Professional Documents
Culture Documents
Association of Testosterone TherapyWith Risk of Venous Thromboembolism
Uploaded by
douglas 87Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Association of Testosterone TherapyWith Risk of Venous Thromboembolism
Uploaded by
douglas 87Copyright:
Available Formats
Research
JAMA Internal Medicine | Original Investigation
Association of Testosterone Therapy With Risk of Venous Thromboembolism
Among Men With and Without Hypogonadism
Rob F. Walker, MPH; Neil A. Zakai, MD, MSc; Richard F. MacLehose, PhD; Logan T. Cowan, PhD;
Terrence J. Adam, RPH, PhD, MD; Alvaro Alonso, MD, PhD; Pamela L. Lutsey, PhD
Supplemental content
IMPORTANCE Testosterone therapy is increasingly prescribed in patients without a diagnosis
of hypogonadism. This therapy may be associated with increased risk of venous
thromboembolism (VTE) through several mechanisms, including elevated hematocrit levels,
which increase blood viscosity.
OBJECTIVE To assess whether short-term testosterone therapy exposure is associated with
increased short-term risk of VTE in men with and without evidence of hypogonadism.
DESIGN, SETTING, AND PARTICIPANTS This case-crossover study analyzed data on 39 622 men
from the IBM MarketScan Commercial Claims and Encounter Database and the Medicare
Supplemental Database from January 1, 2011, to December 31, 2017, with 12 months of
follow-up. Men with VTE cases who were free of cancer at baseline and had 12 months of
continuous enrollment before the VTE event were identified by International Classification of
Diseases codes. Men in the case period were matched with themselves in the control period.
Case periods of 6 months, 3 months, and 1 month before the VTE events were defined, with
equivalent control periods (6 months, 3 months, and 1 month) in the 6 months before the
case period.
EXPOSURES National drug codes were used to identify billed testosterone therapy
prescriptions in the case period (0-6 months before the VTE) and the control period (6-12
months before the VTE).
MAIN OUTCOMES AND MEASURES The main outcome in this case-only experiment was first
VTE event stratified by the presence or absence of hypogonadism.
RESULTS A total of 39 622 men (mean [SD] age, 57.4 [14.2] years) were enrolled in the study,
and 3110 men (7.8%) had evidence of hypogonadism. In age-adjusted models, testosterone
therapy use in all case periods was associated with a higher risk of VTE in men with (odds
ratio [OR], 2.32; 95% CI, 1.97-2.74) and without (OR, 2.02; 95% CI, 1.47-2.77) hypogonadism.
Among men without hypogonadism, the point estimate for testosterone therapy and VTE risk
in the 3-month case period was higher for men younger than 65 years (OR, 2.99; 95% CI,
1.91-4.68) than for older men (OR, 1.68; 95% CI, 0.90-3.14), although this interaction was not
statistically significant (P = .14).
CONCLUSIONS AND RELEVANCE Testosterone therapy was associated with an increase in
short-term risk for VTE among men with and without hypogonadism, with some evidence
that the association was more pronounced among younger men. These findings suggest that
caution should be used when prescribing testosterone therapy.
Author Affiliations: Author
affiliations are listed at the end of this
article.
Corresponding Author: Rob F.
Walker, MPH, Division of
Epidemiology and Community
Health, School of Public Health,
University of Minnesota,
1300 S Second St, Ste 300,
JAMA Intern Med. doi:10.1001/jamainternmed.2019.5135 Minneapolis, MN 55413
Published online November 11, 2019. (walk0493@umn.edu).
(Reprinted) E1
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a UCSF LIBRARY User on 11/11/2019
Research Original Investigation Testosterone Therapy and Venous Thromboembolism Risk in Men With and Without Hypogonadism
T
he clinical indication for testosterone therapy is
primarily to treat hypogonadism, a condition Key Points
in which serum testosterone levels in men
Question Is clinical prescription of testosterone therapy
decrease below a specific threshold, resulting in sexual associated with short-term risk of venous thromboembolism in
dysfunction, altered bone metabolism and body composi- men with and without hypogonadism?
tion, and potential emotional dysregulation.1-4 Although
Findings In this case-crossover study comparing 6-month
testosterone levels may decrease with age, external causes
testosterone use for 39 622 men who had a venous
of clinic al hypogonadism include genetic diseases thromboembolism with testosterone use 6 to 12 months before
or complications from surgery, infection, and medications.4 the venous thromboembolism, use of testosterone therapy in the
Testosterone prescriptions among men increased more 6-month case period was associated with an increased risk of
than 300% from 2001 to 20135,6; the increase is thought venous thromboembolism among men with and without
to be caused by testosterone therapy being prescribed hypogonadism.
for common symptoms, such as low libido and f at Meaning The findings suggest that testosterone therapy is
redistribution, associated with aging, obesity, and diabetes associated with increased short-term risk of venous
and not necessarily with clinical hypogonadism. 7 This thromboembolism among all men prescribed the therapy.
increase in prescription rate was more pronounced among
men aged 18 to 45 years than among older men.5 In 2014,
the US Food and Drug Administration released a warning
about testosterone therapy and the potential risk of heart Methods
attack and stroke; since then, testosterone therapy prescrip-
tions have decreased and eventually plateaued.8,9 Recent Data Source
trends estimate that, in the United States, 2.3 million This case-crossover study included data obtained using inpatient
men older than 30 years (3.2%) were prescribed testoste- and outpatient medical claims provided from the IBM Market-
rone therapy in 2013 and that this trend decreased to Scan Commercial Claims and Encounter Database and the Medi-
approximately 1.15 million men (1.6%) in 2016.6,10 Evidence care Supplemental Database (IBM Watson Health) from January
suggests that testosterone therapy is still being prescribed 1, 2011, through December 31, 2017. The databases contain health
to men without hypogonadism.7 care claims information from US employers, health plans, hos-
Ve n o u s t h ro m b o e m b o l i s m ( V T E ) , c o n s i s t i ng o f pitals, and Medicare programs. Data on all enrollment records
deep vein thrombosis and pulmonary embolism, is a com- and inpatient, outpatient, ancillary, and drug claims are collated
mon condition in the United States, with more than 1 mil- and linked via individual-level identifiers. The MarketScan da-
lion individuals experiencing a VTE annually. 11 Baseline tabases are compliant with the Health Insurance Portability and
testosterone levels are not associated with increase in VTE Accountability Act, and all data are deidentified. As such, per
risk. 12 However, exogenous testosterone therapy may MarketScan operational procedure, enrollee consent was not re-
increase endogenous hematocrit levels, which can increase quired or obtained. This study was deemed to be exempt accord-
blood viscosity, platelet accumulation, and thromboxane ing to the institutional review board process for the University
A2 concentrations for up to 6 months and could subse- of Minnesota.
