Professional Documents
Culture Documents
Procedure For Production of Cryoprecipitate: Table 15-2 Blood Component Characteristics
Uploaded by
sam mohOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Procedure For Production of Cryoprecipitate: Table 15-2 Blood Component Characteristics
Uploaded by
sam mohCopyright:
Available Formats
Chapter 15 Component Preparation 343
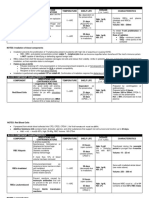
BOX 15–3
Procedure for Production of Cryoprecipitate
1. The venipuncture must be nontraumatic. 6. Express the supernatant plasma into the attached satellite bag. The
2. The whole blood can be cooled before and during production be- cryoprecipitate will be a small white mass in the original plasma
cause platelets are not usually produced along with cryoprecipitate. bag. Leave only 10 to 20 mL of plasma on the precipitate.
The volume of plasma required to remain on the RBCs and the 7. If preparing prestorage pooled cryoprecipitate, identify compatible
platelet concentrate would reduce the amount of plasma available components for pooling and combine at this time.
for cryoprecipitate production enough to significantly reduce the 8. Refreeze the cryoprecipitate immediately. Time elapsed should be
final AHF activity in the precipitate. At least 200 mL of plasma no more than 1 hour at room temperature. A delay in refreezing or
(205 g) should be used to ensure that the final product will contain exposure of the unit to elevated temperatures during processing
at least 80 AHF units. will significantly decrease the factor VIII activity level in the final
3. The plasma must be stored at –18°C or below within 8 hours of product. The centrifuge temperature must be at 1° to 6°C, and it is
collection and within 1 hour from the time freezing was initiated. better if the centrifuge cups are well chilled.
4. The second stage of cryoprecipitate preparation begins by allowing 9. The final product should be placed in a protective container be-
the frozen plasma to thaw slowly in the refrigerator at 1° to 6°C . cause of the brittle nature of the plastic bag at freezer tempera-
This takes 14 to 16 hours when plasma is thawed in a standard tures. Store at –18°C or colder up to 12 months from the date of
blood bank refrigerator. If a circulating cryoprecipitate thaw bath whole blood collection.
(4°C water bath) is used, the thawing time is reduced to about 10. If the supernatant plasma is refrozen at –18°C, it must be labeled
2 to 4 hours. The endpoint is when the plasma becomes slushy. as “plasma cryoprecipitate reduced.”
5. Centrifuge the plasma at 1° to 6°C for a hard spin.
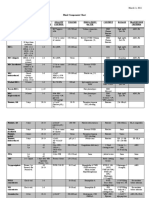
Table 15–2 Blood Component Characteristics
Storage
Component Shelf Life Temp. Quality Control Volume Dosage
Whole blood (WB) CPD 21 d 1°–6°C N/A 450–500 mL hgb 1 g/dL
CPDA-1 35 d hct 3%
CP2D 21 d
Whole blood irradiated Original expiration or 1°–6°C 25 Gy to center of canister 450–500 mL hgb 1 g/dL
28 d post-irradiation
hct 3%
RBCs CPD 21 d 1°–6°C No additive: hct 80% 250–300 mL hgb 1 g/dL
CPDA-1 35 d hct 3%
CP2D 21 d Additive: N/A
