Professional Documents
Culture Documents
Agosto Salgado Et Al 2023 Management of Advanced Thyroid Cancer Overview Advances and Opportunities
Uploaded by
Nicole Antoine-Feill BarónCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Agosto Salgado Et Al 2023 Management of Advanced Thyroid Cancer Overview Advances and Opportunities
Uploaded by
Nicole Antoine-Feill BarónCopyright:
Available Formats
HEAD AND NECK CANCER
Management of Advanced Thyroid Cancer:
Overview, Advances, and Opportunities
Sarimar Agosto Salgado, MD1; Erin Rachel Kaye, MD2; Zoukaa Sargi, MD, MPH3; Christine H. Chung, MD1; and Maria Papaleontiou, MD4
overview
Thyroid cancer is the most common endocrine malignancy with almost one million people living with thyroid
cancer in the United States. Although early-stage well-differentiated thyroid cancers account for the majority
of thyroid cancers on diagnosis and have excellent survival rates, the incidence of advanced-stage disease has
increased over the past few years and confers poorer prognosis. Until recently, patients with advanced thyroid
cancer had limited therapeutic options. However, the landscape of thyroid cancer treatment has dramatically
changed in the past decade with the current availability of several novel effective therapeutic options, leading
to significant advances and improved patient outcomes in the management of advanced disease. In this
review, we summarize the current status of advanced thyroid cancer treatment options and discuss recent
advances made in targeted therapies that have proven promising to clinically benefit patients with advanced
thyroid cancer.
INTRODUCTION challenges in the management of RAIR thyroid cancer,
Thyroid cancer is the most common endocrine and advances in systemic therapies, particularly
malignancy with the prevalence in the United States progress pertaining to targeted therapies.
currently exceeding 900,000 cases. 1 Overall, the
majority of thyroid cancers detected are early-stage DEFINITION OF ADVANCED THYROID CANCER
well-differentiated thyroid cancers (DTCs) that have Advanced thyroid cancer is a term used to describe
an excellent prognosis 1; however, some evidence aggressive tumors; however, there is significant vari-
shows that the incidence of advanced thyroid ability among specialties. Surgeons refer to unresect-
cancers has increased in recent years. 2 In 2022, able tumors as advanced thyroid cancers,
2,230 patients died of thyroid cancer in the United endocrinologists to describe RAIR tumors, and on-
States.1 cologists when there are distant metastases.6 A recent
consensus statement by the American Head and Neck
Follicular-derived thyroid cancers include papillary
Society (AHNS) Endocrine Surgery Section and In-
thyroid cancer, follicular thyroid cancer, Hürthle cell
ternational Thyroid Oncology Group defined advanced
cancer, poorly DTC, and undifferentiated (anaplastic)
thyroid cancer according to four categories. The
thyroid cancer (ATC). Although surgery and radio-
structural/surgical category encompasses the follow-
active iodine (RAI) are the standard of care for DTCs
ing: (1) bulky, invasive, or inoperative locoregional
often leading to cure, patients with radioactive-iodine
disease; (2) recurrence; (3) distant metastases; (4)
refractory (RAIR) disease, DTCs, and ATCs confer
gross residual neck disease without option for reop-
poorer prognosis and pose significant challenges for
eration; (5) rapid progression on imaging; and (6)
treating clinicians. Medullary thyroid cancer (MTC)
imminent threat posed by tumor burden. Tumors re-
arises from parafollicular or C cells and accounts for
fractory to RAI, unresponsive to thyroid-stimulating
Author affiliations
fewer than 5% of thyroid cancer diagnoses but ap-
hormone (TSH) suppression, and rapid calcitonin,
and support proximately 13% of thyroid cancer deaths.3 Overall,
carcinoembryonic antigen, or thyroglobulin doubling
information (if approximately 20% of cases are familial secondary to
applicable) appear
times constitute the biochemical category. The histo-
a germline rearranged during transfection (RET)
at the end of this logic/molecular category includes findings such as
mutation while the remaining cases are sporadic.4
article. poorly differentiated or other aggressive histology
Patients with MTC who present with regional lymph
Accepted on April 5, components, high Ki67 index, high mitotic count or
2023 and published node metastases and/or distant metastases are less
tumor necrosis, and all anaplastic thyroid carcinoma.
at ascopubs.org on likely to be cured of their disease.5
Finally, tumors can be categorized as advanced thyroid
May 15, 2023:
DOI https://doi.org/
This review focuses on the current status of advanced cancer at the discretion of the treating physician if there
10.1200/EDBK_ thyroid cancer treatment options, summarizing the role are features that portend aggressive tumor behavior
389708 of surgery in advanced thyroid cancer management, (clinician prerogative).
2023 ASCO EDUCATIONAL BOOK | asco.org/edbook 1
Downloaded from ascopubs.org by 201.245.214.236 on August 23, 2023 from 201.245.214.236
Copyright © 2023 American Society of Clinical Oncology. All rights reserved.
Agosto Salgado et al
dedicated imaging with CT of the chest (trachea) and MRI
(esophagus) is recommended.9
PRACTICAL APPLICATIONS
• Surgical management of advanced thyroid According to the ATA guidelines, patients with DTC
cancer is challenging and should evolve from are subdivided into three categories with treatment
multidisciplinary discussion integrating indi- implications7:
vidual disease characteristics, expected surgi- 1. Thyroid cancer .4 cm, gross extrathyroidal extension
cal morbidity, and patient preferences. (ETE; clinical T4), nodal disease (clinical N1), or distant
• Common clinical scenarios suggestive of ra- metastasis
dioactive iodine (RAI) refractory thyroid cancer 2. Thyroid cancer .1 cm and ,4 cm without ETE and
include a negative diagnostic RAI uptake whole- without nodal disease or metastasis
body scan, loss of RAI uptake on post-therapy 3. Thyroid cancer ,1 cm without ETE and without nodal
RAI scan, presence of RAI in some tissues but
disease
not others, and metastatic disease progression
despite ability to concentrate RAI, including a For group 1, total thyroidectomy is the recommended
cumulative activity of .600 mCi. treatment. For patients in group 2, either option of lobec-
• An improved understanding of thyroid cancer tomy or total thyroidectomy is acceptable. The decision-
pathogenesis has led to a remarkable change in making process regarding the extent of surgical resection in
the landscape of available systemic targeted these patients involves a cohesive discussion between the
therapies for patients with advanced and re- treatment team and the patient. If RAI is planned or likely to
fractory disease in the past several years. be recommended, total thyroidectomy would be indicated.
