Professional Documents
Culture Documents
10 Adrenergic Agonists (Notes) Atf
Uploaded by
Feven AbrahamOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 Adrenergic Agonists (Notes) Atf
Uploaded by
Feven AbrahamCopyright:
Available Formats
AfraTafreeh.
com
Last edited: 9/28/2022
AUTONOMIC PHARMACOLOGY | ADRENERGIC AGONISTS
Autonomic Pharmacology | Adrenergic Agonists Medical Editor: Ana, Jude
OUTLINE
I) ADRENERGIC NEURONS & RECEPTORS III) ALPHA+BETA AGONIST (D) SUMMARY
(A) NOREPINEPHRINE (A) NOREPINEPHRINE V) APPENDIX
(B) EPINEPHRINE (B) EPINEPHRINE + DOPAMINE VI) REVIEW QUESTIONS
TYPES OF AGONISTS IV) GRAPHICAL REPRESENTATIONS OF VII) REFERENCES
II) BETA-ADRENERGIC AGONISTS CVS EFFECTS OF NOREPINEPHRINE,
(A) BETA-1 AGONISTS EPINEPHRINE, & ISOPROTERENOL
(B) BETA-1+2 AGONIST (A) NOREPINEPHRINE
(C) BETA-2 AGONIST (B) EPINEPHRINE
(D) BETA-3 AGONIST (C) ISOPROTERENOL
I) ADRENERGIC NEURONS & RECEPTORS
(A) NOREPINEPHRINE
(1) Synthesis
Tyrosine enters the neuron through a Na channel
cotransport
Conversion from tyrosine to L-DOPA
L-DOPA gets converted to Dopamine
Dopamine gets converted to Norepinephrine inside
intracellular vesicles
Action potential activates voltage gated Ca++ channels
(2) Receptors
(i) 1 receptor
(iii) 1 receptor
o Works through the Phospholipase C pathway
o Works through stimulation of the Adenylate cyclase
▪ Increases IP3 & DAG
pathway on the cardiac muscle
• Increases intracellular Ca++ in smooth muscle
▪ Increases cAMP
cells
• Increases intracellular Ca++
(i) 2 & 3 receptors
(ii) 2 receptor
o Works through stimulation of the Adenylate cyclase
o Works through the Adenylate cyclase pathway pathway on the cardiac muscle
▪ Inhibits cAMP ▪ Increases cAMP
• Decreases release of neurotransmitters and • Increases intracellular Ca++
hormones
Autonomic Pharmacology | Adrenergic Agonists PHARMACOLOGY: NOTE #10. 1 of 13
(3) Metabolism & recycling
(i) COMT
(ii) Reuptake
a. Enter the vesicles to be released into the
synaptic cleft again.
b. Get metabolized by the MAO enzymes
inside the mitochondria and be broken
down into inactive metabolites.
(B) EPINEPHRINE
Epinephrine and norepinephrine are produced by the
adrenal medulla and released after sympathetic stimuli. (i) Difference between NE & EPI
AfraTafreeh.com
TYPES OF AGONISTS
1) Direct agonists: Bind directly to the adrenergic receptors
to stimulate its effects.
2) Indirect agonists: Work through increasing NE
accumulation by.
a. Inhibiting the COMT enzymes
b. Inhibiting the NE uptake transporters (NERT)
c. Inhibiting the MAO enzymes
3) Mixed agonists: Bind to adrenergic receptors and
increase NE accumulation.
