Professional Documents
Culture Documents
Cods 2015 07 064
Uploaded by
محمود مساعدحلمى أبازيدOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cods 2015 07 064
Uploaded by
محمود مساعدحلمى أبازيدCopyright:
Available Formats
Review Article
Bone Grafts in Periodontics-A Review
Pramod Tatuskar1, Shobha Prakash2
Assistant Professor1, Vice principal, Prof & HOD2
Department of Periodontics, College of Dental Sciences, Davangere
Abstract:
The ultimate goal of periodontal therapy should not be limited to the establishment and maintenance of periodontal health. The
potential for regeneration of the hard and soft periodontal tissues lost to disease should be considered. Of all the bone grafting
materials being developed, the demineralized freeze dried bone allograft (DFDBA) has been used as a substitute for bone
graft for more than four decades. The basis for the use of any bone grafting material is to induce bone formation. In this article
various bone grafts and biomaterials used are reviewed.
Keywords: Allograft, Autograft, Biomaterial, Bone graft.
Introduction
BASIC CONSIDERATIONS:
Bone grafts are used as a filler and scaffold to facilitate
Definitions:
bone formation and promote wound healing. These grafts
are bioresorbable and have no antigen-antibody reaction.
1. Graft: A graft is a viable tissue that after removal from
These bone grafts act as a mineral reservoir which
the donor site is implanted within the lost tissue which is
induces new bone formation. Bone grafting is a surgical
then restored, repaired or regenerated3. Examples:
procedure that replaces missing bone with material from
Autografts, Allografts and Xenografts.
patient’s own body, an artificial, synthetic, or natural
substitute. Bone grafting is possible because bone tissue
2. Biomaterials: These are bone derived materials
has the ability to regenerate completely if provided the
processed in such a way that the cells are no longer vital
space into which it has to grow. As natural bone grows, it
and hence used as bone graft substitutes1.
generally replaces the graft material completely,
Examples:- Freeze dried bone, decalcified or non
resulting in a fully integrated region of new bone. The
decalcified.
upcoming of various bone grafts and biomaterials has
given a big leap to the field of Periodontics. The aim of
- Xenograft from a bovine derived material can be more
periodontal therapy is to control periodontal infection
appropriately called
and inflammation in the periodontium. The continued
function of the periodontally involved tooth requires
Xenogenic bone derived biomaterial.
additional periodontal support and regeneration of the
lost periodontium1,2. This may be achieved by the use of
The biologic mechanisms that provide a rationale for
guided tissue regeneration and various bone grafts and
bone grafting are osteoconduction, osteoinduction, and
biomaterials used as substitutes of bone grafts. These are
osteogenesis 4.
derived from vital or non vital bone sources or consist of
organic orinorganic materials. The main aim of utilizing
bone grafts and performing bone graft related osseous Osteoconduction :
surgeries is to promote bone regeneration. However
these materials should be biologically acceptable to the Occurs when bone graft material serves as a scaffold for
patient without causing any systemic or local hazards or new bone growth, which is perpetuated by the native
side effects1. bone. Osteoblasts from the margin of defect that is being
grafted, utilize the bone graft material as a framework
upon which to spread and generate new bone 5. In the
Corresponding Author:
Dr.Pramod Tatuskar
very least, a bone graft material should be
Assistant Professor osteoconductive.
Department of Periodontics, College of Dental
Sciences, Davangere-577004, Karnataka
Mob no: 9036925136
Email id : pramod_mats@yahoo.co.in
CODS Journal of Dentistry 2015, Volume 7, Issue 2 64
Bone Grafts
Hopeless in Periodontics
to hopeful: Management of an endo-perio......... Pramod
Tatuskar VT et al
P et al
that additional surgical site is required, another potential
Osteoinduction :
location for postoperative pain and complications 6. All
Involves stimulation of osteoprogenitor cells to
bones require blood supply in the transplanted site.
differentiate into osteoblasts and then begins formation of
Depending on where the transplant site is and size of the
new bone. The most widely studied type of osteoinductive
graft, an additional blood supply may be required. For
cell mediators are BMPs. A bone graft material that is
these types of grafts, extraction of the part of
osteoconductive and osteoinductive will not only serve
theperiosteum and accompanying blood vessels along
as a scaffold for
with the donor bone is required. This kind of graft is
known as a free flap graft.
currently existing osteoblasts but will also trigger
formation of new osteoblasts, promoting faster Allografts :
integration of the graft 4.
Allograft is derived from humans. The difference is that
allograft is harvested from an individual other than the
Osteopromotion :
one receiving the graft. Allograft bone is taken from
cadavers that have donated their bone so that it can be
Involves enhancement of osteoinduction without
used for living people who are in need of it; it is typically
possession of osteoinductive properties. For example,
sourced from a bone bank. There are three types of bone
enamel matrix derivative enhances the osteoinductive
allograft available 1,7:
effect of demineralized freeze-dried bone allograft
(DFDBA), but will not stimulate bone growth alone 4.
