Professional Documents
Culture Documents
Soft Tissue Healing and Bony Regeneration Of.3
Soft Tissue Healing and Bony Regeneration Of.3
Uploaded by
adriana Ortega CastilloOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Soft Tissue Healing and Bony Regeneration Of.3
Soft Tissue Healing and Bony Regeneration Of.3
Uploaded by
adriana Ortega CastilloCopyright:
Available Formats
Original Article
– Comparative Study
Soft Tissue Healing and Bony Regeneration of Impacted
Mandibular Third Molar Extraction Sockets, Following
Postoperative Incorporation of Platelet‑rich Fibrin
Downloaded from http://journals.lww.com/aoms by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
Priya Esther Jeyaraj, Ashish Chakranarayan1
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78= on 05/04/2023
Command Military Dental Centre (Northern Command), Udhampur, Jammu and Kashmir, 1Dental Centre, INHS Kalyani, Vishakhapatnam, Andhra Pradesh,
India
Abstract
Introduction: Surgical removal of impacted mandibular third molars is one of the most commonly performed dentoalveolar surgeries
by dental surgeons around the globe. It is known to be associated with clinically significant postoperative morbidity including swelling,
pain, trismus, fever, and infection. In addition, the residual bony defect takes 7 months to 1 year to gradually fill with bone and to reossify.
Aims and Objective: (1) To carry out a prospective study to evaluate differences in soft tissue healing and bony regeneration of impacted
mandibular third molar extraction sites, with and without the incorporation of autologous platelet‑rich fibrin (PRF) within the surgical wounds.
(2) To also compare the incidence of short‑ and long‑term posttreatment complications in both cases. Materials and Methods: Sixty patients
were randomly inducted into two groups, consisting of 30 patients each. The first group, which served as the study group, consisted of patients
in whom fresh autologous PRF were placed within the extraction site immediately following the surgical removal of the impacted mandibular
third molar, before suturing of the mucoperiosteal flap. The second group, which served as the control froup, included those patients in whom
the mucoperiosteal flaps were closed without incorporation of PRF within site.Both groups were evaluated and compared for postoperative
pain, swelling, trismus, soft tissue healing, as well as bone fill of the extraction socket. Results: It was found that the study group in which
autologous PRF had been incorporated into the operative site exhibited quick and complication‑free soft tissue healing as well as a much quicker
reossification and bone fill of the extraction socket, as compared to the control group in which no PRF was used. Conclusion: Incorporation
of PRF within extraction sockets of impacted third molars proved to be beneficial for patients, yielding a quicker postoperative recovery with
fewer complications such as postoperative swelling and edema, pain, and trismus; better overall postoperative results in terms of faster soft
tissue healing as well as an earlier bony regeneration.
Keywords: Bone fill, mandibular third molar extraction sockets, platelet‑rich fibrin, platelet‑rich plasma, reossification
Introduction acute trismus, fever, etc. In some cases, other less frequent
complications, e.g., infection, nerve damage, have also been
Surgical removal of impacted mandibular third molars is one
reported. In addition, the residual bony defect takes several
of the most commonly performed dentoalveolar surgeries by
months to a year to gradually fill with bone and to reossify.[1]
oral and maxillofacial surgeons and dental surgeons around the
globe. It is known to be associated with clinically significant The importance of growth factors in enhancing wound healing
postoperative morbidity including swelling, pain, trismus, has become the focus of research in the present day. Three
fever, and infection. The surgical removal of the mandibular
third molar involves reflection of the mucoperiosteal flap Address for correspondence: Dr. Priya Esther Jeyaraj,
for access, removal of overlying bone, sectioning the Command Military Dental Centre (Northern Command),
tooth (odontectomy), delivery of the tooth, debridement Udhampur, Jammu and Kashmir, India.
E‑mail: jeyarajpriya@yahoo.com
of the socket, and closure of the soft tissue flap. This leads
to a significant surgical insult resulting in postoperative
inflammatory response ranging from pain and swelling to This is an open access journal, and articles are distributed under the terms of the
Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which
allows others to remix, tweak, and build upon the work non-commercially, as long
Access this article online
as appropriate credit is given and the new creations are licensed under the identical
Quick Response Code: terms.
Website:
www.amsjournal.com For reprints contact: reprints@medknow.com
How to cite this article: Jeyaraj PE, Chakranarayan A. Soft tissue healing
DOI: and bony regeneration of impacted mandibular third molar extraction
10.4103/ams.ams_185_17 sockets, following postoperative incorporation of platelet-rich fibrin. Ann
Maxillofac Surg 2018;8:10-8.
10 © 2018 Annals of Maxillofacial Surgery | Published by Wolters Kluwer - Medknow
Jeyaraj and Chakranarayan: Value of PRF in postextraction healing
key elements, namely scaffolds (collagen, bone mineral, etc.), Aims
signaling molecules (growth factors), and cells (osteoblasts,
To evaluate, compare, and document the clinical differences
fibroblasts) facilitate regeneration of particular tissues during
in soft tissue healing and radiographic differences in “bone
the healing process, particularly in the reossification of bony
fill”/reossification of postsurgical bony defects, following
defects and cavities.[1] Platelet‑rich fibrin (PRF) belongs to a transalveolar extractions of impacted mandibular third molars,
new generation of an immune and platelet concentrate collecting with and without incorporation of platelet‑rich fibrin within the
Downloaded from http://journals.lww.com/aoms by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
on a single fibrin membrane, containing all the constituents of extraction sockets and to compare the incidence of short‑term
a blood sample favorable to healing and immunity.[1] Though and long‑term posttreatment complications in both cases.
