Professional Documents
Culture Documents
AIIMS Peds Pulmo Protocols-Version June 2017
Uploaded by
Vijay ArumugamOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AIIMS Peds Pulmo Protocols-Version June 2017
Uploaded by
Vijay ArumugamCopyright:
Available Formats
This Document has been modified with Flexcil app (iOS) https://www.flexcil.
com
AIIMS Peds Pulmo Protocols-June 2017
AIIMS Pediatric Pulmonology Protocols
Version: June 2017
Pediatric Pulmonology Division
Department of Pediatrics
All India Institute of Medical Sciences
New Delhi-110029
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
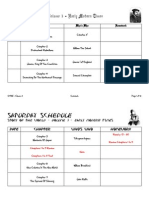
Index
Serial no. Protocol title Page no.
1. Bronchial Asthma 3-15
2. Preschool wheezing 16-25
3. Cystic fibrosis 26-58
4. Non-CF bronchiectasis 59-68
5. Allergic Bronchopulmonary aspergillosis 69-78
6. Interstitial lung disease 79-86
7. Pulmonary hemorrhage 87-92
8. Sarcoidosis 93-99
9. Chemical pleurodesis with Povidone iodine 100-101
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Bronchial Asthma
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Bronchial Asthma
Consider Asthma if there is: Recurrent cough/ wheeze/ breathlessness/chest tightness with one
or more of following characteristics:
1. Seasonal variation: occurs with change in season or more in one season
2. Nocturnal: More in night time
3. Exertional /stress/activity induced symptoms
4. Parents may be able to tell about precipitating events
5. Family history of asthma or allergy
If asthma is suspected, may do a bronchodilator test:
For bronchodilator test: Measure base line PEFR (below 5 years of age)/ or FEV1 (in
children above 5 years of age) and repeat it after 10-15 minutes of giving inhaled
salbutamol (nebulization with 2.5 mg respule/respiratory solution or 4-5 puffs of 100mcg
MDI with spacer). If the difference is > 15% for PEFR and >12% for FEV1then asthma
is confirmed. Bronchodilator test is done by respiratory nurse in room no. 6 on
Wednesday and Saturday and in room no. 5 on Thursday in OPD and in Pediatric
Pulmonary Function test lab in C5 ward (by appointment).
Think of alternative diagnosis: If any of the following is present
• Symptoms present from birth or perinatal lung problem
• Excessive vomiting or posseting
• Severe upper respiratory tract infection
• Persistent wet/productive cough
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
• Feeding difficulties like choking, regurgitation
• Failure to thrive
• Unexpected clinical findings e.g. clubbing, localised or monophonic wheeze, abnormal
voice or cry, dysphagia, inspiratory stridor
• Focal or persisting radiological changes
• Failure to respond to conventional treatment
(particularly inhaled corticosteroids above 400mcg/day or frequent use of steroid tablets)
with good compliance and technique.
Investigations
• To rule out alternative diagnoses if suspected
• Chest X ray initially once to rule out asthma mimickers
• Lung function testing: Spirometry if >5 years age: room no. 6 on Wednesday and
Saturday and in room no. 5 on Thursday in OPD and in Pediatric Pulmonary Function
test lab in C5 ward (by appointment).
Once asthma is diagnosed, assess for the control of asthma by using following symptoms
(Table 1) and for any risk factors for future exacerbations of asthma (Table 2).
Table 1: Assessment of asthma control
Symptoms (in last 4 weeks) Level of control
Day time symptoms >2 times/week Controlled: none of the these
Any limitation of activity Partially controlled: 1-2 of these
Any nocturnal awakening Uncontrolled: ≥3 of these
Need for rescue treatment >2 times/week
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Table 2: Risk factors for future exacerbations of asthma
Modifiable risk factors • Uncontrolled symptoms
• Inadequate ICS
• High SABA usage (>1 canister per month)
• Low FEV1 (<60% predicted)
• Comorbidities: obesity, rhinosinusitis, food allergy
• Exposure: smoking, allergens
• Socioeconomic problems
• Sputum or blood eosinophilia
Non modifiable risk • Ever intubated or PICU admission
factors • >1 severe exacerbation in last 12 months
Long term therapy for asthma: It is based on step-wise approach (Table 3). For long term
management of asthma, there are 2 scenarios: (1) Child not on any regular inhaled steroid
therapy; (2) Child already getting inhaled therapy.
Consider long term therapy in children who are not on regular inhaled steroid therapy, based on
presenting symptoms as shown in Table 5. If child had infrequent symptoms, but exacerbations
are severe enough requiring hospital admission and/or ICU admission, consider regular step 3
treatment (Medium ICS or Low ICS plus LABA) If child already on ICS therapy; assess asthma
control based on Table 1 and step up or step down the therapy based on level of control.
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Table 3: Long term step-wise management of asthma
Step of Controller Other controller option Reliever
treatment
Step 1 No controller
Step 2 Low dose ICS* • LTRA
• Slow release theophyllin
Step 3 <12 yrs: Medium dose ICS • Low dose ICS+LTRA
≥12 yrs: Low dose ICS with • Medium dose ICS
LABA SABA as
required
Step 4 Medium dose ICS with • Medium dose ICS+LTRA
LABA • High dose ICS
• Moderate dose
ICS+Theophyllin (>12
yrs)
Step 5 Low dose oral steroids • Anti IgE (Omalizumab)
*See Table 4.
Table 4: Estimated clinically comparable doses of ICS (Source: IAP- Asthma Training
Module 2016)
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Table -5: Long term therapy in patients who are not on controllers
Presenting symptoms Long term prevention
First choice Other option
Infrequent symptoms No long term therapy (Step
1)
Infrequent symptoms but it is with any Low dose ICS (Step 2) LTRA
risk factors for exacerbation
Symptoms like partly controlled asthma
(symptoms more than twice a week, night
awakening more than once a month)
Symptoms like uncontrolled asthma Medium dose ICS (<12 yrs) Low/medium
(symptoms on most of days, night or dose
awakening more than once a week) Low dose ICS+LABA (>12 ICS+LTRA/The
yrs) (Step 3) ophylline
Severely uncontrolled asthma (daily Medium to high dose Short course
severe symptoms, almost daily night ICS+LABA (Step 4) steroids and
awakening, limited physical activity) high dose ICS or
moderate dose
ICS+ LABA
Classification of asthma severity
Now, severity of asthma is classified based on treatment step required to control the asthma
symptoms. (Table 6)
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Table 6. Classification of asthma severity
Asthma grade Symptoms Treatment step
Intermittent asthma infrequent and mild episodes Step -1
Mild Asthma Frequent and / or severe episodes, Step-2
almost weekly symptoms
Moderate asthma > 1 time a week Step -3
but < 1 time a day
Severe Asthma daily symptoms not responding to Step – 4 or above
ICS with add on therapy
Follow up:
• Call for first follow up in 1 week to ensure technique and compliance of inhaled
medication
• Once, the physician and parents are comfortable with dosing and technique of drugs, call
every 8-12 week or SOS.
• If good control achieved for at least 6 months, consider step down the therapy: decrease
25% dose of ICS every 3 monthly if asthma remained controlled. If child getting ICS plus
LABA, first decrease ICS as suggested above and remove LABA once ICS dose is
reached at 100 g daily of Budesonide or equivalent. If child’s asthma remain controlled
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
on low dose ICS for one year, consider stopping ICS with counselling of parents that
asthma is not cured and child may need ICS in future again.
• If partially or poorly controlled review the technique, compliance, drug dosage, triggers,
co morbid conditions and decide step up therapy
Outline for management of poorly controlled asthma:
Rule out alternate diagnoses
If no control
Check correctable issues:
Compliance, Technique, Triggers
If no control
Look for and address co morbid conditions
Obesity, GER, Allergic rhino-sinusitis
If no control
Step up therapy
If no control
Consider work up for ABPA-if negative:
Omalizumab if total IgE high, test for 1-2
allergens if suggested by history and
10
immunotherapy if needed.
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
When to register the patients in Pediatric Chest Clinic (Thursday 2PM): Mild asthma may be
managed on regular OPD basis. If problems, send them to Pediatrics 3 OPDs
Management of co-morbidities
Allergic Rhinitis:
• Mometasone nasal spray 1 spray each nostril BD for 4 – 8 weeks or
• If allergic rhinitis is associated with adenoid hypertrophy, prolong the use of
Mometasone nasal spray till symptoms of adenoid hypertrophy subsides.
• Tab Monteleukast (Inferior alternative)
< 5yr : 4mg OD
5-10yr: 5mg OD
>10yr : 10mg OD
Allergic conjunctivitis:
Cromal (sodium cromoglycate ) eye drops 1 drop q 6 hrly both eyes for 1 -2 week, than SOS.
Gastroesophageal reflux disease (GERD):
Domeperidone: 0.2-0.3 mg/kg/dose TDS and
Proton Pump Inhibitor (Lansperazole or Pantperazole): 1 mg/kg/day, OD empty stomach.
Obesity:
Physical activity, good food habits, dietician referral.
11
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Management of acute asthma: Refer to AIIMS PICU Protocol for acute asthma.
How to counsel the parents:
1. There is no cure for asthma. However, it can be controlled with regular and proper
inhalation therapy
2. Some children may outgrow asthma symptoms with age. However, its difficult to predict
who would do so.
3. Inhalers deliver the medication directly to airways and better than oral medication
4. Child needs inhaler and would not become habit
5. Inhalation steroids are not harmful for the child growth compared to uncontrolled asthma
itself
6. Alternative therapies like homoeopathy, ayurveda are not well validated
7. Inhalers are safe and more effective than nebulisers
8. Not to stop medication by patient/parents even if the child is symptomatically better
9. Normal physical activity for the age
10. No food restrictions
11. Regular follow up in the clinic
12
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
PEFR: It depends on height of child. Approximate PEFR values based on height may be
considered as shown below in Table.
Height PEFR
100cm 100L/min
110cm 150L/min
120cm 200L/min
130cm 250L/min
140cm 300L/min
150cm 350L/min
Commonly used asthma medications at AIIMS:
Bronchodilators:
Salbutamol:
• MDI 100mcg/puff
• Asthalin respule (2.5mg/2.5ml)
• Asthaline respiratory solution (vial): 5mg/1ml
• Asthalin Syrup (2mg/5ml)
• Asthalin Tablet (2mg, 4mg, 8mg)
13
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Levosalbutamol:
• Duolin respule ( Levosalbutamol 1.25mg and Ipratropium 500mcg/2.5ml)
Inhaled steroids:
Budesonide:
• MDI 100,200mcg/puff
• Budecort respule (500mcg/2ml)
Fluticasone propionate:
• MDI 125,250 mcg/puff
• Fluticasone respules (500mcg/2ml)
Inhaled corticosteroids + LABA:
• Foracort (Budesonide 100/200/400mcg + Formeterol 6mcg/puff)
Methylxanthines:
• Tab.Theophyllin (100mg,200mg,300mg,450mg)
• Syp.Theophyllin (50mg/5ml)
LTRA:
• Montelukast (Tab 4mg, 5mg,10mg)
• Syp Montelukast (5mg/5ml)
Inhaled anticholinergics:
Ipratropium :
14
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
• Ipravent respule (500mcg/2ml)
• MDI Ipratropium (20mcg or 40mcg/puff)
• Duolin respule ( Levosalbutamol 1.25mg and Ipratropium 500mcg/2.5ml)
Steroid Nasal spray:
Mometasone nasal spray: 50 g per spray (Metaspray OR Nasonex)
15
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Preschool Wheezing
16
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Preschool Wheezing
Wheezing in preschool children is a common phenomenon. Almost one out of four infants have
one episode of wheezing by nine month of age and by age of six years, nearly half children have
at least one episode of wheezing.
All respiratory sounds are not wheeze. It is prudent to identify wheeze accurately. History of
wheezing by parents is not always reliable as they often interpret other respiratory sounds as
wheezing also. Documented wheezing by a physician is most reliable tool to make a diagnosis of
wheezing.
Preschool child with wheeze
When a preschool child comes with history of wheeze, first try to confirm that it is wheeze only:
by detailed history, documentation of wheezing in previous visits or if wheezing present during
this visit.
Once wheezing confirmed, evaluate the child by thorough history and examination (Box 1).
17
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Box 1: Features to be evaluated in history and examination in preschool children with
wheezing
HISTORY
1. Is wheezing really present? 12. How frequent are respiratory
2. Was child born preterm and required, symptoms (wheezing)? (Does child
ventilation or prolonged oxygen remain well between episodes?)
therapy? 13. Are there symptoms related to other
3. Did symptoms started at birth or later organ systems?
on? 14. What is severity of symptoms?
4. Was onset sudden or gradual? (requiring hospital admission, IV
5. How is child growing and medications etc.)
developing? 15. What are triggers? Viral infections
6. Are there signs of intestinal only or others also (crying, laughing,
malabsorption including frequent, exercise, season change, cold items,
large volume, or oily stools? smoke, dust mites, construction dust,
7. Is there history of feeding mold, cockroaches etc.)
difficulties? (choking, vomiting) 16. Are symptoms more during night?
8. Is there another child in the home by (which part of night-just after sleep or
whom foreign body aspiration could early morning)
have occurred? 17. Is there response to beta-2 agonist
9. Do symptoms change with position? therapy?
10. Is there frequent rhinitis and ear 18. Does child have personal history of
discharge? eczema?
11. Is there family history of cystic 19. Is there family history of asthma,
fibrosis, immunodeficiency, or allergic rhinitis, and atopy?
tuberculosis? 20. Is child having development delay
PHYSICAL EXAMINATION
Signs of respiratory distress, pulse oximetry (if available)
Anthropometry: for failure to thrive.
Clubbing-almost always indicate a serious underlying condition
Look for any allergy markers (eczema, allergic shiner, Dennie’s lines, allergic crease,
allergic salute, allergic gap, posterior oropharynx cobblestoning etc)
Chest examination:
Look for any chest wall deformity,
wheezing (expiratory, biphasic, mono/polyphonic, localized/generalized)
crepts
CVS examination
Look for organomegaly
Assess for central nervous system abnormality especially development delay, tone,
hearing.
18
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Consider differential diagnoses of wheezing in preschool children as shown in Table 1.
Wheezing due to congenital malformations is present since birth. Foreign body aspiration is most
common between 1-5 years of age.
Table 1: Differential diagnosis for wheezing in preschool children
A. Wheezing secondary to underlying condition
Infections: Suppurative lung diseases
Viral (RSV, rhinovirus, adenovirus, Cystic fibrosis
influenza, parainfluenza, etc) Primary ciliary dyskinesias
Atypical: chlamydia, mycoplasma Bronchiectasis
Bacterial pneumonia
Tracheitis
Retropharyngeal abscess
Tuberculosis
Anatomic abnormalities Aspiration syndromes
Central airway abnormalities GERD
Laryngomalacia, tracheomalacia, and Pharyngeal/swallow dysfunction
/or bronchomalacia
Tracheoesophageal fistula
(specifically H-type fistula) Others
Large laryngeal cleft (resulting in Immunodeficiency-congenital/acquire
aspiration), laryngeal web Bronchopulmonary dysplasia
Airway Compression from outside Interstitial lung disease, including
Vascular ring bronchiolitis obliterans
Mediastinal lymphadenopathy from Anaphylaxis
infection or tumor Inhalation injury-burns
Esophageal foreign body, Esophageal Vocal cord palsy
anomalies (e.g., enteric cyst) Hypocalcemia
Congenital malformations Congenital heart disease with left-to-
Bronchial cyst or lung cyst right shunt (increased pulmonary
Congenital lobar emphysema flow), massive cardiomegaly, left
Aberrant tracheal bronchus atrial enlargement, and dilated
Sequestration pulmonary arteries.
