Professional Documents
Culture Documents
Abdominal Aortic Aneurysm Follow-Up (Without Repair)
Uploaded by
victor contrerasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abdominal Aortic Aneurysm Follow-Up (Without Repair)
Uploaded by
victor contrerasCopyright:
Available Formats
New 2018
American College of Radiology
ACR Appropriateness Criteria®
Abdominal Aortic Aneurysm Follow-up (Without Repair)
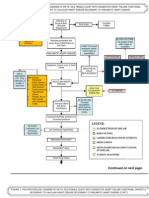
Variant 1: Asymptomatic abdominal aortic aneurysm surveillance (without repair).
Procedure Appropriateness Category Relative Radiation Level
US duplex Doppler aorta abdomen Usually Appropriate O
CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢
MRA abdomen and pelvis with IV contrast Usually Appropriate O
CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢
CT abdomen and pelvis without IV contrast May Be Appropriate ☢☢☢
MRA abdomen and pelvis without with IV
May Be Appropriate O
contrast
MRA abdomen and pelvis without IV contrast May Be Appropriate O
CT abdomen and pelvis without and with IV
May Be Appropriate ☢☢☢☢
contrast
MRI abdomen and pelvis with IV contrast May Be Appropriate O
MRI abdomen and pelvis without and with IV
May Be Appropriate O
contrast
MRI abdomen and pelvis without IV contrast May Be Appropriate (Disagreement) O
Aortography abdomen Usually Not Appropriate ☢☢☢
Radiography chest abdomen pelvis Usually Not Appropriate ☢☢☢
ACR Appropriateness Criteria® 1 AAA Follow-up (Without Repair)
ABDOMINAL AORTIC ANEURYSM FOLLOW-UP (WITHOUT REPAIR)
Expert Panel on Vascular Imaging: Michael Collard, MD, MA a ; Patrick D. Sutphin, MD, PhDb;
Sanjeeva P. Kalva, MDc; Bill S. Majdalany, MDd; Jeremy D. Collins, MDe; Jens Eldrup-Jorgensen, MDf;
Christopher J. Francois, MDg; Suvranu Ganguli, MDh; Andrew J. Gunn, MDi; A. Tuba Kendi, MDj;
Minhajuddin S. Khaja, MD, MBAk; Piotr Obara, MDl; Stephen P. Reis, MDm; Kanupriya Vijay, MD, MBBSn;
Karin E. Dill, MD.o
Summary of Literature Review
Introduction/Background
Abdominal aortic aneurysm (AAA) is defined as an aneurysmal dilation of the abdominal aorta of at least 3 cm in
diameter. This entity has a high degree of morbidity and mortality in the event of rupture [1,2]. To mitigate this
risk, screening programs have been widely instituted to identify small, developing aneurysms. Such screening
reduces morbidity and health care costs related to this disease [3-8]. An increasing number of aneurysms are
identified incidentally on ultrasound (US) and cross-sectional imaging, creating a growing cohort of patients with
known AAA [9-12]. The reported prevalence of AAA in persons >65 years of age ranges from 1.7% to 4.5% for
men and 0.5% to 1.3% for women [11,13,14].
While there is some debate in regards to which aneurysms are most at risk for rupture, there is general agreement
that AAA with a maximum diameter >5.4 cm in males and >4.9 cm in females [15] should undergo prophylactic
repair [2,14,16,17]. In patients with small AAA (males, diameter 3–5.4 cm, and females, diameter 3–4.9 cm), the
risk of rupture is lower; thus surgery and surveillance is indicated. The majority of small AAAs grow slowly, but
there is substantial variation in growth rates between individuals. The intervals between US surveillance
examinations used in randomized screening trials depend on aneurysm size [15,18-21]. However, no consensus
exists regarding the optimal time intervals between US surveillance examinations [15]. Some studies have
reported equivalent results for treatment of small aneurysms and surveillance, and there does not appear to be a
clear preference for early operation [22,23].
Imaging surveillance provides 2 primary purposes. The first is to identify interval growth beyond the threshold for
elective repair. The other is to monitor the growth trajectory and identify a potentially increasing rate of growth,
with growth rates >2 mm per year associated with increased adverse events [20].
For information on interventional planning and follow-up of AAA, please see the ACR Appropriateness Criteria®
topic on “Abdominal Aortic Aneurysm: Interventional Planning and Follow-Up” [24].
Special Imaging Considerations
For the purposes of distinguishing between CT and CT angiography (CTA), ACR Appropriateness Criteria topics
use the definition in the Practice Parameter for the Performance and Interpretation of Body Computed
Tomography Angiography (CTA) [25].
