Professional Documents
Culture Documents
The Dolphin Prone Position in Awake COVID 19.2
Uploaded by
César Avila JimenezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Dolphin Prone Position in Awake COVID 19.2
Uploaded by
César Avila JimenezCopyright:
Available Formats
Clinical
DIMENSION
The “Dolphin” Prone
Position in Awake COVID-
19 Patients
Downloaded from http://journals.lww.com/dccnjournal by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8K2+Ya6H515kE= on 11/01/2021
Alberto Lucchini, RN; Dario Minotti, CCN-RN; Stefania Vanini, CCN-RN;
Flavia Pegoraro, CCN-RN; Luigi Iannuzzi, RN; Stefano Isgrò, MD
[DIMENS CRIT CARE NURS. 2021;40(6):311-314]
Prone positioning (PP) during invasive mechanical ventilazione mitigation strategies suggest the use of a premaneuver
has been demonstrated to improve respiratory mechanics and safety checklist. Thanks are due to the authors for sharing
gas exchange. Prone positioning reduces mortality of most their valuable experience with this issue. Even Bruni and col-
severe acute respiratory distress syndrome patients.1-3 In leagues11 recently described strategies to avoid complications
theory, these benefits should apply also to nonintubated during PP in ICU patients, and they had proposed a checklist
patients, in whom PP may improve oxygenation while to avoid PP complications. This checklist mainly deals with
delaying or even avoiding the need for intubation. Reports the implementation of PP in patients with invasive ventila-
of the application of PP in spontaneously breathing, tion. Although the authors have reported some suggestions
nonintubated adult patients, before the COVID era, are for using PP in awake patients undergoing noninvasive ventila-
limited to few case reports.4-6 During the last 14 months, tion (NIV), some guidance could be added. Prone positioning
PP has been largely used in all intensive care units (ICUs) to during helmet continuous positive airway pressure (CPAP) or
treat patients with COVID-19 acute respiratory failure.3 NIV requires some precautions, to avoid discomfort and skin
Even the use of awake PP, outside ICUs, has been investigated lesions. Awake patients during helmet CPAP may assume PP
by several authors during the COVID-19 pandemic.7-9 Albeit with minimal assistance.12
clear evidence on its impact of outcome is missing in awake
patients, PP is extensively used worldwide with several trials
ongoing. Although the respiratory benefits of PP in acute APPROACH
respiratory distress syndrome have been accepted, the con- Because of a high number of COVID-19 patients with
current complications could be undervalued.10 acute respiratory failure and of the shortage of ICU beds
González-Seguel and colleagues10 performed a scoping and ventilators, in our hospital, we started positioning pa-
review about PP complications, including 41 documents tients in helmet CPAP in general wards since the first days
from 121 eligible studies. They identified more than 40 indi- of March 2020.13-15 We reported experience from our insti-
vidual adverse events, and the highest pooled occurrence tution about patients treated with PP and helmet CPAP in
rates were that of severe desaturation (37.9%), barotrauma the general wards.7 Most patients were receiving CPAP, which
(30.5%), pressure sores (29.7%), ventilation-associated pneu- is a standard of care in our institution, whereas high-flow ox-
monia (28.2%), facial edema (16.7%), arrhythmia (15.4%), ygen were not available, and NIV is limited to a few high-
hypotension (10.2%), and peripheral nerve injuries (8.1%). dependency units.16 Between March 20 and April 9, 2020,
The reported mitigation strategies to reduce PP complications we enrolled 56 patients. Prone positioning was feasible
include alternate face rotation, repositioning every 2 hours, (maintained for at least 3 hours) in 47 patients. Among
and the use of pillows under the chest and pelvis. The reported patients for whom positioning was feasible, most maintained
DOI: 10.1097/DCC.0000000000000505 November/December 2021 311
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.
