Professional Documents
Culture Documents
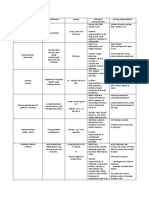
Electrolyte Summary Notes
Uploaded by
nurhana faudzi0 ratings0% found this document useful (0 votes)
17 views9 pagesnot a full version
Original Title
ELECTROLYTE SUMMARY NOTES
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentnot a full version
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
17 views9 pagesElectrolyte Summary Notes
Uploaded by
nurhana faudzinot a full version
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 9
UNIT 1.1 ANAEMIA 7.
Diaphoresis with exertion (excessive sweating due
ANEMIA: Condition of having a lower-than-normal to > metabolism)
numbers of haemoglobin where Hb value is < 12.5 8. Chronic fatigue
g/dL in adult (N: 14-18) DIAGNOSTIC TEST
COMPOSITION OF BLOOD 1. CBC - determine number of RBC & WBC
1. Plasma (55%) 2. Hemoglobin - measure level of Hb in blood
2. Blood cells (45%) 3. Hematocrit - % by volume of RBC in blood
PLASMA 4. Serum iron - measure num. of iron in blood
1. Plasma Protein 5. Serum ferritin - measure level of ferritin in blood
- Albumins (maintains osmotic pressure in blood) 6. Serum folate - check if have enough folate
- Globulins (provide immunity & antibody) MANAGEMENT
- Fibrinogen (clotting factor) 1. Blood transfusion (quickly > RBC in blood)
2. Minerals (cell formation, muscle contraction, 2. > intake of deficient nutrient (best sources of iron)
maintain blood pH) 3. Dietary supplement (iron supplement to > Hb
3. Nutrients (provide energy & heat, fix & replace level)
cells) 4. Changing cooking habit (high protein to > iron
4. Organic waste products (excreted by liver, kidney, absorption)
lungs) 5. < alcohol intake (RBC be destroyed prematurely)
5. Hormones (influences cellular activity) UNIT 1.2 IRON DEFICIENCY ANEMIA
6. Gases (O2 & CO2) DEFINITION – Chronic, hypochromic and microcytic
BLOOD CELLS anaemia due to the insufficient iron in red blood cell
1. Erythrocytes (RBC) that leads to low level of haemoglobin.
2. Leukocytes (WBC) CAUSES
3. Thrombocytes (Platelet) 1. Increased iron loss - GIT bleeding, Hemoptysis,
PRODUCTION OF RBC (erythropoiesis) Haematuria, Menorrhagia, Chronic hemorrhage
1. Stimulus < RBC count and availability of O2, > tissue 2. Decreased Iron Absorption - Malnutrition,
demand for O2 Imbalanced diet intake
2. < O2 level in blood 3. Decreased Iron Absorption - Celiac disease (gene
3. Kidney releases erythropoietin disorder characterized by autoimmune reaction to
4. Erythropoietin stimulate bone marrow ingestion of gluten & destroy small intestine),
5. More RBC produced inflammatory bowel disease, partial gastrectomy
6. > O2 carrying ability of blood 4. Increased Iron Requirements - Pregnancy,
CLASSIFICATION Lactation
1. Hypoproliferative Anemia RISK FACTORS
- underproduction of RBC production 1. Pregnancy - due to lactation process
2. Bleeding 2. Menorrhagia - loss of blood > 7d
- RBC loss 3. Strict vegetarian diets - low intake of iron
3. Hemolytic 4. Older population - reduced in iron absorption
- RBC destruction PATHOPHISIOLOGY
HYPOPROLIFERATIVE ANEMIA 1. Inadequate iron (low intake, absorption loss)
1. Iron deficiency anemia 2. Low formation of Hb
- microcytic hypochromic (large size, < colour) 3. Low Hb level leads to anaemia (signs & symptoms)
2. Vitamin B12 deficiency anemia CLINICAL MANIFESTATION
- macrocytic normochromic (large size, N colour) 1. Asymptomatic unless severe
3. Folic acid deficiency anemia 2. Fatigue
- macrocytic hypochromic (large size, < colour) 3. Headache
PATHOPHYSIOLOGY 4. Dyspnea
1. Lack of RBC reduces O2 being carried 5. Palpitations
2. Inadequate O2 to tissue 6. Pallor
3. Resulting in tissue hypoxia 7. Angular stomatitis (swollen/redness at end of lips)
4. Body attempts to compensate 8. Dizziness
5. > cardiac output by > stroke volume/heart rate 9. Glossitis (inflammation of tongue)
* CO: total blood pumps out by ventricle in a min 10. Cheilosis (inflammation of lips)
* SV: volume of blood pumps out by ventricle each 11. Brittle nails & spoon-shaped nails
contraction (N: 70) DIAGNOSTIC TEST
CLINICAL MANIFESTATION 1. Blood Test
1. Pallor (pale skin colour) - FBC
2. Tachycardia (> PR) - Hematocrit
3. Tachypnea (> RR) - Hemoglobin
4. Dyspnea(difficulty in breathing) - Serum iron
5. Palpitations (noticeably rapid HR) - Serum ferritin
6. Dizziness TIBC (total iron binding capacity) >
- FBC (full blood picture) CLINICAL MANIFESTATION
2. Radiographic Study 1. Weight loss
- OGDS (esophagogastroduodenoscopy) 2. Poor appetite
- gastroscopy 3. Nausea
- sigmoidoscopy 4. Vomiting
3. Stool for occult blood (FOBT) 5. Abdominal distension
- detect the hidden blood in feces 6. Diarrhea
MANAGEMENT 7. Constipation
1. Diagnosis & correction of underlying cause 8. Neurologic disorder (paresthesia, memory loss