Intraluminal foreign body
Adenoidal hypertrophy
B. Wheezing without underlying condition
19
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Next step is to classify wheezing in preschool children
There is lack of consensus to classify wheezing in preschool children. But, for clinical purpose
we can classify wheezing having a specific underlying disorder and wheezing without any
underlying disorder (Table 1). The second group may further be classified as EVW and MTW.
EVW occurs as discrete episodes of 1-4 weeks duration and child is well between episodes and
each episode is usually preceded by a viral respiratory infection. MTW presents with discrete
episodes of wheezing triggered by viral infections but child also has interval symptoms in
response to various triggers like excessive laughing or crying, exercise, smoke, cold air. Children
with MTW often have other associated allergies. Many times, it may be difficult to differentiate
EVW and MTW, therefore, the term “recurrent wheezing” may be used for all preschool
children who had recurrent episodes of wheezing.
Diagnosis of wheezing in preschool children
If a specific condition is suspected on detailed history and examination, investigate for that
disorder (Table 2). If a specific condition is not suspected on history and examination, even chest
x-ray is not required unless symptoms are abnormally severe, recovery is very slow or
incomplete (resulting in prolonged or repeated hospital admission) and parents are very anxious.
Eosinophil count, skin prick test and total IgE are not of any use and are not recommended.
Testing for viruses is considered for research purposes only at present. Tests for GER [GER
scan, Ba swallow, Ph study (if there is high index of suspicion and Ba swallow and GER scan are
normal)] may be considered for children especially to whom wheezing started below one year of
age and there is history of vomiting, cough after some time of feeding and infant keeps neck
20
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
extended. In other cases, investigations are needed only for frequent and severe wheezing which
respond poorly to treatment and require multiple hospitalizations.
Table 2: Suggested investigations for a child with wheezing as per specific history and
examination
History/examination Suspected condition/s Suggested Investigation/s
Child was born preterm and require Bronchopulmonary CXR
ventilation or prolonged oxygen dysplasia (BPD)
requirement.
Symptoms started at birth or soon Congenital anomalies ENT evaluation,
thereafter. Bronchoscopy
Child having failure to thrive Cystic fibrosis (CF), Sweat test, Ig levels, HIV
immunodeficiency.
There is frequent, bulky, or oily stools Cystic fibrosis Sweat test
Child has choking, vomiting during or H type fistula, GERD, CXR, Barium study, GER
after feeding laryngeal cleft scan, ENT, Bronchoscopy,
Ph study
There is another child in the home by FB aspiration especially if Bronchoscopy
whom foreign body aspiration could have sudden onset
occurred
Symptoms are changing with position Airway malformation, ENT evaluation,
adenoids, obstructive bronchoscopy, X-ray soft
sleep apnea tissue neck, sleep study
Continuous rhinitis and frequent ear Primary ciliary dyskinesia FeNO/nasal NO, electron
discharge since early infancy microscopy
Family history of cystic fibrosis, Corresponding disease For corresponding disease
immunodeficiency, or TB.
Clubbing CF, immunodeficiency, Sweat test, Ig levels, HIV
HIV infection
Murmur, loud p2 Congenital heart disease CXR, echocardiography
21
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Treatment
An algorithm, how to approach a preschool child with wheezing, is shown in Figure 1. First step
is to take detailed history and physical examination as suggested above in every preschool child
with recurrent wheezing. If a specific disorder is suspected based on history and examination,
investigate for it and treat if the condition is confirmed. If no specific underlying disorder is
suspected in history and examination or no disorder is identified after appropriate investigation,
we can classify the wheezing as EVW or MTW. The distinction between EVW and MTW may
not be always easy in many preschool children and sometimes EVW may turn into MTW and
vice versa. Therefore, frequency and severity of wheezing episodes should be criteria for
treatment rather than wheezing phenotype. If wheezing episodes are severe enough to require
multiple hospitalizations, episodes are occurring once or twice every month, there is frequent
sleep disturbances and child is symptomatic in between episodes, and episodes are prolonged it
should be treated with inhaled corticosteroids.
The inhaled corticosteroids (ICS) are used is low to moderate doses (200-400 µg of budesonide
or equivalent per day) via metered dose inhaler with spacer and mask. The individual episodes of
wheezing should be treated with inhaled or nebulised short acting beta agonists with oral steroids
in very severe episodes. Metered dose inhaler with spacer and mask is as effective as nebulizer
for ICS and short beta 2 agonists in preschool wheezing and it should be first line device except
in some sick children who are unable to take inhalers.
22
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Figure 1: Approach to treat wheezing in preschool children
A trial of three months with good compliance and proper inhalational technique should be given
before determining the response. If child responds to ICS, we can stop treatment after three
months. If symptoms recur, he or she may be labelled as asthma and should be treated and
followed accordingly. If child does not respond with ICS, despite proper technique and good
compliance, stop them and investigate further. Further investigations may include chest x-ray (if
not done earlier), hemogram, tests for GER, CT chest or bronchoscopy as appropriate. There is
lack of evidence for or against the use of leukotrience receptor antagonists (montelukast) either
daily or intermittent in preschool children with recurrent wheezing in both EVW and MTW
phenotypes and not used at present. Avoid smoking at home in all cases of wheezing.
23
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Facts considered for counselling of parents
Episodic viral wheezing is usually not associated with atopy and rarely progresses to
asthma. In most of the cases, we can say that it is very unlikely to be asthma.
There is no consensus when to label asthma in preschool children. Asthma in preschool
children is considered if there are recurrent episodes of wheezing or coughing with
exercise, laughing, or crying in absence of apparent respiratory infection, there is history
of atopy or asthma in family and symptoms improves within 2-3 months of controller
medications and worsens after cessation. If a preschool child fulfills all above criteria,
then we can label it as asthma. But it is only after use of controller medications and not at
first instance. It is better to use terms EVW and MTW (or simply recurrent wheezing)
initially and asthma can be labelled in follow up.
It is difficult to say which preschool children with recurrent wheezing will have asthma
later in life? But, if there is history of asthma in parents or child has associated atopic
dermatitis and/or allergic rhinitis, and has wheezing without colds, there is more chance
of having asthma later in life. It is based on asthma predictive index (API) (Table 3).
Use of inhaled steroids either intermittently or continuously for preschool wheezing had
no effect on development of asthma and wheezing later in life.
Avoid smoking at home.
24
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Table 3: Asthma Predictive Index* (Modified from J Allergy Clin Immunol 114:1282–1287, 2004)
MAJOR CRITERIA MINOR CRITERIA
Parental asthma Physician diagnosed allergic rhinitis
Physician diagnosed personal eczema Wheezing without cold
Eosinophilia ≥4%
*API is defined as loose index if there is any wheezing episode during first three years of life along with one
major or two minor criteria and as stringent index if there are frequent wheezing episodes during first three
years of life along with one major or two minor criteria. With positive loose index there is 2 to 5 times more
likely to have asthma at 6-13 years of age and risk increases to 4 to 9 times with stringent index.
25
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Cystic Fibrosis
26
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Cystic Fibrosis
Suspect cystic fibrosis (CF) in following conditions and ask for sweat chloride test:
- Recurrent/Chronic sinopulmonary disease
- Persistent/poorly resolving Pneumonias
- Unexplained diffuse lung disease or bronchiectasis
- Malabsorption, gastrointestinal manifestation including fat soluble vitamin
deficiencies
- Nutritional abnormalities including unexplained failure to thrive
- Unexplained or unusual neonatal respiratory distress
- Meconium ileus
- Rectal prolapse
- Prolonged neonatal jaundice
- Late onset hemorrhagic disease of newborn
- Salt depletion syndrome
- Acute or chronic pancreatitis
- Azoospermia
- Family history of CF
- Positive newborn screening (positive Immunoreactive trypsinogen; IRT), if done.
Sweat chloride test is done twice a week (Monday and Wednesday 2 PM onwards) in room no
3067 teaching block (Dr S K Kabra’s office). It is desirable to take appointment from Cystic
27
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Fibrosis Nurse before sending the patients. CF nurse is available in Pediatrics OPD daily 9AM to
1PM. In afternoons she is available in Dr Kabra’s office.
Sweat Chloride test can be done in children more than 2 weeks and more than 2 kg.
Interpretation of sweat test: -
Results must be interpreted in the clinical context
Collected sweat weight should be more than 100 mg for analysis and interpretation
1. Normal sweat Cl- <40 mmol/l;
2. If 2 values of sweat chloride done at least one week apart > 60 mEg/L with sweat weight
more than 100 mg – make a diagnosis of CF with clinical context.
3. If sweat chloride level 40 to 60 mmol/l, need repeating with correlation with clinical
picture.
4. If Chloride value between 40-60 meq/L in two different occasions follow-up as suspected
CF, but give a label of CF on follow-up – if at least one of the mutation is identified, or
other ancillary tests supports diagnosis of CF. Sweat test may be repeated after 4-8
weeks.
If sweat weight (i.e. less than 100 mgs) on repeated occasions – repeat sweat test after 4 - 8
weeks.
False negative results.
Cases are increasingly recognized where the clinical picture of CF is supported by genotyping,
but in the presence of a normal sweat test. However, it is <1% CF patients, therefore it accurate
enough to handle patients with resource poor setting.
28
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Nevertheless, beware of the context is more appropriate before excluding the diagnosis (in highly
suggestive cases) on the basis of a normal sweat test alone. If facilities are available genetic
testing or nasal potential difference testing would be the appropriate next step.
False positive results.
Many theoretical causes as listed in textbooks, most of which do not appear to cause problems in
routine clinical practice. Those which may be encountered include malnutrition or skin disorders
such as severe dermatitis/eczema. Transient increases in sweat electrolytes have also been
reported in young patients with immunodeficiency states.
Work up of CF Patients
After the diagnosis of CF is made – do the following investigations
(i) X ray film of chest (CXR) if not done earlier
(ii) Chest CT scan if indicated (Doubtful patients or in complications)
(iii) Blood test – Liver functions
Renal functions
Complete Blood Counts
Serum Electrolytes (Na, K, Cl)
Calcium, Phosphate, serum alkaline phosphate (SAP)
Blood Sugar
PT/INR – selected patients with bleeding manifestations
(iv) GER scan, Ba swallow (if associated GER is suspected)
(v) Esophageal pH monitoring (if strong suspicion of GER and GER scan and Ba
swallow are normal)
29
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
(vi) USG Abdomen
(vii) Mutational analysis - Blood for CF mutation (send patient with a requisition to
Genetic Unit, Old operation Theatre Building, Near College of Nursing)
(viii) Genetic and antenatal counselling – according to the requirement
All confirmed patients should be directed for counseling by Prof S K Kabra or Dr K R Jat once
diagnosis is made. They should be directed to CF sister and physiotherapist as early as possible
for relevant education. Resident or fellow should be responsible to make sure parents education
regarding the disease process, chest physiotherapy, diet, medication, inhalation techniques and
precautions before they leave clinic or ward premises.
Care of CF patient in Pediatric Chest Clinic (PCC)
All CF patients are followed up in room 05 PCC (Thursday 2 pm) at interval of 6-12 weeks. On
each visit the patient comes to CF Nurse. CF nurse takes out his/her file, records weight, height,
medicines taken by the child. Then spirometry to document FEV1/FVC, FEV1, FVC and
MEF25-75 by CF nurse/technician/registrar (posted in PFT) and after spirometry child is seen by
physiotherapist in room B. She checks the physiotherapy technique and records in the file. CF
nurse/research assistant takes cough swab, deep throat swab after physiotherapy and sputum
culture. After this child is brought to consultant/ Registrar. After assessment and advise by
doctor child goes back to CF nurse for appointment of next visit. CF nurse may be able to
provide some medicines if they are available.
If it is first visit – patient will be registered at room no 10, they should be sent to room 05 for
spirometry (age> 5 years only) and room B to learn chest physiotherapy before discussing the
patient in room 05. New patient they should be educated as indicated above as per newly
diagnosed patient.
30
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Annual Work Up
The idea behind is to identify disease progression and to identify complications. Annual work up
can be done in admitted patients during the ward stay or during PCC visits. Please try to arrange
them in convenient manner for patients.
Anthropometry
Spirometry
LFT: SGOT, SGPT, Serum Bilirubin, Serum Albumin/Globulin, PT/INR
S. Calcium, Phosphate, SAP
Serum Electrolyte Na, K, Cl, Blood urea, Serum Creatinine
USG Abdomen and Liver
Echocardiogram
Fasting Blood Sugar (FBS) Oral Glucose Tolerance Test (OGTT), HbA1C
CBC
S. Total IgE, Aspergillus Specific IgE
Request should be made to draw blood and to hand over Room 22 (5th floor ward
block) or serum samples can be hand over (by resident) to a designated technician at
central Pediatric laboratory room 3059 3rd floor teaching block.
Surveillance of sputum if not done
Chest X-ray and other imaging – if indicated only
31
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Treatment
1. Pancreatic Enzyme Replacement Therapy (PERT)
- Start pancreatic enzyme supplement 3000-5000 IU/kg/day of lipase in divided doses
(1000 IU/kg/main meal and 500 IU/kg/snack).
- Enzymes are to be given with meals.
- Full capsule can be swallowed just at the start of meal with adequate water. When
capsule is broken (as difficult to swallow or to use a portion of cap) it can be mixed
with first part of the meal or jam/apple source and consume at first.
- Preferably use cap Creon 10000– The granules can be sprinkled over food/Jam etc.
and can be given as 1/3 – ½ capsule per feed in young infants and 1 –2 capsules per
meal to older children.
- If Creon cannot be given, start enteric coated enzyme tablets with food. If tablet is
given after crushing – make sure that some food is given after the tablet to avoid
ulceration in oral cavity due to digestion of oral mucosa.
- Gradually increase with monitoring of stool frequency, smell, greasy nature of stool,
pain abdomen and weight gain.
- Doses of pancreatic enzymes can be increased by asking the mother about the number
of stools, volume and smell in stool along with complaints of pain abdomen and
weight gain. If stools are bulky/ foul smelling and floats on water, this indicates need
to increase doses of enzyme.
32
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
- The optimal amount of enzymes is when child passes 1 –2 non- foul smelling stools,
child does not complaint of abdominal discomfort and gains weight. Do not exceed
doses beyond lipase dose of 10000 IU/kg/day (Cap Creon 10000 one cap/kg/day)
- If child is taking crushed enzymes, ranitidine or omeprazole can be prescribed to
decrease the gastric pH
- In patient with tube feeds, granules should not be given through tube as it would
block it. Enzymes should be given through oral route and feed can be given through
NG tube.
- Care should be taken in infants to minimize damage to oral mucosa specially in
infants.
Multiple commercial preparations are available. Most common forms of caps contain enteric
coated caps 10,000 IU/cap or 25 000IU/cap in lipase doses.