ACD 21 d
AS 42 d
RBC aliquots Closed system: same 1°–6°C varies 10 mL/kg
Open system: 24 hr hgb 2 g/dL
RBC irradiated Original outdate or 1°–6°C 25 Gy to center of canister 250–300 mL hgb 1 g/dL
28 d post-irradiation
hct 3%
RBC leukoreduced Closed system: same 1°–6°C <5 106 WBCs 85% RBC 250–300 mL hgb 1 g/dL
recovery
Open system: 24 hr hct 3%
Washed RBCs 24 hr 1°–6°C hct 70–80% 180 mL hgb 1 g/dL
hct 3%
Frozen RBCs 10 years –65°C
RBC deglycerolized 24 hr 1°–6°C 80% RBC recovery 180 mL hgb 1 g/dL
<1% glycerol hct 3%
Platelets, whole-blood 5–7 d 20°–24°C 5.5 1010 plts 50–70 mL 5k–10k/ L
derived (RD)
pH 6.2
Continued
344 PART III Transfusion Practices
Table 15–2 Blood Component Characteristics—cont’d
Storage
Component Shelf Life Temp. Quality Control Volume Dosage
Platelets, apheresis (SD) 5–7 d 20°–24°C 3 1011 plts 200–400 mL 30k–60k/ L
pH 6.2
Platelets, irradiated 5d 20°–24°C 25 Gy to center of canister Same Same
Platelets, pooled 4 hr 20°–24°C pH 6.2 Varies Varies
Platelets, leukoreduced 5d 20°–24°C pH 6.2 RD: 40–70 mL RD: 5–10k/ L
RD: <8.3 105 WBCs SD: 200–400 mL SD: 30–60k/ L
SD: <5 106 WBCs
FFP 1 yr –18°C 200–380 mL Factor 20%–30%
7 yr –65°C 200–1,000 mL 10–20 mL/kg
AFFP 1 yr –18°C
PF24 1 yr –18°C 200–380 mL Same
7 yr –65°C
LP 5 days after WB 1–6°C 200–380 mL Not well
expires liquid characterized
Cryoprecipitate Frozen: 1 yr –18°C FVIII: 80 IU 10–25 mL Fibrinogen
Fibrinogen: 150 mg 5–10 mg/dL
Thawed: 6 hr 20°–24°C
Pooled (open): 4 hours
Cryo-reduced plasma 1 yr 18°C 200–380 mL
Granulocytes 24 hr 20°–24°C 1.0 1010 200–600 mL 1–2 1010/infusion
four daily doses
Granulocytes, irradiated 24 hr 20°–24°C 1.0 1010 200–600 mL Same
hgb = hemoglobin; hct = hematocrit; plts = platelets; WB = whole blood; SD = single donor; RD = random donor
system and subsequently proliferate and mount an immune device is sent through an irradiation cycle, and the minimum
response against the patient’s tissues. In immunocompro- and maximum radiation dose is determined. For irradiation
mised patients, donor T lymphocytes escape destruction devices using a radioactive source, the amount of exposure
because the patient’s immune system lacks the resources nec- time required to achieve the minimum radiation exposure
essary to detect and destroy the foreign cells. When a patient increases as the radioactive source decays.
receives blood from a relative or an HLA-matched donor, the Each facility should have a protocol and procedure for
donor cells may be haploidentical to the patient cells and irradiating blood components, training of personnel using
therefore not express antigens that would trigger the patient’s the irradiator, and issuing of irradiated components. The
immune system to recognize the donor cells as foreign. Irra- expiration date of irradiated RBCs is 28 days from the time
diation damages the nucleic acid of the donor T lymphocytes of irradiation or the original outdate, whichever is sooner.
and therefore makes them unable to proliferate and cause The expiration date of platelets and granulocytes are not
disease. impacted by irradiation.