1. Fresh or fresh-frozen bone
2. FDBA
Osteogenesis :
3. DFDBA
It occurs when vital osteoblasts originating from bone
The use of allografts for bone repair often requires
graft material contributes to the growth of new bone along
sterilization and deactivation of proteins normally found
with bone formation.
in healthy bone. Contained in the extracellular matrix of
The Ideal Requirements for bone grafts or bone graft bone tissue are the full cocktail of bone growth factors,
substitutes may be summarised as follows 1: proteins, and other bioactive materials necessary for
1. Biologic acceptability osteoinduction and successful bone healing; the desired
factors and proteins are removed from the mineralized
2. Predictability tissue by using a demineralizing agent such as
hydrochloric acid. The mineral content of the bone is
3. Clinical feasibility degraded, and the osteoinductive agents remain in a
demineralized bone matrix (DBM).
4. Minimal operative hazard
Xenograft :
5. Minimal post operative sequelae Xenogratfs are bone grafts from a species other than
human, such as bovine and are used as a calcified matrix.
6. Patient acceptance. Alloplastic grafts :
Types and Tissue Sources: Alloplastic grafts may be made from
Autograft : hydroxyapatite, a naturally occurring mineral
(main mineral component of bone), made from bioactive
Autologous or autogenous bone grafting involves
glass. Hydroxyapatite is a synthetic bone graft, which is
utilizing bone obtained from same individual receiving
the most used now due to its osteoconduction, hardness,
the graft. Bone can be harvested from nonessential bones,
and acceptability by bone. Some synthetic bone grafts are
such as from iliac crest, mandibular symphysis (chin
made of calcium carbonate, which start to decrease in
area), and anterior mandibular ramus (coronoid process).
usage because it is completely resorbable in short time
When a block graft will be performed,autogeneous bone
and makes breaking of the bone easier. Finally used is the
is the most preferred because there is less risk of graft
tricalcium phosphate in combination with hydroxyapatite
rejection as the graft is originated from the patient’s
and thus giving effect of both, osteoconduction and
body 6. It would be osteoinductive and osteogenic, as well
resorbability.
as osteoconductive. Disadvantage of autologous grafts is
CODS Journal of Dentistry 2015, Volume 7, Issue 2 65
Bone Grafts in Periodontics Tatuskar P et al
Synthetic variants : i) Dentin:
Although demineralised dentin has been advocated as a
Flexible hydrogel-hydroxyapatite (HA) composite possible graft 12 , it has not gained widespread
which has a mineral to organic matrix ratio, acceptance because clinical results have been some
approximating that of human bone. Artificial bone can what disappointing13.
be created from ceramics such as calcium phosphates
(e.g., HA and tricalcium phosphate), bioglass, and ii) Dura:
calcium sulphate are biologically active depending on The use of lyophilised allogeneic duramater in
solubility in physiological environment8. These periodontal osseous defects has resulted in gain of
materials combine with growth factors, ions such as clinical attachment and reduction in probing depth.
strontium or mixed with bone marrow aspirate to Histologically bone has been seen alongside but never
increase biological activity. The presence of elements in the implant 14.
such as strontium can result in
higher bone mineral density (BMD) and enhanced iii) Sclera:
osteoblast proliferation. Success has been reported with preserved sclera 15, but
there were no signs of osteogenesis within the sclera
Growth factors : and it remained encapsulated at the site 13.
Growth factors enhanced grafts are produced using iv) Cartilage:
recombinant DNA technology. They consist of either Cartilage allografts provide no statistically significant
human growth factors or morphogens (BMPs in advantage in bone or soft tissue repair over flap
conjunction with a carrier medium, such as debridement alone 16.
collagen). The factors and proteins that exist in bone
are responsible for regulating cellular activity.
Growth factors bind to receptors on cell surfaces and
stimulate intracellular environment to act. Generally,
this activity translates to a protein kinase that induces a
series of events resulting in transcription of messenger
ribonucleic acid (mRNA) and ultimately into the
formation of a protein to be used intracellularly or
extracellularly. The combination and simultaneous
activity of many factors results in controlled production
and resorption of bone. These factors, residing in
extracellular matrix of bone, include TGF-beta, insulin
like growth factors I and II, PDGF, FGF, and BMPs 9,10
,Cell-based bone graft substitutes: Stem cells are
cultured in the presence of various additives such as
dexamethasone, ascorbic acid, and b-glycerophosphate
to direct the undifferentiated cell towards osteoblast
lineage. The addition of TGF-beta and BMP-2, BMP-4,
and BMP-7 to the culture media can also influence the
stem cells towards osteogenic lineage. Mesenchymal
stem cells have also been seeded onto bioactive
ceramics conditioned to induce differentiation to
osteoblasts 8,11.
