Professional Documents
Culture Documents
Esophagus Anatomy and Physiology
Uploaded by
Ibtehal Hasan0 ratings0% found this document useful (0 votes)
15 views10 pagesOriginal Title
esophagus anatomy and physiology
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
15 views10 pagesEsophagus Anatomy and Physiology
Uploaded by
Ibtehal HasanCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 10
- The esophagus is the first true gut-tube organ.
Its circular shape and four
histologic layers will serve as a model for the remainder of the GI tract.
- Anatomy of the Esophagus
- The esophagus is long. It starts in the neck and upper
mediastinum (upper third of the esophagus), courses
through the posterior mediastinum (middle third of
esophagus), and then penetrates the diaphragm into
the abdomen, where it connects with the stomach
(lower third of the esophagus). This division into
thirds is an oversimplification—the esophagus is a
continuous organ with a continuous network of
blood vessels, lymphatics, and nerves—but for the
sake of keeping track of the anatomy and pathology
relative to our position in the esophagus, we speak as
if it is literally divided into thirds.
- The esophagus is the most posterior organ, posterior
to the trachea, in the neck and upper mediastinum.
The aorta begins anterior to the trachea and
esophagus but loops around back to be the most
posterior organ of the inferior posterior
mediastinum. The esophagus crosses the diaphragm
at T10—the gastroesophageal junction—the
stomach separated from the esophagus by the lower
esophageal sphincter (LES). We talk about
sphincters at the end of the lesson. But here in
anatomy, the LES serves to mark the end of the
esophagus and the beginning of the stomach.
-
Figure 1: Anatomy of the Esophagus
In the neck, the esophagus is posterior to the trachea, separated by a small gap, filled in by
adventitia. In the superior mediastinum, the aorta originates anteriorly to the trachea and
arches to become the most posterior structure within the mediastinum. The esophagus
penetrates the diaphragm into the stomach. Several branches from the aorta provide the
vascular supply down the length of the esophagus. Most importantly, the veins that drain
the distal esophagus connect to the portal veins and caval veins. In times of increased portal
pressure, blood can exit the portal system to the caval system as esophageal varices.
The arterial supply to the esophagus comes from multiple
arteries, which form more of a web than a direct arterial
supply. The web is redundant—there are no watershed
areas in the esophagus. The lower third of the
esophagus is supplied by a branch of the left gastric artery,
which is itself a branch of the celiac trunk. The middle
third is supplied by branches of the aorta and bronchial
arteries. The upper third is fed by branches of the thyroid
artery. The arterial supply is not very high-yield, but it
establishes the concept of the thirds, and that the vascular
supply is going to come from different sources. This sets up
the discussion about the veins, which become clinically
significant.
The venous drainage follows the concept of the arterial
supply. The lower thirdof the esophagus is drained by
branches of the left gastric vein. This is particularly high-
yield because drainage for the gut is usually to the liver
through the portal vein. The venous drainage in the
mediastinum uses the hemiazygos and azygous veins, as
well as branches of the intercostal veins. There is a
connection between the azygos and hemiazygos veins and
the left gastric vein. The gut is arranged so that the
structures of digestion and absorption send their blood to
the liver via the portal vein, through which the liver does its
thing (Hepatobiliary Course) before returning blood to the
systemic circulation via the hepatic vein and inferior vena
cava. The rest of the body sends blood directly back to the
vena cavae. All veins are interconnected, and blood follows
the path of least resistance. When there is portal
hypertension (GI: Hepatobiliary: Cirrhosis), the flow from
the gut to the liver may reverse, flowing through the
esophageal veins into the azygous veins, causing
esophageal varices. The upper third of the esophagus is
drained by the inferior thyroid veins.
Histology of the Esophagus
We first describe the histological arrangement of the gut in
the esophagus lesson because it is the first of our lessons
that coves a true gut-tube organ. This arrangement is
consistent throughout the gut—from the esophagus to the
top of the pectinate line, the structure of these four layers is
consistent. We will spend a long time on it here, and only
summarize it in future lessons. Because each layer has
sublayers (we did not decide to classify them this way,
medical science did), it tends to really confuse learners.