“CTA uses a thin-section CT acquisition that is timed to coincide with peak arterial or venous
enhancement. The resultant volumetric dataset is interpreted using primary transverse
reconstructions as well as multiplanar reformations and 3-D renderings.”
All elements are essential: 1) timing, 2) reconstructions/reformats, and 3) 3-D renderings. Standard CTs with
contrast also include timing issues and recons/reformats. Only in CTA, however, is 3-D rendering a required
element. This corresponds to the definitions that the CMS has applied to the Current Procedural Terminology
codes.
a
Research Author, UT Southwestern Medical Center, Dallas, Texas. bUT Southwestern Medical Center, Dallas, Texas. cPanel Chair, UT Southwestern
Medical Center, Dallas, Texas. dPanel Vice-chair, University of Michigan Health System, Ann Arbor, Michigan. eMayo Clinic, Rochester, Minnesota. fTufts
University School of Medicine, Boston, Massachusetts; Society for Vascular Surgery. gUniversity of Wisconsin, Madison, Wisconsin. hMassachusetts
General Hospital, Boston, Massachusetts. iUniversity of Alabama at Birmingham, Birmingham, Alabama. jMayo Clinic, Rochester, Minnesota. kUniversity
of Michigan Health System, Ann Arbor, Michigan. lLoyola University Medical Center, Maywood, Illinois. mColumbia University Medical Center, New
York, New York. nUT Southwestern Medical Center, Dallas, Texas. oSpecialty Chair, UMass Memorial Medical Center, Worcester, Massachusetts.
The American College of Radiology seeks and encourages collaboration with other organizations on the development of the ACR Appropriateness
Criteria through society representation on expert panels. Participation by representatives from collaborating societies on the expert panel does not necessarily
imply individual or society endorsement of the final document.
Reprint requests to: publications@acr.org
ACR Appropriateness Criteria® 2 AAA Follow-up (Without Repair)
Discussion of Procedures by Variant
Variant 1: Asymptomatic abdominal aortic aneurysm surveillance (without repair).
US Duplex Doppler Aorta Abdomen
US is the most widely studied and utilized imaging tool for evaluating an AAA, both for screening and during
surveillance. US has been verified as having consistent measurement accuracy, which can approximate the
accuracy demonstrated by CT and MRI or MR angiography (MRA) [17,18,26,27]. Studies have reported that US
may underestimate the maximum AAA diameter by 4 mm, on average, and the interobserver measurement
difference can range from 2 to 10 mm with US compared with <2 mm using CT [27-31]. Evidence is still lacking
as to whether these differences are clinically impactful. Variation in accuracy is believed to be related to
measurement technique. For example, there is debate as to whether to place the measurement caliper on the outer
or inner edge of the vessel, without clear consensus on an ideal methodology [31]. Finally, no significant
difference between rate of growth measurements between US and CT has been found [18,32]. US is also less
capable of identifying specific aneurysm features beyond diameter, such as intraluminal thrombus or adjacent
inflammation, both of which are more easily identified on CT [21,33,34].
CTA Abdomen and Pelvis
CTA of the abdomen and pelvis presents many benefits over the other modalities. Relative to US, CTA is
considered slightly more accurate at determining aneurysm diameter [27,30,31]. The use of iodinated contrast
carries its own risks and contraindications that require consideration [35].
CT Abdomen and Pelvis
The majority of evidence regarding AAA surveillance using CT is based on CTA data and is primarily related to
contrast bolus timing. Contrast-enhanced CT is well established in the literature and is capable of identifying
aortic aneurysms, with many papers discussing incidental AAA identification [9,11,13].
There is no specific literature regarding the use of noncontrast CT in the surveillance of AAA. One study
reviewed the incidence of AAA incidentally found during CT colonography. This included patients who
underwent CT imaging, some with and others without the use of intravenous (IV) contrast. This review did not
distinguish the difference between those patients [11]. This technique could theoretically be of use in patients with
chronic renal disease who have aneurysms less amenable to imaging by US. Noncontrast imaging can be
employed in CTA protocols to evaluate for calcification, with spectral CT scanners offering virtual noncontrast
reconstructions as an alternative.
MRA Abdomen and Pelvis
There are benefits of MRA that make it worth considering in the surveillance of AAA. MRA can be obtained
without the use of IV contrast, making it preferable in patients with advanced chronic renal disease. A prospective
evaluation of nonenhanced MRA compared with contrast-enhanced CTA demonstrated equivalent accuracy of
measurements for preoperative planning of endovascular aneurysm repair suggesting adequacy for surveillance
imaging [36]. Superparamagnetic iron oxide–enhanced MR may be an alternative for patients with chronic renal
disease [37].