Figure 1. Standard prone position in an awake patient with helmet continuous positive airway pressure. This is available in color online at www.
dccnjournal.com.
proning for the initial 3-hour period (median, 3 hours [In- One of the reasons for discomfort, reported by patients
terquartile: 3-4]), and 25 patients maintained PP for longer undergoing PP and helmet CPAP in our hospital, was the dif-
than 3 hours. No other relevant adverse effects or compli- ficulty to maintain a comfortable position, especially for the
cations were observed. If patients asked to resume the vertebral column, when position was maintained for at least
supine position before 3 hours, PP was considered un- 3 hours. To increase patients' comfort, we adopted the “hel-
feasible and the reason was reported. Prone positioning met bundle” in all patients with helmet CPAP.13 The use of
was unfeasible in 9 patients, reasons for which included helmet without armpit braces is preferable, and another
discomfort during positioning (n = 5), coughing (n = 1), important precaution is to prevent the rigid collar from
uncooperativeness of the patient (n = 1), and decrease in generating skin lesions by direct pressure and mechanical
oxygenation and worsening of respiratory mechanics. stress to the neck. Unfortunately, the patient positioning
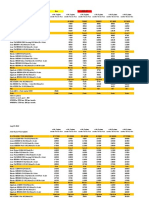
Figure 2. “Dolphin” prone position in an awake patient with helmet continuous positive airway pressure. This is available in color online at
www.dccnjournal.com.
312 Dimensions of Critical Care Nursing Vol. 40 / No. 6
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.
on the hospital beds, to guarantee the right functioning of 4. Feltracco P, Serra E, Barbieri S, et al. Non-invasive ventilation in
prone position for refractory hypoxemia after bilateral lung trans-
helmet CPAP, required the use of pillows under the chest. plantation. Clin Transplant. 2009;23(5):748-750.
As shown in Figure 1, when a patient is in PP with helmet 5. Valter C, Christensen AM, Tollund C, Schønemann NK. Re-
CPAP, the patient's back takes on a concave curvature. This sponse to the prone position in spontaneously breathing patients
with hypoxemic respiratory failure. Acta Anaesthesiol Scand.
“not physiological” position could be one of the reasons of 2003;47:416-418.
patients' discomfort when we tried to maintain position for 6. Scaravilli V, Grasselli G, Castagna L, et al. Prone positioning im-
a long time. For this reason, during the third COVID-19 proves oxygenation in spontaneously breathing non-intubated
patients with hypoxemic acute respiratory failure: a retrospective
wave (February to April 2021), we used a new approach study. J Crit Care. 2015;30:1390-1394. doi:10.1016/j.jcrc.2015.
to place awake patients with helmet CPAP in PP. The nurses 07.008.
encouraged patients to reverse their position on the bed, 7. Coppo A, Bellani G, Winterton D, et al. Feasibility and physiolog-
ical effects of prone positioning in non-intubated patients with
placing their head in the “bed foot area.” In this way, the acute respiratory failure due to COVID-19 (PRON-COVID): a
joint of the bed, normally dedicated to the inclination of prospective cohort study. Lancet Respir Med. 2020;8:765-774.
the lower limbs, was used to achieve a comfortable chest doi:10.1016/S2213-2600(20)30268-X.
8. Thompson AE, Ranard BL, Wei Y, et al. Prone positioning in
position. The inclination of the footrest made possible to awake, nonintubated patients with COVID-19 hypoxemic respi-
avoid use of additional pillows. Above all, using this new ratory failure. JAMA Intern Med. 2020;180:1537-1539. doi:10.
strategy, the patients' spine was able to maintain a neutral 1001/jamainternmed.2020.3030.
9. Perez-Nieto OR, Escarraman-Martinez D, Guerrero-Gutierrez
and natural position. As shown in Figure 2, the addition MA, et al, APRONOX Group. Awake prone positioning and
of a slight Trendelenburg bed inclination helps in achieving oxygen therapy in patients with COVID-19: the APRONOX
optimal patient positioning. study. Eur Respir J. 2021;15:2100265. doi:10.1183/13993003.
00265-2021.
Another positive aspect of this new technique con- 10. González-Seguel F, Pinto-Concha JJ, Aranis N, Leppe J. Adverse
cerns the patient's visual area. During normal PP, patients events of prone positioning in mechanically ventilated adults with
undergoing helmet CPAP had limited vision, and often, acute respiratory distress syndrome. Intensive Crit Care Nurs.
2021;66:103064.
they could only see the wall in front of them. With the 11. Bruni A, Garofalo E, Longhini F. Avoiding complications during
head positioned on the bed foot area, the patients in the prone position ventilation. Intensive Crit Care Nurs. 2021;66:
prone position had a better view, being able to observe 103064. doi:10.1016/j.iccn.2021.103064.