Trade names of enzyme preparations available: Cap Creon 10000 (enteric coated granules
provides 10000 IU of Lipase per cas)), Tabs Festal-N, Pancreoflat, Panzynorm, Enzar forte
(provides 5-6000 IU of lipase per tabs)
2. Dietary supplements: -
- No dietary restriction. Do not restrict fat in diet. Some parents restrict fat in diet as
they feel clinical symptoms are less with fat free diet, this will compromise child’s
growth.
- Encourage – normal diet
- Supplement – skim milk powder, coconut preparation and
Encourage patients to eat sprouts with food.
33
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Calculation of Daily Energy Requirement (DER)
Calculate BMR in Kilocalories from Expected Body Weight in Kilograms Using WHO equation
Age Range (y) Females Males
0-3 61.0 wt - 51 60.9 wt - 54
3-10 22.5 wt + 499 22.7 wt + 495
10-18 12.2 wt + 746 17.5 wt + 651
18-30 14.7 wt + 496 15.3 wt + 679
Calculate the Daily Energy Expenditure (DEE) by Multiplying the BMR by Activity plus
Disease Coefficients
Activity Coefficient (AC) Disease Coefficient (DC) DEE
Confined to bed: BMR X1.3 FEV1 >80% predicted: 0 BMR X (AC+ 0)
Sedentary: BMR X 1.5 FEV140%-79%predicted:0.2 BMR X (AC + 0.2)
Active: BMR X 1.7 FEV1<40%predicted:0.3 - 0.5 BMR X (AC + 0.3)
Calculate DER from DEE
Degree of steatorrhea If normal stool or minimal or no PI DER = DEE
Consider coefficient of absorption (COA) 0.85 if unknown
If Significant adjust PERT, consider coefficient of absorption clinically
If a stool collection is available to determine the fraction of fat intake take the value
DER = DEE X F, F= 0.93/COA For unknown F= 1.1
Usually DER = 1.1 x DEE
34
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
3. Vitamin supplements
Recommendations for vitamin supplementation
Individual Vitamin Daily Supplementation
Vitamin A (IU) Vitamin E (IU) Vitamin D (IU) Vitamin K (mg)
1-12 months 1500 40-50 400 0.3 – 0.5
1-3 years 5000 80-150 400-800 0.3 – 0.5
4-8 years 5000-10000 100-200 400-800 0.3 – 0.5
>8 years 10000 200-400 400-800 0.3 – 0.5
Available preparations (Compositions of preparations are liable to change)
Vi-Syneral drops each 0.6ml contains Vit A 3000 IU Vitamin D3 400 IU
Calcirol sachet: Vitamin D 60,000IU/ sachet
Shelcal-500 tab CaCO3 1250mg (Ca 500mg) Vit D3 250 IU
Shelcal syrup (5ml) Ca 250mg Vit D3 125IU
Evion drops Vit E 50 mg/ml
Evion caps Vit E 200mg/400mg/600mg
Give Vi-Syneral and Evion drops with meals and PERT 1 ml twice a day.
Shelcal in-between meals.
Calcirol one sachet per month.
Vitamin K – oral preparations are currently not available use IV preparation orally once a week
5mg/week.
35
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
4. Salt supplement: -
Salt and fluid intake should be encouraged specially in summer. Additional salt can be
added to meals and electrolyte drinks are advisable.
During summer children should be prescribed with KCl solutions. Widely available
preparation is Potklor 20meq in 15ml
Usual recommendation is 2-3mmol/kg/day.
As it is difficult to consume, it can be given in 2-3 divided doses. It can be diluted in ½ -
1 glass of water. Lime or sugar can be added to improve palatability.
5. Pulmonary Rehabilitation and Airway Clearance
Most important aspect of respiratory management is airway clearance. This can be
achieved with postural drainage, active cycle of breathing, autogenic drainage and use of
various devices. Simple exercises and other physical activities should be encouraged.
Though it is cumbersome and time consuming child and parents should be praised and
encouraged to do regular physiotherapy.
For young children: postural drainage is used. Parents are trained in technique in different
postural and asked to do it at least twice a day.
Older children breathing exercises can be trained. Devices can be used in older children
who can afford for them.
Usage of multiple technique according personal preferences would improve the
compliance of the therapy.
Send parents along with patient to Physiotherapist for training in techniques of
physiotherapy.
Duration of Physiotherapy
36
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Physiotherapy is continued till child has some secretions in airways indicated by rattling
sound in chest while coughing.
If there is suspicion of gastro-esophageal reflux (GER), postural drainage in head low
positive should be avoided.
Physiotherapy is done before feeds.
6. Azithromycin
There is growing interest in the use of macrolides as immune modulating drugs in cystic
fibrosis. They have been shown to decrease sputum viscoelasticity and airway adhesion
of Pseudomonas aeruginosa.
Azithromycin 5mg/kg/daily is the unit recommendation for all CF children.
7. Inhaled medications
Bronchodilators
If a child gives definite history of wheezing – a trial of bronchodilators should be given
as and when required.
It is used in airways clearing techniques to minimize bronchospasms, bronchodilators are
continued twice a day before chest physiotherapy prior to administration of hypertonic
saline.
Salbutamol is preferred usually with MDI (MDI Salbutamol 100ug 2 puff with spacer)
Nebulization could be an alternative in small children. A combination of salbutamol and
ipratropium can be used as an alternative.
Hypertonic saline
37
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Hypertonic saline (HS) can be used in the short term to induce sputum in patients in who
repeated upper airway cultures are negative and as part of their admission physiotherapy
package in all patients.
Child is given bronchodilators (salbutamol) followed by 3 ml of 3% hypertonic saline by
nebulizer. After 20 – 30 minutes chest physiotherapy should be done. It can be given 2-3
times a day.
DNase (Dornase alfa, Pulmozyme)
DNase is a synthetic enzyme that cleaves neutrophil derived DNA in sputum to reduce
viscosity and thus in theory to aid sputum removal. Studies demonstrate 5-8% overall
improvement in FEV1 but this masks a wide response range from deterioration to marked
improvement (over 20%).
However it is expensive (INR 50,000/month)
This should be decided only after discussion with Prof S K Kabra in carefully selected
patients.
Traditionally given in the afternoon 1 hour before physiotherapy. However a study in
older children and adults showed a modest overall improvement when given at bedtime
(ie, 10-12 hours pre morning physiotherapy) with no nocturnal desaturation, but it can
lead to night time coughing so check in clinic after a month or so. First line timing
remains the afternoon.
Dose - Trade name: Pulmozyme 2.5mg by appropriate compressor and nebulizer
N-Acetyl cysteine
A mucolytic agent is not frequently used in cystic fibrosis as no evidence of beneficial
effects and induction of significant bronchospasm.
38
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Use in special situations with consultants decision.
20% solution 1-2ml in infants, 3-5ml in 1-11 years, 5-10ml in > 12 years (Doubled
amount in 10% solution) via nebulizer or direct instillation to bronchus.
Need bronchodilator therapy before administration and NAC should allow 20-30min for
its action.
Mannitol
Inhaled dry powder mannitol is an osmotic agent that may increase mucociliary clearance
in CF by improving cough clearance and rehydrating the airway surface liquid layer.
Currently dry powder mannitol is packaged in gelatine capsules and delivered via a
specific dry powder inhaler device. The large number of capsules used per dose means
that this is a time-consuming therapy. All patients are pre-treated with bronchodilator 15
minutes prior to administration.
Dry powder mannitol, an emerging therapy, is currently not available in India.
Inhaled steroids
Symptomatic wheezing that requires regular bronchodilators, in a similar regimen to IAP
guidelines for asthma. Especially in atopic children. Ideally acute bronchodilator
reversibility should be documented.
In theory it would seem useful due to the nature of the persistent lung inflammation,
benefit has not been proven. However combination inhalers are used to minimize
inflammation in all patients.
Timing – After physiotherapy
Trade name MDI Foracort 100/6 ug 2 puff bd (with spacer)
39
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
8. Chest exacerbations
A chest exacerbation is a serious adverse event. Around 30% never recover their previous
spirometry, and multiple exacerbations are associated with an accelerated decline in lung
function. A rapid and focused response is essential. If the family is worried they will
usually phone the CF sister or duty mobile. Sometimes telephone advice can be given (by
respiratory registrars or more senior doctors only) but often the patient will need to be
seen. Preferred option is in the next chest clinic (Thursday 2pm) but they may be seen in
the pediatric unit 3 opd (Wed/Sat 9 pm) or pediatric emergency services AIIMS (Ground
floor ward block) in urgent circumstances.
Some indicators of chest exacerbation are:
(i) Increased cough, and in particular a new or increased ‘wet’ cough should always
be taken seriously.
(ii) Increased cough – not responding to bronchodilators
(iii) Adverse changes in sputum production (volume, colour, consistency)
(iv) Haemoptysis.
(v) Increased dyspnoea.
(vi) Chest pain or tightness.
(vii) Malaise, fatigue and lethargy.
(viii) Fever > 38º C. Note that most CF chest exacerbations are not accompanied by
fever. (after excluding other causes of fever)
(ix) Loss of appetite or weight loss.
(x) Tachypnea
40
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
(xi) Adverse changes in chest sounds on auscultation (Bronchial breathing, crackles,
wheeze). However, a clear chest on auscultation does not exclude an infective
exacerbation. Much more sensitive is palpating the chest while the patient coughs
or huffs. New or increased palpable secretions should always be taken seriously.
(xii) First time demonstration of pseudomonas in cough swab.
(xiii) Drop in FEV1 or FVC >10% from previous recording.
If the situation is dealt with over the telephone, it is essential that the CF sister is
informed and appropriate follow up is arranged.
It is important to send (or arrange for local pediatrician or local hospital to send) sputum
or a cough swab to microbiology; a nasopharyngeal aspirate (NPA) may be performed in
infants.
A chest x-ray is only occasionally useful. Should be done in selected situations only.
Antibiotics should be prescribed, initially orally (unless the child is obviously very
unwell); with IV antibiotics given if the child fails to respond.
9. Surveillance respiratory cultures
Cough swab/sputum throat swab after chest physiotherapy should be taken from all
children with CF on each clinic visit (every 12 weeks). The report of organism isolated
and their sensitivity should be attached in the file. (Please send the patient to CF nurse/
research assistant in room no 5 for taking cough swabs and sputum cultures)
If positive culture is found in an asymptomatic child careful decision should be made. If
it is Pseudamonas, it should be treated. Other organisms should be considered individual
basis with discussion with consultant. Patient may be contacted telephonically and decide
accordingly.
41
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
10. Antibiotics
Policies & specific organisms
Some principles
Department of pediatrics AIIMS has its own antibiotic policy with capacity level
of administration.
In pseudomonas infections, two anti-pseudomonas antibiotics should be
administered
In our region, Staph aureus and H. Influenza (Non vaccinated children) may be
common in community acquired pneumonias
Antibiotic pattern could be changed according to antibiogram
Selection of antibiotics will be based on following:
o Previous culture report of sputum/cough swabs.
o Severity of present pulmonary exacerbation
o Chronic colonization
o If previous culture report is available and pulmonary exacerbation is mild,
an ambulatory treatment with oral antibiotics for 10 – 14 days should be
prescribed according to sensitivity.
o If culture report is not available or negative and pulmonary
exacerbation is mild, at most, one general course (amoxicillin,
cephalosporin or co-amoxiclav) may be given for a period of minimum 2
weeks.
o If child has already received a course of general course of antibiotics with
modest or no improvement or with history of recurrent general antibiotic
42
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
course with insignificant improvement with negative/absent culture report
one anti-pseudomonal course (ciprofloxacin +Co-trimoxazole) should be
given before resorting to IV antibiotics. Some children need IV antibiotics
from the start according to clinical picture.
o If Pulmonary exacerbation is severe: Severe exacerbation
Admit the patient and start on intravenous antibiotics. Select antibiotics
according to the previous cough swab reports.
o No previous P aeruginosa - must cover common pathogens including S
aureus, H influenzae, Moraxella catarrhalis as well as possible first isolate
of P aeruginosa (especially young infants).
o If culture is not available, start Cefoperazone Sulbatum (Trade name
magnex) + Amikacin and send sputum /cough swabs for bacterial and
fungal cultures daily.
o Some children may be administered IV antibiotics at their local setting or
other hospital according to availability of bed in the ward, severity of the
disease and feasibility.
o Duration of antibiotics is of minimum 2 weeks, that should be continued
for one week after resolution of symptoms (So if for example, the child is
completely well after the 1st week, then they can stop the antibiotics at 2
weeks. If it takes 2 weeks to become symptom free, the antibiotics can be
stopped at 3 weeks.)
11. When to change antibiotics?
43
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
There is no evidence that in vitro sensitivities correlate with in vivo outcome. Therefore,
if the child is improving on ‘best guess’ antibiotics, but the Pseudomonas comes back
‘resistant’, do NOT change drugs without first discussing with the consultant.
12. Antibiotics when pseudomonas infection is noticed
Antibiotic eradication therapy for initial Pseudomonas aeruginosa(Pa) infection is
standard of care in children with cystic fibrosis (CF)
Anti Pseudamonal antibiotics
Cepholosporin (Ceftazidime, Cefipime, Cefoperazone plus Sulbactam)
Carbapenums (Meropenum, Imipenum)
Monobactams (Aztreonam)
Anti pseudamonal Penicillins (Piperacillin plus Tazobactam, Ticarcillin plus Clavulanate)
Aminoglycosides (Amikacin, Tobramycin)
Quinolones (Ciprofloxacin, Levofloxacin, Ofloxacin)
Polymyxin (Colistin), Trimethoprim and Sulfamethoxazole
First isolation
We will carry out standard eradication
3-4 weeks of dual antibiotics Oral or IV (or dual therapy intravenous antibiotics if
unwell)
Inhaled antibiotics (Tobramycin 300mg 12 h or Colistin 40mg/500000 IU 12 h )
28 days
Repeat culture after 04-06 weeks, if negative usual follow up.
Re-growth during the initial 3 month of eradication
44
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Admit for 2 weeks of IV according to sensitivity pattern (IV antibiotics may be
arranged at local setting)
And either: 3 month’s nebulised tobramycin Or 3 further months of alternating
nebulised colistin / tobramycin.
Subsequent regrowths, Repeated or chronic Isolations
Isolations of P aeruginosa are always treated. We assume this is a new isolate so
attempt re-eradication with 3-4 weeks oral dual therapy or IV dual therapy
according sensitivity pattern.
Long term nebulized antibiotics Tobramycin/colistin/Atreonam (75mg TID)
twice daily for 28 days alternative months for 6 months. If they were on nebulized
antibiotics still when they had the new growth, consider switching to an other
nebulised antibiotics. Aztreonam to be use as alternative or 3rd line therapy
13. Staphylococcus aureus
Though some recognized units use anti staph propylaxis, no evidence for its benefit.
Exacerbations
In a well child (clinical judgment) we use oral co-amoxiclav for 4 weeks.
In ill child – IV antibiotics IV Co-amoxyclav or IV Vancomycin or according to culture
total duration of 4 weeks
Re-growths
Two oral anti-staphylococcal antibiotics for 4 weeks.
Chronic infection
If there are more than 2 isolates of S aureus in a year, give prophylaxis with flucloxacillin
45
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
For those repeatedly culturing Staph aureus despite regular high dose flucloxacillin,
consider other treatments, especially in older children. For example co-amoxiclav, fusidic
acid or even rifampicin if this persists.
14. MRSA
The decision to treat chronic MRSA infection is a clinical one based on signs,
symptoms and investigations.
