Professional Documents
Culture Documents
Management of Duodenal Injuries
Uploaded by
Zam Hus0 ratings0% found this document useful (0 votes)
17 views11 pagesOriginal Title
Management of Duodenal injuries
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
17 views11 pagesManagement of Duodenal Injuries
Uploaded by
Zam HusCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 11
Presentation transcript:
Management of Duodenal Trauma Dr. Chow Chi Woo Samuel Department of
Surgery, Queen Elizabeth Hospital
Introduction Duodenal trauma is uncommon D2 most common (35%) 3-5% D2 most
common (35%) > D3 > D4 > D1 Penetrating trauma (78%) Gunshot wounds Stab
wounds Blunt trauma (22%) Motor vehicle collisions Steering wheel Seatbelt Bicycle
handle (paediatrics) Duodenal trauma is uncommon According to literature, it is found
in 3-5% of abdominal traumas D2 is most commonly involved and constitutes 1/3 of
the duodenal injuries, followed by D3, D4 and D1 They are most caused by
penetrating injuries while blunt injuries are less common Associated injuries are
common, esp those related to the pancreas, bile ducts, liver and bowel (usually 1-4
more organs injured) Morbidity is up at 40% and the rate of duodenal fistula (one of
the most important morbidities) is around 7% Mortality is as high at 17%
Introduction Associated injuries are common High mortality (17%) Liver Pancreas
Bowel Major vessels High mortality (17%) High morbidity (40%) Duodenal fistula
(7%)
Intra-operative features Diagnosis High index of suspicion Symptoms/signs usually
not helpful Blunt trauma Radiological Imaging 1. X-ray 2. CT scan (IV + oral
contrast) 3. Fluoroscopy Penetrating trauma Intra-operative features 1. Bile staining at
retroperitoneum 2. Periduodenal hematoma 3. Periduodenal crepitus The diagnosis of
duodenal trauma remains a challenge and requires a high index of suspicion
Symptoms/signs are usually non-specific/minimal and not helpful Relevant trauma
history, positive radiological findings and positive intra-operative features offer
important clues to help diagnose duodenal trauma For history, Penetrating injuries are
usually a result of gunshot or stab wounds Blunt injuries are usually found in motor
vehicle accidents in which the abdomen collides with the steering wheel or bicycle
handle injuries in children Occasionally, they can also be a result of fist injuries For
imaging, XR, CT and fluroscopy are important investigations for blunt duodenal
trauma. CT is the modality of choice, although it can still miss injuries, up to 20% in 1
series Intra-operative features are the mainstay of evaluation for penetrating trauma
and offer the ultimate clue for diagnosis. Positive features include bile staining of the
retroperitoneum and the presence of periduodenal hematoma/ entrapped air bubbles
These are some CTs taken for patients with duodenal trauma The left one shows
transection of D3 The upper right one shows perforation of the lateral D2 wall with
persence of periduodeanl gas The lower right one shows periduodeanl gas with
extravasation of oral contrast
Management Patient factors Disease factors 1. Hemodynamic stability 1. Severity of
injury 2. Associated injuries Now that we have an idea of how to diagnose duodenal
trauma how do we manage it Back to basics The management of duodenal trauma
(like all other conditions) depends on patient factors and disease factors For patient
factors, the hemodynamic status is very important, as I will further elaborate later For
disease factors, the severity of injury and the presence of associated injuries have a
signfiicant impact on management
Grading of Severity Duodenum Organ Injury Scale (OIS) according to The American
Association for the Surgery of Trauma (AAST) Grade Description I Hematoma
Laceration 1 portion of duodenum Partial thickness, no perforation II >1 portion of
duodenum < 50% of circumference III 50-75% of circumference of D2 50-100% of
circumference of D1, 3, 4 IV >75% of circumference of D2 Involve ampulla or distal
CBD V Vascular Duodenopancreatic complex Devascularization of duodenum With
regards to the severity of duodeanl injuries One of the most commonly used grading
systems is the duodenum organ injury scale devised by the American Association for
the Surgery of Trauma There are 5 gradings (I being mildest and V being most
severe). The grading system is based on the nature of the duodenal injury, the extent
of injury, the location of injury and the presence of invovlement of the
biliary/pancreatic system Another grading system is the duodenal severity scale,
which can be divided into and mild and severe and also takes into account the time
interval from injury to repair.
Temporary abdominal closure Damage control Control hemorrhage Provisional repair
Temporary abdominal closure ICU resuscitation Unstable Operative Hemodynamic
stability is one of the most important parameters in guiding management Unstable
patients (shock), should be brough to the operating theatre as soon as possible and
damage control surgery should be done. After stabilization, delayed repair should
follow Delayed repair
Stable 1. Hemorrhage control 2. Decontamination 3. Repair In stable patients, the
story is completely different For penetrating injuries, they should be brought to the
operating theatre for hemorrhage control, decontamination and repair For blunt
injuries, they should get a CT scan. If the CT scan shows an intramural hematoma,
non-operative treatment should be established with NG tube suction and TPN,
However, if the CT scan shows findings suggestive of a perforation, operative
treatment should be adopted. If the CT scan shows equivocal findings, operative
treatment or re-evaluation CT should be done, depending on degree of suspicion -----
Meeting Notes (21/4/16 14:26) ----- colour scheme Perforation 1. Hemorrhage control
2. Decontamination 3. Repair * Associated injuries Penetrating Operative
Intramural hematoma Non-operative Blunt CT scan Equivocal Perforation Stable In
stable patients, the story is completely different For penetrating injuries, they should
be brought to the operating theatre for hemorrhage control, decontamination and
repair For blunt injuries, they should get a CT scan. If the CT scan shows an
intramural hematoma, non-operative treatment should be established with NG tube
suction and TPN, However, if the CT scan shows findings suggestive of a perforation,
operative treatment should be adopted. If the CT scan shows equivocal findings,
operative treatment or re-evaluation CT should be done, depending on degree of
suspicion ----- Meeting Notes (21/4/16 14:26) ----- colour scheme Perforation 1.