platelet and leukocyte cytokines play an important part in the
biology of this biomaterial, the fibrin matrix supporting them
Objectives
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78= on 05/04/2023
certainly constitutes the determining element responsible for the
real therapeutic potential of PRF. Four fundamental events of i. To compare the postoperative pain using a standard scale
cicatrization, namely, angiogenesis, immune control, circulating ii. To compare the postoperative swelling using standard
stem cells trapping, and wound‑covering epithelialization, measurements
have been shown to hasten and augment healing, by virtue iii. To compare the postoperative trismus at various time
intervals
of development of effective neovascularization, accelerated
iv. To compare the periodontal health distal to mandibular
wound closing with fast cicatricial tissue remodeling, and
second molar using periodontal probing at various time
nearly total absence of infectious events. Platelets isolated from
intervals
peripheral blood are an autologous source of growth factors
v. To compare the quality of bone healing at the mandibular
delivered in high concentrations to the site of bone defect or
third molar sockets using IOPA radiographs at various
a region requiring augmentation.[1,2] Growth factors stored in time intervals (at the end of 8 weeks).
the α‑granules of platelets include platelet‑derived growth
factor (PDGF), insulin‑like growth factor, vascular endothelial
growth factor, and transforming growth factor‑β (TGF‑β). Materials and Methods
When platelets in a concentrated form are added to graft The study was carried out at our Centre from October 1, 2016, to
materials, a more predictable outcome is derived. PRF was September 30, 2017. Volunteers were randomly recruited from
first described by Choukroun et al.[1] in France as an agent the patients reporting to the outpatient department who fulfilled
stimulating the chemotactic migration of human mesenchymal the inclusion criteria. A total of 60 patients were included
stem cells to the injury site.[2,3] in the study. These were randomly divided into two groups:
Group 1 and Group 2, consisting of 30 patients each. Group 1,
Some of the applications of PRF in dental surgery have been which served as the study group, consisted of patients in whom
bone grafting for dental implants, onlay and inlay grafts, guided fresh autologous PRF was placed within the extraction socket
bone/tissue regeneration techniques, sinus lift procedures, ridge immediately following the surgical removal of the impacted
augmentation procedures, and closure of cleft, lip, and palate mandibular third molar, before suturing of the mucoperiosteal
defects. It has proved to be of immense value in the repair of flap. Group 2, which served as the control Group, included
bone defects created by small cysts, bone defects following those patients in whom the mucoperiosteal flaps were closed
removal of impacted canines, repair of fistulas between the without incorporation of PRF within the socket.
sinus cavity and mouth, etc. Although a few studies have been
Inclusion criteria
conducted on the efficacy of platelet‑rich plasma (PRP) on
Skeletally matured adult patients above 18 years of age, with
reossification of bone defects created by removal of teeth, a clinically and radiologically (mesioangular, distoangular
lacuna exists on the use of PRF on soft tissue and bony healing or horizontally) impacted mandibular third molars teeth,
following impacted third molar extractions. presenting with one or more of the following features:
This study aims to compare the rate of soft tissue and bony 1. Clinical or radiographic evidence of pathology (pericoronal
healing as well as the incidence of short‑ and long‑term abscess, widening of follicular space)
postextraction complications, following impacted mandibular 2. Recurrent pericoronitis
third molar extractions, between two subject groups, 3. Food impaction
one with and the other without the incorporation of PRF 4. Proximal caries of the adjoining molar
within the extraction site. Clinical comparison of the 5. Cheek biting
postextraction morbidity in terms of pain, swelling, edema, 6. Chronic or recurrent pain in the region
7. Restriction in mandibular movements.
and trismus as well as radiographic comparison of the rate of
“bone‑fill”/reossification of the bony defect would be carried Exclusion criteria
out to establish the efficacy of autologous PRF in soft tissue 1. Age below 18 years
healing and regeneration of bone in mandibular third molar 2. Patients with very poor oral hygiene and/or generalized
extraction sockets. chronic destructive periodontitis
Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 1 ¦ January-June 2018 11
Jeyaraj and Chakranarayan: Value of PRF in postextraction healing
Downloaded from http://journals.lww.com/aoms by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
a b
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78= on 05/04/2023
c d e f
g h i j
Figure 1: (a and b) Horizontally impacted 38 (c and d) transalveolar extraction under local anesthesia. (e) Autologous platelet-rich fibrin prepared
using a tabletop centrifuge. (f-j) Red blood cell layer at the bottom of the centrifugation strata removed and the platelet-rich fibrin segment placed into
the extraction socket, followed by flap closure
PRF prepared using a tabletop centrifuge [Figure 1e and f] was
incorporated into the extraction socket just before closure of
the mucoperiosteal flap [Figure 1f‑j]. In patients from Group 2,
no adjunctive material/procedure was used before suturing the
mucoperiosteal flap.
The PRF membranes were prepared as described by Choukroun
et al.[1] The required quantity of blood (20 ml) was drawn into
Figure 2: Ten Point Visual Analogue Scale for evaluation of post-surgical pain two 10 ml test tubes without an anticoagulant and centrifuged
immediately. Blood was centrifuged using a tabletop centrifuge
3. Medically compromised patients systemically for 12 min at 2700 rpm or for 10 min at 30,000 rpm. The
contraindicated for surgery. following three biological phases or layers form in the resultant
product [Figure 1e].
