Professional Documents
Culture Documents
Disease, Bugs, & Classification
Disease, Bugs, & Classification
Uploaded by
mei yuOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Disease, Bugs, & Classification
Disease, Bugs, & Classification
Uploaded by
mei yuCopyright:
Available Formats
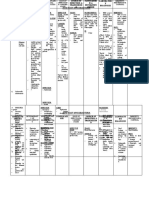
Disease Bug Classification First-line Treatment Duration of Treatment If Beta-Lactam Allergic / Alternatives
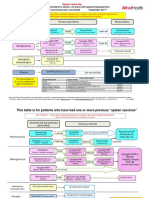
Streptococcus Pneumo Gram + diplococci 1) Dexamethasone given prior to or with 1st dose x10-14 days Moxifloxacin or Levofloxacin + Vanco
Meningitis Haemophilus influenzae Gram - rod 2) Ceftriaxone 2 g IV q12 hrs OR Cefotaxime 2 g IV q4-6 hrs PLUS Vanco x 7 days ± Bactrim (for Listeria coverage)
Neisseria meningitidis Gram - cocci x 7 days
Listeria monocytogenes Gram + rod If pt is < 1 month old, > 50 y.o., or immunocompromised, add AMPICILLIN for Listeria coverage x 21 days
Lower Respiratory Tract Infections
Abx are only indicated for bacterial exacerbations of chronic bronchitis: Azithromycin OR
Bronchitis RSV, adenovirus, rhinovirus, N/A 1) Augmentin x 5-10 days Doxycycline
coronavirus, influenza, parainfluenza 2) Azithromycin
3) Doxycycline
Healthy outpatients w/out abx use within 90 days (NO RISK FOR DRSP) & no comorbidities: Resp. FQ monotherapy
MONOTHERAPY with: Moxifloxacin
1) Macrolide abx Levofloxacin
Streptococcus Pneumo Gram + diplococci 2) Doxycycline Gemifloxacin
Community Acquired Pneumonia Haemophilus influenzae Gram - rod Unhealthy outpatients w/ abx use within 90 days (↑ RISK FOR DRSP) and/or comorbidities: x 5-7 days
Chlamydia pneumoniae Atypical 1) Beta-lactam (pref: cefpodixime cefdinir) + either a macrolide abx OR doxycycline
Mycoplasma pneumoniae Atypical 2) Resp. FQ MONOTHERAPY (Moxifloxacin, Levofloxacin, Gemifloxacin)
Hospitalized inpatients:
1) Beta-lactam (pref: ceftriaxone, cefotaxime) + azithromycin
2) Reserve for beta-lactam allergic: Resp. FQ MONOTHERAPY (Avelox, Levaquin, Factive)
MYCOBACTERIUM TUBERCULOSIS
Tuberculosis (highly contagious) Atypical acid-fast bacili
MSSA Gram + clusters Nafcillin OR Cefazolin x 4-6 weeks PLUS gentamicin (IF PROSTHETIC VALVE) x 2 weeks Vancomycin If bacteria produce a biofilm (slime layer),
When gentamicin used
Infective Endocarditis MRSA Gram + clusters Vancomycin x 4-6 weeks PLUS gentamicin (IF PROSTHETIC VALVE) x 2 weeks for synergy: which is easy to do so on prosthetic valves, use:
Streptococcus viridans Gram + pairs/chains PCN, Ampcillin, OR Ceftriaxone x 4-6 wks ± gentamicin for synergy x 2 weeks Target Pk: 3-4 Vancomycin RIFAMPIN in Staph. prosthetic valve endocarditis -->
Enterococcus Gram + pairs/chains PCN or Ampicillin x 4-6 weeks PLUS gentamicin for synergy x 4-6 weeks Target Tr: < 1 Vancomycin penetrates biofilm
Intra-abdominal Infections
Streptococci Gram + pairs/chains DoC: Ceftriaxone (Rocephin)
Primary Peritonitis (SBP) & Cholecystitis Enteric gram-neg's: Primary/Secondary SBP Px: Bactrim, cipro, ofloxacin x 5-7 days Alt: Ampicillin, gentamicin, FQ's
