Professional Documents
Culture Documents
Masuk Thesis
Uploaded by
Jay SharmaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Masuk Thesis
Uploaded by
Jay SharmaCopyright:
Available Formats
Meibomian gland Dropout and lipid layer thickness in keratoconus population
western UP in India
By
Mr. Masuk Kuraisi
Enrollment no:18168140
Under the guidance of
Ms. Anjali Gautam(M. Optom)
Submitted in partial fulfillment for the degree of
Bachelor of Optometry (B. Optometry)
Submitted to
Department of Optometry
C L Gupta Eye Institute, Moradabad
Date: August 08, 2023 1
DECLARATION
I hereby declare that the contents in this the dissertation titled (Meibomian gland Dropout and
lipid layer thickness in keratoconus population western UP in India) is the outcome of study
conducted by me. I further affirm that it’s entirely my effort and not been copied. The
project/dissertation has been conducted with the purpose of submission in partial fulfillment of
the certificate for Internship in Clinical Optometry, in C L Gupta Eye Institute, Moradabad, UP.
The above-mentioned information is authentic to the best of my understanding.
The project/dissertation was undertaken and carried out by me, under the guidance of Ms. Anjali
Gautam
Name: Masuk Kuraisi Under supervision: Dr. Sanjay Chanda
Enrollment No: 18168140 Mentor name: Anjali Gautam
Signature: Signature:
Date: Date:
Date: August 08, 2023 2
CERTIFICATE
This is to certify that the work which is presented in the project/dissertation titled (Meibomian
gland Dropout and lipid layer thickness in keratoconus population western UP in India) in
partial fulfillment of the certificate for Internship in Clinical Optometry, and submitted to the
Department of Optometry, C.L.Gupta Eye Institute, Moradabad, U.P, is an authentic record of
(Masuk Kuraisi), a final year student of Bachelor of Optometry, (C.L. Gupta Eye
Institute),Moradabad, carried out during the period from 08/08/2022 to 08/08/2023 under the
supervision of Department of Optometry, C L Gupta Eye Institute, Moradabad, U.P.
Mr. Samir Sutar,
HOD, Optometry Education & Services
C L Gupta Eye Institute
Moradabad, U.P, India
Date: August 08, 2023 3
CONSENT FOR RESEARCH
I have read this information brochure carefully/this form has been read to me. I understand the
consequences involved in participation in this research study that are explained to me. I have had
an opportunity to ask questions and I am satisfied with the answers I have been given. I
mother/father/guardian of (Mr. Mansur Kuraisi and Mrs. Aalma begam and also thanks to my
family members as well as my Bach met) hereby voluntarily consent to participate my (son) in the
study on (Meibomian gland dropout in keratoconus) as described in the information brochure. My
child may undergo the series of visual tests and also would participate in the follow-up visit to
ensure the benefit of the spectacle prescribed for daily activities. I wish to be contacted if the
findings are made that have implications for the child or my family.
In making my candidate participate I understand that:
The data will remain confidential and will not be released within legal limits
There will be no cost, nor financial benefit to my candidate for participating I this study.
If the data leads to development of a commercial project in future we will not receive
payment for this
I may at any time withdraw my candidature from participating in this study. This will not
affect future medical treatment
I may be approached again to participate in future studies but i am under no compulsion
to do so
My signature below acknowledges voluntary participation of my candidate in this study,
but in no way releases the staff from their professional and ethical responsibility to me
Name:
Signature
Date: August 08, 2023 4
ACKNOWLEDGEMENT
I accept responsibility and would want to express my gratitude to Ms. Anjali Gautam, (M.
Optom) Optometrist, C.L. Gupta Eye Institute, for providing me with the wonderful opportunity
to work on such a fascinating project. I'd want to thank her for her continual encouragement and
support.
I'd like to express my heartfelt thanks and debt to my parents and family members.
I am appreciative for the help I received from the biostatistician who assisted me in analyzing the
data.
Finally, I want to thank the hospital administration for assisting me in gathering data for the
project analysis.
Thank you
Date: August 08, 2023 5
Contents
ABSTRACT ........................................................................................................................................... 7
CHAPTER: 01 ....................................................................................................................................... 8
Introduction ........................................................................................................................................... 8
Chapter: 02 ............................................................................................................................................ 9
Literature Review .................................................................................................................................. 9
CHAPTER: 03 ..................................................................................................................................... 13
METHODOLOGY .............................................................................................................................. 13
CHAPTER: 04 ..................................................................................................................................... 15
DATA ANALYSIS .............................................................................................................................. 15
CHAPTER: 05 ..................................................................................................................................... 16
RESULT .............................................................................................................................................. 16
CHAPTER: 06 ..................................................................................................................................... 17
DISCUSSION ...................................................................................................................................... 17
CHAPTER: 07 ..................................................................................................................................... 19
CONCLUSION.................................................................................................................................... 19
REFERENCES .................................................................................................................................... 20
Date: August 08, 2023 6
ABSTRACT
Title: Meibomian gland Dropout and lipid layer thickness in keratoconus population in
western UP in India
Purpose: To evaluate the Meibomian Gland dropout in keratoconus patient.