Preoperative assessment 1. The lowermost layer consisted of coagulated red blood
All the study subjects underwent a thorough clinical and corpuscles layer at the bottom of the centrifugation tube,
radiological examination which included: 2. The intermediate/middle layer comprised the rigid and
1. M a x i m u m m o u t h o p e n i n g w i t h Ve r n i e r ’s elastic PRF clot/gel
caliper (inter‑incisal distance) 3. The topmost layer was the supernatant serum consisting
2. Periodontal health by measuring pocket depth distal to of acellular platelet‑poor plasma.
mandibular second molar using William’s periodontal probe
3. Extraoral and intraoral photographs The PRF clots were retrieved from the tubes and incorporated
4. Orthopantomogram into the extraction sites, while the red blood cell gel detached
5. Intraoral periapical radiograph (IOPA) of the impacted and discarded.
mandibular third molar Ibuprofen 400 mg + paracetamol 325 mg and
6. Routine hematological investigation. amoxicillin 500 mg TID for 5 days were prescribed for all patients.
Intraoperative procedure
Transalveolar surgical extraction of the impacted third Results
molar [Figure 1a‑c] was carried out in all the 60 patients Postoperative clinical and radiographic assessment
[Figure 1c and d], followed by establishing adequate hemostasis Postoperatively, all patients of both the groups were evaluated
at the surgical site. In patients from Group 1, autologous fresh for incidence and magnitude of complications, such as follows:
12 Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 1 ¦ January-June 2018
Jeyaraj and Chakranarayan: Value of PRF in postextraction healing
a b c
Downloaded from http://journals.lww.com/aoms by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78= on 05/04/2023
d e f
Figure 3: (Group 1) Orthopantomograms of two cases, preextraction (a and d) and 2 months postextraction with platelet-rich fibrin placement (b and e).
(c and f) Intraoral periapical radiographs 2 months postextraction with platelet-rich fibrin placement showing dense and healthy bone fill in the extraction sockets
1. Pain ‑ 3rd postoperative day
2. Swelling ‑ 3rd postoperative day
3. Trismus ‑ 3rd postoperative day
4. Periodontal health‑on 8th week
5. Bone healing ‑ on 8th week.
Clinical assessment
a b Pain
Degree of postsurgical pain was evaluated
using 10‑point visual analog scale [Figure 2], with a score
of “0” equaling “no pain” and “10” equaling “very severe
pain.”
Pain was evaluated on the 3 rd postoperative day and
recorded [Table 1] for both groups of patients.
c d
Figure 4: (a and b) (Group 1) Intraoral periapical radiographs of mandibular Swelling
right third molar region (a) before extraction. (b) Two months postextraction Degree of postoperative cheek swelling and edema was
with platelet-rich fibrin placement in extraction socket showing dense and estimated by measuring the distances from the tragus to the
healthy bone fill. (c and d) (Group 2) Intraoral periapical radiographs of soft tissue pogonion and from the tragus to the angle of the
mandibular right third molar region (c) before extraction. (d) Two months mouth. Swelling was evaluated on the 3rd postoperative day
postextraction without platelet-rich fibrin placement showing incomplete
in both the groups and recorded as nil, mild, moderate, and
bone fill/reossification of the extraction socket
severe [Table 1 and Graph 1].
Periodontal health of the second molar
The preoperative measurements of probing depth (PD)
on the distobuccal aspect of the second molars were
checked with William’s periodontal probe with millimeter
marking, by measuring pocket depth from free gingival
margin to bottom of the pocket. It was then compared
a b
with postoperative measurements at 8th week following the
extraction and the difference (increase or decrease) was
recorded [Table 1 and Graph 2].
The preoperative baseline PD (PD1) and 8 weeks
postoperative (PD2) were measured in both groups.
They ranged from a mean ± SD of 2.41 ± 0.59 mm to
c d 3.10 ± 0.88 mm, respectively, in Group 1 and from a mean ± SD
Figure 5: (Group 2) Intraoral periapical radiographs of mandibular third of 2.41 ± 0.59 mm to 3.90 ± 0.88 mm, respectively, in Group 2.
molar region following routine extractions without platelet-rich fibrin
placement in extraction sockets, (a and c) two months postextraction Radiographic assessment (bone healing)
revealing radiolucent appearance of the root sockets. (b and d) Six Periapical intraoral radiographs were obtained of the impacted
months postextraction showing beginning of bone fill and trabeculations mandibular third molar tooth sites before surgery, immediately
Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 1 ¦ January-June 2018 13
Jeyaraj and Chakranarayan: Value of PRF in postextraction healing
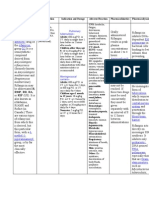
Table 1: Comparison of postoperative complications between the two groups
Average pain score Postoperative swelling Postoperative trismus Increase in Periodontal
(3rd postoperative day) (3rd postoperative day) (3rd postoperative day) Probing Depth (PD) in relation
(yes/no) to 2nd molar (at 8 weeks)
Group 1 Group 2 Group 1 Group 2 Group 1 Group 2 Group 1 Group 2
1 4 Nil Moderate No Yes 0.75 1.5
Downloaded from http://journals.lww.com/aoms by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
2 3 Nil Mild No Yes 0.74 1.2
1 3 Mild Moderate No Yes 0.76 1.7
1 3 Nil Mild No Yes 0.78 1.6
1 2 Nil Moderate No Yes 0.72 1.6
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78= on 05/04/2023
2 3 Nil Mild No No 0.73 1.4
2 2 Nil Moderate No No 0.74 1.3
2 5 Nil Moderate No Yes 0.71 1.6
3 5 Mild Mild No Yes 0.78 1.8
3 4 Mild Mild Yes Yes 0.72 1.6
1 3 Nil Mild No Yes 0.75 1.5
1 4 Nil Moderate No No 0.78 1.5
1 4 Nil Nil No No 0.73 1.4
0 3 Nil Moderate Yes Yes 0.75 1.7
0 3 Mild Nil No Yes 0.75 1.6
1 3 Nil Severe No Yes 0.73 1.7
2 2 Mild Mild No Yes 0.73 1.7
1 1 Mild Mild No Yes 0.74 1.4
0 5 Nil Moderate Yes Yes 0.69 1.3
2 6 Nil Nil Yes No 0.68 1.5
2 4 Mild Moderate No No 0.75 1.2
1 3 Mild Moderate No Yes 0.74 1.4
1 3 Nil Nil No Yes 0.72 1.3
1 5 Nil Moderate No No 0.76 1.5
0 3 Mild Moderate Yes No 1.1 1.4
2 2 Mild Severe Yes No 1.2 1.4
3 1 Mild Moderate No Yes 1.3 1.6
1 4 Nil Severe No Yes 1 1.5
4 3 Nil Mild No Yes 0.78 1.2
3 3 Nil Moderate No Yes 0.75 1.3
PD=Probing depth
after surgical extraction, and at 2 monthly intervals, till 2 ‑ Mostly coarse and some fine trabeculae.