There are four histological layers, starting from within the
gut lumen and working outward: 1) mucosa, 2) submucosa,
3) muscularis externa, and 4) serosa/adventitia. Follow
along with Figure 2 and Figure 3.
Figure 2: Histology of the Esophagus
The histological layers of the esophagus and their sublayers. This illustration has accentuated
the esophagus’s length below the diaphragm in order to elongate and, therefore, visually
separate the layers (and sublayers of the mucosa and muscularis externa).
In a cross-section of the gut tube, viewing these structures
as concentric rings, it is most appropriate to refer to them
as being more inward to or outward from the lumen and
relative to each other. But if the gut tube is sliced
longitudinally and laid flat, the lumen will be on top and
the adventitia on the bottom, and the structures can be said
to be above or below each other. We use the latter method
to describe them. First, we describe the three layers and
identify the sublayers of each layer, and then we go into the
details of each layer.
Figure 3: Histological Layers of the Esophagus
These low-magnification histological samples clearly demonstrate the histological layers. We
are only showing low-magnification views to concentrate on the full thickness of the
esophagus without getting bogged down with the details. The mucosa (with its epithelium),
lamina propria, and muscularis mucosae sit atop the submucosa, and the muscularis externa
lies beneath the submucosa. The first panel does not show the lower margin of the
esophagus, where the serosa (the lining of the peritoneal cavity) or adventitia would be. In
the second panel, the lumen is at the top, and the serosal edge is at the bottom.
The mucosa is made of three sublayers: epithelium, lamina
propria, and muscularis mucosae. The epithelium varies by
location in the GI tract. In the esophagus, it is pharyngeal
epithelium— nonkeratinized stratified squamous
epithelium. Like any epithelium, it has a basement
membrane that separates it from connective tissue. That
connective tissue is the lamina propria. In the lamina
propria are the very small blood vessels, nerves, and
lymphatics that serve the epithelium. Separating the lamina
propria from the submucosa is a very thin muscular band
called the muscularis mucosae. This is not a muscle of
motility. It is not a muscle that changes the diameter of the
lumen. This is also certainly not the muscularis externa
(because their names are similar, readers get them confused
—you will not).
Figure 4: Histological Layers of the Esophageal Mucosa
The mucosa consists of the epithelium (shown here as nonkeratinized stratified squamous
epithelium), the lamina propria and its blood vessels, and the muscularis mucosae. The
successive increases in magnification reveal more detail about the epithelium, its relationship
to the lamina propria, and the stratum basale and stratum spinosum. The stratum spinosum
resembles that of skin, but there is no granulosum or corneum layer. Instead, the cells are
engorged with the glycogen.
The submucosa is a band of connective tissue that spans
the distance below the mucosa and above the muscularis
externa. Technically, it is below the muscularis mucosae of
the mucosa, and above the circular smooth muscle of the
muscularis externa. The submucosa contains submucosal
glands (structures that usually secrete into the lumen) and
the submucosal plexus (Meissner’s plexus), which
influences the production of those glands. The submucosa
is also the conduit for the blood vessels, lymphatics, and
nerves destined for the lamina propria of the mucosa.
Figure 5: Submucosa of the Esophagus
The submucosa lies between the muscularis mucosae and the inner layer of the muscularis
externa. The esophagus can be identified by its nonkeratinizing stratified squamous
epithelium in the mucosa and the presence of mucinous submucosal glands (pale staining
cytoplasm) in the submucosa. The submucosa contains small- to medium-sized arteries.
The muscularis externa has three sublayers—the inner,
circular smooth muscle; the outer, longitudinal smooth
muscle; and the myenteric (Auerbach’s) plexus between the
two muscle sublayers that innervates the muscles and
serves motility. We detail the muscles and how they cause
motility later in this lesson.
The adventitia/serosa is the connective tissue below the
muscularis externa. In it are the large blood vessels,
lymphatics, and nerves that penetrate through the circular
smooth muscle of the muscularis externa to the myenteric
plexus of the muscularis externa—the blood vessels and
nerves that become the submucosal vessels and submucosal
plexus and the blood vessels and nerves of the lamina
propria.