Hemorrhage control 2. Decontamination 3. Repair * Associated injuries Operative
Repair Simple Complex Aim Always ascertain location of ampulla (D2) Close the
defect Restore continuity Always ascertain location of ampulla (D2) Options
Duodenorrhaphy Duodenorrhaphy + diversion Duodenal resection + anastomosis
Jejunal serosal patch Pedicled graft Whipple operation Simple The aim of repair for
duodenal trauma is to close the defect and restore intestinal continuity Options from
simple to complex includes duodenorrhaphy, duodenorrhpahy with diversion,
duodenal resection and anastomosis, jejunal serosal patch in which the serosa of the
jejunum is used to buttress the defect, pedicled graft in which a mesenteric border of a
segment of jejunum with a vascular pedicle is use to patch up the defect, and Whipple
operation, which is the last resort for severe duodenopancratic injuries and carries a
very high mortality. Complex
Duodenorrhaphy 75-85% of duodenal injuries Debride non-viable tissue Tension-free
repair Single/double layer closure Transverse closure < 50% of circumference
Duodenorrhaphy is used to manage up to 85% of all duodenal injuries It comprises
adequate debridement of non-viable followed by tension free repair. The defect is
closed in single/double layer and ideally transversely to avoid stricture Also, its best
when the injuries are < 50% circumference This cartoon shows how a longitudinal
laceration is repaired in a transverse manner
Duodenorrhaphy + Diversion Indication High risk of suture line dehiscence Delayed
injury Large defect Combined injury Aim Divert gastric secretions Promote healing
Options Tube decompression Pyloric exclusion Duodenal diverticulization
Duodenorrhpahy with diversion is often used for to lesions at risk of suture line
dehiscence These include high grade injuries with large defects/combined
duodenopancreatic injuries, as well as delayed injuries The aim of diversion to
exclude the duodenum from the passage of gastric contents rich in bile juice and
pancreatic juice, thereby buying time for the duodenum to heal and to prevent suture
line dehiscence Options of diversion from simple to complex would include tube
decompression, pyloric exlcusion and duodenal diverticulization Simple Complex
Tube decompression External diversion Tube decompression is placement of an
intraluminal tube for external diversion of gastric secretions It can be primary in the
duodenum as shown in the diagram, or antegrade in the stomach proximal to the
repair, or retrograde in the jejunum distal to the repair Triple ostomy technique is
shown in the cartoon on the right, which shows a diversion gastrostomy, a diversion
jejunostomy and a feeding jejunostomy. This technique was first described by stone
and fabian in 1970s,
Pyloric exclusion Internal diversion Pyloric exlcusion was first described by Jordan in
1970s Operative steps include creating a gastrostomy, closing the pylorus via the
gastrostomy with sutures/staple, and finally using the gastrostomy to build a side-to-
side GJ 94% of the pylorus restores patency by 3 weeks time It is a type of internal
diversion in which gastric secretions are diverted through a GJ and the suture line is
protected via a closed pylorus
Duodenal Resection + Anastomosis Large duodenal defects (near-circumferential)
Duodenal transections Segmental resection with end-to-end duodenostomy Adequate
mobilization, tension-free Duodenal resection and anastomosis is suitable for large
near-circumferential duodenal defects and duodenal transections The specific type of
repair depends on the location and the resultant tension of the suture ends As a thumb
of rule, if the duodenum can be mobilize adequately and the sutures ends are tension
free, segmental resection with end to end duodenostomy can be done as shown in the
cartoon on the upper right corner. This type of repair is applicable to lesions in D1,
D3, D4 If the duodenum cannot be mobilized adequately and the sutures ends are at
tension, the distal duodenum should be oversewn and the proximal duodenum should
be used to form a Roux-en-Y end-to-end duodenojejunostomy as shown in the cartoon
on the lower right corner. Alternatively a roux-en-Y side to side duodenojejunostomy
can be done. This type of repair is applicable to lesions at D2, in which mobilization
can be difficult and dangerous due to close proximity to the biliary/pancreatic system,
thereby minimizing disruption of the biliary/pancreatic system
Closure of duodenal stump + end-to-end duodenojejunostomy Antrectomy + closure
of duodenal stump + side-to-side gastrojejunostomy Inadequate mobilization Proximal
to ampulla Closure of duodenal stump + end-to-end duodenojejunostomy Distal to
ampulla
Which repair is the best? Now that we have a whole list of different types of repair
The question is which repair is the best?
Which repair is the best? Low grade injuries For the low grade injuries (Grade 1 and
2) Duodenorrhaphy is a well-accepted safe modality of repair with low complication
Duodenorrhaphy
Which repair is the best? High grade injuries 1. Involve CBD/pancreas 2.
Devascularization Repairable Non-repairable For high grade injuries the picture is
more complicatied for repairable lesions, duodenorrhaphy with diversion or
duodenorrhaphy can be done for non-repairable lesions, duodenal resection with
anastomosis, jejunosal serosal patch or pedicled graft can be done for those lesions
involving biliary/pancreatic system or devasculization injury, treatment is often very
complicated. Possible options include duodenorrhaphy with diversion and wide
drainage, reimplantation of CBD, reconstruction with HJ or in extreme cases whipple
operation 1. Damage Control Surgery + delayed reconstruction 2. Duodenorrhaphy +
diversion + wide drainage Delayed reconstruction 1. Reimplantation of CBD 2.
Hepaticojejunostomy 3. Whipple operation 1. Duodenorrhaphy + diversion 2.
Duodenorrhaphy 1. Duodenal Resection + anastomosis 2. Jejunal serosal patch 3.