2 of 13 PHARMACOLOGY: NOTE #10. Autonomic Pharmacology | Adrenergic Agonists
AfraTafreeh.com
II) ADRENERGIC TARGET ORGANS EFFECTS
1 receptor 2 receptor 1 receptor 2 receptor 3 receptor
Cardiac muscle - - +++ + +
Skeletal muscle - - - ++ -
Vascular smooth muscle +++ + - ++ +
Bronchial smooth muscle - - - ++ -
Liver + - - +++ -
Adipose tissue + + + - ++
CNS ++ ++ ++ ++ -
Bladder neck / prostate +++ + - - +++
(A) 1 RECEPTORS (B) 2 RECEPTORS
(i) Smooth muscle contraction (i) Pre-synaptic nerve terminal
o Located on the pre-synaptic nerve terminal
a. Decrease of blood flow
b. Increase of blood pressure
REMEMBER
BP= SVR X Cardiac Output
(ii) Sphincters contraction
i. Urethra
ii. Rectus and anus
(ii) Pancreatic cells
(iii) Dilator Pupillae contraction
Autonomic Pharmacology | Adrenergic Agonists PHARMACOLOGY: NOTE #10. 3 of 13
(C) 1 RECEPTORS
Located on two areas of the heart and they increase CO (iii) Juxtaglomerular cells
through two different ways
(i) SA and AV node
o Increase conduction
o Vasoconstriction
o Increase ADH
(ii) Cardiac muscle contraction
o Increase contractility
(D) 2 RECEPTORS
(i) Vasodilation
o Vessels supplying the heart and skeletal muscles
AfraTafreeh.com
(ii) Bronchial smooth muscle
(iv) Uterus
(iii) Pancreatic cells
(E) 3 RECEPTORS
(i) Adipose tissue
(ii) Detrusor muscle contraction
4 of 13 PHARMACOLOGY: NOTE #10. Autonomic Pharmacology | Adrenergic Agonists
AfraTafreeh.com
III) ALPHA 1 AGONISTS IV) ALPHA 2 AGONISTS
(1) On arteries → Increase of BP
(A) CLONIDINE
(i) Effects on the CNS
(2) On veins → Increase venous return → Increase BP o Inhibit the release of NE
o Systemic effects
(B) PHENYLEPHRINE
(i) Blood pressure effects
(ii) Effects on the dilator pupilae
(iii) Effect on the nasal cavity vessels
(B) ALPHA-METYLDOPA
Phenylephrine adverse effects: Reflex bradycardia
(C) MIDODRINE
▪ Very good at improving venous return
Autonomic Pharmacology | Adrenergic Agonists PHARMACOLOGY: NOTE #10. 5 of 13
V) BETA-ADRENERGIC AGONISTS
(A) BETA-1 AGONISTS (B) BETA-1+2 AGONIST
Figure 1. Effects of β1 agonists. Figure 2. Effects of β1+2 agonists (i.e. isoproterenol).
Overall effects include: (1) Isoproterenol
o Work on the nodal system (SA, AV nodes) → ↑HR
o Work on contractile cells → ↑contractility → ↑CO Equal affinity for β1 and β2 (β1=β2)
(1) Dobutamine (i) Β1 effects:
Primary β1 agonist ↑HR
Increases HR o Indicated in bradycardia (primary indication)
o Indicated in symptomatic bradycardia ↑contractility → ↑CO
Increases CO to get blood out of heart
o Indicated in acute heart failure or cardiogenic
(ii) Β2 effects:
shock Vasodilates blood vessels → ↓SVR → ↓BP
Adverse effects: o Even though it increases CO, it CANNOT be used in
o Tachycardia/tachyarrhythmias patients with AHF and cardiogenic shock because it
o Exacerbates angina AfraTafreeh.com can ↓BP especially if patients are already hypotensive
▪ Squeezing heart → ↑energy demands; therefore in Relaxes bronchial smooth muscle (bronchodilate)
CAD where ↓oxygen, it can exacerbate angina o Rarely used in asthma
▪ Used in stress test Adverse effects: Tachycardia
6 of 13 PHARMACOLOGY: NOTE #10. Autonomic Pharmacology | Adrenergic Agonists
AfraTafreeh.com
(C) BETA-2 AGONIST (D) BETA-3 AGONIST
Figure 4. Effects of β3 agonists.
(1) Mirabegron
Β3 receptors inhibit the contraction of the detrusor muscle
→ inhibit urination
Indicated for patients with overactive bladder or urinary
urgency
Figure 3. Effects of β2 agonists.
(1) Respiratory Effects
Great bronchodilator
o Good in asthma and COPD
(i) Albuterol
Short-acting β2 agonist (SABA)
Acute treatment in asthma and COPD
(ii) Salmeterol, Formoterol
Long-acting β2 agonist (LABA)
Chronic treatment of COPD and/or asthma
(iii) Terbutaline
Short-acting β2 agonist (48 hrs)
Better used in severe asthma
(2) Uterine Effects
Good for premature labor, as a tocolytic
(i) Terbutaline
Helps in delay of preterm labor
(3) Na-K-ATPase
Increase and stimulates the Na-K-ATPase
o Pumps K into the cell and Na out of the cell
(i) Albuterol
Indicated in hyperkalemia since we want excess K to
shift into the cell
Adverse effect: Drop in K
(4) Other Effects
↑glucose in the blood
o !! Watch out for hyperglycemia
↑afferent and efferent signals to the muscle spindles →
tremors
Autonomic Pharmacology | Adrenergic Agonists PHARMACOLOGY: NOTE #10. 7 of 13
VI) ALPHA+BETA AGONIST
(A) NOREPINEPHRINE (B) EPINEPHRINE + DOPAMINE
Figure 5. Effects of norepinephrine.