Methods: In this prospective case–control study, patients were conducted from the Department of
Ophthalmology of C.L. Gupta eye Institute Moradabad between September 2022 and March 2023.
The study was approved by Institutional Review Board (IRB Number: CLGEI-IEC/22-223/34).
Fifty keratoconus eyes were investigated in this study. The control participants were randomly
selected from patients attending the outpatient clinic, optometry student and staff who had no signs
or symptoms of dry eye or other ocular inflammation.
Result: In this study, Meibomian glands of 50 eyes were studied. In this included 50 eyes from
people with keratoconus and 50 from healthy people. The mean age was 21.04± 6.16 and
22.60±1.24 years of case group and control group respectively. The Mean BCVA and K Max and
Thin cornea was 21.04±6.16 and 54.98±8.89 and 470.98±53.64 respectively.
Conclusion: Meibomian gland dropout is found in the Keratoconus patient recorded by Lipiview.
Patients with KC should be screened for Meibomian gland drop out because of its possible clinical
implications.
Date: August 08, 2023 7
CHAPTER: 01
Introduction
Meibomian glands are located in the tarsal plate and are sebaceous glands that secrete meibum,
which reduces the evaporation of the tear film and enhances its stability and spreading (1). Previous
studies have reported an association of KC with DED (2). Meibomian gland dysfunction (MGD)
is considered the main cause of dry eye disease, leading to evaporative dry eye. The lipid layer in
the tear film is derived mainly from the meibomian glands which are of utmost importance for
preserving the ocular surface (3). Meibomian glands (MG) are sebaceous glands more in upper
eye lids. keratoconus (KC) patients suffer greater symptoms of dry eye and greater tear instability.
The harm to a gland's structure and number can both be caused by the cornea in keratoconus
patient. Keratoconus (KC) is a chronic bilateral disease characterized by asymmetric progressive
thinning most commonly located in the inferior temporal and central corneal regions. Its
prevalence in the different studies ranges from 0.17 to 47.9 per 1000 people [6].and its yearly
incidence ranges from 1.3 to 25.0 per 100,000 persons [6]; however, the actual number may be
higher because there are likely many subclinical instances that go untreated. The majority of the
time, it begins at adolescence and develops over time to stabilize in the third or fourth decades of
life. In the mild to moderate stages of the disease, vision correction in this condition is frequently
accomplished with glasses or contact lenses, but severe KC may necessitate surgery.
DED and MGD are more prevalent in keratoconus patients [3,4,5], and the upper eyelid that covers
the cornea's middle sixth. Therefore, it is clinically vital to understand their effect on these glands
since it might lead to the meibomian gland drop out if it is constantly rubbed against the upper
tarsus plate by the protrusion of the cornea.
The hypothesis is that as in keratoconus patients, the corneal cone directly interacts with both the
eyelids and the tear film; this interaction may have effects on meibomian gland loss and Lipid
layer thickness.
Date: August 08, 2023 8
Chapter: 02
Literature Review
Literature review 1
Mohamed Mostafa et al. Published 2 June 2019 Ophthalmology Department, Faculty of Medicine,
Sohag University, Sohag, to examine the morphological changes in the meibomian glands of
patients with keratoconus as well as to study the relationship between these changes in the
morphology and several tear film parameters. Methods. Examination of the meibomian gland
(MG) of 300 keratoconus patients presenting to the center using infrared noncontact meibography
system (Sirius, CSO, Italy) between January 2017—January 2019. 100 eyes of healthy individuals
were also enrolled as a control group. Tear breakup time (TBUT) test and Schirmer test II were
evaluated. Subjective symptoms were also assessed using Ocular Surface Disease Index (OSDI).
Results. Mean age of keratoconus patients was 19 ± 12 years and 21 ± 14 years in control group.
Average TBUT was 4.9 ± 2.1 sec. and average Schirmer test was 5.3 ± 2.2 mm which was
significantly lower than control group (p = 0.05). Meibomian gland dropout in the lower eyelid of
the keratoconus group was as follows: grade 0 (no loss of meibomian glands): 100 eyes; grade 1
(gland dropout area <1/3 of the total meibomian glands): 85 eyes; grade 2 (gland dropout area 1/3
to 2/3): 68 eyes; and grade 3 (gland dropout >2/3): 47 eyes. Conclusion. Keratoconus shows
significant meibomian gland dropout and distortion that can be recorded by noncontact
meibography. Sirius meibography is a simple, cost-effective method of evaluating meibomian
gland dropout as a part of the routine refractive examination.
Date: August 08, 2023 9
Literature review 2
Erez., et.al July, 2021 to investigate the association of keratoconus (KC) with meibomian gland
dysfunction (MGD) and to describe the epidemiological characteristics of MGD in this disease.
