Professional Documents
Culture Documents
Drugs Hypersensitivity Reaction in Patient With Human Immunodeficiency Virushiv Infection 2155 6121 1000252
Uploaded by
Lindia PrabhaswariCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drugs Hypersensitivity Reaction in Patient With Human Immunodeficiency Virushiv Infection 2155 6121 1000252
Uploaded by
Lindia PrabhaswariCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/316103569
Drugs Hypersensitivity Reaction in Patient with Human Immunodeficiency
Virus (HIV) Infection
Article · March 2017
DOI: 10.4172/2155-6121.1000252
CITATIONS READS
7 408
5 authors, including:
Rahmawati Minhajat I. Djaharuddin
Universitas Hasanuddin Universitas Hasanuddin
50 PUBLICATIONS 211 CITATIONS 43 PUBLICATIONS 210 CITATIONS
SEE PROFILE SEE PROFILE
Syakib Bakri
Universitas Hasanuddin
101 PUBLICATIONS 175 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Kidney and NAFLD View project
rare case chalenging case View project
All content following this page was uploaded by Rahmawati Minhajat on 14 April 2017.
The user has requested enhancement of the downloaded file.
Journal of Allergy & Therapy Minhajat et al., J Allergy Ther 2017, 8:1
DOI: 10.4172/2155-6121.1000252
Case Report OMICS International
Drugs Hypersensitivity Reaction in Patient with Human Immunodeficiency Virus
(HIV) Infection
Rahmawati Minhajat1,2*, Irawaty Djaharuddin3, Risna Halim4, Andi Fachruddin Benyamin5 and Syakib Bakri6
1Internal Medicine Department, Hematology and Medical Oncology Division, Medical Faculty Hasanuddin University, Makassar, Indonesia
2Histology Department, Medical Faculty Hasanuddin University, Makassar, Indonesia
3Internal Medicine Department, Pulmonology Division, Medical Faculty, Hasanuddin University, Makassar, Indonesia
4Internal Medicine Department, Tropic and Infection Division, Medical Faculty, Hasanuddin University, Makassar, Indonesia
5Internal Medicine Department, Hematology and Medical Oncology Division, Medical Faculty, Hasanuddin University, Makassar, Indonesia
6Internal Medicine Department, Nephrology and Hypertension Division, Medical Faculty, Hasanuddin University, Makassar, Indonesia
*Corresponding author: Rahmawati Minhajat, Internal Medicine Department, Hematology and Medical Oncology Division, Medical Faculty Hasanuddin University,
Makassar, Indonesia, E-mail: rahmawatiminhajat@med.unhas.ac.id
Received date: March 14, 2017; Accepted date: March 22, 2017; Published date: March 31, 2017
Copyright: © 2017 Minhajat R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
A case of male, 34 years old with a diagnosis of immunodeficiency syndrome resulting from HIV infection with
suspected pneumonia in the differential diagnosis of pulmonary tuberculosis relapse, in the course of the disease,
patients experienced hypersensitivity reactions to some antibiotics and antituberculosis drugs. Hypersensitivity
reactions were exaggerated by immune response to an allergen in a normal immune system. In this case, we found
the drug hypersensitivity reactions in patients with immunodeficiency. Until now, the exact underlying mechanism is
not fully known but may be due to multifactorial and the dysregulation of the immune system due to HIV infection.
Keywords: AIDS; Immunodeficiency; Hypersensitivity hypersensitivity that is not played by antibodies but by T lymphocytes
[3].
Introduction Drug hypersensitivity reaction in HIV infection often occurs. In
Acquired Immunodeficiency Syndrome (AIDS) is a collection of fact, it is reported to occur 100 times more frequently than non-HIV
symptoms caused by Human Immunodeficiency Virus (HIV) patients. Drug hypersensitivity reactions in HIV-infected patients are
infection, an RNA virus including Retrovirus from the lentivirus clinically similar to drug hypersensitivity reactions in non HIV-
family, which attacks the immune system [1,2]. infected [4]. Although drug hypersensitivity reactions in patients with
HIV infection often occurs but the case is very rarely reported.
The main target of HIV infection is the CD4+ lymphocytes (T
helper/Th) which play a central role in the immune system. In the early We report one case, male 34 years with immunodeficiency
course of the disease, the immune system can control the HIV syndrome due to HIV infection in the course of his illness he
infection, but with the course of the disease, HIV will further cause a experienced a hypersensitivity reaction to some antibiotics and
decrease number of CD4+ lymphocytes, disruption of homeostasis and antituberculosis drugs.
function of other cells in the immune system. This situation will
further lead to various symptoms with a wide clinical spectrum as the Case Report
result of a disturbance in the function of cellular and humoral
A male patient, 34 years old, entered hospital with a chief complaint
immunity. These viruses cause disease through several mechanisms
of shortness of breath experienced since one week before
including immune deficiency that causes opportunistic infections,
hospitalization. Shortness of breath was felt constantly, not influenced
autoimmune reactions and hypersensitivity reactions as well as
by the activity and positional change. Since a week ago, patient
tendency of malignancy [1,2].
experienced productive cough, with white mucous, no blood, left chest
Hypersensitivity reactions are excessive immune response to an pain is felt especially when coughing. Fever experienced since one
allergen in a normal immune system. Drug hypersensitivity is an week, especially at night, no chills, no seizures and no headache. No
excessive immune response to the drug substance or its metabolites nausea and vomiting, loss of appetite three days before entering the
through immunological reactions that occur during or after the use of hospital. Patients gained weight in the last six months but previously
drugs in which this mechanism may be mediated by immunoglobulin experienced a weight loss of about 5-10 kg in five years. Normal
or T lymphocytes. Hypersensitivity reactions according to Gell and urination and defecation.