12. Longhini F, Bruni A, Garofalo E, et al. Helmet continuous posi-
the entrance to the hospital room, in the general wards. tive airway pressure and prone positioning: a proposal for an
We have treated more than 50 patients outside the ICU. early management of COVID-19 patients. Pulmonology. 2020;
Unfortunately, its simplicity and the immediate comfort 26(4):186-191. doi:10.1016/j.pulmoe.2020.04.014.
13. Lucchini A, Giani M, Isgrò S, Rona R, Foti G. The "helmet bun-
communicated by the patients did not allow us to collect dle" in COVID-19 patients undergoing noninvasive ventilation.
comparison data with the old technique. All the nurses Intensive Crit Care Nurs. 2020;58:102859. doi:10.1016/j.iccn.
and patients to whom it was proposed no longer wanted 2020.102859.
14. Coppadoro A, Benini A, Fruscio R, et al. Helmet CPAP to treat
to apply the conventional technique. hypoxic pneumonia outside the ICU: an observational study during
the COVID-19 outbreak. Crit Care. 2021;25:80. doi:10.1186/
s13054-021-03502-y.
CONCLUSIONS 15. Lucchini A, Giani M, Elli S, Villa S, Rona R, Foti G. Nursing Ac-
tivities Score is increased in COVID-19 patients. Intensive Crit
In conclusion, we show that “the dolphin prone position-
Care Nurs. 2020;59:102876. doi:10.1016/j.iccn.2020.102876.
ing” is feasible outside the critical care environment in most 16. Rezoagli E, Villa S, Gatti S, et al. Helmet and face mask for non-
patients, is safe, and might improve patients' comfort in invasive respiratory support in patients with acute hypoxemic
respiratory failure: a retrospective study. J Crit Care. 2021;65:
COVID-19, making it an alternative or adjunct to standard
56-61. doi:10.1016/j.jcrc.2021.05.013.
PP to maintain safe oxygenation. It is our intention to de-
sign a study to compare 2 techniques. We think this small ABOUT THE AUTHORS
report could help nurses to perform PP in awake patients
Alberto Lucchini, RN, is a head nurse, General Intensive Care Unit,
undergoing helmet CPAP or NIV.
Emergency Department, ASST Monza - San Gerardo Hospital; and
University of Milano-Bicocca, Italy.
References Dario Minotti, CCN-RN, General Intensive Care Unit, Emergency
1. Taccone P, Pesenti A, Latini R, et al. Prone positioning in patients Department, ASST Monza - San Gerardo Hospital; and University of
with moderate and severe acute respiratory distress syndrome: a Milano-Bicocca, Italy.
randomized controlled trial. JAMA. 2009;302:1977-1984. doi:
10.1001/jama.2009.1614. Stefania Vanini, CCN-RN, General Intensive Care Unit, Emergency
2. Guérin C, Reignier J, Richard J-C, et al. Prone positioning in se- Department, ASST Monza - San Gerardo Hospital; and University of
vere acute respiratory distress syndrome. N Engl J Med. 2013; Milano-Bicocca, Italy.
368:2159-2168. doi:10.1056/NEJMoa1214103.
3. Guérin C, Albert RK, Beitler J, et al. Prone position in ARDS pa-
Flavia Pegoraro, CCN-RN, General Intensive Care Unit, Emergency
tients: why, when, how and for whom. Intensive Care Med. 2020; Department, ASST Monza - San Gerardo Hospital; and University of
46:2385-2396. doi:10.1007/s00134-020-06306-w. Milano-Bicocca, Italy.
November/December 2021 313
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.
Luigi Iannuzzi, RN, General Intensive Care Unit, Emergency Department, The authors have disclosed that they have no significant relationship with,
ASST Monza - San Gerardo Hospital; and University of Milano-Bicocca, or financial interest in, any commercial companies pertaining to this article.
Italy. Address correspondence and reprint requests to: Alberto Lucchini, RN,
Stefano Isgrò, MD, Medical Emergency Team, Emergency Department, General Intensive Care Unit, San Gerardo Hospital – ASST Monza, Milan-
ASST Monza - San Gerardo Hospital; and University of Milano-Bicocca, Bicocca University, Via Pergolesi 33, Monza (MB), Italy (alberto.lucchini@
Italy. unimib.it; a.lucchini@asst-monza.it).