Methods: In this observational study, 120 KC patients seen in the Department of Ophthalmology
of the Complex Hospitalario Universitario de Santiago de Compostela and 87 controls were
analyzed. The Ocular surface disease index (OSDI) questionnaire was administered and several
DED tests and an evaluation of the meibomian glands and lid margin were performed. MGD signs
and DED tests were compared between the groups. Symptoms were further analyzed in patients
and controls with and without MGD. Results: KC was significantly associated with MGD after
adjusting for age and sex [adjusted odds ratio (ORa), 2.40]. The frequency of MGD in KC patients
[59 (49.2%) KC patients and 25 (28.7%) controls had MGD] correlated with the severity of KC (r
= 0.206) (P = 0.020). Mean OSDI score in KC patients with and without MGD was 31.1 ± 24.1
and 35.2 ± 26.0 (P = 0.326), and 17.2 ± 22.7 and 13.3 ± 14.1 in controls with and without it (P =
0.366). The most common MGD signs coincided in both groups. Staining with fluorescein (P =
0.000) and lissamine green (P = 0.019) was higher in KC patients, but no differences were detected
with TBUT (P = 0.116) or the Schirmer test (P = 0.637). Hypersecretory MGD was the most
prevalent variant in both groups. Conclusions: MGD and DED are common in KC patients. MGD
correlates with the severity of KC and is indistinguishable from MGD in patients without KC. No
association was found with symptoms. Patients with KC should be screened for MGD because of
its possible clinical implications. Further research is needed to clarify the role of MGD in
keratoconus patient
Date: August 08, 2023 10
Literature review 3
Zhou., et.al Sept, 2022. Title Decrease in Tear Film Lipid Layer Thickness in Patients with
Keratoconus. Keratoconus (KC) is a progressive corneal disorder characterized by thinning and
protrusion, mostly of the inferotemporal and central corneal regions. Dysfunction of the
meibomian gland, the excretions of which form the lipid layer of the tear film, has been reported
to be associated with KC. Thus, this manuscript investigates the correlation among lipid layer
thickness (LLT), partial blink rate (PBR), and KC of different degrees. This retrospective study
included 54 patients and 24 healthy controls. The anterior corneal curvature, LLT, and PBR were
taken from the unilateral eye of all 78 participants. The difference in those ocular parameters
between the moderate and severe groups and the control group is significant. No significant
association was found between anterior corneal curvature and LLT (r = −0.2, p = 0.15) across all
the patients. However, there was a significant negative correlation between anterior corneal
curvature and LLT in moderate (r = −0.6, p < 0.05) and severe (r = −0.7, p < 0.05) keratoconus
cases. The results also show a significant negative correlation between anterior corneal curvature
and PBR (r = −0.41, p < 0.05). Therefore, we conclude that the severity of keratoconus is
associated with the thinning of LLT and the reduction of PBR. This may relate to a further
epithelial abnormality with the reduced protection of tear film from the air, leading to the release
of proteolytic enzymes that degrade stromal collagen and weaken the cornea
Date: August 08, 2023 11
Literature review 4
Ömür Ö. Uçakhan et.al First published online May 18, 2023 Purpose To evaluate morphological
and functional state of the meibomian glands (MG) in keratoconus patients. One hundred eyes of
100 keratoconus patients and 100 eyes of 100 age-matched control subjects were included into this
study. Ocular Surface Disease Index (OSDI) scores, non-invasive break up time (NIBUT), findings
of meibography, staining with fluorescein of the ocular surface, tear film break-up time (TBUT),
and Schirmer I test were documented in all patients’ eyes and control eyes and were compared
between the groups. Results The mean TBUT and NIBUT were significantly lower, corneal
staining and OSDI scores were statistically greater in the keratoconus group (p < 0.05). The mean
meiboscore, partial gland, gland dropout and gland thickening scores for upper/lower eyelids were
significantly greater in keratoconus patients than controls (p < 0.05). The NIBUT measurements
significantly correlated with MG loss in upper/lower eyelids (p < 0.05). The severity of
keratoconus seemed to correlate with meiboscore, partial gland, gland thickening scores in
upper/lower eyelids. Conclusion Our data suggests that corneal ectasia in keratoconus is related
with alterations in ocular surface, tear film function and MG morphology. Early screening and
treatment of MG dysfunction may improve ocular surface quality and allow better disease
management in keratoconus patients.
Research gap
As per knowledge, Very Few studies focus of meibomian gland loss in Keratoconus patient. None
of study determine the severity of Meibomian gland loss in correlation with keratoconus severity.
So new addition study is carried out to find out. Also, Different technologies were used in previous
study for meibography such as Infrared Meibography, Confocal Meibography, Optical Coherence
Meibography so for comparison we used LipiView II® Ocular Surface Interferometer
Meibography.
Date: August 08, 2023 12
CHAPTER: 03
METHODOLOGY
In this prospective case–control study, patients were conducted from the Department of
Ophthalmology of C.L. Gupta eye Institute Moradabad between September 2022 and March 2023.
