Professional Documents
Culture Documents
16 (1.7)
Uploaded by
JOHAN STEVEN COSME ARANZAZUCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
16 (1.7)
Uploaded by
JOHAN STEVEN COSME ARANZAZUCopyright:
Available Formats
Since January 2020 Elsevier has created a COVID-19 resource centre with
free information in English and Mandarin on the novel coronavirus COVID-
19. The COVID-19 resource centre is hosted on Elsevier Connect, the
company's public news and information website.
Elsevier hereby grants permission to make all its COVID-19-related
research that is available on the COVID-19 resource centre - including this
research content - immediately available in PubMed Central and other
publicly funded repositories, such as the WHO COVID database with rights
for unrestricted research re-use and analyses in any form or by any means
with acknowledgement of the original source. These permissions are
granted for free by Elsevier for as long as the COVID-19 resource centre
remains active.
Medicina Clínica 159 (2022) e53
www.elsevier.es/medicinaclinica
Letter to the Editor
High-flow nasal cannulas in COVID-19 Secondly, in addition to their failure to describe the statistical
pneumonia analysis carried out, we found a lack of variables of great interest
in these patients in the comparative section. For example, based on
Cánulas nasales de alto flujo en la neumonía por COVID-19 the work published by Liu et al., we believe that variables such as
the age, number of comorbidities, ROX index, Glasgow Coma Scale
Dear Editor: Score, and use of vasopressors on the first day of the high-flow nasal
cannula (HFNC) therapy, all of which are independent risk factors
After reading with special interest García-Pereña et al.’s article,1 for HFNC therapy failure in a multivariate regression,5 cannot be
available online in your journal, we would like to share some reflec- ignored in this type of study.
tions and comments. Finally, we would like to emphasize that another plausible inter-
The authors assume in their paper that non-intubated patients pretation, considering the data presented by García-Pereña et al.,1
presenting with an SpO2 /FiO2 ratio ≤100 have a severe acute is the fact that delayed intubation in these patients increases mor-
respiratory distress syndrome (ARDS). It is important to point tality in this cohort, with the likelihood of this statement being false
out that unless these patients were breathing ambient aire, FiO2 being only 6.1% (p = 0.0061).
ranges can vary by more than 10% depending on the device used
(nasal tubes, Ventimask or Multi-vent mask).2 Along these lines, References
based on Todd et al.’s work,3 the relationship between SpO2 /FiO2
and PaO2 /FiO2 is known to be described based on the following 1. García-Pereña L, Ramos Sesma V, Tornero Divieso ML, Lluna Carrascosa A, Velasco
Fuentes S, Parra-Ruiz J. Benefits of early use of high-flow-nasal-cannula (HFNC)
equation: SpO2 /FiO2 = 64 + 0.84 × (PaO2 /FiO2 ) (p < 0.0001; r = 0.89). in patients with COVID-19 associated pneumonia. Med Clin (Barc). 2021;16,
Threshold SpO2 /FiO2 ratio values of 235 and 315 yielded a sen- http://dx.doi.org/10.1016/j.medcli.2021.05.015. S0025-7753(21)00322-00325.
sitivity of 85% with a specificity of 85% and a sensitivity of 91% 2. Tobin M. Basing respiratory management of COVID-19 on physi-
ological principles. Am J Respir Crit Care Med. 2020;11:1319–20,
with a specificity of 56%, respectively, for PaO2 /FiO2 ratios of 200 http://dx.doi.org/10.1164/rccm.202004-1076ED.
and 300. 3. Rice TW, Wheeler AP, Bernard GR, Hayden DL, Schoenfeld DA, Ware
Although the current Berlin definition might be deficient for LB. National Institutes of Health, National Heart, Lung, and Blood Insti-
tute ARDS Network. Comparison of the SpO2 /FiO2 ratio and the PaO2 /FiO2
reaching a diagnosis of ARDS, some authors believe that the devel-
ratio in patients with acute lung injury or ARDS. Chest. 2007;132:410–7,
opment and application of standards to define disease processes http://dx.doi.org/10.1378/chest.07-0617.
improves the quality of medical care. Failure to do so could lead 4. Grieco DL, Maggiore SM, Roca O, Spinelli E, Patel BK, Thille AW, et al. Non-invasive
to interpretation errors that could have ominous implications for ventilatory support and high-flow nasal oxygen as first-line treatment of acute
hypoxemic respiratory failure and ARDS. Intensive Care Med. 2021;47:851–66.