6 months. The radiographs were obtained with a standardized 1 ‑ Delicate, finely meshed trabeculae.
paralleling technique, using a radiovisiography unit. The bone 0 ‑ Granular, nearly homogenous patterns; individual
healing of the third molar socket was assessed using IOPA trabeculae essentially absent.
radiographs using a standard periapical X‑ray.
Bone healing in the two groups was evaluated and compared
The criteria of bone healing and scoring system were based on at the end of the 8th week [Table 2 and Graphs 3‑5].
modification of method used by Kelly et al. Two parameters
namely overall density score and trabecular pattern score
Statistical analysis
All the data was compiled and ANOVA test was used to
were assessed.
analyze the same using SPSS software version 16 (Statistical
Overall density score Package for the Social Sciences 2016 for Windows-IBM
3 ‑ Marked increase in radiographic density reaching normal corporation, NY, USA). At 95% confidence interval, the
limits. following test statistics for Group 1 and Group 2, respectively,
2 ‑ Moderate increase in radiographic density. were observed [Tables 3 and 4].
1 ‑ Mild increase in radiographic density.
It was observed that incorporation of PRF within extraction
0 ‑ Nil increase in radiographic density.
sockets of impacted third molars proved to be immensely
Trabecular pattern score beneficial in patients in Group 1, resulting in quicker
3 ‑ All trabeculae substantially coarse. postoperative recovery clinically and reduced morbidity, with
14 Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 1 ¦ January-June 2018
Jeyaraj and Chakranarayan: Value of PRF in postextraction healing
Downloaded from http://journals.lww.com/aoms by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78= on 05/04/2023
Graph 1: Comparison of postoperative pain between the two Groups at 3 days postsurgery
Graph 2: Comparison of periodontal health of adjacent second molar between the two Groups at 8 weeks postsurgery
Graph 3: Comparison of overall bone density score of extraction sockets between the two groups at 8 weeks postsurgery
fewer postoperative complications such as pain, swelling, as compared to Group 1 patients, in terms of bone density as
trismus, and periodontal pocket in relation to the adjacent well as trabeculations [Figures 4c, d and 5].
second molar. There was also observed improved and faster
bone regeneration, with good quality of bone fill in terms of Discussion
bone density as well as trabeculations, of the extraction socket
Socket healing is a highly coordinated sequence of biochemical,
radiographically, within 8 weeks [Figures 3 and 4a and b]. On
physiologic, cellular, and molecular responses involving
the other hand, patients in Group 2, who underwent surgical
numerous cell types, growth factors, hormones, cytokines,
extraction without incorporation of PRF, exhibited increased
and other proteins, which is directed toward restoring tissue
frequency of postoperative complications such as pain,
integrity and functional capacity after injury.
swelling, trismus, and deeper periodontal pockets in relation to
the adjacent tooth. Further, the radiological evidence of bone Reconstruction of bony defects represents a challenging
fill of the extraction sockets at the end of 8 weeks was inferior problem for the surgical community. Many defects in facial
Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 1 ¦ January-June 2018 15
Jeyaraj and Chakranarayan: Value of PRF in postextraction healing
Downloaded from http://journals.lww.com/aoms by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78= on 05/04/2023
Graph 4: Comparison of trabecular pattern score of extraction sockets between the two groups at 8 weeks postsurgery
Graph 5: Comparison of total bone density of extraction sockets between the two groups at 8 weeks postsurgery
skeleton may significantly impair proper prosthetic and PRF can be considered as a healing biomaterial, consisting
functional rehabilitation of the stomatognathic system.[3] of a fibrin matrix polymerized in a tetramolecular structure,
incorporated with platelets, leukocyte, and cytokines and
Various glass materials, autografts, alloplastic materials
stem cells, featuring all the necessary parameters permitting
have been tested to enhance socket healing and to minimize
the postoperative sequelae after the third molar surgery. optimal healing. Despite the fact that cytokines trapped
Platelet‑rich growth factors are also very successful in in PRF are gradually released and able to accelerate the
stimulating bone regeneration and promote healing after the cellular phenomenon, the structure of the fibrin network is
surgical removal of the third molar tooth. PRP is one of the the key element of all improved PRF healing processes.[1]
platelet releasing growth factor that has been successfully used All of the known clinical applications of PRF highlight an
to accelerate soft‑tissue and hard‑tissue healing. accelerated tissue cicatrization due to the development of
effective neovascularization, accelerated wound closing with
The growth factors present in PRP are well‑known including fast cicatricial tissue remodeling, and nearly total absence
TGF‑1 and TGF‑2, vascular endothelial growth factor, three of infectious events. Preparation of PRF was first described
isomers of Platelet Derived Growth Factor (PDGF), namely by Choukroun et al. in 2006.[1] Studies have revealed that
PDGF- AA, PDGF- BB and PDGF-AB, and endothelial PRF could be an immune regulation node with inflammation
growth factor. These growth factors are considered to have the retrocontrol abilities. This concept could explain the reduction of
ability to accelerate chemotaxis, mitogenesis, angiogenesis, postoperative infections when PRF is used as surgical additive.