The study was approved by Institutional Review Board (IRB Number: CLGEI-IEC/22-223/34).
Fifty keratoconus eyes were investigated in this study. The control participants were randomly
selected from patients attending the outpatient clinic, optometry student and staff who had no signs
or symptoms of dry eye or other ocular inflammation.
In this study, patients with keratoconus and ages under 30 were included.
Exclusion criteria included any other ophthalmic disorder especially blepharitis, acute ocular
disorder, undergone previous eye surgery, current corneal erosion, or chronic use of eye drops for
at least 3 months prior to examination, contact lens wearers, eyes with keratoconus grade 4, and
chronic systemic disease. The diagnosis of keratoconus was based on classic corneal
biomicroscopic and topographic findings in accordance with the criteria of Rabinowitz and
McDonnell [8]. Neither the control nor the KC patients reported wearing contact lenses. All
assessments were performed by the same Clinical optometrist.
Measurements
Non-contact infrared meibography of the upper and lower eyelid was examine by the JOHNSON
& JOHNSON VISION LIPIVIEW II SYSTEM by the experienced clinical optometrist.
LipiView II (Tear Science, Inc., Morrisville, NC), an interferometer that was introduced in 2011,
was used to noninvasively quantify the signs of MGD. LipiView II® Ocular Surface
Interferometer was applied to evaluate the tear film LLT and to monitor blinking patterns by
capturing 20 s videos. The LLT results were converted from interferometric color units into
nanometers and the numbers of incomplete blinks and total blinks were calculated.
Minibiographies were produced in the same lab under consistent lighting circumstances. The
number of UL and LL glands present was counted, and the area of gland loss was measured in
Date: August 08, 2023 13
percentage. The partial blink rates (PBR), the LLT, and the proportion of MG dropouts were
recorded
Date: August 08, 2023 14
CHAPTER: 04
DATA ANALYSIS
Statistical analysis was performed using SPSS software (Statistical Package for Social Sciences
[IBM SPSS Statistics for Windows, version 25.0. Armonk, NY: IBM Corp]). Normality of the
data distribution was tested using the Kolmogorov–Smirnov test (P < 0.05). Demographic
characteristics were summarized using descriptive statistics (frequencies, percentage, mean, and
standard deviation). Levene’s Test for Equality of Variances and t-test for Equality of Means was
used to determine age and the examination (K max, thin cornea, Bad score, Partial blink rate, Total
Blink rate, LLT, MD drop out) differences among Keratoconus patients and control subjects. P
value of 0.05 or less was considered statistically significant.
Date: August 08, 2023 15
CHAPTER: 05
RESULT
In this study, Meibomian glands of 50 eyes were studied. In this included 50 eyes from people
with keratoconus and 50 from healthy people. The mean age was 21.04± 6.16 and 22.60±1.24
years of case group and control group respectively. The Mean BCVA and K Max and Thin cornea
was 21.04±6.16 and 54.98±8.89 and 470.98±53.64 respectively.
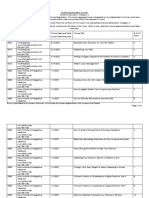
Table 1 shows the difference between the KC and Control group of clinical tests. KC group and
the control group were age and sex matched statistical difference. The percentage of gland loss of
Upper and lower eye lids statistically significant differences between both groups with the lower
values belonging to the KC group. No significant difference in partial blink rate, total blink rate,
LLT was obtained between control and keratoconus group. In comparison to the control group, the
keratoconus group had a much higher rate of MG dropouts. The value is clinically significant.
Mean ± SD Control group KC group P value
(n=50 eyes ) (n=50 eyes )
Partial blink rate 3.04±2.87 3.72±4.78 0.391
Total blink rate 4.48±3.25 5.30±5.45 0.364
Lipid layer thickness (nm) 67.78±16.02 72.56±22.45 0.224
No. MGs present (UL) 29.32±2.73 24.52±4.40 <0.001
No. MGs present (LL) 23.38±2.57 23.96±2.89 0.292
MG drop out ( %) (UL) 2.98±6.08 12.40±17.15 <0.001
MG drop out ( %) (LL) 0.6±3.59 10.9±16.40 <0.001
Date: August 08, 2023 16
CHAPTER: 06
DISCUSSION
Our results of meibography imaging by lipiview showed significant difference between the
keratoconus group and the control group. Keratoconus groups shows higher meibomian gland
dropout in upper eyelids when compared to the control group. And as expected. Different
technologies were used for meibography [9] such as infrared meibography, [10], confocal
meibography [11] and optical coherence meibography [12].
Ömür Ö. Uçakhan et.al (2023) found that corneal ectasia in keratoconus is related with alterations
in ocular surface, tear film function and MG morphology.
Mohamed et. Al (2019) suggest that the Keratoconus shows significant meibomian gland dropout
and distortion that can be recorded by noncontact meibography.