clinical practice. 5. Liu L, Xie J, Wu W, Chen H, Li S, He H, et al. A simple nomogram for
In fact, an imprudent (time-dependent) use of non-invasive sup- predicting failure of non-invasive respiratory strategies in adults with COVID-
port systems may result in delayed endotracheal intubation and a 19: a retrospective multicentre study. Lancet Digit Health. 2021;3:e166–74,
http://dx.doi.org/10.1016/S2589-7500(20)30316-2.
worse clinical outcome. The presence of a pulmonary lesion causes
the distribution of inspiratory forces through the lung tissue to
Alejandro González-Castro a,∗ , Aurio Fajardo Campoverde b ,
be heterogeneous. An intense inspiratory effort interacts with the
Angello Roncalli c
solid behavior of the injured lung, thus generating a vertical gra-
dient in the regional transpulmonary pressure. This occurs mainly a Servicio de Medicina Intensiva, Hospital Universitario Marqués de
at the onset of inspiration and may shift pulmonary gas from the
Valdecilla, Santander. Spain
non-dependent, anterior lung regions to the dependent posterior b Unidad de Paciente Critico, Hospital Clínico Viña del Mar, Viña del
regions, a phenomenon known as Pendelluft that causes additional
Mar, Chile
regional overstretching in the dependent lung regions. Finally, it c Unidad de Fisioterapia Respiratoria, General Hospital of the State of
causes an increase in transmural pulmonary capillary pressure and
Alagoas, Maceió, Brazil
facilitates transvascular fluid leakage, which further aggravates
the interstitial and alveolar edema. These mechanisms might lead ∗ Corresponding author.
to spontaneous breathing resulting in a patient self-inflicted lung
E-mail address: e409@humv.es (A. González-Castro).
injury (P-SILI).4
2387-0206/© 2021 Elsevier España, S.L.U. All rights reserved.
You might also like
- Fast Arithmetic TipsDocument20 pagesFast Arithmetic TipsDumitru D. DRAGHIANo ratings yet
- Earth Works Volume Conversion and Swell FactorsDocument4 pagesEarth Works Volume Conversion and Swell FactorsJj BarakaNo ratings yet
- Stock TakeDocument14 pagesStock Takesafare2222No ratings yet
- R. Paul Wil - Rico ChetDocument7 pagesR. Paul Wil - Rico ChetJason Griffin100% (1)
- Cot 1 Detailed Lesson Plan in Science 10Document3 pagesCot 1 Detailed Lesson Plan in Science 10Arlen FuentebellaNo ratings yet
- R. Pasnau - Divisions of Epistemic LaborDocument42 pagesR. Pasnau - Divisions of Epistemic LaborMarisa La BarberaNo ratings yet
- Jitante Stotram v4 PDFDocument71 pagesJitante Stotram v4 PDFRamadevaNo ratings yet
- KF2.5-200 - With-M-C - GB - 03-15 KRACHT Bomba PDFDocument8 pagesKF2.5-200 - With-M-C - GB - 03-15 KRACHT Bomba PDFJairo Andrés FA100% (1)
- HELMETDocument11 pagesHELMETAndré MoutellaNo ratings yet
- High-Flow, Noninvasive Ventilation and Awake (Nonintubation) Proning in Patients With Coronavirus Disease 2019 With Respiratory FailureDocument11 pagesHigh-Flow, Noninvasive Ventilation and Awake (Nonintubation) Proning in Patients With Coronavirus Disease 2019 With Respiratory FailureCamila Fernanda Rivera ArayaNo ratings yet
- Use of Helmet Cpap in COVID-19 - A Practical ReviewDocument10 pagesUse of Helmet Cpap in COVID-19 - A Practical ReviewDoménica SánchezNo ratings yet
- The Pathophysiology and Dangers of Silent Hypoxemia in COVID-19 Lung InjuryDocument24 pagesThe Pathophysiology and Dangers of Silent Hypoxemia in COVID-19 Lung Injurypulmo unandNo ratings yet
- Redefining ARDS: A Paradigm Shift: Perspective Open AccessDocument7 pagesRedefining ARDS: A Paradigm Shift: Perspective Open Accesseyobhabtamu3No ratings yet