(gallbladder inflamm.) Proteus mirabilus Gram - rods
E. coli Gram - rods
Klebsiella Gram - rods
Single Agent (MonoTx
Streptococci Gram + pairs/chains
that covers
Infection Severity: anaerobes): Two Agents:
Enteric gram-neg's: Gram - rods Cefoxitin Cefazolin, Cefuroxime,
Bacteroides fragilis Gram - anaerobe Mild-Mod. Ertapenem Ceftriaxone, PLUS Flagyl (covers anaerobes) x 4-7 days
Secondary Peritonitis & Cholangitis
maybe Enterococcus Gram + pairs/chains Moxifloxacin Cipro, Levo None
(infection of common bile duct)
CAPES (severe ICU cases): Carbapenem Cefepime, Ceftazidime x 7-14 days
Citrobacter Gram - Severe (in ICU) (except Ertapenem) Cipro, Levo PLUS Flagyl (covers anaerobes) If intra-abdom. abscess
Acinetobacter Gram - Zosyn Aztreonam, AMG present: ≥ 14 days
Pseudomonas Gram -
Enterobacter Gram -
Serratia Gram -
Staphylococcus Gram + clusters MonoTx options: Combo Tx: VANCOMYCIN PLUS x 7-14 days
Streptococcus Gram + pairs/chains Unasyn Ceftaizidime (FORTAZ, TAZICEF)
MRSA Gram + clusters Zosyn Cefepime (MAXIPIME) Deep Tissue Infection:
Diabetic Foot Infection Pseudomonas aeruginosa Gram - rods Primaxin Zosyn x 2-4 weeks None
Peptostreptococcus clostridium Gram + anaerobe Merrem Azactam
Bacteroides fragilis Gram - anaerobe Invanz Any carbapenem Osteomyelitis:
Polymicrobial Tigecycline (TYGACIL) Consider adding Flagyl if ceftazidime, cefepime, or azactam x4-6 weeks
Moxifloxacin (AVELOX) were chosen for anaerobic coverage
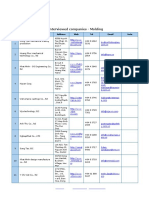
STI's
Syphilis (primary, secondary, or early 1) Doxy 100 mg PO BID x 14 days OR 2)
latent [<1 yr duration]) PCN G benzathine 2.4 million units IM x 1 dose (NEVER ADM. BICILLIN L-A IV --> SEIZURES/DEATH) Tetracycline 500 mg PO QID x 14 days
Syphilis (Late latent [>1 yr duration], Treponema pallidum Gram - spirochete
tertiary, or latent syphilis of unknown 1) Doxy 100 mg PO BID x 28 days OR 2)
duration) PCN G benzathine 7.2 million units total adm. as 3 2.4 million units IM q. week for three doses x 3 weeks Tetracycline 500 mg PO QID x 28 days
Beta-Lactam allergy: Zithromax 2 g PO x1 dose
PLUS EITHER gemiflox. 320 mg PO x1 dose OR
Gonorrhea Neisseria gonorrhoeae Gram - diplococci x 1 dose Gentamicin 240 mg IM x1 dose w/ a test for cure
Ceftriaxone 250 mg IM x1 dose PLUS EITHER (also covers Chlamydia co-infection) in 1 week
Alt: Cefixime 400 mg PO x1 dose +
Azithromycin 1 g PO x1 dose OR Doxy 100 mg PO BID x7 days Zithromax/Doxy with a test for cure in 1 week
Chlamydia Chlamydia trachomatis Gram - Azithromycin 1 g PO x1 dose OR Doxy 100 mg PO BID x7 days x1 dose Erythromycin, Levofloxacin, Ofloxacin
Trichomoniasis (yellow-green discharge) Flagyl 2 g PO x1 dose OR Tinidazole 2 g PO x1 dose Alt: Flagyl 500 mg PO BID x 7 days
Trichomonas vaginalis Protozoan x1 dose
Bacterial Vaginosis (fishy odor & basic pH Cleocin intravaginal 2% cream, Cleocin ovules
> 4.5 Idk dunno Flagyl 500 mg PO BID x7 days OR Flagyl 0.75% gel 5g intravaginally QD x 5 days (weakens condoms), Tindazole 1 g or 2 g
Ricketssial Disease & Related Infections