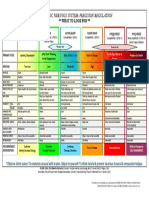
BONE GRAFTS AND BONE GRAFT
SUBSTITUTES(Table-1) :
I) Non-osseous material :
A) Organic;-
CODS Journal of Dentistry 2015, Volume 7, Issue 2 66
Bone Grafts in Periodontics Tatuskar P et al
B) Inorganic;- ii) Intra-oral cancellous bone marrow transplants:
i) Plaster of Paris: Haitt and Schallhorn have described the use of
cancellous bone obtained from the maxillarytuberosity,
Plaster of Paris (Calcium sulphate) is biocompatible edentulous areas and healing sockets. The maxillary
and porous thereby allowing fluid exchange, which tuberosity frequently contains a good amount of
prevents nap necrosis. Plaster of Paris resorbs cancellous bone, particularly if the third molars are
completely in 1-2 weeks 17. Also, because plaster of absent. Foci of red marrow are also occasionally
paris is so rapidly resorbed, it is questionable whether it observed. Edentulous ridges can be approached with a
is of any benefit. flap, and cancellous bone and marrow are removed with
curettes. Sockets are allowed to heal for 8-12 weeks, and
ii) Bio active glasses: the apical portion is utilised as donor material. The
particles are reduced to small pieces 15.
There are 2 forms of bioactive glass currently available,
perio glass (Bio glass synthetic bone graft particulate) b) Bone swaging:
and biogran (resorbable synthetic bone graft). Bio This technique requires the existence of an edentulous
active glasses are composed of SI02, CaO, Na20, P205 area adjacent to the defect, from which the bone is pushed
and bond to bone is through the development of a into contact with the root surface without fracturing the
surface layer of carbonate hydroxyapatite (HA). When bone at its base15.
exposed to tissue fluids invivo, the bioactive glass is
covered by a double layer composed of silica gel and a B) Iliac bone and marrow autografts:
calcium phosphate-rich (apatite) layer. This calcium
phosphate-rich layer promotes adsorption and Schallhorn, in 1968, described the first autogenous iliac
concentration of proteins used by osteoblasts to form a bone graft in one case report where a bone marrow biopsy
mineralised extracellular matrix. It is theorized that was immediately implanted into interproximal bony
these bioactive properties guide and promote craters between both lower canines and lateral incisors.
osteogenesis, allowing rapid and quick formation of At 5 months re-entry, the defects appeared completely
new bone 18. filled. Autografts of iliac bone and marrow possess a high
osteogenic potential, even in supra crestal bone fill and
II. Bone derived material : class II furcations. They are able to induce
cementogenesis, bone regeneration and Sharpey's fibres
A) Intraoral autografts : reattachment with functionally oriented periodontal
ligament. Fresh iliac bone and marrow are responsible for
a) (i) Osseous coagulum and bone blend: a high rate of resorption and ankylosis. The need for an
extra oral surgical site and for a sampling techmque
Robinson, in 1969, having considered that the grafted performed by a trained specialist represent serious
particles of bone should be of smaller size and that limitations to this procedure 1.
mineralised fragments can induce osteogenesis,
developed a technique, which he termed osseous BIOMATERIALS
coagulum, using the material evacuated during osseous (Table-2): I. Bone derived biomaterials
surgery. The donor bone is obtained from any intra-oral A. Freeze dried human bone :
source, usually areas requiring osseous correction. A
number 6 or 8 round carbide bur, rotating at 25000 These are bone graft substitutes which are available
to 30000 rpm, without irrigation, produces bone dust through bone banks and are obtained from autopsy of
which when coated with blood makes an osseous human donors within 24 hours after death and are further
coagulum. Robinson showed the feasibility of the lyophilized after a series of physical and chemical
technique in several case reports with re- entries from 3 processing. In this procedure the guide lines of the
to 24 months. Diem et al in 1972, proposed the use of American Association of Tissue Banks is followed 1. It
an amalgam trituration capsule and a pestle to includes:
reduce bone fragments to a workable, plastic like
mass, called Bone Blend 1.
CODS Journal of Dentistry 2015, Volume 7, Issue 2 67
Bone Grafts in Periodontics Tatuskar P et al
acetone, hexachlorophene, common detergents and
Tween 80 may even enhance bone induction. Heating
above 60°C inhibits bone formation.
B. Freeze Dried Bovine Bone :
i) Boplant :
The use of Boplant, a bovine bone processed by
detergent, chloroform and methanol extraction to
reduce lipid content, washed, sterilized in antiseptic
solution and lyophilized was first used way back in
1966 1. The extensive usage of this material led to the
conclusion that the material was incorporated by new
bone formation, and it was accepted as a well
tolerated, non resorbable, osteoconductive material.
It was observed that the osteogenic potential of
decalcified Boplant did not appear greater than that of
mineralized Boplant 1,19.