MRI Abdomen and Pelvis
There is no relevant literature regarding the use of MRI for AAA surveillance in this setting; although, MRI may
be useful in some cases. Similar to CT, there is excellent reproducibility in measurements between MRI
examinations, a critical characteristic in monitoring for subtle changes in AAA size.
Aortography Abdomen
There is no relevant literature regarding the use of conventional angiography in the surveillance of AAA.
Noninvasive techniques to monitor aneurysm characteristics make this invasive option less reasonable.
Radiography Chest Abdomen Pelvis
There is no relevant literature regarding the use of radiography in the surveillance of AAA. Calcified aneurysms
may be identifiable by radiography.
Summary of Recommendations
• Variant 1: US duplex Doppler aorta of the abdomen, CTA of the abdomen and pelvis with IV contrast, or
MRA of the abdomen and pelvis with IV contrast is usually appropriate for the surveillance of patients with
an asymptomatic AAA not undergoing repair. These procedures are equivalent alternatives. The panel did not
ACR Appropriateness Criteria® 3 AAA Follow-up (Without Repair)
agree on recommending MRI of the abdomen and pelvis without IV contrast for asymptomatic AAA
surveillance without repair. There is insufficient medical literature to conclude whether or not these patients
would benefit from this procedure. The use of MRI of the abdomen and pelvis without IV contrast in this
patient population is controversial but may be appropriate.
Supporting Documents
The evidence table, literature search, and appendix for this topic are available at https://acsearch.acr.org/list. The
appendix includes the strength of evidence assessment and the final rating round tabulations for each
recommendation.
For additional information on the Appropriateness Criteria methodology and other supporting documents go to
www.acr.org/ac.
Appropriateness Category Names and Definitions
Appropriateness
Appropriateness Category Name Appropriateness Category Definition
Rating
The imaging procedure or treatment is indicated in
Usually Appropriate 7, 8, or 9 the specified clinical scenarios at a favorable risk-
benefit ratio for patients.
The imaging procedure or treatment may be
indicated in the specified clinical scenarios as an
May Be Appropriate 4, 5, or 6 alternative to imaging procedures or treatments with
a more favorable risk-benefit ratio, or the risk-benefit
ratio for patients is equivocal.
The individual ratings are too dispersed from the
panel median. The different label provides
May Be Appropriate transparency regarding the panel’s recommendation.
5
(Disagreement) “May be appropriate” is the rating category and a
rating of 5 is assigned.
The imaging procedure or treatment is unlikely to be
indicated in the specified clinical scenarios, or the
Usually Not Appropriate 1, 2, or 3 risk-benefit ratio for patients is likely to be
unfavorable.
Relative Radiation Level Information
Potential adverse health effects associated with radiation exposure are an important factor to consider when
selecting the appropriate imaging procedure. Because there is a wide range of radiation exposures associated with
different diagnostic procedures, a relative radiation level (RRL) indication has been included for each imaging
examination. The RRLs are based on effective dose, which is a radiation dose quantity that is used to estimate
population total radiation risk associated with an imaging procedure. Patients in the pediatric age group are at
inherently higher risk from exposure, because of both organ sensitivity and longer life expectancy (relevant to the
long latency that appears to accompany radiation exposure). For these reasons, the RRL dose estimate ranges for
pediatric examinations are lower as compared with those specified for adults (see Table below). Additional
information regarding radiation dose assessment for imaging examinations can be found in the ACR
Appropriateness Criteria® Radiation Dose Assessment Introduction document [38].
ACR Appropriateness Criteria® 4 AAA Follow-up (Without Repair)
Relative Radiation Level Designations
Adult Effective Dose Estimate Pediatric Effective Dose Estimate
Relative Radiation Level*
Range Range
O 0 mSv 0 mSv
☢ <0.1 mSv <0.03 mSv
☢☢ 0.1-1 mSv 0.03-0.3 mSv
☢☢☢ 1-10 mSv 0.3-3 mSv
☢☢☢☢ 10-30 mSv 3-10 mSv
☢☢☢☢☢ 30-100 mSv 10-30 mSv
*RRL assignments for some of the examinations cannot be made, because the actual patient doses in these procedures vary
as a function of a number of factors (eg, region of the body exposed to ionizing radiation, the imaging guidance that is
used). The RRLs for these examinations are designated as “Varies”.
References
1. Ahmed R, Ghoorah K, Kunadian V. Abdominal Aortic Aneurysms and Risk Factors for Adverse Events.
Cardiol Rev 2016;24:88-93.