2. Diet modification (high iron food) depression, cognitive prob)
3. Supplemental iron DIAGNOSTIC TEST
4. Monitoring on the compliant on treatment 1. Blood Test
5. Change of lifestyle (avoid alcohol & correct cooking - FBC
method) - FBP
IRON ABSOPRTION - Reticulocyte count (measure RBC to evaluate bone
INHIBITING marrow in producing RBC/low reticulocyte)
1. Coffee and tea (tannins inhibits absorption) - Hb & HCT level
2. Milk (casein binds to iron & slow down absorption) - Cobalamin Test (measure how much VB12 in blood)
3. Dietary supplement contained Ca, Zn, Mg or Cu - Schilling Test (oral radioactive VB12>check
(compete for absorption) urine>absence means PA) *not practice now
4. Antacid, H2 blockers & proton pump inhibitors MEDICAL MANAGEMENT
(neutralizes stomach acid) 1. Cobalamin Therapy
5. Tetracycline antibiotics (ferrous sulphate < - Lifelong therapy
absorption) - Parental administration of VB12 (injection)
FACILITING - cyanocobalamin/hydroxocobalamin
1. Vitamin C (acidic foods) UNIT 1.4 - FOLIC ACID DEFICIENCY ANAMEIA
2. Non enteric coated iron tablets (to protect iron in DEFINITION - Insufficient of Folic acid (VitB) for the
gastric environment) formation of heme, pigmented, iron-containing
3. Fasting ingestion of iron supplement (absorb portion of haemoglobin in RBC
better when fasting for about 8h) ETIOLOGY
HEALTH TEACHING ON TAKING IRON SUPPLEMET 1. Diet
1. Take iron tablet on empty stomach (absorption < Lack intake of green leafy vegetables, fruits
with foods) & nuts
2. > intake of Vit C (enhance iron absorption) 2. Chronic alcoholism
3. Encourage intake of high fibres (minimize Impairs folate absorption in small intestine
constipation) 3. Eating disorder
4. Remind pt that stool will be dark colour (due to the Anorexia causes not eating foods
active agent in iron pills) containing folic acid
COMPLICATIONS 4. Hemodialysis patient
1. Heart failure - low Hb to carry O2 Remove folate by diffusion & lead to a
2. Problems during pregnancy - premature births & deficiency after several weeks of therapy
low weight of baby 5. Medications such as long-term use of anti-
3. Growth problems - delay growth & development convulsant medications
4. Susceptibility to infections - prone to get one Medications can antagonize folate
UNIT 1.3 - PERNICIOUS ANAEMIA utilization & inhibit its absorption
DEFINITION - Autoimmune disorder characterized by CLINICAL MANIFESTATION
the absence of intrinsic factor in gastric secretions, 1. Weight loss
leading to malabsorption of cobalamin (VitB12) 2. Poor appetite
ETIOLOGY & RISK FACTORS 3. Nausea
1. Gastric Atrophy 4. Vomiting
- no parietal cell so intrinsic factor can’t be produced 5. Abdominal distension
2. Loss of intrinsic factor or loss of parietal cells 6. Diarrhea
- gastrectomy 7. Constipation
- ileal resection UNIT 1.5 - BLOOD TRANSFUSSION
- congenital DEFINITION - Procedure of administering whole
PATHOPHYSIOLOGY blood or blood components via intravenous route
1. < or no cobalamin PURPOSE
2. Impaired DNA synthesis & cell replication 1. To replace circulatory blood volume
3. RBC precursor (erythroblast /reticulocyte) don’t 2. To replace plasma loss by replacing plasma protein
divide normally & RBC poorly function 3. To correct any blood components deficiency
4. Production of myelin on nerve is affected = Packed cells
neurologic deterioration Platelets concentration
Cryoprecipitate (clotting factors) - systemic disorder occurs when immune
TYPE OF BLOOD PRODCUCT cell recognize host as foreign & attack them
1. Whole Blood Infection
Large amount contains plasma & osmotic - sepsis
components (albumin) to help draw fluid 9. Check for accuracy & completeness of
back into vessels from surrounding tissue documentation
2. Packed RBC (PRBC) I/O chart
Made up of removal of virtually all plasma Observation chart
to > O2 level Nursing notes (time start, time completion,
3. Fresh Frozen Plasma (FFP) reactions)
To > clotting factor level, albumin, globulin NURSING RESPONSIBILITY BEFORE
& fibrinogen 1. Blood must be transfused within 30min after it had
4. Cryoprecipitate been collected to prevent bacterial growth &
Consist all clotting factors (fibrinogen, destruction of RBC
Factor VIII, Factor IX) 2. Practice aseptic technique when administer blood
5. Platelet concentrate (50ml) transfusion
To > platelet count in dengue patient 3. Blood transfusion must be counterchecked with
CALCULATION OF DROP PER MIN another SN regarding:
mls ordered x 20 (drop factor fixed) Name
min Age
TIME FRAME FOR TRANSFUSSION Sex
1. Whole blood: within 4 hours Blood group
2. Packed cells: within 4 hours Date of expiry
3. FFP: Within 30 mins 4. Check for signed consent for transfusion for
4. Cryoprecipitate: within 30 mins medical legal purpose
5. Platelets concentrate: within 30 mins 5. Inform pt & explain procedure to allay anxiety &
