or may be due to tumors
Gigantism (craniopharyngiomas)
Adults - structural or functional abnormalities of Disruption of the pituitary stalk (e.g., tumors,
the pituitary trauma, or inflammation) interrupted flow of
Decline of GH is an inevitable consequence of dopamine from the hypothalamus to the
aging lactotrophs
Children GH Deficiency TRH directly stimulates prolactin secretion
Several genetic defects identified in the GH ↑ in TRH (primary hypothyroidism) = ↑
axis prolactin levels
Recessive mutation in the GHRH gene Stimulation of Prolactin
causing a failure of GH secretion - most Pathologic Physiologic
common Neural suckling reflex (due to Exercise
Lose of GH gene itself - rare chest wall injuries)
Mutation result to GH insensitivity have Renal failure Seizures
also been reported - involve GH receptor, PCOS
IGF-I biosynthesis, IGF-I receptors, Primary hypothyroidism
defects in GH signal transduction Prolactin is not only regulated by dopamine but
Patients do not respond normally also by: GnRH, TRH, and vasoactive intestinal
to exogenously administered GH polypeptide
Structural lesions of the pituitary or Stimulation of breasts in nursing causes the
hypothalamus release of prolactin-secreting hormones from the
May be associated with other anterior hypothalamus through a spinal reflex arc
pituitary hormone deficiencies Physiologic effect of prolactin: lactation
Adult GH Deficiency Usual consequence of prolcatin excess: hypogonadism
Complete or even partial failure of the Suppression of gonadotropin secretion from the
anterior pituitary pituitary
Symptoms are vague and include: social Inhibition of gonadotropin action at the gonad
withdrawal, fatigues, loss of motivation, and Suppression of ovulation is seen in lactating
diminished feeling of well being postpartum women
Osteoporosis and alterations in body Prolactinoma
composition It is a pituitary tumor that directly secretes
Therapy prolactin
It has become relatively simple with the Most common type of functional pituitary tumor
advent of recombinant human GH Symptoms vary in age and sex
GH has been employed by athletes as a performance Premenopausal woman - menstrual
enhancing substance and as an aid in injury recover irregularity/amenorrhea, infertility, or
galactorrhea
Prolactin Postmenopausal women - symptoms of
pituitary mass (headaches or visual
It is structurally related to GH and human placental complaints)
lactogen Men - same with postmenopausal women
Produced by the lactotrophs in the pituitary and may be presented with erectile
It is considered as a stress hormone dysfunction and reduced libido
It has a vital relationship to reproduction Prolactin induced hypoginadism maybe
DIRECT EFFECTOR - it has diffuse target tissue and lacks presented with osteoporosis
a single endocrine end organ Other causes of Hyperprolactinemia
Major hypothalmic regulation is tonic inhibition rather It may be of physiologic, pharmacologic, and
than intermittent stimulation pathologic causes
Ibig sabihin, di nagsstimulate si hypothalamus, Prolactinoma is indicated if the prolactin level
pinapatigil niya yung secretion ni pituitary is >150 ng/mL with correlation to the tumor size
Prolactin Inhibitory Factor (PIF) was once Moderate elevations in prolactin (25-100ng/mL) is
considered a polypeptide hormone capable of caused by the following
inhibiting prolactin secretion Pituitary stalk interruption
Dopamine - ONLY neuroendocrine signal that Use of dopaminergic antagonist medications