2. Lim J, Wolff J, Rodd CD, Cooper DG, Earnshaw JJ. Outcome in Men with a Screen-detected Abdominal
Aortic Aneurysm Who are not Fit for Intervention. Eur J Vasc Endovasc Surg 2015;50:732-6.
3. Chun KC, Teng KY, Van Spyk EN, Carson JG, Lee ES. Outcomes of an abdominal aortic aneurysm
screening program. J Vasc Surg 2013;57:376-81.
4. Giardina S, Pane B, Spinella G, et al. An economic evaluation of an abdominal aortic aneurysm screening
program in Italy. J Vasc Surg 2011;54:938-46.
5. Macdonald AJ, Faleh O, Welch G, Kettlewell S. Missed opportunities for the detection of abdominal aortic
aneurysms. Eur J Vasc Endovasc Surg 2008;35:698-700.
6. Schmidt T, Muhlberger N, Chemelli-Steingruber IE, et al. Benefit, risks and cost-effectiveness of screening
for abdominal aortic aneurysm. Rofo 2010;182:573-80.
7. Stather PW, Dattani N, Bown MJ, Earnshaw JJ, Lees TA. International variations in AAA screening. Eur J
Vasc Endovasc Surg 2013;45:231-4.
8. Wild JB, Stather PW, Biancari F, et al. A multicentre observational study of the outcomes of screening
detected sub-aneurysmal aortic dilatation. Eur J Vasc Endovasc Surg 2013;45:128-34.
9. Al-Thani H, El-Menyar A, Shabana A, Tabeb A, Al-Sulaiti M, Almalki A. Incidental abdominal aneurysms: a
retrospective study of 13,115 patients who underwent a computed tomography scan. Angiology 2014;65:388-
95.
10. Dell'Atti L. Incidence of abdominal aortic aneurysm during diagnostic ultrasound for urologic disease: our
experience. Arch Ital Urol Androl 2012;84:230-3.
11. Khashram M, Jones GT, Roake JA. Prevalence of abdominal aortic aneurysm (AAA) in a population
undergoing computed tomography colonography in Canterbury, New Zealand. Eur J Vasc Endovasc Surg
2015;50:199-205.
12. Trompeter AJ, Paremain GP. Incidental abdominal aortic aneurysm on lumbosacral magnetic resonance
imaging - a case series. Magn Reson Imaging 2010;28:455-7.
13. Claridge R, Arnold S, Morrison N, van Rij AM. Measuring abdominal aortic diameters in routine abdominal
computed tomography scans and implications for abdominal aortic aneurysm screening. J Vasc Surg
2017;65:1637-42.
14. Lo RC, Schermerhorn ML. Abdominal aortic aneurysms in women. J Vasc Surg 2016;63:839-44.
15. Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the
care of patients with an abdominal aortic aneurysm. J Vasc Surg 2018;67:2-77 e2.
16. Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 Practice Guidelines for the management of patients
with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative
report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for
Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of
Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to
Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the
ACR Appropriateness Criteria® 5 AAA Follow-up (Without Repair)
American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood
Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease
Foundation. Circulation 2006;113:e463-654.
17. Kitagawa A, Mastracci TM, von Allmen R, Powell JT. The role of diameter versus volume as the best
prognostic measurement of abdominal aortic aneurysms. J Vasc Surg 2013;58:258-65.
18. Bown MJ, Sweeting MJ, Brown LC, Powell JT, Thompson SG. Surveillance intervals for small abdominal
aortic aneurysms: a meta-analysis. JAMA 2013;309:806-13.
19. Mell MW, Baker LC. Payer status, preoperative surveillance, and rupture of abdominal aortic aneurysms in
the US Medicare population. Ann Vasc Surg 2014;28:1378-83.
20. Thompson AR, Cooper JA, Ashton HA, Hafez H. Growth rates of small abdominal aortic aneurysms correlate
with clinical events. Br J Surg 2010;97:37-44.
21. van Walraven C, Wong J, Morant K, et al. Radiographic monitoring of incidental abdominal aortic
aneurysms: a retrospective population-based cohort study. Open Med 2011;5:e67-76.
22. Cao P, De Rango P, Verzini F, et al. Comparison of surveillance versus aortic endografting for small
aneurysm repair (CAESAR): results from a randomised trial. Eur J Vasc Endovasc Surg 2011;41:13-25.
23. Ouriel K, Clair DG, Kent KC, Zarins CK, Positive Impact of Endovascular Options for treating Aneurysms
Early I. Endovascular repair compared with surveillance for patients with small abdominal aortic aneurysms.
J Vasc Surg 2010;51:1081-7.