and synthesis of collagen matrix and favor tissue repair when [3]
Studies have also shown that PRF, unlike the other platelet
applied on bone wounds. concentrates, would be able to progressively release cytokines
PRF is a newer material which is referred to as a second‑generation during fibrin matrix remodeling; such a mechanism might
platelet concentrate. It contains all constituents of a blood sample explain the clinically observed healing properties of PRF.[4]
favorable for healing and immunity on a single fibrin membrane.[3]
A few studies have been carried out in dental implantology,
The existing literature mainly deals with the use of PRP in examining the possible use of PRF as a grafting material in
extraction sockets as well as in other areas with nonplacement maxillary sinus augmentation procedures. PRF mixed with
in control sites. However, there is limited information available freeze‑dried bone allograft has been shown to reduce healing
concerning the healing of extraction sockets using PRF. time before implant placement.[5,6]
16 Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 1 ¦ January-June 2018
Jeyaraj and Chakranarayan: Value of PRF in postextraction healing
Table 2: Comparison of the bone fill and reossification between the two groups at the end of 8 weeks
Group 1 Group 2
Overall density Trabecular pattern Total bone density Overall density Trabecular pattern Total bone density
score score score score score score
3 3 6 0 1 1
3 2 5 1 0 1
Downloaded from http://journals.lww.com/aoms by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
3 2 5 2 2 4
3 3 6 1 1 2
2 3 5 1 1 2
2 3 5 1 1 2
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78= on 05/04/2023
2 2 4 0 1 1
3 2 5 0 0 0
1 1 2 0 1 1
2 3 5 0 0 0
2 3 5 1 2 3
3 2 5 1 1 2
3 2 5 1 1 2
2 1 3 2 1 3
3 2 5 1 2 3
2 3 5 0 1 1
2 2 4 0 1 1
3 2 5 1 0 1
3 2 5 1 0 1
3 3 6 2 0 2
3 3 6 2 1 3
2 3 5 1 0 1
3 3 6 2 1 3
2 3 5 2 1 3
3 2 5 1 1 2
2 2 4 0 0 0
3 5 0 1 1
3 3 6 0 1 1
3 3 6 1 1 2
2 3 5 1 0 1
Table 3: Test statistics for Group 1
Average pain Periodontal PD in Overall bone density Trabecular pattern Total bone density in
in Group 1 Group 1 in Group 1 score in Group 1 Group 1
χ2 14.333a 15.067b 13.400c 9.800c 34.000a
df 4 12 2 2 4
Asymptotic significant 0.006 0.238 0.001 0.007 0.000
Monte Carlo significant
Significant 0.009d 0.255d 0.001d 0.010d 0.000d
95% CI
Lower bound 0.007 0.246 0.000 0.008 0.000
Upper bound 0.011 0.263 0.001 0.012 0.000
PD=Probing depth; CI=Confidence interval
From a clinical standpoint, although this biomaterial study was carried out to evaluate the effect of PRF on the
appears to accelerate physiologic healing, the numerous early bone healing process with bone scintigraphy based on
perspectives of PRF have still to be clinically tested.[7] This technetium‑99 m methylene diphosphonate uptake in the
initial research evaluating the effects of PRF on the soft and third molar extraction sockets.[8] It was demonstrated that
hard tissue healing of postextraction sockets of impacted PRF exhibits the potential characteristics of an autologous
third molars, both impartially and rigorously, will make it fibrin matrix,[9,10] with abundant fibrin and inflammatory cells.
possible to plan several future PRF applications, particularly However, the study suggested that further investigation was
in the field of oral and maxillofacial surgery. An interesting required to determine whether the presence of crystal‑like
Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 1 ¦ January-June 2018 17
Jeyaraj and Chakranarayan: Value of PRF in postextraction healing
Table 4: Test statistics for Group 2
Average pain Periodontal PD Overall bone density Trabecular pattern Total bone density
in Group 2 in Group 2 in Group 2 score in Group 2 in Group 2
χ2 18.400a 5.000b 3.200c 11.400c 12.333d
df 5 6 2 2 4
Asymptotic significant 0.002 0.544 0.202 0.003 0.015
Downloaded from http://journals.lww.com/aoms by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
Monte Carlo significant
Significant 0.004e 0.569e 0.211e 0.003e 0.014e
95% CI
Lower bound 0.003 0.559 0.203 0.002 0.011
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78= on 05/04/2023
Upper bound 0.005 0.579 0.219 0.004 0.016
PD=Probing depth; CI=Confidence interval
particles on the outer surface of PRF actually alters bone References
and soft tissue healing. 1. Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C,
The present study demonstrates the benefits of intraoperative Dohan SL, et al. Platelet‑Rich Fibrin (PRF): A second‑generation
platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg
incorporation of Autologous PRF in impacted third Oral Med Oral Pathol Oral Radiol Endod 2006;101:e56‑60.
molar extraction sockets, resulting in clinically as well as 2. Ogundipe OK, Ugboko VI, Owotade FJ. Can autologous platelet‑rich
radiographically appreciable postoperative results, in terms of plasma gel enhance healing after surgical extraction of mandibular third
soft as well as hard tissue recovery, healing, and regeneration. molars? J Oral Maxillofac Surg 2011;69:2305‑10.
3. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J,
et al. Platelet‑rich fibrin (PRF): A second‑generation platelet
Conclusion concentrate. Part III: Leucocyte activation: A new feature for platelet
concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endod
In view of the fact that the use of PRF placed in the extraction 2006;101:e51‑5.
socket resulted in reduced morbidity postoperatively, and 4. Freymiller EG, Aghaloo TL. Platelet‑rich plasma: Ready or not? J Oral
improved bone healing radiologically, it is recommended that Maxillofac Surg 2004;62:484‑8.
a larger sample may be studied in conjunction with a detailed 5. Diss A, Dohan DM, Mouhyi J, Mahler P. Osteotome sinus floor
elevation using Choukroun’s platelet‑rich fibrin as grafting
and more objective radiological parameters and protocols to
material: A 1‑year prospective pilot study with microthreaded
verify the findings of this study and possibly incorporate the implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod
use of PRF as part of standard extraction procedure especially 2008;105:572‑9.
for difficult extractions or for extraction of those teeth to be 6. Kim SG, Kim WK, Park JC, Kim HJ. A comparative study of
replaced using dental implants. osseointegration of avana implants in a demineralized freeze‑dried
bone alone or with platelet‑rich plasma. J Oral Maxillofac Surg
Declaration of patient consent 2002;60:1018‑25.