⍺>β
o Primarily an ⍺ agonist; β activity at higher doses Figure 6. Effects of epinephrine and dopamine.
o Affects the nodal system at higher doses Epinephrine: β > ⍺
Dopamine: D (dopamine receptor) > β > ⍺
(1) Β1 effects (at higher doses):
(1) B1 effects:
↑↑HR
↑↑contractility → ↑↑CO ↑↑HR → ↑↑CO
o Indicated in bradycardia and for epinephrine, cardiac
(2) A1 effects:
arrest
Constriction of the blood vessels → ↑SVR → ↑DBP (just ↑↑contractility → ↑↑CO
like phenylephrine) o Indicated in AHF and cardiogenic shock
Squeezing more blood into the heart → ↑venous return →
↑preload → ↑SV → ↑CO → ↑SBP AfraTafreeh.com
In the blood vessels, there are ⍺1 and β2 receptors. At
low doses, epinephrine prefers the β2 receptor whereas
Indicated in cases of hypotension (shock, most
commonly in septic shock) at higher doses, it prefers ⍺1 receptors.
o Low doses:
(3) Reflex Bradycardia ▪ ↓⍺1 receptors → ↓SVR → ↓BP
Vasoconstriction → (+) barorceptors → send signals to ▪ ↑β2 receptors → ↓SVR → ↓BP
the CNS → vagus nerve → releases acetylcholine → o High doses:
reflex bradycardia ▪ ↑⍺1 receptors → ↑SVR → ↑BP
o When combined with the mild ↑HR by the β1 ▪ Only at high doses do epinephrine and
receptors → ↓HR overall dopamine have effects on BP
▪ Indicated in hypotension (septic, cardiogenic)
(4) Normalization of CO
(2) B2 effects:
Vasoconstriction → ↑SVR → ↑afterload → ↓SV → ↓CO
o ↓CO brought by the ⍺1 effect is normalized by the Bronchodilation
slight ↑CO by β1 Can be used in asthma, COPD, and anaphylactic shock
(particularly epinephrine)
In clinical settings, Zach has not yet seen a patient o Dopamine CANNOT be used in these conditions as it
who experienced reflex bradycardia or a drop in CO does not have enough β2 agonist activity as
but these things are to consider for the Boards. compared to epinephrine
8 of 13 PHARMACOLOGY: NOTE #10. Autonomic Pharmacology | Adrenergic Agonists
AfraTafreeh.com
VII) GRAPHICAL REPRESENTATIONS OF CVS EFFECTS OF NOREPINEPHRINE, EPINEPHRINE, & ISOPROTERENOL
Comparing the vascular effects of norepinephrine, epinephrine, and isoproterenol
Determines how these agonists affect the following parameters: HR, BP, SVR, CO, MAP, and SVR
(A) NOREPINEPHRINE (B) EPINEPHRINE
Figure 7. Graphical representation of parameters in Figure 8. Graphical representation of parameters in
norepinephrine. epinephrine.
Recall: ⍺ > β Recall: β > ⍺
Table 1. Effects of norepinephrine on CVS parameters. Table 2. Effects of epinephrine on CVS parameters.
REMARKS EFFECT REMARKS
EFFECT
Reflex bradycardia d/t ⍺1 receptor Works in the conduction system through
Deflection points d/t ↑β1 receptors the β1 receptors
↓HR ↑↑HR
Theoretically, it is similar to phenylephrine o No reflex bradycardia because there
are no ⍺1 receptors
↑↑SBP d/t the following:
o ⍺1 receptors on the arteries and veins ↑SBP d/t ↑contractility from β1 receptors
o β1 receptors → ↑CO → ↑SBP
↑↑SBP o SBP is dependent on afterload,
↑↑DBP DBP is dependent upon SVR and blood ↑SBP preload, and contractility
volume (BV) ↓DBP
o ⍺1 receptors increases DBP ↓DBP because of β2 > ⍺1
o β2 causes vasodilation
High SVR d/t ⍺1 receptors o ⍺1 causes vasoconstriction
o ⍺1: squeezes vessels → ↑SVR
↑SVR o There is correlation between SVR and ↓SVR Correlated with DBP
DBP
↑↑CO Due to β1 receptor activity
β1: ↑CO
No effect ⍺1: ↑afterload → ↓CO Because of ↓DBP and ↑PP → evens out
on CO Both of these cancel out → evens out the leading to slight increase in MAP
effect on CO ↑MAP Significant increase IF there is ⍺1
receptor activity in higher doses
Dependent on DBP, which is dependent
on SVR ↑PP Due to ↑SBP and ↓DBP
o ↑↑DBP → ↑↑SVR → ↑↑MAP
↑↑MAP 2 1
𝑀𝐴𝑃 = 3 (𝐷𝐵𝑃) + 3 (𝑆𝐵𝑃)
1
𝑀𝐴𝑃 = 𝐷𝐵𝑃 + 3 (𝑃𝑃)
Pulse pressure is the difference between
SBP and DBP
↑PP Slight increase in PP because both SBP
and DBP increase
Autonomic Pharmacology | Adrenergic Agonists PHARMACOLOGY: NOTE #10. 9 of 13
(C) ISOPROTERENOL (D) SUMMARY
Table 4. Summary of the effects of norepinephrine,
epinephrine, and isoproterenol on CVS parameters.