BLOOD TRANSFUSSION gain cooperation
1. Obtained from blood bank after branulla is 6. Ask pt to pass urine to ensure pt is comfortable
inserted during procedure
2. Confirm pt’s identification 7. Insert large bore of branulla (20G)
Wrist band 8. Check IV canulla is present
Pt state name) 9. Check pt’s bital sign for baseline data to detect any
3. Confirm prescription by checking the doc order transfusion reaction
Verify right blood with doc 10. Administer IV diuretics as ordered prior to
Verify right blood transfusion type transfusion to prevent pulmonary edema
Verify screening 11. Assess pt:
Verify expiry date Itching
Verify consent Hives
4. Perform baseline monitoring of vital sign Fever & chills
BP (1st h: every 15mins, 2nd h: every SOB
30mins, 3rd h: hourly) Swelling
5. Prime line with 0.9% N/S. Infuse first 50ml of N/S Backache
6. Transfuse blood pack & titrate flow rate NURSING RESPONSIBILITY DURING
accordingly 1. Blood to be transfused within 30min after removal
Start transfusion with 10dpm from refrigerator
Monitor pt within first 15mins of 2. Observe flow rate of blood transfusion
transfusion (restlessness, hives, SOB, 3. Observe infusion site for extravasation or branulla
nausea/vomit, flushing, fever/chills, dislodgement
hematuria) 4. Ensure tubing is not kinked & no air bubble &
Check vital sign hourly till completed blood clot
7. Monitor time limit of transfusion 5. Observe pt closely for any reaction & monitor vital
Inform pt time of completion sign
8. Identify reactions 6. Inform pt about sign & symptoms of reaction &
Febrile non-hemolytic transfusion reaction advice to report to nurse or doc
- fever > 38’C 7. Maintain I/O chart balance
Acute hemolytic transfusion reaction (triad 8. Duration of transfusion don’t exceed 4h due to >
components) risk of bacterial proliferation
- fever, flank pain, red/brown urine 9. Never inject any med into branulla with blood
Anaphylactic reaction because bacterial contamination of blood product
- acute BP drop & airways narrow 10. Change blood tubing each time for a new pack
Transfusion-associated graft-vs-host NURSING RESPONSIBILITY AFTER
disease (GVHD) 1. Dispose used material into clinical waste
2. Empty blood packs to be returned to blood bank 4. Bacterial & viral infections such as TB & hepatitis
according to hosp policy Supress 3 cells line caused pancytopenia
3. N/S solution should be infused after transfusion is PATHOPHYSIOLOGY
completed to flush the line BM become > fatty cells, < in hemopoietic cell
ADVERSE REACTIONS II
1. Febril Non-hemolytic reaction Insufficient RBC
Due to presence of donor leukocytes II
Treat with antipyretics Resulting in pancytopenia
2. Acute Hemolytic reaction CLINICAL MENIFESTATIONS
Due to incompatible of donor & recipient’s 1. Result in < Hb, < O2 transport, lead to weakness
blood Fatigue
Most dangerous Pallor
3. Allergic reaction SOB
Due to sensitivity reaction to plasma Tachycardia & heart failure
protein Headache
Treat with antihistamine BM failure
4. Anaphylactic reaction Bleeding
Treat with adrenaline, corticosteroid (anti- Infection
inflammatory) Bruises
5. Circulatory overload DIAGNOSTIC TEST
Due to fast blood flow 1. Blood test
Treat with diuretics FBC - Hb <7gm, RBC normocytic
Dyspnea, tachycardia, jugular vein < total iron binding capacity
distension > Iron serum level
6. Infection (sepsis) 2. Bone marrow Biopsy
Due to delay of transfusion, > 4h Dry tap: Condition when no marrow in
NURSING MANAGEMENT FOR REACTION aspiration
1. Stop transfusion temporarily & inform doc Blood tap: Obtain blood but no marrow
2. St up N/S infusion (another site) at low rate particle from aspiration
3. Send blood pack & tubing to blood bank for repeat MANAGEMENT
typing & culture 1. Early identification & correction of underlying prob
4. Obtain blood specimen for blood investigation in 2. Most measure aims at prevention of infection &
laboratory bleeding
5. Obtain urine specimen for investigation in lab to 3. BM transplant
detect hemoglobin in urine 4. Medication
6. Monitor pt’s vital sign Erythropoietin stimulates production of
7. Monitor urine output RBC
8. Fill in “Adverse Transfusion Reaction Report Form” Filgrastim stimulates production of WBC
9. Document reactions & actions in nursing notes IV anti-thymosin immunoglobulin
UNIT 2.1 APLASTIC ANEMIA - Action: kill T-lymphocyte in immune
DEFINITION system to prevent it from attacking BM
Disorder of unknown etiology characterized stem cells
by low num. of WBC (leukopenia) & low - Given by IV for 8-12 a day for 4 days
platelet count (thrombocytopenia) PREVENT INFECTION
resulting from aplasia of bone marrow 1. Prevent high risk places
(bone marrow w/o its tissue) Crowded
Condition where bone marrow doesn’t Hospital
produce sufficient new cells to replenish 2. Personal hygiene
