Professional Documents
Culture Documents
Investigations Must Be Within 6 Months of Date of Referral: NCL Alcohol Pathway
Investigations Must Be Within 6 Months of Date of Referral: NCL Alcohol Pathway
Uploaded by
jyothi vallabhaneniOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Investigations Must Be Within 6 Months of Date of Referral: NCL Alcohol Pathway
Investigations Must Be Within 6 Months of Date of Referral: NCL Alcohol Pathway
Uploaded by
jyothi vallabhaneniCopyright:
Available Formats
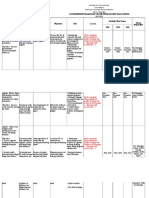
Latest Version Final version February 2023
Previous December 2013, February 2016, February
Versions 2019 “Must do” actions for GP’s / (Triaged
Pi
by RSS)
Review Date February 2026
B Recommendations for Primary Care
Approving Body NCL ICB CAG R Red flag / urgent referral
Adult Abnormal Liver Function Tests Primary Care NCL-Wide /
Borough(s) NCL-Wide O Routine referral
Clinical Pathway Author(s) Dr Nick Dattani, Louis China, Douglas
P Public health intervention
Macdonald G Audio-visual aids for patients and GP
For any queries regarding the content of this document e-mail: nclicb.pathways@nhs.net Click icon for clinical evidence
1.0 (B) Right-click to use hyperlink
Patient has Abnormal LFTs:
Note: Alpha-numeric step references are
History and Examination with attention to Alcohol consumption, Metabolic
to aid printing in black & white and colour
Syndrome, BMI, blindness
Hepatotoxic Drugs &
test for HBsAg and HCV Ab
Investigations must be within 6
months of date of referral
2.0 (R) 3.0 (B) 4.0 (B) 5.0 (B)
Isolated Raised Normal Bilirubin with Normal Bilirubin with
Jaundice (Bil>40) and/or Bilirubin with other Hepatitic LFTs Cholestatic LFTs
significantly abnormal normal LFTs (ALT>ALP) (ALP>ALT)
LFTs and/or Liver aetiology
Concerns re↓albumin or suggested by ↑GGT
prolonged INR (if done) otherwise organise bone
7.0 (B) 9.0 (B) 10.0 (R)
Suspected malignancy aetiology and check
Most commonly due to Gilbert’s Vitamin D)
syndrome (unconjugated ALT<300 IU/L ALT>300 IU/L
hyperbilirubinaemia - affects
5% of the population and is
benign)
6.0 (R) 11.0 (Pi) 12.0 (R)
Less commonly due to
haemolysis Seek telephone
Urgent Ultrasound and/or
advice with on-call
Urgent 2 week referral or
medical team or
admission to appropriate Repeat within one month
8.0 (B) 8.1 (G) hepatology team
specialty with AST ,GGT, FBC to confirm
depending on
Repeat LFTs still elevated
availability
fasting sample Consider HCV and HBV
with split If alcohol consumption >14U/
bilirubin and Week advice and review NCL
13.0 (Pi)
FBC. Consider Alcohol Pathway [2]
reticulocytes Consider Ultrasound
and LDH if Advice and
haemolysis Guidance
suspected. If in doubt
If Gilbert’s
confirmed then
inform patient If abnormal
and provide
information [1]
14.0 (Pi)
Ultrasound & request Extended
Liver Test Panel which
includes:
• Hepatitis B & C
• Autoantibodies (ANA, USS Normal
AMA, smooth muscle Ab,
LKM*)
• Ferritin / Transferrin satn
• Caeruloplasmin USS abnormal
• Immunoglobulins
• A1 antitrypsin
• also HBA1c
Abnormal USS
Isolated raised LFTs but
appearances and/or
normal USS and Panel
Abnormal Liver Test Panel
15.0 (B) 16.0 (B) 17.0 (G)
If clinically appropriate seek
Manage in Primary Care: Fatty Liver Suggested by USS and Advise & Guidance
Lifestyle advice and repeat LFTs in 1 year Extended Liver Test Panel Negative for Refer to Liver Specialist for
other Pathology Page 2 (Fatty Liver) possible:
(if remains abnormal to Advice and • Viral Hepatitis
Guidance) • ALD with Advanced
Fibrosis
15.1 (G)
• PSC, PBC, Autoimmune
Hepatitis
• Gallstone disease
• Hepatic Vascular Disorders
• Hepatic Metabolic
Disorders
17.1 (O)
18.0 (R)
Consider urgent referral
pathway as clinically
appropriate
Consider doing LFTS
• if sx of liver/bile system disease e.g. abdo pain/nausea/vomiting/jaundice/fatigue/anorexia
• pt drinks excessively
• pt taking medication that affects the liver
• pt has diabetes or other metabolic disorder
• obesity
• GGT – useful in cholestasis or monitoring
• changes in alcohol consumption
Please note - LFTS are normal in up to 25% patients with cirrhosis. If If there are risk factors for liver disease (e.g. harmful alcohol, viral hepatitis) please test according to the relevant pathway.