We are aware that this study focuses on the anatomic details of the MG rather the function of the
meibum. In general, meibography provides a feasible method of recording and documenting the
MGs for better diagnosis of its dysfunction in various diseases and its severity. It should be taken
into account that meibography should be used in context of clinical findings and symptoms.
Lipiview meibography is a simple, noncontact, cost-effective method of evaluating meibomian
gland dropout as a part of the routine eye examination.
Accessible screening of MGs dropout in KC patients allows for better management and decrease
the patient symptoms. Effective management of keratoconus disease makes it possible to decrease
patient ocular discomfort and save the MG till the older age and thus reduce the mechanical stress
on the already vulnerable corneas.
Thus, treatment of underlying cause such as dry eye, MGs Drop out, and blepharitis might be
important to prevent keratoconus progression little bit and guarantee symptom relief. Eye rubbing
Date: August 08, 2023 17
could contribute to the worsening of MGs pathology and its partly by transferring pathogens to the
eyelids. In view of this, patients should be instructed about eyelid hygiene in addition to refraining
from eye rubbing.
Patients with keratoconus often present with anterior protrusion of eye cornea that leads
mechanical trauma to the meibomian glans.
Therefore, detection of meibomian gland deficiency in patients with keratoconus is mandatory
Patients with keratoconus often require multiple surgical and non-surgical interventions.
Clinicians must raise awareness among patients that improvement of the eye surface and decreased
rubbing are important treatment goals
The appropriate treatment would reduce burning sensation, irritation, tearing, photophobia, blurred
vision, and red eyes related to dry eye and ocular surface inflammation, thereby decreasing eye
rubbing. Effective management of MG drop out disease might decrease eye rubbing. This study
demonstrates significant alterations in the ocular surface parameters like MGs drop out in upper
and lower lids in a patient with keratoconus. In further studies, evaluation of an older group of KC
patients would help elucidate the progress of the MG dysfunction. We hope that these findings
inspire future studies about the associations of such relevant ocular conditions, which profoundly
impact patient quality of life and vision.
Limitation
This study has less sample size.
Date: August 08, 2023 18
CHAPTER: 07
CONCLUSION
Meibomian gland dropout is found in the Keratoconus patient recorded by Lipiview.
Patients with KC should be screened for Meibomian gland drop out because of its possible clinical
implications.
Date: August 08, 2023 19
REFERENCES
1. Arita R, Fukuoka S, Morishige N. New insights into the morphology and function of
meibomian glands. Exp Eye Res 2017; 163:64–71. https://doi.org/10.1016/j.
exer.2017.06.010.
2. Carracedo G, Recchioni A, Alejandre-Alba N, Martin-Gil A, Crooke A, Morote I-A, et
al. Signs and symptoms of dry eye in keratoconus patients: A pilot study. Curr Eye Res
2015;40(11):1088–94. https://doi.org/10.3109/02713683.2014.987871.
3. R. Arita, K. Itoh, K. Inoue, and S. Amano, “Noncontact infrared meibography to
document age-related changes of the meibomian glands in a normal population,”
Ophthalmology, vol. 115, no. 5, pp. 911–915, 2008.
4. Mohamed Mostafa E, Abdellah MM, Elhawary AM, Mounir A, Madrid-Costa D.
Noncontact Meibography in Patients with Keratoconus. J Ophthalmol 2019;2019.
https://doi.org/10.1155/2019/2965872.
5. Mostovoy D, Vinker S, Mimouni M, Goldich Y, Levartovsky S, Kaiserman I. The
association of keratoconus with blepharitis. Clin Exp Optom 2018;101(3):339–44.
https://doi.org/10.1111/cxo.12643.
6. Hwang S, Lim DH, Chung TY. Prevalence and Incidence of Keratoconus in South Korea:
A Nationwide Population-based Study. Am J Ophthalmol. 2018 Aug;192:56-64. doi:
10.1016/j.ajo.2018.04.027. Epub 2018 May 8. PMID: 29750946.