• Bone procured from the human donor within 24
hours after death. ii) Demineralized bovine bone powder (DBP):
It is prepared from cortical portions of bovine bone
• It is frozen to -1790 C for 4 weeks.
after 1 hour extraction in 100 % ethanol and ethyl
ether. It is then pulverized in liquid nitrogen mill,
• Graft is freeze dried.
demineralized for 3 hours in 0.5 N HCI and washed
with water, absolute ethanol and anhydrous ether until
• Graft is defatted in chloroform menthol for 6 hours at
neutral pH is achieved1
25°C.
iii) Bovine derived Hydroxyapatite :
• Autodigested in phosphate buffers containing
This is a xenogenic bone graft substitute, described as
iodoacetate acid and sodium azide for 72 hours at
100 % crystalline, naturally porous, bovine derived
37°C.
hydroxyapatite. The use of this material was reported
in two cases by Callan and Rohrer, in 1993 1.
• Demineralized in 0.6 N HCL for 3 days at 4°C.
iv) Anorganic bovine bone (ABB):
• After each step bone is washed with triple distilled
water. This is also a xenogenic variety, said to contain
carbonate apatite. It is defatted and collagen is eluted.
• Refrozen and freeze dried. Though various studies were conducted by Thaller et
al in 1993 and 1994 on animal models, there has been
• Ground under cryogenic conditions to yield a no study testing ABB in human periodontal defects to
particle size of 125-1000 microns. date 1.
The osteo inductive capacity of these materials is Risks of disease transmission :
governed by the processing procedure. The inductive Transmission of blood borne and tissue borne disease
activity gradually decreases atjd eventually is reduced has raised concern about allogenic bone graft
to 0 within a period of 15 days when decalcification substitutes 1,13. The xenogenic bone has also recently
with 0.6 N HCL is performed at 25°C. wheareas in been suspected of potentially transmitting prion
cold temperature (2°C), the inductive activity is fairly diseases. AIDS and Creutzfeldt - Jakob diseases (CJD)
maintained even at 30 days. Ethyl or isopropyl are at risk of getting transmitted by allotransplantation
alcohols in 0.6 N HCL produces total inactivation of and bovine spongiform encephalopathy (BSE) could
inductive substitute. Delipidization with ether, alcohol, get transmitted by bovine bone transplantation. Both
BSE and CJD belong to a group of diseases affecting
CNS in animals as well as in humans.
CODS Journal of Dentistry 2015, Volume 7, Issue 2 68
Bone Grafts in Periodontics Tatuskar P et al
Scrapie is the prototype of these diseases. It affects ed. Bone grafts and biomaterials used as bone graft
mainly sheep, while BSE, a new affects bovines. In substitutes. Berlin, Quintic ssenz Verlag, 1997-313.
human CJD, Gerstmann – Straussler - Sheinker (GSS)
2. Polson A.M. Periodontal regneration Current status
disease and Kurv represents the main form of this
and directins. 151 edition; Quintessence publishing
disease. These are characterized by excitability, itching,
Co., Inc 1995, 9-10: 71-112.
ataxia, paralysis and death. The diagnosis of this disease
is by autopsy. At autopsy, the brain show spongiform 3. Grant, Stern, List garten, Periodontics. (6th edi-
changes, formation of amyloid plaques and tion). The C.V. Mosby Company 1988; 838-82.
accumulation of abnormal form of host encoded
4. Giannoudis PV, Dinopoulos H, Tsiridis E. Bone
proteins.
substitutes: An update Injury 2005;36(Suppl
3):S20-7.
Prevention of HIV transmission:
5. Laurencin C, Khan Y, El-Amin SF. Bone graft substi-
HIV can be transmitted to patients receiving kidney, tutes. Expert Rev Med Devices 2006;3:49-57.
heart and liver transplants, as well as skin grafts and
6. Conrad EU, Gretch DR, Obermeyer KR, Moogk MS,
bone grafts. Rigorous screening of potential donors by
Sayers M, Wilson JJ,et al. Transimission of the hepa-
medical and social screening, HIV antibody test, HIV
titis-C virus by tissue transplantation. J Bone Joint
antigen test, autopsy and special lymph node
Surg Am 1995;77:214-24.
examinations is critical. Buck et al 1989, have
calculated that the risk could be as low as 0.00006% 1. 7. Centres for disease control and prevention. Septic
Mellonig et al 1992, have demonstrated that HIV arthritis following anterior cruciate ligament recon-
infected bone graft is rendered free of virus struction using tendon allografts: Floridaand Louisi-
contamination after the DFDBA processing 1. ana, 2000. MMWR Morb Mortal Wkly Rep
2001;50:1081-3.
Fate of Graft Material:
8. Centres for disease control and prevention
Once the material is placed in the bony defect it may act (CDC ). Update: Allograft-associated bacterial
in a number of ways which may decide the fate of the infections: United States, 2002. MMWR Morb
graft material2-20. The various possibilities include: Mortal Wkly Rep 2002;51:207-10.