INHIBITS prolactin and is now considered to the Primary thyroidal failure
elusive PIF Renal failure
Medications that cause hyperprolactinemia PCOS
Phenothiazines Breast or genital stimulation
Butyrophenones Significant hyperprolactinemia in pregnancy
Metoclopramide In most circumstances, prolactin is a 23-kD
Reserpine Macroprolactinemia (150-kD) - patients are
Tricyclic anti-depressants asymptomatic
α-methyldopa
Antipsychotics that antagonize the dopamine D2
receptor
It can be excluded by precipitating serum Idiopathic Galactorrhea
samples with polyethylene glycol prior to A condition in which lactation occuring in
measuring prolactin women with normal prolactin levels
Clinical Evaluation of Hyperprolactinemia It can be seen with women who became
Careful history and physical examination is pregnant several times and has no pathologic
enough to exclude non-endocrine causes of implication
hyperprolactinemia
Hypopituitarism
Examination of TSH and free T4 - to eliminate
primary hypothyroidism Definitions/Characteristics
Evaluation of other anterior pituitary function It is a condition where there is a failure of either
Evaluation of sellar anatomy with a high- the pituitary or the hypothalamus results in the
resolution MRI should be obtained loss of anterior pituitary function
Management of Prolactinoma Panhypopituitarism - It is the complete loss of
Goal of the therapy: reduction of tumor mass, function of the pituitary gland
restoration of normal gonadal function and Monotropic hormone deficiency - a loss of only a
fertility, prevention of osteoporosis, and single pituitary hormone
preservation of normal anterior and posterior A loss of a tropic hormone = malfunctioning
function of the end endocrine gland
Possible therapeutic options: simple A loss of direct effectors = may not be readily
observation, surgery, radiotherapy, or apparent
medical managements with dopamine Primary and Secondary Hypo___
agonists. Kapag PRIMARY, yung organ mismo yung may
Management of prolactinoma also depend on problema. Kunyare, Priamary Hypothyroidism,
the tumor size (macroadenoma or increased ang TSH pero low ang kanyang T4.
microadenoma) Kapag SECONDARY, si pituitary ang may problema.
Dopamine Agonists Secondary Hypothyroidism, low ang TSH kaya low
Most commonly used therapy for din ang iyong T4
microprolactinomas Etiology of Hypopituitarism/Causes
Tumor shrinkage is noted in more than Pituitary tumors
90% of patients treated with either It can cause panhypopituitarism, by
bromocriptine mesylate (Parlodel) or compressing or replacing normal tissue or
cabergoline (Dostinex) dopamine interrupting the flow of hypothalmic
receptor agonists hormones by destroying the pituitary stalk
The said drugs also shrink prolactin- Large, nonsecreting tumors (e.g.,
secreting macroadenomas chromophobe adenomas or null cell tumors)
Resumption of menses and restoration or macroprolactinomas
of fertility Parasellar tumors (e.g., menangiomas and
Adverse effects of bromocriptine: gliomas)
Orthostatic hypotension Metastatic tumors (e.g., breast and lungs)
Dizzines Hypothalmic tumors (e.g.,
Nausea craniopharyngiomas or dysgerminomas)
GI adverse effects Hemorrhage in pituitary tumor is rare but
Cabergoline has fewer adverse affects may lead to complete pituitary failure
It has the ability to interact with 5- Postpartum ischemic necrosis
hydroxytryptamine (5-HT) Occur after a complicated delivery (Sheehan’s
serotonergic receptor leading to Syndrome)