Pedicled graft
High grade repairable injuries Optimal repair remains debatable Duodenorrhaphy +
pyloric exclusion Classically recommended (Vaughan, Degiannis, Cogbill) Problems
Increased operative time and hospital stay, extra anastomosis, suture line ulcers Role
downplayed (Seamon) Duodenorrhaphy + tube decompression Controversial (Stone,
Hasson, Ivatury, Girgin) Increased hospital stay, dislodgement, obstruction
Duodenorrhaphy Gaining popularity (DuBose, Velmahos, Siboni) Concept of “less is
better” Duodenorrhaphy Pyloric exclusion For high grade repairable injuries the
optimal repair for high grade repairable injuries is a debatable topic Duodenorrhaphy
+ pyloric exclusion is classically recommended by many authors including Vaughan
who showed a low fistula rate (5%) in 75 patients treated with pyloric exclusion,
Degiannis who showed a lower fistula rate in pyloric exclusion compared to primary
repair in a total of 31 patients with severe duodenal trauma, cogbill who showed a low
mortality rate with the use of pyloric exclusion in 27 patients. However it has been
criticized for its increased OT time and hospital stay, the formation of an extra
anastomosis and the risk of suture line ulcers Duodenorrhaphy + tube decompression
has always been controversial. While authors like stone (237 patients, 0.5% fistula
rate vs 19.3%) and hasson (9% mortality and 2.3% fistual rate vs 19.4% and 11.8%)
have supported tube compression by showing lower mortality rate and fistula rate
when comparing with those without decompression, others like Ivatury (60 patients,
comparing primary repair with tube duodenostomy) and Girgin (67 patients,
comparing primary repair and tube duodenostomy) questioned its role. Ivatury
showed increased mortality and morbidity while Girgin showed no benefit in outcome
with increased hospital stay. Problems of an additional tube would include increased
hospital stay, tube dislodgement and obstruction Duodenorrhaphy was never a popular
choice for high grade injuries in the past. However, in recent years it has gained
popularity with the introduction of the concept of less is better Duodenorrhaphy
Mainstay for low grade injuries Emerging role for high grade injuries Siboni et al.
2015 2220 patients with isolated blunt duodenal injuries No difference in mortality
and sepsis (PR vs GE) Shorter hospital stay Pyloric exclusion Mainstay for high grade
injuries Role downplayed Seamon et al. Greater complication rate, pancreatic fistula
rate and increased hospital stay in PE group Velmahos et al. No difference in
morbdiity/mortality/ICU/hospital stay (PE vs PR) DuBose et al. PE contribute to
longer hospital stay and confers no survival/outcome benefit
What else…… Feeding jejunostomy Periduodenal drains Early enteral nutrition
Periduodenal drains Closed suction drain Controlled fistula No level I evidence
Surgeon preference So what else can we do intra-operatively Feeding jejunostomy can
be done to ensure early enteral nutrition, esp for patients who are anticipated to fast
for a longer period of time this is esp important for trauma patients who are in a
severe catabolic state and require good nutrititional support for recovery Periduodenal
drains if placed, should be closed suction drains. By far, there is no level I evidence to
support or refute its use The benefit of it is it can act as a controlled fistula in case of
leakage. Ultimately, its use depends on surgeon preference
Summary Duodenal trauma is DEADLY and requires a HIGH INDEX OF
SUSPICION for diagnosis Management depends on HEMODYNAMICS, INJURY
SEVERITY and ASSOCIATED INJURIES DUODENORRHAPHY is good enough
for most injuries – keep it simple, but consider DIVERSION when in doubt Never
forget DAMAGE CONTROL To conclude my presentation I hope that you can bring
with you these few take home messages First, management of duodenal trauma is
challenging. Diagnosis is not easy, most decisions are made on table, morbidity and
mortality are high, operation is technically demanding. Second, surgical treatments
are diverse with no gold standard. The complexity of treatments are highly variable
Third, unstable patients require damage control surgery. This is important, bearing in
mind saving the patient is more important than doing a perfect repair Fourth, most
injuries can be managed with duodenorrhaphy. with its well-documented role in low
grade injuries and emerging role in high grade injuries, Fifth, the management of high
grade injuries sometimes require complex repair, including pyloric exclusion,
resection and anastomoses or even whipple Last but not least, treatment must be
individualized and catered to the patient’s best interest. ----- Meeting Notes (21/4/16
14:26) ----- Outline Summary Background Seat belt
References Vaughan GD, Frazier OH, Graham DY, et al.. The use of pyloric
exclusion in the management of severe duodenal injuries. Am J Surg.
1977;134(6):785-90. Degiannis E, Krawczykowski D, Velmahos GC, et al. Pyloric
exclusion in severe penetrating injuries of the duodenum. World J Surg.
1993;17(6):751-4 Cogbill T H, Moore E E, Feliciano D V. et al. Conservative
management of duodenal trauma: a multicenter perspective. J Trauma.
(1990);30:1469–1475. Seamon MJ, Pieri PG, Fisher CA, et al. A ten-year
retrospective review: does pyloric exclusion improve clinical outcome after
penetrating duodenal and combined pancreaticoduodenal injuries? J Trauma.
2007;62(4):829-33.Stone HH, Fabian TC. Management of duodenal wounds. J
Trauma 1979;19:334-9 Hasson JE, Stern D, Moss GS. Penetrating duodenal trauma. J
Trauma. 1984 Jun;24(6):471–474. Ivatury RR, Gaudino J, Ascer E, et al. Treatment of
penetrating duodenal injuries: primary repair vs. repair with decompressive enter-
ostomy/serosal patch. J Trauma 1985;25:337-41 Girgin S, Gedik E, Yağmur Y, et al.
Management of duodenal injury: our experience and the value of tube duodenostomy.