If treatment is indicated, for 1st isolation in sputum/cough swab, we attempt
eradication as there are evidence showing MRSA adversely effects lung function.
The child should be treated for 3 months with 2 oral agents, usually Trimethprim-
Sulphamethoxazole plus fusidic acid or rifampicin (Should be decided)
Prophylactic flucloxacillin or co-amoxiclav should be stopped in patients with
MRSA until the MRSA is successfully eradicated.
Vancomycin and teicoplanin are IV drugs active against MRSA. Teicoplanin does
not require blood levels and is the preferred choice.
Consider using linezolid, available orally and IV, when traditional agents fail
(consultant decision).
Check current Hospital Policy on MRSA also remember surface decontamination
protocols.
Nebulised vancomycin can also be considered.
15. Haemophilus influenza
H. influ incidence has been reduced with vaccination and as all CF children are on
Azithromycin.
Well child – oral co amoxyclav.
46
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Ill child – IV antibiotics.
16. Burkholderia cepacia complex
Usually isolate in older patients.
Treatment according to sensitivity pattern.
17. Influenza
Viral infection should be suspected with contact history and during epidemics with
compatible historical grounds.
It is indicated to start Oseltamivir (Tamiflu) for suspected influenza, but it is advisable to
send influenza antigen/PCR test.
18. Non-tuberculous mycobacteria (NTM)
Induced sputum sample can be sent to room 2056 for LJ for atypical mycobacteria.
However therapy should be started with establishment of causal relationship only by
consultant.
19. Home IV antibiotics
IV antibiotics could be arranged at local hospital for ill children who need admissions.
Ambulatory or recovering patients antibiotics might be arranged at domestic setting.
20. Allergic bronchopulmonary aspergillosis
(ABPA) is a serious potential cause of lung damage and is not uncommon in CF
(prevalence varies 0.6 - 11%). Early pick-up depends on screening and high clinical
suspicion. There are rare reports of an ABPA-like picture being a complication of other
strains of Aspergillus, and other fungi, such as Scedosporium apiospermum.
ABPA is suspected if there is:
47
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Increased wheezing/chest tightness, particularly if failing to respond to antibiotics
and inhaled medications.
Fever and malaise.
Thick sputum with brown or black bronchial casts.
CF exacerbation not responding to antibiotics.
Older children.
Diagnosis of ABPA: sample for Total IgE, Aspergillus specific IgE, and IgG against
aspergillus is sent to room no. 22, C5 ward or Peds central lab. Hemogram and CXR (CT
chest on case to case basis) done. ABPA diagnosed based on following criteria:
Major Criteria (Both should be there)
1) Total serum IgE > 1000kU/L (>500 may be taken as positive)
2) Aspergillos Specific IgE 0.35kUA/L OR Positive skin prick test for Aspergillous
fumigatus if done.
Minor Criteria (2 out of 3 should be there)
1) Compatible imaging finding
2) Eosinophilia (AEC >500)
3) IgG positivity for Af (>27 mgA/L)
Treatment
Oral Prednisolone 1-2 mg/kg OD daily for 2 weeks, then gradually tail off with
maximum rate of 5mg/2weeks over next 3-6 months.
Antifungal (for 24 weeks): Oral Itraconazole: 5 mg/kg/day; if total less than 200 mg OD,
if >200 mg BD (max 200 mg BD) or Voriconazole*: below 12 yrs of age; 6 mg/kg/dose
(max 200 mg per dose) BD on day 1, then 4 mg/kg/dose (max 100 mg per dose) BD; >
48
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
12 years and weight <40 kg, 200 mg BD on day 1, then 100 mg BD; >12 yrs and > 40 kg,
400 mg BD on day 1, than 200 mg BD.
(*Doses from Hilliard et al. Voriconazole therapy in children with cystic fibrosis. J
Cystic Fibrosis. 2005; 4:215-20.)
21. Hemoptysis
Streaky haemoptysis is common with chronic infection but may indicate deterioration so
sputum should be cultured and a course of antibiotics considered. Haemoptysis must be
differentiated from haemetemesis. The source is usually from areas of chronic airway
inflammation. Massive, profuse haemoptysis due to vessel rupture can be life threatening
(>250 mls/24 hours is the conventional level, but anything more than half a cupful over
24 hours merits assessment. Bad haemoptysis is usually seen in patients with bad lung
function, but has been reported in patients with normal spirometry. The usual site of
bleeding is tortuous bronchial arteries has the possibility of pulmonary embolism.
Adolescents and teenagers may experience a gurgling sensation which is a reliable
lateralising symptom indicating the bleeding site. The patient is likely to be very scared -
reassurance is essential.
Primary management is resuscitation if needed, lay patient on side (gurgling side down),
and give oxygen. Consider stopping hypertonic saline if massive haemoptysis if the HS is
causing more coughing. Physiotherapy may have to be adapted. If the child is taking
NSAIDs, stop them.
Consider following investigations:
Hemogram including platelets count.
Coagulation profile
49
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Arrange cross-match blood.
Sputum culture
CXR (can show new infiltrates but little use in localising the bleeding source).
CT Angiogram of Chest
Initial management -
Give blood and correct coagulation defects if necessary (IV vitamin K/ FFP /
cryoprecipitate).
Start intravenous antibiotics; cover for S aureus as part of the antibiotic regimen,
irrespective of previous culture results.
Continue with gentle regular physiotherapy, but omit chest clapping for 24 hours.
This is essential and contact physiotherapists for advice.
Medical, Selective bronchial angiography and embolization, surgical management
refer guidelines for pulmonary haemorrhage.
22. Pneumothorax
Pneumothorax can be a complication of advanced lung disease. Conservative treatment
might not be adequate because underline lung is unhealthy. Therefore it might often be
complicated with recurrences and Broncho pleural fistula.
Suspect pneumothorax, if there is:
unexpected deterioration,
unexplained chest pain, or
sudden worsening breathlessness.
unequal air entry and increased resonance one side.
50
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
If in doubt, do a CXR but CT scan may be needed to detect it or determine optimal site
for drain placement. The incidence of pneumothorax increases with age (overall 8%) and
is a marker of severe lung disease. It carries a bad prognosis, particularly if the chest
drain cannot be rapidly removed. It is advisable to admit all patient with pneumothorax to
hospital.
A tension pneumothorax is an emergency that requires urgent treatment with a chest
drain, regardless of the CF. A small asymptomatic pneumothorax can be managed by
high flow oxygen and observation. It may resolve but in an already hypoxic patient, such
a leak may cause decompensation.
If the patient is decompensating or has a large pneumothorax, management includes -
Monitor SpO2 and give oxygen (check for CO2 retention).
Intercostal chest drain with local anaesthesia and subsequent oral analgesia.
Antibiotics (IV antibiotics are prudent in all but the most trivial pneumothoraces).
Gentle physiotherapy must be continued, techniques and adjuncts may need
changing (no PEP masks or Positive Pressure Breathing). Deep breathing with
inspiratory holds is encouraged. Please discuss this with the physiotherapist after
discussing with Prof S K Kabra.
Recurrent pneumothoraxes can be managed with medical or surgical pleurodhesis.
However, it should be a conscious decision as it may hamper the feasibility of future
heart lung transplant. (Refer to Protocol of Medical pleurodesis by Povidone iodine)
Broncho pleural fistula could be managed with application of valve, glue or occluder at
the selected bronchi or may consider surgical management.
51
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
23. Oxygen Therapy and Non Invasive Ventilation
Children who have advanced lung disease frequent monitoring of oxygen saturation is
recommended with portable device especially at nights and after moderate physical
activities (portable saturation devices are available at Yusuf Sarai market/several places
in New Delhi with price range of INR 1000 – 2500).
If frequent nocturnal/exercise induced desaturations are documented arterial blood gases
should be done to determine degree of carbon dioxide retention.
If no significant carbon dioxide retention, home oxygen therapy is adequate. Oxygen
concentrator is preferred over oxygen cylinders. It should be discussed with parents and
family in appropriate manner.
Eg 10L Oxygen cylinder (P1V1 = P2V2) assume pressure 150 atm
150 X 10 = 1500 L O2 at 1 atm, if flow rate 2L/min,
it can be used 1500/120 = 12.5 hours.
If significant carbon dioxide retention, NIV (BIPAP) with oxygen supplementation is
advisable. Feasibility, economical capabilities, availability, and disease prognosis should
be discussed among pulmonology team before offering such options.
NIPPV would help to improve ventilation with supporting work of breathing, in addition
it would help to improve mucus clearance by the principle being that positive pressure
gets air ‘behind the sputum’, aiding its clearance.
24. ENT complications
Nasal polyps
Are uncommon in children but may occur in up to 40% of adults with CF.
Uncommon < 5 years and onset is generally between 8-10 years.
52
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Aetiology is uncertain but may be related to infection, allergy, immune factors,
altered secretions and abnormal cilia. There is also an association with chronic
sinus infection.
Usually asymptomatic.
Can result in chronic nasal obstruction, which increases airway resistance and
may lead to mouth-breathing and obstructive sleep apnoea syndrome. It can also
cause headaches and impair smell and taste.
Diagnosis is made by simply looking up the nose with a light but sometimes it is
difficult to differentiate polyps from inflamed turbinates.
If troublesome:
o Initial treatment is usually a steroid nasal spray such as mometasone (Meta
spray).
o Anti-histamines are of limited value
o If unsuccessful, surgery should be considered, but due to the high
recurrence rate (60-90%), multiple procedures may be necessary.
o Refer to ENT unit.
Sinusitis
Although almost all children with CF have chronic paranasal sinus retention of
secretions and mucosal inflammation, only 1% are symptomatic.
Chronic sinusitis is commonly associated with nasal polyposis.
Sinusitis may cause headaches, which are persistent and localised. Other
symptoms are related to chronic nasal obstruction (mouth-breathing, snoring, loss
53
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
of sense of smell and taste) and purulent drainage (postnasal drip, cacosmia – foul
smells in the nose, constant throat-clearing, halitosis).
X-ray of the sinuses can be done but it might have limited value.
Nasal swabs should be done as a wide spectrum of bacteria may be involved.
Long-term oral antibiotics for 3-6 weeks
ENT interventions may be required in complicated and refractory patients.
25. GI Complications
DIOS (Distal Intestinal Obstructive Syndrome)
Distal Intestinal Obstructive Syndrome (DIOS) is a common complication in CF
(paediatric lifetime prevalence of ~8%). The incidence varies widely but it mostly affects
those with pancreatic insufficiency. The pathophysiology is not fully understood, but
there are often multiple contributory factors including
Severe genotype
Pancreatic insufficiency
Inadequate salt intake
Dehydration
Poorly controlled fat malabsorption
History of meconium ileus or DIOS
Post organ transplantation
Viscid muco-faeculent material accumulates in the terminal ileum / caecum leading to
partial obstruction with pain usually in the right lower quadrant, abdominal fullness and a
palpable mass in the right iliac fossa.
54
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Suspect DIOS if there is:
Acute periumbilical or right lower quadrant abdominal pain
Vomiting
Abdominal fullness
Palpable mass in right lower quadrant
Consider other D/Ds of similar presentation: Constipation, UTI, Pancreatitis,
Intussusception, cholangitis etc.
A plain abdominal x-ray (AXR) is usually all that is necessary to diagnose DIOS
or constipation. Intestinal fluid levels and iliocaecal mass suggest DIOS.
Serum Electrolyte with VBG is helpful specially in situation with dehadration
Other investigations according to suspected D/Ds
Management of DIOS
Rehydration
Gastrografin enemas - well hydrate before, during and post treatment, as
gastrografin is highly osmotic. This is often done as an in-patient,
especially in the more severe cases IV fluids may be required. The
suggested fluids below are the minimum. Be particularly careful in babies
& infants who can easily become dehydrated.
Polyethylene glycol
Laxatives(Lactulose) – post treatment
Avoid dehydration electrolyte imbalances
Surgical management if everything failed only.
Constipation
55
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
If severe should be considered as part of DIOS spectrum. However beware
increasing enzyme doses when all that is needed is simple constipation
treatment. Main differential from DIOS is that constipation tends to be
limited to rectum.
Treatment:
Ensure adequate fluid intake.
Lactulose
26. Liver Disease
Palpation of an enlarged liver and/or spleen.
Routine annual assessment ultrasound on alternate years from aged 5 years and
above. It will be repeated in 1 year if abnormal.
Liver function tests (transaminases) have a poor sensitivity and specificity.
Prolonged prothrombin time (although more likely to be due to malabsorption of
vitamin K than liver disease).
Ursodeoxycholic acid (increases bile flow): 10-15 mg/kg bd
Vitamin K
Splenomegaly could be due to portal hypertension, Pediatric Gastro Team should be
consulted in relevant patients.
27. CF related diabetes (CFRD)
When to suspect
Poor weight gain without indefinable cause
Polyuria, polydipsia
RBS > 7.8 mmol/L (140 mg/dl)
56
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
HbA1C > 6.5%
Oral glucose tolerance test (OGTT)
How it works - Glucose levels are measured before and after a standard oral glucose load.
Preparation
The child is fasted from midnight although drinks of plain water are allowed.
Dose of glucose
1.75 g/kg glucose to a maximum of 75 g, as glucose monohydrate diluted in water
(200-300 mls).
Samples
- Take blood for glucose at 0 mins (fasting) and give the glucose drink.
- Take blood for glucose at 60 and 120 minutes.
WHO criteria for diabetes and prediabetes
Diabetes- any of these
Fasting glucose ≥7.0 mmol/L (126 mg/dl)
Two-hour post glucose challenge value ≥11.1 mmol/L (200 mg/dl).
HbA1C value of ≥6.5% (48 mmol/mol) can be used as a diagnostic test for
diabetes. (A value of <6.5% does not exclude diabetes).
Impaired glucose tolerance (IGT)
Fasting glucose <7.0 mmol/L (126 mg/dl) and a two-hour glucose post glucose
challenge of ≥7.8 mmol/L (140) but <11.1 mmol/L (200 mg/dl)
Impaired fasting glucose (IFG)
Fasting glucose of 6.1 - 6.9 mmol/L (110-124)
57
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Individuals with CF who have diabetes or impaired glucose tolerance have worse
pulmonary outcomes.
The primary cause of the abnormal glucose tolerance in CF is insulin deficiency so the
treatment for this is insulin. Insulin has been shown to improve lung function and
nutritional status in CF.
Pediatric Endocrinology team should be consulted to start treatment.
58
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Non-cystic fibrosis
Bronchiectasis
59
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Non-cystic fibrosis Bronchiectasis
When to suspect Bronchiectasis?
Children presenting with one or more of the following clinical features should be further
evaluated to assess the possibility of a bronchiectasis (suppurative lung disease).
1. Persistent productive or moist cough almost daily for 8 weeks without periods of
complete remission (Persistent symptoms in between viral colds in young children).
2. Asthma does not respond to appropriate treatment with good compliance or atypical
presentations.
3. Prolonged acute cough (>3 weeks) with worsening symptoms (becoming more intense
and frequent).
4. Pertussis like illness does not resolve even after 6 months.
5. Following an episode of severe pneumonia; incomplete resolution of symptoms, physical
signs or radiological changes.
6. Recurrent pneumonia (two episodes within 12 months or more than two in any time –
localized or multifocal).
7. Chest deformity, finger clubbing or persistent crepitations in the chest without obvious
explanation.