Coombs are classified into four types: type I reaction is immediate
No history of asthma and food or medication allergies, no history of
hypersensitivity played by IgE, the type II reaction is a cytotoxic
recurrent diarrhea, no history of blood transfusion, there is a history of
reaction played by IgM/IgG, type III reaction or immune complex
smoking since high school and drug abuse, no history of free sex.
reaction played by IgM/IgG, and type IV reactions are delayed type
Other data regarding the history of previous illness was ever treated
with typhoid fever in 1998, 2001 and 2004. In 2004 history of Morbili,
J Allergy Ther, an open access journal Volume 8 • Issue 1 • 1000252
ISSN:2155-6121
Citation: Minhajat R, Djaharuddin I, Halim R, Benyamin AF, Bakri S (2017) Drugs Hypersensitivity Reaction in Patient with Human
Immunodeficiency Virus (HIV) Infection. J Allergy Ther 8: 252. doi:10.4172/2155-6121.1000252
Page 2 of 4
2005 hospitalized with heart valve disorder, and 2009 patients had given high-protein, high-calorie diet, oxygen, isotonic infusion fluid
recurrent stomatitis accompanied by infection of left and dextra and paracetamol. Until the third day of treatment, patients often
inguinal. Patient was given Ciprofoxacin but allergic skin symptoms experienced shortness of breath, fever (37.80°C to 39.50°C), coughing
appeared after a few minutes taking the drug. Since January 2010 he with sputum. Oral candidiasis, bronkovesikuler respiratory sounds,
was diagnosed with lung tuberculosis. Patient was given oral anti- rales at the apex of the left lung. Laboratory results; leukocytes
tuberculosis drugs, 4 Fixed Dose Combination (4FDC) four times a 9,800/uL, hemoglobin; 10.3 g/dl, the red blood cells: 5.42 x 106/uL,
day. Allergy symptoms such as skin rash appeared at the whole body hematocrit; 33.8%, platelets; 274,000 /uL, monocytes; 9%, segment;
accompanied by itching and shortness of breath which occured after 82%, lymphocytes; 9% , eosinophil 8%, erythrocyte sedimentation rate;
approximately one week taking the 4FDC medication. FDC then 74 mm 1st h and 92 mm at 2nd hour, renal function within normal
replaced with separate medicine (Rifampicin/INH/Pyrazinamide/ limits and chest X-ray impression: bilateral bronchopneumonia.
Ethambutol). About a week later the same allergy symptoms appeared, Additional therapy was given Ceftriaxone injection 1 g/12 h, skin test
and then the patient was declared allergic to Rifampicin and before ceftriaxon injection found positive allergic reactions such as
Pyrazinamide. erythema and edema locally. Ceftriaxone then replaced by 200 mg
Ofloxacin twice daily. Laboratory results of HIV rapid test is reactive
The physical examination found, the impression was seriously ill,
(positive), CD4 laboratory results; the absolute value was 18 cells/pl
well-nourished with body mass index (BMI) of 23.3 kg/m2, compos
(Normal range 410-1590 cells/pl) and the percentage was 2% (Normal
mentis, blood pressure 120/80 mmHg, respiratory 30 times per minute
range 31-60), the T-helper lymphocytes count was very less. Patient
thoracoabdominal, 38, 20°C axillary temperature, pulse 92 times/
confirmed positive HIV. Added ARV therapy (Lamivudine,
minute. Examination of the oral cavity found oral candidiasis.
Zidovudine and efavirenz) twice daily, Ceftazidine 1 g/12 h/IV, but the
Bronkovesikuler breath sounds on thoracic auscultation, additional
results show positive skin test allergy (local erythema and edema).
sound was rales at the apex of the left lung, no wheezing.
Ceftazidine replaced with Cefotaxime 1 g twice daily intravenous.
Based on the history and physical examination, working diagnosis Other drugs are co-trimoxazole, Bromhexine HCL and Fluconazole
was suspected pneumonia with differential diagnosis pulmonary TB (Table 1).
relaps and suspected immunodeficiency syndrome. Initial therapy was
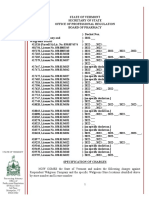
Time September 2009 January 2010 July 2010 July 2010
Drug name Ciprofloxacin Rifampicin Ceftriaxon Ceftazidine
Pyrazinamide
Time of reaction after taking the A few minutes A week 5 minutes 5 minutes
drug
Symptoms Red spots on the skin of the whole Red spots on the skin the whole Red spots and edema when Red spots and edema when
body accompanied by intense body accompanied by intense skin tests skin tests
itching and nausea itching and shortness of breath
Table 1: Summary of drugs hypersensitivity reaction history.