q u e nt l y i n c r e a s e r i s k o f b l o o d c l o t f o r m at i o n a n d
subsequent VTE events.13-15 Testosterone therapy is most Study Population and VTE Definition
commonly administered via transdermal gels, patches, or The initial cohort included 93 205 men aged 18 to 99 years with
intramuscular routes, each having their own rate of absorp- at least 1 inpatient or 2 outpatient claims for VTE 7 to 184 days
tion and prescription strengths that potentially affect apart (International Classification of Diseases, Ninth Revision,
cardiovascular pathophysiologic factors.16 Pathophysiologic Clinical Modification [ICD-9-CM] and International Statistical
research suggests that exogenous testosterone therapy Classification of Diseases, Tenth Revision, Clinical Modifica-
could increase VTE risk, but the 2 largest observational tion [ICD-10-CM] codes provided in eTable 1 in the Supple-
studies17,18 evaluating this association reached conflicting ment), with 1 corresponding anticoagulant prescription within
c o n c l u s i o n s . Fu r t h e r m o re , t h e s e s t u d i e s 1 7, 1 8 we re 31 days of the initial VTE date. The positive predictive value
underpowered to examine testosterone therapy use within was 91% in a validation study that used a similar definition,
important clinical subgroups, such as by clinical hypogo- incorporating both inpatient and outpatient ICD-9-CM codes
nadism status, 1 9 age, route of testosterone therapy and requiring evidence of treatment.20-23
exposure, and duration of testosterone therapy use. After restriction of the sample to men with at least 12
Using a c ase-c rossover design, this study tested months of continuous enrollment before their VTE, 52 203 men
our primary hypothesis that exposure to testosterone remained. A total of 12 581 men with prevalent cancer were ex-
therapy is associated with increased risk of incident VTE cluded, and the final analytic sample included 39 622 men with
among men stratified by clinical hypogonadism status. 12 months of follow-up before their VTE. For all men, only the
Secondary analyses stratifying by age group (<65 years incident VTE event was considered in these analyses.
vs ≥65 years), route of testosterone therapy exposure, and The US Endocrine Society defines hypogonadism as “con-
different case periods were performed to assess various sistently low serum total testosterone and/or free testosterone
risk profiles. concentrations”24(p 1716) with trademark symptoms (loss of body
E2 JAMA Internal Medicine Published online November 11, 2019 (Reprinted) jamainternalmedicine.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a UCSF LIBRARY User on 11/11/2019
Testosterone Therapy and Venous Thromboembolism Risk in Men With and Without Hypogonadism Original Investigation Research
hair, small testis size, and delayed sexual development). Market-
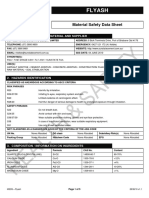
Figure. Study Design
Scan data do not contain specific laboratory values of tests or de-
tailed information about patient symptoms. Therefore, hypogo- A Main analysis
nadism for the main analysis was defined by the ICD-9-CM codes Control period Case period
257.xx and the ICD-10-CM codes E29.x and E89.5, which capture
6 mo 6 mo
an array of hypogonadism diagnoses, including postirradiation 3 mo 3 mo
and postsurgical diagnoses. These codes were based on a previ- 1 mo 1 mo
ous study17 that used claims data that controlled for hypogonad-
6-12 mo 0-6 mo Incident
ism status and a review of the diagnosis code descriptions. A sen-
VTE
sitivity analysis was performed defining hypogonadism using a
different set of ICD-9-CM and ICD-10-CM codes spanning vari- B Exploratory analysis
ous testicular, pituitary, and hypothalamic disorders used in an
Control period Case period
analysis performed by Jasuja et al.25
Study Design 6-3 mo 3-1 mo 1 mo 6-3 mo 3-1 mo 1 mo
A case-crossover study design was used in which each man
6-12 mo 0-6 mo Incident
with VTE served as his own control. We defined exposure case VTE
periods of 6 months, 3 months, and 1 month before the inci-
dent VTE event, with equivalent exposure control periods (6 Schematic of the main (A) and exploratory (B) case-crossover study designs.
months, 3 months, and 1 month) starting 6 months before the VTE indicate venous thromboembolism.
incident VTE event (Figure, A). Various case period lengths
were selected to assess the time frame in which VTE events
could be triggered after testosterone prescription exposure. Be-
cause each case patient serves as his own control, the case- To explore multiplicative interaction associations, we con-
crossover design mitigates confounders that are time invari- ducted the same overall analyses stratified by age category
ant during a patient’s observation period. (<65 vs ≥65 years) and route of testosterone (transdermal vs
intramuscular). Multiplicative interactive associations were for-
mally tested by adding an interaction term in the original lo-
Identification of Testosterone Therapy Prescriptions
gistic regression models. An exploratory analysis was con-
The main exposure of interest was a received drug claim for
ducted that classified testosterone therapy use differently to
testosterone therapy 1 month, 3 months, or 6 months before
look for lagged associations. Time windows of less than 1, 1 to
an individual’s first VTE event. The case periods were
3, or 3 to 6 months before the first VTE event and the corre-
defined based on the time that testosterone therapy is thought
sponding time windows for the control period 6 months be-
to affect the previously mentioned pathophysiologic factors
fore the VTE were used for all analyses (Figure, B). Use of
known to increase VTE risk. We defined 612 different formu-
testosterone therapy in the 3- to 6-month case period was used
lations for testosterone therapy, including a variety of pre-
as a reference category (instead of no testosterone therapy use)
scription brands, strengths, and routes using a therapeutic de-
to detect different risk profiles from the 1- to 3-month and
tail code (6808010090) unique to MarketScan databases (RED
1-month case periods. All statistical analyses were performed
BOOK, IBM Watson Health). Route of exposure was classified
with SAS statistical software, version 9.4 (SAS Institute Inc).
as transdermal (includes both gel and patch methods of ap-
A 2-sided test for P < .05 was used as the significance
plication) or intramuscular injection. A sensitivity analysis was
threshold.
performed that defined testosterone therapy use as having
more than 1 testosterone therapy prescription fill within the
3-month and 6-month case periods.
Results
Statistical Analysis A total of 39 622 men (mean [SD] age, 57.4 [14.2] years) were
The presence of a testosterone prescription 1, 3, and 6 months enrolled in the study, with 3110 men (7.8%) diagnosed with hy-
before the incident VTE date was compared with the equiva- pogonadism and 29 182 men (73.7%) younger than 65 years.
lent control periods that occurred 6 months before the VTE date. Among the 36 512 men without hypogonadism, 374 (1.0%) were
Conditional logistic regression was used to estimate the odds ra- ever prescribed testosterone in the year before their VTE event.
tios (ORs) and corresponding 95% CIs for the risk of VTE asso- Among the 3110 men with hypogonadism, 1330 (42.8%) were
ciated with testosterone use in the case period compared with prescribed testosterone in the 12 months before their VTE
the control period. Hospitalization has been found to be asso- event. Compared with men without evidence of hypogonad-
ciated with VTE,26,27 and the number of medical encounters may ism, men with hypogonadism had more outpatient encoun-
be an indicator of general health. As such, in multivariable mod- ters in the year before their VTE (Table 1). All analyses were
els, we controlled for the number of inpatient hospitalizations, stratified by hypogonadism status; primary results for men
outpatient visits, and emergency department hospitalizations without hypogonadism are provided in Table 2 and for men
that occurred in the case and control periods. with hypogonadism in Table 3.
jamainternalmedicine.com (Reprinted) JAMA Internal Medicine Published online November 11, 2019 E3
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a UCSF LIBRARY User on 11/11/2019
Research Original Investigation Testosterone Therapy and Venous Thromboembolism Risk in Men With and Without Hypogonadism
sitivity analysis that required men to have more than 1 testos-
Table 1. Characteristics of Men With and Without Hypogonadism,
MarketScan Database, 2011-2017a terone prescription fill (eTable 4 in the Supplement), with ORs
of 2.46 (95% CI, 1.38-4.39) for the 6-month case period and 3.75
No
Hypogonadism Hypogonadism (95% CI, 1.95-7.22) for the 3-month case period.