8. Unexplained chest imaging findings or persistent abnormalities more than 12 weeks
following the initial illness.
9. Recurrent respiratory symptoms in children with gastro-esophageal reflux disease,
swallowing problems, or upper airway abnormalities
60
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
10. A positive sputum/other respiratory sample culture for an unusual organism in a child
with chronic respiratory symptoms (Staphylococcus aureus, Haemophilus influenzae,
Pseudomonas aeruginosa, non-tuberculous mycobacteria)
11. Unexplained hemoptysis
Confirm if Bronchiectasis is suspected:
A baseline CXR should be done in all children (if not done already) with clinical suspicion
of a suppurative lung disease.
Chest XR findings- prominent bronchovascular markings, dilated bronchi, loss of lung volume,
peribronchial thickening (Apparently normal CXR does not rule out bronchiectasis)
HRCT of chest should be done to confirm the diagnosis of bronchiectasis if clinical features
and CXR are strongly suggestive of a suppurative lung disease.
HRCT findings of bronchiectasis:
1. Diameter of a bronchus is more than the diameter of adjacent pulmonary artery in axial
section (signet ring appearance)
2. Bronchial wall thickening (the internal diameter of the bronchus is <80% of the external
diameter)
3. Lack of normal tapering of bronchi towards the periphery of lung, producing a tramline
or flared appearance.
4. Bronchi seen at the most peripheral part of lungs
HRCT also useful to categorise bronchiectasis into cylindrical, varicose or cystic.
Bronchiectasis, diagnosed with positive imaging findings, in a child with clinical features
support the diagnosis of a suppurative lung disease.
61
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Aetiology of non-CF suppurative lung diseases:
Underlying causes can be identified in about 2/3 rd of cases
1. Post infectious- commonest cause (about 25-35% of identified cases) - Following severe
pneumonia, Measles, Pertussis, Tuberculosis, Stevens Johnson Syndrome (SJS).
2. Primary ciliary dyskinesia (PCD)
3. Immune deficiency disorders- primary or acquired
4. ABPA
5. Aspiration syndromes
6. Airway obstruction- Foreign body aspiration, Intra or extra luminal compression due to
lymph node, tumour mass, cysts, vascular ring
7. Congenital malformations- Pulmonary sequestration and airway malformations-
Laryngo-tracheo-bronchomalacia, Tracheo-esophageal fistula, laryngeal cleft, congenital
cartilage abnormalities
Children with clinical and radiological features of chronic suppurative lung disease should be
further evaluated to identify a possible underlying aetiology.
It is important to exclude cystic fibrosis (CF) first, because the management protocol and
prognosis are different despite some similarities in clinical features.
Clinical features which point towards a specific aetiology.
1. CF: Apart from recurrent or persistent respiratory symptoms; a family history, features of
malabsorption (frequent, bulky, foul smelling and oily stools), history of meconium ileus,
failure to thrive.
62
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
2. PCD: Daily wet cough since early childhood, history of neonatal respiratory distress
particularly in a term baby, chronic ear problem (glue ear, serous otitis media, ear
perforation) or hearing defect, persistent rhinitis, congenital heart defect, situs
abnormality (situs inversus or heterotaxy)
3. Immunodeficiency disorder: recurrent documented pneumonia, ear infections, skin
rashes, recurrent abscess formation, oral thrush, multisite infections.
4. Aspiration syndromes: cough and/or choking with feeds/meals, recurrent vomiting or
regurgitations, underlying neurological diseases leading to aspirations.
5. Forgotten foreign body: history of foreign body aspirations, sudden onset of symptoms
(coughing, chocking, respiratory distress) followed by persistent respiratory symptoms.
6. ABPA: History of asthma, recurrent or persistent symptoms despite adequate treatment
and good compliance
7. Past history of tuberculosis, measles, pertussis and Stevens Johnson Syndrome (SJS):
sequel of corresponding disease.
Investigations for etiology of bronchiectasis:
Investigations are planned according to clinical clues to establish a possible aetiology and assess
the severity and complications.
1. Sweat chloride test-
To exclude cystic fibrosis: Take an appointment from CF nurse at pediatric OPD daily 9.00am-
1.00pm. Test is done at Room: 3067, IIIrd floor, Teaching block on Mondays and Wednesdays at
2.00 pm.
63
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
If 2 values of sweat chloride > 60 mmol/L (done at least one week apart with sweat
weight >100 mg): Diagnosis of CF is made and CF management protocol should be
followed.
If sweat chloride <40 mmol/L: managed as Non-CF suppurative lung diseases.
IF sweat chloride values between 40 – 60 mmol/L: Follow-up as suspected CF and repeat
sweat test and further investigations including mutation analysis are done according to
the clinical features and course of the illness.
2. Nasal and exhale Nitric Oxide levels-
Screening test for PCD in suspected cases.
Done at room: D of pediatric OPD in Wednesdays and Saturdays at 9.00 am and Thursdays at
2.00 pm.
Nasal NO value <70 ppb and FENO value <15ppb are strongly suggestive of PCD in
appropriate clinical background but does not confirm the diagnosis.
3. Nasal scrapings for electron microscopic studies-
Confirmatory test for PCD. Done if nasal NO assessment suggest PCD.
4. Serum Immunoglobulin levels and lymphocytes subsets in children with suspected primary
immunodeficiency disorders.
5. For suspected cases of ABPA: Serum total IgE levels and Aspergillus fumigatus specific IgE
levels:
Done at central pediatric lab and samples are collected at Room:22, 5th floor, Ward block.
6. Bronchoscopy-
Identify suspected structural airway abnormalities and foreign bodies.
Indicated if there are clinical and/or radiological evidence of localized bronchiectasis.
64
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Sometimes done to obtain BAL samples for microbiological testing if clinically indicated.
7. Sputum/throat swabs for bacterial and if necessary fungal cultures. Sputum/Gastric
aspirates for AFB, MGIT culture and GeneXpert in cases suspected of post TB bronchiectasis to
exclude the active disease and/or drug resistance.
8. Pulmonary function tests-
Spirometry in children older than 5 years.
Done at the time of diagnosis and then regularly (3-6 months) in follow up visits. Bronchodilator
reversibility is also done initially to assess the possible reversible airway disease.
9. ANA-ANCA: If post ILD traction bronchiectasis is suspected based on history and imaging
findings.
Management:
Break and limit the cycle of infection and inflammation
Goals of therapy-
1. Improve Quality of life
2. Reduce the frequency and severity of exacerbations
3. Prevent further complications
4. Preserve lung function.
5. Facilitate normal growth and development
Management strategies:
1. General measures:
Maintaining good hydration
Adequate nutrition,
65
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Immunization against common respiratory pathogens- Up to date vaccination for
pertussis, measles, pneumococcal, H. influenzae type b and annual influenza (if parents
affording and willing) vaccinations.
Protection against possible exacerbating factors - smoke (biomass burning, tobacco) and
irritants.
2. Airway clearance techniques-
Following sequence is followed. The available evidence regarding the type of mucolytic agent
and most appropriate airway clearance technique is still inconclusive.
i) MDI salbutamol (100µg)/ 2 puffs with a spacer (to facilitate mobilization of mucous and
prevent possible bronchospasms induced by hypertonic saline)
ii) Nebulization with 3% saline 3 ml
iii) Chest physiotherapy
Done by child alone- Active cycle of breathing techniques and Autogenic drainage (for
older children)
Done by the care giver manually - Chest percussion, Chest wall vibrations, Modified
postural drainage
Use of devices: Positive expiratory pressure (PED device) or Oscillating positive
expiratory pressure (Flutter, Acapella)
A combination of these methods would be ideal
Done twice daily about 20-30 min per session before meals, in symptomatic children.
Frequency may be increased according to the disease severity and exacerbations.
If parents can’t afford nebulization, only chest physiotherapy is advised.
66
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
3. Inhaled corticosteroids:
Used if there associated wheezing.
MDI- Foracort 100µg/ 2 puffs/ BD with a spacer after completion of chest physiotherapy.
4. Antibiotics:
Indicated if there is evidence of pulmonary exacerbations. Clues are fever without other
reason, increased expectoration (frequency, amount and purulent), weight loss, decrease in
FEV1.
Choice of antibiotics depends on sputum culture if available. Otherwise used empirically -
For children with mild to moderate exacerbations who do not require admission can use oral
amoxicillin or Co-amoxyclav (ciprofloxacin if Psedomonas positive in recent cultures) for
10-14 days.
Children with frequent or severe (requiring hospitalization) are started on septran prophylaxis
irrespective of their immune status.
Long term inhaled antibiotics- No evidence to support the routine use and it is not used.
5. Long-term oral macrolides:
No strong evidence to support the routine use for all children as in cystic fibrosis.
Not used currently for non-CF bronchiectasis.
6. Management of underling disease:
Children with GERD- use general measures and proton pump inhibitors.
Children with immunodeficiency disorders- use prophylactic Co-trimoxazole and
Itraconazole
Children with hypogammaglobulinemia use regular intravenous immunoglobulin once in
3-4 week.
67
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
7. Surgical management:
Poorly controlled localized diseases following adequate medical management and children with
recurrent hemoptysis poorly responding or not amenable to interventional radiological
management are referred for lobectomy or rarely pneumonectomy.
Follow up:
Diagnosed children are followed up in 3-6 months intervals (more frequently depending on the
severity) at Pediatric Chest Clinic (Thursday 2.00pm).
Every visit send the child and parents/care givers to physiotherapist to review the
technique and compliance of airway clearance.
Assess the inhaler technique and PEFR if on inhaler steroids.
Assess the symptoms of cough, degree of sputum production, weight gain, number of
exacerbations since last visit, how disease affected child’s physical activities and
schooling.
Assess and promote the avoidance of exposure to exacerbating factors like tobacco
smoke and other air pollutants.
Document the Oxygen saturation in room air with Oxymetry.
Arrange spirometry once in 3-6 months.
Arrange sputum/throat swab for cultures in symptomatic children or children with
previous positive cultures in regular intervals (6-12 weeks)
Review and complete the work up for underlying aetiology
Educate the parents/care givers regarding the nature of the disease.
Identify possible exacerbations and treat accordingly.
68
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Allergic bronchopulmonary
aspergillosis (ABPA)
69
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Allergic bronchopulmonary aspergillosis (ABPA)
Allergic bronchopulmonary aspergillosis (ABPA) is an immunological pulmonary disorder
caused by hypersensitivity to Aspergillus fumigatus, manifesting with poorly controlled
asthma, recurrent pulmonary infiltrates and bronchiectasis. Table 1 shows spectrum of allergic
disorders associated with Aspergillus.
The prevalence of ABPA is believed to be about 1 to 2% in patients with asthma and 2 to 15% in
patients with cystic fibrosis (CF).
Predisposing conditions for ABPA:
Asthma
Cystic fibrosis
COPD
Non CF Bronchiectasis- Post tubercular bonchiectasis
Immunodeficiency- HIV
Table 1. Spectrum of allergic disorders associated with Aspergillus
1. Aspergillus sensitization (AS) Presence of immediate cutaneous
hypersensitivity (or elevated IgE levels)
against antigens of A. fumigatus
2. Allergic bronchopulmonary Hypersensitivity to Aspergillus fumigatus in
aspergillosis (ABPA) patients with asthma and cystic fibrosis
(CF) with total IgE values> 1000 IU/ml,
radiological findings of recurrent pulmonary
70
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
infiltrates with or without bronchiectasis
and mucus plugging
3. Allergic bronchopulmonary mycosis ABPA like syndrome caused by fungi other
(ABPM) than A. fumigatus
4. Severe asthma with fungal Characterized by the presence of severe
sensitization (SAFS) asthma and fungal sensitization akin to
ABPA, but without bronchiectasis and
mucus plugging, and total IgE values <
1000 IU/mL
When to suspect ABPA?
Underlying asthma: poorly controlled asthma, wheezing, hemoptysis, productive cough,
expectoration of brownish black mucus plugs.
Underlying cystic fibrosis: wheezing, fever, malaise and thick sputum with brown or black
mucus plugs or casts, no clinical response to conventional nebulised or intravenous antibiotic
therapy.
Approach to diagnosis:
History: Symptoms suggestive of underlying asthma/atopy and cystic fibrosis, low grade fever,
weight loss, malaise, fatigue, uncontrolled asthma, wheezing, productive cough, expectoration of
brownish black mucus plugs, hemoptysis.
Examination: cyanosis, digital clubbing (depending upon severity and chronicity of disease),
wheeze, crepts, bronchial breathing, Loud P2 (in case of associated pulmonary hypertension) or
features of cor pulmonale.
71
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Investigations: consider following tests if ABPA is suspected:
1. Complete hemogram with peripheral smear examination for eosinophilia
2. Serum Total IgE levels
3. Aspergillus specific IgE and IgG levels
4. Skin prick test for Immediate cutaneous hypersensitivity to Aspergillus (if available)
5. Chest X Ray- Findings of transient of fleeting pulmonary opacities, tramline opacities,
toothpaste shadows, finger in glove opacities, consolidation, mass like opacities
6. HRCT Chest- Findings of Central bronchiectasis, parallel-line opacities extending to the
periphery, bronchoceles, high attenuation mucous plugs
7. 2 D echocardiography (if clinical features of pulmonary hypertension)
8. To determine the underlying cause: Spirometry with bronchodilator reversibility test,
Sweat chloride test
Diagnose ABPA if criteria for ABPA are fulfilled as shown in Table 2: Clinical and
radiological staging is shown in Table 3 and 4 respectively.
Table 2. Diagnostic criteria of ABPA
Predisposing conditions Bronchial asthma, cystic fibrosis chronic obstructive
pulmonary disease, post-tuberculous fibrocavitary
disease
Essential criteria (both should be Serum Aspergillus fumigatus-specific IgE levels >0.35
present) kUA/L or positive skin prick test†
Elevated serum total IgE levels > 1000 IU/ml*
Other criteria (at least two of Serum Aspergillus fumigatus-specific IgG levels >27
three) mgA/L
Thoracic imaging findings consistent with ABPA#
72
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Peripheral blood eosinophil count >500 cells/μL
(may be historical)
* An IgE value <1000 IU/mL may be acceptable, if all other criteria are met (especially if the serum
Aspergillus fumigatus-specific IgG levels >27 mgA/L)
# Features on HRCT chest and/or chest radiograph consistent with ABPA include transient abnormalities
(i.e. nodules, consolidation, mucoid impaction, hyperattenuating mucus, fleeting opacities,
toothpaste/gloved finger opacities, tram-track opacities) or permanent (i.e. parallel lines, ring shadows,
bronchiectasis and pleuropulmonary fibrosis).
† A positive type I Aspergillus skin test may be considered as a criterion in the place of serum
Aspergillus fumigatus-specific IgE levels only if the latter test is not available.