development of valcular heart Failure to lactate in the puerperium
disease Infiltrative Diseases
Neurosurgery Hemochromatosis
It is only considered when: Sarcidosis
Pituitary tumor apoplexy Histiocytosis
(hemorrhage) Fungal infections, tuberculsosis, and syphilis - can
Acute visual loss due to involve hypothalamus or pituitary
macoradenoma Lymphocytic hypophysitis
Cystic prolactinoma Autoimmune disease of the pituitary, may
Intolerance to medical therapy only affect a single cell type in the pituitary
Tumor resistance to dopaminergic It could lead to monotropic hormone
agonists deficiency or can involve all cell types,
Cure rates are INVERSELY yielding total loss of function
proportional to the tumor size Ipilimumab
Radiotherapy A monoclonal antibody that blocks cytotoxic
Only for high surgical risk with T-lymphocyte-associated antigen 4 (CTLA-4)
intolerance of dopamine agonists
It is proven to increase survival in melanoma Function: regulate renal free water excretion for water
patients balance
Associated with lymphocytic hypophysitis Vasopressin receptors (V2) in the kidney are
Severe Head Trauma concentrated in the renal collecting tubulus and
It may shear the pituitary stalk or may the ascending limb of the loop of Henle
interrupt the portal circulation
V2 → bind to adenylate cyclase → activated! → induce
Radiotherapy induced panhypopituitarism insertion of aquaporin-2 (water channel protein) in the
Familial panhypopituitarism tubular luminal membrane
Idiopathic hypopituitarism
Hypopituitarism Etiology It is a potent pressor agent and effects blood
1. Pituitary tumors clotting
2. Parapituitary/Hypothalmic tumors Vasopressin promotes Factor VII release from
3. Trauma hepatocytes and von Willebrand factor
4. Radiation therapy/Surgery release from endothelium
5. Infarction V1a and V1b are coupled to phospholipase C
6. Infection Hypothalmic osmoreceptors and Vascular
7. Infiltrative disease baroreceptors - It regulate the release of vasopressin
8. Immunologic from the posterior pituitary
9. Familial Osmoreceptors
These are extremely sensitive to even small
10. Idiopathic
changes in plasma osmolality
↑Plasma osmolality = ↑ vasopressin
Treatment of Panhypotuitarism
baroreceptors causing reduction in renal free
Replacement therapy
water clearance, lowering plasma osmolality
Pulsatile GH infusions - induced puberty and
Vascular Baroreceptors
restored fertility in patients with Kallman’s
It is located in the left atrium, aortic arch, and
syndrome
carotid arteries
Gonadotropin preparation - restored ovulation/
Vasopressin is released in response to a fall in
spermatogenesis
blood volume or blood pressure
Posterior Pituitary Hormones A 5%-10% fall in arterial blood pressure in
normal humans will trigger vasopressin
An extension of the forebrain and represents the
release
storage region for vasopressin and oxytocin
Diabetes Insipidus
These peptide hormone are synthesized in the
Polyuria and polydipsia is a consequence of
supraoptic and paraventricular nuclei of the
vasopressin deficency
hypothalamus and transported to the neurohypophysis
Causes of Hypothalmic DI include:
via their axons in the hypothalamoneurohypophyseal
Apparent autoimmunity to vasopressin-
tract
secreting neurons
The synthesis of these hormones is tightly linked to the
Trauma
production of neurohypophysin (larger protein)
Diseases affecting pituitary stalk function
Neurohypophysis - storage area for hypothalmic
Various CNS or pituitary tumors
hormones