On the 15th day of treatment, the patient was allowed to go home (PZA) and rifampicin in HIV-infected patients will be at risk of drug
and outpatient care. At that time the patient's condition is good, no hypersensitivity 20 times more often than those who not HIV-infected
fever, no shortness of breath, a temperature of 36°C, respiratory 16 [5]. The drugs often reported allergic reactions in patients who are
times per minute, no oral candidiasis, respiratory sound HIV positive is trimethoprim-sulfamethoxazole, penicillin group,
bronchovesicular with rales at the apex of the left lung. antituberculosis, antiretroviral, non-steroidal anti-inflammatory drugs
(NSAIDs) and anticonvulsants [6]. The reason underlying the increase
Discussion in drug hypersensitivity reactions in people infected with HIV have
not clearly known, but the dysregulation of the immune system on T
We reported a case, male 34 years with immunodeficiency and B lymphocytes is likely play a role and some multifactorial
syndrome resulting from HIV infection with suspected pneumonia, including changes in drug metabolism, oxidative stress, cytokine
pulmonary TB relapse, and in the course of his illness, patients profile, hyperactivation of the immune system and genetic factors are
experienced hypersensitivity reactions to some antibiotics and suspected play a role for this mechanism. HIV itself can be a dangerous
antituberculosis drugs. Further discussion on this case focused on the signal that tends to cause an immune response than the immune
drug hypersensitivity reactions in immunodeficiency due to HIV tolerance [5,7].
infection.
The pathogenesis of hypersensitivity reactions in HIV infection is
Patient in this case did not have a history of allergic diseases or not clearly known, considered through an allergic reaction (immune
allergies to drugs and food. A tendency to experience allergic reactions mediated) or because of unknown causes toxic. However, this
begins to occur after the appearance of symptoms of hypersensitivity reaction cannot be put into one of the four types of
immunodeficiency disease. Reported that a hypersensitivity reaction to hypersensitivity reactions by Gell and Coombs classification. This is
trimethoprim-sulfametoksazole occurs 60% in HIV-positive patients indeed very contradictory that hypersensitivity reaction occurs in
and only 5% in immunocompetent or immunodeficient not due to people who 'energy' against some other stimulants [8].
HIV infection. Giving antituberculosis isoniazid (INH), pyrazinamide
J Allergy Ther, an open access journal Volume 8 • Issue 1 • 1000252
ISSN:2155-6121
Citation: Minhajat R, Djaharuddin I, Halim R, Benyamin AF, Bakri S (2017) Drugs Hypersensitivity Reaction in Patient with Human
Immunodeficiency Virus (HIV) Infection. J Allergy Ther 8: 252. doi:10.4172/2155-6121.1000252
Page 3 of 4
Some conditions are thought to play a role [1,9], disregulations on with some viruses common in HIV positive patients. Virus can interact
the immune system: reaction to amoxicillin, trimethoprim- with the immune system through several points; during drug
sulfametokzasol and OAT medicine often occurs in low CD4 levels metabolism, during the presentation of medicine/drug metabolites by
(20-<200/uL). Histopathologic examination showed similar dendritic cells as antigen presenting cells (APC) to lymphocytes and
abnormalities, independent to the drug precipitating, estimated as the when cytokine and kemokin production [18-20].
general nature pathogenesis [2]. Co-infection with other viruses: such
In 1992, from Zimbabwe reported that the anti-tuberculosis drug
as Epstein-Barr virus (EBV), cytomegalovirus (CMV) and some other
reactions more frequently in HIV-positive patients (98 of 363 patients)
respiratory viruses reported to be associated with the occurrence of
than patients who were not infected with HIV (64 of 543). Most
skin rash due to Ampicillin. Not found the incidence of skin rash when
frequent clinical manifestations of hypersensitivity reactions due to
the acute phase of infection by these viruses has passed [3]. The dose
OAT medicine in HIV-positive patients are skin hypersensitive (64%).
and duration of using drug also play a role: It’s found that
This reaction arises almost entirely within the first 8 weeks giving OAT
hypersensitivity reaction often occur for the high-dose trimethoprim-
[21,22]. In this case, the patient has an allergy when taking
sulfametokzasol when compared with low doses as a prophylactic. The
OAT 4FDC, reddish spots appeared at the entire body accompanied by
longer the medicine consumed, the higher possibility of a
itching and shortness of breath that comes after a week of taking the
hypersensitivity reaction [4]. Other factors ecg immunoglobulins that
medication. After administration of antituberculosis medicine
are specific to a particular drug and drug structure and its metabolism
separately, the patient then known allergic to Rifampicin and
in the body.