Table 3. Clinical staging of ABPA in asthma
Stage Definition Features
0 Asymptomatic No previous diagnosis of ABPA
Controlled asthma (according to GINA/EPR-3 guidelines)
Fulfilling the diagnostic criteria of ABPA
1 Acute No previous diagnosis of ABPA
Uncontrolled asthma/symptoms consistent with ABPA
Meeting the diagnostic criteria of ABPA
1a with mucoid Mucoid impaction observed on chest imaging or
impaction bronchoscopy
1b without mucoid Absence of mucoid impaction on chest imaging or
impaction bronchoscopy
2 Response Clinical and/or radiological improvement AND
Decline in IgE by ≥25% of baseline at 8 weeks
3 Exacerbation Clinical and/or radiological worsening AND
Increase in IgE by ≥50% from the baseline established
during response/remission
73
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
4 Remission Sustained clinico-radiological improvement AND
IgE levels persisting at or below baseline (or increase by
<50%) for ≥6 months off treatment
5 5a: Treatment ≥2 exacerbations within 6 months of stopping therapy OR
dependent Worsening of clinical and/or radiological condition, along
ABPA with immunological worsening (rise in IgE levels) on
tapering oral steroids/azoles
5b: Systemic glucocorticoids required for control of asthma
Glucocorticoid while the ABPA activity is controlled (as indicated by IgE
dependent levels and thoracic imaging)
asthma
6 Advanced ABPA Extensive bronchiectasis due to ABPA on chest imaging
AND
Complications (cor pulmonale and/or chronic type II
respiratory failure)
Table 4. Radiological staging of ABPA
Classification Features
ABPA-S (Serological ABPA) All the diagnostic features of ABPA (Table 2) but no
abnormality resulting from ABPA on HRCT chest
ABPA-B (ABPA with All the diagnostic features of ABPA including
bronchiectasis) bronchiectasis on HRCT chest
ABPA-HAM (ABPA with high All the diagnostic features of ABPA including
attenuation mucus) presence of high-attenuation mucus
ABPA-CPF (ABPA with chronic ABPA with at least two to three other radiological
pleuropulmonary fibrosis) features such as pulmonary fibrosis, parenchymal
scarring, fibro-cavitary lesions, aspergilloma and
pleural thickening without presence of mucoid
impaction or high-attenuation mucus
74
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Management:
It consists of:
1. Anti-inflammatory therapy (systemic corticosteroids)- to suppress the immune activity
2. Antifungal agents- to reduce the fungal load in the airways
3. Environmental control
Treatment is started with oral steroids and antifungal (usually Itraconazole). See Figure 2 and
Table 5. Steroids are used for 3-4 months and itraconazole for 6 months. Exacerbation after
stopping the therapy is treated similarly.
Table 5: Drugs along with doses used for ABPA management
Drugs Doses Comments
Oral steroids Low dose steroids- Prednisolone 0.5 Low dose steroids preferred
mg/kg/day for 1–2 weeks, then on alternate because of less side effects
days for 6–8 weeks. Then taper by 5–10 mg
every 2 weeks and discontinue (Total
duration 3-4 months)
High-dose glucocorticoids: Prednisolone,
0.75 mg/kg for 6 weeks, 0.5 mg/kg for 6
weeks, then tapered by 5 mg every 6 weeks
to continue for a total duration of at least 6–
12 months.
Oral Itraconazole 5mg/kg/day to a maximum of 400mg/day Monotherapy not indicated
for at least 24 weeks, usually given once To be used in combination
daily if dose is < 200mg/day. If the once with steroids
daily dose exceeds 200mg/day, a twice Risk of resistance with long
daily regimen should be followed. term therapy
Cross resistance to other
azoles may occur
75
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Oral Voriconazole* below 12 yrs of age; 6 mg/kg/dose (max
200 mg per dose) BD on day 1, then 4
mg/kg/dose (max 100 mg per dose) BD; >
12 years and weight <40 kg, 200 mg BD on
day 1, then 100 mg BD; >12 yrs and > 40
kg, 400 mg BD on day 1, than 200 mg BD.
Nebulized Amphotericin B deoxycholate Indicate in side effects or
Amphotericin B Daily: 5-40 mg twice daily intolerance to azole or
Intermittent: 20 mg (10 mg twice daily) resistance to azole antifungal
thrice weekly agents
Liposomal amphotericin B
Intermittent: 25 mg twice weekly
Amphotericin B lipid complex
Intermittent: 50 mg twice weekly
Intravenous 10-30 mg/kg/day for 3 days every 3-4 Indicated in steroid
Methylprednisolone weeks dependent ABPA and as
steroid sparing agent
Omalizumab See figure 3 for doses. Available (Xolair) Indicated in recurrent
150 mg vial in 1.2 ml. Use only 150 mg at exacerbations or treatment-
one injection site. dependent ABPA
*Doses from Hilliard et al. Voriconazole therapy in children with cystic fibrosis. J Cystic Fibrosis.
2005; 4:215-20.
76
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Figure 3: Doses of Omalizumab (Reference:
https://www.gene.com/download/pdf/xolair_prescribing.pdf)
Monitoring:
1. History and physical examination, chest radiograph, total IgE levels and spirometry every
8-12 weeks till clinic-radiological improvement and demonstration of >25% decline in
IgE levels.
2. Total serum IgE levels at every 3 to 6 months after remission.
3. Chest radiograph even in an asymptomatic patient if IgE level doubles.
4. Spirometry should be obtained at least 3 to 6 monthly. An unexpected decline of 15% in
functional vital capacity (FVC) might be an indication of ABPA exacerbation.
77
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
5. Monitor for side effects of:
Prolonged corticosteroid therapy- Cushingoid features, B.P., RBS, DEXA scan,
Adrenal suppression
Prolonged Itraconazole therapy- LFTs
6. Explore the possibility of mould exposure in the patient’s environment, especially for
refractory cases.
Patients with Asthma or Cystic fibrosis fulfilling the diagnostic criteria of ABPA
ABPA Stage 1 (Acute) or Stage 3 (Exacerbation)
Start treatment with oral steroids (preferably low dose as above) and
oral Itraconazole (5 mg/kg/day. Max 400 mg/day) for 6 months
Response (Stage 2) No Response or Treatment
dependent (Stage 5)
Follow-up: clinically, chest
radiograph, spirometry, IgE consider voriconazole or nebulized
levels (total) every 8-12 weeks Ampho B, continue low-dose
glucocorticoids; If still not controlled:
Omalizumab
Remission (Stage 4)
Fig 2. Approach to treatment of ABPA
78
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Childhood interstitial lung
disease (ChILD)
79
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Childhood interstitial lung disease
The spectrum of interstitial lung disease (ILD) includes a large, heterogeneous group of mostly
rare pulmonary disorders characterized by abnormalities of the distal lung units and disordered
gas exchange. Because many of the included disorders extend beyond or do not even involve the
interstitium, ILD in children (chILD) is considered a syndrome of diffuse and interstitial lung
disease. Childhood ILDs are different from adult disease in various aspects in being rare and
wider spectrum as compared to that in adults.
Classification:
chILD Research Network has given the new classification scheme for childhood ILDs (Box 1).
When to suspect ILD?
A child with diffuse lung disease (DLD) is suspected to have ILD if he fulfils the criteria for
chILD syndrome that prompts further diagnostic evaluation. The chILD syndrome is defined
when a child with DLD has the common causes of DLD excluded as the primary diagnosis and
has at least three of the following four criteria:
(1) respiratory symptoms (e.g., cough, rapid and/or difficult breathing, or exercise intolerance);
(2) respiratory signs (e.g., resting tachypnea, adventitious sounds, retractions, digital clubbing,
failure to thrive, or respiratory failure);
(3) hypoxemia;
(4) diffuse abnormalities on CXR or a CT scan.
The chILD syndrome requires exclusion of more common causes of DLD like cystic fibrosis,
congenital or acquired immunodeficiency, congenital heart disease, bronchopulmonary
dysplasia, pulmonary infection, primary ciliary dyskinesia presenting with new born respiratory
distress, and recurrent aspiration.
80
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Box 1: Classification of ChILD (Source: Am J Respir Crit Care Med Vol 188, Iss. 3, pp 376–394, Aug 1, 2013)
I. Disorders more prevalent in infancy II. Disorders not specific to infancy
A. Diffuse developmental disorders A. Disorders of the normal host
1. Acinar dysplasia 1. Infectious and postinfectious processes
2. Congenital alveolar dysplasia 2. Disorders related to environmental
3. Alveolar–capillary dysplasia with pulmonary agents: hypersensitivity pneumonia,
vein misalignment toxic inhalation.
3. Aspiration syndromes
B. Growth abnormalities 4. Eosinophilic pneumonia
1. Pulmonary hypoplasia
2. Chronic neonatal lung disease B. Disorders related to systemic disease
a) Prematurity-related chronic lung disease processes
(bronchopulmonary dysplasia) 1. Immune-related disorders
b) Acquired chronic lung disease in term 2. Storage disease
infants 3. Sarcoidosis
3. Structural pulmonary changes with 4. Langerhans cell histiocytosis
chromosomal abnormalities 5. Malignant infiltrates
a) Trisomy 21
b) Others C. Disorders of the immunocompromised
4. Associated with congenital heart disease in host
chromosomally normal Children 1. Opportunistic infection
2. Disorders related to therapeutic
C. Specific conditions of undefined etiology intervention
1. Pulmonary interstitial glycogenosis 3. Disorders related to transplantation and
2. Neuroendocrine cell hyperplasia of infancy rejection syndromes
4. Diffuse alveolar damage of unknown
D. Surfactant dysfunction mutations and related etiology
disorders
1. SPFTB genetic mutations—PAP and variant D. Disorders masquerading as interstitial
dominant histologic pattern disease
2. SPFTC genetic mutations—CPI dominant 1. Arterial hypertensive vasculopathy
histologic pattern; also DIP and NSIP 2. Congestive vasculopathy, including
3. ABCA3 genetic mutations—PAP variant veno-occlusive disease
dominant pattern; also CPI, DIP, NSIP 3. Lymphatic disorders
4. Others with histology consistent with 4. Congestive changes related to cardiac
surfactant dysfunction disorder without a yet dysfunction
recognized genetic disorder
III. Unclassified—includes end-stage
disease, nondiagnostic biopsies, and those
with inadequate material
81
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Approach to diagnosis:
Once the child fulfils chILD criteria, further diagnostic evaluation should be done in order to
specify the exact diagnosis as it has management and prognostic implications.
The diagnostic approach is based on the age of the patient, severity and progression of the
disease and family history of ILD and early infant deaths.
Step 1: Identifying the Diffuse lung disease
1. Detailed history and physical examination
2. Chest X Ray
3. HRCT/CECT Chest
Step 2: Exclusion of common causes of Diffuse lung disease (depending upon the likely
cause based on history and examination)
1. Complete hemogram- Clues for infection, immunodeficiency
2. 2 D Echocardiography (to rule out cardiovascular cause of DLD, Pulmonary hypertension)
3. Upper GI contrast studies, GER scan, 24 hour pH study
4. Sweat chloride test
5. Nasal NO
6. HIV serology
7. Immunoglobulin profile, T, B cell markers, Dihydrorhodamine test
8. CECT/HRCT chest (If not done before)
Step 3: Evaluation of specific chILD diagnosis
According to the age of presentation, this step can be divided into children less than 2 years and
those more than 2 years.
82
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
a) Children less than 2 years:
1. Thin section CT Chest (Preferably Controlled ventilation HRCT or Conventional HRCT
Chest)
2. Infant Pulmonary function tests
3. Bronchoscopy with bronchoalveolar lavage (PAS positive material, Bombesin staining)
4. Lung biopsy (Using VATS or open thoracotomy)
5. Genetic testing (for children suspected with surfactant dysfunction mutation disorders)
b) Children more than 2 years (investigations can be narrowed down based on history
and examination):
1. Urine R/M
2. ANA (dsDNA if ANA is positive), ANCA
3. Urine Calcium: creatinine ratio
4. Serum ACE levels
5. Thin section CT Chest
6. Pulmonary function tests
7. Bronchoscopy with bronchoalveolar lavage (Cellular morphology, CD4:CD8 ratio, PAS
positive material)
8. Serum precipitins to the likely antigen (for hypersensitivity pneumonitis)
9. Lung biopsy (Using VATS or open thoracotomy)
10. Genetic testing (for children suspected with surfactant dysfunction mutation disorders)
83
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Treatment (See Figure 1)
For moderate to severe disease, start oral steroids at dose of 1-2 mg/kg/day followed by
tapering doses till alternate day regime. For very severe disease, initial treatment should
be pulsed methyprednisolone at 30 mg/kg/day for 3 consecutive days for at least 3
monthly cycles. When the disease is under control, oral pednisolone in alternate day
regime is given.
Hydroxychloroquine is used as steroid sparing agent in the dose of 6-10 mg/kg/day. In
severe cases, Hydroxychloroquine started in beginning along with steroids. In case of
ineffective response to steroids and Hydroxychloroquine, other agents such as
azathioprine (2–3 mg/kg/day, maximum dose 150 mg/day), cyclophosphamide (1-1.5
mg/kg/day) OR cyclosporine (4 mg/kg/day in two divided doses) may be used.
Specific treatment strategies for certain type of ILD:
(1) Pulmonary alveolar proteinosis: Whole lung lavage,
(2) Pulmonary haemangiomatosis interferon–γ,
(3) cytomegalovirus: Ganciclovir
(4) Wegener’s granulomatosis: pulsed cyclophosphamide.
(5) Sarcoidosis: refer to Sarcoidosis protocol.
(6) Hypersensitivity pneumonitis: Avoidance of involved trigger.
Adjuvant therapies:
1. If there associated pulmonary arterial hypertension: Diuretics and sildenafil.
2. Oxygen therapy is used in case of hypoxia (SpO2 <92% at room air).
3. Aggressive treatment of pulmonary infections.
4. Good nutrition.
84
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
5. Immunizations against pneumococcus, influenza and hemophilius, if parents
can afford.
If child is in Acute exacerbation: Start steroids -oral prednisolone 0.5mg/kg/day for 2 weeks
and as the symptoms improved slowly taper steroid (2.5mg/week and reduced to 5-7.5mg
alternate day depending on symptoms. Follow these paitients 3 monthly. Do not stop steroids
abruptly, these patient required to be on low dose steroids for a longer time (around 1 yr). If child
remained in remission for at least 1 yearr then stop steroid and follow 3-6 monthly.
If the child is not improving on the steroids or features of steroid toxicity appears then child to be
started on Azathioprine (3-5mg/kg/day, Tab 50mg) and Hydroxychloroquine (5-10mg/kg/day,
Tab 200mg, if not started earlier) and follow up 3 monthly for disease status and side effects of
drug ( LFT, RFT, Hemogram).
Follow up in Pediatric chest clinic:
Aim is to keep the child in remission for at least 1 year.
Every visit :
Ask about history of any cough, breathlessness, wheezing, cyanosis, fever
Look for respiratory distress, cyanosis, tachypnea , chest findings
Check SPo2 in every visit and spirometry ( PFT at least once in 6 month)
Diagnosed as acute exacerbation if child is tachypneic, presence of crepts/ rhonchi,
hypoxemic.
85
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Diagnose ILD on basis of tachypnea, clubbing,
hypoxemia with HRCT Chest findings
Start on steroids 0.5mg/kg/day for 2 weeks
Taper off steroids 2.5mg every weekly till 5-
7.5mg alternate day ( to be continued) and
review after 3 months
Improvement No Improvement tachypnea improved, no
hypoxemia
Do not stop steroid, continue low Continue steroid, add Azathioprine (3-
dose steroid and monitor child every 3 5mg/kg/day, Tab 50mg) and HCQ (5-10
monthly. Check spo2 every visit and mg/kg/day, Tab 200mg, it not started earlier)
PFT every 6 monthly Monitor 3 monthly for disease status and side
effects of drugs (LFT/ RFT/ Hemogram) IF
improvement and child remained in remission for 1
yr first stop steroids, then HCQ or Azathioprine).