Bone graft material may have no effect at all. The bone 9. Valdes MA, Thakur NA , Namdari S, Ciombor
graft material may act as a scaffolding material for the DM, Palumbo M. Recombinant bone morphogenic
host site to lay new bone. The bone graft material may protein-2 in orthopaedic surgery: A review. Arch
itself deposit new bone because of its own viability. Orthop Trauma Surg 2009;129:1651-7.
10.Mulconrey DS, Birdwell KH, Flynn J, Cronen GA,
Conclusion : Rose PS. Bone morphogenic protein (RhBMP-2) as
Therefore it is evident that Bone grafts and bio materials
a substitute for iliac crest bone graft in multilevel
used' in Periodontal therapies have shown remarkable
adult spinal deformity surgery: Minimum two-yeare-
results as compared to the simple procedures like open
valuation of fusion. Spine (Phila Pa 1976)
curettage, and flap debridement surgery alone for
2008;33:2153-9.
periodontal osseous defects. At present, barrier
techniques to prevent epithelial downgrowth, with or 11.Waked W, Grauer J. Silicates and bone fusion. Ortho-
without autogenous bone or decalcified freeze-dried pedics 2008;31:591-7.
bone allograft, are widely used. Coral - derived
12.Register, A.A..Human bone induction by allogeneic
materials can be used when non human derived grafts
dentin matrix. J Periodontol 1972; 43:459.
are preferred. Bone substitutes will definitely have an
increased role to play in the future of periodontal 13.Dragoo M.R. Clinical and histologic evaluation of
regeneration. alloplasts and allografts in regenerative periodontal
surgery in humans. Int J Periodont Rest Dent 1983;
References : 3(2): 8.
1. Jean-Pirr Olika Youn. Proceedings of the 2nd Euro-
pean workshop on Periodontics. In Niklous P. Lang,
CODS Journal of Dentistry 2015, Volume 7, Issue 2 69
Bone Grafts in Periodontics Tatuskar P et al
14.Busschop J, & De Boener, J. Clinical and histologic Am. Advances in Periodontics 1998;Part II 42(3):
characteristics of lyophilized allogeneic duramater in 491-501.
periodontal bony defects in humans.J Clin. Periodon- 19.Mellonig, Bowers G.M. Comparison of bone graft
tol 1982; 9: 141. materials. (Part I) J Periodontol 1981; 52: 291.
15.Carranza F.A. & Newman M.G. Clinical periodon- 20.Genco, Goldman, Cohen. Contemporary periodontic.
tology, eighth edition, W.B. Saunders Company, 1st Edition. The C.V.Mosby Company,1990;
1996; 622-39. 585-604.
16.Chodroff, R.E. & Ammons, W.F. Periodontal repair
and surgical debridement with and without cartilage
allografts. J Clin. Periodontol 1984;11:295. How to cite this article:
17.Alderman NE. Sterile plaster of Paris as an implant in Tatuskar P, Prakash S. Bone Grafts in Periodontics
the infrabony environment. A preliminary study.J -A Review. CODS J Dent 2015;7: 64-70.
Periodontol 1969; 40: 11. Source of support: Nil. Conflict of interest: None Declared.
18.Aichelmann - Reidy ME & Yukna R.A. Bone replace-
ment grafts. The bone substitutes. Dent. Clin. North
CODS Journal of Dentistry 2015, Volume 7, Issue 2 70
You might also like
- Sistema NervosoDocument1 pageSistema NervosoPerisson Dantas100% (2)
- Psychiatry An Evidence Based Text PDFDocument1,336 pagesPsychiatry An Evidence Based Text PDFOscar Ayala100% (1)
- Defectos Óseos - Diagnóstico Radiográfico"Document101 pagesDefectos Óseos - Diagnóstico Radiográfico"Nucleo AlgodonesNo ratings yet
- SoW - PPE - Attachment 5Document31 pagesSoW - PPE - Attachment 5أحمد خيرالدين عليNo ratings yet
- Bone Grafts in DentistryDocument6 pagesBone Grafts in DentistryOsama MohamedNo ratings yet
- Grafts and Grafting Techniques in Implants - A ReviewDocument25 pagesGrafts and Grafting Techniques in Implants - A ReviewIJAR JOURNALNo ratings yet
- Basic of Bone GraftingDocument29 pagesBasic of Bone GraftingdoctorniravNo ratings yet
- Bone Grafts and Bone Graft Substitutes in Orthopaedic Trauma SurgeryDocument10 pagesBone Grafts and Bone Graft Substitutes in Orthopaedic Trauma SurgeryJay ChaNo ratings yet