24. Francois CJ, Skulborstad EP, Majdalany BS, et al. ACR Appropriateness Criteria® Abdominal Aortic
Aneurysm: Interventional Planning and Follow-Up. J Am Coll Radiol 2018;15:S2-S12.
25. American College of Radiology. ACR–NASCI–SIR–SPR Practice Parameter for the Performance and
Interpretation of Body Computed Tomography Angiography (CTA). Available at: https://www.acr.org/-
/media/ACR/Files/Practice-Parameters/body-cta.pdf. Accessed November 30, 2018.
26. Hafez H, Druce PS, Ashton HA. Abdominal aortic aneurysm development in men following a "normal" aortic
ultrasound scan. Eur J Vasc Endovasc Surg 2008;36:553-8.
27. Keefer A, Hislop S, Singh MJ, Gillespie D, Illig KA. The influence of aneurysm size on anatomic suitability
for endovascular repair. J Vasc Surg 2010;52:873-7.
28. Beales L, Wolstenhulme S, Evans JA, West R, Scott DJ. Reproducibility of ultrasound measurement of the
abdominal aorta. Br J Surg 2011;98:1517-25.
29. Gurtelschmid M, Bjorck M, Wanhainen A. Comparison of three ultrasound methods of measuring the
diameter of the abdominal aorta. Br J Surg 2014;101:633-6.
30. Kauffmann C, Tang A, Therasse E, et al. Measurements and detection of abdominal aortic aneurysm growth:
Accuracy and reproducibility of a segmentation software. Eur J Radiol 2012;81:1688-94.
31. Wanhainen A, Mani K, Golledge J. Surrogate Markers of Abdominal Aortic Aneurysm Progression.
Arterioscler Thromb Vasc Biol 2016;36:236-44.
32. Sweeting MJ, Thompson SG, Brown LC, Powell JT. Meta-analysis of individual patient data to examine
factors affecting growth and rupture of small abdominal aortic aneurysms. Br J Surg 2012;99:655-65.
33. Labruto F, Blomqvist L, Swedenborg J. Imaging the intraluminal thrombus of abdominal aortic aneurysms:
techniques, findings, and clinical implications. J Vasc Interv Radiol 2011;22:1069-75; quiz 75.
34. Martufi G, Forneris A, Appoo JJ, Di Martino ES. Is There a Role for Biomechanical Engineering in Helping
to Elucidate the Risk Profile of the Thoracic Aorta? Ann Thorac Surg 2016;101:390-8.
35. American College of Radiology. Manual on Contrast Media. Available at: https://www.acr.org/Clinical-
Resources/Contrast-Manual. Accessed November 30, 2018.
36. Goshima S, Kanematsu M, Kondo H, et al. Preoperative planning for endovascular aortic repair of abdominal
aortic aneurysms: feasibility of nonenhanced MR angiography versus contrast-enhanced CT angiography.
Radiology 2013;267:948-55.
37. Ichihashi S, Marugami N, Tanaka T, et al. Preliminary experience with superparamagnetic iron oxide-
enhanced dynamic magnetic resonance imaging and comparison with contrast-enhanced computed
tomography in endoleak detection after endovascular aneurysm repair. J Vasc Surg 2013;58:66-72.
38. American College of Radiology. ACR Appropriateness Criteria® Radiation Dose Assessment Introduction.
Available at: https://www.acr.org/-/media/ACR/Files/Appropriateness-
Criteria/RadiationDoseAssessmentIntro.pdf. Accessed November 30, 2018.
ACR Appropriateness Criteria® 6 AAA Follow-up (Without Repair)
The ACR Committee on Appropriateness Criteria and its expert panels have developed criteria for determining appropriate imaging examinations for
diagnosis and treatment of specified medical condition(s). These criteria are intended to guide radiologists, radiation oncologists and referring physicians
in making decisions regarding radiologic imaging and treatment. Generally, the complexity and severity of a patient’s clinical condition should dictate the
selection of appropriate imaging procedures or treatments. Only those examinations generally used for evaluation of the patient’s condition are ranked.
Other imaging studies necessary to evaluate other co-existent diseases or other medical consequences of this condition are not considered in this
document. The availability of equipment or personnel may influence the selection of appropriate imaging procedures or treatments. Imaging techniques
classified as investigational by the FDA have not been considered in developing these criteria; however, study of new equipment and applications should
be encouraged. The ultimate decision regarding the appropriateness of any specific radiologic examination or treatment must be made by the referring
physician and radiologist in light of all the circumstances presented in an individual examination.