7. Kim JS, et al. Assessment of the tear film lipid layer thickness after cataract surgery.
Semin Ophthalmol. 2018;33:231–6. 15. Qiu W, et al. Evaluation of the
Date: August 08, 2023 20
You might also like
- Ready To PassDocument218 pagesReady To PassvalsaNo ratings yet
- Aqar Report 2018-19 Saurashtra UniversityDocument33 pagesAqar Report 2018-19 Saurashtra UniversityAcross BordersNo ratings yet
- Text Book Vision SceinciesDocument316 pagesText Book Vision SceinciesCarpetali GatitaNo ratings yet
- AntibioticsDocument7 pagesAntibioticsCeleste Largo Arayan-LedesmaNo ratings yet
- NP4 Recalls7Document11 pagesNP4 Recalls7AhrisJeannine EscuadroNo ratings yet
- Trail Making Test: Regression-Based Norms For The Portuguese PopulationDocument10 pagesTrail Making Test: Regression-Based Norms For The Portuguese PopulationPotenciar teNo ratings yet
- Cmocfinal PDFDocument128 pagesCmocfinal PDFDiwakar RaoNo ratings yet
- Dissertation Report MBADocument21 pagesDissertation Report MBAVivek Vishal Giri0% (1)
- Drug Study: Medication Indication Contraindicati0N Side Effects Use Caution inDocument17 pagesDrug Study: Medication Indication Contraindicati0N Side Effects Use Caution inAngely Dianne Santiago II100% (2)
- Oet R - SarsDocument16 pagesOet R - SarsVic Kwan100% (1)
- Rishiraj Final Thesis For SubmissionDocument32 pagesRishiraj Final Thesis For SubmissionJay SharmaNo ratings yet
- Kudakwashe Research Project Proposal 19 MayDocument14 pagesKudakwashe Research Project Proposal 19 MayKudakwashe MagogoNo ratings yet
- ENTrain Workshop Brochure-3Document8 pagesENTrain Workshop Brochure-3tapan khanNo ratings yet
- Textbook of Visual Science and Clinical OptometryDocument19 pagesTextbook of Visual Science and Clinical OptometryPeter MubiNo ratings yet
- Vis-Con 2024-1Document15 pagesVis-Con 2024-1Deepthi Chandra Shekar SuraNo ratings yet
- KNOWLEDGE AND ALTITUDE ON THE USE OF INTRAUTERINE COPPER DEVICE IUD AMONG WOMEN ATTENDING MCHFP CLINIC IN EMBU LEVEL 5 HOSPITAL Maureen CompleteDocument37 pagesKNOWLEDGE AND ALTITUDE ON THE USE OF INTRAUTERINE COPPER DEVICE IUD AMONG WOMEN ATTENDING MCHFP CLINIC IN EMBU LEVEL 5 HOSPITAL Maureen CompleteTWIN SISTERSNo ratings yet
- Demographic and Clinical Pattern of Uveitis in Tertiary Eye Care Institute of Central IndiaDocument7 pagesDemographic and Clinical Pattern of Uveitis in Tertiary Eye Care Institute of Central Indiajassi nishadNo ratings yet
- 012 PDFDocument7 pages012 PDFjassi nishadNo ratings yet
- Knowledge and Attitude of Dentists Towards Cone Beam Computed Tomography in Mangalore - A Questionnaire SurveyDocument6 pagesKnowledge and Attitude of Dentists Towards Cone Beam Computed Tomography in Mangalore - A Questionnaire SurveyAswin krishnamoorthyNo ratings yet
- Prakash 07 PDFDocument43 pagesPrakash 07 PDFPrakashNo ratings yet
- Corneal OpacityDocument43 pagesCorneal Opacityendalew mulugetaNo ratings yet
- 1 ProposalDocument37 pages1 ProposalMelakeselam GedamuNo ratings yet
- TFOS DEWS II Management Ther PDFDocument55 pagesTFOS DEWS II Management Ther PDFHenry LaksmanaNo ratings yet
- Letter YGA 2024 (Oral Free Com.) - Dr. Cindy Kesty (Indonesia) DevelopingDocument2 pagesLetter YGA 2024 (Oral Free Com.) - Dr. Cindy Kesty (Indonesia) DevelopingannisanadyapNo ratings yet
- KeralaJOphthalmol323252-5519404 151954Document6 pagesKeralaJOphthalmol323252-5519404 151954nitaNo ratings yet
- Ophthalmology: Journal of and Advance ResearchDocument14 pagesOphthalmology: Journal of and Advance ResearchAthenaeum Scientific PublishersNo ratings yet
- Zaamin Amul SIP ReportDocument38 pagesZaamin Amul SIP ReportPallav KumarNo ratings yet
- PROJECT (Rittik Shee, Mha 1st)Document22 pagesPROJECT (Rittik Shee, Mha 1st)R SheeNo ratings yet
- Yoga ResumeDocument4 pagesYoga ResumeYoga SriNo ratings yet
- Ziba ThesisDocument57 pagesZiba ThesisJANANI MNo ratings yet
- Swathi Viswanath (Resume)Document1 pageSwathi Viswanath (Resume)PLUG - INNo ratings yet
- Tugas Bedah EkstirpatioDocument36 pagesTugas Bedah EkstirpatioAnonymous WAeeFpNNo ratings yet
- Joyce Research, 2023 FINAL EDITINGDocument39 pagesJoyce Research, 2023 FINAL EDITINGGodwin AgbenorlawoeduagahNo ratings yet