Pyrazinamide. In the combination therapy, it is difficult to determine
CD4+ lymphocytes is a central regulator of the immune system which drug caused the reaction but Rifampicin is reported as the most
that these cells have two types of T helper-1 (Th-1) and -2 (Th-2) frequent cause of reaction [23]. These patients also have allergic
which are differentiated by cytokines released. Th-1 cells produce reactions to quinolones class. Anaphylactic reaction to ciprofloxacin
interferon gamma (INF-ɣ) and interleukin (IL)-2 which is an were reported more frequently found in HIV-positive patients and
important mediator of the cellular immune response, while Th-2 often fatal [23,24].
produces IL-4, IL-5, IL-6 and IL-10 which is an important mediator for
Action taken in the event of drug hypersensitivity reactions in
the humoral immune respon that help B lymphocytes produce
patients with immunodeficiency is to stop or avoid medications shown
antibodies [10]. HIV infection not only causes immunodeficiency, but
to cause hypersensitivity reactions and replace with other drugs with
also lead to dysregulation of the immune system. It plays an important
the same therapeutic purposes. Desensitization or the role of using
role in the progression of the HIV disease [11]. Once infected by HIV,
corticosteroids as immunosuppresant is fully unknown. Treatment
changes in cytokine profiles appears as it found an increase in
aimed essentially for the underlying disease in which hypersensitivity
production of IL-4 which is always accompanied by increased
reactions will disappear along with the improvement of the patient's
production of IL-5 and decreased production of INF-ɣ [10]. Clerici et
immune system [2].
al. reported that in the early phase of HIV infection, the cytokines
produced by Th-1 and Th-2 still in a normal balance, but later, the
cytokines produced by Th-2 (IL-4) increase while cytokine produced Summary
by Th-1 (IL-2) decrease. It supports the shift from Th-1 to Th-2 in the We reported a case, male 34 years with immunodeficiency
early phase of HIV infection [12]. Clinical findings that support an syndrome resulting from HIV infection with suspected pneumonia,
increase in the production of Th-2 cytokine is the allergic pulmonary TB relapse, and in the course of his illness, patients
manifestation and increase levels of IgE in patients infected with HIV, experienced hypersensitivity reactions to some antibiotics and OAT.
in which the increase serum levels of IgE significantly associated with a
reduction in CD4+ cells count (less than 200/mm2) [13-15]. In the Patient in this case did not have a history of allergic diseases or
further clinical course, the progressive decline in the production of allergies to drugs and food. A tendency to experience allergic reactions
IL-2 and IL-4 cytokines occur. In the humoral immune system, HIV to some medicines begin occurs after the appearance of
itself causes the stimulation of B lymphocytes polyclonally and immunodeficiency disease symptoms. The clinical symptoms of allergy
unspecificaly which cause a problem because of an unappropriate reaction were reddish spots at entire body accompanied by itching and
immune response [12]. shortness of breath.
The results of in vitro studies demonstrate that HIV-infected cells Drugs hypersensitivity reactions are more common in HIV-infected
may be more susceptible to damage and cell death directly due to the patients. Until now, the exact mechanism underlying this reaction is
reaction of drug metabolites, further damage or cell death is then not fully known but may be due to multifactorial and the dysregulation
interpreted as a "danger signal" and stimulate the T lymphocytes to of the immune system by HIV infection. However, at
initiate a series of immune responses and the release of cytokines immunodeficiency drugs hypersensitivity cannot be entered in the one
which manifests as a drugs hypersensitivity reaction [16]. Glutathione of four types of hypersensitivity reactions by Gell and Coombs
deficiency in HIV infection is considered as another mechanism that classification.
may be the cause. Other studies demonstrate that HIV replication is
stimulated by Tat protein, which is the Tat protein expression References
associated with increased oxidative stress, decreased glutathione
biosynthesis and cellular concentration. Glutathione seems to play a 1. French RF, Stewart GJ, Penny R, Levy JA (1997) How HIV produces
immune deficiency: Managing HIV. Med J Aust 164: 166-171.
role in protection of cells from a toxic metabolite substance [5,17].
2. Carr A, Cooper DA, Penny R (1991) Allergic manifestations of human
Some types of viral infection is associated with the occurrence of immunodeficiency virus (HIV) infection. J Clin Immunol 11: 55-64.
an allergic reaction to medicine. The virus include; human herpes virus 3. Rajan TV (2003) The Gell-Coombs classification of hypersensitivity
6 (HHV-6), Epstein-Barr virus (EBV) and paramixovirus. Co-infection reactions: a re-interpretation. Trends Immunol 24: 376-379.
J Allergy Ther, an open access journal Volume 8 • Issue 1 • 1000252
ISSN:2155-6121
Citation: Minhajat R, Djaharuddin I, Halim R, Benyamin AF, Bakri S (2017) Drugs Hypersensitivity Reaction in Patient with Human
Immunodeficiency Virus (HIV) Infection. J Allergy Ther 8: 252. doi:10.4172/2155-6121.1000252
Page 4 of 4
4. Coopman SA, Johnson RA, Platt R (1993) Cutaneous disease and drug 15. Wright DN, Nelson RP Jr, Ledford DK, Fernandez-Caldas E, Trudeau
reactions in HIV infection. N Engl J Med 23: 1670-1674. WL, et al. (1990) Serum IgE and human immunodeficiency virus (HIV)
5. Phillips E, Mallal S (2007) Drug hypersensitivity in HIV. Curr Opin infection. J Allergy Clin Immunol 85: 445-452.
Allergy Clin Immunol 7: 324-330. 16. Naisbitt DJ, Vilar FJ, Stalford AC, Wilkins EG, Pirmohamed M, et al.