blood cells Mask
*Pancytopenia: lower counts of RBC, WBC &
Hand washing
platelets
3. Antibiotic
ETIOLOGY Whenever have infection
1. Congenital Non-prophylactic is important of normal
Trait abnormality since birth such as flora
immune system attacks stem cells in BM PREVENT HEMORRHAGE
2. Exposure to toxic substances such as industrial
1. Transfuse 6-8 units of platelet when there’s
chemicals
haemorrhage
Benzenes
TREAT ANEMIA
3. Chemotherapy medications
1. Keep Hb 12-14mg%
Temporary side effects due to
2. Donor blood < 24h
chemotherapy drugs damage healthy stem
3. Repeat transfusion after 6-8 weeks when Hb<7-9
cells
BONE MARROW
1. Done to pt <40y 2. Anterior superior iliac chest
2. Procedure pt who can’t lie on their abdomen
Immunosuppressive drug 3. Sternum
- 2-3 weeks pt don’t have immunity only in adults & kids > 12y, only aspiration
- isolate pt to avoid acquire disease dangerous
Transplant intravenously 4. Anterior medial surface of tibia
After 3 weeks, pt regains immune function infants < 1y
& hemopoietic cells 5. Spinous process of L3-L4 vertebrae
To prevent host versus graft reaction rarely used
Complication is 50% liver failure resulting INSTRUMENTS REQUIRED
from host versus graft reaction 1. 16-18 gauge, 1-1 ¾ inch BM biopsy needle
MEDICATION 2. 10-20ml sterile syringe
1. IV anti-thymocyte immunoglobulin for 1 week 3. Clean slide
2. Anabolic agent for mild aplastic anemia 4. Clear petri or watch glass
(100mg) 6-12month 5. EDTA & saline
3. High dose of corticosteroid 6. Surgery prep. Equipment
Osteoporotic fracture, susceptibility to 7. Sedative/anesthesia
infection glucose intolerance NURSING RESPONSIBILITY AFTER
4. Epoetin Injection 1. Make sure pt comfortable
Stimulate RBC production in BM 2. Maintain supine position for 6h if taken from iliac
PROGNOSIS OF APLASTIC ANEMIA crest, lie pt on affected site
1. Difficult to predict 3. Observe client
2. Very serious vital sign
Die within 6 month – 1 year after hematoma
presentation of symptoms pain/discomfort
UNIT 2.2 BONE MARROW puncture after 48h for warmth & redness
Perform when peripheral blood smears 4. Ensure specimen is labelled correctly with form
failed to diagnose the abnormalities & 5. Clean up BM aspiration set & send to CSSD (centre
diseases sterile supply department) for autoclaving
TYPE OF BONE MARROW EXAMINATION COMPLICATION
1. BM aspiration 1. Excessive bleeding
Use a thin needle to remove small amount concern with bleeding
of liquid BM in the back of hipbone (pelvis) disorder/thrombocytopenic
2. BM biopsy Iatrogenic marrow infection
Remove small piece of bone tissue & UNIT 2.3 SICKLE CELL ANEMIA
enclosed marrow DEFINITION - Inheritance Hb disorder when RBC are
INDICATIONS FOR BM ASPIRATION in abnormal crescent shape
1. Diagnosis of cause & severity of haematological PATHOPHYSIOLOGY
conditions: When exposed to < in O2
Anemia II
Leukemia (acute & chronic) Defective Hb forms a gel like substance contains Hb
Myelodysplastic disorder (cancer/ crystals with affected RBS
immature cells in BM), Myeloproliferative II
neoplasm (overproduction) Crystal clump together assumes a crescent sickle
Fever of unknown origin shape
Thrombocytopenia II
Pancytopenia Neutropenia (< neutrophils) Sickled cells become rigid, sticky & fragile (hemolysis)
Immunodeficiency Cells impede circulation, causing microinfarcts tissue
2. Staging hepoxia
Used to assess severity, progress of CLINICAL MANIFESTATION
disease, distribution of disease & enable 1. Hb: < 7-10
administration of potentially curative 2. Pallor
radiation therapy (Hodgkin Lymphoma) 3. Fatigue (lack of O2 due to low Hb)
3. Therapeutic monitoring to note progress of disease 4. < tolerance for exercise
& effectiveness of therapy (Hodgkin & Non- 5. Jaundice (> bilirubin)
Lymphoma) 6. Tachycardia
STAFF REQUIRED 7. Cardiac murmurs (abnormal heart sound)
1. Doc to perform 8. Cardiomegaly (heart enlargement)
2. Nurse to assist SICKLE CELL CRISIS
3. Lab technician 1. Sudden onset
COMMON SITE OF COLLECTION 2. Serious symptoms require immediate medical
1. Posterior superior iliac crest attention
3. Acute chest syndrome 2. Transportation
4. Heart failure & dysrhythmias Bilirubin leaves site of production &
5. Microvascular-occlusive transported in plasma bound to albumin
Tissue pain & necrosis caused by plugs of Binding capacity of serum albumin to bind
sickled cells in microcirculation bilirubin
BLOOD TEST 3. Hepatic uptake
1. FBC Selective & highly efficient system for
< HCT removing unconjugated bilirubin from
2. Full Blood Picture plasma
Sickled cells smear Transferred to endoplasmic reticulum (site
TREATMENT of bilirubin conjugation)
1. Pain management 4. Conjugation
NSAID (Ibuprofen) Binding unconjugated bilirubin to
Morphine glucuronic acid
2. Exchange transfusion (acute chest syndrome) 5. Excretion