Characteristic (n = 36 512) (n = 3110) In exploratory analyses, we considered exposure periods
Age, mean (SD), y 57.4 (14.4) 57.5 (10.9) of less than 1 month, 1 to 3 months, and 3 to 6 months. Use of
Age <65 y 53 512 (73.3) 4852 (78.0) testosterone therapy in the less than 1-month and 1- to 3-month
Ever used testosterone therapy 374 (1.0) 1330 (42.8) case periods was associated with approximately a doubling in
Testosterone therapy routeb the risk of VTE (<1-month OR, 1.96; 95% CI, 1.24-3.10; 1- to
Intramuscular 139/573 (24.3) 809/2189 (37.0) 3-month OR, 2.24; 95% CI, 1.42-3.54); however, no associa-
Transdermal 432/573 (75.4) 1371/2189 (62.7) tion was found in the 3- to 6-month period (OR, 0.99; 95% CI,
Other 2/573 (0.3) 9/2189 (0.3) 0.65-1.53). Risk in the less than 1-month and 1- to 3-month case
No. of inpatient hospitalizations, 0.2 (0.5) 0.2 (0.6) periods (OR, 1.87; 95% CI, 1.01-3.46) was statistically signifi-
mean (SD)c
cantly different from that in the 3- to 6-month case period (OR,
No. of outpatient encounters, 3.5 (13.4) 5.7 (4.8)
mean (SD)c 2.08; 95% CI, 1.17-3.70).
No. of emergency department 0.3 (0.6) 0.4 (0.8)
encounters, mean (SD)c Testosterone Therapy and VTE
a
Data are presented as number (percentage) unless otherwise indicated. Among Men With Hypogonadism
b
Denominators of 573 and 2189 are the amount of unique testosterone Among men with hypogonadism, testosterone therapy use was
prescriptions in the case and control periods during the 12-month also higher in the total 6-month case period (n = 1069) com-
study period.
pared with the control period (n = 697) (Table 3). Testoste-
c
Numbers for inpatient hospitalizations, outpatient encounters, and
rone prescriptions in the 1-month (OR, 1.66; 95% CI,
emergency department visits correspond to the 12-month period before the
initial venous thromboembolism date. 1.34-2.04), 3-month (OR, 2.28; 95% CI, 1.91-2.72), and 6-month
(OR, 2.32; 95% CI, 1.97-2.74) case periods were also associ-
ated with approximately double the risk of VTE compared with
Testosterone Therapy and VTE the control periods 6 months earlier after adjusting for con-
Among Men Without Hypogonadism founders. There was no evidence of interactive associations
Among the men without hypogonadism, testosterone pre- by age group or route of testosterone therapy exposure
scription was more common in the 6 months immediately be- (Table 4).
fore the VTE event (case period; n = 294) than in the control Sensitivity analyses yielded higher adjusted estimates
period (n = 177) (Table 2). Use of testosterone therapy in the when an alternate definition of hypogonadism was used
case period was associated with a doubling of VTE risk when (eTable 3 in the Supplement). In the other sensitivity analysis
using the 1-month case period (OR, 1.96; 95% CI, 1.24-3.10), with testosterone therapy use defined as having filled more
3-month case period (OR, 2.46; 95% CI, 1.71-3.53), and 6-month than 1 prescription, magnitudes of association were larger
case period (OR, 2.02; 95% CI, 1.47-2.77) compared with tes- (eTable 4 in the Supplement). This sensitivity analysis yielded
tosterone therapy use in the equivalent control periods after ORs of 2.95 (95% CI, 2.34-3.71) for the 6-month case period and
adjusting for the number of inpatient hospitalizations, outpa- 3.34 (95% CI, 2.42-4.60) for the 3-month case period.
tient encounters, and emergency department encounters. In the exploratory analyses, we also analyzed the expo-
eTable 2 in the Supplement provides additional information sure periods of 1 to 3 months and 3 to 6 months. Among men
on the cross-classification of testosterone therapy use in the with hypogonadism, the adjusted ORs were 1.96 (95% CI, 1.60-
case and control periods for all period lengths. 2.41) for the 1- to 3-month case period and 1.33 (95% CI, 1.06-
Stratified analyses were also conducted to explore poten- 1.66) for the 3- to 6-month case period. Risk in the 1- to 3-month
tial interactive associations by age category and route of tes- case period was statistically significantly different from that
tosterone therapy exposure (Table 4). Although the interac- in the 3- to 6-month case period (OR, 1.49; 95% CI, 1.12, 1.97),
tions were not statistically significant, men younger than 65 whereas risks in the less than 1-month vs 3- to 6-month case
years without hypogonadism using testosterone therapy in the periods were not statistically significant (OR, 1.31; 95% CI, 0.98-
6-month (OR, 2.33; 95% CI, 1.60-3.40) and 3-month case pe- 1.76). Exploratory analysis results stratified by age category and
riods (OR, 2.99; 95% CI, 1.91-4.68) had greater VTE risk com- testosterone therapy route are provided in eTable 5 in the
pared with men 65 years and older using testosterone therapy Supplement.
in the 6-month (OR, 1.41; 95% CI, 0.77-2.56) and 3-month case
periods (OR, 1.68; 95% CI, 0.90-3.14). Estimates were similar
when comparing the 1-month testosterone therapy use with
the control period for both age groups. No significant interac-
Discussion
tions were apparent when analyses were stratified by route of Using a large medical claims database and a case-crossover ap-
testosterone therapy (transdermal vs intramuscular). proach, this study found that men without cancer prescribed
Sensitivity analyses using the alternative hypogonadism testosterone therapy had approximately twice the risk of VTE
definition yielded similar association estimates (eTable 3 in the within the 1-, 3-, and 6-month case periods compared with the
Supplement). Magnitudes of association were larger in the sen- equivalent control periods 6 months earlier. The association
E4 JAMA Internal Medicine Published online November 11, 2019 (Reprinted) jamainternalmedicine.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a UCSF LIBRARY User on 11/11/2019
Testosterone Therapy and Venous Thromboembolism Risk in Men With and Without Hypogonadism Original Investigation Research
Table 2. Overall Association of Testosterone Therapy Prescription With Risk of Venous Thromboembolism
Among Men Without Hypogonadism, Main and Exploratory Analyses, MarketScan Database, 2011-2017
Testosterone Therapy Prescription, No. (%) Odds Ratio (95% CI)
Testosterone Therapy Case
Period Case Period Control Perioda Crudeb Adjustedc
Main Analysis (n = 36 512)
6 mo 294 (0.8) 177 (0.5) 2.46 (1.90-3.19) 2.02 (1.47-2.77)
3 mo 220 (0.6) 119 (0.3) 2.53 (1.90-3.37) 2.46 (1.71-3.53)
1 mo 96 (0.3) 59 (0.2) 1.82 (1.27-2.62) 1.96 (1.24-3.10)
Exploratory Analysis (n = 36 512)
3-6 mo 74 (0.2) 58 (0.2) 1.29 (0.91-1.84) 0.99 (0.65-1.53)
1-3 mo 124 (0.3) 60 (0.2) 2.64 (1.83-3.82) 2.24 (1.42-3.54)
1 mo 96 (0.3) 59 (0.2) 1.82 (1.27-1.62) 1.96 (1.24-3.10)
a
Control period for the main analysis is the equivalent-length period (6, 3, or 1 analyses, men were matched on identification numbers (ie, they served as
month[s]) exactly 6 months before the first venous thromboembolism their own controls).
diagnosis. Control period for the exploratory analysis is the equivalent-length c
Analyses adjusted for total number of hospitalizations, outpatient encounters,
period (3-6, 1-3, or 1 month[s]) exactly 6 months before the first venous and emergency department encounters in the case and control periods.