Low vasopressin levels and elevated plasma
The said hormones have an autocrine and paracrine
osmolality is a reasonable secure diagnosis of DI
function
Therapeutic trial of vasopressin or a synthetic
Autocrine - the cell signal signals itself
analog such as desmopressin (dDAVP) and assess
Paracrine - the cell signals the nearby cell
patient’s response
Oxytocin Amelioration of both polyuria and polydipsia
would be considered a positive response and
presumptive diagnosis of DI is mafe
It is a cyclic nonapeptide, with a disulfide bridge
Vasopressin excess leads to pathologic retention of
connecting amino acid residues 1 and 6
water
C terminus is amidated
Conivaptan and Tolvaptan (V2 receptor antagonists) -
Function: lactation, labor and parturition
for management of euvolemic hyponatremia due to
Positive Feedback Loop
vasopressin excess
Instead na patigilin ng oxytocin yung contraction,
mas magrerelease ng oxytocin to contract
Pitocin - a synthetic oxytocin to induce labor
Oxytocin has been shown to have effects on pituitary,
renal, cardiac, metabolic, and immune function
Vasopressin
Cyclic nonapeptide with an identical disulfide bridge; it
differs from oxytocin by only two amino acids
You might also like
- 68th AACC Annual Scientific Meeting Abstract eBookFrom Everand68th AACC Annual Scientific Meeting Abstract eBookNo ratings yet
- Hematology CruzDocument97 pagesHematology CruzSarah EugenioNo ratings yet
- CM, Other Body FluidsDocument76 pagesCM, Other Body FluidsStephany PolinarNo ratings yet
- Surgical Pathology For Dentistry Students - Surgical Pathology of Thyroid and Adrenal GlandsDocument38 pagesSurgical Pathology For Dentistry Students - Surgical Pathology of Thyroid and Adrenal Glandssorin niky mocanu100% (1)
- IlovemymomDocument149 pagesIlovemymomREYSYMAE CABRALNo ratings yet
- Lymphoid NeoplasmsDocument7 pagesLymphoid NeoplasmsMaribel SchullNo ratings yet
- Lymphoproliferative disorders diagnosis and treatmentDocument29 pagesLymphoproliferative disorders diagnosis and treatmentShaza ElkourashyNo ratings yet
- HEMA-1 Up To PG 30.-1-31Document31 pagesHEMA-1 Up To PG 30.-1-31Angela ReyesNo ratings yet
- Molecular Oncology in Gynecologic CancerDocument7 pagesMolecular Oncology in Gynecologic CancerChristine Evan HoNo ratings yet
- Liver Function TestDocument9 pagesLiver Function TestFarah Krisna Sadavao AndangNo ratings yet
- Immunopharmacology: Dr. Hamad AlshabiDocument8 pagesImmunopharmacology: Dr. Hamad AlshabiHamad Alshabi100% (1)
- Automation in Clinical ChemistryDocument28 pagesAutomation in Clinical ChemistryJoyce VitalNo ratings yet
- Interpretation of Liver Enzyme Tests - A Rapid GuideDocument3 pagesInterpretation of Liver Enzyme Tests - A Rapid Guidesserggios100% (2)
- Unit 3 Part 4 Organ-Specific Autoimmune DisordersDocument23 pagesUnit 3 Part 4 Organ-Specific Autoimmune DisordersReman AlingasaNo ratings yet
- Autoimmune DiseasesDocument41 pagesAutoimmune DiseasesGanesh V GaonkarNo ratings yet
- Antimicrobial Agents: Prof. Khaled H. Abu-ElteenDocument133 pagesAntimicrobial Agents: Prof. Khaled H. Abu-ElteenMing GamonganNo ratings yet
- 33-Hemostasis and Coagulation ProfileDocument40 pages33-Hemostasis and Coagulation ProfileOsman Mohamed MuhumedNo ratings yet
- Bone Marrow TransplantationDocument21 pagesBone Marrow TransplantationMorrison George100% (1)
- Lecture Notes in Medical Technology - Lecture #5 - THYROID FUNCTION TESTSDocument14 pagesLecture Notes in Medical Technology - Lecture #5 - THYROID FUNCTION TESTSKat JornadalNo ratings yet