3. Blood transfusion Conjugated bilirubin is excreted into bile
4. Pharmacology Transported to small intestine & excreted
Hydroxyurea: chemotherapy agent > HbF (< as stool
formation of sickled cells) 6. Enterohepatic (GIT) circulation
5. Oxygen therapy Deconjugation of bilirubin in intestine
6. Peripheral bloods stem cell transplant resulting formation of urobilinogen where
COMPLICATIONTS it’s absorbed & transported by portal
1. Pulmonary embolism circulation
2. Pulmonary infarction Urobilinogen excreted in urine & converted
3. Pulmonary hypertension to stercobilinogen b4 excreted in feces as
4. Death stercobilin
NURSING PRIORITIES TYPE JAUNDICE
1. Promote adequate cellular O2 1. Prehepatic (haemolytic)
2. Alleviate pain Due to > production bilirubin with
3. Prevent complications erythrocyte destruction
4. Provide information about disease process, Extrinsic causes like reabsorption of large
prognosis & treatment needs haematoma
UNIT 2. 4 JAUDICE (ICTERUS) Intrinsic defects in RBC leading to hemolytic
DEFINITION - Yellowish discolouration of skin, anemia
mucous membrane & sclera off eyes due to elevated 2. Hepatic (hepatocellular)
levels of serum bilirubin > 2.5mg/dL Due to dysfunction of hepatocytes < ability
(hyperbilirubinemia) to remove bilirubin from blood & convert it
BILIRUBIN METABOLISM into bile
- Formed by breakdown of heme in RBC & Caused by virus infection, alcohol, rare
liver excretes it out genetic (Gilbert’s syndrome), medication
TYPE OF BILIRUBIN (acetaminophen toxicity)
1. Unconjugated bilirubin (indirect) 3. Post-hepatic (obstructive)
Heme released from Hb, it’s converted to Due to obstruction of flow of bile &
unconjugated resulting in clogged-up bile through
Unconjugated is not H2O soluble & it travels hepatocytes to blood
in bloodstream to liver Caused by cholestasis due to gallstone &
2. Conjugated bilirubin (direct) cancer at head pancreas
Bilirubin converted from unconjugated > CLINICAL MANIFESTAION
conjugated in liver 1. Severity symptoms depends on underlying causes
H2O soluble & progress of diseases
Conjugated turns into bile & enters small 2. Yellow colouration of skin & sclera
intestine & eventually eliminated 3. If infection:
BILE Fever & chills
1. Some bile will be absorbed in kidney Abdominal pain
2. Emulsify lipid in small intestine Flu-like symptoms
3. Store in gall bladder Dark urine & clay stool
BILIRUBIN METABOLISM 4. If not infection:
1. Production Weight loss
Bilirubin is end product of catabolism of Itchy skin
heme, major source is circulating Hb Nausea & vomit
75% unconjugated bilirubin produced from Malaise
normal destruction of RBS Anorexia
Fatigue 4. If progressed to hemeloytic anemia, > aggressive
Dark urine treatment maybe required
Clay stool MANAGEMENT
5. If biliary tract cancer: 1. Severe hemolytic
Weight loss Hospitalized
Itchy skin Blood transfusion
Nausea & vomit O2 therapy
Malaise PATIENT EDUCATION
Anorexia fatigue 1. Genetic counselling & screening fam history of
Dark urine G6PD
Clay stool 2. Explain pathophysiology & process of disease
DIAGNOSTIC TEST 3. Medical alert bracelet for disease identification
1. Blood test 4. Avoid triggers
AST & ALT < Fava beans
GGT < Naphthalene mothball
Total bilirubin < Oxidant drugs
Prothrombin Time (PT) prolonged - Antibiotic: sulfamethoxazole
2. Urine test - Antimalarials: primaquine
Urobilinogen > - Antipyretics: aspirin
3. Ultrasound COMPLICATIONS
4. ERCP 1. Prolonged neonatal jaundice, possible kernicterus
Endoscopic retrograde (brain damage)
Cholangiopancreatography 2. Ophthalmological damage due to intraocular IV
TREATMENT hemolysis (eye bleeding)
1. Treatment depends on underlying cause 3. Susceptibility to infection
2. Injection IV Vit K 4. Hemolytic crises in response:
3. Antihistamine Illness
4. Antiemetics Certain drugs
COMPLICATIONS Certain foods (beans)
1. Neonatal Certain chemicals
Acute bilirubin encephalopathy 5. Severe crises caused acute kidney failure
Kernicterus (> bilirubin lead to brain 2.6 THALASSEMIA
damage) DEFINITION - Disorder of the Hb due to lack of globin
2. Adult chain that leads to hemolysis
Anemia GENETIC TYPE OF THALASSEMIA
Bleeding 1. Beta thalassemia: < production of normal beta
Infection/sepsis globin chain
Chronic hepatitis 2. Alpha thalassemia: < normal alpha globin chain
Cancer PATHOPHYSIOLOGY
Liver failure 1. Results when there’s deletion in production of
Kidney failure globin chain from any/all globin genes
2.5 GLUCOSE 6-PHOSPHATE DEHYDROGENASE 2. Genes responsible for regulating synthesis &
DEFICIENCY (G6PD) structure of globins
DEFINITION - Is a genetic abnormality that lack of 3. Hb formed is unstable & precipitates to form Heinz
G6PD leads to hemolysis of RBC due to the bodies which may damage RBC
obstruction of the membrane TYPE OF THALASSEMIA