• Treatment decisions regarding use of targeted Finally, for patients in group 3, watchful waiting with sur-
therapies for advanced thyroid cancer should veillance may be an option in cases of low-risk differentiated
be made judiciously by a multidisciplinary team tumors; if surgery is preferred, thyroid lobectomy is rec-
while weighing risks versus benefits and un- ommended unless there is an indication to remove the
dertaking close surveillance for disease pro- contralateral lobe or a history of previous head and neck
gression and adverse events. radiation or familial thyroid carcinoma.7,10
The ATA guidelines also incorporate indications for nodal
dissection. With clinically evident central compartment and/
ROLE OF SURGERY IN ADVANCED THYROID CANCER or lateral neck disease, dissection is recommended at the
time of initial surgery. Central compartment lymph node
DTC
dissection, or level VI, includes pretracheal and para-
The 2015 American Thyroid Association (ATA) guidelines tracheal nodes. Lateral neck dissection typically incorpo-
established protocols for surgically managing tumors on the rates level II-IV nodal levels, extending from the skull base
basis of size, stage, and aggressive features.7 The guidelines superiorly to the clavicle inferiorly and from the strap
provide guidance regarding surgical indications and extent muscles medially to the posterior border of the sternoclei-
of surgery (lobectomy v total thyroidectomy). There has domastoid muscle laterally. Nodal dissection of an addi-
been a shift toward lobectomy in certain cases, as detailed tional level may be incorporated if there is clinically evident
below. nodal disease. Prophylactic central compartment dissection
Preoperative workup in patients with thyroid cancer in- can be considered in patients with advanced papillary
cludes imaging and thyroid function tests. Ultrasound is carcinoma (T3 or T4), clinically involved lateral nodes, or if
the recommended initial imaging modality and should the nodal tissue may guide adjuvant treatment.7
include the thyroid, central compartment, and bilateral In regard to management of invasive DTC, which occurs in
lateral neck nodes.7 Additional imaging, that is, computed up to 15% of patients, the AHNS published a series of
tomography (CT) and magnetic resonance imaging (MRI) consensus statements in 2014.9 These consensus state-
with intravenous contrast, is recommended in patients ments can be used to guide preoperative workup and
with advanced thyroid cancer, suspicion for local invasion, intraoperative management. The recurrent laryngeal nerve
and multiple or bulky lymphadenopathy. Chest CT should (RLN) is involved in 33%-61% of patients with invasive
be considered if there is concern for low mediastinal cancer. Fiberoptic laryngoscopy is the preferred method of
nodes or pulmonary metastasis. Positron emission to- laryngeal evaluation, particularly when voice is abnormal, if
mography (PET) may be used in recurrent cases or history of thyroid surgery, or if ETE is suspected. Man-
for surveillance.8 In cases of advanced disease when agement of the RLN during surgery varies according
invasion is suspected, additional preoperative workup to preoperative function, degree of invasion, and status
including larynx evaluation, swallow function, and of the contralateral nerve and has important functional
2 2023 ASCO EDUCATIONAL BOOK | asco.org/edbook
Downloaded from ascopubs.org by 201.245.214.236 on August 23, 2023 from 201.245.214.236
Copyright © 2023 American Society of Clinical Oncology. All rights reserved.
Updates in Advanced Thyroid Cancer Management
implications for voice, breathing, and swallow. Although Finally, in 2016, the AHNS published a consensus state-
intraoperative RLN monitoring is commonly used for eval- ment recommending revision surgery for tumor and nodal
uation of nerve status, the nerve should still be identified recurrence, if feasible. In revision surgery, the primary goal
intraoperatively.7,11,12 Postoperative unilateral dysfunction is is to remove recurrent cancer in the thyroid or nodal tissue,
often evident if voice changes occur and may lead to as- remove remaining thyroid tissue, and perform nodal dis-
piration, whereas bilateral dysfunction typically presents section in regions suspected to have microscopic disease.17
with shortness of breath and stridor. Preservation of the
Medullary Thyroid Carcinoma
parathyroid glands should be attempted with dissection
along the thyroid capsule to avoid inadvertent injury to their Total thyroidectomy and central neck dissection (level VI),
vascular supply. Intraoperatively, the thyroid specimen with dissection of lymph nodes in the lateral compartments
should be carefully examined after removal for any para- (levels II-V) depending on calcitonin levels and ultrasound
thyroid tissue. If identified, the parathyroid should be findings, is a standard treatment for patients with sporadic
reimplanted into nearby muscle, and postoperative calcium or hereditary MTC.18,19 When preoperative imaging is
and parathyroid hormone levels should be monitored.7 positive in the ipsilateral lateral neck compartment but
negative in the contralateral neck compartment, contra-
Additional structures including the trachea and larynx may
lateral neck dissection should be considered if the basal
be abutted or directly invaded in patients with advanced
serum calcitonin level is .200 pg/mL.18
DTC. If invasion is suspected, direct laryngoscopy and
bronchoscopy are performed. The extent of invasion helps Anaplastic Thyroid Carcinoma
to guide the recommended intraoperative decision making,
Surgical options must be carefully evaluated in patients with
for example, whether to perform a tracheal shave versus a
ATC while balancing risks and benefits with goals of care.
circumferential tracheal resection or partial versus total
The primary goal for resectable tumors (stages IVA and IVB)
laryngectomy.9 Because esophageal invasion usually in-
is an aggressive approach with complete resection, followed
volves only the muscularis layer, extent of invasion may not
by definitive chemoradiation. In stage IVC ATC, the limited
be seen on esophagoscopy. Similar to the larynx and tra-
benefit from surgery must be carefully weighed against
chea, esophageal resection may be limited to the outer
other palliative approaches, such as radiation and systemic
layers or involve composite resection if intraluminal tumor is
therapy.20
present.9 Although rare, in cases of suspected major vas-
cular invasion by tumor, CT or magnetic resonance an- RAIR-DTC
giogram is performed preoperatively. If the carotid artery is After thyroidectomy, RAI remains the most frequently used
involved, balloon occlusion testing and potential carotid adjuvant therapy for follicular-derived thyroid cancers, with
sacrifice may be considered in select cases of differentiated, the main goals to improve disease-specific survival, reduce
locally advanced cancers.9 recurrence rates, and improve progression-free survival
It is important to note that nearly one-quarter of patients with (PFS).7 However, several patients with advanced DTC are
invasive cancer die from airway obstruction secondary to radioactive-iodine resistant/refractory. According to the
tracheal invasion and 28% from respiratory failure sec- 2015 ATA guidelines, DTCs are considered refractory to RAI
ondary to lung involvement.13 Patients with locally invasive when (1) they do not concentrate RAI at the time of initial
cancer who are candidates for surgical resection and treatment, such as in patients with structurally evident
achieve gross total resection have good outcomes, with one disease and a negative RAI uptake whole-body scan,
study reporting .90% 5-year disease-free survival.14 Tu- suggesting that RAI treatment would provide no clinical
mors invading the prevertebral fascia or encasing the ca- benefit; (2) they lose their ability to concentrate RAI in the
rotid artery are classified as unresectable; however, there setting of previous RAI uptake, often occurring in patients
are instances when near total gross resection may be in- with multiple large metastases; (3) concentrate RAI in some
dicated for palliation in well-differentiated tumors with tissues but not others, evident by comparing findings from a
overall good outcome.15 In addition, palliation with tra- RAI whole-body scan with those from a 18FDG-PET scan;
cheostomy may be recommended in patients where airway or (4) there is metastatic disease progression despite
obstruction from tumor is imminent or when planned for ability to concentrate RAI.7 However, the exact definition of
nonsurgical therapy.16 Finally, as more targeted therapies RAIR-DTC is still controversial, and different definitions have
are being selectively used, some patients who would not been proposed by different societies. A recent consortium of
have been good candidates for surgery may now be con- experts from the ATA, the European Association of Nuclear
sidered for surgical treatment either for local disease control Medicine, the Society of Nuclear Medicine and Molecular
or for palliation. The nuances stemming from having re- Imaging, and the European Thyroid Association noted that
ceived neoadjuvant treatment and the implications on no current definition, classification, criterion, or clinical
surgery remain to be studied. scenario is an absolute indicator that a patient has RAIR-
2023 ASCO EDUCATIONAL BOOK | asco.org/edbook 3
Downloaded from ascopubs.org by 201.245.214.236 on August 23, 2023 from 201.245.214.236
Copyright © 2023 American Society of Clinical Oncology. All rights reserved.
Agosto Salgado et al
DTC.21 The common clinical scenarios suggesting that a with distant metastases to the lungs and/or bone are often
patient may have RAIR-DTC derived from this consortium offered local therapies before consideration of systemic
are outlined in Table 1 and provide a framework addressing treatments.28
important management issues in patients with RAIR-DTC.