NE EPI IPT
HR ↓ ↑↑ ↑↑
SBP ↑↑ ↑ ↑↑
DBP ↑↑ ↓ ↓↓
SVR ↑ ↓ ↓↓
CO NE ↑↑ ↑↑
MAP ↑↑ ↑ ↓
PP ↑ ↑ ↑↑
*NE: norepinephrine
*EPI: epinephrine
Figure 9. Graphical representation of CVS parameters in *IPT: isoproterenol
isoproterenol. *NE: no effect
Recall: β1 = β2; no ⍺-receptor activity
Table 3. Effects of isoproterenol on CVS parameters.
EFFECT REMARKS
↑↑HR D/t β1 receptor activity
↑↑SBP d/t ↑↑contractility from β1 receptor
↑↑SBP ↓↓DBP d/t intense vasodilation from β2
↓↓DBP receptor activity → ↓↓SVR
↓↓SVR Due to ↓↓SVR from β2 receptor activity
Dependent upon HR, CO, preload, and
↑↑CO contractility
↑↑contractility + ↑↑HR → ↑↑CO
Dependent on DBP, which is a more
↓MAP important factor
↓↓DBP with ↑PP
↑↑PP D/t ↑↑SBP and ↓↓DBP
AfraTafreeh.com
10 of 13 PHARMACOLOGY: NOTE #10. Autonomic Pharmacology | Adrenergic Agonists
AfraTafreeh.com
VIII) APPENDIX
(1) ADRENERGIC TARGET ORGANS EFFECTS
1 receptor 2 receptor 1 receptor 2 receptor 3 receptor
Cardiac muscle - - +++ + +
Skeletal muscle - - - ++ -
Vascular smooth muscle +++ + - ++ +
Bronchial smooth muscle - - - ++ -
Liver + - - +++ -
Adipose tissue + + + - ++
CNS ++ ++ ++ ++ -
Bladder neck / prostate +++ + - - +++
ADVERSE
DRUG DRUG EFFECTS INDICATIONS REMARKS
EFFECTS
CLASS
β-adrenergic agonists
Works on the nodal system ↑HR: symptomatic
β1 → ↑HR bradycardia Tachycardia
Dobutamine
agonists Works on contractile cells → ↑CO: AHF or cardiogenic ↑angina
↑contractility → ↑CO shock
CANNOT be used in
β1 = β2
patients with AHF and
β1: ↑HR and ↑CO
cardiogenic shock
β1+2 β2: Bradycardia (primary
Isoproterenol Tachycardia because it can ↓BP
agonists o ↓BP through indication) especially if patients
vasodilation → ↓SVR
are already
o Bronchodilate
hypotensive
Respiratory: bronchodilator Asthma and COPD:
Uterine: tocolytic o Albuterol: acute
Others: treatment
o (+) Na-K-ATPase o Salmeterol, formoterol:
Albuterol (SABA) activity = pumps K into Drop in K →
chronic treatment
β2 Salmeterol, hypokalemia
the cell and Na out of o Terbutaline: acute
agonists Formoterol (LABA) Hyperglycemia
the cell treatment in severe
Terbutaline (SABA) Tremors
o ↑serum glucose asthma
o ↑afferent and efferent Terbutaline: tocolytic; delay
signals to the muscle premature labor
spindles Albuterol: hyperkalemia
β3 (-) contraction of the detrusor Overactive bladder or urinary
Mirabegron
agonists muscle → ↓urination urgency
Combined ⍺ and β agonist
(⍺ > β)
β1: ↑↑HR, ↑↑contractility (=
Hypotension Reflex bradycardia
Norepinephrine ↑↑CO)
Shock (septic, in particular) Normalization of CO
⍺1: ↑DBP through
vasoconstriction, ↑SBP
Only in high doses
do epi and
β > ⍺ (epinephrine) Bradycardia dopamine have BP
⍺+β
D > β > ⍺ (dopamine) Cardiac arrest effects
agonists
β1: ↑↑HR, ↑↑contractility (epinephrine) Dopamine CANNOT
Epinephrine and (=CO) AHF and cardiogenic shock be used in asthma,
Dopamine o Low doses: ↓⍺1 = ↓BP; Asthma, COPD, COPD, and
↑β2 = ↓BP anaphylactic shock anaphylaxis
o High doses: ↑⍺1 = ↑BP (epinephrine) because it does not
β2: bronchodilation Hypotension (high doses) have enough β2
agonist activity vs
epinephrine.