- JSciSoc493339-2898536 080305Document9 pagesJSciSoc493339-2898536 080305garciadeluisaNo ratings yet
- FACE RECOGNITION (RESEARCH PAPER) 1 Wala Pa NahumanDocument34 pagesFACE RECOGNITION (RESEARCH PAPER) 1 Wala Pa NahumanHana Loren BalberanNo ratings yet
- Cahit Gurel MS Thesis Development of A Face Recognition SystemDocument82 pagesCahit Gurel MS Thesis Development of A Face Recognition SystemSıla KOÇERNo ratings yet
- Sonali WordDocument19 pagesSonali Wordsarjak shahNo ratings yet
- Development of Novel Analytical Methods For Detection and DetermiDocument184 pagesDevelopment of Novel Analytical Methods For Detection and DetermiCole VincentNo ratings yet
- ShahinaDocument31 pagesShahinaShahina ShaikhNo ratings yet
- Development and Validation ofDocument129 pagesDevelopment and Validation ofEman Abd ELbadieNo ratings yet
- SIP REPORT Akashay (AutoRecovered)Document67 pagesSIP REPORT Akashay (AutoRecovered)Akashay JainNo ratings yet
- Sample Statement of Purpose (SOP) For MS in BiotechnologyDocument2 pagesSample Statement of Purpose (SOP) For MS in BiotechnologyAxcNo ratings yet
- Phacoemulsification Versus Small Incision Cataract Surgery For Treatment ofDocument7 pagesPhacoemulsification Versus Small Incision Cataract Surgery For Treatment ofRagni MishraNo ratings yet
- Summer Internship Project KunalDocument62 pagesSummer Internship Project KunalimsakshibajajNo ratings yet
- RAGHU Final ProjectDocument50 pagesRAGHU Final ProjectPrakashNo ratings yet
- 1 - Bio-Data of DR - Vijayan Gurumurthy Iyer 26.07.2022Document180 pages1 - Bio-Data of DR - Vijayan Gurumurthy Iyer 26.07.2022Dr Vijayan Gurumurthy IyerNo ratings yet
- Final MDT SeifeDocument49 pagesFinal MDT Seifeseife slassieNo ratings yet
- PHD Thesis Submission Guidelines UgcDocument5 pagesPHD Thesis Submission Guidelines UgcBrooke Heidt100% (2)
- 220301118libin Sam BabyDocument117 pages220301118libin Sam BabySHRIKANT DODNo ratings yet
- A Simple Technique To Measure The Volume of Removed Buccal FatDocument3 pagesA Simple Technique To Measure The Volume of Removed Buccal FatGuilherme GuerraNo ratings yet
- Cherry EyeDocument6 pagesCherry EyeREGINE YEO ZHI SHUENNo ratings yet
- Ethical Committee ApprovalDocument2 pagesEthical Committee Approvalganeshkumar jayakrishnanNo ratings yet
- 2203003smitham PDFDocument79 pages2203003smitham PDFchavali deepthiNo ratings yet
- Literatur Desi Angraini 2Document93 pagesLiteratur Desi Angraini 2Sandika AmrizalNo ratings yet
- Poster Presentation FlyerDocument2 pagesPoster Presentation FlyerVescop 18-21No ratings yet
- Accredited Biomechanical Taping™ Practitioner - Part A - Dynamic TapeDocument1 pageAccredited Biomechanical Taping™ Practitioner - Part A - Dynamic Tapekifa82No ratings yet
- Summer Internship Report PM-22-18Document51 pagesSummer Internship Report PM-22-18Adnan TajirNo ratings yet
- 1 COH Bidar SSR 6 5 CollegeDocument127 pages1 COH Bidar SSR 6 5 CollegeBhuvana SundariNo ratings yet
- Imba 18 17Document102 pagesImba 18 17Bhat UmarNo ratings yet
- GDV - BIOWELL Workshop - Hummingbird Edited 01082014 PDFDocument4 pagesGDV - BIOWELL Workshop - Hummingbird Edited 01082014 PDFgururajkgvwfNo ratings yet
- Please Note: All Distance Education Courses Are At-Will and May Be Taken at Any Time, Within A Year, After The Course Approval Date or Last DateDocument4 pagesPlease Note: All Distance Education Courses Are At-Will and May Be Taken at Any Time, Within A Year, After The Course Approval Date or Last Dateel mamouniNo ratings yet
- Penang Physicians Congress FlyerDocument14 pagesPenang Physicians Congress FlyerSomuNo ratings yet
- Dissertation UMI Ken (Autosaved) 11 EditedDocument118 pagesDissertation UMI Ken (Autosaved) 11 Editedkitderoger_391648570No ratings yet
- Management of Vitreous Floaters An International Survey The European VitreoRetinal Society Floaters Study ReportDocument10 pagesManagement of Vitreous Floaters An International Survey The European VitreoRetinal Society Floaters Study Reportmistic0No ratings yet
- Partial Extraction Therapy in Implant DentistryFrom EverandPartial Extraction Therapy in Implant DentistryUdatta KherNo ratings yet