ACR Appropriateness Criteria® 7 AAA Follow-up (Without Repair)
You might also like
- Penetrating TraumaDocument29 pagesPenetrating TraumaArdianto SucintaNo ratings yet
- Hospital and Critical CareDocument16 pagesHospital and Critical CareMarivy GalonNo ratings yet
- Imaging Abdominal Trauma Focus On FAST Revisi DR - BahtiarDocument54 pagesImaging Abdominal Trauma Focus On FAST Revisi DR - BahtiarJackson HakimNo ratings yet
- Surgery MrcsDocument339 pagesSurgery Mrcsdr_shafiq80% (10)
- Pancreatic Adenocarcinoma ImagingDocument9 pagesPancreatic Adenocarcinoma ImagingDinesh RamaswamyNo ratings yet
- Colorectal SurgeryDocument73 pagesColorectal SurgeryShashidhara PuttarajNo ratings yet
- Pathophysiology of Congestive Heart FailureDocument2 pagesPathophysiology of Congestive Heart FailureAnonymous XvwKtnSrMR100% (10)
- The ACM v2.0 International PDFDocument76 pagesThe ACM v2.0 International PDFTiago SilvaNo ratings yet
- Imaging AppendicitisDocument75 pagesImaging AppendicitiswilandayuNo ratings yet
- Blunt Abdominal TraumaDocument20 pagesBlunt Abdominal TraumaDeusah EzrahNo ratings yet
- List of Emergency Drugs and Their Action PDFDocument3 pagesList of Emergency Drugs and Their Action PDFDr. Vishal SengarNo ratings yet
- Abdominal Aortic Aneurysm-Interventional Planning and Follow-UpDocument13 pagesAbdominal Aortic Aneurysm-Interventional Planning and Follow-Upvictor contrerasNo ratings yet
- Aaa RepairDocument5 pagesAaa RepairLakshmi Mounica GrandhiNo ratings yet
- Acute Nonspecific Chest Pain-Low Probability of Coronary Artery DiseaseDocument10 pagesAcute Nonspecific Chest Pain-Low Probability of Coronary Artery Diseasevictor contrerasNo ratings yet
- Blunt Abdominal TraumaDocument11 pagesBlunt Abdominal TraumaRahmat SyahiliNo ratings yet
- Abnormal Uterine BleedingDocument12 pagesAbnormal Uterine Bleedingvictor contrerasNo ratings yet
- Hematuria PDFDocument11 pagesHematuria PDFPipitNo ratings yet
- Postmenopausal Subacute or Chronic Pelvic PainDocument9 pagesPostmenopausal Subacute or Chronic Pelvic PainM SNo ratings yet
- ACR Appropriateness Criteria Pancreatic CystDocument9 pagesACR Appropriateness Criteria Pancreatic CystSole GonzalezNo ratings yet
- American College of Radiology ACR Appropriateness CriteriaDocument10 pagesAmerican College of Radiology ACR Appropriateness CriteriaNovia ChrisnawatiNo ratings yet
- Scrotal PainDocument7 pagesScrotal PainPipitNo ratings yet
- Abdominal Aortic Aneurysm ImagingDocument7 pagesAbdominal Aortic Aneurysm ImagingVishal GaikwadNo ratings yet
- Adrenal Mass EvaluationDocument19 pagesAdrenal Mass Evaluationpj rakNo ratings yet
- Online Radiography Continuing EducationDocument39 pagesOnline Radiography Continuing EducationAndy WijayaNo ratings yet
- Screening Guidelines and Treatment Options For Abdominal Aortic AneurysmsDocument36 pagesScreening Guidelines and Treatment Options For Abdominal Aortic AneurysmsmazriyahyaNo ratings yet
- Acute PancreatitisDocument16 pagesAcute PancreatitisLoredana BoghezNo ratings yet
- Acute Hip Pain-Suspected FractureDocument9 pagesAcute Hip Pain-Suspected FractureMario UmañaNo ratings yet
- Occupational Lung DiseasesDocument13 pagesOccupational Lung DiseasesVianney OlveraNo ratings yet
- Jurnal Radiologi FixDocument44 pagesJurnal Radiologi FixAfifa Prima GittaNo ratings yet
- 1.2.2. Emergency Abdominal ImagingDocument51 pages1.2.2. Emergency Abdominal ImagingNoura AdzmiaNo ratings yet
- Dynamic CT Findings of A Polypoid Gastric - ChrisnaDocument4 pagesDynamic CT Findings of A Polypoid Gastric - ChrisnaferonicaNo ratings yet