Rocky Mountain Spotted Fever Rickettsia rickettsii Gram - coccobacillus Doxycycline 100 mg PO/IV BID x 5-7 days None
Typhus Rickettsia typhi Gram - Doxycycline 100 mg PO/IV BID x 7 days None
Amoxil 500 mg PO TID x 14-21 days OR
Lyme Disease
Borrelia burgdorferi Gram - spirochete Doxycycline 100 mg PO BID x 10-21 days Cefuroxime 500 mg PO BID x 14-21 days
Ehrlichiosis Ehrlichia chaffeensis Gram - Doxycycline 100 mg PO/IV BID x 7-14 days None
Tularemia Francisella tularensis Gram - aerobic coccobacilli Gentamicin IV 5 mg/kg/day TDD DIVIDED q8 hrs OR Tobramycin IV 5 mg/kg/day TDD DIVIDED q8 hrs x 7-14 days None
Skin & Skin Structure Infections
Impetigo (blister-like rash, honey-colored Impetigo: Topical Mupirocin (BACTROBAN) OR retapamulin (ALTABAX) OR
Streptococcus Gram + pairs/chains No duration given
crusts)
MSSA Gram + clusters if numerous lesions: Cephalexin (KEFLEX)
Folliculitis (hair follicle infection) Folliculitis, Furuncles, & Carbuncles:
Furuncle (boil; hair follicle infection into
surrounding tissue) Staphylococcus aureus, incl. MRSA Gram + clusters 1) Cephalexin (for MSSA) OR No duration given
Carbuncle (group of infected furuncles) 2) Bactrim (for CA-MRSA) OR
3) Doxycycline (for CA-MRSA)
None
Streptococcus pyogenes Gram + pairs/chains Mild Cellulitis: PO abx must cover both Strep. & MSSA:
Cellulitis (mild non-purulent infection) x 5 days
Staphylococcus aureus Gram + clusters Cephalexin, Clindamycin, PCN VK, Dicloxacillin
Abscess (mild-mod. purulent infection) CA-MRSA Gram + clusters Single abscess, no systemic sx: I&D No duration given
Systemic sx present, or multiple sites: Bactrim, Doxy, Minocycline, or Clindamycin
Severe purulent SSTI - needs IV abx none given N/A Use IV abx that cover MRSA: Vanco, Dapto, Linezolid/Tedizolid, Ceftaroline, x 7-14 days
Telavancin/Dalbavancin/Oritavancin. Transition pt to PO abx once stable.
Necrotizing fasciitis Streptococcus pyogenes Gram + pairs/chains Refer to SICU. No duration given
Clostridium spp. Gram + anaerobe Empiric Tx: Vancomycin + beta-lactam (Zosyn, Primaxin, Merrem)
Diarrhea
Bacterial causes: Pref. treatment if fever, bloody stools, dysentery, or pt is PREGNANT or PEDIATRIC (NO FQ's!!)
E. coli Gram - rods 1) Azithromycin 1 g PO x1 dose OR
Campylobacter jejuni Gram - spirochete 2) Azithromycin 500 mg PO QD x1-3 days
Shigella Gram - rods
Salmonella Gram - rods Otherwise, if pt doesn't have any of the above characteristics, choose one of the following:
Viral causes: 1) Ciprofloxacin 750 mg PO x1 dose OR Cipro 500 mg PO BID x 3 days OR
Norovirus N/A 2) Levo 500 mg PO x1 dose OR Levo 500 mg QD x1-3 days OR
Traveler's Diarrhea Rotavirus N/A 3) Ofloxacin 400 mg PO x1 dose OR 400 mg BID x3 days OR See previous column None
Protozoal causes: 4) Rifaximin 200 mg PO TID x3 days
Found on surfaces/food/water
Giardia contaminated with feces from
infected humans/animals Protozoal Infections (ex. Giardia or Cryptosporidium):
Entamoeba histolytica Anaerobic parasitic amoeba 1) Flagyl OR AVOID ANTIMOTILITY AGENTS IN
Cryptosporidium Apicomplexan parasitic alveolates 2) Tinidazole OR BLOODY DIARRHEA OR FEBRILE PTS.