As we move from the adventitia/serosa to the lumen, the
vessels get smaller and smaller until they become the
capillaries that feed the most distal epithelial cells.
Adventitia is connective tissue. Serosa is when that
adventitia is separated from another organ’s adventitia by
the lining of the peritoneal cavity—the mesothelium. We
get into this concept in GI: Abdominal Wall: Embryology
of the Peritoneal Cavity. So if this doesn’t jive yet, don’t
worry, it will.
Esophageal Physiology of Swallowing
We covered the initial phases of swallowing in the lesson
on the mouth, GI: Digestion and Absorption: Start to
Finish: The Mouth. There, we covered the oral phase and
the pharyngeal phase. Food was directed to the oropharynx.
The food bolus passed by the palatine arches and struck the
mucosa of the oropharynx. The pharyngeal phase is
involuntary: the trachea closes and the esophagus opens.
The food bolus is now ready to be moved into the stomach
through the esophagus. Here, we continue with the
esophageal phase.
Figure 6: The Phases of Swallowing
You saw this in this last lesson. It’s just here to reorient you.
The esophageal phase is involuntary and mediated by the
parasympathetics. The esophageal phase begins with the
relaxation of the upper esophageal sphincter, which allows
the food bolus to pass into the esophagus. The esophagus
must then move the bolus from the top to the bottom of the
esophagus. This process is facilitated by gravity. The
esophagus can move food up into the stomach if the patient
is inverted, but it isn’t very good at it (try drinking milk
while doing a headstand). But because the esophagus can
direct a food bolus against gravity, the esophagus must do
more than simply act as a tube through which the food
falls. Indeed, the esophagus has muscle all around its
circumference that can contract in a sequential, coordinated
fashion to propel the food bolus in one direction.
The muscularis externa of the upper third of the esophagus
isn’t like we described above. It is skeletal muscle,
reflecting the muscle and mucosa from which it is derived
—the pharynx. In the lower third of the esophagus, the
muscularis externa has the circular and longitudinal
sublayers—smooth muscle. The transition happens closer
to the top than the bottom, but the point is that there is a
change. Primary peristalsis, the coordinated, sequential
contraction and relaxation of esophageal smooth muscle
segments as caused by the food bolus hitting the palatine
arches and the back of the oropharynx, is regulated by the
vagus nerve. Secondary peristalsis, the coordinated,
sequential contraction and relaxation of esophageal smooth
muscle segments as caused by the food bolus being stuck in
the esophagus, is regulated by the stretching of the enteric
plexus. You get one shot at primary peristalsis per food
bolus. If the food bolus gets stuck, the esophagus can take
care of itself. Both forms of peristalsis require smooth
muscle changes.
Peristaltic propulsion occurs as a result of the contraction
of the circular muscle and relaxation of the longitudinal
muscle in the propulsive or upstream segment together with
the relaxation of the circular muscle and contraction of the
longitudinal muscle in the downstream receiving segment.
Now that we’ve said it the way textbooks do, let’s say it
again without the complexity of the longitudinal muscle
business.
The vagus nerve is going to open up the segment receiving
the bolus. At the same time, the vagus nerve is going to
close the segment the bolus is currently in, starting just
behind the food bolus. Like the squeezing of a tube of
toothpaste (aimed at the floor if the person is upright), the
food bolus is moved into the next segment. At which time
the next segment is relaxed, and the segment it is currently
in is contracted. The vagus nerve is in control but acts
through the myenteric plexus. Preganglionic fibers of the
vagus nerve synapse on ganglionic neurons in the
myenteric plexus. Those ganglionic neurons have short
postganglionic projections to the smooth muscle nearby.
The presynaptic fibers always release acetylcholine and
activate ionotropic acetylcholine receptors on ganglionic
neurons. The postganglionic fibers can either release
smooth muscle-contracting acetylcholine (via M -G - 3 q
IP /Ca second messengers) or smooth muscle-
3
2+
relaxing nitric oxide (via guanylyl cyclase-cGMP dilation).