- Multimodality Approach For Imaging of Non-Traumatic Acute Abdominal EmergenciesDocument13 pagesMultimodality Approach For Imaging of Non-Traumatic Acute Abdominal EmergenciesfalisNo ratings yet
- Abdominal USG in EDDocument9 pagesAbdominal USG in EDanon_773331597No ratings yet
- Iaim 2015 0206 17Document13 pagesIaim 2015 0206 17fahrunisaNo ratings yet
- Infective EndocarditisDocument13 pagesInfective Endocarditispaquidermo85No ratings yet
- Abdominal ImagingDocument45 pagesAbdominal ImagingFahriansyah Mp Tmc100% (1)
- Onset Flank PainDocument11 pagesOnset Flank PainPipitNo ratings yet
- MCQ Year 3,26th July (Omega 7)Document28 pagesMCQ Year 3,26th July (Omega 7)Ammal Dzulfiqar Ismail100% (1)
- Batchala 2021Document6 pagesBatchala 2021qrscentralNo ratings yet
- Update Imagenes ApendicitisDocument14 pagesUpdate Imagenes ApendicitisAlejandra MuglisaNo ratings yet
- Clinical Anatomy - 2020 - Le Saint Grant - Arterial Anatomy of The Anterior Abdominal Wall Ultrasound Evaluation As ADocument6 pagesClinical Anatomy - 2020 - Le Saint Grant - Arterial Anatomy of The Anterior Abdominal Wall Ultrasound Evaluation As AarifNo ratings yet
- Imaging The Female Pelvis: When Should MRI Be Considered?: Jennifer Hubert, MD, and Diane Bergin, MDDocument14 pagesImaging The Female Pelvis: When Should MRI Be Considered?: Jennifer Hubert, MD, and Diane Bergin, MDradiologyliNo ratings yet
- Major Blunt TraumaDocument18 pagesMajor Blunt TraumaghassanNo ratings yet
- Approach Considerations: View Media GalleryDocument5 pagesApproach Considerations: View Media GalleryAziil LiizaNo ratings yet
- Jurnal Bahasa Inggris Radiologi AapDocument11 pagesJurnal Bahasa Inggris Radiologi AapDessy leonni100% (1)
- Breast PainDocument9 pagesBreast PainmarysrbNo ratings yet
- Role of Computed Tomography (CT) Scan in Staging of Cervical CarcinomaDocument6 pagesRole of Computed Tomography (CT) Scan in Staging of Cervical CarcinomaTriponiaNo ratings yet
- Abdominal Aortic Aneurysm: A Comprehensive ReviewDocument5 pagesAbdominal Aortic Aneurysm: A Comprehensive Reviewnico rifandhaNo ratings yet
- Ultrazvuk AbdomenaDocument10 pagesUltrazvuk AbdomenaLejlaNo ratings yet
- Rationale Diagnostic ProceduresDocument22 pagesRationale Diagnostic ProceduresShaktisila FatrahadyNo ratings yet
- QCHMWRV F4 FJ 7 XJ Q9 DW 6 Q8 P BDocument11 pagesQCHMWRV F4 FJ 7 XJ Q9 DW 6 Q8 P BFavio Alvarez De BejarNo ratings yet
- Theroleofradiation Therapyforpancreatic Cancerintheadjuvantand NeoadjuvantsettingsDocument23 pagesTheroleofradiation Therapyforpancreatic Cancerintheadjuvantand Neoadjuvantsettings980Denis FernandezNo ratings yet
- ACR Appropriateness Criteria Right Upper Quadrant PainDocument9 pagesACR Appropriateness Criteria Right Upper Quadrant PainDoc Tor StrangeNo ratings yet
- Modifications of X-RayDocument6 pagesModifications of X-Rayolajumokeojo9No ratings yet
- Management of Asymptomatic Abdominal Aortic Aneurysm - UpToDateDocument53 pagesManagement of Asymptomatic Abdominal Aortic Aneurysm - UpToDateGiancarlo Maruri MunarettoNo ratings yet
- Baumann 2016 IJROBP Development Validation of Bladder Contouring AtlasDocument9 pagesBaumann 2016 IJROBP Development Validation of Bladder Contouring AtlaszanNo ratings yet
- Appendicitis Imaging: Practice EssentialsDocument6 pagesAppendicitis Imaging: Practice EssentialsAjp Ryuzaki CaesarNo ratings yet
- Clinical Features and Diagnosis of Abdominal Aortic Aneurysm - UpToDateDocument53 pagesClinical Features and Diagnosis of Abdominal Aortic Aneurysm - UpToDateALVARO ARIASNo ratings yet
- Acute Onset Flank Pain PDFDocument6 pagesAcute Onset Flank Pain PDFYuliana WiralestariNo ratings yet