[1] Gilberts’s Syndrome
http://www.nhs.uk/conditions/gilbertssyndrome/Pages/Introduction.aspx
[2] NCL Alcohol Pathway
[EDITING NOTE: To add in URL for NCL alcohol pathway once uploaded onto GP website]
*LKM=liver & kidney microsomal Ab
AMA = mitochondrial antibody
ANA = anti nuclear Ab
You might also like
- Chocolate Causes Weight LossDocument8 pagesChocolate Causes Weight LossGawker.com83% (6)
- F45 Recovery Catalogue V1.4Document9 pagesF45 Recovery Catalogue V1.4Sylvester JaiyeolaNo ratings yet
- NRS 490 RS LiteratureEvaluationTableDocument6 pagesNRS 490 RS LiteratureEvaluationTableHw Solution100% (14)
- Pickhardt 2020 Positive Oral Contrast Material For Abdominal CT Current Clinical Indications and Areas of ControversyDocument10 pagesPickhardt 2020 Positive Oral Contrast Material For Abdominal CT Current Clinical Indications and Areas of ControversyLucas ParretNo ratings yet
- NCCN Head-And-neck 2020 Glándulas SalivaresDocument9 pagesNCCN Head-And-neck 2020 Glándulas Salivaresd.ayala1006No ratings yet
- (Summary Report) Drug Rehabilitation Program FinalDocument9 pages(Summary Report) Drug Rehabilitation Program FinalCharrie Mae Mallo100% (1)
- Pre Read On IberogastDocument17 pagesPre Read On Iberogasttranlamtuyen1911No ratings yet
- Updated Mental Health MDM Log Framework FVDocument12 pagesUpdated Mental Health MDM Log Framework FVWikileaks2024No ratings yet
- Demographic Disparities in Unimproved Drinking Water and Sanitation in Ghana. A Nationally Representative Cross-Sectional StudyDocument12 pagesDemographic Disparities in Unimproved Drinking Water and Sanitation in Ghana. A Nationally Representative Cross-Sectional StudyeerhuangaNo ratings yet
- Equality Work Plan PDFDocument16 pagesEquality Work Plan PDFGilbert KamanziNo ratings yet
- Project Brief-CBRP MIOPDocument2 pagesProject Brief-CBRP MIOPJomidy Midtanggal50% (2)
- Nichols Ashp Poster 120219Document1 pageNichols Ashp Poster 120219api-490034937No ratings yet
- Concepcion - Misamis Occidental - CBDRP - 4th Qtr. 2022Document1 pageConcepcion - Misamis Occidental - CBDRP - 4th Qtr. 2022Dilg ConcepcionNo ratings yet
- Contoh Journal Di PDIDocument6 pagesContoh Journal Di PDIAyu Fitri LestariNo ratings yet
- Muscles Where Botox Injection InjectedDocument9 pagesMuscles Where Botox Injection InjectedSylvia GraceNo ratings yet
- Good Pharmacy Practice Assessment Among Community Pharmacies in LebanonDocument11 pagesGood Pharmacy Practice Assessment Among Community Pharmacies in LebanonYusril AhmadNo ratings yet
- Clinical Nursing Concerns For Type 2 Diabetes MellitusDocument2 pagesClinical Nursing Concerns For Type 2 Diabetes MellitusclarimerNo ratings yet
- DR (Surg CDR) Gaurav Narula CAR T-Cells Next Generation Hemat Practice - YHOP 18 PDFDocument59 pagesDR (Surg CDR) Gaurav Narula CAR T-Cells Next Generation Hemat Practice - YHOP 18 PDFSaradha PellatiNo ratings yet
- Bpops Accomplishment Report UpdatedDocument74 pagesBpops Accomplishment Report UpdatedLheonard SapnuNo ratings yet