Vasoactive intestinal peptide also dilates, but we’re trying
to keep this limited in scope.
Figure 7: Primary vs. Secondary Peristalsis
A food bolus contacting the oropharynx initiates primary peristalsis, in which the vagus
nerve coordinates a series of contractions (ACh) and dilations (NO) down the length of the
esophagus. If the food bolus gets stuck, distention of the esophagus results in another
peristaltic wave independent of the vagus nerve.
Most of the GI tract has the usual arrangement of circular
and longitudinal muscles. Most of the GI tract isn’t
contracted at rest. Contraction occurs to move the food
bolus, but every once in a while, there are
sphincters. Sphincters have very developed circular layers
of the muscularis externa. In their default position,
sphincters are tightly contracted. This means, wherever
they exist, they separate two compartments of the gut tube.
The lower esophageal sphincter (LES) separates the
esophagus from the stomach, acting as a two-way valve.
Acidic stomach contents shouldn’t come into the esophagus
(reflux), and a food bolus can’t get into the stomach unless
the sphincter opens. As the vagus conducts peristalsis, it
also coordinates the opening of the LES.
Figure 8: Vagal Innervation of the Esophagus and LES
Preganglionic fibers run down the vagus nerve to the myenteric plexus. There, they will
activate either contraction-stimulating, ACh-releasing postganglionic neurons or
contraction-inhibiting, NO-releasing postganglionic neurons. The peristaltic contraction is
timed with the opening of the LES to allow the food bolus in.
As we will remind you in every organ system, smooth
muscle contracts via calcium and dilates via cGMP. Almost
always, calcium is released from the endoplasmic reticulum
after the activation of the GPCR associated with G . q
Multiple pathways activate cGMP and, therefore, dilation
—the most notable is nitric oxide or the GPCR associated
with G .
s
Citations
Figures 3, 4, 5: Originating from the University of Alabama at
Birmingham, Department of Pathology PEIR Digital Library
at http://peir.net pursuant to a license grant by the UAB Research
Foundation.
You might also like
- Circulatory System: A Tutorial Study GuideFrom EverandCirculatory System: A Tutorial Study GuideRating: 5 out of 5 stars5/5 (3)
- The Jejunoileum: Anatomy The Abdomen Small and Large IntestineDocument7 pagesThe Jejunoileum: Anatomy The Abdomen Small and Large IntestineWaeel AbdullatifNo ratings yet
- Esophageal SurgeryDocument11 pagesEsophageal Surgerydr_kumananNo ratings yet
- Colon Benign Conditions - Surgery NotesDocument85 pagesColon Benign Conditions - Surgery NotesNagulan ChanemougameNo ratings yet
- Anatomy of Esophagus and StomachDocument65 pagesAnatomy of Esophagus and Stomachmackiecc100% (2)
- IntestinesDocument56 pagesIntestinesShimmering MoonNo ratings yet
- Clinical Anatomy of The Esophagus and StomachDocument82 pagesClinical Anatomy of The Esophagus and StomachmackieccNo ratings yet
- 3.digestive SystemDocument103 pages3.digestive Systemokoti.omutanyi22No ratings yet
- My StomachDocument24 pagesMy StomachPriya GKNo ratings yet
- Small Intestine AnatomyDocument4 pagesSmall Intestine AnatomyMaria Natalie IrwandaNo ratings yet