- 5 - Must To Know Clinical MicrosDocument44 pages5 - Must To Know Clinical MicrosRudolph Jr. TaubNo ratings yet
- Clinical Chemistry 2 LAB: Electrolytes, Sodium, Potassium, ChloridesDocument2 pagesClinical Chemistry 2 LAB: Electrolytes, Sodium, Potassium, ChloridesEmiaj Francinne Mendoza100% (1)
- Clinical Chemistry Lecture: Exercise, Training EffectsDocument3 pagesClinical Chemistry Lecture: Exercise, Training EffectsHenry QuimbaNo ratings yet
- Red Blood Cell Anomalies: Elliptocytes & Oval MacrocyteDocument12 pagesRed Blood Cell Anomalies: Elliptocytes & Oval MacrocyteSHUPATUSSAI100% (1)
- Biochemical Makers of Cardiac DiseaseDocument45 pagesBiochemical Makers of Cardiac DiseaseSalman RashidNo ratings yet
- Lupus AnticoagulantDocument27 pagesLupus AnticoagulantAndrew Arnold David Villanueva100% (1)
- Hematology 1 NotesDocument40 pagesHematology 1 NotesAyessa SheinleeNo ratings yet
- CBCDocument12 pagesCBCDaNa Al-jomah100% (1)
- Automation in Clinical ChemistryDocument2 pagesAutomation in Clinical ChemistrySEBASTIEN ZOE RODRIGUEZNo ratings yet
- Diagnostic Cardiac EnzymesDocument27 pagesDiagnostic Cardiac Enzymesد.لطفي دحمانNo ratings yet
- Iron Metabolism: DR Mukhtiar BaigDocument58 pagesIron Metabolism: DR Mukhtiar BaigdrmukhtiarbaigNo ratings yet
- Laboratory Diagnosis of Hypersensitivity and AutoimmunityDocument41 pagesLaboratory Diagnosis of Hypersensitivity and AutoimmunityDenish Calmax AngolNo ratings yet
- Blood Components Where Do They Come From?: Introduction To HaematologyDocument11 pagesBlood Components Where Do They Come From?: Introduction To Haematologydorsa koraeiNo ratings yet
- Basic Examination of Urine - Dr. PinedaDocument20 pagesBasic Examination of Urine - Dr. PinedaElei GarciaNo ratings yet
- Therapeutics: Thyroid DisordersDocument24 pagesTherapeutics: Thyroid DisordersSharas FarhadNo ratings yet
- 2021 FA Microbiology ChangesDocument88 pages2021 FA Microbiology ChangesFlor FurmanNo ratings yet
- Premature Ovarian Failure Incidence Risk Factors ADocument4 pagesPremature Ovarian Failure Incidence Risk Factors Aamit danielNo ratings yet
- Diseases of ImmunityDocument13 pagesDiseases of ImmunityRose AnnNo ratings yet
- Quality Lectures - Pre-Analytic Variables - Dr. Tamer SolimanDocument323 pagesQuality Lectures - Pre-Analytic Variables - Dr. Tamer Solimanola bakryNo ratings yet
- CC1 - Topic 1Document11 pagesCC1 - Topic 1Marie MontemarNo ratings yet
- Molecular Diagnosis in HaematologyDocument23 pagesMolecular Diagnosis in HaematologyUmar'Farouq Oni100% (1)
- Non Protein CompoundsDocument64 pagesNon Protein CompoundsAbigail Mayled LausNo ratings yet
- TSH Acculite Clia Rev 4Document2 pagesTSH Acculite Clia Rev 4ghumantuNo ratings yet
- Examination of Urine Formation and CompositionDocument7 pagesExamination of Urine Formation and CompositionDaniel LamasonNo ratings yet
- Plasma ProteinsDocument8 pagesPlasma ProteinsAaryan50% (2)
- Thyroid Autoimmune DiseasesDocument21 pagesThyroid Autoimmune Diseasesmicheal1960No ratings yet
- Protein Metab 2 Dra. SantosDocument7 pagesProtein Metab 2 Dra. SantosMelissa SalayogNo ratings yet
- Endocrine 160110083024Document65 pagesEndocrine 160110083024Ryan CracknellNo ratings yet
- Antimicrobial DrugsDocument44 pagesAntimicrobial Drugsreza tavayefNo ratings yet
- HaematologyDocument68 pagesHaematologytapoolnoNo ratings yet
- Approved Nigerian National Blood PolicyDocument24 pagesApproved Nigerian National Blood PolicyUkaegbu Chibueze JnrNo ratings yet