- Tracy Whyte, Community Physiotherapist, BSC (Hons) NCHC South PlaceDocument1 pageTracy Whyte, Community Physiotherapist, BSC (Hons) NCHC South Placeapi-286232866No ratings yet
- Patrizia Mecocci, Anna Bladstro M and Karina StenderDocument7 pagesPatrizia Mecocci, Anna Bladstro M and Karina StenderDian GbligNo ratings yet
- E052477 FullDocument6 pagesE052477 FullZidna NanaNo ratings yet
- Final - Final Maginhawang Baga Apsr - de LeonDocument12 pagesFinal - Final Maginhawang Baga Apsr - de LeonMaria Lowella de leonNo ratings yet
- Quality Improvement Studies in Pediatric Critical Care MedicineDocument7 pagesQuality Improvement Studies in Pediatric Critical Care MedicinenadiaNo ratings yet
- Global Palliative Care ResearchDocument12 pagesGlobal Palliative Care ResearchTiyen GlandiaNo ratings yet
- Cbydp Model Plan For BarangaysDocument38 pagesCbydp Model Plan For BarangaysJeffrey floresca BulaoNo ratings yet
- Nutrition in Emergencies PlanDocument7 pagesNutrition in Emergencies PlanAimee AkishiaNo ratings yet
- Certification CBRP 2022 - ConcepcionDocument84 pagesCertification CBRP 2022 - ConcepcionDilg ConcepcionNo ratings yet
- Concepcion - Misamis Occidental - CBDRP - 1st Qtr. 2022Document3 pagesConcepcion - Misamis Occidental - CBDRP - 1st Qtr. 2022Dilg ConcepcionNo ratings yet
- Assessment of Benzyl Isothiocyanate As An Adjunct.9Document7 pagesAssessment of Benzyl Isothiocyanate As An Adjunct.9Debjyoti DebnathNo ratings yet
- Concepcion - Misamis Occidental - CBDRP - 3rd Qtr. 2022Document2 pagesConcepcion - Misamis Occidental - CBDRP - 3rd Qtr. 2022Dilg ConcepcionNo ratings yet
- Gender Analysis Context Frameworks and Applications: Gichelle Cruz PCW-NGRP Batch 2Document45 pagesGender Analysis Context Frameworks and Applications: Gichelle Cruz PCW-NGRP Batch 2keith tanuecoNo ratings yet
- Hellicobacter Pylori Quick Reference GuideDocument26 pagesHellicobacter Pylori Quick Reference GuidebiiicaNo ratings yet
- Barangay Peace and Order and Public Safety PlanDocument3 pagesBarangay Peace and Order and Public Safety Plannorie garces100% (1)
- Consumer Insights Update: PZ Cussons Ghana January 2014Document3 pagesConsumer Insights Update: PZ Cussons Ghana January 2014EdemNo ratings yet
- Raising The Awareness About The Importance of Iron in Children in The CommunityDocument51 pagesRaising The Awareness About The Importance of Iron in Children in The CommunityMega LestariNo ratings yet
- LL ALLUZIENCE Liquid Formulation of AbobotulinumtoxinA A 6-MonthDocument13 pagesLL ALLUZIENCE Liquid Formulation of AbobotulinumtoxinA A 6-MonthAnderson GomesNo ratings yet
- Ijic 22 2 6418 s2Document46 pagesIjic 22 2 6418 s2Beaulah HunidzariraNo ratings yet
- Excipients Used in Tablet Formulation Pharmaceutical Information by Charan KarumuriDocument15 pagesExcipients Used in Tablet Formulation Pharmaceutical Information by Charan KarumuriYuppie RajNo ratings yet
- GAD Plan and Budget 2021Document6 pagesGAD Plan and Budget 2021magrocapalonga24No ratings yet