thromboembolism diagnosis.
b
Crude analyses were conditioned on matching factors. In the case-crossover
Table 3. Overall Association of Testosterone Therapy Prescription With Risk of Venous Thromboembolism
Among Men With Hypogonadism, Main and Exploratory Analyses, MarketScan Database, 2011-2017
Testosterone Therapy Prescription, No. (%) Odds Ratio (95% CI)
Testosterone Therapy Case
Period Case Period Control Perioda Crudeb Adjustedc
Main Analysis (n = 3110)
6 mo 1069 (34) 697 (22) 2.43 (2.10-2.80) 2.32 (1.97-2.74)
3 mo 802 (26) 494 (16) 2.36 (2.02-2.75) 2.28 (1.91-2.72)
1 mo 342 (11) 229 (7) 1.62 (1.35-1.96) 1.66 (1.34-2.04)
Exploratory Analysis (n = 3110)
3-6 mo 267 (9) 203 (7) 1.36 (1.12-1.65) 1.33 (1.06-1.66)
1-3 mo 460 (15) 265 (9) 2.11 (1.77-2.53) 1.96 (1.60-2.41)
1 mo 342 (11) 229 (7) 1.62 (1.35-1.96) 1.66 (1.34-2.04)
a
Control period for the main analysis was the equivalent-length period (6, 3, or 1 analyses, men were matched on identification numbers (ie, they serve as their
month[s]) exactly 6 months before the first venous thromboembolism own controls).
diagnosis. Control period for the exploratory analysis was the c
Analyses adjusted for total number of hospitalizations, outpatient encounters,
equivalent-length period (3-6, 1-3, or 1 month[s]) exactly 6 months before the and emergency department encounters in the case and control periods.
first venous thromboembolism diagnosis.
b
Crude analyses were conditioned on matching factors. In the case-crossover
Table 4. Covariate-Adjusted Associations of Testosterone Therapy Prescription With Risk of Venous Thromboembolism
Among Men With Differing Hypogonadism Status Stratified by Age and Route of Testosterone Exposure, MarketScan Database, 2011-2017
Odds Ratio (95% CI) by Age Inter- Odds Ratio (95% CI) by Route of Therapy
Testosterone action P Interaction
Therapy Case Period <65 Years ≥65 Years Value Transdermal Intramuscular P Value
Hypogonadism
6 mo 2.40 (1.99-2.88) 2.05 (1.44-2.93) .48 2.28 (1.86-2.80) 2.28 (1.72-3.03) .97
3 mo 2.28 (1.87-2.79) 2.26 (1.54-3.32) .97 2.21 (1.77-2.77) 2.30 (1.70-3.11) .83
1 mo 1.76 (1.38-2.23) 1.32 (0.83-2.09) .30 1.69 (1.29-2.22) 1.49 (1.05-2.12) .76
No Hypogonadism
6 mo 2.33 (1.60-3.40) 1.41 (0.77-2.56) .11 2.09 (1.46-2.99) 1.64 (0.82-3.30) .99
3 mo 2.99 (1.91-4.68) 1.68 (0.90-3.14) .14 2.52 (1.67-3.82) 1.96 (0.90-4.27) .82
1 mo 2.09 (1.18-3.69) 1.62 (0.74-3.51) .76 2.31 (1.35-3.97) 1.28 (0.50-3.22) .72
was stronger among men younger than 65 years compared with tion, our study provides novel information about the time
men who were older; however, these differences were not sta- frame of exposure most pertinent to risk, with risk being great-
tistically significant. Associations between testosterone est in the first 3 months after testosterone therapy initiation.
therapy and risk of VTE did not differ whether the route of tes- These findings complement prior work8,28,29 suggesting that
tosterone therapy was transdermal or intramuscular. In addi- testosterone therapy use is associated with greater risk of stroke
jamainternalmedicine.com (Reprinted) JAMA Internal Medicine Published online November 11, 2019 E5
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a UCSF LIBRARY User on 11/11/2019
Research Original Investigation Testosterone Therapy and Venous Thromboembolism Risk in Men With and Without Hypogonadism
and myocardial infarction and suggest that practitioners should diovascular disease outcomes, especially if there is no clini-
be cautious when prescribing testosterone therapy. cal indication for starting therapy.
Prior observational studies about testosterone therapy and In the present analysis, VTE risk did not vary by route of
VTE are scarce and have been inconclusive about whether tes- exposure. The article by Baillargeon et al,17 which reported no
tosterone therapy affects VTE risk. A prior case-control study overall association of testosterone therapy with VTE risk, also
by Martinez et al18 also stratified by hypogonadism status and did not find differences when transdermal and intramuscu-
compared 19 000 men with VTE with 900 000 controls. Only lar testosterone therapy were evaluated separately. Likewise,
21 men without hypogonadism were current testosterone a meta-analysis of randomized clinical trials by Borst et al,33
therapy users, and testosterone therapy use was associated with relatively small sample sizes and short follow-up times,
with a 1.69-fold (95% CI, 1.09-2.63) increased risk of VTE. also reported no overall association of testosterone therapy
Among those with hypogonadism, 48 were receiving testos- with cardiovascular risk and found no difference when trans-
terone therapy, and current testosterone therapy use was as- dermal and intramuscular testosterone therapies were evalu-
sociated with a relative risk of 1.08 (95% CI, 0.75-1.55). In ad- ated. Venous thromboembolism was not specifically exam-
dition, Baillargeon et al17 performed a case-control study of ined as an outcome. At present, there is no compelling evidence
30 000 men and 7500 VTE events identified from a large claims that the association of the risk of VTE with testosterone therapy
database in the United States (OptumInsight). The investiga- varies according to route of exposure.
tors found no significant association in that analysis, in which
158 VTE events among testosterone therapy users occurred and Strengths and Limitations
the focus was on testosterone use in the 15 to 60 days before A strength of this study is the use of a large administrative
the VTE event. That study used a traditional matched case- claims data. To our knowledge, we had the largest number of
control design, and unmeasured time-invariant confound- cases included in a study evaluating testosterone therapy as
ers, such as smoking status and physical activity, could not be a potential VTE risk factor. One of the strengths of the case-
directly addressed in the analyses. Our study corrects for this crossover design is its ability to account for time-invariant un-
unmeasured confounding with the case-crossover design and measured confounding. With patients acting as their own con-
appears to improve on the article by Baillargeon et al17 by hav- trols, relatively static or slowly varying factors (eg, obesity,
ing a larger number of exposed cases (374 testosterone therapy smoking status, and family history of VTE) are assumed to re-
users without hypogonadism and 1330 testosterone therapy main constant during the case and control periods.35 This de-
users with hypogonadism) to analyze different case periods, sign can be particularly useful in the context of administra-
hypogonadism status, and age categories. Findings from tive data with information on important potential covariates
smaller observational studies and randomized clinical (eg, obesity or family history) not available in the data set. An
trials15,30-33 have been inconsistent, with some reporting tes- assumption of the case-crossover design is that exposures are
tosterone therapy to be a risk factor and others reporting no transient. Our exploratory analysis showed that the associa-
association. Other studies6,17,31 recruited only hypogonadal tion of testosterone therapy with VTE was transient because
men or either controlled for or matched men by hypogonad- the association was attenuated within the 3- to 6-month ex-
ism status but did not investigate the association of testoste- posure category compared with the 1-month and 1- to 3-month
rone therapy on the large population of men without hypo- categories.