Importantly, factors such as the amount of RAI uptake on SYSTEMIC THERAPY IN ADVANCED THYROID CANCER
post-therapy whole-body scans compared with the total RAI
The decision to initiate systemic therapy in thyroid cancer is
dose the patient received, tolerability of side effects, and
an area in endocrine oncology where significant clinical
tumor response to previous RAI treatments should be
practice variability exists. The specific histopathological
considered to optimize therapy in these patients.
variables play a role in the timing of antineoplastic treat-
Patients with inoperable and/or metastatic RAIR-DTC have ment. In general, the sole increase of tumor markers is not
a worse overall prognosis than those who have RAI- decisive in starting systemic therapy for thyroid cancer.
sensitive follicular-derived thyroid cancers.21-23 Before Patients with metastatic RAIR-DTC and MTC with asymp-
the routine availability of targeted therapies, studies tomatic disease and small tumors with slow indolent pro-
showed that patients with RAIR-DTC had median 5-year gression are amenable to close active surveillance with
disease-specific survival rates of 60%-70%, and those with serial imaging.29 Specifically, for RAIR-DTC and MTC, tar-
metastatic RAIR-DTC had the worse outcomes with a geted therapy is recommended for (1) rapidly progressive
median 10-year survival rate of 10%.23,24 The significance tumors not amenable or failure to alternative localized
of identifying patients who may harbor RAIR disease lies therapies, (2) symptomatic disease, or (3) tumors in a
with the need for early intervention in these patients to threatening location.7,30
improve disease-free progression and survival, with mo-
The evolving availability of different molecular testing mo-
lecular testing and mutational mapping having emerged as dalities has allowed the incorporation of precision oncology
adjuncts to imaging and pathology of identification of more
for prognostic and therapeutic purposes in advanced thy-
aggressive disease.
roid cancer and is consistent with current National Com-
Many patients with RAIR-DTC have slow-growing, low- prehensive Cancer Network guidelines.31 Given the
volume disease. For patients with asymptomatic RAIR- potential for druggable targets, the preferred somatic testing
DTC which may persist for years, low tumor burden or approach is next-generation sequencing (NGS) in contrast
minimal progression over time, watchful waiting with TSH to single-gene tests.6 All ATC tumors should undergo mo-
suppression, and periodic imaging can be used.25-27 In lecular testing. However, immunohistochemistry (IHC)
patients with locoregional recurrence, surgical intervention evaluation for BRAF V600E should also be incorporated into
is usually used as the therapeutic approach of choice, with the initial assessment of ATC while awaiting NGS results;
external-beam radiation therapy used in combination with rapid BRAF V600E IHC–positive results can lead to early
surgery in select cases.25 Typically, symptomatic patients therapeutic interventions with dabrafenib and trametinib.
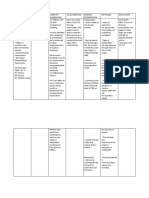
TABLE 1. Common Clinical Scenarios Suggestive of RAIR-DTC
Clinical Scenario Considerations
131
No RAI uptake on diagnostic I scan Adequate low-iodine diet and TSH stimulation before scan
High-resolution imaging with SPECT/CT scan provides more functional detail than planar imaging
No RAI uptake on a post-therapy 131I scan Post-therapy 131
I scans may miss up to 12% of DTC metastases that have RAI uptake
(performed several days after therapy)
RAI uptake is only present in some but not Can treat RAI-avid tumor tissues with 131I and use local treatment modalities for non–RAI-avid tissues
other tumor tissues
131
Progression of DTC metastases despite I Metric used for successful response to previous 131I therapy, duration of response, metric used to
uptake determine progression of disease post-131I therapy, amount of 131I activity previously administered,
potential for administering higher 131I activity, side effects, and patient preferences should be
considered when deciding to pursue additional 131I administrations
Progression of DTC metastases despite Increased likelihood of DTC becoming RAIR with increased cumulative 131I activity and number of
cumulative 131I activity of .600 mCi doses
Response to previous treatments, duration of response, individual 131I activity administered in each
previous treatment, side effects, and patient preferences should be considered when deciding to
pursue additional 131I administrations
Abbreviations: DTC, differentiated thyroid cancer; mCi, millicuries; RAI, radioactive iodine; RAIR, radioactive-iodine refractory; SPECT/CT, single-photon
emission computed tomography with computed tomography; TSH, thyroid-stimulating hormone.
4 2023 ASCO EDUCATIONAL BOOK | asco.org/edbook
Downloaded from ascopubs.org by 201.245.214.236 on August 23, 2023 from 201.245.214.236
Copyright © 2023 American Society of Clinical Oncology. All rights reserved.
Updates in Advanced Thyroid Cancer Management
For the remaining thyroid cancer variants, molecular testing classified predominantly as grade 1-2. Common noted side
should be considered in the setting of RAIR-DTC, locally effects included hand-foot skin reaction (76.3%), diarrhea
invasive or unresectable tumors, distant metastatic disease, (68.6%), alopecia (67.1%), rash (50.2%), fatigue (49.8%),
and aggressive histological features and on the basis of the weight loss (46.9%), hypertension (40.6%), anorexia (31.
clinician’s judgment.6 Available systemic targeted therapies 9%), and mucositis (23.2%), among others.32
for advanced thyroid cancers and their mechanism of action
Furthermore, lenvatinib, an MKI aiming at vascular epi-
are outlined in Table 2 and Figure 1.
thelial growth factor receptor (VEGFR), fibroblast growth
factor receptors, RET, KIT, and platelet-derived growth
DTC factor receptor α, has shown substantial responses in ad-
Initial oral antineoplastic regimens for advanced thyroid vanced thyroid cancer. In the SELECT trial, the lenvatinib-
cancers consisted of multikinase inhibitors (MKIs). The treated cohort attained a PFS of 18.3 months compared with
DECISION study, a phase III multicenter randomized, 3.6 months in the placebo group (HR, 0.21; 99% CI, 0.14 to
double-blind clinical trial, evaluated the utilization of sor- 0.31; P , .001).33 In patients pretreated with another MKI,
afenib 400 mg twice daily versus placebo. Study treatment lenvatinib, the PFS was 15.1 months. The ORR is 64.8% in
in this trial continued until radiographically documented the oral antineoplastic cohort; the majority were partial re-
disease progression, unacceptable toxicity, noncompliance sponses (63.2%) by RECIST 1.1. In addition, lenvatinib has
or withdrawal of consent. Sorafenib resulted in a meaningful demonstrated a benefit in the overall survival of patients
improvement in PFS of 10.8 versus 5.8 months in the older than 65 years. Frequently noted adverse events in-
placebo cohort (hazard ratio [HR], 0.59; 95% CI, 0.45 to 0. cluded hypertension (67.8%), diarrhea (59.4%), fatigue
76; P , .0001). The overall response rate (ORR) was 12.2% (59%), decreased appetite (50.2%), weight loss (46.4%),
versus 0.5% in favor of sorafenib.32 Adverse events oc- nausea (41%), stomatitis (35.6%), palmar-plantar eryth-
curred in most patients (98.6%) treated with this MKI, rodysesthesia syndrome (31.8%), proteinuria (31%),
TABLE 2. Summary of Systemic Targeted Therapies in Advanced Thyroid Cancer
Targeted Therapy Tumor Target Response Common Side Effects
Multikinase inhibitors-DTC
Sorafenib VEGFR, PDGFR, PFS, 10.8 months Hand-foot, diarrhea, alopecia, rash,
RET ORR, 12% fatigue, weight loss, HTN
Lenvatinib VEGFR, PDGFR, RET, PFS, 18.3 months HTN, diarrhea, fatigue, decreased
FGFR ORR, 64.8% appetite, weight loss, nausea
Multikinase inhibitors-MTC
Vandetanib RET, VEGFR, EGFR ORR, 45% Diarrhea, rash, HTN, nausea,
headache
Cabozantinib RET, VEGFR, c-MET Diarrhea, HTN, hand-foot syndrome
BRAF/MEK inhibitors
Dabrafenib and trametinib BRAF V600E DTC: dabrafenib alone ORR, 42% v dabrafenib plus Fever, fatigue, nausea, chills, skin
trametinib ORR, 48% toxicities (rash, skin cancers)
ATC: ORR, 61%
RET inhibitors
Selpercatinib RET RET fusion-TC (previously treated) ORR, 79% Dry mouth, gastrointestinal side
RET-mutant MTC (no previous treatment) ORR, 73% effects, elevated liver enzymes,
RET-mutant MTC (previously treated) ORR, 69% QT prolongation
Pralsetinib RET RET fusion-TC ORR, 85.7% Dry mouth, gastrointestinal side
RET-mutant MTC (no previous treatment) ORR, 71% effects, elevated liver enzymes,
RET-mutant MTC (previously treated) ORR, 60% QT prolongation
NTRK inhibitors
Larotrectinib NTRK NTRK fusion-TC ORR, 71% Myalgia, fatigue, elevated liver
enzymes, edema, gastrointestinal
side effects
Abbreviations: ATC, anaplastic thyroid cancer; DTC, differentiated thyroid cancer; EGFR, epidermal growth factor receptor; FGFR, fibroblast growth factor;
HTN, hypertension; MTC, medullary thyroid cancer; ORR, overall response rate; PDGFR, platelet-derived growth factor α; PFS, progression-free survival;
RET, rearranged during transfection; TC, thyroid cancer; VEGFR, vascular epithelial growth factor receptor.