*X-linked recessive, commonly in men Thalassemia trait/minor
CLINICAL MANIFESTATION Carry genetic trait but don’t usually
1. Pallor experience any health probs except mild
2. Tachycardia anemia
3. SOB May have either alpha or beta trait,
4. Jaundice depends on which form of protein lack
5. Hemoglobulinuria TYPE OFBETA THALASSEMIA
6. Tae colour urine 1. Thalassemia Major (Cooley/s Anemia)
DIAGNOSTIC TEST Severe B-thalassemia
1. Neonatal screening Presence of 2 mutated genes caused either
Check blood right after birth severe < or no any beta globin
TREATMENT 2. Thalassemia Minor
1. Removing triggers that’s caused symptoms Presence of 1 normal gene & 1 mutation
2. If infection, infection is treated accordingly Caused mild-moderate mild anemia
3. If current medication then discontinue CLINICAL MANIFESTATION
1. Minor
Characterized by mild anemia Give drug to < iron level
2. Beta 3. Folate supplement
Symptoms appear at first 2 years > RBC formation
- fatigue & weakness 4. BM transplant
- pallor or jaundice Change mother cell due to gene
- protruding abdomen with enlarged spleen 5. Surgical treatment
& liver Enlargement of spleen
- dark urine 6. Supportive measure
- abnormal facial bone & poor growth Need extra observation
- poor appetite 7. Genetic counselling
- adolescent with severe form of beta may Sharing opinion about having child or not
experience delayed puberty BENEFITS BLOOD TRANSFUSION
DIAGNOSTIC TEST 1. Improve tissue oxygenation & prevent chronic
1. Physical examination may reveal hypoxia
hepatosplenomegaly - extramedullary hematopoiesis 2. Improve normal growth & development
2. FBP 3. Prevent erythropoiesis thus avoiding expansion of
Microcytic hypochromic anemia BM & extra medullary hemolysisi
Immature RBC 4. Reduce hemolysis
3. FBC reveals anemia 5. Reduce hepatosplenectomy
4. Hb electrophoresis 6. Reduce GIT absorption of iron
Measure different type Hb COMPLICATION TRANSFUSION
5. Mutational analysis to detect thalassemia that 1. Non hemolytic febrile transfusion reaction
can’t be detected with Hb electrophoresis 2. Allergic reaction
COMPLICATIONS THALASSEMIA MAJOR 3. Acute & delayed hemolytic reactions
1. Severe anemia 4. Transfusion associated circulatory overload
Ineffective erythropoiesis 5. Alloimmunization (immune response to foreign
Extramedullary hematopoiesis antigens after exposure to genetically different cells)
2. Iron overload resulting from: 6. Iron overload
Transfusion 7. Transfusion transmitted infections
Iron absorption CHELATING AGENTS
3. Pallor & jaundice 1. Deferoxamine (DFO)
Excessive bilirubin 2. Deferipone (Kelfer)
4. Skull & bones maybe deformed 3. Deferasirox (Exjade)
Due to erythroid hyperplasia with TREATMENT OF THALASSEMIA
intramedullary expansion cortical bone 1. Chelation therapy
thinning (compact bone thinner) Remove excess iron
5. Cardiac failure related to severe anemia or iron 2. Folate supplements
overload Folic acid
Severe anemia 3. Transplant
Iron overload BM
6. Repeated blood transfusion Stem cells
Hepatomegaly or chronic hepatitis due to SURGICAL TREATMENT
iron overload 1. Splenectomy
7. Gallbladder contains bilirubin stones due to To < transfusion requirements
lifelong hemolytic state 2. Surgical or orthodontic correction
8. Hepatosplenomegaly To correct skeletal deformities of skull &
9. Iron overload caused endocrine dysfunction maxilla caused by erythroid hyperplasia
10. Transfusion-associated viral hepatitis resulting in 3. Cholecystectomy due to presence of bilirubin
portal hypotensionn stones
COMPLICATION MANAGEMENT THALASSEMIA MAJOR
1. Iron overload 1. Further treatment
2. Infection Gene replacement
3. Bone deformities 2. Supportive care
4. Enlarged spleen Management of endocrine & cardiac
Due to destruction of large num. RBC complications
5. Slowed growth rate PREVENTION OF THALASSEMIA
Slow child’s growth & delays puberty 1. Carrier screening
6. Congestive heart failure Minor or carrier can be detected by Hb
MANAGEMENT electrophoresis
1. Periodic transfusion 2. Population education, mass screening, genetic
Packed cell blood transfusion counselling & antenatal diagnosis & therapeutic
2. Iron chelation absorption of affected pregnancy
UNIT 3 POLYCYTHEMIA
You might also like
- Gmo Persuasive SpeechDocument2 pagesGmo Persuasive Speechnaomi88GnR44% (9)
- Lesson Plan AnemiaDocument19 pagesLesson Plan AnemiaDeepak Parida84% (56)
- Aortic StenosisDocument14 pagesAortic Stenosisjyoti singh100% (3)
- Handbook of AnesthesiologyDocument176 pagesHandbook of AnesthesiologyarmelzahfauziNo ratings yet
- GNM 1st Year Trhering Topic Handout 2020Document13 pagesGNM 1st Year Trhering Topic Handout 2020shapan biswaNo ratings yet
- Management of Patient With AnemiaDocument58 pagesManagement of Patient With AnemiaDoaa HussainNo ratings yet