Autonomic Pharmacology | Adrenergic Agonists PHARMACOLOGY: NOTE #10. 11 of 13
IX) REVIEW QUESTIONS
4) Which of the following is correct regarding
adrenergic neurotransmission?
a) Norepinephrine is the major neurotransmitter
released from sympathetic nerve terminals.
b) Norepinephrine is mainly released from the adrenal
glands.
c) TCA and cocaine prevent the release from
norepinephrine from the nerve terminals.
d) Monoamine oxidase (MAO) converts dopamine to
norepinephrine in the nerve terminal.
5) Which of the following adrenergic drugs is used in
the treatment of overactive bladder?
a) Epinephrine
b) Dobutamine
c) Phenylephrine
d) Mirabegron
6) Which of the following classes of adrenergic agents
has utility in the management of hypertension?
a) ⍺1 agonist
b) ⍺2 agonist
c) β1 agonist
d) β3 agonist
7) Which of the following is correct regarding
responses mediated by the adrenergic receptors?
a) Stimulation of alpha1 receptors inc BP
b) Stimulation of sympathetic presynaptic alpha2
receptors inc NE release
c) Stimulation of B2 receptors inc HR (tachycardia)
d) Stimulation of B2 receptors causes
bronchoconstriction
8) An asthma patient was given a non-selective beta-
AfraTafreeh.com
agonist to relieve bronchoconstriction. Which
adverse effect would you expect in this patient?
a) Bradycardia
b) Tachycardia
c) Hypotension
d) Worsening bronchoconstriction
9) A 22-year-old male is brought to the ER with
suspected cocaine overdose. Which of the following
symptoms is most likely in this patient?
a) Hypertension
b) Bronchoconstriction
c) Bradycardia
d) Miosis (pupil constriction)
X) REFERENCES
12 of 13 PHARMACOLOGY: NOTE #10. Autonomic Pharmacology | Adrenergic Agonists
AfraTafreeh.com
XI) ANSWERS TO QUESTIONS
QUESTION ANSWER
1) Sarin is a nerve gas that is an organophosphate C. Atropine
cholinesterase inhibitor. Which agent could be used
as an antidote to sarin poisoning? Organophosphate cholinesterase inhibitor are irreversible
a. Pilocarpine drugs.
b. Carbachol
c. Atropine Cholinesterase inhibitors are going to increase ACh in the
d. Physostigmine synapse which can lead to cholinergic crisis.This drug blocks
the effect of ACh at different types of muscarinic receptors.
2) A patient with asthma was prescribed a β2 agonist for B. Ipratropium
acute relief of bronchospasm, but did not respond to
treatment. Which drug is the most likely next option Β2 agonists are supposed to work in the bronchial smooth
for this patient? muscle leading to bronchodilation. If beta-2 agonists do not
a. Benztropine work, other drugs like a muscarinic antagonist against to MR-3
b. Ipratropium can work in bronchodilation. An example would be
c. Oxybutynin ipratropium.
d. Physostigmine
3) A 50-year-old male who is noncompliant with C. Tiotropium
medications was recently diagnosed with COPD. His
physician would like to prescribed an inhaled Ipratropium is for acute relief of bronchoconstriction. For this
anticholinergic that is dosed once or twice daily. case, a longer acting muscarinic antagonist dosed once or
Which drug is most appropriate for this patient? twice daily therefore tiotropium.
a. Atropine
a. Ipratropium
b. Tiotropium
c. Trospium
4) Which is the most effective drug for motion sickness C. Scopolamine
for a person planning to go on a cruise?
a. Atropine Remember that the vestibular function is connected to the
b. Fesoterodine emetic center in the medulla that has a lot of muscarinic
c. Scopolamine receptors. A drug that can block the muscarinic receptors in
d. Tropicamide the emetic center is scopolamine.
5) Which drug is useful in treating sinus bradycardia? A. Atropine
a. Atropine
a. Cisatracurium Sinus bradycardia is usually due to the vagus nerve that
b. Neostigmine releases too much ACh to the AV node leading to slowing
c. Succinylcholine down of heart rate. The best drug to inhibit this is atropine.