All authors have approved the final article that all those entitled to
authorship are listed as authors. Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.
Call for
Manuscripts
If you are a critical care nurse, nurse educator, nurse manager, nurse practitioner, clinical nurse
specialist, researcher, other healthcare professional, or knowledgeable about topics of interest
to critical care nurses, Dimensions of Critical Care Nursing would like to hear from you.
We are seeking manuscripts on innovative critical care topics with direct application to
clinical practice, leadership, education, or research. We are also interested in any topic related
to quality, safety, and healthcare redesign. Specifically, we are interested in manuscripts on
the latest critical care technology, drugs, research, procedures, leadership strategies, ethical
issues, career development, and patient/family education.
Do not submit articles that have been previously published elsewhere or are under
consideration for publication in other journals or books.
Send your query letter, outline or manuscript to:
Dimensions of Critical Care Nursing
Kathleen Ahern Gould, PhD, RN
Editor-in-Chief
Dimensions of Critical Care Nursing
dccneditor@wolterskluwer.com
For more specific author guidelines, visit our Web site: www.dccnjournal.com
Thank you for your interest in DCCN. We will make every effort to be sure you are satisfied
with the service you receive from us!
DOI: 10.1097/01.DCC.0000795228.10781.fa
314 Dimensions of Critical Care Nursing Vol. 40 / No. 6
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.
You might also like
- Gibbs2020 2Document14 pagesGibbs2020 2Dan ZhouNo ratings yet
- Combination of Preoperative ProgressivePneumoperitoneum and Botulinum Toxin A Enablesthe Laparoscopic Transabdominal Preperitoneal Approachfor Repairing Giant Inguinoscrotal Hernias 2020Document7 pagesCombination of Preoperative ProgressivePneumoperitoneum and Botulinum Toxin A Enablesthe Laparoscopic Transabdominal Preperitoneal Approachfor Repairing Giant Inguinoscrotal Hernias 2020carlos.alberto.palacios.serratNo ratings yet
- Intensive & Critical Care Nursing: M. Sanz-Moncusí, J. Rosselló-Sancho, J.M. Garcia-AlaminoDocument3 pagesIntensive & Critical Care Nursing: M. Sanz-Moncusí, J. Rosselló-Sancho, J.M. Garcia-AlaminoJimena Vásquez RodríguezNo ratings yet
- Efficiency of Prolonged Prone Positioning For Mechanically Ventilated Patients Infected With COVID-19Document11 pagesEfficiency of Prolonged Prone Positioning For Mechanically Ventilated Patients Infected With COVID-19Riyan NuelNo ratings yet
- Preoperative PhysiotherapyDocument15 pagesPreoperative PhysiotherapysstavrosNo ratings yet
- TMP 392 FDocument4 pagesTMP 392 FFrontiersNo ratings yet
- Grafica 2 BiennDocument16 pagesGrafica 2 Biennwincu roNo ratings yet
- JournalDocument6 pagesJournalTri Setya NingrumNo ratings yet
- Task No 1. La Ode Muhammad Ady Ardyawan - 2022-02-0412Document4 pagesTask No 1. La Ode Muhammad Ady Ardyawan - 2022-02-0412Ardyawan Adry VjNo ratings yet
- Prone Position in Patients With Acute Respiratory Distress SyndromeDocument11 pagesProne Position in Patients With Acute Respiratory Distress SyndromeduckjqtNo ratings yet
- Archives Review Article 2019Document7 pagesArchives Review Article 2019Harpreet SinghNo ratings yet
- Commentary On The First Line Support For.16Document5 pagesCommentary On The First Line Support For.16shubham2812No ratings yet
- Airway Management in The Critically Ill: ReviewDocument9 pagesAirway Management in The Critically Ill: ReviewQuarmina HesseNo ratings yet