- Kelainan Darah 1 FKG 2020Document74 pagesKelainan Darah 1 FKG 2020Jeremy Kartika SoeryonoNo ratings yet
- Anaemia: Red Cell IndicesDocument10 pagesAnaemia: Red Cell IndicesRazib HasanNo ratings yet
- Red Blood Cell Disorders I. AnemiaDocument11 pagesRed Blood Cell Disorders I. AnemiaGea MarieNo ratings yet
- Harsa Kuriakose M Pharm 1 Year Department of Pharmacy Practice Grace College of PharmacyDocument31 pagesHarsa Kuriakose M Pharm 1 Year Department of Pharmacy Practice Grace College of PharmacykeerthanaNo ratings yet
- Pediateric Group 6 AnemiaDocument69 pagesPediateric Group 6 AnemiaAbdelruhman SobhyNo ratings yet
- Iron Deficiency Anemia & ManagementDocument60 pagesIron Deficiency Anemia & Managementswap58war100% (1)
- Anemia - Aortic Stenosis B5Document8 pagesAnemia - Aortic Stenosis B5Aila HinlogNo ratings yet
- Anemia Def Fe 2015Document20 pagesAnemia Def Fe 2015ChingHuaNo ratings yet
- Case 1Document3 pagesCase 1asamh alsalieNo ratings yet
- Module 5 ERYTHROCYTE DISORDERSDocument23 pagesModule 5 ERYTHROCYTE DISORDERSPauline Louise S. DURANNo ratings yet
- Iron Deficiency Anemia-NouDocument49 pagesIron Deficiency Anemia-NouDM XyzNo ratings yet
- Anemia 07oct FINALDocument77 pagesAnemia 07oct FINALDr pragya joshiNo ratings yet
- Presentation Ms 1 (Group 2) ANEMIADocument29 pagesPresentation Ms 1 (Group 2) ANEMIApetronaila paulNo ratings yet
- By: Dinsy Paul Juliet James Priya K Sravan Kumar. Potturi Govinda AjmeraDocument78 pagesBy: Dinsy Paul Juliet James Priya K Sravan Kumar. Potturi Govinda Ajmerashameer muhammedNo ratings yet
- 2019 Hematology (1) (Autosaved)Document67 pages2019 Hematology (1) (Autosaved)Rasheda PickettNo ratings yet
- RBC Micro-Macro MeasurementsDocument11 pagesRBC Micro-Macro MeasurementsDingdongLopezNo ratings yet
- Topic 29: Pathophysiology of Red Cell Series: 1. HematopoiesisDocument10 pagesTopic 29: Pathophysiology of Red Cell Series: 1. HematopoiesisAelita RuseelNo ratings yet
- Nutritional AnemiaDocument78 pagesNutritional AnemiaJoUng DjelauNo ratings yet
- Curs Hematologie An Feripriva EN Martie 2023 POSTATDocument55 pagesCurs Hematologie An Feripriva EN Martie 2023 POSTATErland BordNo ratings yet
- Nutritional Anemia: Dr. Mardiana, M.Kes, SP - GK Department of Clinical Nutrition Hasanuddin University MakassarDocument77 pagesNutritional Anemia: Dr. Mardiana, M.Kes, SP - GK Department of Clinical Nutrition Hasanuddin University MakassarDianaNo ratings yet
- Iron Deficiency in CKD PatientsDocument49 pagesIron Deficiency in CKD Patientsswap58warNo ratings yet
- Kuliah AnemiaDocument185 pagesKuliah AnemiaAchmad Nur AffendickNo ratings yet
- Red Cell DisordersDocument60 pagesRed Cell DisordersASMANI MATETENo ratings yet
- Nutritional Therapy For Deficiency AnemiasDocument49 pagesNutritional Therapy For Deficiency AnemiasKartikaPANo ratings yet
- Dr. Haryanto - Kuliah Anemi Deff Fe 2011Document20 pagesDr. Haryanto - Kuliah Anemi Deff Fe 2011YeniNo ratings yet
- K15. Obat Anti-AnemiaDocument24 pagesK15. Obat Anti-AnemiaSyafira Ristiana PutriNo ratings yet
- NCM103 9th Hema IDocument10 pagesNCM103 9th Hema IKamx MohammedNo ratings yet
- Anemia GiziDocument47 pagesAnemia Giziadink mochammadNo ratings yet
- Formed Elements of The BloodDocument88 pagesFormed Elements of The BloodKirk08No ratings yet
- Iron Deficiency and Iron OverloadDocument9 pagesIron Deficiency and Iron Overloadkat9210No ratings yet
- AnaemiaDocument4 pagesAnaemiaRichardNo ratings yet
- ANEMIADocument3 pagesANEMIAjessa tabanginNo ratings yet
- 8 - Basics in Deficiency AnaemiasDocument59 pages8 - Basics in Deficiency AnaemiasWasana MendisNo ratings yet
- Hematology - Oncology Div.: Child Health Depart.-School of Medicine University of Sumatera UtaraDocument37 pagesHematology - Oncology Div.: Child Health Depart.-School of Medicine University of Sumatera UtaracccccNo ratings yet
- Purpose: Be Able To Explain Definition of AnemiaDocument59 pagesPurpose: Be Able To Explain Definition of AnemiamelimindNo ratings yet
- Anemia 1Document41 pagesAnemia 1julie kiskuNo ratings yet
- Anemia NoteDocument1 pageAnemia NoteAthirahRaraNo ratings yet
- Approach To Anemia-Iron Deficiency, Megaloblastic and Hemolytic AnemiaDocument106 pagesApproach To Anemia-Iron Deficiency, Megaloblastic and Hemolytic Anemiasarath chandranNo ratings yet
- Hema 2 - ANEMIADocument45 pagesHema 2 - ANEMIARayana UbasNo ratings yet
- Chapter 2Document43 pagesChapter 2Puvaneswary SegharanNo ratings yet
- Nutritional Anemia-Apr 2015Document110 pagesNutritional Anemia-Apr 2015MJ PutraNo ratings yet
- Anemia: Dr. Tutik Harjianti, SP PDDocument47 pagesAnemia: Dr. Tutik Harjianti, SP PDsujidahNo ratings yet
- Anaemia & BleedingDocument123 pagesAnaemia & BleedingDyana MalikNo ratings yet
- 1 - AnemiaDocument25 pages1 - AnemiaDr. Anju K PailyNo ratings yet