Both the FDA and AABB recommend a minimum dose of
gamma irradiation of 25 Gy to the central portion of the Washing
blood unit, with no less than 15 Gy delivered to any part
of the blood unit.28 Irradiation may be achieved by using Red blood cells prepared using the methods previously
either a radioactive source (cesium-137 or cobalt-60) or described in this chapter are stored for up to 42 days
x-ray. To confirm a product was irradiated, a radiochromic suspended in a solution that contains additive solution (in-
film label is affixed to the component before it is placed into cluding saline, amino acids, and sugars) in addition to a
the metal canister of the irradiator. Darkening of the film small volume of residual plasma and anticoagulant that is
confirms irradiation requirements. Irradiation devices also not removed during manufacturing. Platelets are also
require semiannual or annual dose delivery verification using stored in a mixture of donor plasma and anticoagulant
an outside source. To determine dose delivery, a detection solution, with or without additive. The process of removing
You might also like
- Blood Components ChartDocument3 pagesBlood Components ChartCreativeCovers J.No ratings yet
- Blood Components (E-Learning Activity) : Francisco, Frances Lorraine RDocument3 pagesBlood Components (E-Learning Activity) : Francisco, Frances Lorraine RFrances FranciscoNo ratings yet
- Blood Components (E-Learning Activity) : Francisco, Frances Lorraine RDocument3 pagesBlood Components (E-Learning Activity) : Francisco, Frances Lorraine RpixiedustNo ratings yet
- Blood ComponentsDocument4 pagesBlood ComponentsGerald John PazNo ratings yet
- Blood Components Chart: Shelf-Life, Storage, IndicationsDocument3 pagesBlood Components Chart: Shelf-Life, Storage, IndicationsDanica Gel FernandezNo ratings yet
- Blood ComponentsDocument4 pagesBlood ComponentsRay Angelo RobidilloNo ratings yet
- Reference: Harmening, D. M. (2012) - Modern Blood Banking & Transfusion Practices (6th Ed.) - Pp. 434Document5 pagesReference: Harmening, D. M. (2012) - Modern Blood Banking & Transfusion Practices (6th Ed.) - Pp. 434Kolin N Jandoc100% (1)
- Blood ComponentDocument40 pagesBlood ComponentMostafa Ragab Mohammad100% (1)
- 4 Blood ComponentsDocument40 pages4 Blood ComponentsAhmad Ali shahNo ratings yet
- Harmening Chapter Summary and Questions CompilationDocument63 pagesHarmening Chapter Summary and Questions CompilationShaira Rae BillenaNo ratings yet
- Blood ComponentsDocument51 pagesBlood ComponentsMandy A. Delfin100% (1)
- Blood Transfusion and Conservation During SurgeryDocument86 pagesBlood Transfusion and Conservation During SurgeryajefolakemijohnNo ratings yet
- L1 - BB LecDocument11 pagesL1 - BB LecJUDEA WILCH ORJENo ratings yet
- Blood Banking Components Preparation GuideDocument5 pagesBlood Banking Components Preparation GuideBONNA FAYE CHRISZEL HUI YING TANNo ratings yet
- Blood Banking ProceduresDocument5 pagesBlood Banking ProceduresTalon General Hospital Laboratory DepartmentNo ratings yet
- Blood and Blood ProductsDocument24 pagesBlood and Blood Productscnecardio100% (3)
- Unit 2 Blood and Blood ComponentsDocument35 pagesUnit 2 Blood and Blood ComponentsPravin AmbadeNo ratings yet
- Blood Components-Practical: Written By: Presented To DateDocument5 pagesBlood Components-Practical: Written By: Presented To Datefayzah alshammariNo ratings yet
- BB Hand Out MidtermDocument21 pagesBB Hand Out MidtermFatimaMendozaNo ratings yet
- Unit 2 Blood and Blood Components: Terry Kotrla, MS, MT (ASCP) BBDocument35 pagesUnit 2 Blood and Blood Components: Terry Kotrla, MS, MT (ASCP) BBAllan MacacapagalNo ratings yet