- Factors Affecting Clinical Outcomes Among Patients With Esophageal Varices BleedingDocument16 pagesFactors Affecting Clinical Outcomes Among Patients With Esophageal Varices BleedingMohamed ZezoNo ratings yet
- SURGERY - 1.5 Colon, Rectum, and Anus (Lecture)Document8 pagesSURGERY - 1.5 Colon, Rectum, and Anus (Lecture)Bianca Jane Maaliw100% (1)
- Unit 4 ReviewDocument53 pagesUnit 4 ReviewRoberta BansahNo ratings yet
- Post-Graduate Medical: JournalDocument5 pagesPost-Graduate Medical: JournallynaayusofNo ratings yet
- Anatomy and Physiology of RectumDocument5 pagesAnatomy and Physiology of RectumDoreen Claire M. WallangNo ratings yet
- 3.1 Anterior Abdominal Wall (Bea)Document5 pages3.1 Anterior Abdominal Wall (Bea)Norjetalexis CabreraNo ratings yet
- 18 IntestinesDocument28 pages18 Intestinesafzal sulemaniNo ratings yet
- The Boundaries of The Anterior Abdominal WallDocument63 pagesThe Boundaries of The Anterior Abdominal WallbeeNo ratings yet
- The Boundaries of The Anterior Abdominal Wall AreDocument62 pagesThe Boundaries of The Anterior Abdominal Wall ArebeeNo ratings yet
- ANAPHYG2Document8 pagesANAPHYG2Sam PenadosNo ratings yet
- OesophagusDocument3 pagesOesophagusХина КападиаNo ratings yet
- Bab IDocument9 pagesBab II Wayan Rendi AwendikaNo ratings yet
- The Abdominal AortaDocument9 pagesThe Abdominal AortaJuan Jose LeonNo ratings yet
- Digestive System: Digestive Glands. Alimentary CanalDocument27 pagesDigestive System: Digestive Glands. Alimentary CanalAnkit NariyaNo ratings yet
- Anatomy of The Rectum and Anal Canal: The Rectum Is The Part of The Colon Between The Sigmoid ColonDocument25 pagesAnatomy of The Rectum and Anal Canal: The Rectum Is The Part of The Colon Between The Sigmoid ColonJoy GhoseNo ratings yet
- 3 RD ENGDocument25 pages3 RD ENGVkcegcaNo ratings yet
- 14 StomachDocument24 pages14 Stomachafzal sulemaniNo ratings yet
- Structures of The ForegutDocument13 pagesStructures of The ForegutJatan KothariNo ratings yet
- Esophagus: Pipe or Gullet, Is An Organ in Vertebrates Through Which Food PassesDocument12 pagesEsophagus: Pipe or Gullet, Is An Organ in Vertebrates Through Which Food PassesCrow LordNo ratings yet
- Anatomy of Digestive SystemDocument20 pagesAnatomy of Digestive Systemolive jollyNo ratings yet
- Abdominal CavityDocument85 pagesAbdominal CavityMac HaNo ratings yet
- The AbdomenDocument2 pagesThe Abdomenrubie ann tillorNo ratings yet
- The Digestive System 3Document4 pagesThe Digestive System 3geniusgurl91No ratings yet
- Lecture 4Document14 pagesLecture 4X RamboNo ratings yet
- Anatomy of The KidneyDocument2 pagesAnatomy of The KidneychinecheremnfNo ratings yet
- Anatomy Abdominal Wall ThorekDocument26 pagesAnatomy Abdominal Wall ThorekAlna Shelah IbañezNo ratings yet
- Lecture 2 - Anatomy of The Ureters, Bladder and UrethraDocument7 pagesLecture 2 - Anatomy of The Ureters, Bladder and UrethraNatalie LiNo ratings yet
- RectumDocument43 pagesRectummidhunramesh007100% (4)
- Marking Scheme For Ant 414 (Functional Anatomy of Abdomen, Pelvis and Perineum) For 2017/2018 SessionDocument5 pagesMarking Scheme For Ant 414 (Functional Anatomy of Abdomen, Pelvis and Perineum) For 2017/2018 SessionmomoduNo ratings yet
- Anorectal Anatomy & Surgical ManagementDocument164 pagesAnorectal Anatomy & Surgical Managementsgod34No ratings yet