Autonomic Pharmacology | Adrenergic Agonists PHARMACOLOGY: NOTE #10. 13 of 13
You might also like
- ED Dilution Guide 2018 - Jan 2019Document42 pagesED Dilution Guide 2018 - Jan 2019asyrafrusydi9901No ratings yet
- Prehospital MedicationsDocument123 pagesPrehospital Medicationshilwaalfi100% (1)
- 02 AntiarrhythmicAgentsDocument83 pages02 AntiarrhythmicAgentsSiddhant BanwatNo ratings yet
- Vasoactive DrugsDocument61 pagesVasoactive DrugsAde Gustina SiahaanNo ratings yet
- Arrhythmia 2Document31 pagesArrhythmia 2rittvedNo ratings yet
- Endocrine Notes - All in One FileDocument182 pagesEndocrine Notes - All in One FilekjNo ratings yet
- Traumatic Brain InjuryDocument49 pagesTraumatic Brain InjuryCHANGEZ KHAN SARDARNo ratings yet
- Drugs in Cardiac EnmergenciesDocument94 pagesDrugs in Cardiac EnmergenciesVijayan VelayudhanNo ratings yet
- Arrhythmias: Sing Khien Tiong Gpst1Document34 pagesArrhythmias: Sing Khien Tiong Gpst1preethi preethaNo ratings yet
- Patterns of RespirationDocument67 pagesPatterns of Respirationsteven hkNo ratings yet
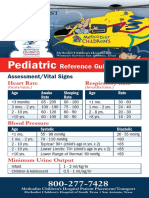
- AirCare Pediatric Reference GuideDocument8 pagesAirCare Pediatric Reference GuideN/ANo ratings yet
- Guide to Respiratory Exam - OSCE ChecklistDocument33 pagesGuide to Respiratory Exam - OSCE ChecklistBasmah 7No ratings yet
- 4 Adrenergic and Anti-Adrenergic DrugsDocument51 pages4 Adrenergic and Anti-Adrenergic DrugsLoai Mohammed IssaNo ratings yet
- Paramedic Exam Guide to Immunizations & Research MethodsDocument21 pagesParamedic Exam Guide to Immunizations & Research MethodsBarry GruenbaumNo ratings yet
- ICU IV Infusion GuidelinesDocument2 pagesICU IV Infusion Guidelinessgod34No ratings yet
- Free Medical ECG Interpretation PresentationsDocument30 pagesFree Medical ECG Interpretation PresentationsRohini SelvarajahNo ratings yet
- Phtls 9e Print Phtls Textbook With Digital Access To Course Manual EbookDocument14 pagesPhtls 9e Print Phtls Textbook With Digital Access To Course Manual EbookRoi Ben DavidNo ratings yet
- HW InotropesDocument3 pagesHW InotropesNatalie YeohNo ratings yet
- Adrenergic Agonist and AntagonistDocument35 pagesAdrenergic Agonist and AntagonistFirjat AfiataNo ratings yet
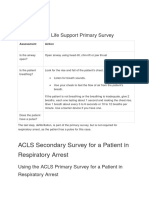
- ACLS Secondary Survey For A Patient in Respiratory Arrest: BLS Arrest Figure 1. Basic Life Support Primary SurveyDocument30 pagesACLS Secondary Survey For A Patient in Respiratory Arrest: BLS Arrest Figure 1. Basic Life Support Primary SurveyLusia NataliaNo ratings yet
- The Brain and Cranial NervesDocument4 pagesThe Brain and Cranial NervesJet ToralbaNo ratings yet
- Drug List: Medication Adult Dosing Pediatric DosingDocument14 pagesDrug List: Medication Adult Dosing Pediatric DosingAndrew JamesNo ratings yet
- EMS Calculating Drip RatesDocument17 pagesEMS Calculating Drip Ratesزهرة النرجسNo ratings yet
- 1 Ep PDFDocument35 pages1 Ep PDFMiguel LizarragaNo ratings yet
- 360 Sled Kit Project Plans: Included ItemsDocument12 pages360 Sled Kit Project Plans: Included ItemsJaime Montiel100% (1)
- Management of Shock: Role of Inotropic & Vasoactive DrugsDocument50 pagesManagement of Shock: Role of Inotropic & Vasoactive DrugsbajaocNo ratings yet
- Medications Used in Code Blue EmergenciesDocument24 pagesMedications Used in Code Blue EmergenciesAhmed Ali Mohammed AlbashirNo ratings yet
- ACLS Algorithms Adult 2010 Revised May 31 2011Document12 pagesACLS Algorithms Adult 2010 Revised May 31 2011arturschander3614No ratings yet
- Computation of Common Vasoactive DripsDocument23 pagesComputation of Common Vasoactive DripsRoxanneGailBigcasGoleroNo ratings yet