2023 ASCO EDUCATIONAL BOOK | asco.org/edbook 5
Downloaded from ascopubs.org by 201.245.214.236 on August 23, 2023 from 201.245.214.236
Copyright © 2023 American Society of Clinical Oncology. All rights reserved.
Agosto Salgado et al
FIG 1. Available systemic targeted therapies for advanced thyroid cancer and mechanisms of action. ERK, extracellular-regulated kinase; FGFR, fibroblast
growth factor; mTOR, mammalian target of rapamycin; PDGFR, platelet-derived growth factor α; PI3K, phosphatidylinositol 3-kinase; RET, rearranged during
transfection; VEGFR, vascular epithelial growth factor receptor.
vomiting (28.4%), headache (27.6%), and dysphonia (24. was similar to previous discussed antiangiogenic MKIs,
1%), among others.33 including any-grade diarrhea (62%), palmar-plantar
erythrodysesthesia (47%), and hypertension (32%).34
Both sorafenib and lenvatinib are Food and Drug Admin-
Smaller studies have explored the utilization of additional
istration (FDA)–approved therapies in the United States for
MKIs in RAIR-DTC, including pazopanib, sunitinib, van-
advanced RAIR-DTC. Given the development of resistance
detanib, and axitinib.35-38
mechanisms resulting in progression, many patients with
advanced thyroid cancer require an eventual change in Although MKIs described above are used without any
treatment. Recently, cabozantinib has received FDA ap- biomarker selection, there are several inhibitors that are
proval as second-line therapy for RAIR-DTC on the basis of approved only in presence of specific gene alterations. For
COSMIC-311 study results. In this trial, which enrolled BRAF V600E–altered RAIR-DTC, the utilization of BRAF
patients after progression on anti-VEGFR therapy, cabo- and MEK inhibitors has been studied, given the success of
zantinib resulted in a PFS of 11 months over 1.9 months in these therapies in other solid tumors. Recently, a phase
placebo with an ORR of 11%.34 The best overall responses II open-label multicenter clinical study explored the
included 11% partial responses, 69% stable disease, and a implementation of BRAF inhibitor dabrafenib alone or in
confirmed complete response (1%).34 Adverse event profile combination with a MEK inhibitor.39 Using a modified
6 2023 ASCO EDUCATIONAL BOOK | asco.org/edbook
Downloaded from ascopubs.org by 201.245.214.236 on August 23, 2023 from 201.245.214.236
Copyright © 2023 American Society of Clinical Oncology. All rights reserved.
Updates in Advanced Thyroid Cancer Management
RECIST including minor responses (decreased tumor by discontinuation of targeted therapy after an additional RAI
20%-29%), partial and complete responses, the ORR- treatment, resulting in tumor control. Nevertheless, further
modified RECIST was 42% for dabrafenib monotherapy studies are warranted to identify the best responders to
versus 48% dabrafenib with trametinib (P = .67). Periodic ensure the appropriate selection of candidates and ideal
dermatological assessments are recommended as skin implementation time on the disease course.45-48
toxicities can occur, especially if treated with dabrafenib
monotherapy (65%). Pyrexia was present in both cohorts in Medullary Thyroid Carcinoma
more than 50% of patients. In addition, BRAF inhibitor Vandetanib, an MKI-targeting RET, VEGFR, and epidermal
alone was commonly associated with hyperglycemia, growth factor receptor, was, to our knowlege, the first FDA-
whereas the BRAF/MEK inhibitor had a frequency of 52% approved targeted therapy for MTC.49-51 After safety and
for fatigue, nausea, and chills.39 tolerability data from phase II trials, the phase III ZETA trial
Highly selective RET inhibitors, including selpercatinib and demonstrated improvement in the PFS compared with
pralsetinib, have been approved for metastatic RET-mutant placebo; however, this trial did not require progression at the
MTC and RET fusion–positive progressive RAIR-DTC. In time of enrollment. Cabozantinib-treated patients had an
previously treated RET fusion–positive thyroid cancer, the improvement in PFS of 11 months versus 4 months in
objective response was 79% with a PFS of 20.1 months. placebo.52
Best response distribution by RECIST 1.1 was 5% complete Both RET inhibitors, selpercatinib and pralsetinib, induced
responses, 74% partial responses, and 21% stable dis- sustained responses in RET-mutant MTC. RET-mutant MTC
ease.40 In this group of patients with thyroid cancer, who cases without previous targeted therapies treated with
were on pralsetinib, the ORR was 85.7% with a PFS of 19. selpercatinib had an objective response of 73% and 69%
4 months.41 Both antineoplastic agents had dose reduction for pretreated patients.40 Pralsetinib resulted in an ORR of
requirements in ,45% of patients, which is a reflection that 71% for RET-mutant, treatment-naı̈ve MTC versus 60% in
the majority of adverse events were minor in severity (grade the cohort previously treated by vandetanib, cabozantinib,
1-2). Common adverse events of RET inhibitors include dry or both TKIs.41 As expected with targeted therapies, the
mouth, gastrointestinal side effects, elevated transami- predominant responses were partial responses, 67% and
nases, and QT prolongation. With selpercatinib, grade 3 58% in the previously mentioned cohorts, respectively.41
events occurred in a minority of patients including hyper- Neoadjuvant RET inhibitor treatment has shown promise to
tension (12%) and high liver enzymes (17%), and in ,5% facilitate successful resection of thyroid cancers; this novel
headache, diarrhea, QT prolongation, and weight gain.40 utilization of targeted therapy is currently studied in clinical
Cytopenias are more frequently developed with pralsetinib; trials.53,54
grade 3 side effects noted (.10%) included hypertension,
neutropenia, lymphopenia, and anemia. Severe rare side Anaplastic Thyroid Carcinoma
effects may happen, including pneumonitis in a minority of ATC, as a stage IV highly lethal malignancy, benefits from
patients (4%) or hypersensitivity reactions.41,42 NTRK gene expedited comprehensive evaluation, airway assessment,
rearrangements have been reported in up to 6.7% of and molecular testing (BRAF V600E and NGS). For re-
papillary thyroid cancers; in pediatric patients, the fre- sectable tumors (stage IVA-IVB), surgical resection is
quency of NTRK fusions is higher.43 Grouped data from followed by definitive chemoradiation. Between 20% and
several phase I/II trials revealed a 71% ORR for larotrectinib, 50% of ATC tumors are driven by BRAF V600E mutation,
a NTRK inhibitor.44 Common side effects included myalgia, allowing for combination dabrafenib and trametinib
fatigue, nausea, transaminitis, edema, and gastrointestinal therapy in a neoadjuvant approach for stage IVB unre-
symptoms; nevertheless, toxicities were low grade sectable tumors or as up-front long-term therapy for stage
and ,10% dose reductions.44 IVC disease.20 Combination BRAF/MEK inhibitor in
The profound responses and toxicity profile of the gene BRAF-altered ATC has demonstrated an ORR of 61%,
alteration–specific antineoplastic agents such as the RET, including complete responses.55 Targeted therapies have
NTRK, and ALK inhibitors highlight the importance of en- improved overall survival in ATC.56 RET or NTRK inhib-
suring that patients with advanced thyroid cancer undergo itors may be used in the management of ATC tumors with
comprehensive molecular testing, including comprehensive the respective identified fusion drivers. In addition, im-
evaluation of mutations and gene rearrangements. In ad- munotherapy, particularly in combination therapies,
dition, several clinical trials and case reports demonstrate whether along BRAF/MEK inhibitor or antiangiogenics,
restoration of iodine uptake in tumors, an approach has provided further therapeutic pathways for patients
known as redifferentiation, after a course of the gene with ATC.57-59 Consideration for enrollment in ongoing
alteration–specific inhibitors targeting BRAF, MEK, RET, or clinical trials is recommended given the rarity and ag-
NTRK. The advantages include the possibility of gressiveness of this tumor.