- Component Therapy-Transfusion of TheDocument8 pagesComponent Therapy-Transfusion of TheGennelyn Ross Delos ReyesNo ratings yet
- Major Histocompatibility Complex Part 1 TranscriptDocument24 pagesMajor Histocompatibility Complex Part 1 Transcriptapi-273068056No ratings yet
- Intro To TDM and ToxicologyDocument46 pagesIntro To TDM and ToxicologyAl-hadad AndromacheNo ratings yet
- Enzymes Speed Up Cellular ReactionsDocument54 pagesEnzymes Speed Up Cellular ReactionsCesar Augusto Airampo Macedo100% (1)
- LABORATORY MEASUREMENTS OF PLATELET ACTIVITIESDocument73 pagesLABORATORY MEASUREMENTS OF PLATELET ACTIVITIESMary Lyka ReyesNo ratings yet
- Classification and Causes of Anemia ExplainedDocument30 pagesClassification and Causes of Anemia ExplainedhercolaniumNo ratings yet
- 1 Hemoglobinopathies BookDocument26 pages1 Hemoglobinopathies BookRhoda Lom-ocNo ratings yet
- C19 2 Hemopoiesis Eythropoiesis LeukopoiesisDocument11 pagesC19 2 Hemopoiesis Eythropoiesis Leukopoiesisnurul azisyah auraNo ratings yet
- Coagulation CascadeDocument4 pagesCoagulation CascadezainabNo ratings yet
- Staining & CytopathologyDocument12 pagesStaining & CytopathologyStephanie Kate ArriolaNo ratings yet
- STRASINGER: Study QuestionsDocument48 pagesSTRASINGER: Study QuestionsyannaNo ratings yet
- Art 6 Identify Your ArtDocument2 pagesArt 6 Identify Your ArtCamella Beatrice Lujan ValleNo ratings yet
- CC Wall NotesDocument10 pagesCC Wall NotesCamella Beatrice Lujan ValleNo ratings yet
- Molbog Villangca Hema 1A Compre Reviewer 2Document53 pagesMolbog Villangca Hema 1A Compre Reviewer 2Camella Beatrice Lujan ValleNo ratings yet
- BacteMycoViro Wall NotesDocument20 pagesBacteMycoViro Wall NotesCamella Beatrice Lujan ValleNo ratings yet
- Clinical Chemistry - NPNDocument7 pagesClinical Chemistry - NPNCamella Beatrice Lujan ValleNo ratings yet
- Recombinant DnaDocument35 pagesRecombinant DnaCamella Beatrice Lujan ValleNo ratings yet
- RBC ANOMALIES AND INCLUSIONS With Their Associated DiseasesDocument2 pagesRBC ANOMALIES AND INCLUSIONS With Their Associated DiseasesCamella Beatrice Lujan ValleNo ratings yet
- Tube Collection GuideDocument2 pagesTube Collection GuideCamella Beatrice Lujan ValleNo ratings yet
- Decalcification - Valle, Camella BS MLS 3BDocument1 pageDecalcification - Valle, Camella BS MLS 3BCamella Beatrice Lujan ValleNo ratings yet
- Bacteria Characteristic NotesDocument4 pagesBacteria Characteristic NotesCamella Beatrice Lujan ValleNo ratings yet
- How To Use An Automatic MicropipetteDocument3 pagesHow To Use An Automatic MicropipetteCamella Beatrice Lujan ValleNo ratings yet
- Reagent Strip Color ChartDocument1 pageReagent Strip Color ChartCamella Beatrice Lujan ValleNo ratings yet
- Gram Staining Is A Different Staining Method That Is Used To Differentiate Between Gram Positive From Gram NegativeDocument1 pageGram Staining Is A Different Staining Method That Is Used To Differentiate Between Gram Positive From Gram NegativeCamella Beatrice Lujan ValleNo ratings yet
- VALLE MLS 3B Dysplasia Anaplasia MetaplasiaDocument1 pageVALLE MLS 3B Dysplasia Anaplasia MetaplasiaCamella Beatrice Lujan ValleNo ratings yet
- Basic Hematologic TerminologiesDocument1 pageBasic Hematologic TerminologiesCamella Beatrice Lujan ValleNo ratings yet
- PPE - SafetyDocument3 pagesPPE - SafetyCamella Beatrice Lujan ValleNo ratings yet
- Oral Test in Practical Research 2Document9 pagesOral Test in Practical Research 2Junlei GaribayNo ratings yet