Ulus Travma Acil Cerrahi Derg. 2009;15:467-72. Siboni S, Benjamin E, Haltmeier T,
et al. Isolated Blunt Duodenal Trauma: Simple Repair, Low Mortality. Am Surg. 2015
Oct;81(10)961-4 Velmahos GC,Constantinou C,Kasotakis G. Safety of repair for
severe duodenal injuries. World J Surg 2008;32:7-12. DuBose JJ, Inaba K, Teixeira
PG, et al. Pyloric exclusion in the treatment of severe duodenal injuries: results from
the National Trauma Data Bank. Am Surg. 2008;74:925–9. Ivatury RR, Malhotra AK,
Aboutanos MB, et al. Duodenal Injuries: A Review. Eur J Trauma Emerg Surg
2007;33:231-7 Ordoñez C, García A, Parra MW, et al. Complex penetrating duodenal
injuries: less is better. J Trauma Acute Care Surg. 2014;76(5):1177-83. Am Surg.
2015 Oct;81(10):961-4. Isolated Blunt Duodenal Trauma: Simple Repair, Low
Mortality. Siboni S1, Benjamin E, Haltmeier T, Inaba K, Demetriades D.
Question Time
Radiological Imaging in abdominal xray we may see retroperitoneal gas or free gas
under diaphragm Both of the XRs are taken in patients with duodenal trauma For the
XR on the right, the red arrow illustates the presence of retroperitoneal gas, which
outlines the right psoas muscle whereas For the XR on the left, thewhite arrow
delineates the retroperitoneal gas, which outlines the right kidney
Less is better Damage control approach Duodenorrhaphy is advocated for high grade
injuries Siboni et al. 2015 2220 patients with isolated blunt duodenal injuries No
difference in mortality and sepsis Shorter hospital stay Velmahos et al. 2008 50
patients with severe duodenal injuries No difference in
morbidity/mortality/ICU/hospital stay DuBose et al. 2008 147 patients with severe
duodenal injuries No difference in survival/outcome Role of pyloric exclusion
downplayed Seamon et al. 2007 29 patients with duodenal injuries ≥ II Greater
complication rate, pancreatic fistula rate and increased hospital stay What is less is
better? In short, it means doing less may be more beneficial This is in line with the
damage control approach Duodenorrhaphy is advocated for high grade injuries as
shown in recent literature Siboni has shown that there is no difference in mortality and
sepsis in 2000 patients with isolated blunt duodenal injuries when treated with
duodenorrhaphy compared with the addition of a gastroenterostomy. Hospital stay
was also shorter. These findings are echoed by Velhamos and DuBose On the
contrary, the role of pyloric exclusion is downplayed Seamon demonstrated greater
complcation rate, pancreatic fistula rate and increased hospital stay in 29 patients with
severe duodenal injuries comparing duodenorrhpahy and pyloric exxlusion
Seemingly, recent studies have demonstrated a shift in the paradigm from
duodenpharrhphy with pyloric exlcusion to duodenorrphay alone as the repair of
choice for high grade duodenal injuries Schroeppel TJ et al 2016 Penetrating duodenal
trauma: A 19-year experience Primary suture repair should be the initial approach
considered for most injuries Siboni et al 2015 Isolated blunt duodenal trauma: Simple
Repair, Low Mortality Retro study Siboni on 3798 patients, database 2015 paper
(2220 with isolated duodenal injury) Compare primary repair and GE patients Seamon
MJ A ten-year retrospective review: does pyloric exclusion improve clinical outcome
after penetrating duodenal and combined pancreaticoduodenal injuries? J Trauma.
2007 Apr;62(4):829-33. Barone JE, Pyloric exclusion leads to a trend toward more
complications, a higher pancreatic fistula rate, and a longer hospital length of stay. J
Trauma. 2007 Sep;63(3):720 DuBose JJ, Demetriades D Pyloric exclusion in the
treatment of severe duodenal injuries: results from the National Trauma Data Bank.
Am Surg. 2008 Oct;74(10):925-9 Fraga Pyloric exclusion was associated with
multiple complictions and a high mortality rate Ivatury Duodenal injury review
Sriussadaporn Management of blunt duodenal injuries Jansen Duodenal injuries:
Surgical management adapted to circumstances Degiannis E et al. Pyloric exclusion in
severe penetrating injuries of the duodenum Cogbill Conservative management of
duodenal trauma: a multicenter perspective Martin TD Severe duodenal injuries.
Treatment with pyloric exlcusion and gastrojejunostomy Controversial Stone and
Fabian Lower rate of duodenal fistula 0.4% vs 18% (tube duodenostomy vs no tube
duodenostomy) Ivatury et al Higher rate of duodenal fistula 27.3% vs 1.6% (tube
duodenostomy vs no tube duodenostomy) Cogbill et al Tube duodenostomy
unnecessary and ineffective in preventing post-op complications
Duodenum 25-30cm (12 fingerbreaths) 4 parts Retroperitoneal 1st (Superior) 2nd
(Descending) Bile/pancreatic duct opening 3rd (Transverse) Mesenteric vessels 4th
(Ascending) Retroperitoneal Exception: 1st part 2cm Complex anatomical relations
25-30cm (12 fingerbreaths)
Blood supply Physiology Arterial Venous Pancreaticoduodenal artery Superior
(GDA) Inferior (SMA) Retroduodenal artery Supraduodenal artery Venous
Posterosuperior arcade portal vein Anteroinferior arcade SMV Physiology
Conduit for mixing of gastric juice/bile/pancreatic secretions 10L/day
Fluoroscopic studies Gastrograffin/barium follow through Features Leakage of
contrast “Stacked coin sign” (intramural hematoma) Limitation Timaran CH et al.