gonadism who receive it. Use of a large administrative claims database was also a
Furthermore, our study provides novel information about limitation of this study. Other common weaknesses, such as
the time frame of exposure to testosterone therapy and risk misclassification and time-variant confounding found in claims
of VTE. Our exploratory analysis found evidence that risk es- databases, were minimized as best as possible given the data
timates were higher in the 1- to 3-month and less than 1-month available. The VTE definition that we used had a good posi-
case periods compared with the 3- to 6-month case periods. tive predictive value (91%) when validated in a different study
This observation is analogous to patterns seen for oral contra- population.23 We are not aware of any validation studies of hy-
ceptives and VTE risk, whereby women are at greatest risk pogonadism diagnosis or testosterone therapy prescription
shortly after beginning oral contraceptive use, and provides claims. Because there is no consensus regarding how to de-
hypothesis-generating information for future research on tes- fine hypogonadism in administrative data, we used 2 differ-
tosterone therapy and VTE.34 ent definitions: one similar to that used by Martinez et al18 and
Hypogonadism diagnosis, age, and route of testosterone Baillargeon et al17 and another similar to that used by Jasuja
exposure were identified a priori as subgroups of particular in- et al.25 The estimates were similar regardless of which defini-
terest. Among men without hypogonadism, risk was greater tion was used. Studies validating algorithms to define hypo-
among men younger than 65 years compared with those who gonadism in administrative data are needed. The testoste-
were older, although the interaction was not statistically sig- rone therapy codes used in this study were the same as those
nificant. This finding is of potential public health importance used by another claims-based study17 and resulted in preva-
because of recent trends in increased testosterone therapy pre- lence that matched current trend analysis numbers.5 Phar-
scriptions among men younger than 65 years.5 Men younger macy claims reflect whether patients fill their prescriptions;
than 65 years who begin testosterone therapy early to deter however, whether the patient takes the prescription cannot be
common health symptoms potentially associated with aging assessed in administrative data. In addition, despite the large
may be exposing themselves to greater risk of early-onset car- data set, precision of some stratified analyses was not opti-
E6 JAMA Internal Medicine Published online November 11, 2019 (Reprinted) jamainternalmedicine.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a UCSF LIBRARY User on 11/11/2019
Testosterone Therapy and Venous Thromboembolism Risk in Men With and Without Hypogonadism Original Investigation Research
mal because of the sparsity of men prescribed testosterone prescription. These data combined with prior data suggest that
therapy in subcategories. future clinical trials of testosterone therapy, regardless of the
indication, should capture VTE events as part of safety end
points. Relative VTE risk may be exacerbated for men younger
than 65 years using testosterone therapy with and without
Conclusions clinical indications. Men experiencing common symptoms that
Men without cancer who were prescribed testosterone therapy result from natural aging have considered testosterone therapy
in our study’s case period had an increased risk of incident VTE as a treatment; however, men without hypogonadism should
compared with that in an equivalent control period 6 months assess cardiovascular disease risk with their physicians
before the VTE. This risk of VTE was present for men with and before prescription to minimize adverse cardiovascular
without hypogonadism who received a testosterone therapy outcomes.
ARTICLE INFORMATION approval of the manuscript; and decision to submit 10. Petering RC, Brooks NA. Testosterone therapy:
Accepted for Publication: September 3, 2019. the manuscript for publication. review of clinical applications. Am Fam Physician.
2017;96(7):441-449.
Published Online: November 11, 2019. REFERENCES
doi:10.1001/jamainternmed.2019.5135 11. Benjamin EJ, Muntner P, Alonso A, et al;
1. Khera M, Adaikan G, Buvat J, et al. Diagnosis and American Heart Association Council on
Author Affiliations: Division of Epidemiology and treatment of testosterone deficiency: Epidemiology and Prevention Statistics Committee
Community Health, School of Public Health, recommendations from the Fourth International and Stroke Statistics Subcommittee. Heart disease
University of Minnesota, Minneapolis (Walker, Consultation for Sexual Medicine (ICSM 2015). J Sex and stroke statistics-2019 update: a report from the
MacLehose, Lutsey); Department of Medicine, The Med. 2016;13(12):1787-1804. doi:10.1016/j.jsxm. American Heart Association. Circulation. 2019;139
Robert Larner, M.D. College of Medicine, University 2016.10.009 (10):e56-e528. doi:10.1161/CIR.
of Vermont, Burlington (Zakai); Department of 0000000000000659
Pathology and Laboratory Medicine, The Robert 2. Wu FC, Tajar A, Beynon JM, et al; EMAS Group.
Larner, M.D. College of Medicine, University of Identification of late-onset hypogonadism in 12. Holmegard HN, Nordestgaard BG, Schnohr P,
Vermont, Burlington (Zakai); Department of middle-aged and elderly men. N Engl J Med. 2010; Tybjaerg-Hansen A, Benn M. Endogenous sex
Biostatistics, Epidemiology, and Environmental 363(2):123-135. doi:10.1056/NEJMoa0911101 hormones and risk of venous thromboembolism in
Health Sciences, Jiann-Ping Hsu College of Public 3. Buvat J, Maggi M, Guay A, Torres LO. women and men. J Thromb Haemost. 2014;12(3):
Health, Georgia Southern University, Statesboro Testosterone deficiency in men: systematic review 297-305. doi:10.1111/jth.12484
(Cowan); Department of Pharmaceutical Care and and standard operating procedures for diagnosis 13. Ajayi AA, Mathur R, Halushka PV. Testosterone
Health Systems, College of Pharmacy, University of and treatment. J Sex Med. 2013;10(1):245-284. doi: increases human platelet thromboxane A2 receptor
Minnesota, Minneapolis (Adam); Department of 10.1111/j.1743-6109.2012.02783.x density and aggregation responses. Circulation.
Epidemiology, Rollins Emory University School of 4. Corona G, Dicuio M, Rastrelli G, et al. 1995;91(11):2742-2747. doi:10.1161/01.CIR.91.11.2742
Public Health, Atlanta, Georgia (Alonso). Testosterone treatment and cardiovascular and 14. Fernández-Balsells MM, Murad MH, Lane M,
Author Contributions: Mr Walker and Dr Lutsey venous thromboembolism risk: what is ‘new’? et al. Clinical review 1: adverse effects of
had full access to all the data in the study and take J Investig Med. 2017;65(6):964-973. doi:10.1136/ testosterone therapy in adult men: a systematic
responsibility for the integrity of the data and the jim-2017-000411 review and meta-analysis. J Clin Endocrinol Metab.
accuracy of the data analysis. 5. Rao PK, Boulet SL, Mehta A, et al. Trends in 2010;95(6):2560-2575. doi:10.1210/jc.2009-2575
Concept and design: Walker, Zakai, MacLehose, testosterone replacement therapy use from 2003 15. Glueck CJ, Wang P. Testosterone therapy,
Cowan, Lutsey. to 2013 among reproductive-age men in the United thrombosis, thrombophilia, cardiovascular events.
Acquisition, analysis, or interpretation of data: States. J Urol. 2017;197(4):1121-1126. doi:10.1016/j. Metabolism. 2014;63(8):989-994. doi:10.1016/j.
Walker, Zakai, Cowan, Adam, Alonso, Lutsey. juro.2016.10.063 metabol.2014.05.005
Drafting of the manuscript: Walker, Cowan, Lutsey.
Critical revision of the manuscript for important 6. Baillargeon J, Kuo YF, Westra JR, Urban RJ, 16. Shoskes JJ, Wilson MK, Spinner ML.
intellectual content: All authors. Goodwin JS. Testosterone prescribing in the United Pharmacology of testosterone replacement therapy
Statistical analysis: Walker, MacLehose, Cowan. States, 2002-2016. JAMA. 2018;320(2):200-202. preparations. Transl Androl Urol. 2016;5(6):834-843.