- Suraendra 156.3Document13 pagesSuraendra 156.3Jay SharmaNo ratings yet
- T Ekrk NH T Ekrk NH: Jk/ks&jk/ksDocument2 pagesT Ekrk NH T Ekrk NH: Jk/ks&jk/ksJay SharmaNo ratings yet
- FormDocument1 pageFormJay SharmaNo ratings yet
- SectionDocument18 pagesSectionJay SharmaNo ratings yet
- 2Document57 pages2Jay SharmaNo ratings yet
- For ManagerDocument1 pageFor ManagerJay SharmaNo ratings yet
- Self-Certification FormDocument3 pagesSelf-Certification FormHRM ServicesNo ratings yet
- CardiologíaDocument3 pagesCardiologíajakpowerNo ratings yet
- Modul Bahasa InggrisDocument30 pagesModul Bahasa InggrisVienska ValeriandraNo ratings yet
- Health Policy Balochistan WHO 2018-30Document34 pagesHealth Policy Balochistan WHO 2018-30Aitzal AhmedNo ratings yet
- Toliongco vs. CADocument17 pagesToliongco vs. CAAnonymous KaNu0py71No ratings yet
- Chapter 3.1. Spontaneous Generation: Learning ObjectivesDocument6 pagesChapter 3.1. Spontaneous Generation: Learning ObjectivesMerylle Dane AlbaNo ratings yet
- CMV Infection As A Possible Cause of Chronic Diarrhea in Patient With Autosomal Recessive Hyper Ige Syndrome Case ReportDocument2 pagesCMV Infection As A Possible Cause of Chronic Diarrhea in Patient With Autosomal Recessive Hyper Ige Syndrome Case ReportBIOMEDSCIDIRECT PUBLICATIONSNo ratings yet
- Basic, High-Risk, and Critical Care Intrapartum Nursing: Clinical Competencies and Education Guide, 6th EditionDocument22 pagesBasic, High-Risk, and Critical Care Intrapartum Nursing: Clinical Competencies and Education Guide, 6th EditionAji SadamNo ratings yet
- The Economic Burden of Cardiovascular Disease and Hypertension in Low-And Middle-Income Countries: A Systematic ReviewDocument11 pagesThe Economic Burden of Cardiovascular Disease and Hypertension in Low-And Middle-Income Countries: A Systematic ReviewJordán MaulénNo ratings yet
- Case StudiesDocument5 pagesCase Studiespragna novaNo ratings yet
- Smoking As A Risk Factor For Dry Socket ComplicationDocument15 pagesSmoking As A Risk Factor For Dry Socket ComplicationI Gusti Ayu WulanNo ratings yet
- Hazard Report Form SampleDocument2 pagesHazard Report Form Samplewelly1980okNo ratings yet
- 10 Tips To Prevent Spreading Impetigo, and Avoid Getting It AgainDocument2 pages10 Tips To Prevent Spreading Impetigo, and Avoid Getting It Againputri aisheNo ratings yet
- IMMUNOTECH™ - A Immunomodulator in Poultry by ABTL EnzymesDocument4 pagesIMMUNOTECH™ - A Immunomodulator in Poultry by ABTL EnzymesabtlenzymesNo ratings yet
- XI Rancangan Soal PtsDocument8 pagesXI Rancangan Soal PtsHanida Dwi Astuti SuwarnoNo ratings yet
- Contemporary WorldDocument9 pagesContemporary WorldBranden Mark Salvio BlanzaNo ratings yet
- Stretch Mark PowerpointDocument14 pagesStretch Mark Powerpointdhaval88No ratings yet
- 91637-Meninges Brain and Spain - Majda ThurnherDocument14 pages91637-Meninges Brain and Spain - Majda ThurnherFaith ManiquisNo ratings yet
- Hubungan Durasi Penggunaan Alat Elektronik Dengan Tension Type Headache Pada Mahasiswa Fakultas Kedokteran Universitas Udayana Angkatan 2018Document34 pagesHubungan Durasi Penggunaan Alat Elektronik Dengan Tension Type Headache Pada Mahasiswa Fakultas Kedokteran Universitas Udayana Angkatan 2018Rio Ersa AnandaNo ratings yet
- Identification Death Dying Declaration AGE: Presented byDocument82 pagesIdentification Death Dying Declaration AGE: Presented bySaveeza Kabsha AbbasiNo ratings yet
- B6119 Mosquitoes and The Diseases They TransmitDocument8 pagesB6119 Mosquitoes and The Diseases They Transmitnirmal dNo ratings yet
- Anglais - College Prive Montesquieu - Sequence 3 - Annee Scolaire 2020 - 2021 - Classe de 6ème CamerounDocument3 pagesAnglais - College Prive Montesquieu - Sequence 3 - Annee Scolaire 2020 - 2021 - Classe de 6ème CamerounJacky MadoNo ratings yet
- JDentResRev83194-5251648 143516Document6 pagesJDentResRev83194-5251648 143516Harnoor GhumanNo ratings yet
- Review of Studies On Flight Attendant Health and Comfort in Airliner CabinsDocument9 pagesReview of Studies On Flight Attendant Health and Comfort in Airliner CabinsStudentNo ratings yet