- Management Guidelines For Penetrating Abdominal Trauma: Walter L. Biffl and Ernest E. MooreDocument9 pagesManagement Guidelines For Penetrating Abdominal Trauma: Walter L. Biffl and Ernest E. MooreArsy Mira PertiwiNo ratings yet
- Defreitas 2018Document6 pagesDefreitas 2018drrajeshb77No ratings yet
- The SAGES Manual of Colorectal SurgeryFrom EverandThe SAGES Manual of Colorectal SurgeryPatricia SyllaNo ratings yet
- Stages of ShockDocument1 pageStages of ShockronaNo ratings yet
- Comparison of Inflammatory Markers in HTNDocument6 pagesComparison of Inflammatory Markers in HTNDan JohnstonNo ratings yet
- SyncopeDocument6 pagesSyncopeDodi TambunNo ratings yet
- Electrophysiology of The HeartDocument32 pagesElectrophysiology of The HeartJohn Carlo ConsultaNo ratings yet
- 5 ECG Changes of Hyperkalemia You Need To Know: 1. Tall 'Tented' T WavesDocument4 pages5 ECG Changes of Hyperkalemia You Need To Know: 1. Tall 'Tented' T Wavesricky hutagalungNo ratings yet
- 6th Bio Final Term 2021-2022.Document3 pages6th Bio Final Term 2021-2022.Navya ChaplotNo ratings yet
- Simulacro Enarm 2011Document81 pagesSimulacro Enarm 2011Ricardo López SánchezNo ratings yet
- Intermittent Left Bundle Branch Block - A Diagnostic DilemmaDocument4 pagesIntermittent Left Bundle Branch Block - A Diagnostic DilemmaCorina GrosuNo ratings yet
- Cardiovascular System AnatomyDocument13 pagesCardiovascular System AnatomyDwi Junita SariNo ratings yet
- Programme Gulfpcr2023Document21 pagesProgramme Gulfpcr2023Abid KhanNo ratings yet
- Test Bank For Interpreting Ecgs A Practical Approach 3rd Edition Bruce ShadeDocument11 pagesTest Bank For Interpreting Ecgs A Practical Approach 3rd Edition Bruce ShadeLisaTurnerMDkfym100% (27)
- A Case of Severe Tuberculous Pericardial EffusionDocument2 pagesA Case of Severe Tuberculous Pericardial Effusionsweet hanaNo ratings yet
- Conserving Blood During Cardiac Surgery at Huntington University Hospital (A)Document6 pagesConserving Blood During Cardiac Surgery at Huntington University Hospital (A)Touba KhalidNo ratings yet
- Cardio-Oncology Clinical ReviewDocument58 pagesCardio-Oncology Clinical ReviewNickname TanatornNo ratings yet
- Acp Dipiro Eg Hypertension FinalDocument83 pagesAcp Dipiro Eg Hypertension FinalAlberto CombiNo ratings yet
- MCQs InternalDocument20 pagesMCQs InternalOsama AlhumisiNo ratings yet
- Review Jurnal ProcainamidDocument9 pagesReview Jurnal ProcainamidEko FebryandiNo ratings yet
- Jurnal Pakai 3 (Etiologi) Efusi PerikardiumDocument10 pagesJurnal Pakai 3 (Etiologi) Efusi PerikardiumSatrya DitaNo ratings yet
- Spontaneous Coronary Artery Dissection With Clinical Presentation of Acute Myocardial InfarctionDocument3 pagesSpontaneous Coronary Artery Dissection With Clinical Presentation of Acute Myocardial InfarctionSabrina JonesNo ratings yet
- Fibrion-Tetagam DXMDocument33 pagesFibrion-Tetagam DXMDella Puspita SariNo ratings yet
- Tests Module 2Document59 pagesTests Module 2Haruna Bzaki100% (1)
- Ginekologija Sa AkusertsvomDocument2 pagesGinekologija Sa AkusertsvomZaklina RistovicNo ratings yet
- Naskah Publikasi Agiliaaa-1Document5 pagesNaskah Publikasi Agiliaaa-1Indra AlazharNo ratings yet
- ECG NotesDocument8 pagesECG NotesPeer TutorNo ratings yet
- Luka Bakar E.C Air Panas Grade IIA 18 %: Oleh: Rizal Palero S.Ked PEMBIMBING: Dr. Jimmy Vareta, Sp. BDocument18 pagesLuka Bakar E.C Air Panas Grade IIA 18 %: Oleh: Rizal Palero S.Ked PEMBIMBING: Dr. Jimmy Vareta, Sp. BRizal PaleroNo ratings yet
- Dry Foot GangreneDocument2 pagesDry Foot Gangreneenjey19No ratings yet