Cyclospora Apicomplexan parasitic alveolates 3) Nitazoxnid
D/C ALL ABX. D/c all meds that could cause diarrhea. FLAGYL IS NO LONGER REC.
DO NOT USE ANTI-MOTILITY AGENTS: AS 1ST-LINE TMT FOR C. DIFF
(Loperamide [IMODIUM], atropine/diphenoxylate [LOMOTIL], or opioids)
Infection Severity: 1st inf(x): 2nd inf(x)/1st recurrence: 3rd inf(x)/2nd recurrence:
Mild-Mod. If vancomycin was used to
treat 1st inf(x) -->
Vancomycin 125 mg VANCO TAPER/PULSE
PO QID OR Vanco Taper/Pulse Tx:
C.diff-associated diarrhea Clostridium difficile Gram + obligate anaerobe OR Fidaxomycin 200 mg 125 mg PO QID x 10-14 days, See previous column None
Severe: Fidaxomycin 200 mg PO BID x 10 days then BID x 1 week,
WBC ≥ 15,000 or PO BID x 10 days then QD x 1 week,
SCr ≥ 1.5x baseline If Flagyl was used to then q2-3 days x 2-8 weeks
Severe & Complicated: Vanco 500 mg PO QID treat 1st inf(x) -->
HypoTN, shock, ileus, PLUS Flagyl IV 500 mg Vancomycin 125 mg
or toxic megacolon q8 hrs PO QID x 10 days
Options for recurring C.diff inf(x) or pts at high risk for recurrence (immunosupp. or receiving chemoTx):
1) Fidaxomicin (DIFICID)
2) Fecal stool transplant
3) Bezlotoxumab (ZINPLAVA) - binds to C.diff toxin B. Adm. as 1x IV infusion.
You might also like
- BZZ BZZ BZZ: Sketchy MicroDocument18 pagesBZZ BZZ BZZ: Sketchy Microkissandtell88% (8)
- Infectious Diseases IDocument7 pagesInfectious Diseases ITiff VoNo ratings yet
- CNS Infection GuidanceDocument2 pagesCNS Infection GuidanceGus LionsNo ratings yet
- 246 - Respiratory Pathology Pneumonia - Treatment and PreventionDocument4 pages246 - Respiratory Pathology Pneumonia - Treatment and PreventionPranav PunjabiNo ratings yet
- Adult UriDocument7 pagesAdult UriYanna RizkiaNo ratings yet
- Bagan 4 (Systemic Fungal Infection (SFI) in A Neonate) + Bagan 2Document2 pagesBagan 4 (Systemic Fungal Infection (SFI) in A Neonate) + Bagan 2bethanessNo ratings yet
- Penggolongan Obat Berdasar Kelas TerapiDocument6 pagesPenggolongan Obat Berdasar Kelas TerapiSyaira MuhlisaNo ratings yet
- Empiric Treatment Guidelines Common InfectionsDocument9 pagesEmpiric Treatment Guidelines Common InfectionsShiza Batool100% (1)
- DRUG of CHOICE - InfectiousDocument1 pageDRUG of CHOICE - InfectiousJoseph De JoyaNo ratings yet
- Chapter 28 Infections: Perioperative Antimicrobial PPXDocument10 pagesChapter 28 Infections: Perioperative Antimicrobial PPXDrashtibahen PatelNo ratings yet
- HSB Pneumonia Antibiotic AlgorithmDocument4 pagesHSB Pneumonia Antibiotic AlgorithmDr.Senthil KumarNo ratings yet
- SHC Antimicrobial Prophylaxis in Surgery RecommendationsDocument3 pagesSHC Antimicrobial Prophylaxis in Surgery RecommendationsCatherine MorrisNo ratings yet
- Rapid Blood Pathogen Identification Panel: Staphylococcus Genus Analyte Will Be DetectedDocument8 pagesRapid Blood Pathogen Identification Panel: Staphylococcus Genus Analyte Will Be DetectedAlessia JankowskiNo ratings yet
- Management of CAP in Adults - Ontario GovernmentDocument2 pagesManagement of CAP in Adults - Ontario GovernmentSukhvir AujlaNo ratings yet