- 240-Article Text-799-3-10-20190203Document6 pages240-Article Text-799-3-10-20190203EVANDRO FRANCO DA ROCHANo ratings yet
- 240-Article Text-799-3-10-20190203Document6 pages240-Article Text-799-3-10-20190203EVANDRO FRANCO DA ROCHANo ratings yet
- Aaid Joi D 17 00053Document11 pagesAaid Joi D 17 00053Yun De LinNo ratings yet
- Basic Knowledge of Bone Grafting: March 2012Document29 pagesBasic Knowledge of Bone Grafting: March 2012Nadira NurinNo ratings yet
- Tissue Engineering For Periodontal RegenDocument11 pagesTissue Engineering For Periodontal RegenMara CondorNo ratings yet
- Graft ImplantDocument8 pagesGraft ImplantswagataNo ratings yet
- 11 Durga Raju MachaDocument7 pages11 Durga Raju MachaKrupali JainNo ratings yet
- Tooth Derived Bone Graft MaterialDocument4 pagesTooth Derived Bone Graft MaterialrnvisNo ratings yet
- 2 R Comparacion Materiales y Resultados Revision 2017Document11 pages2 R Comparacion Materiales y Resultados Revision 2017feli.riam24No ratings yet
- Bonegraftingforimplant Surgery: Ladi Doonquah,, Pierre-John Holmes,, Laxman Kumar Ranganathan,, Hughette RobertsonDocument19 pagesBonegraftingforimplant Surgery: Ladi Doonquah,, Pierre-John Holmes,, Laxman Kumar Ranganathan,, Hughette RobertsonJason LeeNo ratings yet
- 2010 - Efficacy of Horizontal and Vertical Bone Augmentation ProceduresDocument24 pages2010 - Efficacy of Horizontal and Vertical Bone Augmentation ProceduresLenny GrauNo ratings yet
- Journey of Bone Graft Materials in Periodontal Therapy: A Chronological ReviewDocument5 pagesJourney of Bone Graft Materials in Periodontal Therapy: A Chronological ReviewShinta rahma MansyurNo ratings yet
- Bone and Bone SubstitutesDocument13 pagesBone and Bone Substitutesnoufabdulaziz00No ratings yet
- Alloplastic Bone GraftsDocument62 pagesAlloplastic Bone GraftsMaysaa mahdiNo ratings yet
- Predictable and Sustainable Preprosthetic Surgery: The Crossroads of Bone Metabolism, Molecular Biology, and BiomaterialsDocument2 pagesPredictable and Sustainable Preprosthetic Surgery: The Crossroads of Bone Metabolism, Molecular Biology, and BiomaterialsRahul PNo ratings yet
- Materials 14 01096 v2Document24 pagesMaterials 14 01096 v2Maysaa mahdiNo ratings yet
- Guided Bone Regeneration of An Atrophic Mandible With A Heterologous Bone BlockDocument6 pagesGuided Bone Regeneration of An Atrophic Mandible With A Heterologous Bone BlockGabriela Marie CruzNo ratings yet
- Retrospective Study: Lateral Ridge Augmentation Using Autogenous Dentin: Tooth-Shell Technique vs. Bone-Shell TechniqueDocument12 pagesRetrospective Study: Lateral Ridge Augmentation Using Autogenous Dentin: Tooth-Shell Technique vs. Bone-Shell TechniqueNarissaporn ChaiprakitNo ratings yet
- Jkaoms 38 2Document7 pagesJkaoms 38 2Thu Phuong NguyenNo ratings yet
- Ejournal Lisa RosulliaDocument8 pagesEjournal Lisa RosulliaLisa RosulliaNo ratings yet
- Lec BONE GRAFTING ZS 2023Document89 pagesLec BONE GRAFTING ZS 2023MohamedAliNo ratings yet
- Bone Regeneration: Dr. José María Aguado Dra. Stefania Arena Dra. Rocío GrandeDocument58 pagesBone Regeneration: Dr. José María Aguado Dra. Stefania Arena Dra. Rocío GrandeZineb SqualliNo ratings yet
- 12-D22 1963 Dian Agustin Wahjuningrum2 David Buntoro Kamadjaja IndonesiaDocument6 pages12-D22 1963 Dian Agustin Wahjuningrum2 David Buntoro Kamadjaja Indonesiadrg.montessoNo ratings yet
- 1 s2.0 S1883195817300889 Main PDFDocument10 pages1 s2.0 S1883195817300889 Main PDFridwan hardiNo ratings yet
- Biodontics: A ReviewDocument4 pagesBiodontics: A ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Autogenous Bone Harvest For Implant ReconstructionDocument12 pagesAutogenous Bone Harvest For Implant Reconstructioncmfvaldesr7No ratings yet
- Implanto Chapter 74-78Document104 pagesImplanto Chapter 74-78whatever200020100% (1)