6. Dlova CN, Mosam A (2006) Drug reactions and the skin in HIV/AIDS. (2000) Plasma cysteine deficiency and decreased reduction of
South Afr J HIV Med 7: 18-22. nitrososulfamethoxazole with HIV infection. AIDS Res Hum
7. Chaponda M, Pirmohamed M (2011) Pirmohamed M Hypersensitivity Retroviruses 16: 1929-1938.
reactions to HIV therapy. Br J Clin Pharmacol 71: 659-671. 17. Walmsley SL, Winn LM, Harrison ML, Uetrecht JP, Wells PG, et al. (1997)
8. Carr A, Garsia R (1996) How HIV leads to hypersensitivity reactions: Oxidative stress and thio depletion in plasma and peripheral blood
Managing HIV. Med J Aust 164: 227-229. lymphocytes from HIV-infected patients: toxicological and pathological
implications. AIDS 11: 1689-1697.
9. Merati TP, Djauzi S (2011) Respon imun infeksi HIV. Jakarta Allergy and
Immunology Network. 18. Torres MJ, Mayorga C, Blanca M (2009) Nonimmediate allergic reactions
induced by drugs: pathogenesis and diagnostic tests. J Investig Allergol
10. Meyaard L, Otto SA, Keet IP (1994) Changes in cytokine secretion
Clin Immuno 19: 80-90.
patterns of CD4+ T-cell clones in human immunodeficiency virus
infection. Blood 84: 4262-4268. 19. Merk HF, Niederau D, Hertl M, Jugert F (1991) Drug metabolism and
drug allergy. New Trends in Allergy III pp: 269-280.
11. Calabrese LH (1988) Autoimmune manifestations of human
immunodeficiency virus (HIV) infection. Clin Lab Med 8: 269-279. 20. Levy M (1984) The combined effect of virus and drugs in drug-induced
diseases. Med Hypotheses 14: 293-296.
12. Clerici M, Hakim FT, Venzon DJ, Blatt S, Hendrix CW, et al. (1993)
Changes in interleukin-2 and interleukin-4 production in asymptomatic 21. Empson M, Bishop AG, Nightingale B, Garsia R (1999) Atopy, anergic
human immunodeficiency virus-seropositive individuals. J Clin Invest 91: status, and cytokineexpression in HIV-infected subjects. J Allergy Clin
759-765. Immunol 103: 833-842.
13. Small CB, Kaufman A, Armenaka M, Rosenstreich DL (1993) Sinusitis 22. Pozniak AL, MacLeod GA, Mahari M, Legg W, Weinberg J, et al. (1992)
and atopy in human immunodeficiency virus infection. J Infect Dis 167: The influence of HIV status on single and multiple drug reactions to
283-290. antituberculous therapy in Africa. AIDS 6: 809-814.
14. Sample S, Chernoff DN, Lenahan GA, Serwonska MH, Rangi S, et al. 23. Bates CM (1996) HIV medicine: drug side effects and interactions.
(1990) Elevated serum concentrations of IgE antibodies to environmental Postgrad Med 72: 30-33.
antigens in HIV-seropositive male homosexuals. J Allergy Clin Immunol 24. Peters B, Pinching AJ (1989) Fatal anaphylaxis associated with
86: 876-880. ciprofloxacin in a patient with AIDS related complex. BMJ 298: 605.
J Allergy Ther, an open access journal Volume 8 • Issue 1 • 1000252
ISSN:2155-6121
View publication stats
You might also like
- Immunology: A Brief Review On Immune Mediated DiseasesDocument7 pagesImmunology: A Brief Review On Immune Mediated DiseasesYSR SarmaNo ratings yet
- Nelson 2017Document28 pagesNelson 2017Santiago GonzalezNo ratings yet
- Viral Immunology and ImmunopathologyFrom EverandViral Immunology and ImmunopathologyAbner Louis NotkinsNo ratings yet
- HHS Public Access: Antibiotic AllergyDocument32 pagesHHS Public Access: Antibiotic AllergyInanda DamantiaNo ratings yet
- AllergyDocument86 pagesAllergyhoor e ainNo ratings yet
- 323 323 1 PBDocument9 pages323 323 1 PBjimejaikelNo ratings yet
- 07 ImmunopathologyDocument4 pages07 Immunopathologylight liNo ratings yet
- AIDS Research and TherapyDocument14 pagesAIDS Research and TherapyliaNo ratings yet
- Hypersensitivity To Drugs and Their Mechanisms: Name: Mellya Rizki Pitriani Student ID: B1B017031Document10 pagesHypersensitivity To Drugs and Their Mechanisms: Name: Mellya Rizki Pitriani Student ID: B1B017031Mellya RizkiNo ratings yet
- CTN PPT Aisiri RaoDocument14 pagesCTN PPT Aisiri RaoAisiri RaoNo ratings yet
- Bioorganic Chemistry: Yagyesh Kapoor, Kapil Kumar TDocument25 pagesBioorganic Chemistry: Yagyesh Kapoor, Kapil Kumar TAlexandru SavaNo ratings yet
- Analysis: The Antibiotic Course Has Had Its DayDocument5 pagesAnalysis: The Antibiotic Course Has Had Its Daysimx88No ratings yet