7. Shanaman R, Filstein MR, Danesh‑Meyer MJ. Localized ridge
The authors certify that they have obtained all appropriate augmentation using GBR and platelet‑rich plasma: Case reports. Int J
patient consent forms. In the form the patient(s) has/have Periodontics Restorative Dent 2001;21:345‑55.
given his/her/their consent for his/her/their images and other 8. Gürbüzer B, Pikdöken L, Tunali M, Urhan M, Küçükodaci Z, Ercan F,
clinical information to be reported in the journal. The patients et al. Scintigraphic evaluation of osteoblastic activity in extraction
understand that their names and initials will not be published sockets treated with platelet‑rich fibrin. J Oral Maxillofac Surg
2010;68:980‑9.
and due efforts will be made to conceal their identity, but 9. Marx ER. Platelet‑rich plasma: A source of multiple autologous
anonymity cannot be guaranteed. growth factors for bone grafts. In: Lynch SE, Genco RJ, Marx RE,
editors. Tissue Engineering, Applications in Maxillofacial Surgery
Financial support and sponsorship and Periodontics. Illinois: Quintessence Publishing Co, Inc.; 1999.
Nil. p. 71‑82.
10. Tsay RC, Vo J, Burke A, Eisig SB, Lu HH, Landesberg R, et al.
Conflicts of interest Differential growth factor retention by platelet‑rich plasma composites.
There are no conflicts of interest. J Oral Maxillofac Surg 2005;63:521‑8.
18 Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 1 ¦ January-June 2018
You might also like
- Paed HistDocument123 pagesPaed HistG VenkateshNo ratings yet
- Drug Study RifampicinDocument2 pagesDrug Study RifampicinJamil Lorca100% (5)
- The Keyhole Access Expansion Technique For FlaplesDocument6 pagesThe Keyhole Access Expansion Technique For FlaplesKyoko CPNo ratings yet
- Disease Pathognomonic Sign: Muddy Brown CastsDocument1 pageDisease Pathognomonic Sign: Muddy Brown CastsRafey AhmedNo ratings yet
- The International Journal of Periodontics & Restorative DentistryDocument10 pagesThe International Journal of Periodontics & Restorative DentistryViorel FaneaNo ratings yet
- Woc ArdsDocument2 pagesWoc Ardssyarifah salmaNo ratings yet
- Typhoid Fever: Infectious DiseaseDocument52 pagesTyphoid Fever: Infectious Disease12. Akshit AtwalNo ratings yet
- Comparative - Evaluation - of - Temporal - Fascia - And.17 2Document5 pagesComparative - Evaluation - of - Temporal - Fascia - And.17 2Tabishur RahmanNo ratings yet
- Factors Affecting Functional Outcome of Distal Tibia Fractures Treated by Plating Using Minimal Invasive Percutaneous Plate Osteosynthesis TechniqueDocument10 pagesFactors Affecting Functional Outcome of Distal Tibia Fractures Treated by Plating Using Minimal Invasive Percutaneous Plate Osteosynthesis TechniqueIJAR JOURNALNo ratings yet
- World J PL v12n3p18 enDocument6 pagesWorld J PL v12n3p18 enyekije4553No ratings yet
- ch13Document6 pagesch13boopathiraja.chinnasamyNo ratings yet
- Management of Trismus by Masseter Myotomy: January 2014Document4 pagesManagement of Trismus by Masseter Myotomy: January 2014Afifah Ratih RosavinaNo ratings yet
- Harrsion 1991 PDFDocument8 pagesHarrsion 1991 PDFrozh rasulNo ratings yet
- Branski (2011)Document7 pagesBranski (2011)TommysNo ratings yet
- ArthrocentesisDocument10 pagesArthrocentesisPranave PNo ratings yet
- Sayedel Ahl2015Document5 pagesSayedel Ahl2015Sung Soon ChangNo ratings yet
- Mozzati2014 - Song Sieu Am Trong NH Răng 8Document4 pagesMozzati2014 - Song Sieu Am Trong NH Răng 8Hoàng VũNo ratings yet
- Soleus Muscle Flap For The Coverage of Pre-Tibial Defect of Middle Third of LegDocument6 pagesSoleus Muscle Flap For The Coverage of Pre-Tibial Defect of Middle Third of LegHassan KhanNo ratings yet
- India 2015 31 Pcientes - FuncionaDocument8 pagesIndia 2015 31 Pcientes - FuncionaGabriel Filipe Tosin ScivskiNo ratings yet
- Mar2012 CC NoyesDocument17 pagesMar2012 CC NoyesJavierLarenasNo ratings yet
- Opcoes Reconstrucao EscrotoDocument13 pagesOpcoes Reconstrucao EscrotoRenan OliveiraNo ratings yet
- Platelet-Rich Fibrin Enhances Wound Epithelialization in The Skin Graft Donor SiteDocument9 pagesPlatelet-Rich Fibrin Enhances Wound Epithelialization in The Skin Graft Donor Siteyanuararipratama89No ratings yet
- Minimally Invasive Transgingival Implant Therapy: A Literature ReviewDocument6 pagesMinimally Invasive Transgingival Implant Therapy: A Literature ReviewEmilio RodríguezNo ratings yet
- 2021 Submucosal and Intramuscular Dexamethasone For The Control of Pain, Trismus and Edema After Third Molar Surgeries ¿Is It Necessary?Document5 pages2021 Submucosal and Intramuscular Dexamethasone For The Control of Pain, Trismus and Edema After Third Molar Surgeries ¿Is It Necessary?kaarlaamendezNo ratings yet