2023 ASCO EDUCATIONAL BOOK | asco.org/edbook 7
Downloaded from ascopubs.org by 201.245.214.236 on August 23, 2023 from 201.245.214.236
Copyright © 2023 American Society of Clinical Oncology. All rights reserved.
Agosto Salgado et al
CONCLUSION cancer leading to improved PFS; however, questions
Management of advanced thyroid cancer requires a still remain in regard to optimal timing of systemic
multidisciplinary approach to optimize patient outcomes treatment initiation for advanced thyroid cancer and
and provide access to the latest cutting-edge therapies. relevant variables that inform decision making. Future
There has been significant progress in understanding the studies on redifferentiation and neoadjuvant therapy in
genetic landscape and molecular basis of thyroid cancer, the presence of bulky neck disease, immunotherapy, and
leading to the development of novel targeted therapies for development of other gene alteration–specific therapies
advanced disease. These advances have revolutionized will hopefully further advance the field leading to thyroid
the management of patients with advanced thyroid cancer cure.
AFFILIATIONS Relationships are self-held unless noted. I = Immediate Family Member,
1
Department of Head and Neck-Endocrine Oncology, H. Lee Moffitt Inst = My Institution. Relationships may not relate to the subject matter of
Cancer Center and Research Institute, Tampa, FL this manuscript. For more information about ASCO’s conflict of interest
2
Department of Otolaryngology-Head and Neck Surgery, University of policy, please refer to www.asco.org/rwc.
Miami Miller School of Medicine, Miami, FL Sarimar Agosto Salgado
3
Department of Otolaryngology and Neurosurgery, University of Miami Consulting or Advisory Role: Eisai, Blueprint Medicines, Exelixis, Lilly
Miller School of Medicine, Miami, FL Research Funding: Lilly
4
Department of Internal Medicine, Division of Metabolism, Endocrinology
and Diabetes, University of Michigan, Ann Arbor, MI Zoukaa Sargi
Stock and Other Ownership Interests: CRISPR Therapeutics, Incyte
Christine H. Chung
CORRESPONDING AUTHOR Consulting or Advisory Role: Exelixis, Merck, Brooklyn
Maria Papaleontiou, MD, Department of Internal Medicine, Division of ImmunoTherapeutics, Fulgent Pharma, Genmab
Metabolism, Endocrinology and Diabetes, University of Michigan, North Research Funding: AstraZeneca (Inst), Bristol Myers Squibb (Inst), Lilly
Campus Research Complex, 2800 Plymouth Rd, Bldg 16, Rm 453S, Ann (Inst), Merck (Inst), Regeneron (Inst), Brooklyn ImmunoTherapeutics
Arbor, Michigan 48109; e-mail: mpapaleo@med.umich.edu. (Inst), Iovance Biotherapeutics (Inst)
No other potential conflicts of interest were reported.
AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS OF
INTEREST AND DATA AVAILABILITY STATEMENT
The following represents disclosure information provided by authors of
this manuscript. All relationships are considered compensated.
REFERENCES
1. National Cancer Institute Surveillance Epidemiology and End Results Program: Cancer stat facts: Thyroid cancer. https://seer.cancer.gov/statfacts/html/thyro.
html
2. Lim H, Devesa SS, Sosa JA, et al: Trends in thyroid cancer incidence and mortality in the United States, 1974-2013. JAMA 317:1338-1348, 2017
3. Randle RW, Balentine CJ, Leverson GE, et al: Trends in the presentation, treatment, and survival of patients with medullary thyroid cancer over the past 30 years.
Surgery 161:137-146, 2017
4. Bai Y, Niu D, Yao Q, et al: Updates in the advances of sporadic medullary thyroid carcinoma: From the molecules to the clinic. Gland Surg 9:1847-1856, 2020
5. Torresan F, Cavedon E, Mian C, et al: Long-term outcome after surgery for medullary thyroid carcinoma: A single-center experience. World J Surg 42:367-375,
2018
6. Shonka DC Jr, Ho A, Chintakuntlawar AV, et al: American Head and Neck Society Endocrine Surgery Section and International Thyroid Oncology Group
consensus statement on mutational testing in thyroid cancer: Defining advanced thyroid cancer and its targeted treatment. Head Neck 44:1277-1300, 2022
7. Haugen BR, Alexander EK, Bible KC, et al: 2015 American Thyroid Association Management guidelines for adult patients with thyroid nodules and differentiated
thyroid cancer: The American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26:1-133, 2016
8. Zampella E, Klain M, Pace L, et al: PET/CT in the management of differentiated thyroid cancer. Diagn Interv Imaging 102:515-523, 2021
9. Shindo ML, Caruana SM, Kandil E, et al: Management of invasive well-differentiated thyroid cancer: An American Head and Neck Society consensus statement.
AHNS consensus statement. Head Neck 36:1379-1390, 2014
10. Pasqual E, Sosa JA, Chen Y, et al: Trends in the management of localized papillary thyroid carcinoma in the United States (2000-2018). Thyroid 32:397-410,
2022
11. Marti JL, Holm T, Randolph G: Universal use of intraoperative nerve monitoring by recently fellowship-trained thyroid surgeons is common, associated with higher
surgical volume, and impacts intraoperative decision-making. World J Surg 40:337-343, 2016
8 2023 ASCO EDUCATIONAL BOOK | asco.org/edbook
Downloaded from ascopubs.org by 201.245.214.236 on August 23, 2023 from 201.245.214.236
Copyright © 2023 American Society of Clinical Oncology. All rights reserved.
