Professional Documents
Culture Documents
MSI CA Checklist - Counselling v4.0
MSI CA Checklist - Counselling v4.0
Uploaded by
Abubakar JallohOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MSI CA Checklist - Counselling v4.0
MSI CA Checklist - Counselling v4.0
Uploaded by
Abubakar JallohCopyright:
Available Formats
MSI Competency Assessment Checklist: Counselling
Clinical Staff Name: ______________________ Designation: ______________________
General Counselling Pre-Procedure Yes/No/NA Notes
1. * Maintains privacy and confidentiality
2. Greets and employs a client-centred style of communication when
speaking to clients
3. Uses language the client is comfortable with
4. * Follows a structured counselling approach like REDI (Rapport,
Explore, Decide and Implement) or according to local protocols
5. * Asks client about the service(s) they are seeking and if they have
something specific in mind
6. * Provides comprehensive and correct information on service
options that fits with client's reproductive health needs and
lifestyle preferences
7. * Explains dual protection to clients
8. Uses flipchart or other job aids appropriately to explain service
options
9. * Supports clients to make own decisions after weighing up all
information including advantages, disadvantages and
consequences of each option
10. * Explains how the chosen service would be provided; its side
effects; and possible complications which may require referral
to higher level facility in rare cases
11. Checks that client fully understands the chosen option by asking
them to repeat key points
12. * Checks that client’s decision for chosen service is voluntary
13. * Takes informed consent appropriately with consideration for
vulnerable groups such as young people; illiterate; clients with
history of sexual abuse or violence, long term physical, mental,
intellectual or sensory impairments and mental health illness
14. * Documents written informed consent appropriately as per MSI/
local protocols
MSI Competency Assessment Checklist: Counselling v4.0 Page 1 of 4
15. Indicates how and where to access the chosen service.
If appropriate, discusses scheduling; and interim or partner
contraception
Method-Specific Counselling Yes/No/NA Notes
TUBAL LIGATION
16. * Emphasises that although tubal ligation is a permanent method
there is a very small chance of failure
17. If postpartum, discusses with the client if their decision would
change if the baby were to die or suffer from health problems
VASECTOMY
18. * Emphasises that although vasectomy is a permanent method
there is a very small chance of failure
19. * Explains that the method will become effective only after 3
months so an additional contraceptive method will be required
during this time
IUD/IUS
20. * Emphasises that IUD/IUS are long acting reversible
contraceptives that are very effective
21. Explains that the client can switch method if unhappy with the
method
IMPLANTS
22. * Emphasises that implants are long acting reversible
contraceptives that are very effective
23. Explains that the client can switch method if unhappy with the
method
PROGESTIN-ONLY INJECTABLE
24. Emphasises that progestin-only injectable is a reversible
contraceptive with a very small chance of failure if the injection
is repeated at the right time
25. Explains that after stopping the injection there may be a delay
in return to fertility of up to one year
ORAL CONTRACEPTIVE PILL
MSI Competency Assessment Checklist: Counselling v4.0 Page 2 of 4
26. * Emphasises that oral contraceptive pills are short acting
contraceptives with a small chance of failure if the pill is taken
correctly
27. Explains hormonal side effects and risks associated with taking
oestrogen
CONDOM
28. Emphasises that a new condom needs to be used correctly for
every sexual encounter for maximum effectiveness
29. Emphasises that condoms are the only contraceptive method that
can protect against both pregnancy and sexually transmitted
infections and HIV
EMERGENCY CONTRACEPTION
30. * Explains that emergency contraception (EC pill and copper
IUD) helps to prevent pregnancy when taken up to 5 days after
unprotected sex but the sooner they are taken, the more
effective they will be
31. Explains that emergency contraceptive pills (ECPs) will not
protect from pregnancy from any episodes of unprotected sex
that occur after they take the ECPs
SAC/ PAC
32. * Emphasises key characteristics of SAC/PAC option chosen
33. * Explores PAFP needs and explains options
General Counselling: Post-Procedure Yes/No/NA Notes
34. * Provides post procedure instructions orally and in writing if
possible for the following:
• Follow-up care
• Follow-up visits where required or as per local protocols
• To return or call any time for advice or medical attention
• Warning signs and what to do in such cases
• Contact number (preferably 24/7) for any emergency related to
the service
35. Discusses arrangement for discharge (e.g. person accompanying
client to home)
MSI Competency Assessment Checklist: Counselling v4.0 Page 3 of 4
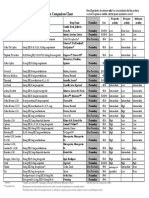
Result of Competency Assessment
* Attach Competency Assessment Checklist if clinical staff is assessed as level 2
Service Assessed: Counselling Tick as
appropriate
Level 1
• Individual completed all steps correctly.
• Competent to provide this service independently subject to regular re-assessment.
Level 2 *
• Individual missed one or more of the steps.
• Cannot provide this service independently. Must offer this service only under direct
supervision of a competent clinical staff till endorsed as fully competent by the
competent clinical staff.