- 2021 AJEM High Flow Nasal Cannula For AdultDocument8 pages2021 AJEM High Flow Nasal Cannula For AdultRenzoFcoLavanLopezNo ratings yet
- Dead Space in ARDS Die HardDocument3 pagesDead Space in ARDS Die HardJose Morato E FlavianeNo ratings yet
- Editorials: Basing Respiratory Management of COVID-19 On Physiological PrinciplesDocument2 pagesEditorials: Basing Respiratory Management of COVID-19 On Physiological PrinciplesnoviaNo ratings yet
- Pathophysiological Patterns For TriagepdfDocument3 pagesPathophysiological Patterns For TriagepdfMayra VinuezaNo ratings yet
- CRISIS ventilator A 3D printed option for ventilator surge in mass respiratory pandemicsDocument8 pagesCRISIS ventilator A 3D printed option for ventilator surge in mass respiratory pandemicsdjaroslavskyNo ratings yet
- Respiratory Support For Adult Patients With COVID-19Document7 pagesRespiratory Support For Adult Patients With COVID-19SekarNo ratings yet
- References: Safety Considerations For Neuraxial Anaesthesia in Parturients With COVID-19Document2 pagesReferences: Safety Considerations For Neuraxial Anaesthesia in Parturients With COVID-19Muhammad RenaldiNo ratings yet
- Current Incidence and Outcome of The Acute Respiratory Distress SyndromeDocument6 pagesCurrent Incidence and Outcome of The Acute Respiratory Distress Syndromedarius2311No ratings yet
- An Intermediate Respiratory Care Unit in Every - 2023 - Archivos de BronconeumoDocument3 pagesAn Intermediate Respiratory Care Unit in Every - 2023 - Archivos de BronconeumoJuan Manuel Claros BustosNo ratings yet
- Early View: High-Flow Nasal Cannula For COVID-19 Patients: Low Risk of Bio-Aerosol DispersionDocument9 pagesEarly View: High-Flow Nasal Cannula For COVID-19 Patients: Low Risk of Bio-Aerosol DispersionSekarNo ratings yet
- Respirar 15 1 Art6 BDocument14 pagesRespirar 15 1 Art6 BJose Angel BurgaNo ratings yet
- CF Ventilation ManagementDocument10 pagesCF Ventilation ManagementSherry SaidNo ratings yet
- Reabilitação Nas Doenças IntersticiaisDocument13 pagesReabilitação Nas Doenças IntersticiaisBruno AlmeidaNo ratings yet
- HFNO vs NIV in COVID-19: Advantages and DisadvantagesDocument4 pagesHFNO vs NIV in COVID-19: Advantages and Disadvantagesevi nur janahNo ratings yet
- Predictors of Intubation in COVID-19 Patients Treated With out-of-ICU Continuous Positive Airway PressureDocument8 pagesPredictors of Intubation in COVID-19 Patients Treated With out-of-ICU Continuous Positive Airway PressureLucatntNo ratings yet
- Research PaperDocument11 pagesResearch Paperapi-625175559No ratings yet
- Ventilacion Mecanica en COVID 19 Una Perspectiva FisiologicaDocument11 pagesVentilacion Mecanica en COVID 19 Una Perspectiva FisiologicaPablo gonzález sánchezNo ratings yet
- Year in Review 2019: High-Flow Nasal Cannula Oxygen Therapy For Adult SubjectsDocument13 pagesYear in Review 2019: High-Flow Nasal Cannula Oxygen Therapy For Adult SubjectsRicardoNo ratings yet
- Pulmonary Physiotherapy in Covid 19 5850Document2 pagesPulmonary Physiotherapy in Covid 19 5850juan felipeNo ratings yet
- PathoPhysiology of Ards 2017Document22 pagesPathoPhysiology of Ards 2017Andi sutandiNo ratings yet
- Roberts 2019 Year in Review Adult Invasive MechDocument6 pagesRoberts 2019 Year in Review Adult Invasive MechJose Luis Escobar zabaleguiNo ratings yet
- The Pathophysiology of Happy' Hypoxemia in COVID-19: Review Open AccessDocument9 pagesThe Pathophysiology of Happy' Hypoxemia in COVID-19: Review Open AccessMuhammad Taufiq AmrullahNo ratings yet