Updates in Advanced Thyroid Cancer Management
12. Schneider R, Machens A, Lorenz K, et al: Intraoperative nerve monitoring in thyroid surgery-shifting current paradigms. Gland Surg 9:S120-S128, 2020
13. Enomoto K, Inohara H: Surgical strategy of locally advanced differentiated thyroid cancer. Auris Nasus Larynx 50:23-31, 2023
14. Wang LY, Nixon IJ, Patel SG, et al: Operative management of locally advanced, differentiated thyroid cancer. Surgery 160:738-746, 2016
15. Avenia N, Vannucci J, Monacelli M, et al: Thyroid cancer invading the airway: Diagnosis and management. Int J Surg 28:S75-S78, 2016 (suppl 1)
16. Wang TS, Sosa JA: Thyroid surgery for differentiated thyroid cancer—Recent advances and future directions. Nat Rev Endocrinol 14:670-683, 2018
17. Scharpf J, Tuttle M, Wong R, et al: Comprehensive management of recurrent thyroid cancer: An American Head and Neck Society consensus statement: AHNS
consensus statement. Head Neck 38:1862-1869, 2016
18. Wells SA Jr, Asa SL, Dralle H, et al: Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid 25:567-610,
2015
19. Machens A, Dralle H: Biomarker-based risk stratification for previously untreated medullary thyroid cancer. J Clin Endocrinol Metab 95:2655-2663, 2010
20. Bible KC, Kebebew E, Brierley J, et al: 2021 American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer: American
Thyroid Association anaplastic thyroid cancer guidelines task force. Thyroid 31:337-386, 2021
21. Tuttle RM, Ahuja S, Avram AM, et al: Controversies, consensus, and collaboration in the use of (131)I therapy in differentiated thyroid cancer: A joint statement
from the American Thyroid Association, the European Association of Nuclear Medicine, the Society of Nuclear Medicine and Molecular Imaging, and the
European Thyroid Association. Thyroid 29:461-470, 2019
22. Schlumberger M, Brose M, Elisei R, et al: Definition and management of radioactive iodine-refractory differentiated thyroid cancer. Lancet Diabetes Endocrinol
2:356-358, 2014
23. Durante C, Haddy N, Baudin E, et al: Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: Benefits and
limits of radioiodine therapy. J Clin Endocrinol Metab 91:2892-2899, 2006
24. Nixon IJ, Whitcher MM, Palmer FL, et al: The impact of distant metastases at presentation on prognosis in patients with differentiated carcinoma of the thyroid
gland. Thyroid 22:884-889, 2012
25. Vaisman F, Carvalho DP, Vaisman M: A new appraisal of iodine refractory thyroid cancer. Endocr Relat Cancer 22:R301-R310, 2015
26. Vaisman F, Tala H, Grewal R, et al: In differentiated thyroid cancer, an incomplete structural response to therapy is associated with significantly worse clinical
outcomes than only an incomplete thyroglobulin response. Thyroid 21:1317-1322, 2011
27. Tam S, Amit M, Boonsripitayanon M, et al: Effect of tumor size and minimal extrathyroidal extension in patients with differentiated thyroid cancer. Thyroid
28:982-990, 2018
28. Schmidt A, Iglesias L, Klain M, et al: Radioactive iodine-refractory differentiated thyroid cancer: An uncommon but challenging situation. Arch Endocrinol Metab
61:81-89, 2017
29. Pacini F: Which patient with thyroid cancer deserves systemic therapy and when? Best Pract Res Clin Endocrinol Metab 31:291-294, 2017
30. Wells SA, Asa SL, Dralle H, et al: Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid 25:567-610,
2015
31. National Comprehensive Cancer Network: NCCN guidelines for thyroid carcinoma, 2022. www.nccn.org
32. Brose MS, Nutting CM, Jarzab B, et al: Sorafenib in radioactive iodine-refractory, locally advanced or metastatic differentiated thyroid cancer: A randomised,
double-blind, phase 3 trial. Lancet 384:319-328, 2014
33. Schlumberger M, Tahara M, Wirth LJ, et al: Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. N Engl J Med 372:621-630, 2015
34. Brose MS, Robinson BG, Sherman SI, et al: Cabozantinib for previously treated radioiodine-refractory differentiated thyroid cancer: Updated results from the
phase 3 COSMIC-311 trial. Cancer 128:4203-4212, 2022
35. Bible KC, Menefee ME, Lin CJ, et al: An international phase 2 study of pazopanib in progressive and metastatic thyroglobulin antibody negative radioactive iodine
refractory differentiated thyroid cancer. Thyroid 30:1254-1262, 2020
36. Bikas A, Kundra P, Desale S, et al: Phase 2 clinical trial of sunitinib as adjunctive treatment in patients with advanced differentiated thyroid cancer. Eur J
Endocrinol 174:373-380, 2016
37. Leboulleux S, Bastholt L, Krause T, et al: Vandetanib in locally advanced or metastatic differentiated thyroid cancer: A randomised, double-blind, phase 2 trial.
Lancet Oncol 13:897-905, 2012
38. Capdevila J, Trigo JM, Aller J, et al: Axitinib treatment in advanced RAI-resistant differentiated thyroid cancer (DTC) and refractory medullary thyroid cancer
(MTC). Eur J Endocrinol 177:309-317, 2017
39. Busaidy NL, Konda B, Wei L, et al: Dabrafenib versus dabrafenib + trametinib in BRAF-mutated radioactive iodine refractory differentiated thyroid cancer: Results
of a randomized, phase 2, open-label multicenter trial. Thyroid 32:1184-1192, 2022
40. Wirth LJ, Sherman E, Robinson B, et al: Efficacy of selpercatinib in RET-altered thyroid cancers. N Engl J Med 383:825-835, 2020
41. Subbiah V, Hu MI, Wirth LJ, et al: Pralsetinib for patients with advanced or metastatic RET-altered thyroid cancer (ARROW): A multi-cohort, open-label,
registrational, phase 1/2 study. Lancet Diabetes Endocrinol 9:491-501, 2021
42. McCoach CE, Rolfo C, Drilon A, et al: Hypersensitivity reactions to selpercatinib treatment with or without prior immune checkpoint inhibitor therapy in patients
with NSCLC in LIBRETTO-001. J Thorac Oncol 17:768-778, 2022
2023 ASCO EDUCATIONAL BOOK | asco.org/edbook 9
Downloaded from ascopubs.org by 201.245.214.236 on August 23, 2023 from 201.245.214.236
Copyright © 2023 American Society of Clinical Oncology. All rights reserved.
Agosto Salgado et al
43. Pekova B, Sykorova V, Mastnikova K, et al: NTRK fusion genes in thyroid carcinomas: Clinicopathological characteristics and their impacts on prognosis. Cancers
13:1932, 2021
44. Waguespack SG, Drilon A, Lin JJ, et al: Efficacy and safety of larotrectinib in patients with TRK fusion-positive thyroid carcinoma. Eur J Endocrinol 186:631-643,
2022
45. Hofmann M-C, Kunnimalaiyaan M, Wang JR, et al: Molecular mechanisms of resistance to kinase inhibitors and redifferentiation in thyroid cancers. Endocr Relat
Cancer 29:R173-R190, 2022
46. Lamartina L, Anizan N, Dupuy C, et al: Redifferentiation-facilitated radioiodine therapy in thyroid cancer. Endocr Relat Cancer 28:T179-T191, 2021
47. Jaber T, Waguespack SG, Cabanillas ME, et al: Targeted therapy in advanced thyroid cancer to resensitize tumors to radioactive iodine. J Clin Endocrinol Metab
103:3698-3705, 2018
48. Rothenberg SM, McFadden DG, Palmer EL, et al: Redifferentiation of iodine-refractory BRAF V600E-mutant metastatic papillary thyroid cancer with dabrafenib.