- Blood Component TherapyDocument82 pagesBlood Component TherapyVivek GuptaNo ratings yet
- RBC Procedures123Document6 pagesRBC Procedures123Naomi NicoleNo ratings yet
- Blood ComponentDocument60 pagesBlood ComponentAvi DhakalNo ratings yet
- University of Santo Tomas Immunohematology and Transfusion MedicineDocument7 pagesUniversity of Santo Tomas Immunohematology and Transfusion MedicineWynlor Abarca100% (1)
- Blood Components GuideDocument67 pagesBlood Components GuideAhamed Minver100% (1)
- Blood Bank SectionDocument6 pagesBlood Bank SectionSamanthaCadaDevillaNo ratings yet
- Blood Transfusion ScienceDocument23 pagesBlood Transfusion Sciencedorsa koraeiNo ratings yet
- Blood Banking Chapter 1Document9 pagesBlood Banking Chapter 1throwawyNo ratings yet
- Summary Carts and MCqs 1Document29 pagesSummary Carts and MCqs 1Sarah YousufNo ratings yet
- Summary Chart: Fundamental ConceptsDocument16 pagesSummary Chart: Fundamental ConceptsFiona Marie Kyla TunayNo ratings yet
- Blood ComponentsDocument101 pagesBlood ComponentsNyxa AbdullaNo ratings yet
- Creatinine PAP FS Test for Kidney FunctionDocument2 pagesCreatinine PAP FS Test for Kidney FunctionAPRILLA DENTINo ratings yet
- (BB) Component ProcessingDocument7 pages(BB) Component ProcessingIya BangalanNo ratings yet
- بنك دم مراجعةDocument68 pagesبنك دم مراجعةYaRa HamarshehNo ratings yet
- Harmening QuestionsDocument19 pagesHarmening QuestionsJeremiah Gatchalian100% (1)
- CSC Dos TestDocument5 pagesCSC Dos TestAnand GaridipuriNo ratings yet
- Clincal Patho SummaryDocument29 pagesClincal Patho Summaryahmed abd elazizNo ratings yet
- Manual CBC 1 3: - Wbcs - Platelets Count - PCV or HCT - Retics Count - HB Estimation 3 3 4 5 6Document25 pagesManual CBC 1 3: - Wbcs - Platelets Count - PCV or HCT - Retics Count - HB Estimation 3 3 4 5 6Aqila MumtazNo ratings yet
- Cardigan 2011Document5 pagesCardigan 2011MaulidaNo ratings yet
- Who Should Receive Blood ComponentsDocument6 pagesWho Should Receive Blood ComponentsMaxine AraralNo ratings yet
- Blood ComponentDocument4 pagesBlood ComponentVictor GonzalesNo ratings yet
- Colles, ChristineDocument6 pagesColles, ChristineChristine CollesNo ratings yet
- Blood ComponentsDocument24 pagesBlood ComponentsNukematsu MawiNo ratings yet
- Ward Report Highlights Severe CasesDocument9 pagesWard Report Highlights Severe CasesrezaNo ratings yet
- Local Media5289763584533511516Document8 pagesLocal Media5289763584533511516Haniya KhanNo ratings yet
- Ward Report Thursday, February 23 2017Document3 pagesWard Report Thursday, February 23 2017rezaNo ratings yet
- Laporan Jaga Bangsal 3-5-2017Document9 pagesLaporan Jaga Bangsal 3-5-2017rezaNo ratings yet
- B-Blood Banking History 2-4-21: RequiredDocument5 pagesB-Blood Banking History 2-4-21: RequiredFlorenz AninoNo ratings yet
- ZINCDocument1 pageZINCZinar sawinZinarNo ratings yet
- LTD 2013Document476 pagesLTD 2013Gracia MayaNo ratings yet
- UltracompetentesDocument8 pagesUltracompetentesHerta FrankelNo ratings yet
- Shanz - Clinpath Le 2Document3 pagesShanz - Clinpath Le 2Petrina XuNo ratings yet
- bloodcomponentsanditsuses-150109110156-conversion-gate02Document53 pagesbloodcomponentsanditsuses-150109110156-conversion-gate02shravyasavitha9No ratings yet
- Fluitest CK MB: Order Information: SpecimenDocument4 pagesFluitest CK MB: Order Information: SpecimenShina AuliaNo ratings yet
- 1 - Blood - Component - Separation - Doc Filename UTF-8''1 Blood Component SeparationDocument5 pages1 - Blood - Component - Separation - Doc Filename UTF-8''1 Blood Component SeparationLeoNo ratings yet
- Enzymatic Creatinine - Dimension - Rev H DXDCM 09008b838086ee77-1517966132155Document16 pagesEnzymatic Creatinine - Dimension - Rev H DXDCM 09008b838086ee77-1517966132155Rizka Diana PutriNo ratings yet