- Re-Thinking Early Intubation of COVID-19 Patients: Is It Time for a ChangeDocument4 pagesRe-Thinking Early Intubation of COVID-19 Patients: Is It Time for a ChangeGilberto ValenciaNo ratings yet
- 2023 Ards PelosiDocument25 pages2023 Ards PelosiMiky DinuNo ratings yet
- Respiratory Medicine Case ReportsDocument3 pagesRespiratory Medicine Case ReportsAzhari BaedlawiNo ratings yet
- SpO2FiO2 As A Predictor of Non-Invasive Ventilation Failure in Children With Hypoxemic Respiratory InsufficiencyDocument10 pagesSpO2FiO2 As A Predictor of Non-Invasive Ventilation Failure in Children With Hypoxemic Respiratory InsufficiencypelaojaegerNo ratings yet
- Awake Prone Positioning in COVID-19Document2 pagesAwake Prone Positioning in COVID-19Rima HanifatiNo ratings yet
- Pi Is 0749070421000439Document21 pagesPi Is 0749070421000439Vlady78No ratings yet
- Positive End Expiratory Pressure in COVID 19 Related ARD - 2021 - Journal of CriDocument3 pagesPositive End Expiratory Pressure in COVID 19 Related ARD - 2021 - Journal of CriJosé Carlos Bernaola ZevallosNo ratings yet
- 2022 Miguel Angel Diaz - Clinical Features and Outcomes Associated With BroDocument7 pages2022 Miguel Angel Diaz - Clinical Features and Outcomes Associated With BroSteve aokiNo ratings yet
- A Belgian Survey On The Diagnosis of Asthma - COPD Overlap SyndromeDocument13 pagesA Belgian Survey On The Diagnosis of Asthma - COPD Overlap SyndromesyahrulNo ratings yet
- Pi Is 0003999321003269Document12 pagesPi Is 0003999321003269Amanda SchaefferNo ratings yet
- Respiratory Function in Patients Post-Infection by COVID-19: A Systematic Review and Meta-AnalysisDocument10 pagesRespiratory Function in Patients Post-Infection by COVID-19: A Systematic Review and Meta-AnalysisHendri WahyudiNo ratings yet
- Proning in Non-Intubated (PINI) in Times of COVID-19: Case Series and A ReviewDocument7 pagesProning in Non-Intubated (PINI) in Times of COVID-19: Case Series and A ReviewCarlos ZepedaNo ratings yet
- 1 s2.0 S0140673622010522 MainDocument18 pages1 s2.0 S0140673622010522 MainsilviaNo ratings yet
- Ventilatory Strategies in Obstructive Lung. Parrilla2014Document10 pagesVentilatory Strategies in Obstructive Lung. Parrilla2014EzeBorjesNo ratings yet
- Prone For COVID: Are You Awake?: EditorialDocument2 pagesProne For COVID: Are You Awake?: EditorialMahtosurup GodavarthyNo ratings yet
- Fisiopatologia de SDRADocument19 pagesFisiopatologia de SDRARuben HerediaNo ratings yet
- The Acute Respiratory Distress Syndrome: Review SeriesDocument10 pagesThe Acute Respiratory Distress Syndrome: Review Seriesadek07No ratings yet
- Hfo 3Document8 pagesHfo 3markus_danusantosoNo ratings yet
- Jurnal AnosmiaDocument5 pagesJurnal Anosmiadhea handyaraNo ratings yet
- Comment: Lancet Respir Med 2017Document2 pagesComment: Lancet Respir Med 2017Novy DitaNo ratings yet
- Imcrj 13 341Document5 pagesImcrj 13 341TisaNo ratings yet
- Finster Er 2020Document2 pagesFinster Er 2020Arief PurwoditoNo ratings yet
- Addendum CTS CSRT COVID PFT Version 2 Dec-18 2020Document2 pagesAddendum CTS CSRT COVID PFT Version 2 Dec-18 2020Chen Prencess TomabieneNo ratings yet
- Incidence of Deep Venous Thrombosis in Patients WiDocument8 pagesIncidence of Deep Venous Thrombosis in Patients WiZainab MotiwalaNo ratings yet
- Aerosol Genera CovidDocument2 pagesAerosol Genera Covidrodolfo riosNo ratings yet
- ARBR 2806 Edit ReportDocument5 pagesARBR 2806 Edit ReportJosé Manuel Valencia GallardoNo ratings yet
- Letter TO THE Editor: Is The Nasal Airway The Main Mode of Transmission For Pharyngeal Tuberculosis?Document2 pagesLetter TO THE Editor: Is The Nasal Airway The Main Mode of Transmission For Pharyngeal Tuberculosis?joshkelNo ratings yet