Obtained funding: Lutsey. doi:10.1001/jama.2018.7999 doi:10.21037/tau.2016.07.10
Administrative, technical, or material support: 7. Layton JB, Li D, Meier CR, et al. Testosterone lab 17. Baillargeon J, Urban RJ, Morgentaler A, et al.
MacLehose, Cowan, Adam, Lutsey. testing and initiation in the United Kingdom and the Risk of venous thromboembolism in men receiving
Supervision: Zakai, Lutsey. United States, 2000 to 2011. J Clin Endocrinol Metab. testosterone therapy. Mayo Clin Proc. 2015;90(8):
Conflict of Interest Disclosures: Mr Walker and 2014;99(3):835-842. doi:10.1210/jc.2013-3570 1038-1045. doi:10.1016/j.mayocp.2015.05.012
Drs Adam and Lutsey reported receiving grants 8. US Food and Drug Administration. FDA Drug 18. Martinez C, Suissa S, Rietbrock S, et al.
from the National Heart, Lung, and Blood Institute, Safety Communication: FDA Cautions About Using Testosterone treatment and risk of venous
National Institutes of Health during the conduct of Testosterone Products for Low Testosterone Due to thromboembolism: population based case-control
the study. Drs Zakai and Alonso reported receiving Aging; Requires Labeling Change to Inform of study. BMJ. 2016;355:i5968. doi:10.1136/bmj.i5968
grants from National Institutes of Health during the Possible Increased Risk of Heart Attack and Stroke 19. Houghton DE, Alsawas M, Barrioneuvo P, et al.
conduct of the study. No other disclosures were With Use. White Oak, MD: US Food and Drug Testosterone therapy and venous
reported. Administration; March 3, 2015. https://www.fda. thromboembolism: a systematic review and
Funding/Support: This study was funded and gov/drugs/drug-safety-and-availability/fda-drug- meta-analysis. Thromb Res. 2018;172:94-103. doi:
supported by grant R01-HL131579 (Mr Walker and safety-communication-fda-cautions-about-using- 10.1016/j.thromres.2018.10.023
Drs Adam and Lutsey) from the National Heart, testosterone-products-low-testosterone-due.
Accessed October 7, 2019. 20. Birman-Deych E, Waterman AD, Yan Y, Nilasena
Lung, and Blood Institute, National Institutes DS, Radford MJ, Gage BF. Accuracy of ICD-9-CM
of Health. 9. US Food and Drug Administration. Testosterone codes for identifying cardiovascular and stroke risk
Role of the Funder/Sponsor: The funding source Products: FDA/CDER Statement—Risk of Venous factors. Med Care. 2005;43(5):480-485. doi:10.
had no role in the design and conduct of the study; Blood Clots. White Oak, MD: US Food and Drug 1097/01.mlr.0000160417.39497.a9
collection, management, analysis, and Administration; June 20, 2014. http://www.
safetyalertregistry.com/alerts/2558. Accessed 21. Cushman M, Tsai AW, White RH, et al. Deep vein
interpretation of the data; preparation, review, or thrombosis and pulmonary embolism in two
October 9, 2019.
cohorts: the longitudinal investigation of
jamainternalmedicine.com (Reprinted) JAMA Internal Medicine Published online November 11, 2019 E7
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a UCSF LIBRARY User on 11/11/2019
Research Original Investigation Testosterone Therapy and Venous Thromboembolism Risk in Men With and Without Hypogonadism
thromboembolism etiology. Am J Med. 2004;117(1): 26. Rogers MA, Levine DA, Blumberg N, Flanders 31. Ramasamy R, Scovell J, Mederos M, Ren R, Jain
19-25. doi:10.1016/j.amjmed.2004.01.018 SA, Chopra V, Langa KM. Triggers of hospitalization L, Lipshultz L. Association between testosterone
22. Fang MC, Fan D, Sung SH, et al. Validity of using for venous thromboembolism. Circulation. 2012;125 supplementation therapy and thrombotic events in
inpatient and outpatient administrative codes to (17):2092-2099. doi:10.1161/CIRCULATIONAHA.111. elderly men. Urology. 2015;86(2):283-285. doi:10.
identify acute venous thromboembolism: the CVRN 084467 1016/j.urology.2015.03.049
VTE study. Med Care. 2017;55(12):e137-e143. doi: 27. Bjøri E, Johnsen HS, Hansen JB, Brækkan SK. 32. Sharma R, Oni OA, Chen G, et al. Association
10.1097/MLR.0000000000000524 Hospitalization as a trigger for venous between testosterone replacement therapy and the
23. Sanfilippo KM, Wang TF, Gage BF, Liu W, Carson thromboembolism: results from a population-based incidence of DVT and pulmonary embolism:
KR. Improving accuracy of International case-crossover study. Thromb Res. 2019;176:115-119. a retrospective cohort study of the Veterans
Classification of Diseases codes for venous doi:10.1016/j.thromres.2019.02.024 Administration database. Chest. 2016;150(3):563-
thromboembolism in administrative data. Thromb 28. Tan RS, Cook KR, Reilly WG. Myocardial 571. doi:10.1016/j.chest.2016.05.007
Res. 2015;135(4):616-620. doi:10.1016/j. infarction and stroke risk in young healthy men 33. Borst SE, Shuster JJ, Zou B, et al. Cardiovascular
thromres.2015.01.012 treated with injectable testosterone. Int J Endocrinol. risks and elevation of serum DHT vary by route of
24. Bhasin S, Brito JP, Cunningham GR, et al. 2015;2015:970750. doi:10.1155/2015/970750 testosterone administration: a systematic review
Testosterone therapy in men with hypogonadism: 29. Vigen R, O’Donnell CI, Barón AE, et al. and meta-analysis. BMC Med. 2014;12:211. doi:10.
an Endocrine Society Clinical Practice Guideline. Association of testosterone therapy with mortality, 1186/s12916-014-0211-5
J Clin Endocrinol Metab. 2018;103(5):1715-1744. doi: myocardial infarction, and stroke in men with low 34. Gialeraki A, Valsami S, Pittaras T,
10.1210/jc.2018-00229 testosterone levels. JAMA. 2013;310(17):1829-1836. Panayiotakopoulos G, Politou M. Oral
25. Jasuja GK, Bhasin S, Reisman JI, et al. Who gets doi:10.1001/jama.2013.280386 contraceptives and HRT risk of thrombosis. Clin
testosterone? patient characteristics associated 30. Glueck CJ, Prince M, Patel N, et al. Appl Thromb Hemost. 2018;24(2):217-225. doi:10.