- Application of Bone Substitutes and Its Future Prospective in Regenerative MedicineDocument21 pagesApplication of Bone Substitutes and Its Future Prospective in Regenerative MedicineATHARVA MULENo ratings yet
- Surface Texturing of Implant MaterialsDocument17 pagesSurface Texturing of Implant MaterialsYashi VermaNo ratings yet
- Alveolarbone Graftingand Reconstruction Procedurespriorto ImplantplacementDocument10 pagesAlveolarbone Graftingand Reconstruction Procedurespriorto ImplantplacementKranti PrajapatiNo ratings yet
- Advances in Biology of Orthodontic Tooth Movement - A ReviewDocument10 pagesAdvances in Biology of Orthodontic Tooth Movement - A ReviewMarwan AlareqiNo ratings yet
- Types of Bone Graft Materials Jumping Gap (Distance)Document5 pagesTypes of Bone Graft Materials Jumping Gap (Distance)Mazen T. ShembeshNo ratings yet
- Bone Graft AlternativesDocument6 pagesBone Graft Alternativesyudha anantha khaerul putraNo ratings yet
- Healing of Tooth Extraction Socket: Dr. Pankaj Datta Dr. Shilpa Khullar Dr. Mittal ADocument3 pagesHealing of Tooth Extraction Socket: Dr. Pankaj Datta Dr. Shilpa Khullar Dr. Mittal AwatidinaNo ratings yet
- Bone GraftsDocument39 pagesBone GraftsyogeshNo ratings yet
- Bone Grafts SatyaDocument153 pagesBone Grafts SatyaArchanaNo ratings yet
- Prosthodontic Implant DrivenDocument7 pagesProsthodontic Implant DrivenbuccalNo ratings yet
- Bone Grafting With Coralline HydroxyapatiteDocument11 pagesBone Grafting With Coralline HydroxyapatiteFellicia RachmadianaNo ratings yet
- J Tissue Eng Regen Med - 2014 - Detsch - The Role of Osteoclasts in Bone Tissue EngineeringDocument17 pagesJ Tissue Eng Regen Med - 2014 - Detsch - The Role of Osteoclasts in Bone Tissue EngineeringVinícius Gabriel da SilvaNo ratings yet
- Alveolar Distraction Osteogenesis and ImplantologyDocument4 pagesAlveolar Distraction Osteogenesis and ImplantologyIJAR JOURNALNo ratings yet
- JIMC PublikasiDocument5 pagesJIMC PublikasiDewi Sartieka PutriNo ratings yet
- Bone Graft Materials-527Document5 pagesBone Graft Materials-527safiraNo ratings yet
- Bone Grafting: Classification by OriginDocument4 pagesBone Grafting: Classification by OriginHerlangga Fadhillah AkbarNo ratings yet
- NIH Public Access: Bone Tissue Engineering: Recent Advances and ChallengesDocument59 pagesNIH Public Access: Bone Tissue Engineering: Recent Advances and ChallengesCarlosNo ratings yet
- Bone Augmentation TechniquesDocument20 pagesBone Augmentation TechniquesGabriela Ciornei100% (1)
- PIIS0030589809000881Document12 pagesPIIS0030589809000881dr. Joko WibowoNo ratings yet
- Zhu 2021Document12 pagesZhu 2021Alexander Fabián GNo ratings yet
- An Ethical Perspective To Using Bone Grafts in DentistryDocument4 pagesAn Ethical Perspective To Using Bone Grafts in DentistryAdel HadyNo ratings yet
- Bone Grafts 2006Document12 pagesBone Grafts 2006dhewienaraliaNo ratings yet
- Bone Biology and OsseointegrationDocument42 pagesBone Biology and OsseointegrationParinita reddyNo ratings yet
- World Journal of OrthopaedicsDocument7 pagesWorld Journal of OrthopaedicsD JahnviNo ratings yet
- Bone Grafts in Periodontal Surgery - A Review: July 2014Document4 pagesBone Grafts in Periodontal Surgery - A Review: July 2014Fajri AliNo ratings yet
- Bonegrafting 180324163620Document105 pagesBonegrafting 180324163620Ankit Damor100% (1)
- Review Article: Guided Bone Regeneration: A Literature ReviewDocument16 pagesReview Article: Guided Bone Regeneration: A Literature ReviewMazenShbeebNo ratings yet
- Short ImplantsFrom EverandShort ImplantsBoyd J. TomasettiNo ratings yet
- 711 - 2Document9 pages711 - 2ayucicuNo ratings yet
- 711 - 2Document9 pages711 - 2ayucicuNo ratings yet
- 711 - 2Document9 pages711 - 2ayucicuNo ratings yet
- 711 - 2Document9 pages711 - 2ayucicuNo ratings yet
- Cods 2015 07 064Document7 pagesCods 2015 07 064محمود مساعدحلمى أبازيدNo ratings yet
- 711 - 2Document9 pages711 - 2ayucicuNo ratings yet
- 711 - 2Document9 pages711 - 2ayucicuNo ratings yet