Sensitivity 54%, specificity 98% Difficult to interpret Series of 96 patients with CT
findings suspicious of duodenal injury
Delayed treatment Complex duodenal injury Drainage of abscess Inflammed and
unhealthy tissue Retroperitoneal abscess Drainage of abscess Retroperitoneal
laparostomy Pyloric exclusion + duodenostomy Controlled fistula Feeding
jejunostomy
Intramural hematoma Non-operative Stable CT scan Perforation Operative
Reconstruction Blunt Injury Unstable Operative Damage control
Management Algorithm These are two management algorithms for duodenal trauma
The right one is proposed by Moore while the left one is prposed by the western
trauma association As you can see, there are differences between the two I will not go
into details for each algorithm I just want to illustrate that by now, there is no
standardized treatment for duodenal trauma This is one of the management algorithms
proposed by Moore For patients with unstable hemodynamics or peritonitis,
laparotomy should be done For patients, which are stable and can undergo further
workup, CT/contrast studies should be done If findings suggestive of perforation,
laparotomy should be done while if duodenal hematoma is found, non-operative
treatment with NG suction and TPN can be done Following laparotomy Duodenal
injuries can be graded For grade I and II lesions, hematomas can either be managed
conservatively and evaucated if large lacerations are repaired by duodenorrhaphy For
grade III lesions, duodenrrhaphy and pyloric exclusion or roux-en-Y
jejunoduodenostomy should be performed For grade IV and V lesions, these patients
are often unstable and damage control surgery should be done first, they should then
be reassesed later for reconstruction or whipple It is noteworthy that that author is in
favour of the use of jejunostomy to ensure early enteral nutrition
Intramural hematoma More common in children Obstruction within 48 hours “Coiled
spring/stacked coin sign” NG tube suction + TPN Desai et al Success rate 89%
Czyrko et al Success rate 83% Failed conservative (2-3 weeks) exploration Involves
serosa/subserosa
Intramural hematoma If detected intra-operatively Evacuate hematoma and repair wall
Partial tear full thickness tear Explore and exclude perforation, leave hematoma
intact, nasogastric tube suction
Morbidity Asensio et al. Duodenal fistula Intra-abdominal abscess 7% Intra-
abdominal abscess 11-18% Pancreatitis 3-15% Duodenal obstruction 1-2% Bile duct
fistula 1% Review of 15 series with 1408 patients with duodenal injuries
Mortality Overall Disease-specific Risk factors 17% 6.5-12.5% Delayed diagnosis
Associated injuries Disease specific related to duodenal fistula, sepsis, MOF, abscess
Associated with fistula (0-3.9%) Delayed diagnosis Cogbill 14.4% blunt trauma,
penetrating trauma 3.6% Early dieath: Exsanguination from associated
vascular/liver/spleen injuries late death 1-2 weeks, MOF sepsis Time to diagnosis
Roman and colleagues Delay > 24 hours 4/10 died 3/10 duodenal fistulas Lucas and
Ledgerwood Mortality 40% Delay < 24 hours Mortality 11% Snyder and coworkers
Delay 2/4 died 2/4 duodenal fistulas
Pedicled graft Jejunal Serosal Patch Buttress duodenal defect with serosa of jejunum
Large defects Unproven efficacy Graft Jejunum Vascular pedicle Large defects
Unproven efficacy Described by Kobbold and Thal Resected areas of duodenal wall
in dogs (1.5 x 3cm) Injuries were repaired by sewing the serosa of a loop of jejunum
to the edges of the duodenal defect After the animals were sacrificed, a histologic
study showed mucosal resurfacing of the jejunal serosa Since then, this technique has
been used on human patients using a patch from a Roux-en-Y limb.
Grading of Severity Duodenal Severity Scale Mild Severe Determinants of injury
severity Agent Stab Blunt/Missile Size <75% wall ≥75% wall Duodenal site 3, 4 1, 2
Injury-repair interval (hr) <24 ≥24 Adjacent Injury No CBD No pancreatic injury
CBD Pancreatic injury Outcome Mortality 0% 6% Morbidity 2% 10% Mild : low
mortality and morbidity Snyder
Plain radiograph Retroperitoneal gas Free gas under diaphragm Obliteration of right
psoas muscle
Computerized Tomography Contrast extravasation Pneumoperitoneum
Retroperitoneal hematoma Unusual bowel morphology Unexplained periduodenal
fluid
Computerized Tomography Mainstay of evaluation for blunt trauma Limitations Allen
et al. Diagnostic delay in 20% Ballard et al Diagnostic delay in 27% Importance of re-
evaluation CT or exploration
Operative Exposure Laparotomy Cattel and Braasch Maneuver Kocher Maneuver
Transection of Ligament of Treitz Laparotomy Kocher Maneuver D1, D2, D3
Pancreatic head Periampullary area Distal CBD Cattel and Braasch Maneuver D3
Body of pancreas Transection of the ligament of Treitz D4 Kocher: Incise lateral
attachments Sweep D2/3 medially using sharp/blunt dissection Visualize
anterior/posterior D2/D3, head of pancreas, infrarenal IVC Cattel and Braasch
maneuver Incise avascular line of Toldt Mobilize right colon and hepatic flexure
Incise retroperitoneal attachments of SB from the RLQ to DJ junction Reflect SB out
of abdominal cavity Visualize D4 Preserve IMV Rotate right to left to visualize
anterior D3 and D4
Whipple procedure Pancreatico-duodenectomy Indications Uncontrolled
peripancreatic hemorrhage Extensive injury to proximal pancreatic duct, distal
common bile duct and ampulla Combined devascularizing injuries to duodenum and
head of pancreas High mortality rate Velmahos et al 33% 2-stage vs 1-stage 247
patients PD for 7 patients Mortality due to vascular injuries Feliciano Simple
duodenal injuries with nonductal pancreatic injury primary repair and drainage
Extensive duodenal injuries combined with pancreatic injuries not involving duct to
the right of SM vessels repair or resection, pyloric exclusion, GJ, drainage
Lacerations in HOP with ductal involvement, devascularizing lesions of duodenum,
duodenal lacerations with destruction of ampulla nad CBD PD (1 stage or 2 stage,
duodeanl repair, pyloric exlcusion and wide drainage)
Jejunal Serosal Patch Pedicled graft Described by Kobbold and Thal Resected areas of
duodenal wall in dogs (1.5 x 3cm) Injuries were repaired by sewing the serosa of a
loop of jejunum to the edges of the duodenal defect After the animals were sacrificed,
a histologic study showed mucosal resurfacing of the jejunal serosa Since then, this
technique has been used on human patients using a patch from a Roux-en-Y limb.