Clin Cancer Res 21:1028-1035, 2015
49. Wells SA Jr, Gosnell JE, Gagel RF, et al: Vandetanib for the treatment of patients with locally advanced or metastatic hereditary medullary thyroid cancer. J Clin
Oncol 28:767-772, 2010
50. Robinson BG, Paz-Ares L, Krebs A, et al: Vandetanib (100 mg) in patients with locally advanced or metastatic hereditary medullary thyroid cancer. J Clin
Endocrinol Metab 95:2664-2671, 2010
51. Wells SA Jr, Robinson BG, Gagel RF, et al: Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: A randomized, double-blind
phase III trial. J Clin Oncol 30:134-141, 2012
52. Elisei R, Schlumberger MJ, Müller SP, et al: Cabozantinib in progressive medullary thyroid cancer. J Clin Oncol 31:3639-3646, 2013
53. Jozaghi Y, Zafereo M, Williams MD, et al: Neoadjuvant selpercatinib for advanced medullary thyroid cancer. Head Neck 43:E7-E12, 2021
54. Contrera KJ, Gule-Monroe MK, Hu MI, et al: Neoadjuvant selective RET inhibitor for medullary thyroid cancer: A case series. Thyroid 33:129-132, 2023
55. Subbiah V, Kreitman RJ, Wainberg ZA, et al: Dabrafenib plus trametinib in patients with BRAF V600E-mutant anaplastic thyroid cancer: Updated analysis from
the phase II ROAR basket study. Ann Oncol 33:406-415, 2022
56. Maniakas A, Dadu R, Busaidy NL, et al: Evaluation of overall survival in patients with anaplastic thyroid carcinoma, 2000-2019. JAMA Oncol 6:1397-1404, 2020
57. Cabanillas ME, Dadu R, Ferrarotto R, et al: Atezolizumab combinations with targeted therapy for anaplastic thyroid carcinoma (ATC). J Clin Oncol 38, 2020
(suppl 15; abstr 6514)
58. Capdevila J, Wirth LJ, Ernst T, et al: PD-1 blockade in anaplastic thyroid carcinoma. J Clin Oncol 38:2620-2627, 2020
59. Dierks C, Seufert J, Aumann K, et al: Combination of lenvatinib and pembrolizumab is an effective treatment option for anaplastic and poorly differentiated thyroid
carcinoma. Thyroid 31:1076-1085, 2021
10 2023 ASCO EDUCATIONAL BOOK | asco.org/edbook
Downloaded from ascopubs.org by 201.245.214.236 on August 23, 2023 from 201.245.214.236
Copyright © 2023 American Society of Clinical Oncology. All rights reserved.
You might also like
- Thyroid Cancer: Burden of Illness and Management of Disease: J o U R N A L o F C A N C e RDocument7 pagesThyroid Cancer: Burden of Illness and Management of Disease: J o U R N A L o F C A N C e RRum Afida RasfaNo ratings yet
- Management of Thyroid NeoplasmsDocument38 pagesManagement of Thyroid NeoplasmsPuy PatcharamaiNo ratings yet
- Jurnal OnkologiDocument9 pagesJurnal OnkologiIrham HasbiNo ratings yet
- Male Breast Cancer: An Institutional ExperienceDocument5 pagesMale Breast Cancer: An Institutional ExperienceIJAR JOURNALNo ratings yet
- 10 3322@caac 21559Document25 pages10 3322@caac 21559DIANA ALEXANDRA RAMIREZ MONTAÑONo ratings yet
- Cancer TiroidesDocument13 pagesCancer TiroidesAlmendra PalmNo ratings yet
- 1 s2.0 S014067362300020X MainDocument14 pages1 s2.0 S014067362300020X MainGERIATRIA 72No ratings yet
- Biomarkers For The Diagnosis of Cholangiocarcinoma A Systematic Review 2018Document10 pagesBiomarkers For The Diagnosis of Cholangiocarcinoma A Systematic Review 2018Anna MariaNo ratings yet
- Medullary Thyroid Cancer in The Era of Tyrosine Kinase Inhibitors: To Treat or Not To Treat-And With Which Drug-Those Are The QuestionsDocument7 pagesMedullary Thyroid Cancer in The Era of Tyrosine Kinase Inhibitors: To Treat or Not To Treat-And With Which Drug-Those Are The QuestionsIulia JulyNo ratings yet
- Aace/Aaes Medical/Surgical Guidelines For Clinical Practice: Management of Thyroid CarcinomaDocument19 pagesAace/Aaes Medical/Surgical Guidelines For Clinical Practice: Management of Thyroid CarcinomaMariappan ArumugamNo ratings yet
- Annals of Medicine and SurgeryDocument5 pagesAnnals of Medicine and SurgeryUsee TvNo ratings yet
- Mic Coli 2017Document6 pagesMic Coli 2017Orlando CervantesNo ratings yet
- Head Neck - 2023 - Weaver - A Molecular Guide To Systemic Therapy in Salivary Gland CarcinomaDocument12 pagesHead Neck - 2023 - Weaver - A Molecular Guide To Systemic Therapy in Salivary Gland CarcinomaafissaNo ratings yet
- 10 1016@j Jfma 2018 01 015Document10 pages10 1016@j Jfma 2018 01 015darpa22No ratings yet
- New Treatment Options For Metastatic Thyroid CancerDocument6 pagesNew Treatment Options For Metastatic Thyroid CancermarcelinaNo ratings yet
- MainDocument8 pagesMainIoana CucuNo ratings yet
- Pathology 3 1045Document9 pagesPathology 3 1045Mada Dwi HariNo ratings yet
- Thyroid CancerDocument13 pagesThyroid CancerAccounting CV BakerNo ratings yet
- The Role of Radiotherapy in Ovarian Cancer: ReviewDocument6 pagesThe Role of Radiotherapy in Ovarian Cancer: ReviewMaria MuñozNo ratings yet
- Apicella 2015Document16 pagesApicella 2015bawoji1763No ratings yet
- Seminar: Maria E Cabanillas, David G Mcfadden, Cosimo DuranteDocument13 pagesSeminar: Maria E Cabanillas, David G Mcfadden, Cosimo DurantePedro Gómez RNo ratings yet
- Papillary Thyroid Carcinoma Hobnail Variant A Report of Two Cases 5816 PDFDocument5 pagesPapillary Thyroid Carcinoma Hobnail Variant A Report of Two Cases 5816 PDFriswani tangibaliNo ratings yet
- Pet Scan en Ca de TiroidesDocument9 pagesPet Scan en Ca de TiroidesdrmolinammNo ratings yet
- NEJM Iod RadioactivDocument10 pagesNEJM Iod RadioactivLaura ZaifuNo ratings yet
- Breast CancerhggDocument20 pagesBreast CancerhggCatherine RajanNo ratings yet
- Thyroid Cancer: Burden of Illness and Management of Disease: J o U R N A L o F C A N C e RDocument7 pagesThyroid Cancer: Burden of Illness and Management of Disease: J o U R N A L o F C A N C e REndang Rahayu Fuji LestaryNo ratings yet
- 559 ArticleDocument9 pages559 ArticleRye CalderonNo ratings yet
- No Longer Well Differentiated Diagnostic Criteria and Clin 2023 Surgical PaDocument12 pagesNo Longer Well Differentiated Diagnostic Criteria and Clin 2023 Surgical ParubenmacaNo ratings yet
- Nejmoa 2111953Document10 pagesNejmoa 2111953Andreea VlădanNo ratings yet
- Hepatocellular Carcinoma: Clinical Frontiers and PerspectivesDocument13 pagesHepatocellular Carcinoma: Clinical Frontiers and PerspectivesMisnariahIdrusNo ratings yet
- W de WenisimoDocument18 pagesW de WenisimoBJ CarminatorNo ratings yet
- Anaplastic Thyroid Cancer BrochureDocument3 pagesAnaplastic Thyroid Cancer Brochurey8cp6nqvn2No ratings yet