- UNIT 9 (Digestive System)Document8 pagesUNIT 9 (Digestive System)Workinesh Kaynabo KambaloNo ratings yet
- Abdominal Visceral OrgansDocument5 pagesAbdominal Visceral OrgansYudi Kelsi KaharapNo ratings yet
- Ac 2Document104 pagesAc 2saide limNo ratings yet
- Chapter I-V-1-Anatomy-Dr-Mark-MakaryDocument17 pagesChapter I-V-1-Anatomy-Dr-Mark-MakaryMark MakaryNo ratings yet
- Anatomy and Physiology of Colon of Case StudyDocument4 pagesAnatomy and Physiology of Colon of Case StudySimran JosanNo ratings yet
- Anatomi Fisiologi Dada AbdomenDocument16 pagesAnatomi Fisiologi Dada AbdomenemiliatamaraNo ratings yet
- Anatomy of UreterDocument19 pagesAnatomy of Ureterfabunmiopeyemiv23No ratings yet
- 323 Lecture 11Document45 pages323 Lecture 11Philip GituriNo ratings yet
- Lecture 5 Serous Sacs, Features and FunctionsDocument7 pagesLecture 5 Serous Sacs, Features and Functionssomebody_maNo ratings yet
- Stomach and Duodenum 10-27Document32 pagesStomach and Duodenum 10-27Ditas ChuNo ratings yet
- ССС 2019Document83 pagesССС 2019bekafop813No ratings yet
- Anatomy SpleenDocument32 pagesAnatomy SpleenBijo K BennyNo ratings yet
- Tugas Mandiri FloDocument24 pagesTugas Mandiri FloDom TorettoNo ratings yet
- 5.2 AbdomenDocument4 pages5.2 Abdomensaxman011No ratings yet
- Anatomy of OesophagusDocument25 pagesAnatomy of OesophagusRabi SyedNo ratings yet
- Anatomy of StomachDocument4 pagesAnatomy of StomachIntan Putri Maisarah100% (1)
- iNTERNAL oRGANSDocument92 pagesiNTERNAL oRGANSönemsiz biriNo ratings yet
- Anatomy of The Abdomen: Dr. Ahmad Kamil Shahwan Ph.D. General SurgeryDocument87 pagesAnatomy of The Abdomen: Dr. Ahmad Kamil Shahwan Ph.D. General SurgeryDaniel SitungkirNo ratings yet
- Journal of Entomology and Zoology Volume Eleven, Number Two, June 1919From EverandJournal of Entomology and Zoology Volume Eleven, Number Two, June 1919No ratings yet
- Qualtative ResearchDocument53 pagesQualtative ResearchIbtehal HasanNo ratings yet
- PBL Problem 1 Unit IV Week 1Document4 pagesPBL Problem 1 Unit IV Week 1Ibtehal HasanNo ratings yet
- Summar Resaerch ArticlesDocument1 pageSummar Resaerch ArticlesIbtehal HasanNo ratings yet
- Oral ExaminationDocument5 pagesOral ExaminationIbtehal HasanNo ratings yet
- Summar Resaerch ArticlesDocument1 pageSummar Resaerch ArticlesIbtehal HasanNo ratings yet
- Lecture Scanners FT v4Document75 pagesLecture Scanners FT v4Ibtehal HasanNo ratings yet
- Effect of Orofacial Myofunctional Exercise Using An Oral Rehabilitation Tool On Labial Closure Strength, Tongue Elevation Strength and Skin ElasticityDocument4 pagesEffect of Orofacial Myofunctional Exercise Using An Oral Rehabilitation Tool On Labial Closure Strength, Tongue Elevation Strength and Skin ElasticityUniversity Malaya's Dental Sciences ResearchNo ratings yet
- PAPER (ENG) - Swallowing Disturbance Questionnaire For Detecting DysphagiaDocument5 pagesPAPER (ENG) - Swallowing Disturbance Questionnaire For Detecting DysphagiaAldo Hip NaranjoNo ratings yet
- GastrointestinalDocument39 pagesGastrointestinalالمسوول الاعلاميNo ratings yet
- Rehabilitation of Glossectomy Cases With Tongue Prosthesis: A Literature ReviewDocument4 pagesRehabilitation of Glossectomy Cases With Tongue Prosthesis: A Literature ReviewmujtabaNo ratings yet