- Reusing Dental Implants?: An Experimental Study For Detecting The Success Rates of Re-OsseointegrationDocument7 pagesReusing Dental Implants?: An Experimental Study For Detecting The Success Rates of Re-OsseointegrationSatya AsatyaNo ratings yet
- Initial Experience With Application of Single Layer Modified Kugel Mesh For Inguinal Hernia Repair: Case Series of 72 Consecutive PatientsDocument6 pagesInitial Experience With Application of Single Layer Modified Kugel Mesh For Inguinal Hernia Repair: Case Series of 72 Consecutive Patientsnur hasnahNo ratings yet
- 3786-Article Text-7170-2-10-20190703 PDFDocument6 pages3786-Article Text-7170-2-10-20190703 PDFSalman MemonNo ratings yet
- Hyperbaric Oxygen Therapy For Reconstructive Urology WoundsDocument12 pagesHyperbaric Oxygen Therapy For Reconstructive Urology WoundsmibnukhaldunNo ratings yet
- Nova Classificação Saude Peri Implantar. Araujo 2018. Peri Implant HealthDocument8 pagesNova Classificação Saude Peri Implantar. Araujo 2018. Peri Implant HealthERYSON THIAGO DO PRADO BATISTANo ratings yet
- Implant Placement Procedure - One Stage VS Two StageDocument6 pagesImplant Placement Procedure - One Stage VS Two StageMirela BurciuNo ratings yet
- Immediate Prostheses On One Piece Trans Mucosal Implants in Flapless Surgical Procedures Case Series Report Part I Full Arch RehabilitationsDocument6 pagesImmediate Prostheses On One Piece Trans Mucosal Implants in Flapless Surgical Procedures Case Series Report Part I Full Arch RehabilitationsSalem Fathi BermawiNo ratings yet
- Combined Therapy With Mineral Trioxide ADocument5 pagesCombined Therapy With Mineral Trioxide AMihaela TuculinaNo ratings yet
- Treatment of TMJ Ankylosis in JordanianDocument7 pagesTreatment of TMJ Ankylosis in Jordanianshagun singhNo ratings yet
- Management of Pain, Swelling, Healing and Bone Regeneration After Removal of Lower Arch Wisdom TeethDocument11 pagesManagement of Pain, Swelling, Healing and Bone Regeneration After Removal of Lower Arch Wisdom TeethInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Effectiveness of Human Amnion As A Graft MaterialDocument6 pagesEffectiveness of Human Amnion As A Graft MaterialJuan Sierra ZambranoNo ratings yet
- SJ BDJ 2014 354Document8 pagesSJ BDJ 2014 354aziz alsohailNo ratings yet
- Iprf VS AcDocument8 pagesIprf VS Aczakarya hasaninNo ratings yet
- Wound: CtosureDocument8 pagesWound: CtosureAnonymous kdBDppigENo ratings yet
- PEMF - Mandibular FractureDocument7 pagesPEMF - Mandibular FractureMáté TóthNo ratings yet
- Comparison and Review of Indirect Myofascial Release Therapy, IASTM, and ART To Inform CDMDocument6 pagesComparison and Review of Indirect Myofascial Release Therapy, IASTM, and ART To Inform CDMkrayfieldNo ratings yet
- New Technique For Magnetic Compression Anastomosis.8Document10 pagesNew Technique For Magnetic Compression Anastomosis.8sjmc.surgeryresidentsNo ratings yet
- Thompson 2006Document6 pagesThompson 2006Rafal SmolinskiNo ratings yet
- 2019 - Comparison of Bite Force in Patients After Treatment of Mandibular Fractures With 3-Dimensional Locking Miniplate and Standard MiniplatesDocument4 pages2019 - Comparison of Bite Force in Patients After Treatment of Mandibular Fractures With 3-Dimensional Locking Miniplate and Standard MiniplatesLeandro Nascimento Rodrigues dos santosNo ratings yet
- Anemark 1969-2-2 (02-07)Document6 pagesAnemark 1969-2-2 (02-07)Carolina Dávila RamírezNo ratings yet
- Roccuzzo 2007Document9 pagesRoccuzzo 2007Juliana Gomes BarretoNo ratings yet
- OsteomyelitisDocument8 pagesOsteomyelitiskenapayaNo ratings yet
- Management of External Cervical Root Resorption in Mandibular MolarDocument7 pagesManagement of External Cervical Root Resorption in Mandibular MolarKomal JadhavNo ratings yet
- Infection Following Bone Tumor Resection and Reconstruction With Tumoral Prostheses: A Literature Review F. CDocument9 pagesInfection Following Bone Tumor Resection and Reconstruction With Tumoral Prostheses: A Literature Review F. CWilson MartinezNo ratings yet
- Ijdr 202273 08Document5 pagesIjdr 202273 08Dadi SindhuNo ratings yet
- Prospective Study of Management of Close or CompouDocument5 pagesProspective Study of Management of Close or CompoumaudiaNo ratings yet
- Cierre de Piel de Herida de Estoma Con Tecnica Purse-StringDocument7 pagesCierre de Piel de Herida de Estoma Con Tecnica Purse-Stringjesus aguirreNo ratings yet
- Postop Retraction TTDocument5 pagesPostop Retraction TTKye Hoon ParkNo ratings yet
- 01 Jdmfs.v7i2.1000Document4 pages01 Jdmfs.v7i2.1000scavenger .CSGO.No ratings yet
- 06 - Open Fractures - FinalDocument5 pages06 - Open Fractures - FinalSphamandla HlatshwayoNo ratings yet