- Empiric Antibiotic ListDocument2 pagesEmpiric Antibiotic ListpasswordNo ratings yet
- Pneumonia Treatment Algorithm With Addendum For Aspiration 2015-2016.01.19Document2 pagesPneumonia Treatment Algorithm With Addendum For Aspiration 2015-2016.01.19Irsalina TriastutikNo ratings yet
- MrsaDocument13 pagesMrsaPaula Grace MorfeNo ratings yet
- Delafloxacin JCDocument11 pagesDelafloxacin JCDanny PhamNo ratings yet
- Infectious Hour (Antibiotics)Document90 pagesInfectious Hour (Antibiotics)Jill PardoNo ratings yet
- Hosp Ops II Week 3 Questions 1Document2 pagesHosp Ops II Week 3 Questions 1api-650133203No ratings yet
- Newyork-Presbyterian Hospital Sites: Columbia University Medical Center Guideline: Medication Use Manual Page 1 of 12Document12 pagesNewyork-Presbyterian Hospital Sites: Columbia University Medical Center Guideline: Medication Use Manual Page 1 of 12Ebey SomanNo ratings yet
- Acid Fast Bacteria: Mycobacterium TuberculosisDocument7 pagesAcid Fast Bacteria: Mycobacterium TuberculosisDesi RahmawatyNo ratings yet
- Meningitis Protocole المعدل 1-2-2016Document3 pagesMeningitis Protocole المعدل 1-2-2016Hamza El-ȜfifiNo ratings yet
- Onco Emergencies TLS (Increased U, K, Phos Decreased Ca) HyperleukocytosisDocument18 pagesOnco Emergencies TLS (Increased U, K, Phos Decreased Ca) HyperleukocytosisMaceyJamesNo ratings yet
- Principles of Antibiotic Selection - 1Document2 pagesPrinciples of Antibiotic Selection - 1YukiC123No ratings yet
- Drug Study RyDocument30 pagesDrug Study RyRyrey Abraham PacamanaNo ratings yet
- 1 s2.0 S0163445316300123 MainDocument2 pages1 s2.0 S0163445316300123 MainZara SaeedNo ratings yet
- Bakteri 1Document33 pagesBakteri 1aiysahmirzaNo ratings yet
- Drug Study Format and SampleDocument6 pagesDrug Study Format and SampleA.No ratings yet
- Respiratory DO PicsDocument5 pagesRespiratory DO Picsstefani bravoNo ratings yet
- Antibiotics in Critically IllnessDocument106 pagesAntibiotics in Critically IllnessFransisca Dewi KumalaNo ratings yet
- Viral Exanthem in PregnancyDocument3 pagesViral Exanthem in PregnancyCatherine Blanche LeeNo ratings yet
- Pediatric Hospital-Acquired and Ventilator-Associated Pneumonia Topic DiscussionDocument5 pagesPediatric Hospital-Acquired and Ventilator-Associated Pneumonia Topic Discussionapi-602288180No ratings yet
- Infectious Disease, Pulmonology, and GI Study NotesDocument22 pagesInfectious Disease, Pulmonology, and GI Study NotesAlexis TranNo ratings yet
- Drug Study of OxytocinDocument4 pagesDrug Study of OxytocinNichole DancelNo ratings yet
- World Health Organization (WHO) Emergency Use Authorization (EUA) Qualified COVID-19 VaccinesDocument2 pagesWorld Health Organization (WHO) Emergency Use Authorization (EUA) Qualified COVID-19 VaccinesNguyen Dang HaNo ratings yet
- Antibiotic Regimens For Neonatal Sepsis - UpToDateDocument2 pagesAntibiotic Regimens For Neonatal Sepsis - UpToDateMohd MaghyrehNo ratings yet
- RECOMMENDATIONS Spleen Registry PDFDocument3 pagesRECOMMENDATIONS Spleen Registry PDFannNo ratings yet