- Test Bank For High Acuity Nursing 5th Edition Kathleen WagnerDocument22 pagesTest Bank For High Acuity Nursing 5th Edition Kathleen WagnerDavidRobinsonfikq100% (39)
- AnakDocument8 pagesAnakIvan HoNo ratings yet
- HHS Public Access: Controversies in Drug Allergy: Testing For Delayed ReactionsDocument16 pagesHHS Public Access: Controversies in Drug Allergy: Testing For Delayed ReactionsВалерия НикитинаNo ratings yet
- Basic Immunology Introduction:: Hypersensitivity ReactionsDocument10 pagesBasic Immunology Introduction:: Hypersensitivity ReactionsRashed ShatnawiNo ratings yet
- Andosan™-An Anti-Allergic and Anti-Inflammatory Ingredient Prepared From Agaricus Blazei MushroomDocument11 pagesAndosan™-An Anti-Allergic and Anti-Inflammatory Ingredient Prepared From Agaricus Blazei MushroomMartinaNo ratings yet
- Immunology Breakthrough by SlidesgoDocument18 pagesImmunology Breakthrough by SlidesgoTooba NaeemNo ratings yet
- Immunity and InfectionsDocument4 pagesImmunity and InfectionsvinnNo ratings yet
- Antibiotic Allergy When To Test Challenge or Desensitise 2161 0703 1000234Document7 pagesAntibiotic Allergy When To Test Challenge or Desensitise 2161 0703 1000234Heba HanyNo ratings yet
- Materi Dr. R. A. Myrna Alia, M.kes, Sp.a (K)Document33 pagesMateri Dr. R. A. Myrna Alia, M.kes, Sp.a (K)Handoyo KooNo ratings yet
- ASCIA HP Clinical Update Antibiotic Allergy 2014Document6 pagesASCIA HP Clinical Update Antibiotic Allergy 2014kkkssbbNo ratings yet
- HIV and Immune Reconstitution Inflammatory Syndrome HIV IRISDocument8 pagesHIV and Immune Reconstitution Inflammatory Syndrome HIV IRISntnquynhproNo ratings yet
- Allergy and Related DisordersDocument63 pagesAllergy and Related DisordersavisenicNo ratings yet
- Evaluation of Antibiotic Sensitivity Pattern in Acute TonsillitisDocument5 pagesEvaluation of Antibiotic Sensitivity Pattern in Acute TonsillitisyoanaNo ratings yet
- OJDOH - ms.ID.000638 2puplished AllergicDocument6 pagesOJDOH - ms.ID.000638 2puplished Allergicshayma rafatNo ratings yet
- Clinical Immunology DR - TahaDocument106 pagesClinical Immunology DR - TahaYaseen AhmadNo ratings yet
- Rare Fungal Infection Linked To A Case of Juvenile ArthritisDocument9 pagesRare Fungal Infection Linked To A Case of Juvenile ArthritisAhmad Fari Arief LopaNo ratings yet
- Pattern of Clinical Presentations in Immunocompromised PatientDocument14 pagesPattern of Clinical Presentations in Immunocompromised Patientkj185No ratings yet
- Nihms 661031 PDFDocument13 pagesNihms 661031 PDFryouchiimamuraNo ratings yet
- Drugallergy: Abdul Waheed,, Tiffany Hill,, Nidhi DhawanDocument8 pagesDrugallergy: Abdul Waheed,, Tiffany Hill,, Nidhi DhawanHusni mubarakNo ratings yet
- MJR 28 2 64Document6 pagesMJR 28 2 64jone6No ratings yet
- Congenital ImmunodeficiencyDocument6 pagesCongenital ImmunodeficiencyJewel Berbano IINo ratings yet
- Hypersensitivity Rev BWDocument34 pagesHypersensitivity Rev BWGuhanNo ratings yet
- Allergic Rhinitis (NEJM 2015) PDFDocument8 pagesAllergic Rhinitis (NEJM 2015) PDFEduardo MenaNo ratings yet
- Herxheimer ReactionDocument3 pagesHerxheimer ReactionatpickerNo ratings yet
- Rifka Humaida - Strategy To Handle Resistance of AntibioticsDocument11 pagesRifka Humaida - Strategy To Handle Resistance of AntibioticsHeru SigitNo ratings yet
- Ceftriaxone-Induced Fatal Anaphylaxis Shock at An Emergency Department: A Case ReportDocument3 pagesCeftriaxone-Induced Fatal Anaphylaxis Shock at An Emergency Department: A Case ReportHeLena NukaNo ratings yet
- Medical Immunology: Optimal Clinical Trial Designs For Immune-Based Therapies in Persistent Viral InfectionsDocument4 pagesMedical Immunology: Optimal Clinical Trial Designs For Immune-Based Therapies in Persistent Viral InfectionsFrontiersNo ratings yet
- Immediate Hypersensitivity and Serum IgE AntibodyDocument9 pagesImmediate Hypersensitivity and Serum IgE AntibodyMini LaksmiNo ratings yet
- NIH Public Access: Author ManuscriptDocument27 pagesNIH Public Access: Author ManuscriptIesanu MaraNo ratings yet
- Mohapatra 2010Document13 pagesMohapatra 2010zavoianu.diana21No ratings yet
- Insulin HypersensitivityDocument9 pagesInsulin HypersensitivityApróné Török IbolyaNo ratings yet