- Edinburgh Rcsed Presentation Governance Healthcare 20220830Document21 pagesEdinburgh Rcsed Presentation Governance Healthcare 20220830Guilherme KlafkeNo ratings yet
- Bmjopen 2017 021414Document9 pagesBmjopen 2017 021414aleneNo ratings yet
- 7 RM 2017 2022 Chapter 7 - As of 20171010Document2 pages7 RM 2017 2022 Chapter 7 - As of 20171010ianNo ratings yet
- Behavior Change Communication For Urban Health A Situation AssessmentDocument57 pagesBehavior Change Communication For Urban Health A Situation AssessmentAmit PaliwalNo ratings yet
- Target Population - Health Assessment Matrix - 2021 - 220628 - 092416Document1 pageTarget Population - Health Assessment Matrix - 2021 - 220628 - 092416Reza ApriansyahNo ratings yet
- 3 - NCG - INDIA - Rev - Preventive Oncology - Primary - CareDocument33 pages3 - NCG - INDIA - Rev - Preventive Oncology - Primary - Carenadeem khanNo ratings yet
- ET Health Page-1Document1 pageET Health Page-1Kdmfuffad liNo ratings yet
- Pregnancy Bukan JurnalDocument2 pagesPregnancy Bukan JurnalClaudia LisaniNo ratings yet
- Definitions of PHC ExpendituresDocument9 pagesDefinitions of PHC ExpendituresJean M Huaman FiallegaNo ratings yet
- 3 Leadership and GovernanceDocument39 pages3 Leadership and GovernanceayeleNo ratings yet
- Wilson David Benchmark Indicators PresentationDocument26 pagesWilson David Benchmark Indicators PresentationKristin Faye OlaloNo ratings yet
- Day 1 - Thursday - 1030 AM - Andrew BucklerDocument21 pagesDay 1 - Thursday - 1030 AM - Andrew BucklerPrevent Cancer FoundationNo ratings yet
- 4 Community-Oriented-Primary-Care-Reviewer - NSoriano.v112020Document8 pages4 Community-Oriented-Primary-Care-Reviewer - NSoriano.v112020Mauri ChuaNo ratings yet
- RHU Exit Report: Alfonso: UPCM Class 2020Document98 pagesRHU Exit Report: Alfonso: UPCM Class 2020makabayan san juanNo ratings yet
- 2022 BMJ Open - Models of Care For Low Back PainDocument7 pages2022 BMJ Open - Models of Care For Low Back PainMiguel Arévalo-CárdenasNo ratings yet
- 3 RD JC PDF - SindhuDocument18 pages3 RD JC PDF - SindhuDadi SindhuNo ratings yet
- Social Prescribing - Less Rhetoric and More EvidenceDocument17 pagesSocial Prescribing - Less Rhetoric and More EvidenceScribdNo ratings yet
- Symposium Board 1Document1 pageSymposium Board 1api-482373029No ratings yet
- Https - WWW - Ncbi - NLM - Nih - Gov PMC Articles PMC4716702Document13 pagesHttps - WWW - Ncbi - NLM - Nih - Gov PMC Articles PMC4716702dori sanchezNo ratings yet
- Sample Accomplishment ReportDocument2 pagesSample Accomplishment ReportLaurie Angela AgatiNo ratings yet
- A. LguDocument719 pagesA. Lgunathan carreonNo ratings yet
- Cystic Fibrosis Case StudyDocument5 pagesCystic Fibrosis Case StudyCLAIRE BLANCHE PABONNo ratings yet
- Diastolic Heart Failure AssessmentDocument16 pagesDiastolic Heart Failure AssessmentMd. ashfaque Ahemmed khanNo ratings yet
- Pharmaceutical Specialty Sales Manager in Cleveland Akron OH Resume William WegrynDocument2 pagesPharmaceutical Specialty Sales Manager in Cleveland Akron OH Resume William WegrynWilliamWegrynNo ratings yet