- PulmoDocument18 pagesPulmoAllum KaribasappaNo ratings yet
- Drug Analysis Drug Classification Indication Contraindication Mechanism of Action Side Effects/adverse Effects Nursing ResponsibilitiesDocument3 pagesDrug Analysis Drug Classification Indication Contraindication Mechanism of Action Side Effects/adverse Effects Nursing ResponsibilitiesCarmela VargasNo ratings yet
- CeftriaxoneDocument7 pagesCeftriaxoneGreats HalomoanNo ratings yet
- PDS Position Paper On Covid Vaccination - Final - 3 7 21Document7 pagesPDS Position Paper On Covid Vaccination - Final - 3 7 21KROPTECK GNo ratings yet
- InfectionDocument96 pagesInfectionBassem Georguos LabibNo ratings yet
- Antibiotics Chart Antibiotics ChartDocument9 pagesAntibiotics Chart Antibiotics ChartAnaliza Kitongan Lantayan100% (1)
- Communicable Disease Nursing Part II Diseases (1) 2Document21 pagesCommunicable Disease Nursing Part II Diseases (1) 2MK LiNo ratings yet
- Comm DiseasesDocument5 pagesComm DiseasesZaireXandraReyesNo ratings yet
- 6 Antimicrobial 2Document6 pages6 Antimicrobial 2TMC PGI GENER MICKONo ratings yet
- Infections in Primary CareDocument5 pagesInfections in Primary CareAtta Muhammad Memon100% (1)
- 1a Antiinfective DrugsDocument4 pages1a Antiinfective DrugsMaria Donabella OngueNo ratings yet
- Family Planning Personal NotesDocument4 pagesFamily Planning Personal NotesOB-GYNE DEPARTMENTNo ratings yet
- 18.2-Family Enterobacteriaceae ChartsDocument3 pages18.2-Family Enterobacteriaceae ChartsJesette KhoNo ratings yet
- Antibiotics10 PDFDocument19 pagesAntibiotics10 PDFDharani TharanNo ratings yet
- Antibiotics10 PDFDocument19 pagesAntibiotics10 PDFDharani TharanNo ratings yet
- Pneumonia ADULTDocument6 pagesPneumonia ADULTSebastian TjuwatjaNo ratings yet
- Drug Study - Cefazolin DoxycyclineDocument2 pagesDrug Study - Cefazolin DoxycyclineDan Dan Soi T50% (2)
- Group 9 - Bacteriology Reporting (Written Report)Document6 pagesGroup 9 - Bacteriology Reporting (Written Report)DENISE MARA�ANo ratings yet
- St. Vincent's Hospital Antibiotic Policy: GreenDocument2 pagesSt. Vincent's Hospital Antibiotic Policy: GreenistiqomahNo ratings yet
- Ab Ispa Ispb Flu TBCDocument10 pagesAb Ispa Ispb Flu TBCRizki YulisetiawanNo ratings yet
- Drug Study With NCPDocument4 pagesDrug Study With NCPJoanne Kathleen SantolicesNo ratings yet
- What Do You Hear The Effect of Stadium Noise On Football Players Passing PerformancesDocument27 pagesWhat Do You Hear The Effect of Stadium Noise On Football Players Passing PerformancesJorge Rubio LópezNo ratings yet
- Restaurant ManagerDocument2 pagesRestaurant Managerapi-77697357No ratings yet
- Summary of Lesson 3Document5 pagesSummary of Lesson 3dumba tambilinaNo ratings yet
- A Mercy by Toni MorrisonDocument2 pagesA Mercy by Toni MorrisonAbda PerveenNo ratings yet
- An Introduction To Transportation EngineeringDocument680 pagesAn Introduction To Transportation Engineeringrocket75% (4)
- The Worldisanapple: (Alberto S. Florentino)Document16 pagesThe Worldisanapple: (Alberto S. Florentino)MA. GI-AN SOLATORIONo ratings yet