- Allergy: Lars A HansonDocument9 pagesAllergy: Lars A HansonFrancisco BecerraNo ratings yet
- Alergias A FungosDocument10 pagesAlergias A FungosLuiz JmnNo ratings yet
- Microbio. Chapter 16 StudyDocument8 pagesMicrobio. Chapter 16 Studyaphillips1No ratings yet
- The Immune Hallmarks of Severe CovidDocument30 pagesThe Immune Hallmarks of Severe CovidRaghu NadhNo ratings yet
- 1-s2.0-S0952791517301036-Willem Van de Veen Immune Tolerance 2017Document22 pages1-s2.0-S0952791517301036-Willem Van de Veen Immune Tolerance 2017vivekverma3509No ratings yet
- Johnson 2004Document9 pagesJohnson 2004Abdul Wahab 2008126345No ratings yet
- Case Study UrtiDocument9 pagesCase Study UrtiHomework PingNo ratings yet
- Allergy, Asthma & Clinical Immunology Volume 14 Issue S2 2018 (Doi 10.1186 - S13223-018-0289-Y) Warrington, Richard Silviu-Dan, Fanny Wong, Tiffany - Drug AllergyDocument11 pagesAllergy, Asthma & Clinical Immunology Volume 14 Issue S2 2018 (Doi 10.1186 - S13223-018-0289-Y) Warrington, Richard Silviu-Dan, Fanny Wong, Tiffany - Drug AllergyViantika MerryliaNo ratings yet
- Probiotics and Prebiotics in Atopic Dermatitis: Pros and Cons (Review)Document8 pagesProbiotics and Prebiotics in Atopic Dermatitis: Pros and Cons (Review)larissaNo ratings yet
- Lectuer 3 - Epidemiology in CHN - XXDocument50 pagesLectuer 3 - Epidemiology in CHN - XXObada DyabNo ratings yet
- Allergy: Back To IndexDocument8 pagesAllergy: Back To IndexjnsenguptaNo ratings yet
- Drug AllergyDocument61 pagesDrug Allergyadysti100% (1)
- AIDS Research and TherapyDocument10 pagesAIDS Research and TherapyliaNo ratings yet
- Anifrolumab, An Anti-Interferon-Alpha Receptor Monoclonal Antibody, in Moderate To Severe Systemic Lupus ErythematosusDocument38 pagesAnifrolumab, An Anti-Interferon-Alpha Receptor Monoclonal Antibody, in Moderate To Severe Systemic Lupus ErythematosusRaisa Mentari MoeisNo ratings yet
- New Schatz2018Document44 pagesNew Schatz2018abhijeet abhijeetNo ratings yet
- Smith 2008Document27 pagesSmith 2008Lindia PrabhaswariNo ratings yet
- KDIGO AKI Guideline DownloadDocument141 pagesKDIGO AKI Guideline DownloadSandi AuliaNo ratings yet
- MRI Imaging Features of HIV Related Central Nervous System Diseases: Diagnosis by Pattern Recognition in Daily PracticeDocument16 pagesMRI Imaging Features of HIV Related Central Nervous System Diseases: Diagnosis by Pattern Recognition in Daily PracticeLindia PrabhaswariNo ratings yet
- Fneur 12 741884 2Document8 pagesFneur 12 741884 2Lindia PrabhaswariNo ratings yet
- Ciz 1197Document8 pagesCiz 1197Lindia PrabhaswariNo ratings yet
- Guidelines Adult Adolescent OiDocument627 pagesGuidelines Adult Adolescent OiLindia PrabhaswariNo ratings yet
- Brit J Clinical Pharma - 2010 - ChapondaDocument13 pagesBrit J Clinical Pharma - 2010 - ChapondaLindia PrabhaswariNo ratings yet
- A Challenging Diagnosis That Eventually Results in A Life-Threatening Condition: Addison's Disease and Adrenal CrisisDocument4 pagesA Challenging Diagnosis That Eventually Results in A Life-Threatening Condition: Addison's Disease and Adrenal CrisisLindia PrabhaswariNo ratings yet
- 1 s2.0 S2352396416304108 MainDocument11 pages1 s2.0 S2352396416304108 MainLindia PrabhaswariNo ratings yet
- Sugisaki 2018Document8 pagesSugisaki 2018Lindia PrabhaswariNo ratings yet
- Hubungan Jenis Persalinan Dengan Kejadian Asfiksia Neonatorum Di Ruang Perinatologi Dan Neonatal DenpasarDocument5 pagesHubungan Jenis Persalinan Dengan Kejadian Asfiksia Neonatorum Di Ruang Perinatologi Dan Neonatal DenpasarLindia PrabhaswariNo ratings yet
- Case 9-2017: A 27-Year-Old Woman With Nausea, Vomiting, Confusion, and HyponatremiaDocument9 pagesCase 9-2017: A 27-Year-Old Woman With Nausea, Vomiting, Confusion, and HyponatremiaLindia PrabhaswariNo ratings yet
- Counterfeit and Substandard Drugs in TanzaniaDocument6 pagesCounterfeit and Substandard Drugs in TanzaniaPetro KarungamyeNo ratings yet
- DR Ian Johnston, Department of Anaesthesia, Raigmore Hospital, Inverness, University of AberdeenDocument5 pagesDR Ian Johnston, Department of Anaesthesia, Raigmore Hospital, Inverness, University of Aberdeenharsha mummakaNo ratings yet