with testosterone prescribing in the Veteran Affairs Thrombophilia in 67 patients with thrombotic 1177/1076029616683802
System: a cross-sectional study. J Gen Intern Med. events after starting testosterone therapy. Clin Appl 35. Mittleman MA, Mostofsky E. Exchangeability in
2017;32(3):304-311. doi:10.1007/s11606-016- Thromb Hemost. 2016;22(6):548-553. doi:10.1177/ the case-crossover design. Int J Epidemiol. 2014;43
3940-7 1076029615619486 (5):1645-1655. doi:10.1093/ije/dyu081
E8 JAMA Internal Medicine Published online November 11, 2019 (Reprinted) jamainternalmedicine.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a UCSF LIBRARY User on 11/11/2019
You might also like
- Testosterone Resistance: Fighting for the Men’S Health HormoneFrom EverandTestosterone Resistance: Fighting for the Men’S Health HormoneNo ratings yet
- Alternatives To Testosterone Therapy - Eric Lo, Et AlDocument8 pagesAlternatives To Testosterone Therapy - Eric Lo, Et AlRENENo ratings yet
- Testosterone Therapy For Transgender Men: ReviewDocument11 pagesTestosterone Therapy For Transgender Men: ReviewJuanNo ratings yet
- Oestrogen and Anti-Androgen Therapy For Transgender WomenDocument10 pagesOestrogen and Anti-Androgen Therapy For Transgender WomenHugo GushikenNo ratings yet
- AndrologyDocument298 pagesAndrologyPrakash JanakiramanNo ratings yet
- Testosterone Deficiency and Replacement in Older Men: (Journal of The Norwegian Medical Association)Document3 pagesTestosterone Deficiency and Replacement in Older Men: (Journal of The Norwegian Medical Association)ehg770271No ratings yet
- Hormonios e Trans... Maturitas (Exemplos Do Que Fazer No Meu, Resultados Importantes)Document20 pagesHormonios e Trans... Maturitas (Exemplos Do Que Fazer No Meu, Resultados Importantes)Higor FerreiraNo ratings yet
- Acne Fulminans in A Transgender Boy After An Increase in TestosteroneDocument3 pagesAcne Fulminans in A Transgender Boy After An Increase in TestosteroneMilikPremiumstock90No ratings yet
- CollegePharmacy BHRT Abstracts ReviewsDocument46 pagesCollegePharmacy BHRT Abstracts ReviewsJoyce IpadNo ratings yet
- (Bhasin) Lições Aprendidas Sobre Testosterona TrialsDocument18 pages(Bhasin) Lições Aprendidas Sobre Testosterona TrialsIlfran Magalhães Silva IINo ratings yet
- Testosterone Therapy: Many Players and Much Controversy: VOL. 103 NO. 5 / MAY 2015Document2 pagesTestosterone Therapy: Many Players and Much Controversy: VOL. 103 NO. 5 / MAY 2015Pangala NitaNo ratings yet
- Hipogonadismo MasculinoDocument2 pagesHipogonadismo MasculinoTony Miguel Saba SabaNo ratings yet
- Journal of Sports Medicine, 18:557-62, 1992. Between Questioned MenDocument4 pagesJournal of Sports Medicine, 18:557-62, 1992. Between Questioned MenMaurício DâmasoNo ratings yet
- Do Statins Lower TestosteroneDocument3 pagesDo Statins Lower TestosteroneNandia SeptiyoriniNo ratings yet
- Testosterone: How To Maximize Benefits and Minimize Side EffectsDocument14 pagesTestosterone: How To Maximize Benefits and Minimize Side Effectsnelsonvergel100% (3)
- Testosterone Deficiency JUDocument10 pagesTestosterone Deficiency JUbrandon rodriguezNo ratings yet
- Andropause Current ConceptsDocument9 pagesAndropause Current ConceptsHAVIZ YUADNo ratings yet
- Testosterone Therapy in Men With Androgen Deficiency Syndromes: An Endocrine Society Clinical Practice GuidelineDocument24 pagesTestosterone Therapy in Men With Androgen Deficiency Syndromes: An Endocrine Society Clinical Practice GuidelineHeidy Bravo RamosNo ratings yet
- Testosterone Implants Benefits and MythsDocument7 pagesTestosterone Implants Benefits and MythsSmartway PharmaceuticalsNo ratings yet
- Benefits and Risks of Testosterone Treatment of Older Men With HypogonadismDocument10 pagesBenefits and Risks of Testosterone Treatment of Older Men With HypogonadismPaolo MessinaNo ratings yet
- Low Testosterone in Male Cancer Patients and SurvivorsDocument4 pagesLow Testosterone in Male Cancer Patients and SurvivorsfrankiesdumpsterNo ratings yet
- Blood Testosterone Threshold For Androgen Deficiency SymptomsDocument5 pagesBlood Testosterone Threshold For Androgen Deficiency SymptomsLukaNo ratings yet
- Association of Testosterone and Anemia in OlderDocument11 pagesAssociation of Testosterone and Anemia in OlderRaja Iqbal Mulya HarahapNo ratings yet
- Bhasin Testosterone Guidelines 2018Document30 pagesBhasin Testosterone Guidelines 2018KINETO62No ratings yet
- Andrology - 2017 - Velho - Effects of Testosterone Therapy On BMI... (Resultados Esperados)Document8 pagesAndrology - 2017 - Velho - Effects of Testosterone Therapy On BMI... (Resultados Esperados)Higor FerreiraNo ratings yet
- Are Men at RiskDocument9 pagesAre Men at Riskapi-567522710No ratings yet
- Efeitos Da Terapia Hormonal Nos Lipides Trans (Discussão (Os Anteriores Também) e Resultados Esperados)Document13 pagesEfeitos Da Terapia Hormonal Nos Lipides Trans (Discussão (Os Anteriores Também) e Resultados Esperados)Higor FerreiraNo ratings yet
- Nahata, Chen, Moravek, Quinn, Sutter, Taylor, Tishelman, & Gomez-Lobo, 2019Document7 pagesNahata, Chen, Moravek, Quinn, Sutter, Taylor, Tishelman, & Gomez-Lobo, 2019Anonymous 75M6uB3OwNo ratings yet
- JC 2018-00229 PDFDocument30 pagesJC 2018-00229 PDFEmrahNo ratings yet
- 2016 04 Lancet Article Testosterone Therapy TransgenderDocument3 pages2016 04 Lancet Article Testosterone Therapy TransgenderManuela Martín-Bejarano GarcíaNo ratings yet
- Individualized Medicine: Sex, Hormones, Genetics, and Adverse Drug ReactionsDocument9 pagesIndividualized Medicine: Sex, Hormones, Genetics, and Adverse Drug ReactionsrosianaNo ratings yet
- JGR 3 019Document7 pagesJGR 3 019patgarettNo ratings yet
- Testosterone Research PaperDocument8 pagesTestosterone Research Paperfvf442bf100% (1)
- Ageing Research Reviews: Nikolai Jaschke, Andrew Wang, Lorenz C. Hofbauer, Martina Rauner, Tilman D. RachnerDocument8 pagesAgeing Research Reviews: Nikolai Jaschke, Andrew Wang, Lorenz C. Hofbauer, Martina Rauner, Tilman D. RachnerRares SanduNo ratings yet
- Testosterone Replacement Therapy and Components of The Metabolic SyndromeDocument11 pagesTestosterone Replacement Therapy and Components of The Metabolic SyndromeOscar PonceNo ratings yet
- 1-S2.0-S0889159103000783-Main XXXDocument8 pages1-S2.0-S0889159103000783-Main XXXSaiber PanNo ratings yet
- Do Androgens Modulate The Pathophysiological Pathways of InflammationDocument30 pagesDo Androgens Modulate The Pathophysiological Pathways of Inflammationendro purwokoNo ratings yet