- MN105613 PICU2022 Book ProofDocument60 pagesMN105613 PICU2022 Book ProofErwin Dela GanaNo ratings yet
- ST - Elevation Myocardial InfarctionDocument25 pagesST - Elevation Myocardial InfarctionJo CanensNo ratings yet
- The Body Fluid CompartmentsDocument6 pagesThe Body Fluid CompartmentsAlya Putri KhairaniNo ratings yet
- Greater Sydney Area HEMS Prehospital RSI ManualDocument20 pagesGreater Sydney Area HEMS Prehospital RSI ManualMiguel XanaduNo ratings yet
- Pharmacotherapy of Cardiac ArrhythmiasDocument68 pagesPharmacotherapy of Cardiac ArrhythmiasABREHAM BUKULONo ratings yet
- Drugs Used for Treatment Stable Angina PectorisDocument29 pagesDrugs Used for Treatment Stable Angina PectorisAditya Andra PerdanaNo ratings yet
- Capnography and Its ApplicationsDocument37 pagesCapnography and Its ApplicationsTraceNo ratings yet
- Cardiac Arrythmias in The ED Menbeu Edited From AnaDocument106 pagesCardiac Arrythmias in The ED Menbeu Edited From AnaTemesgen Geleta100% (1)
- Pharm Fall Cardiovascular Pharmacology Study Guide-106Document47 pagesPharm Fall Cardiovascular Pharmacology Study Guide-106sean liyanageNo ratings yet
- Poison/drug-Induced Tachycardia, 2/3 Heart Blocks: DigoxinDocument2 pagesPoison/drug-Induced Tachycardia, 2/3 Heart Blocks: DigoxinimperiouxxNo ratings yet
- ELECTROCARDIOGRAM by Aldrin Jayson AlmadenDocument23 pagesELECTROCARDIOGRAM by Aldrin Jayson AlmadenItsMe AJNo ratings yet
- KegawatdaruratanDocument164 pagesKegawatdaruratanmeida astriani gozaziNo ratings yet
- 2 Cardiovascular System: Describe The Systemic Circulation in The Body and Give Its ImportanceDocument28 pages2 Cardiovascular System: Describe The Systemic Circulation in The Body and Give Its ImportanceBhavin ChangelaNo ratings yet
- Advanced Cardiovascular Life Support (ACLS)Document73 pagesAdvanced Cardiovascular Life Support (ACLS)maya_fitrianaNo ratings yet
- ECG Dysrhthmias IIIDocument31 pagesECG Dysrhthmias IIIAmani KayedNo ratings yet
- HBP C315HIS Implant Procedure-eLearnDocument35 pagesHBP C315HIS Implant Procedure-eLearnRichiNo ratings yet
- Adrenergic and NonadrenergicDocument49 pagesAdrenergic and Nonadrenergicsweta sumanNo ratings yet
- Clinical Examination of CVSDocument33 pagesClinical Examination of CVSmahnoorNo ratings yet
- Anasthetic DrugsDocument62 pagesAnasthetic DrugsMilda InayahNo ratings yet
- Alpha and beta adrenergic receptor effectsDocument1 pageAlpha and beta adrenergic receptor effectssas345sas345No ratings yet
- ICE DrugsDocument2 pagesICE DrugsRichelle FrondaNo ratings yet
- Cardiac Output: Dr. AthulyaDocument29 pagesCardiac Output: Dr. AthulyaamrendraNo ratings yet
- Hemodynamic Drug InfusionsDocument45 pagesHemodynamic Drug InfusionsDawit MucheNo ratings yet
- Medication DilutionDocument22 pagesMedication DilutionYaser Salman100% (1)
- Problems With OxygenationDocument92 pagesProblems With OxygenationEbiNo ratings yet
- MCEM B CVS TachycardiaDocument12 pagesMCEM B CVS TachycardiaRajin MaahiNo ratings yet
- National ECG Workshop AIMST MMA 2015Document217 pagesNational ECG Workshop AIMST MMA 2015Sara100% (1)
- Autonomic Nervous System - Part 1Document8 pagesAutonomic Nervous System - Part 1karageeNo ratings yet
- Pharmacology High YieldDocument167 pagesPharmacology High YieldAbdelaziz Shokry100% (1)
- Review of PharmacologyDocument12 pagesReview of PharmacologyqueenNo ratings yet
- 11 Adrenergic Antagonists (Notes) AtfDocument14 pages11 Adrenergic Antagonists (Notes) AtfAnuki TodriaNo ratings yet
- Visual Mnemonics For Biochemistry PDFDocument162 pagesVisual Mnemonics For Biochemistry PDFMahin Rahman100% (2)