- 711 - 2Document9 pages711 - 2ayucicuNo ratings yet
- 711 - 2Document9 pages711 - 2ayucicuNo ratings yet
- FINALBONEGRAFTSOH2015Document16 pagesFINALBONEGRAFTSOH2015د.محمد مليحةNo ratings yet
- Cods 2015 07 064Document7 pagesCods 2015 07 064محمود مساعدحلمى أبازيدNo ratings yet
- Tneb Nhis 2021 BP No 162 17721Document166 pagesTneb Nhis 2021 BP No 162 17721Gnaneswaran SubramanianNo ratings yet
- Tuskegee ExperimentDocument2 pagesTuskegee ExperimentAniya LewisNo ratings yet
- Tuberculosis Patient Teaching Checklist: TB Skin Test (Mantoux) Fact Sheet TB Blood Test (IGRA) Fact SheetDocument2 pagesTuberculosis Patient Teaching Checklist: TB Skin Test (Mantoux) Fact Sheet TB Blood Test (IGRA) Fact SheetDaniel GarratonNo ratings yet
- Case Presentation 1Document18 pagesCase Presentation 1api-390677852No ratings yet
- LCSW Additional CourseworkDocument8 pagesLCSW Additional Courseworkiuhvgsvcf100% (2)
- Safety Data Sheet: Product Name: MOBILGARD 540Document12 pagesSafety Data Sheet: Product Name: MOBILGARD 540Om Prakash RajNo ratings yet
- Approval and Registration of Third-Party Inspection Agencies For Lifting EquipmentDocument47 pagesApproval and Registration of Third-Party Inspection Agencies For Lifting Equipmentegy pureNo ratings yet
- Ammonia SafetyDocument46 pagesAmmonia SafetyMikechal AwacayNo ratings yet
- AbraDocument4 pagesAbralhhjklllNo ratings yet
- Vit and Hormone in Relation To Growth and Development / Orthodontic Courses by Indian Dental AcademyDocument38 pagesVit and Hormone in Relation To Growth and Development / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Jamie's Story 15q21.3-22.2 DeletionDocument1 pageJamie's Story 15q21.3-22.2 DeletionNatasha RadcliffeNo ratings yet
- TASSDocument11 pagesTASSNike KeketNo ratings yet
- ADHERENCE and INVASION ASSAYS A092Document2 pagesADHERENCE and INVASION ASSAYS A092Samrah Anwar0% (2)
- Form g11Document23 pagesForm g11Armely NiedoNo ratings yet
- EndophthalmitisDocument2 pagesEndophthalmitisakillerbeast632No ratings yet
- Shaukat Khanum Memorial Cancer Hospital & Research CentreDocument2 pagesShaukat Khanum Memorial Cancer Hospital & Research CentreMa BeNo ratings yet
- Prevalence of Water Borne Diseases Within Households in The Bamendankwemunicipalitynorth West Cameroon 2332 0893 1000122Document7 pagesPrevalence of Water Borne Diseases Within Households in The Bamendankwemunicipalitynorth West Cameroon 2332 0893 1000122Welly SuryaNo ratings yet
- Claims FAQDocument4 pagesClaims FAQSaiCharan GarimellaNo ratings yet
- Application Form For Accreditation SPDocument4 pagesApplication Form For Accreditation SPMyk Twentytwenty NBeyondNo ratings yet
- Liquidation Report: To Liquidate The MOOE Cash Advanced Made by Kibao Elementary School Per Check # 298152dated 9/16/16Document3 pagesLiquidation Report: To Liquidate The MOOE Cash Advanced Made by Kibao Elementary School Per Check # 298152dated 9/16/16December Cool50% (2)
- Far Eastern University Dr. Nicanor Reyes Medical Foundation: Reportable Events (Staff Nurse/Nursing Aide)Document3 pagesFar Eastern University Dr. Nicanor Reyes Medical Foundation: Reportable Events (Staff Nurse/Nursing Aide)Jupiter WhitesideNo ratings yet
- Personal Business Model Canvas v1.1.8 A2Document1 pagePersonal Business Model Canvas v1.1.8 A2Laura Natalia SalcedoNo ratings yet
- Kacee-New ResumeDocument4 pagesKacee-New Resumeapi-678307618No ratings yet
- Computer: Assisted Semen AnalysisDocument9 pagesComputer: Assisted Semen AnalysisFayssal BenfoddaNo ratings yet
- Final Report-1Document12 pagesFinal Report-1ECEB139 PERURI SAMBA SIVA SRIDHARNo ratings yet
- Promethazine (Phenergan)Document1 pagePromethazine (Phenergan)Adrianne BazoNo ratings yet
- United States Patent (19) 11 Patent Number: 5,676,977: Antelman 45 Date of Patent: Oct. 14, 1997Document4 pagesUnited States Patent (19) 11 Patent Number: 5,676,977: Antelman 45 Date of Patent: Oct. 14, 1997Sunita MarturNo ratings yet