- Testosterone Supplementation in Men: A Practical Guide For The Gynecologist and ObstetricianDocument7 pagesTestosterone Supplementation in Men: A Practical Guide For The Gynecologist and ObstetricianAnca CucuNo ratings yet
- (14796813 - Journal of Molecular Endocrinology) Hormone Therapy and Breast Cancer - Emerging Steroid Receptor MechanismsDocument28 pages(14796813 - Journal of Molecular Endocrinology) Hormone Therapy and Breast Cancer - Emerging Steroid Receptor MechanismsThiago TvborgesNo ratings yet
- Truth About TestosteroneDocument34 pagesTruth About TestosteroneNaturalBioHealthNo ratings yet
- Andrology - 2017 - Semet - The Impact of Drugs On Male Fertility A ReviewDocument24 pagesAndrology - 2017 - Semet - The Impact of Drugs On Male Fertility A ReviewAbhishek RampalNo ratings yet
- TestosteronaDocument11 pagesTestosteronaJoão CaetanoNo ratings yet
- Soldera 2018Document8 pagesSoldera 2018chemistpl420No ratings yet
- Hormone Replacement Therapy in Cancer SurvivorsDocument13 pagesHormone Replacement Therapy in Cancer Survivorsiulia bNo ratings yet
- Postmenopausal Hormone Therapy and MortalityDocument7 pagesPostmenopausal Hormone Therapy and MortalityElenita BastosNo ratings yet
- Troponinas CardiacasDocument4 pagesTroponinas CardiacasDANNA SOPHIA RAMIREZ TOLENo ratings yet
- The Effects of Short-Term and Long-TermDocument7 pagesThe Effects of Short-Term and Long-Termdouglas 87No ratings yet
- Psychiatry Research: Review ArticleDocument7 pagesPsychiatry Research: Review ArticlejhuNo ratings yet
- Exogenous Testosterone Does Not Induce or Exacerbate The Metabol 2018 (Parecido Com Minha Ideia, Usar o Método)Document25 pagesExogenous Testosterone Does Not Induce or Exacerbate The Metabol 2018 (Parecido Com Minha Ideia, Usar o Método)Higor FerreiraNo ratings yet
- Bvad 040Document7 pagesBvad 040pump BlumpNo ratings yet
- Gene Therapy Julie C. Casper Usha Palaniswamy Introduction To Biology March 3, 2014Document8 pagesGene Therapy Julie C. Casper Usha Palaniswamy Introduction To Biology March 3, 2014Julie Crumpler CasperNo ratings yet
- Impact of Early Medical Treatment For Transgender Youth: Protocol For The Longitudinal, Observational Trans Youth Care StudyDocument10 pagesImpact of Early Medical Treatment For Transgender Youth: Protocol For The Longitudinal, Observational Trans Youth Care StudycatalinavillenaNo ratings yet
- Male Hormonal Contraception: Looking Back and Moving ForwardDocument9 pagesMale Hormonal Contraception: Looking Back and Moving ForwardAbian MursyidNo ratings yet
- Serum Testosterone Levels in Male Hypogonadism - Why and When To Check-A Review 2017Document9 pagesSerum Testosterone Levels in Male Hypogonadism - Why and When To Check-A Review 2017Sara Velásquez JNo ratings yet
- Trazodone - Erectile DysfunctionDocument6 pagesTrazodone - Erectile DysfunctionteddypolNo ratings yet
- Screenshot 2023-04-23 at 12.23.43 PM PDFDocument5 pagesScreenshot 2023-04-23 at 12.23.43 PM PDFAditya ChakureNo ratings yet
- Rethinking Postmenopausal Hormone TherapyDocument2 pagesRethinking Postmenopausal Hormone TherapyDanielle Moon100% (1)
- Sex Differences in Anxiety and Depression Role of TestosteroneDocument35 pagesSex Differences in Anxiety and Depression Role of Testosteronepopa.irinaNo ratings yet
- Terapia Hormonal en La Menopausia Conceptos Controversias y Abordaje Del TratamientoDocument33 pagesTerapia Hormonal en La Menopausia Conceptos Controversias y Abordaje Del TratamientoHugo Corrales-SantanderNo ratings yet
- Patho SlidesDocument79 pagesPatho SlidesFYMNo ratings yet
- 02-05-15 EditionDocument28 pages02-05-15 EditionSan Mateo Daily JournalNo ratings yet
- CV AliDocument8 pagesCV AliCryptic SufiNo ratings yet
- Greatest Breakthrough in Medical History Keith Kohl 29Document29 pagesGreatest Breakthrough in Medical History Keith Kohl 29Jonas BarbosaNo ratings yet
- MCQs Endo FinalDocument6 pagesMCQs Endo Finalhassan qureshiNo ratings yet
- Template Laporan Data Covid-19 Yang DirawatDocument10 pagesTemplate Laporan Data Covid-19 Yang DirawatMita AdyaNo ratings yet
- Asphyxia 2Document55 pagesAsphyxia 2api-19916399100% (1)
- HypothyroidismDocument10 pagesHypothyroidismJayson TrajanoNo ratings yet
- First Aid Level 1 Learner Guide 2014Document94 pagesFirst Aid Level 1 Learner Guide 2014Ndaba ZamsNo ratings yet
- GATKwr8 S 3 Variant Calling With MuTectDocument37 pagesGATKwr8 S 3 Variant Calling With MuTectKartikeya SinghNo ratings yet
- Mental Health in IndiaDocument6 pagesMental Health in IndiaStarlin MythriNo ratings yet
- Disease Deep Dive Kathryn CrimDocument7 pagesDisease Deep Dive Kathryn Crimapi-579320483No ratings yet
- Challenges in Commercial Pig Production in Botswan PDFDocument11 pagesChallenges in Commercial Pig Production in Botswan PDFMbiganyi MfumiNo ratings yet
- Psychiatric NursingDocument21 pagesPsychiatric NursingFreeNursingNotes92% (38)
- Major Insect Pest Management of Sugarcane CropDocument11 pagesMajor Insect Pest Management of Sugarcane CropAbdul GhaffarNo ratings yet
- CHCAGE001 PPSlides V1.0Document86 pagesCHCAGE001 PPSlides V1.0Leanne EvansNo ratings yet
- Classification of Vacutainer Tubes by Color and FunctionDocument5 pagesClassification of Vacutainer Tubes by Color and FunctionNandor SiliNo ratings yet
- Name: - Teacher: - Gade and Section: - DateDocument3 pagesName: - Teacher: - Gade and Section: - DateDhess Mulleda MantalaNo ratings yet
- Family of TilikumDocument1 pageFamily of TilikumThe Orca Project Corp100% (1)
- Diacalauto en DT Rev03 0851501 Rev02Document8 pagesDiacalauto en DT Rev03 0851501 Rev02vijayramaswamy0% (1)
- Wikipedia Withania SomniferaDocument4 pagesWikipedia Withania SomniferasonostufodiprovareNo ratings yet
- Name - How To Make A Gardening JournalDocument2 pagesName - How To Make A Gardening JournalDiana Gomez ObleaNo ratings yet
- Flyash Msds KenzoDocument5 pagesFlyash Msds KenzoErianto XuNo ratings yet
- Thermit PortionsDocument9 pagesThermit PortionsMix MiscevicNo ratings yet
- Laboratory Evaluation of PlateletsDocument4 pagesLaboratory Evaluation of Plateletscherry nokiaNo ratings yet
- 1628083670Document332 pages1628083670bmj123No ratings yet
- Dermatology Chap6. Bacterial Infections of Skin 2020-3-23Document368 pagesDermatology Chap6. Bacterial Infections of Skin 2020-3-23Mohsin Tanmoy100% (1)
- Structure of Chemical Componds ImpuritiesDocument6 pagesStructure of Chemical Componds ImpuritiesJorge Oswaldo Toro Jaimes100% (1)
- Appendicitis Pregnancy ElnasharDocument47 pagesAppendicitis Pregnancy ElnasharErwynsonsaut SimanjuntakNo ratings yet
- Giger and DavidhizarDocument4 pagesGiger and DavidhizarHv EstokNo ratings yet