- Everything You Wanted To Know About ADHD But Forgot You Wanted To AskDocument76 pagesEverything You Wanted To Know About ADHD But Forgot You Wanted To AskPola PremNo ratings yet
- 41.5A: Epinephrine and Norepinephrine: Key PointsDocument2 pages41.5A: Epinephrine and Norepinephrine: Key PointsAshley MudzingwaNo ratings yet
- Measureable Changes in The Neuro-Endocrinal Mechanism Following Spinal Manipulation - 2015Document6 pagesMeasureable Changes in The Neuro-Endocrinal Mechanism Following Spinal Manipulation - 2015Renan O. Pravatta PivettaNo ratings yet
- Adrenergic and Anti-Adrenergic DrugsDocument54 pagesAdrenergic and Anti-Adrenergic DrugsChittaranjan Padhy100% (1)
- Apotek Pesanan Obat FarmasiDocument16 pagesApotek Pesanan Obat Farmasik24 bambukuningNo ratings yet
- Test Eng Examen 2017 FRDocument274 pagesTest Eng Examen 2017 FRRaduNo ratings yet
- Dhikav - Neuropsychopharmacology - CH 3Document13 pagesDhikav - Neuropsychopharmacology - CH 3anurag kumarNo ratings yet
- Golongan Obat Prekursor Dan OotDocument2 pagesGolongan Obat Prekursor Dan Ootherfandi ahmadNo ratings yet
- Norepinephrine For Spinal Hypotension During Cesarean DeliveryDocument3 pagesNorepinephrine For Spinal Hypotension During Cesarean DeliveryANGELICANo ratings yet
- List of Nootropics (Scientific Literature)Document11 pagesList of Nootropics (Scientific Literature)Nicula RobertNo ratings yet
- Administration of Inotropes Evidence Based Nursing PolicyDocument8 pagesAdministration of Inotropes Evidence Based Nursing PolicyRonald ThakorNo ratings yet
- TMP F578Document10 pagesTMP F578FrontiersNo ratings yet
- Full Test Kit InfoDocument232 pagesFull Test Kit InfoolivierNo ratings yet
- 101 Study Tips PDFDocument25 pages101 Study Tips PDFEdu Fact100% (1)
- Catecholamine Influences On Dorsolateral Prefrontal Cortical NetworksDocument11 pagesCatecholamine Influences On Dorsolateral Prefrontal Cortical NetworkstleticNo ratings yet
- Adrenergic Drugs (Sympathomimetics, Adrenomimetics)Document43 pagesAdrenergic Drugs (Sympathomimetics, Adrenomimetics)cancivNo ratings yet
- Brain Based Learning Teaching The Way... Z LibraryDocument241 pagesBrain Based Learning Teaching The Way... Z LibraryJOANNA REAN SAGUIRELNo ratings yet
- Specialized Products From Amino Acids - Part 2Document16 pagesSpecialized Products From Amino Acids - Part 2Leon WarrenNo ratings yet
- Maintaining Homeostasis and the Autonomic Nervous SystemDocument30 pagesMaintaining Homeostasis and the Autonomic Nervous SystemThrecia RotaNo ratings yet
- Autonomic DrugsDocument4 pagesAutonomic DrugsSabrinaNo ratings yet
- Franke Et Al. - Methylphenidate, Modafinil, Caffeine, ChessDocument13 pagesFranke Et Al. - Methylphenidate, Modafinil, Caffeine, ChessJulien Bernier Ouellet0% (1)
- Julius Fast Sexual Chemistry Ocrd PDFDocument212 pagesJulius Fast Sexual Chemistry Ocrd PDFsairajNo ratings yet
- Gut Feminism by Elizabeth WilsonDocument25 pagesGut Feminism by Elizabeth WilsonDuke University Press50% (2)
- Obat Beta BlockerDocument3 pagesObat Beta BlockerLisa RosulliaNo ratings yet
- (Physio A) 1.4 Autonomics (Valerio)Document7 pages(Physio A) 1.4 Autonomics (Valerio)Leah VicenteNo ratings yet
- Adrenergic & Antiadrenergic DrugsDocument54 pagesAdrenergic & Antiadrenergic DrugsUzma KhanNo ratings yet
- FOR5MODULEDocument6 pagesFOR5MODULEQueenda Arcibal100% (1)
- Nursing Sympathomimetics and SympatholyticsDocument87 pagesNursing Sympathomimetics and SympatholyticsFrancis PeterosNo ratings yet
- Adrenal Support - NSP ProductDocument1 pageAdrenal Support - NSP ProductScribdOnlineReaderNo ratings yet