Duodenal diverticulization Berne 1968 Procedure Duodenorrhaphy Gastric
antrectomy Vagotomy Tube duodenostomy T-tube common bile duct drainage End-
to-side gastrojejunostomy Complicated Out-of-date
Damage control Hemorrhage control Provisional repair closure of perforation
resection without anastomosis Temporary abdominal closure Intensive care unit
resuscitation Damage control is an important concept, especially in trauma It includes
hemorrhage control by means of plication of bleeders and packing, provisional repair
aiming at closing up perforation with sutures/staples or resection without establish
continuity, temporary abdominal closure and ICU resuscitation The aim is to achieve
rapid surgery with temporary control, while minimizing physiological disturbance,
thereby reversing and preventing the progression of the lethal triad of trauma
You might also like
- Care of The Acutely Unwell FinalDocument100 pagesCare of The Acutely Unwell Finalgireeshsachin100% (1)
- Duodenal InjuryDocument54 pagesDuodenal InjuryTony HardianNo ratings yet
- MnemonicS in OphthaDocument22 pagesMnemonicS in Ophthaabuahmed&janaNo ratings yet
- Nurses NotesDocument1 pageNurses Notesmona_javier100% (4)
- Diverticulitis Cure: The Ultimate Diverticulitis Diet: Diverticulitis Recipes: Your Ultimate Diverticulitis CookbookFrom EverandDiverticulitis Cure: The Ultimate Diverticulitis Diet: Diverticulitis Recipes: Your Ultimate Diverticulitis CookbookNo ratings yet
- Study of Cancer Investigatory ProjectDocument15 pagesStudy of Cancer Investigatory ProjectsaralaNo ratings yet
- Penetrating Abdominal Trauma Emergency ManagementDocument29 pagesPenetrating Abdominal Trauma Emergency Managementanjali singhNo ratings yet
- Low Back Pain Handbook. A Guide For The Practicing Clinician by Andrew J. Cole, M.D., F.a.C.S.M. and Stanley A. Herring, M.D., F.a.C.S.M. (Eds.)Document579 pagesLow Back Pain Handbook. A Guide For The Practicing Clinician by Andrew J. Cole, M.D., F.a.C.S.M. and Stanley A. Herring, M.D., F.a.C.S.M. (Eds.)David GermánNo ratings yet
- Gastroduodenal Perforation Causes and ManagementDocument4 pagesGastroduodenal Perforation Causes and ManagementMaresp21No ratings yet
- Abdominal TraumaDocument52 pagesAbdominal TraumaDONALD UNASHENo ratings yet
- 4thQ Week1 PPT DigestiveDocument49 pages4thQ Week1 PPT DigestiveGeronimo SantiagoNo ratings yet
- Feeding techniques for babies with cleft lip or palateDocument14 pagesFeeding techniques for babies with cleft lip or palateTrishaNo ratings yet
- Complex pancreatico-duodenal injuries: A multidisciplinary approachDocument22 pagesComplex pancreatico-duodenal injuries: A multidisciplinary approachMaudonat MegNo ratings yet
- Colorectal Surgery: Clinical Care and ManagementFrom EverandColorectal Surgery: Clinical Care and ManagementBruce GeorgeNo ratings yet
- Differences Between HVAC For Hospitals and That For Other BuildingsDocument29 pagesDifferences Between HVAC For Hospitals and That For Other BuildingsMostafa Elmaghraby 467No ratings yet
- By Dr. Nouran Abou Khedr: Xeroderma PigmentosumDocument6 pagesBy Dr. Nouran Abou Khedr: Xeroderma PigmentosumBahaa ShaabanNo ratings yet
- Multilevel Duodenal Injury After Blunt TraumaDocument5 pagesMultilevel Duodenal Injury After Blunt TraumaHanny RusliNo ratings yet
- Management of Duodenal Trauma: ReviewDocument4 pagesManagement of Duodenal Trauma: ReviewAladesuruOlumideAdewaleNo ratings yet
- Genitourinary trauma guideDocument42 pagesGenitourinary trauma guideOrin SujasmanNo ratings yet
- Peitzman Trauma HepáticoDocument11 pagesPeitzman Trauma HepáticoLety Carmona ArevaloNo ratings yet
- Specific Abdominal Trauma: Evaluation and ManagementDocument74 pagesSpecific Abdominal Trauma: Evaluation and ManagementjeevanNo ratings yet
- Current Management of Hepatic TraumaDocument11 pagesCurrent Management of Hepatic TraumaPerla RuizNo ratings yet
- Duodenal Trauma: Luke R Johnston, Gary Wind and Matthew J BradleyDocument9 pagesDuodenal Trauma: Luke R Johnston, Gary Wind and Matthew J BradleyHenry Espinoz ChavNo ratings yet
- Duodenal Injuries ReviewDocument7 pagesDuodenal Injuries Revieweztouch12No ratings yet
- TraumaDocument10 pagesTraumaIda_Maryani94No ratings yet
- AntrectomyDocument15 pagesAntrectomyOhana S.No ratings yet
- DIAFRAGMADocument9 pagesDIAFRAGMAmishponce12No ratings yet
- Complicationsafter Pancreaticoduodenectomy: Robert SimonDocument10 pagesComplicationsafter Pancreaticoduodenectomy: Robert SimonŞükriye AngaNo ratings yet