- Highlights Clinical Checklist (Wearing Ppe) : Tube Position Control - Protective VentilationDocument1 pageHighlights Clinical Checklist (Wearing Ppe) : Tube Position Control - Protective VentilationIacriNo ratings yet
- Prone Position in Adult Critical Care 2019 PDFDocument40 pagesProne Position in Adult Critical Care 2019 PDFKuroi RavenNo ratings yet
- Pediatric Pulmonology 2021, Dell'ortoDocument8 pagesPediatric Pulmonology 2021, Dell'ortoRadu CiprianNo ratings yet
- Feasib in TelereDocument3 pagesFeasib in TelereNelson LoboNo ratings yet
- Beclomethasone/formoterol Versus Budesonide/formoterol Combination Therapy in AsthmaDocument8 pagesBeclomethasone/formoterol Versus Budesonide/formoterol Combination Therapy in AsthmalalaNo ratings yet
- 156 JCardiopulmRehabilPrev 2020Document4 pages156 JCardiopulmRehabilPrev 2020Ruby FirdausNo ratings yet
- GIZZI 2012 - Surfactant and Non Invasive Ventilation For Preterm InfantsDocument4 pagesGIZZI 2012 - Surfactant and Non Invasive Ventilation For Preterm InfantsRafael JustinoNo ratings yet
- Post Extubation Stridor UHL Paediatric Intensive Care GuidelineDocument6 pagesPost Extubation Stridor UHL Paediatric Intensive Care Guidelineandreea.spasenieNo ratings yet
- 390 FullDocument28 pages390 FullsukiyantoNo ratings yet
- Guidance For Prone Positioning in Adult Critical CareDocument40 pagesGuidance For Prone Positioning in Adult Critical CareAnnisa Eka FebryantiNo ratings yet
- Review: The Changing Face of Pneumonia Maids PatientsDocument9 pagesReview: The Changing Face of Pneumonia Maids Patientsmail junkNo ratings yet
- Economic Evaluation Alongside The Probiotics To Prevent Severe Pneumonia and Endotracheal Colonization Trial (E-PROSPECT) : Study ProtocolDocument8 pagesEconomic Evaluation Alongside The Probiotics To Prevent Severe Pneumonia and Endotracheal Colonization Trial (E-PROSPECT) : Study ProtocolSharan SahotaNo ratings yet
- Anesthesia For Advanced Bronchoscopic Procedures: State-of-the-Art ReviewDocument13 pagesAnesthesia For Advanced Bronchoscopic Procedures: State-of-the-Art ReviewRichard PhoNo ratings yet
- Daytime Alternatives For Non-Invasive Mechanical Ventilation in Neuromuscular DisordersDocument10 pagesDaytime Alternatives For Non-Invasive Mechanical Ventilation in Neuromuscular DisordersL ANo ratings yet
- Articulo Tesis 9Document8 pagesArticulo Tesis 9Lourdes MarcosNo ratings yet
- Guia Fisioterapia en UPCDocument11 pagesGuia Fisioterapia en UPCPatricio Romero MartinezNo ratings yet
- Synchronized Nasal Intermittent Positive Pressure Ventilation of The Newborn: Technical Issues and Clinical ResultsDocument7 pagesSynchronized Nasal Intermittent Positive Pressure Ventilation of The Newborn: Technical Issues and Clinical ResultsMaluNo ratings yet
- ICU-acquired Pneumonia: Is It Time To Use This Term?: EditorialDocument2 pagesICU-acquired Pneumonia: Is It Time To Use This Term?: EditorialkenniNo ratings yet
- Lerman 2019Document6 pagesLerman 2019Dany Azzam ArdianNo ratings yet
- Ophthalmological Care Management of Cataract.16Document1 pageOphthalmological Care Management of Cataract.16library SDHBNo ratings yet
- Perioperative ERAS Approach Defining The Role of Desflurane - Slide Deck FinalDocument69 pagesPerioperative ERAS Approach Defining The Role of Desflurane - Slide Deck FinalHelmiHassanNo ratings yet
- Peritoneal Dialysis in Critically Ill Patients .17Document9 pagesPeritoneal Dialysis in Critically Ill Patients .17miguel aghelNo ratings yet