Stop steroid if child remained in Duration of treatment vary according to patient
remission for atleast 1 yr. Intermittent response to drugs and will be individualized.
exacerbations should be treated with
steroids as initial treatment
Figure 1: Management of interstitial lung disease
86
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Pulmonary Hemorrhage
87
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Pulmonary Hemorrhage
Pulmonary hemorrhage may arise from relatively low volume but high pressure bronchial
circulation or low pressure but high volume pulmonary circulation. Hemorrhages involving
bronchial circulation are usually large in volume and hence associated with hemoptysis.
Whereas, hemorrhages involving pulmonary circulation are usually intra-alveolar and may or
may not be associated with hemoptysis. Irrespective of the source of bleeding, pulmonary
hemorrhages lead to significant morbidity and rarely mortality.
Causes of pulmonary hemorrhage:
Infections related complications, mechanical trauma, vascular disorders and congenital lung
malformation usually lead to focal hemorrhages (Box 1).
Box 1: Causes of Focal Pulmonary Hemorrhage in Children
Infection related sequelae Coagulopathy
Bronchitis Von Willebrand's disease
Bronchiectasis Thrombocytopenia
Cystic fibrosis Anticoagulants
Primary ciliary dyskinesia Congenital Lung Malformations
Immunodeficiency Sequestration
Lung abscess Congenital pulmonary airway
Pneumonia malformations
Mechanical trauma Bronchogenic cyst
Airway laceration Miscellaneous
Lung contusion Catamenial
Artificial airway Factitious
Suction catheters Neoplasm
Foreign body
Inhalation injury
Vascular Disorders
Pulmonary embolism/thrombosis
Pulmonary arteriovenous malformation
Pulmonary hemangioma
Source: Kendig, 8th Ed 2012
88
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Disruption of the alveolar-capillary basement membrane due to immune or non-immune
mediated disorders lead to diffuse alveolar hemorrhages (DAH) and it is commonly known as
pulmonary hemosiderosis (Box 2). Sources of bleeding in DAH are capillaries and small vessels
of the pulmonary circulation. The hallmark of immune mediated DAH is pulmonary capillaritis
and it is usually developed secondary to small vessel vasculitis or connective tissue disorders.
Box 2: Causes of Diffuse Alveolar Hemorrhage
Immune Mediated (Associated with pulmonary capillaritis - diagnosed by histopathology)
Idiopathic pulmonary capillaritis
ANCA associated vasculitis
o Granulomatosis with polyangitis (Wegener's Granulomatosis)
o Microscopic polyangiitis
Goodpasture's syndrome
Systemic lupus erythematosus
Henoch-Schönlein purpura
Behçet's disease
Cryoglobulinemic vasculitis
Juvenile idiopathic arthritis
Nonimmune Mediated (Not associated with pulmonary capillaritis)
Idiopathic pulmonary hemosiderosis
Acute idiopathic pulmonary hemorrhage of infancy
Heiner's syndrome (cow's milk protein hypersensitivity)
Celiac disease (Lane-Hamilton Syndrome)
Pulmonary lymphangioleiomyomatosis (LAM)
Asphyxiation/abuse
Cardiovascular causes
o Pulmonary vein atresia/stenosis
o Total anomalous pulmonary venous return
o Pulmonary veno-occlusive disease (PVOD)
o Mitral stenosis
o Left-sided heart failure
o Pulmonary capillary hemangiomatosis (PCH)
o Pulmonary telangiectasia
Source: Kendig, 8th Ed 2012.
Idiopathic Pulmonary Hemosiderosis (IPH):
It is a diagnosis of exclusion. IPH is a form of DAH without the evidence of capillaritis and
secondary causes (mentioned in Box 1 and 2) have to be excluded before making the diagnosis.
89
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Approach to pulmonary hemorrhage
When to suspect pulmonary hemorrhage?
Pulmonary Hemorrhage is suspected if there is frank hemoptysis or if there is respiratory
symptoms, anemia, varying degree of hypoxia and diffuse alveolar infiltrates on chest
radiographs.
Hemoptysis must be differentiated from hematemesis or local bleeding from nose or oral cavity.
Approach to diagnosis
Step 1: Confirm pulmonary hemorrhage
1. Frank hemoptysis without any doubt will suggest pulmonary hemorrhage.
2. Sputum, GA, or BAL for hemosiderin-laden macrophages - confirms chronic or recurrent
pulmonary hemorrhage
Step 2: Evaluate for etiology of pulmonary hemorrhage
Once pulmonary hemorrhage is confirmed, evaluate further for possible etiology. Detailed
history and examination for the pathologies as shown in Box-1 and Box-2.
Consider following work-up: every child will not require all investigations and it may be tailored
based on history, examination and results of some basic investigations.
1. Hemogram with PS for type of anemia,
2. Chest X-ray
3. PT/LFT/RFT
4. Urine R/M
5. CECT/HRCT Chest (Angiogram depending on CXR and chest CT findings)
6. 2DEcho (If suspecting cardio vascular etiology)
90
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
7. ANA (Anti dsDNA, if ANA positive)
8. ANCA [anti-PR3 antibodies (c-ANCA pattern), Anti-MPO antibodies (p-ANCA pattern)]
9. Celiac serology
10. Rheumatoid factor
11. Precipitating antibody (IgG) and specific IgE against Cow’s milk protein, Total IgE
(Especially in infants suspecting Heiner’s syndrome)
12. Stool for occult blood (for Heiner syndrome)
13. Anti-GBM antibody (If evidence of renal involvement present)
14. APLA work up
15. Lung biopsy (In selected cases, mainly to diagnose/exclude pulmonary capillaritis)
A diagnosis of idiopathic pulmonary Hemosiderosis (IPH) is made when alveolar hemorrhage
is confirmed by hemosiderin laden macrophages in GA/Sputum/BAL and no underlying cause is
found following a work-up as above.
Treatment
In acute hemorrhage:
Supportive care: O2, IV Fluids, Blood and blood product transfusion if required. Correct any
coagulation defects if present. Rarely may need ventilatory support.
Following the acute management: Arrange work up to identify the possible etiology.
If life threatening pulmonary hemorrhage with possible or diagnosed immune mediated etiology-
consider intravenous pulse steroid, cyclophosphamide or IVIG at the beginning.
Rest of the management and follow up of pulmonary hemorrhage are depended on the
underlying etiology.
91
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
If diagnosis of IPH is made, follow this regimen:
Start oral prednisolone 1-2 mg/kg/day along with
Inhaled steroids: Budecort 200 µg BD or Foracort 200 µg BD (> 5yrs of age),
Tab HCQ (200 mg Tab) 3-5mg/kg/day, and
Iron 3-4 mg/kg/day (if anemia present).
No response or
Response poor response
present
Start tapering oral steroids after 2-4 weeks
by 2.5 mg weekly till 5 mg alternate day* Add azathioprine
Continue inhaled steroids and HCQ as same (50 mg Tab) 1-3
(Stop Iron if anemia improved) mg/kg/day
Response No response or
present poor response
Monitor every 3 months*
If disease is in remission for 12 months
Stop oral steroids Arrange lung biopsy if not done
Followed by HCQ Complete immunological work up
(and azathioprine if added) Consider cyclophosphamide
Lastly ICS
Over a period of 3-6 months
*Treat each acute exacerbation with oral steroids 1-2 mg/kg/day for 1-2 months then taper off
slowly as mentioned above. If frequent relapse on tapering steroids, consider steroid sparing
agent- azathioprine and try to taper off steroids.
92
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Sarcoidosis
93
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Sarcoidosis
When to suspect:
Multisystem involvement
Skin - Erythema nodosum, papules, nodules, plaques, changes in old scars, erythema
nodosum, hypopigmented or hyperpigmented lesions, lupus pernio, ichthyosis and
erythroderma.
Parotid enlargement
Uveitis
Bilateral facial nerve palsy
Seizures – otherwise unexplained
Hepatosplenomegaly & lymphadenopathy
Hypercalcemia with Hyperphosphatemia, High 25-hydroxycholecalciferol and
Hypercalciuria
Anemia, Pancytopenia, thrombocytopenia,
Cardiac arrhythmias
Bilateral Hilar Lymphadenopathy in chest radiograph
Spondyloarthritis
Noncaseating epithelioid cell granulomas
Clinical features and laboratory abnormalities in sarcoidosis are shown in Box 1.
94
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Box 1: Clinical features and laboratory abnormalities in sarcoidosis
Clinical Features Laboratory findings
Fever Raised ESR, anemia, leukopenia, thrombocytopenia,
Weight loss pancytopenia, rarely eosinophilia.
Cough Hypercalcemia, Hyperphosphatemia, hypercalciuria (elevated
Fatigue/lethargy urinary calcium creatinine ratio), elevated serum 25-hydroxy
Bone and joint pain cholecalciferol.
Arthritis Liver
Red eye, photophobia Increased SGOT,SGPT, alkaline phosphatase
Parotidenlargement Increased total proteins
MaculopapularRash Decreased serum albumin
Plaques and nodules Radiology
Erythemanodosum BHL with homogenous nonnecrotic mediastinal nodes,
Uveitis acute or healed subpleural and perilymphatic pulmonary nodules, GGO, fibrotic
Lymphadenopathy changes in advanced disease
Hepatomegaly Pulmonary Function Test
Splenomegaly Reduced FVC, FEV1 and DLCO
Dyspnea,crepitations, BAL
rhonchi High lymphocytic low neutrophils and eosinophils (<1%) and
Cyanosis, clubbing increased CD4/CD8 ratio >2:1
Others
Increased serum ACE level
95
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Initial Evaluation:
Complete history and physical examination including careful examination of lungs,
peripheral lymph nodes, skin, eyes, parotid glands, liver, spleen, nervous system, and
joints
Chest radiograph PA and lateral view.
HRCT chest – to see lung parenchyma, CECT chest +/- Abdomen to see lymph nodes.
(HRCT + CECT chest and USG KUB is an alternative)
Mtx test
Spirometry to assess FVC, FEV1, FEV1/FVC, PEF, MEF 25-75, Bronchodilator
reversibility
CBC including Hb, TLC, DLC, platelet, ESR
LFT, RFT
Serum Calcium, Phosphate, SAP, Serum 25-hydroxy Cholecalciferol Level, Urine
calcium:creatinine ratio
USG – ABD KUB – to see nephrocalcinosis
ACE level ( send blood sample to CN Centre)
Eye evaluation ( Slit lamp, tonometry, fundus) – All suspected children
Biopsy of affected organ (FNA –cytology would be an alternative) – Select most feasible
site with good yei
All tissue samples- TB work up – AFB, geneXpert, MGIT.
Bronchoscopy (well described in adults) with sarcoidosis. Airway changes are best
appreciated with bronchoscopy and include specific changes of waxy yellow mucosal
nodules and non-specific changes such as erythema, edema, granularity, and
96
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
cobblestoning of airway mucosa and bronchial stenosis, typically in the lobar and
segmental bronchi.
BAL- Cytopathology – 1069, Should do BAL- AFB, geneXpert, BAL MGIT.
If EBUS-FNA – Cytology, AFB, geneXpert, MGIT
BAL-CD4:CD8 ratio in fresh sample Dr Mitra’s lab room 92 ground floor teaching block
– near director’s office. An appointment should be taken before procedure. BAL analysis
will be done on Tuesdays and Thursdays (Not on Fridays).
ECG
Echocardiogramme and further cardiological evaluation if cardiac involvement.
MRI Brain +/- Spine and CSF – CNS involvement
Diagnosis:
Multisystem involvement with characteristic features.
Tissue study – well organized non-caseating granulomas in a vicinity of normal tissue.
FNA may replace biopsy.
Exclude other causes of granulomas [immunodeficiency syndromes (CGD), fungal* and
mycobacterial infections*, ulcerative colitis, and Wegener's granulomatosis*,
Brucellosis, Hypersensitive pneumonitis] * Usually - Caseating
Treatment: Steroids
Steroids are the cornerstone of therapy. The following criteria should prompt consideration for
corticosteroid treatment:
97
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Pulmonary parenchymal involvement, evidence of restrictive lung disease.
Cardiac, neurologic, ocular, renal involvement or Hypercalcemia, even with mild
symptoms
Severe debilitating symptoms from any organ involvement
Corticosteroid (1-2 mg/kg/day) for 4 weeks and then is tapered.
A response to therapy is usually seen within 6 to 12 weeks of initiation of therapy,
Steroid therapy typically needs to be continued for 6-12 months in order to prevent
relapse. Relapses are treated with increasing doses of corticosteroids.
Second Line/Combined Therapy
To minimize the duration and toxicity of steroids and to improve the clinical outcome
disease modifying drugs are used Low-dose methotrexate (MTX 7.5-10 mg/m2/weekly
usually combined with weekly folinic acid) – eg MTX every Thursday, Folinic- Sunday
Azathioprine, Cyclophosphomide, Cyclosporine, Tacrolimus, MMF, Infliximab can be
used
HCQs for specific cases .
Follow-up Monitoring
Every 3 monthly – (Earlier if indicated) up to 3 years after discontinuation of therapy.
CBC, RFT, LFT, Serum Ca, Phosphate, SAP, Serum ACE, Calcium: Creatinine - At
diagnosis, at 03 months, then 06 monthly till therapy is over. (Do earlier if indicated)
Chest radiograph – At diagnosis, at 03 months (If positive findings at diagnosis), 06
months – Plan according to the need.
98
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
PFT/Spirometry – At Diagnosis, 03 months, 06 months then annually if achieved normal
findings – 03-06 month value needed if clinically indicated.
Monitor side effects of therapy : BP , Eye examination, RBS/FBS,
For Methotrexate toxicity, monitor CBC, LFT every 3 months.
Approach:
Diagnose Sarcoidosis : multisystem involvement- lympadenopathy,
hepatosplenomegaly, skin rash, arthritis with non caseating granuloma
Investigations: CBC with ESR, LFT, RFT, ACE Level, Serum calcium, Urinary calcium
creatinine ratio, increase 25Dihydroxy cholecalciferol, Chest x-ray ( AP/ Lateral),
CECT Chest, PFT, Mantoux, Biopsy and Bronchoscopy BAL elevated CD4:CD8 ratio
Start treatment if patient is symptomatic:
Steroids 1-2mg/kg/day for 4 weeks then tapered 2.5 mg weekly (5mg/2 weeks) to 5-
7.5mg A/D for a period of 6-12 months.
In case of steroid toxicity/ resistant:
Methotrexate (10-15mg/m2 weekly (max dose 25mg) or Azathioprine,
Cyclophosphomide, Cyclosporine, Tacrolimus, MMF, Infliximab
Monitor every 3 monthly, ask about the symptom status
Investigations as above
Stop steroids :
Patient should be asymptomatic
Received steroid treatment for about 6-12 months
MTX will be continued till 12-24 months
Follow patient every 3 monthly after stopping treatment for at least 3 yrs
Normal ACE level , normal physical examination
99
If Child is on MTX/ HCQ then stop it after 3- 6months after stopping steroids
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Pleurodesis with Povidone
iodine for Recurrent
pneumothorax
100
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Pleurodesis with Povidone iodine for Recurrent pneumothorax
Prerequisite for the procedure:
(1) Lung had expanded before procedure
(2) Column in chest tube is not moving fast s/o broncho-pleural fistula
(3) Hemodynamically stable
(4) Normal renal function test.