- The Spleen: Splenic Trauma and Splenectomy: TrunkDocument3 pagesThe Spleen: Splenic Trauma and Splenectomy: TrunkAsish GeiorgeNo ratings yet
- Materi Rupture BladderDocument4 pagesMateri Rupture Bladderendah desfindaNo ratings yet
- Duodenal Injuries: E. Degiannis and K. BoffardDocument7 pagesDuodenal Injuries: E. Degiannis and K. BoffardDaniel Suarez ParapatNo ratings yet
- Wolters Kluwer - Medknow Publications: Journal of Emergencies, Trauma and ShockDocument16 pagesWolters Kluwer - Medknow Publications: Journal of Emergencies, Trauma and Shocktri ayunitaNo ratings yet
- Colorectal TraumaDocument44 pagesColorectal TraumaicalNo ratings yet
- 3santucci 408 414Document7 pages3santucci 408 414Muh Ayyub PrimadiNo ratings yet
- ABC of Liver and Pancreatic TraumaDocument3 pagesABC of Liver and Pancreatic TraumaDiana DeciuNo ratings yet
- Essential Update: Study Suggests Limited Sensitivity For Pelvic Radiography in Pediatric Blunt Torso TraumaDocument5 pagesEssential Update: Study Suggests Limited Sensitivity For Pelvic Radiography in Pediatric Blunt Torso TraumashiaNo ratings yet
- Duodenal Injuries: E. Degiannis and K. BoffardDocument7 pagesDuodenal Injuries: E. Degiannis and K. BoffardriftaNo ratings yet
- Abdominal TraumaDocument59 pagesAbdominal TraumaEirene Sophie Wutoy HallatuNo ratings yet
- Duodenal Repair Literature ReviewDocument34 pagesDuodenal Repair Literature ReviewTsega WesenNo ratings yet
- Imaging in Duodenal Ulcers: More..Document12 pagesImaging in Duodenal Ulcers: More..Sulaiman NulhakimNo ratings yet
- Torso Trauma ManagementDocument64 pagesTorso Trauma ManagementHafizur RashidNo ratings yet
- Erik Pancreatic TraumaDocument31 pagesErik Pancreatic TraumaIgnatius JesinNo ratings yet
- Open Adhesiolysis: BackgroundDocument8 pagesOpen Adhesiolysis: BackgroundV15CERA FK UNANDNo ratings yet
- Surgicalmanagementof Abdominaltrauma: Hollow Viscus InjuryDocument11 pagesSurgicalmanagementof Abdominaltrauma: Hollow Viscus Injurysyairodhi rodziNo ratings yet
- 17-09-2019 Lower GI FINALDocument32 pages17-09-2019 Lower GI FINALNaima HabibNo ratings yet
- Endoscopic Management of Complications From Laparoscopic Cholecystectomy - UpToDateDocument16 pagesEndoscopic Management of Complications From Laparoscopic Cholecystectomy - UpToDateLuis Miguel Díaz VegaNo ratings yet
- Ahmed 2011Document7 pagesAhmed 2011wiraNo ratings yet
- Management of Liver Trauma in Adults: Nasim Ahmed, Jerome J VernickDocument7 pagesManagement of Liver Trauma in Adults: Nasim Ahmed, Jerome J VernickwiraNo ratings yet
- SplitPDFFile 801 To 1000Document200 pagesSplitPDFFile 801 To 1000Shafan ShajahanNo ratings yet
- Small Bowel ObstructionDocument17 pagesSmall Bowel ObstructionXavi Diaz100% (1)
- DR HK Leung Queen Elizabeth Hospital Joint Hospital Surgical Grand RoundDocument29 pagesDR HK Leung Queen Elizabeth Hospital Joint Hospital Surgical Grand RoundNoy FaridaNo ratings yet
- PBEI Incisional Hernia PDFDocument31 pagesPBEI Incisional Hernia PDFAdi WijayantoNo ratings yet
- Interventional Approaches Gallbladder DiseaseDocument9 pagesInterventional Approaches Gallbladder DiseaseAntônio GoulartNo ratings yet
- AppendectomyDocument7 pagesAppendectomyLeis FatwaNo ratings yet
- Rhode Island Hospital: Related Emedicine TopicsDocument6 pagesRhode Island Hospital: Related Emedicine TopicsApril Shane OreiroNo ratings yet
- Bladder injury causes, symptoms, diagnosis and treatmentDocument7 pagesBladder injury causes, symptoms, diagnosis and treatmentcorsaruNo ratings yet
- Genitourina Ry Trauma: Skdi 3BDocument33 pagesGenitourina Ry Trauma: Skdi 3BSartikaOdock100% (1)
- Diverticulum DiseaseDocument6 pagesDiverticulum Diseasen_robinNo ratings yet
- Open CholecystectomyDocument11 pagesOpen CholecystectomyDaywalker PedragozaNo ratings yet
- Penetrating Abdominal Trauma Emergency ManagementDocument25 pagesPenetrating Abdominal Trauma Emergency Managementanjali singhNo ratings yet
- AB__PENETRANTEDocument29 pagesAB__PENETRANTENina JácomeNo ratings yet
- Surgery News Summer 2012 Newsletter - Spotlight On Colorectal SurgeryDocument4 pagesSurgery News Summer 2012 Newsletter - Spotlight On Colorectal SurgeryContinuum Hospitals of New YorkNo ratings yet
- Complications of Gynecologic Surgery: Intraoperative and Postoperative RisksDocument17 pagesComplications of Gynecologic Surgery: Intraoperative and Postoperative RisksAnditha Namira RSNo ratings yet
- ER UGI Bleed Scenarios: Focus on Stabilization and Source ControlDocument4 pagesER UGI Bleed Scenarios: Focus on Stabilization and Source Controljbuzz28No ratings yet