- DUTY SDH + CKDDocument6 pagesDUTY SDH + CKDadelia putri wirandaniNo ratings yet
- Glucose Uptake Colorimetric Assay Kit: For Research Use Only!Document2 pagesGlucose Uptake Colorimetric Assay Kit: For Research Use Only!HariniNo ratings yet
- Blood Bank 3Document20 pagesBlood Bank 3moonfire2009100% (2)
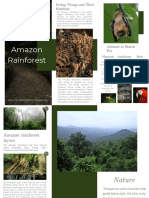
- Life in the Amazon RainforestDocument2 pagesLife in the Amazon RainforestRaquel Gomes SantosNo ratings yet
- 0610 Summer 11 Question Paper 11Document16 pages0610 Summer 11 Question Paper 11Choudhry WalidNo ratings yet
- 1Document2 pages1indrajitrohjNo ratings yet
- King Alfred: England's Scholarly Warrior KingDocument39 pagesKing Alfred: England's Scholarly Warrior KingChong Beng LimNo ratings yet
- Harvest Moon - Friend's of Mineral TownDocument63 pagesHarvest Moon - Friend's of Mineral TownNate Mercer100% (1)
- Kami Export - The Call of The Wild PDFDocument10 pagesKami Export - The Call of The Wild PDFursjinalNo ratings yet
- Hamlet Reinaissance Ideas, The World and Death PDFDocument2 pagesHamlet Reinaissance Ideas, The World and Death PDFCarlos Rodríguez RuedaNo ratings yet
- Supervert - Perversity Think TankDocument64 pagesSupervert - Perversity Think TankMatias MoulinNo ratings yet
- Grade 7 English 1st QuarterDocument6 pagesGrade 7 English 1st QuarterAlexandra NalapoNo ratings yet
- The Mesozoic Era Age of DinosaursDocument196 pagesThe Mesozoic Era Age of DinosaursSANDRA BALLESTEROSNo ratings yet
- Pap SmearDocument10 pagesPap SmearEunice Jade Claravall ArgonzaNo ratings yet
- 2 Functions of ZoosDocument3 pages2 Functions of ZoosAlicia AugustNo ratings yet
- Does RH Negative Blood Type Equal Alien HeritageDocument16 pagesDoes RH Negative Blood Type Equal Alien Heritageddj.tech26889% (9)
- Call of Cthulhu - The Arkham Gazette #3 (7E Conversion)Document20 pagesCall of Cthulhu - The Arkham Gazette #3 (7E Conversion)tommy fletcher100% (2)
- ZootopiaDocument6 pagesZootopiaapi-305795027No ratings yet
- Summary Homework BookletDocument18 pagesSummary Homework Bookletapi-320022467No ratings yet
- Synopsis of Orthodontic TreatmentDocument173 pagesSynopsis of Orthodontic TreatmentAnonymous u1XwdxXNo ratings yet
- Hewes Primate Communication and The Gestural Origin of LanguageDocument20 pagesHewes Primate Communication and The Gestural Origin of LanguageHernán Robledo NakagawaNo ratings yet
- LDC Model Questions Part 4Document13 pagesLDC Model Questions Part 4AdwaithNo ratings yet
- Figures of SpeechDocument52 pagesFigures of SpeechJaja CalabaoNo ratings yet
- Urinary Incontinence From Harrison's IMDocument2 pagesUrinary Incontinence From Harrison's IMnashey08No ratings yet
- Vocabulary A5Document149 pagesVocabulary A5Milton MollojaNo ratings yet
- Chap 18 Body Fluids and Circulation Mind Map Class 11 PDF - WatermarkDocument3 pagesChap 18 Body Fluids and Circulation Mind Map Class 11 PDF - Watermarkmominameen7No ratings yet
- The Olive Tree: Appetizers SaladsDocument5 pagesThe Olive Tree: Appetizers SaladsTkeyahNo ratings yet
- Symbaroum - The Art of SymbaroumDocument56 pagesSymbaroum - The Art of SymbaroumThibault Mlt Ericson100% (2)
- Fiitjee: Admission TestDocument7 pagesFiitjee: Admission TestAshwin SinghNo ratings yet
- FAR - Biological AssetsDocument1 pageFAR - Biological AssetsJun JunNo ratings yet
- What A Wagging Dog Tail Really Means - New Scientific Data - Psychology TodayDocument13 pagesWhat A Wagging Dog Tail Really Means - New Scientific Data - Psychology TodayAlanGonzalezNo ratings yet
- Fairmont Felted Bowls: ComplimentaryDocument2 pagesFairmont Felted Bowls: ComplimentaryKateByeeNo ratings yet