- Flores v. Comelec (Partial Invalidity) DigestDocument2 pagesFlores v. Comelec (Partial Invalidity) DigestConcon FabricanteNo ratings yet
- AnalyseDocument5 pagesAnalyseMinh SangNo ratings yet
- CoU - Education Profile NewDocument13 pagesCoU - Education Profile NewSam EdiauNo ratings yet
- United States Court of Appeals, Third CircuitDocument22 pagesUnited States Court of Appeals, Third CircuitScribd Government DocsNo ratings yet
- Machine Learning Random Forest Algorithm - JavatpointDocument14 pagesMachine Learning Random Forest Algorithm - JavatpointRAMZI AzeddineNo ratings yet
- People Vs AntonioDocument15 pagesPeople Vs AntonioJomar TenezaNo ratings yet
- Case Study - Nestle - Mod 01Document6 pagesCase Study - Nestle - Mod 01Lakshmi KsrinivasNo ratings yet
- AS Trial - 2004 Sep - P1Document14 pagesAS Trial - 2004 Sep - P1Syafiq ShazwanNo ratings yet
- Common Psychosocial Problem in Adolescence: - Substance Abuse - Juvenile Delinquency - Smoking and AlcoholismDocument59 pagesCommon Psychosocial Problem in Adolescence: - Substance Abuse - Juvenile Delinquency - Smoking and AlcoholismSamjhana GautamNo ratings yet
- Onse Magazine 1Document60 pagesOnse Magazine 1항즈키만Mikoh-shieNo ratings yet
- Master BudgetDocument4 pagesMaster BudgetFawad Khan Waseem0% (1)
- I Tonya Reflection Reaction PaperDocument2 pagesI Tonya Reflection Reaction PaperAlgen UbasaNo ratings yet
- Equipment Qualification and Validation of Tablet Compression MachineDocument3 pagesEquipment Qualification and Validation of Tablet Compression MachineRajaSekhararayudu SanaNo ratings yet
- (Absensi Kuliah) 5A-Kajian Barat Atas Qur'anDocument2 pages(Absensi Kuliah) 5A-Kajian Barat Atas Qur'anZulhamdani SalayanNo ratings yet
- Psak 73Document10 pagesPsak 73analisa akuntansiNo ratings yet
- Ayodeji Ogunyemi Measuring and Improving The Quality of Supreme Audit Institutions of Developing Countries - Likely Challenges WWW Icgfm OrgDocument11 pagesAyodeji Ogunyemi Measuring and Improving The Quality of Supreme Audit Institutions of Developing Countries - Likely Challenges WWW Icgfm OrgFreeBalanceGRP100% (1)
- Siargao Division Office: KM 3, Dapa, Surigao Del NorteDocument2 pagesSiargao Division Office: KM 3, Dapa, Surigao Del NorteDazel Dizon GumaNo ratings yet
- Answers To SE630 HW2Document7 pagesAnswers To SE630 HW2GebBerheNo ratings yet
- Yutaka Nishiyama - Gauss' Method of Constructing A Regular HeptadecagonDocument14 pagesYutaka Nishiyama - Gauss' Method of Constructing A Regular HeptadecagonEduardo MullerNo ratings yet
- Macdonald Strategies in Pakistan and SouDocument5 pagesMacdonald Strategies in Pakistan and SouAbdullahNiaziNo ratings yet
- 2005 Weiss DissertationDocument422 pages2005 Weiss DissertationNessa100% (2)
- Assignment 1: Muhammad Areeb ShahidDocument4 pagesAssignment 1: Muhammad Areeb ShahidAreeb ShahidNo ratings yet
- Jade PresentationDocument11 pagesJade PresentationaaaaaaaNo ratings yet
- Bruce Lee - BiographyDocument7 pagesBruce Lee - BiographyLaishram PilotNo ratings yet