- Nutrion Terapi of AnemiaDocument4 pagesNutrion Terapi of AnemiaRian LianNo ratings yet
- Blood DisordersDocument72 pagesBlood DisordersAngel Bar100% (1)
- Problem-Oriented Approach To Anemia in The HorseDocument87 pagesProblem-Oriented Approach To Anemia in The HorseanggianggrainiulfaNo ratings yet
- Chapter Two Anemiarev - ATDocument153 pagesChapter Two Anemiarev - ATAemro TadeleNo ratings yet
- Nutritional Disorders: Dr-Nabiha Najati MBCHB, CABP, 2018-2019Document28 pagesNutritional Disorders: Dr-Nabiha Najati MBCHB, CABP, 2018-2019tanishqsaxena100210No ratings yet
- Physiology Clinical NotesDocument10 pagesPhysiology Clinical NotesMohammed EljackNo ratings yet
- Physiology I Blood & ImmunityDocument13 pagesPhysiology I Blood & Immunitynadine azmyNo ratings yet
- Hematology PDFDocument85 pagesHematology PDFammarNo ratings yet
- Hematinics (Iron and Vitamin B12)Document53 pagesHematinics (Iron and Vitamin B12)shareksultan5No ratings yet
- A Simple Guide to Anemia, Treatment and Related DiseasesFrom EverandA Simple Guide to Anemia, Treatment and Related DiseasesRating: 4.5 out of 5 stars4.5/5 (2)
- Hypophosphatemia, (Low Phosphate) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHypophosphatemia, (Low Phosphate) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Disorders of Adrenal GlandsDocument48 pagesDisorders of Adrenal GlandsCharlz ZipaganNo ratings yet
- Name of Infection/virus Acquired at What Time How To Test For It Likely S/s HSVDocument1 pageName of Infection/virus Acquired at What Time How To Test For It Likely S/s HSVC RNo ratings yet
- Renal Concept MapDocument1 pageRenal Concept MapShaira Ann CalambaNo ratings yet
- Renal Cell Carcinoma Tuberous SclerosisDocument48 pagesRenal Cell Carcinoma Tuberous SclerosisPiyushNo ratings yet
- E C T Document PDFDocument17 pagesE C T Document PDFDhAiRyA ArOrANo ratings yet
- PHARMACEUTICAL INORGANIC CHEMISTRY: Gastrointestinal Agents (Antacid)Document9 pagesPHARMACEUTICAL INORGANIC CHEMISTRY: Gastrointestinal Agents (Antacid)MD REFATNo ratings yet
- Generic Name (Brand Name) Classification Dosage Indication/ Contraindication Nursing ResponsibilitiesDocument3 pagesGeneric Name (Brand Name) Classification Dosage Indication/ Contraindication Nursing ResponsibilitiesJoe Anne Maniulit, MSN, RNNo ratings yet
- All India Post Graduate Medical Entrance Exam ForumsDocument57 pagesAll India Post Graduate Medical Entrance Exam ForumsabhishekbmcNo ratings yet
- Does This Patient Have Clubbing PDFDocument7 pagesDoes This Patient Have Clubbing PDFAhraxazel Galicia ReynaNo ratings yet
- TRACHEOSTOMYDocument31 pagesTRACHEOSTOMYHari PranotoNo ratings yet
- Pneumonitis and Pneumonia After AspirationDocument12 pagesPneumonitis and Pneumonia After AspirationmitahalidNo ratings yet
- Tetralogy of Fallot (TOF) : Dr. Sayeedur Rahman Khan Rumi MD Final Part Student Nhfh&RiDocument49 pagesTetralogy of Fallot (TOF) : Dr. Sayeedur Rahman Khan Rumi MD Final Part Student Nhfh&RiPrazNo ratings yet
- COVID - 19 and Sudden Sensorineural Hearing Loss ADocument8 pagesCOVID - 19 and Sudden Sensorineural Hearing Loss Abay aji15No ratings yet
- Porphyria: By: Sheena Joy Barredo Mls 3DDocument31 pagesPorphyria: By: Sheena Joy Barredo Mls 3DEdgar DumagpiNo ratings yet
- Treating and Monitoring Hypomagnesaemia For Non-Critical Areas of TrustDocument3 pagesTreating and Monitoring Hypomagnesaemia For Non-Critical Areas of Trustramy.elantaryNo ratings yet
- Peadiatric Advanced Life Support (Pals)Document18 pagesPeadiatric Advanced Life Support (Pals)SREEDEVI T SURESHNo ratings yet
- Parkinson's DiseaseDocument28 pagesParkinson's DiseaseJan Michael CorpuzNo ratings yet
- 3Document13 pages3Urologi Unpad Februari 2023No ratings yet
- Mcqs and Seqs of BiochemistryDocument6 pagesMcqs and Seqs of BiochemistrymisbahnazNo ratings yet
- Notes File - MergedDocument99 pagesNotes File - MergedMian. Shoaib.No ratings yet
- Onconephrology: Update in Anticancer Drug-Related NephrotoxicityDocument13 pagesOnconephrology: Update in Anticancer Drug-Related NephrotoxicityFreddy Shanner Chávez VásquezNo ratings yet
- Pathophysiology of Selected Autoimmune Diseases: Lecture From Pathological Physiology November 11, 2004Document50 pagesPathophysiology of Selected Autoimmune Diseases: Lecture From Pathological Physiology November 11, 2004Meity ElvinaNo ratings yet
- PPR Koumakis Dementia Care FrameworksDocument15 pagesPPR Koumakis Dementia Care FrameworksLuis Eduardo Ronquillo OrdoñezNo ratings yet
- Dementia Prac QuesDocument16 pagesDementia Prac QuesApril Ann HortilanoNo ratings yet
- WRL0005Document36 pagesWRL0005NewdeersciNo ratings yet
- 11 Fibro Osseous LesionsDocument22 pages11 Fibro Osseous Lesionsفراس الموسويNo ratings yet
- Classification of Epilepsie1981 - ILAEDocument13 pagesClassification of Epilepsie1981 - ILAEarmythunderNo ratings yet