- The Role of Ablative Radiotherapy in Older Adults With Limited Metastatic DiseaseDocument7 pagesThe Role of Ablative Radiotherapy in Older Adults With Limited Metastatic DiseaseRaul Matute MartinNo ratings yet
- Fonc 07 00177Document13 pagesFonc 07 00177Ihenanacho HappinessNo ratings yet
- Rebel Lo 2021Document27 pagesRebel Lo 2021cydolusNo ratings yet
- PG Art 34580-10Document15 pagesPG Art 34580-10Horia MineaNo ratings yet
- Thyroid Carcinoma: Phenotypic Features, Underlying Biology and Potential Relevance For Targeting TherapyDocument25 pagesThyroid Carcinoma: Phenotypic Features, Underlying Biology and Potential Relevance For Targeting TherapyrakaNo ratings yet
- Radioterapia Tumor PhyllodesDocument5 pagesRadioterapia Tumor Phyllodesmanuel barrientosNo ratings yet
- Nihms 938445Document30 pagesNihms 938445Berry BancinNo ratings yet
- Thyroid Cancer Metabolism A Review 2167 7948 1000200Document7 pagesThyroid Cancer Metabolism A Review 2167 7948 1000200yukii celloNo ratings yet
- Ca Tiroid 2 PDFDocument11 pagesCa Tiroid 2 PDFAlfindyNo ratings yet
- Cancer de Cervix 2019pdfDocument6 pagesCancer de Cervix 2019pdfCristian RodríguezNo ratings yet
- Prostate cancerPRIMERDocument27 pagesProstate cancerPRIMERLuan MarcosNo ratings yet
- Prostate Cancer Therapy - What You Must KnowFrom EverandProstate Cancer Therapy - What You Must KnowRating: 4 out of 5 stars4/5 (1)
- 2017 Article 52-2Document9 pages2017 Article 52-2Lorena RamosNo ratings yet
- Radioterapia en CacUDocument6 pagesRadioterapia en CacUVicente RamosNo ratings yet
- EJGO2022054 Cervical CaDocument8 pagesEJGO2022054 Cervical CaRahmayantiYuliaNo ratings yet
- Current Controversies in The Initial Post-Surgical Radioactive Iodine Therapy For Thyroid Cancer: A Narrative ReviewDocument12 pagesCurrent Controversies in The Initial Post-Surgical Radioactive Iodine Therapy For Thyroid Cancer: A Narrative ReviewAura GorneaNo ratings yet
- Critical Reviews in Oncology / HematologyDocument14 pagesCritical Reviews in Oncology / HematologyMIGUEL MORENONo ratings yet
- Breast Disease: Diagnosis and Pathology, Volume 1From EverandBreast Disease: Diagnosis and Pathology, Volume 1Adnan AydinerNo ratings yet
- Organo TropismDocument12 pagesOrgano TropismKL TongsonNo ratings yet
- Testis CancerDocument9 pagesTestis CancerMuhammad Tawfiq ZamriNo ratings yet
- Jurnal Kanker TestisDocument9 pagesJurnal Kanker TestisDiatni FibriNo ratings yet
- 624 PDFDocument9 pages624 PDFTri AryantiNo ratings yet
- Efficacy of Trans-Arterial Radio Embolization With Yattrium-90 For Hepatic MalignanciesDocument8 pagesEfficacy of Trans-Arterial Radio Embolization With Yattrium-90 For Hepatic MalignanciesIJAR JOURNALNo ratings yet
- 10 1016@j Jaccao 2020 04 007Document10 pages10 1016@j Jaccao 2020 04 007ramangNo ratings yet
- Prasad 2017Document9 pagesPrasad 2017Dhruv MahajanNo ratings yet
- Treating Local Advanced HN Cancer When Cisplatin Is Not OptionDocument7 pagesTreating Local Advanced HN Cancer When Cisplatin Is Not OptionbrenomendespNo ratings yet
- Jgo 18 00214Document19 pagesJgo 18 00214Robert ChristevenNo ratings yet
- 2022 The Intensive Care Management of Acute Ischaemic StrokeDocument9 pages2022 The Intensive Care Management of Acute Ischaemic StrokeOmar Alejandro Agudelo ZuluagaNo ratings yet
- Jco.2022.40.17 Suppl - Lba6003Document1 pageJco.2022.40.17 Suppl - Lba6003Paulo Roberto Zanfolim GarciaNo ratings yet
- Dupuytren's ContractureDocument40 pagesDupuytren's ContractureGafencu SergiuNo ratings yet
- Nursing DiagnosisDocument2 pagesNursing DiagnosisUriel CrispinoNo ratings yet
- Half Yearly, English, Class XDocument3 pagesHalf Yearly, English, Class XChiku PatilNo ratings yet
- CD Exams 2020 ComtriDocument16 pagesCD Exams 2020 ComtriArlly Faena AbadNo ratings yet
- P4 - Primary and Secondary Survey in EmergencyDocument22 pagesP4 - Primary and Secondary Survey in Emergencylia agustinaNo ratings yet
- EETS Vs MTS Meta AnalysisDocument13 pagesEETS Vs MTS Meta AnalysisMary Christina ElsaNo ratings yet
- LUTSDocument9 pagesLUTSHatem SadekNo ratings yet
- My Incomplete Project EVALUATION OF SYMPTOMSDocument16 pagesMy Incomplete Project EVALUATION OF SYMPTOMSIram KhanNo ratings yet
- Swallowing Disorders 2022Document29 pagesSwallowing Disorders 2022Mohammed AhmedNo ratings yet
- CorrosivesDocument25 pagesCorrosivesahmed.farag.ali2020No ratings yet
- Referral Form NavanDocument2 pagesReferral Form Navankayleighquinn89No ratings yet
- DM and GlucoseDocument1 pageDM and GlucoseibunaraNo ratings yet
- Evolve Resources For Goulds Pathophysiology For The Health Professions 6th Edition Hubert Test BankDocument9 pagesEvolve Resources For Goulds Pathophysiology For The Health Professions 6th Edition Hubert Test Bankhungden8pne100% (26)
- Diabetes and ExerciseDocument12 pagesDiabetes and ExercisePranav SNo ratings yet
- 10 ĐỀ THI KSCL LẦN 2 NĂM HỌC 2021Document4 pages10 ĐỀ THI KSCL LẦN 2 NĂM HỌC 2021Sơn Cao ThanhNo ratings yet
- Combinepdf 2Document96 pagesCombinepdf 2Dexter John CarpioNo ratings yet
- Jama Oka 2023 CG 230017 1701464130.47792Document2 pagesJama Oka 2023 CG 230017 1701464130.47792Aadityarajsinh GohilNo ratings yet
- 2021.2 - Obs-Gynae - Clinical-TaskDocument59 pages2021.2 - Obs-Gynae - Clinical-TaskLucas Victor AlmeidaNo ratings yet
- Mechanisms, Mitigation, and Management of Urinary Toxicity From Prostate RadiotherapyDocument10 pagesMechanisms, Mitigation, and Management of Urinary Toxicity From Prostate RadiotherapyZuriNo ratings yet
- Blog Post About National Poultry Day 2023Document63 pagesBlog Post About National Poultry Day 2023ZETTYNo ratings yet
- Algoritma Kanker KolorektalDocument8 pagesAlgoritma Kanker KolorektalHasan NyambeNo ratings yet
- Revision Part 1Document4 pagesRevision Part 1lobna adelNo ratings yet
- Mcmi III Essentials InterpretationDocument56 pagesMcmi III Essentials InterpretationZeine Daoudi100% (6)
- Shooting Script-2Document3 pagesShooting Script-2api-690980823No ratings yet
- CBCR Joint Pain Student VersionDocument4 pagesCBCR Joint Pain Student VersionNika GianashviliNo ratings yet
- What Causes You To Lose Your CoolDocument1 pageWhat Causes You To Lose Your CoolMary Angelie AmbojiaNo ratings yet
- Test Bank For Goulds Pathophysiology For The Health Professions 6th Edition by HubertDocument6 pagesTest Bank For Goulds Pathophysiology For The Health Professions 6th Edition by HubertFranklin Roberts100% (38)
- NCP 3rd YearDocument6 pagesNCP 3rd YearTotoro AblogNo ratings yet