- contoh copdDocument13 pagescontoh copdAdistha Eka Noveyani,No ratings yet
- Pneumothorax in COVID-19 Disease-Incidence and Clinical CharacteristicsDocument9 pagesPneumothorax in COVID-19 Disease-Incidence and Clinical CharacteristicsFolder PulmoNo ratings yet
- 1 s2.0 S003139551730072XDocument21 pages1 s2.0 S003139551730072XvgmanjunathNo ratings yet
- COVID-19 Indirect Contact Transmission Through The Oral Mucosa Must Not Be IgnoredDocument4 pagesCOVID-19 Indirect Contact Transmission Through The Oral Mucosa Must Not Be IgnoredSergio Losada AmayaNo ratings yet
- Karim 2019Document3 pagesKarim 2019belveraqsunnyNo ratings yet
- Anatomija Za Umetnike PDFDocument4 pagesAnatomija Za Umetnike PDFДанило ВујачићNo ratings yet
- Business Research Study Material - Calicut UniversityDocument50 pagesBusiness Research Study Material - Calicut UniversityDr Linda Mary SimonNo ratings yet
- Makalah KesehatanDocument9 pagesMakalah KesehatanKUCLUK GamingNo ratings yet
- Roberson-FRIT 7236 Assessment PlanDocument13 pagesRoberson-FRIT 7236 Assessment PlanMarie RNo ratings yet
- Unit 1 Lesson 2 PDFDocument20 pagesUnit 1 Lesson 2 PDFKristyll ArguellesNo ratings yet
- EngM6 TB WebDocument161 pagesEngM6 TB WebNong BillNo ratings yet
- RuelliaDocument21 pagesRuelliabioandreyNo ratings yet
- Analie T. Caro: Personal ParticularsDocument4 pagesAnalie T. Caro: Personal ParticularsAnalie Tañamor CaroNo ratings yet
- Cooper Tire Warranty InformationDocument28 pagesCooper Tire Warranty InformationAbdulAziz AlGhamdiNo ratings yet
- The Man Who Married A Hen, Stories of A Zambian SchoolboyDocument78 pagesThe Man Who Married A Hen, Stories of A Zambian SchoolboyGerard StoutNo ratings yet
- The dangers of electrostatic phenomenaDocument14 pagesThe dangers of electrostatic phenomenaYaminNo ratings yet
- Understanding Customer Loyaltyfor Retail StoreandtheinfluencingfactorsDocument15 pagesUnderstanding Customer Loyaltyfor Retail StoreandtheinfluencingfactorsTanmay PaulNo ratings yet
- Bobcat Sambron Telescopics Handler Tec3070 3092 Spare Parts Catalog 63902 1Document15 pagesBobcat Sambron Telescopics Handler Tec3070 3092 Spare Parts Catalog 63902 1elijahmitchellmd220597jrpNo ratings yet
- WRITTEN ASSIGNMENT Unit 2 - The Peer Assessment Strategy - 1Document2 pagesWRITTEN ASSIGNMENT Unit 2 - The Peer Assessment Strategy - 1asdsafsvvsgNo ratings yet
- Pilani MTech SS PDFDocument12 pagesPilani MTech SS PDFonline accountNo ratings yet
- Moana Taka PartnershipDocument2 pagesMoana Taka Partnershipself sayidNo ratings yet
- Uss Port Royal (CG 73)Document9 pagesUss Port Royal (CG 73)samlagroneNo ratings yet
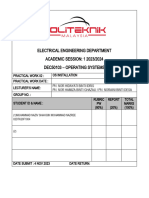
- Dec50103 PW2 F1004Document14 pagesDec50103 PW2 F1004Not GamingNo ratings yet
- Let's think step by step:- The common factor of 32, 45 and 50 is 5- 32/5 = 6.4 meters - 45/5 = 9 meters- 50/5 = 10 meters- So the best option is the 50 meter wire.b. How did you get the answerDocument59 pagesLet's think step by step:- The common factor of 32, 45 and 50 is 5- 32/5 = 6.4 meters - 45/5 = 9 meters- 50/5 = 10 meters- So the best option is the 50 meter wire.b. How did you get the answerjsphmnsycjrscribdNo ratings yet
- RGB PDFDocument35 pagesRGB PDFGestion Medios Zamba ColorsNo ratings yet
- NB-CPR 17-722r8 - General Guidance On AVCP (Working Copy)Document25 pagesNB-CPR 17-722r8 - General Guidance On AVCP (Working Copy)halexing5957No ratings yet
- Country/Airport City Laboratory: AfghanistanDocument25 pagesCountry/Airport City Laboratory: AfghanistanLudovic DumitruNo ratings yet