(5) No known hypothyroidism
(6) No known allergy to iodine
Procedure:
1. Counsel the family regarding need and possible side effects of pleurodesis. Explain of difficulty
for lung transplantation after the procedure, if family planning for transplantation.
2. Prepare lignocaine solution: 2mg/kg lignocaine in 20 ml saline in older children (>5 yr) 10 ml in
young children (< 5yrs).
3. Inject lignocaine solution into pleural cavity through chest tube.
4. Weight for 15 minutes.
5. Prepare povidone iodine solution: total volume 2 ml/kg with 1:4 dilution of 10% povidone iodine
with normal saline.
6. Inject required amount (2ml/kg) of diluted povidone iodine into pleural cavity through chest tube.
7. Clamp the chest tube for 4 hours.
8. Release the clamp after 4 hrs.
9. Get a chest x-ray; if lung remain expanded in chest x-ray remove chest tube.
10. Monitor the child throughout the procedure and 24 hrs there after.
11. Perform thyroid function test
101
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
This Document has been modified with Flexcil app (iOS) https://www.flexcil.com
AIIMS Peds Pulmo Protocols-June 2017
Contributors
Dr S K Kabra Dr Samriti Gupta
Dr Rakesh Lodha Dr Krishna M Gulla
Dr Kana Ram Jat Dr Ganganath Gunathilaka
Dr Jhuma Sankar Dr Channa de Silva
Dr Aparna Mukherjee Dr Arvind Kumar
Dr Nitin Dhochak
102
Flexcil - The Smart Study Toolkit & PDF, Annotate, Note
You might also like
- BRONCHIAL ASTHMA Presentation2Document40 pagesBRONCHIAL ASTHMA Presentation2Shami PokhrelNo ratings yet
- Bronchial AsthmaDocument29 pagesBronchial AsthmaDrShaheen100% (5)
- Asthma Diagnosis & Treatment GuideDocument5 pagesAsthma Diagnosis & Treatment GuideShalini ShanmugalingamNo ratings yet
- Asthma: For Use of A Registered Medical Practitioner OnlyDocument31 pagesAsthma: For Use of A Registered Medical Practitioner OnlyCCU FellowsNo ratings yet
- Pedia Bronchial Asthma-1Document43 pagesPedia Bronchial Asthma-1MAHEJS HDNo ratings yet
- Drug Selection Patterns in Asthma and Hyperre Active Airway Disease in ChildrenDocument16 pagesDrug Selection Patterns in Asthma and Hyperre Active Airway Disease in ChildrenInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Guideline For Management Protocol of Children With Fever and Respiratory SymptomsDocument44 pagesGuideline For Management Protocol of Children With Fever and Respiratory SymptomsKushagr GautamNo ratings yet
- Respirology 2023 FinalDocument127 pagesRespirology 2023 FinalBelinda ELISHANo ratings yet
- Bronchial AsthmaDocument59 pagesBronchial Asthmashefalika mandremNo ratings yet
- 2020 Gina Guidelines On The Management of AsthmaDocument38 pages2020 Gina Guidelines On The Management of AsthmaLouije MombzNo ratings yet
- Bronchial Thermoplasty and Guided Bronchoscopy Part OneDocument25 pagesBronchial Thermoplasty and Guided Bronchoscopy Part OneFistiNo ratings yet
- Difficult Asthma GuidelinesDocument6 pagesDifficult Asthma GuidelinesLee SakieNo ratings yet
- Anaphylaxis HandoutDocument3 pagesAnaphylaxis HandoutLakshay Chanana0% (1)
- Covid-19 Management: FAQs by HCWsDocument31 pagesCovid-19 Management: FAQs by HCWsKabirNo ratings yet
- Peds 2 - Pulmonary Disorders of ChildrenDocument27 pagesPeds 2 - Pulmonary Disorders of ChildrenMinh Nguyễn Phương HồngNo ratings yet
- As Ma 2Document6 pagesAs Ma 2api-3728652No ratings yet
- File 18585Document15 pagesFile 18585Mohammed MuthanaNo ratings yet
- OkojijijkDocument11 pagesOkojijijkLatrell GelacioNo ratings yet
- Bronchial Asthma 085523Document29 pagesBronchial Asthma 085523Satrumin ShirimaNo ratings yet
- Asthma in Children: April 2014Document35 pagesAsthma in Children: April 2014abdisalaan hassanNo ratings yet
- Farmasi Klinis 2 - Asma Akut (Eksaserbasi Asma) - From: Gina 2017 - By: Amelia Lorensia - 2017Document52 pagesFarmasi Klinis 2 - Asma Akut (Eksaserbasi Asma) - From: Gina 2017 - By: Amelia Lorensia - 2017Alifah SyarafinaNo ratings yet
- Childhood Asthma Research PaperDocument4 pagesChildhood Asthma Research Paperaflbtjglu100% (1)
- Asthma Handbook: Summaries and Resources To Support Best PracticeDocument28 pagesAsthma Handbook: Summaries and Resources To Support Best Practicenandar wirawanNo ratings yet
- ContentServer - 2022-02-07T120904.099Document8 pagesContentServer - 2022-02-07T120904.099Cesar Jesus Jara VargasNo ratings yet
- Asthma and COPDDocument79 pagesAsthma and COPDDawit g/kidanNo ratings yet
- Guia de Asma Severa en Niños y Adolescentes Un Documento Practica para MedicosDocument11 pagesGuia de Asma Severa en Niños y Adolescentes Un Documento Practica para MedicosktriveraNo ratings yet
- COVID-19 Infection in Children GuideDocument12 pagesCOVID-19 Infection in Children GuideSutirtha RoyNo ratings yet
- 4832 concept mapDocument7 pages4832 concept mapapi-739571122No ratings yet
- BRONCHIOLITISDocument19 pagesBRONCHIOLITISKamilla AbdullahNo ratings yet
- A Presentation On Bronchial Asthma: Presented byDocument72 pagesA Presentation On Bronchial Asthma: Presented bydyakusumaNo ratings yet
- Diagnosis and Management of Asthma in Children Under The Age ofDocument18 pagesDiagnosis and Management of Asthma in Children Under The Age ofahmedNo ratings yet
- GINA Guidelines 2019 SummaryDocument36 pagesGINA Guidelines 2019 Summaryfelly iswaNo ratings yet
- Presented By: MANOJ MANDAL 1 Year P.C BSC NSG, Mibe, GSNDocument42 pagesPresented By: MANOJ MANDAL 1 Year P.C BSC NSG, Mibe, GSNfurr singhNo ratings yet
- Journal 4zDocument3 pagesJournal 4zAceking MarquezNo ratings yet
- AsthmaDocument8 pagesAsthmahusainozelNo ratings yet
- Pediatric Home Sleep Apnea TestingDocument14 pagesPediatric Home Sleep Apnea TestingBenja GuzmánNo ratings yet
- Global Inititive For Asthma (GINA)Document10 pagesGlobal Inititive For Asthma (GINA)Shahiza IsaNo ratings yet
- COVID 19. 4 - 13 KashmerDocument42 pagesCOVID 19. 4 - 13 KashmerIshfaq GanaiNo ratings yet
- VRS Vs AsmaDocument9 pagesVRS Vs AsmaPablo ParicahuaNo ratings yet
- Treatment of Children With COVID-19: Position Paper of The Italian Society of Pediatric Infectious DiseaseDocument17 pagesTreatment of Children With COVID-19: Position Paper of The Italian Society of Pediatric Infectious DiseasecurteanancaNo ratings yet
- Nursing Interventions: Asthma: PathoDocument4 pagesNursing Interventions: Asthma: Pathomische20No ratings yet
- Asthma Control: Guideline BasedDocument38 pagesAsthma Control: Guideline BaseddianutamiaNo ratings yet
- 6 - Asthma GuidelinesDocument21 pages6 - Asthma Guidelineshassan mohamedNo ratings yet
- Pulmonology - Cases With AnswersDocument4 pagesPulmonology - Cases With AnswersSimran PiñheiroNo ratings yet
- CASE PRESENTATIONDocument34 pagesCASE PRESENTATIONPhilbert Russell Del ValleNo ratings yet
- GP Reg - Asthma and Spirometry 2011Document114 pagesGP Reg - Asthma and Spirometry 2011minerva_stanciuNo ratings yet
- Draft For Concept MapDocument4 pagesDraft For Concept MapMartin AlcantaraNo ratings yet
- AshmaDocument51 pagesAshmaAliyi MuktarNo ratings yet
- Snijders 2007Document6 pagesSnijders 2007carlaNo ratings yet
- Pediatr Pulmonol 2018 53 10 1422-1428Document7 pagesPediatr Pulmonol 2018 53 10 1422-1428baltazarottonelloNo ratings yet
- Children With Chronic Non Specific CoughDocument7 pagesChildren With Chronic Non Specific CoughAzmachamberAzmacareNo ratings yet
- Asthma Diagnosis and Treatment OverviewDocument82 pagesAsthma Diagnosis and Treatment OverviewImmanuel100% (1)
- Nebulizer ProquestDocument10 pagesNebulizer ProquestFadhli WijayaNo ratings yet
- AsthmaDocument23 pagesAsthmaLeoNo ratings yet
- Med - Asma BronquialDocument6 pagesMed - Asma BronquialEduardo PierluissiNo ratings yet
- Bronchial Asthma Diagnosis and ManagementDocument61 pagesBronchial Asthma Diagnosis and Managementsebghatullah mubarezNo ratings yet
- Asthma InvestigationDocument20 pagesAsthma InvestigationQasim HaleimiNo ratings yet
- Bronchial Asthma: A Comprehensive ReviewDocument39 pagesBronchial Asthma: A Comprehensive ReviewmiazaraNo ratings yet
- Asthma in Children My PresentationDocument49 pagesAsthma in Children My PresentationPutra Skate100% (2)
- Consensus Guidelines On Management of Childhood Convulsive Status EpilepticusDocument16 pagesConsensus Guidelines On Management of Childhood Convulsive Status EpilepticusS palNo ratings yet
- Neonatal Hypoglycemia 2Document6 pagesNeonatal Hypoglycemia 2Lalo LanNo ratings yet
- Neonatal Neurosonography: A Pictorial Essay: EuroradiologyDocument13 pagesNeonatal Neurosonography: A Pictorial Essay: EuroradiologyAnom RahartoNo ratings yet
- Emergency Triage Assessment and Treatment ETAT 2005Document83 pagesEmergency Triage Assessment and Treatment ETAT 2005RaymundoLauroTijerinaGarciaNo ratings yet
- Developmental Pediatrics in Office PracticeDocument60 pagesDevelopmental Pediatrics in Office PracticeVijay ArumugamNo ratings yet
- Spinal Cord Niraj sir-LTDocument54 pagesSpinal Cord Niraj sir-LTVijay ArumugamNo ratings yet
- Motor Vehicles Act SummaryDocument111 pagesMotor Vehicles Act SummarySardaar Harpreet Singh HoraNo ratings yet
- JVC Mini DV and S-VHS Deck Instruction Sheet: I. Capturing FootageDocument3 pagesJVC Mini DV and S-VHS Deck Instruction Sheet: I. Capturing Footagecabonedu0340No ratings yet
- Test Your Knowledge - Python and Automation - Coursera100Document1 pageTest Your Knowledge - Python and Automation - Coursera100Mario 1229No ratings yet
- Asma G.SDocument5 pagesAsma G.SAfia FaheemNo ratings yet
- Department of Labor: Logsafe Fall 01Document8 pagesDepartment of Labor: Logsafe Fall 01USA_DepartmentOfLaborNo ratings yet
- 1964-1986 OMC Sterndrive ManualDocument572 pages1964-1986 OMC Sterndrive ManualBarry Pieters75% (4)
- CV - Diego Allendes - Civil EngineerDocument1 pageCV - Diego Allendes - Civil EngineerPari D. ShitPostingNo ratings yet
- All Case Studies Blood Student Copy FINAL 2019Document14 pagesAll Case Studies Blood Student Copy FINAL 2019saud rehmanNo ratings yet
- Review On Birth Asphyxia by TibinDocument22 pagesReview On Birth Asphyxia by Tibintibinj67No ratings yet
- Reading Mats in English and FilipinoDocument29 pagesReading Mats in English and FilipinoVenus Mantaring LastraNo ratings yet
- AYUDA Multi-Words VerbsDocument6 pagesAYUDA Multi-Words VerbsGabriel RodriguezNo ratings yet
- Exercise in Class 1 English 1 PERSONAL PRONOUNSDocument2 pagesExercise in Class 1 English 1 PERSONAL PRONOUNSDarkness jhlp100% (1)
- Madbarz Routines Plan: Strength - AdvancedDocument18 pagesMadbarz Routines Plan: Strength - AdvancedJuan Sebastian AnguloNo ratings yet
- Awareness on Waste Management of StudentsDocument48 pagesAwareness on Waste Management of StudentsJosenia Constantino87% (23)
- Beautiful Fighting Girl - Book ReviewDocument3 pagesBeautiful Fighting Girl - Book ReviewCharisse Mae Berco - MaribongNo ratings yet
- PRACTICE-10 BảnDocument5 pagesPRACTICE-10 BảnBinh Pham ThanhNo ratings yet
- D20 Modern - Evil Dead PDFDocument39 pagesD20 Modern - Evil Dead PDFLester Cooper100% (1)
- 15 Resources To Learn C - Sharp PDFDocument4 pages15 Resources To Learn C - Sharp PDFSức Mạnh Niềm TinNo ratings yet
- Public High School Teachers' Strategies for Addressing Challenges in Conducting Action ResearchDocument75 pagesPublic High School Teachers' Strategies for Addressing Challenges in Conducting Action ResearchMilbert Loyloy SalmasanNo ratings yet
- Contract Day Watchman SHS - O. SanoDocument2 pagesContract Day Watchman SHS - O. SanoZaldy Tabugoca100% (2)
- B2 First Unit 11 Test: VocabularyDocument3 pagesB2 First Unit 11 Test: VocabularyNatalia KhaletskaNo ratings yet
- STOW - Vol. 3 - ScheduleDocument12 pagesSTOW - Vol. 3 - ScheduleDavid A. Malin Jr.100% (2)
- Importance of Research in ArchitectureDocument9 pagesImportance of Research in ArchitectureKathleen Mae SoriaNo ratings yet
- Psat Exam 2013Document34 pagesPsat Exam 2013tacobeo50% (4)
- UST Medicine I Schedule 2016-2017Document6 pagesUST Medicine I Schedule 2016-2017ina17_eaglerNo ratings yet
- Post Graduate Medical (Government Quota) Course Session:2021 - 2022 List of Candidates Allotted On - 04.03.2022 (Round 2)Document104 pagesPost Graduate Medical (Government Quota) Course Session:2021 - 2022 List of Candidates Allotted On - 04.03.2022 (Round 2)Aravind RaviNo ratings yet
- Yukot, LeeYDocument5 pagesYukot, LeeYDevansh GoelNo ratings yet
- 2018 Gauss 7 ContestDocument4 pages2018 Gauss 7 ContestpriyagvNo ratings yet
- Geoboards in The ClassroomDocument37 pagesGeoboards in The ClassroomDanielle VezinaNo ratings yet
- The American Colonial and Contemporary ArchitectureDocument2 pagesThe American Colonial and Contemporary ArchitectureHaha HahaNo ratings yet