- Colgajo BuccinadorDocument6 pagesColgajo BuccinadorLeya Contreras AmorettiNo ratings yet
- Cabello 2015Document22 pagesCabello 2015Vannia BautistaNo ratings yet
- Flap Design 3rd MolarDocument6 pagesFlap Design 3rd MolarArindam DuttaNo ratings yet
- Contents - 2006 - Oral and Maxillofacial Surgery Clinics of North AmericaDocument3 pagesContents - 2006 - Oral and Maxillofacial Surgery Clinics of North AmericaMugdha FrancisNo ratings yet
- Pathophysiology: Laboratory StudiesDocument8 pagesPathophysiology: Laboratory Studiesrahma perwitasariNo ratings yet
- Is Synthetic Meshplasty The Only Methodfor Inguinal Hernia Repair or Are There Other Resourceful Alternatives?Document7 pagesIs Synthetic Meshplasty The Only Methodfor Inguinal Hernia Repair or Are There Other Resourceful Alternatives?IJAR JOURNALNo ratings yet
- Injury: F. Lavini, C. Dall'Oca, S. Mezzari, T. Maluta, E. Luminari, F. Perusi, E. Vecchini, B. MagnanDocument6 pagesInjury: F. Lavini, C. Dall'Oca, S. Mezzari, T. Maluta, E. Luminari, F. Perusi, E. Vecchini, B. MagnanTefera LeteboNo ratings yet
- Canalplasty For Exostosis With Maximal Skin PreservationDocument9 pagesCanalplasty For Exostosis With Maximal Skin PreservationAbegail LacsonNo ratings yet
- Jkfs 32 102Document5 pagesJkfs 32 102Filip starcevicNo ratings yet
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentFrom EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNo ratings yet
- Advances in Vestibular Schwannoma Microneurosurgery: Improving Results with New TechnologiesFrom EverandAdvances in Vestibular Schwannoma Microneurosurgery: Improving Results with New TechnologiesLuciano MastronardiNo ratings yet
- DRUG STUDY (Lung Cancer)Document10 pagesDRUG STUDY (Lung Cancer)Jobelle AcenaNo ratings yet
- A Diagnostic Scoring System For Myxedema ComaDocument36 pagesA Diagnostic Scoring System For Myxedema ComaSarnings SalamNo ratings yet
- Diskusi Topik 2 (PPOK) - Nafisa Zulpa Elhapidi - 406202067Document59 pagesDiskusi Topik 2 (PPOK) - Nafisa Zulpa Elhapidi - 406202067nafisa zulfaelNo ratings yet
- Kerley's LineDocument3 pagesKerley's LineCitie VillaNo ratings yet
- Use of Expired CO Monitoring in The ICU: Dennis Bing, RRTDocument24 pagesUse of Expired CO Monitoring in The ICU: Dennis Bing, RRTasyi-2No ratings yet
- Viral Ds. QuesDocument6 pagesViral Ds. QuesArchanaNo ratings yet
- Vital Signs 1 Multiple Choice Test PDFDocument4 pagesVital Signs 1 Multiple Choice Test PDFDrKhaalid Hassan ElmiNo ratings yet
- Just Another Sebaceous Cyst?: I. Clinical QuestionDocument3 pagesJust Another Sebaceous Cyst?: I. Clinical QuestionJaessa FelicianoNo ratings yet
- Ruptured and Herniated Disc AnimationDocument4 pagesRuptured and Herniated Disc Animationgaby yepesNo ratings yet
- Nursing Care Plan - Alteration in Bowel Elimination - ConstipationDocument1 pageNursing Care Plan - Alteration in Bowel Elimination - ConstipationArlan AbraganNo ratings yet
- Diagnosis in OrthopedicsDocument214 pagesDiagnosis in OrthopedicsMr. question100% (1)
- StudiesDocument130 pagesStudiesShruti100% (2)
- Application Documents For 2024 "Study in ZUEL" Freshman ScholarshipDocument10 pagesApplication Documents For 2024 "Study in ZUEL" Freshman Scholarshipnhubinh.helen163No ratings yet
- 8 Plasma Derivatives ProductsDocument12 pages8 Plasma Derivatives ProductssayednourNo ratings yet
- Acute GlomerulonephritisDocument27 pagesAcute GlomerulonephritisKumara GuruNo ratings yet
- Skill 9 Hip & Sitz BathDocument15 pagesSkill 9 Hip & Sitz BathBautista AubergineNo ratings yet
- Ineffective Tissue Perfusion Related To Decreased HGB Concentration in Blood Secondary ToDocument6 pagesIneffective Tissue Perfusion Related To Decreased HGB Concentration in Blood Secondary Toericke_tanNo ratings yet
- Cataract - GlaucomaDocument2 pagesCataract - GlaucomaggukNo ratings yet
- OtomikosisDocument23 pagesOtomikosisMega Hayyu IsfiatiNo ratings yet
- 1.6+7 Laboratory Investigation and Film Interpretation WITHOUT ANSWERSDocument21 pages1.6+7 Laboratory Investigation and Film Interpretation WITHOUT ANSWERSAlex KamougerosNo ratings yet
- NCM 117 Midterm ReviewerDocument17 pagesNCM 117 Midterm ReviewerPia Rose RoqueNo ratings yet
- Stepwise Approach To Continuous Glucose Monitoring Interpretation For Internists and Family PhysiciansDocument10 pagesStepwise Approach To Continuous Glucose Monitoring Interpretation For Internists and Family PhysiciansRafael Baybay100% (1)
- Tetratology Hand OutsDocument1 pageTetratology Hand OutsAngielyn Montibon JesusNo ratings yet
- Froelich Syndrome and HomoeopathyDocument13 pagesFroelich Syndrome and HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (1)
- SolutionDocument6 pagesSolutionAmanda IrvingNo ratings yet