- Non-Melanoma Skin Cancer of The Head and Neck 2015Document214 pagesNon-Melanoma Skin Cancer of The Head and Neck 2015Alejandro Santini BlascoNo ratings yet
- Hepatotoxicity Induced by Greater CelandineDocument7 pagesHepatotoxicity Induced by Greater CelandineGabrielAbarcaNo ratings yet
- The Immune System: Morphofunctional Peculiarities, Methods of Examination, Semiology of DiseasesDocument45 pagesThe Immune System: Morphofunctional Peculiarities, Methods of Examination, Semiology of DiseasesHIDE & ATTACKNo ratings yet
- Vaccine Research StatusDocument112 pagesVaccine Research StatusJunko Tsukuda100% (1)
- The History of Surgical Anesthesia PDFDocument276 pagesThe History of Surgical Anesthesia PDFRui Pereira100% (2)
- Integrative Medicine and Patient Centered Care PDFDocument35 pagesIntegrative Medicine and Patient Centered Care PDFCristobal Carrasco100% (1)
- Dental ReviewDocument361 pagesDental ReviewSonia LeeNo ratings yet
- Marshman Counseling ResumeDocument1 pageMarshman Counseling Resumeapi-598396829No ratings yet
- Digesting Light and ColorDocument3 pagesDigesting Light and ColorMunirah KasimNo ratings yet
- Case Study TBDocument8 pagesCase Study TBCesar Emmanuel Abigania100% (2)
- Worksheet in HCX - Absence - BRANCHES (1) (AutoRecovered)Document66 pagesWorksheet in HCX - Absence - BRANCHES (1) (AutoRecovered)Christian de LunaNo ratings yet
- 33 Diagnosis Keperawatan Jiwa NANDADocument1 page33 Diagnosis Keperawatan Jiwa NANDAAnonymous W09Ufp8VJNo ratings yet
- Sample Health Teaching PlanDocument1 pageSample Health Teaching PlanGia Espinosa OcbeñaNo ratings yet
- LevetiracetamDocument3 pagesLevetiracetamGwyn Rosales100% (2)
- Ra CatalogueDocument24 pagesRa CatalogueauliaiNo ratings yet
- Research Paper On The Benefits of ExerciseDocument8 pagesResearch Paper On The Benefits of Exercisegxuqjkhkf100% (1)
- Clinical Manifestations, Prevention and Treatment of Stroke in WomenDocument6 pagesClinical Manifestations, Prevention and Treatment of Stroke in WomenCentral Asian StudiesNo ratings yet
- English CatalogDocument29 pagesEnglish CatalogMarcos RojasNo ratings yet
- Askep Tumor Wilms: Ni Nyoman Udiani, S.Kep - Ns.,M.KepDocument36 pagesAskep Tumor Wilms: Ni Nyoman Udiani, S.Kep - Ns.,M.KepRelysa Magdalena IssiNo ratings yet
- ADHD Guidance-September 2013Document6 pagesADHD Guidance-September 2013Claude JousselinNo ratings yet
- Superwarfarin:: A Wifes Means To An Evil EndDocument14 pagesSuperwarfarin:: A Wifes Means To An Evil EndgarciamattNo ratings yet
- Diet Restrictions and Exercise in Metas Breadt CancerDocument14 pagesDiet Restrictions and Exercise in Metas Breadt CancerNurul Fatimah MaulaNo ratings yet
- Anestesia CardDocument4 pagesAnestesia CarderyxspNo ratings yet
- Cantollas, Vea Ann A. - Resume 1Document1 pageCantollas, Vea Ann A. - Resume 1Vea Ann CantollasNo ratings yet
- Pulmonary Function TestsDocument29 pagesPulmonary Function TestsOrion JohnNo ratings yet