- Wei Mai (Parte 2) - Yin Wei MaiDocument15 pagesWei Mai (Parte 2) - Yin Wei MaiAlexandre HenriquesNo ratings yet
- Progressive Balbar Palsy: Dr. Mohamed Ali 3 Year MD IM ResidentDocument15 pagesProgressive Balbar Palsy: Dr. Mohamed Ali 3 Year MD IM ResidentMohamed AliNo ratings yet
- 11 PharynxDocument8 pages11 PharynxNur Ain Faezah RoslanNo ratings yet
- 4.3 Swallowing - Center - Concepts - and - ProceduresDocument7 pages4.3 Swallowing - Center - Concepts - and - Proceduresluribe662No ratings yet
- Dysphagia From A Neurogeriatric Point of ViewDocument6 pagesDysphagia From A Neurogeriatric Point of ViewVanessaCarrilloNo ratings yet
- Chapter 7 - The Digestive SystemDocument65 pagesChapter 7 - The Digestive SystemLama AlqarniNo ratings yet
- Canine and Feline Mega EsophagusDocument10 pagesCanine and Feline Mega Esophagustaner_soysurenNo ratings yet
- Dysphagia Management of Pediatric Patients With Cerebral PalsyDocument17 pagesDysphagia Management of Pediatric Patients With Cerebral PalsyDaniela AdarosNo ratings yet
- NCP GoiterDocument2 pagesNCP GoiterShaira De La CruzNo ratings yet
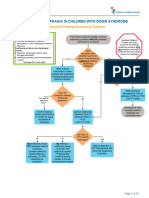
- Aspiration and Dysphagia in Children With Down SyndromeDocument23 pagesAspiration and Dysphagia in Children With Down SyndromeJessa MaeNo ratings yet
- Digestive SystemDocument60 pagesDigestive SystemdrynwhylNo ratings yet
- Videofluoroscopic Swallowing StudiesDocument25 pagesVideofluoroscopic Swallowing StudiesPriisciilla Vicencio100% (1)
- Git PhysioDocument102 pagesGit PhysioPahw BaluisNo ratings yet
- Table of Head and Neck MusclesDocument5 pagesTable of Head and Neck Musclesororoangel0% (1)
- 2007 CASLPA Position Paper On Dysphagia in AdultsDocument8 pages2007 CASLPA Position Paper On Dysphagia in AdultsEva Sala RenauNo ratings yet
- LX Suspension and UES Myotomy Kos 2008Document7 pagesLX Suspension and UES Myotomy Kos 2008DEVNo ratings yet
- Pemicu 1 Blok GIT: Theffany 405120198 Fakultas Kedokteran Universitas TarumanagaraDocument99 pagesPemicu 1 Blok GIT: Theffany 405120198 Fakultas Kedokteran Universitas TarumanagaraTheffany KasiranNo ratings yet
- GIT NotesDocument23 pagesGIT NotesGrey SyNo ratings yet
- Anatomy & Physiology of PharynxDocument22 pagesAnatomy & Physiology of PharynxArvind SangaviNo ratings yet
- Swallowing Analyses of Neonates and Infants in Breastfeeding and Bottle-Feeding: Impact On Video Uoroscopy Swallow StudiesDocument11 pagesSwallowing Analyses of Neonates and Infants in Breastfeeding and Bottle-Feeding: Impact On Video Uoroscopy Swallow Studiesantonio gabriel egea castilloNo ratings yet
- Abnormal Swallow Infantile and AdultDocument2 pagesAbnormal Swallow Infantile and Adultfinix33No ratings yet
- Bingo Cards 2x2Document5 pagesBingo Cards 2x2Marta Pérez MadridNo ratings yet
- NCP On SahDocument21 pagesNCP On SahDr-Sanjay SinghaniaNo ratings yet
- Speech and Language Therapy Exercises - vn2 A5Document8 pagesSpeech and Language Therapy Exercises - vn2 A5Mian Imran IqbalNo ratings yet
- Dysphagia Diagnosis 1and Treatment (Olle Ekberg) (Z-Lib - Org) (1) - 83-284Document202 pagesDysphagia Diagnosis 1and Treatment (Olle Ekberg) (Z-Lib - Org) (1) - 83-284Macarena Paz ÁlvarezNo ratings yet
- DysphagiaDocument8 pagesDysphagiaDini MarsyaNo ratings yet