- Esophagectomy Procedure and ManagementDocument17 pagesEsophagectomy Procedure and ManagementAbdallah DarrasNo ratings yet
- Abdominal TraumaDocument9 pagesAbdominal TraumaSh ReyaNo ratings yet
- Robotic Hernia Surgery: A Comprehensive Illustrated GuideFrom EverandRobotic Hernia Surgery: A Comprehensive Illustrated GuideOmar Yusef KudsiNo ratings yet
- Endoscopic Management of Colorectal T1(SM) CarcinomaFrom EverandEndoscopic Management of Colorectal T1(SM) CarcinomaShinji TanakaNo ratings yet
- MSMD Thesis Evaluation Rating Scale.Document4 pagesMSMD Thesis Evaluation Rating Scale.Zam HusNo ratings yet
- 845 MazuskiDocument59 pages845 MazuskiZam HusNo ratings yet
- Therapeutic Guidelines Antimicrobial Prophylaxis SurgeryDocument86 pagesTherapeutic Guidelines Antimicrobial Prophylaxis SurgeryhendryfransiskusNo ratings yet
- Synopses Not SubmittedDocument2 pagesSynopses Not SubmittedZam HusNo ratings yet
- Er Audit: 27/04/23 ThursdayDocument5 pagesEr Audit: 27/04/23 ThursdayZam HusNo ratings yet
- Doudenum Article PDFDocument6 pagesDoudenum Article PDFZam HusNo ratings yet
- CV Aoun AliDocument1 pageCV Aoun AliZam HusNo ratings yet
- Main PDFDocument6 pagesMain PDFZam HusNo ratings yet
- Imm Uro Questions-1Document5 pagesImm Uro Questions-1Zam HusNo ratings yet
- Histology Question Pool PDFDocument70 pagesHistology Question Pool PDFZam HusNo ratings yet
- Nnis34hl Wow9226200Document4 pagesNnis34hl Wow9226200Zam HusNo ratings yet
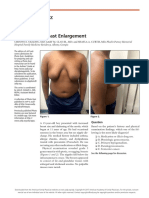
- Photo Quiz: Severe Male Breast EnlargementDocument2 pagesPhoto Quiz: Severe Male Breast EnlargementZam HusNo ratings yet
- Segaletal 2019GeriatricAnxietyScaleDocument8 pagesSegaletal 2019GeriatricAnxietyScaleMapodettNo ratings yet
- Amoeba Sisters' guide to the 11 human body systemsDocument5 pagesAmoeba Sisters' guide to the 11 human body systemsANTONIA GUTIERREZ GARCIANo ratings yet
- Interaksi Obat Obat MaagDocument8 pagesInteraksi Obat Obat MaagSiti NurohmahhNo ratings yet
- Fresenius 2008T Dialysis System - User's Troubleshooting ManualDocument20 pagesFresenius 2008T Dialysis System - User's Troubleshooting ManualCesar AlfaroNo ratings yet
- Drug Study 7th Floor Ucmed RotationDocument6 pagesDrug Study 7th Floor Ucmed RotationVinz OñoNo ratings yet
- Epidemiology Related Terminology and Their DifferencesDocument3 pagesEpidemiology Related Terminology and Their DifferencesHasnat KhanNo ratings yet
- MH Case Study Fall 2021Document10 pagesMH Case Study Fall 2021api-593123385No ratings yet
- Donna Eveline Prisca Panduu 1061050030 Pembimbing: Dr. Karyadi Prayanangga, SP - AnDocument20 pagesDonna Eveline Prisca Panduu 1061050030 Pembimbing: Dr. Karyadi Prayanangga, SP - AndonnaevelineNo ratings yet
- Dermtimes - Vitiligo Treatment SuccessDocument2 pagesDermtimes - Vitiligo Treatment SuccessradqudahNo ratings yet
- HallucinogensDocument18 pagesHallucinogensDavyne Nioore Gabriel100% (1)
- IVT Completion Case Form EditedDocument1 pageIVT Completion Case Form EditedNURSETOPNOTCHERNo ratings yet
- Osteoartritis: Dr. Dewi Nur Fiana.,Sp - KFRDocument28 pagesOsteoartritis: Dr. Dewi Nur Fiana.,Sp - KFRgita cahayaNo ratings yet
- Definisi & PICO 3, 4Document5 pagesDefinisi & PICO 3, 4Dionisius KevinNo ratings yet
- 5 Minute Spotlight - Vacuum Extraction and Forceps DeliveryDocument2 pages5 Minute Spotlight - Vacuum Extraction and Forceps DeliveryMikeNo ratings yet
- Clinical Trial Using A Silver-Coated Screw-Rod System and One-Year Follow-Up of The First 50 PatientsDocument12 pagesClinical Trial Using A Silver-Coated Screw-Rod System and One-Year Follow-Up of The First 50 Patientsguugle gogleNo ratings yet
- Metaplastic (Chronic) Atrophic Gastritis - UpToDate PDFDocument16 pagesMetaplastic (Chronic) Atrophic Gastritis - UpToDate PDFDinaNo ratings yet
- What Are The Signs of Autism in GirlsDocument8 pagesWhat Are The Signs of Autism in GirlsAna Sofia Nunes JorgeNo ratings yet
- Acquired Metabolic Disorders of The Nervous SystemDocument17 pagesAcquired Metabolic Disorders of The Nervous SystemRondy Omandam ArdosaNo ratings yet
- Exercises After Breast Surgery: A Guide For WomenDocument15 pagesExercises After Breast Surgery: A Guide For WomenAtul PannuNo ratings yet
- D-Dimer Antigen Current Concepts and Future Prospe-2Document40 pagesD-Dimer Antigen Current Concepts and Future Prospe-2fajar jamaloedinzNo ratings yet
- Pharma Medical Director Cardiology in NYC Resume Ronald HabermanDocument3 pagesPharma Medical Director Cardiology in NYC Resume Ronald HabermanRonaldHabermanNo ratings yet