- Core Clinical Content For Postgraduate Anaesthetic Training and Continuing Professional DevelopmentDocument50 pagesCore Clinical Content For Postgraduate Anaesthetic Training and Continuing Professional DevelopmentAbeNo ratings yet
- Non-Invasive Positive Pressure Ventilation in Acute Respiratory Failure: Providing Competent CareDocument9 pagesNon-Invasive Positive Pressure Ventilation in Acute Respiratory Failure: Providing Competent CareAndana TrisaviNo ratings yet
- Advances in Interventional Diagnostic Bronchoscopy For Peripheral Pulmonary LesionsDocument15 pagesAdvances in Interventional Diagnostic Bronchoscopy For Peripheral Pulmonary LesionsAlaaNo ratings yet
- A National Survey of The Diagnosis and Management of Suspected Ventilator-Associated PneumoniaDocument12 pagesA National Survey of The Diagnosis and Management of Suspected Ventilator-Associated PneumoniamochkurniawanNo ratings yet
- Ask The Experts: Evidence-Based Practice: Percussion and Vibration TherapyDocument3 pagesAsk The Experts: Evidence-Based Practice: Percussion and Vibration Therapysebastian arayaNo ratings yet
- Advances and Perspectives in The Use of Carbon Nanotubes in Vaccine DevelopmentDocument25 pagesAdvances and Perspectives in The Use of Carbon Nanotubes in Vaccine DevelopmentEEEEEE EEEEEEENo ratings yet
- Flow Matters: Clinical Practice GuidelinesDocument3 pagesFlow Matters: Clinical Practice GuidelinesThanh TrầnNo ratings yet
- Fenotipos Displasia BroncopulmonarDocument21 pagesFenotipos Displasia BroncopulmonarCarolina GarcíaNo ratings yet
- Zhu 2023 Oi 230637 1687872003.91163Document15 pagesZhu 2023 Oi 230637 1687872003.91163Lucia NiculaeNo ratings yet
- Pediatric Anesthesia - 2010 - MANI - Overview of Total Intravenous Anesthesia in ChildrenDocument12 pagesPediatric Anesthesia - 2010 - MANI - Overview of Total Intravenous Anesthesia in ChildrenRAGHU NATH KARMAKERNo ratings yet
- P 194 14icml-1Document1 pageP 194 14icml-1shaza elkourashyNo ratings yet
- Neumonã A Neonatal Severa Por Legionella-579Document6 pagesNeumonã A Neonatal Severa Por Legionella-579Mirna Karime Gar CerNo ratings yet
- Anesthesia For Tracheolaryngeal Surgeries ENTDocument6 pagesAnesthesia For Tracheolaryngeal Surgeries ENTMaryamMahmoodNo ratings yet
- 238 FullDocument10 pages238 FullJorge CastroNo ratings yet
- COVID-19 Management in HongKongDocument1 pageCOVID-19 Management in HongKongShahzad KamranNo ratings yet
- JIR 306849 N Acetylcysteine As Adjuvant Therapy For Covid 19 Ndash ADocument21 pagesJIR 306849 N Acetylcysteine As Adjuvant Therapy For Covid 19 Ndash ARefa OktoyardaNo ratings yet
- 191 1 FullDocument1 page191 1 FullburhanNo ratings yet
- Non-Invasive Ventilation in Acute Respiratory Failure: Bts GuidelineDocument21 pagesNon-Invasive Ventilation in Acute Respiratory Failure: Bts GuidelineddubbNo ratings yet
- Renal Doppler Based Assessment of Regional Organ.18Document2 pagesRenal Doppler Based Assessment of Regional Organ.18Mario TGNo ratings yet
- Paediatric Total Intravenous Anaesthesia BJA 2016Document5 pagesPaediatric Total Intravenous Anaesthesia BJA 2016RicardoNo ratings yet
- Prevention of VAP Use For Bundle Approach 10.1016@j.ajic.2016.04.237Document4 pagesPrevention of VAP Use For Bundle Approach 10.1016@j.ajic.2016.04.237sarintiNo ratings yet
- WRIGHT 2016 - Continuous Positive Airway Pressure To Prevent Neonatal Lung InjuryDocument10 pagesWRIGHT 2016 - Continuous Positive Airway Pressure To Prevent Neonatal Lung InjuryRafael JustinoNo ratings yet
- 08 AE 5585 Crespo IngDocument3 pages08 AE 5585 Crespo Ingcarlosalayon2No ratings yet