- Nucleotide Metabolism: Introduction and de Novo Purine MetabolismDocument4 pagesNucleotide Metabolism: Introduction and de Novo Purine Metabolismkang seulgi can set me on fire with her gaze aloneNo ratings yet
- Study of Effect of Pilocarpine On Rabbit EyeDocument3 pagesStudy of Effect of Pilocarpine On Rabbit EyeSajjad AliNo ratings yet
- Hydralazine Drug StudyDocument1 pageHydralazine Drug StudySabrina MascardoNo ratings yet
- Epilepsy and Oral Hormonal Contraception-Indian Perspective: Review ArticleDocument6 pagesEpilepsy and Oral Hormonal Contraception-Indian Perspective: Review ArticleKirubakaranNo ratings yet
- 8.2.1.7 Bukti Evaluasi Ketersediaan FormulariumDocument4 pages8.2.1.7 Bukti Evaluasi Ketersediaan FormulariumAgil WijayantiNo ratings yet
- ?management Atopic Dermatitis - Dr. DinaDocument45 pages?management Atopic Dermatitis - Dr. DinaGlory Evergreen100% (1)
- Adrenoceptor AntagonistsDocument72 pagesAdrenoceptor AntagonistsAmit ShahNo ratings yet
- Common Drugs Used in The EmergencyDocument5 pagesCommon Drugs Used in The Emergencyhatem alsrour88% (25)
- LPN Jan 1Document49 pagesLPN Jan 1wltnz0418No ratings yet
- Cerebral CirculationDocument25 pagesCerebral Circulation20AR018 HARIHARA SUBRAMANIANNo ratings yet
- Hyponatremia in Cirrhosis: An Update: Joseph J. Alukal, MD, Savio John, MD and Paul J. Thuluvath, MD, FRCPDocument11 pagesHyponatremia in Cirrhosis: An Update: Joseph J. Alukal, MD, Savio John, MD and Paul J. Thuluvath, MD, FRCPMuzaffar MehdiNo ratings yet
- AmbitCapital HealthcareNEGATIVEUnravelingoftheIndianparadox AugDocument58 pagesAmbitCapital HealthcareNEGATIVEUnravelingoftheIndianparadox Augkumar somyaNo ratings yet
- B. Schematic Pathophysiology TETANUS-a Disease Condition Caused by Clostridium TetaniDocument5 pagesB. Schematic Pathophysiology TETANUS-a Disease Condition Caused by Clostridium TetaniWilliam Soneja CalapiniNo ratings yet
- Vielight Inventors Notes For Neuro Alpha and Neuro Gamma 2017Document17 pagesVielight Inventors Notes For Neuro Alpha and Neuro Gamma 2017arexixNo ratings yet
- Walgreens Specification of ChargesDocument40 pagesWalgreens Specification of ChargesMichael Cusanelli100% (2)
- Phytochemistry, Pharmacology, and Clinical Trials of Morus AlbaDocument14 pagesPhytochemistry, Pharmacology, and Clinical Trials of Morus AlbaArief WibisonoNo ratings yet
- Nag2019 PDFDocument288 pagesNag2019 PDFmashupNo ratings yet
- Alkaloid & Its General PropertiesDocument4 pagesAlkaloid & Its General Propertiesshankul kumar100% (9)
- GPHC Pre-Registration Complete Exam Question List JUNE 2017 - NOV 2021Document50 pagesGPHC Pre-Registration Complete Exam Question List JUNE 2017 - NOV 2021Summer Sunshine TVNo ratings yet
- Nanoformulations of Curcumin: An Emerging Paradigm For Improved Remedial ApplicationDocument19 pagesNanoformulations of Curcumin: An Emerging Paradigm For Improved Remedial ApplicationĐặng TrườngNo ratings yet
- Netter's Internal Medicine 2nd Ed 13Document9 pagesNetter's Internal Medicine 2nd Ed 13Panagiotis SouldatosNo ratings yet
- PCX - ReportDocument49 pagesPCX - ReportAbhishek GaurNo ratings yet
- Allergy: Molecule Strength Dosage Form Reference ATHENA India ATHENA FranceDocument2 pagesAllergy: Molecule Strength Dosage Form Reference ATHENA India ATHENA FranceUsama SayedNo ratings yet
- Hemostat Thromboplastin-SI: Determination of Prothrombin Time (PT)Document2 pagesHemostat Thromboplastin-SI: Determination of Prothrombin Time (PT)Lemi MaluluNo ratings yet
- Drug StudyDocument79 pagesDrug StudyShea Janson MercurioNo ratings yet
- Inotrope: Medical UsesDocument3 pagesInotrope: Medical UsesCake ManNo ratings yet
- Gs Selection Medline Embase DPDocument3,876 pagesGs Selection Medline Embase DPDavid Camilo PinzonNo ratings yet
- Phytochemicals From Phyllanthus Niruri Linn. and Their Pharmacological Properties: A ReviewDocument13 pagesPhytochemicals From Phyllanthus Niruri Linn. and Their Pharmacological Properties: A ReviewSiti khaizatul minnahNo ratings yet
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (30)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainFrom EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainRating: 4 out of 5 stars4/5 (95)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (60)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (45)