- Choosing Ayurveda As A Healthcare PractiDocument16 pagesChoosing Ayurveda As A Healthcare PractiAndie PebblesNo ratings yet
- Architecture Statement of PurposeDocument4 pagesArchitecture Statement of PurposeAZAR HOSNo ratings yet
- Find The Thévenin Equivalent With Respect To The 7k Ohm ResistorDocument27 pagesFind The Thévenin Equivalent With Respect To The 7k Ohm ResistorVipan SharmaNo ratings yet
- 2 Saliva PhysiologyDocument20 pages2 Saliva PhysiologyvelangniNo ratings yet
- Writing Noble & Upper-Class CharactersDocument179 pagesWriting Noble & Upper-Class CharactersDobrila ĐokićNo ratings yet
- Babylonian-Egyptian Ancient CivilizationDocument34 pagesBabylonian-Egyptian Ancient CivilizationRiza Mae BayoNo ratings yet
- DCC - RPG Errata PDFDocument3 pagesDCC - RPG Errata PDFPaul StraitNo ratings yet
- Labor JurisdictionDocument37 pagesLabor JurisdictionChoystel Mae Artigas100% (1)
- REduce BAil 22Document2 pagesREduce BAil 22Pboy SolanNo ratings yet
- Lec 4 - Understanding Culture and Cultural Changes in IndiaDocument45 pagesLec 4 - Understanding Culture and Cultural Changes in Indiabrokenheart1984No ratings yet
- Part 5&6.cronbach Alpha and Sample Size ComputationDocument8 pagesPart 5&6.cronbach Alpha and Sample Size ComputationHazel AnnNo ratings yet
- Lesson 4-The Taximan StoryDocument3 pagesLesson 4-The Taximan StoryZian Tallongon100% (2)
- A Literature Review On The Vehicle Routing Problem With Multiple Depepots PDFDocument15 pagesA Literature Review On The Vehicle Routing Problem With Multiple Depepots PDFcarandatruNo ratings yet
- Contextual Factors Chart1Document4 pagesContextual Factors Chart1api-213553729No ratings yet
- Poka YokeDocument25 pagesPoka YokepatilpradnyaNo ratings yet
- CS602 Current Final Term Papers 2018 To 2020Document3 pagesCS602 Current Final Term Papers 2018 To 2020Jawad AliNo ratings yet
- Constructing Worlds Photography and ArchDocument6 pagesConstructing Worlds Photography and ArchRodrigo AlcocerNo ratings yet
- LT033 PDFDocument38 pagesLT033 PDFAlexandr ChuvakovNo ratings yet
- OLD ENGLISH LITERATURE: ELEGIES, RELIGIOUS POEMS, RIDDLES, AND CHARMSDocument6 pagesOLD ENGLISH LITERATURE: ELEGIES, RELIGIOUS POEMS, RIDDLES, AND CHARMSCodruța Elena CociugNo ratings yet
- GEO123 Worksheet 8Document4 pagesGEO123 Worksheet 8Hilmi HusinNo ratings yet
- SHCT 167 Reeves - English Evangelicals and Tudor Obedience, C. 1527-1570 2013 PDFDocument222 pagesSHCT 167 Reeves - English Evangelicals and Tudor Obedience, C. 1527-1570 2013 PDFL'uomo della Rinascitá100% (1)
- Tu Cuerpo Habla Enric CorberaDocument70 pagesTu Cuerpo Habla Enric CorberaJohn Freddy Villa CastroNo ratings yet
- Activity Guide and Evaluation Rubric - Activity 7 - Creating A WIX PageDocument5 pagesActivity Guide and Evaluation Rubric - Activity 7 - Creating A WIX PageLina VergaraNo ratings yet
- ACCFA V CUGCO Case DigestDocument2 pagesACCFA V CUGCO Case DigestLoren yNo ratings yet
- UWORLD Notes by Subject (Main Division) (Usmle Grassroots)Document80 pagesUWORLD Notes by Subject (Main Division) (Usmle Grassroots)Mital Bhakta83% (18)
- Caste and Class An Interlinked ViewDocument12 pagesCaste and Class An Interlinked ViewghisaramNo ratings yet
- Emcee King & QueenDocument8 pagesEmcee King & QueenMaryHazelClaveBeniga100% (10)
- 3 Week Lit 121Document48 pages3 Week Lit 121Cassandra Dianne Ferolino MacadoNo ratings yet
- Clinical Lab TechnqDocument67 pagesClinical Lab TechnqRatnamala SarmaNo ratings yet