- Non Invasive HFO Time For Consideration 2017Document3 pagesNon Invasive HFO Time For Consideration 2017OsmanyNo ratings yet
- PL SQLDocument12 pagesPL SQLIsha ThakreNo ratings yet
- PESTEL Analysis of NigeriaDocument3 pagesPESTEL Analysis of NigeriaSUHANI JAIN 2023275No ratings yet
- Ejectment Complaint With Judicial AffidavitDocument15 pagesEjectment Complaint With Judicial AffidavitMichael Parreño Villagracia94% (16)
- EE-211 Circuit Analysis: Dr. Hadeed Ahmed SherDocument28 pagesEE-211 Circuit Analysis: Dr. Hadeed Ahmed SherHadeedAhmedSherNo ratings yet
- BCA2 DbmsnotesDocument96 pagesBCA2 DbmsnotesMohd TausifNo ratings yet
- 02 - Syllabus Property Discussion GuideDocument67 pages02 - Syllabus Property Discussion GuideGianna CantoriaNo ratings yet
- Cu Dan EcoparkDocument248 pagesCu Dan Ecoparktomtem50% (2)
- Italian in 30 Days - The WorkbookDocument254 pagesItalian in 30 Days - The WorkbookMariia Okseniuk100% (8)
- Tube and CouplerDocument1 pageTube and CouplerShams TabrezNo ratings yet
- Globelics Athens 2017 Program BookletDocument60 pagesGlobelics Athens 2017 Program BookletIsrael Sanches Marcellino100% (1)
- Challenges of Transmission System Operation During The NATO Bombing of The Republic of SerbiaDocument62 pagesChallenges of Transmission System Operation During The NATO Bombing of The Republic of SerbiakeramicarNo ratings yet
- Ford Ranger ManualDocument266 pagesFord Ranger ManualHerWagner100% (9)
- Mara Et Al. - 2020 - Strategies For Coping With LGBT Discrimination atDocument16 pagesMara Et Al. - 2020 - Strategies For Coping With LGBT Discrimination atRMADVNo ratings yet
- Resume Kevin WaldronDocument2 pagesResume Kevin WaldronKevin WaldronNo ratings yet
- CB2203 2023-24 Sem B Assignment 2Document3 pagesCB2203 2023-24 Sem B Assignment 2c wan cheungNo ratings yet
- Calculated Uncertainty of Temperature Due To The Size-of-Source EffectDocument8 pagesCalculated Uncertainty of Temperature Due To The Size-of-Source EffectRONALD ALFONSO PACHECO TORRESNo ratings yet
- Research Qualitative FormatDocument2 pagesResearch Qualitative FormatNHELBY VERAFLOR100% (1)
- 05-21 Captoday NGSDocument4 pages05-21 Captoday NGSImam Al-DoaibesNo ratings yet
- G.R. No. 171951 Garcia V People CDDocument2 pagesG.R. No. 171951 Garcia V People CDLester Fiel PanopioNo ratings yet
- Welding Safety: Lesson 1Document9 pagesWelding Safety: Lesson 1cyrelle rose jumentoNo ratings yet
- PM Project CharterDocument8 pagesPM Project CharterMuhammad AididNo ratings yet
- 03 Ot-1Document15 pages03 Ot-1umang.parmar112597No ratings yet
- Peñablanca, Cagayan: Medical Colleges of Northern PhilippinesDocument2 pagesPeñablanca, Cagayan: Medical Colleges of Northern PhilippinesKaren mae alvarroNo ratings yet
- PPL (H) : Part-FCL Question BankDocument25 pagesPPL (H) : Part-FCL Question BankChance 101No ratings yet
- DAN Aluform PresentationDocument38 pagesDAN Aluform PresentationahsNo ratings yet
- Design of Compact 180 Degree Hybrid Coupler Using T-Shape StructureDocument5 pagesDesign of Compact 180 Degree Hybrid Coupler Using T-Shape StructureEmerson Eduardo Rodrigues SetimNo ratings yet
- D4N Mini Safety Limit Switch C130 E1 01 DsDocument24 pagesD4N Mini Safety Limit Switch C130 E1 01 DsciprianNo ratings yet
- Ryzen Price 22 08 15Document3 pagesRyzen Price 22 08 15Jhover BernalNo ratings yet
- Keyman Insurance Lic India PolicyDocument2 pagesKeyman Insurance Lic India PolicyPriyanka KumariNo ratings yet
- Curtiss Wright February2017 BulletinDocument60 pagesCurtiss Wright February2017 Bulletinal marmokaNo ratings yet