Other observations:
Specify actions to be taken to achieve/maintain competency:
Clinical Staff Name: Clinical Staff Signature:
Competency Assessor Name: Competency Assessor Signature:
Date of Assessment: Location:
MSI Competency Assessment Checklist: Counselling v4.0 Page 4 of 4
You might also like
- Nclex ExamDocument164 pagesNclex ExamZara Andrei100% (17)
- Credentialing and PrivilegingDocument113 pagesCredentialing and PrivilegingRobert Montuya100% (2)
- IV Study Guide 2013Document78 pagesIV Study Guide 2013Kaloy KamaoNo ratings yet
- Human Sexuality in A Changing World 10th Edition.c2Document625 pagesHuman Sexuality in A Changing World 10th Edition.c2jake100% (1)
- DEVELOPING PHYSIOTHERAPY LED SHOULDER CLINICS: A PROPOSAL TO ADJUST SCOPE OF PRACTICE BY TENDAYI MUTSOPOTSI Bsc. HPT (Hons) MSc. ORTHO-MEDDocument15 pagesDEVELOPING PHYSIOTHERAPY LED SHOULDER CLINICS: A PROPOSAL TO ADJUST SCOPE OF PRACTICE BY TENDAYI MUTSOPOTSI Bsc. HPT (Hons) MSc. ORTHO-MEDPhysiotherapy Care SpecialistsNo ratings yet
- DefensibleDocumentationElements PDFDocument2 pagesDefensibleDocumentationElements PDFdr_finch511No ratings yet
- NBME OBGYN2 6 Wrong With Answers SearchableDocument50 pagesNBME OBGYN2 6 Wrong With Answers Searchabledramcdover96% (26)
- Legal and Ethical Aspects of Critical Care NursingDocument66 pagesLegal and Ethical Aspects of Critical Care NursingJamille Abenir Lopez100% (2)
- DelegationDocument29 pagesDelegationMichelle Soriano100% (1)
- Acute CareDocument88 pagesAcute Caresabrinapaige23100% (1)
- Nursing AuditDocument6 pagesNursing Auditpak huda100% (1)
- Nursing Process QuizDocument8 pagesNursing Process QuizLinda Boeye100% (1)
- Nclex ExamDocument27 pagesNclex ExamNasip MacatoonNo ratings yet
- International Patient Safety Goals IPSGDocument20 pagesInternational Patient Safety Goals IPSGShafique HussainNo ratings yet
- Adaptation Nurse Job DescriptionDocument12 pagesAdaptation Nurse Job DescriptionM LubisNo ratings yet
- Population Dynamics NewDocument169 pagesPopulation Dynamics Newhiral mistry100% (1)
- Restraint Use and Patient Care: Nnual CompetencyDocument35 pagesRestraint Use and Patient Care: Nnual CompetencyrustiejadeNo ratings yet
- Unesco Als Ls2 Science m06 (v3.2)Document64 pagesUnesco Als Ls2 Science m06 (v3.2)als midsayap1100% (1)
- B) Reassurance That This Is Normal InitiallyDocument51 pagesB) Reassurance That This Is Normal InitiallygofisheeNo ratings yet
- Postoperative Management in AdultsDocument58 pagesPostoperative Management in AdultsAjay KumarNo ratings yet
- NP 1 Top SecretDocument14 pagesNP 1 Top SecretJomar ValdezNo ratings yet
- NCLEX-RN Exam Prep 2024-2025: 500 NCLEX-RN Test Prep Questions and Answers with ExplanationsFrom EverandNCLEX-RN Exam Prep 2024-2025: 500 NCLEX-RN Test Prep Questions and Answers with ExplanationsNo ratings yet
- Test Bank Medical Surgical Nursing Making Connections To Practice 2nd Edition Hoffman SullivanDocument24 pagesTest Bank Medical Surgical Nursing Making Connections To Practice 2nd Edition Hoffman SullivanCathy Guajardo100% (32)
- Handouts-Standards of Professional Care in Intravenous TherapyDocument13 pagesHandouts-Standards of Professional Care in Intravenous TherapyTony DemaguilNo ratings yet
- Ethico-Legal Relevant To Health AssessmentDocument13 pagesEthico-Legal Relevant To Health AssessmentLorelie Asis80% (15)
- CV TemplateDocument21 pagesCV TemplateUmair ZubairNo ratings yet
- MSI CA Checklist - Counselling v3.0Document4 pagesMSI CA Checklist - Counselling v3.0Abubakar JallohNo ratings yet
- MSI CA Checklist - Emergency Contraception v1.0Document2 pagesMSI CA Checklist - Emergency Contraception v1.0Abubakar JallohNo ratings yet
- MSI CA Checklist - Hormonal Contraceptive Pills, Rings and Patches v1.0Document3 pagesMSI CA Checklist - Hormonal Contraceptive Pills, Rings and Patches v1.0Abubakar JallohNo ratings yet
- Learning Guides and Practice Checklists For Male Circumcision Counselling and Clinical SkillsDocument79 pagesLearning Guides and Practice Checklists For Male Circumcision Counselling and Clinical SkillsDomenico BevilacquaNo ratings yet
- Referral-Process SystemDocument40 pagesReferral-Process SystemCommunity B100% (1)
- Bahasa Inggris Bu YuliDocument8 pagesBahasa Inggris Bu YuliNova FitriaNo ratings yet
- Policy For Patients Requiring One To One ObservationDocument25 pagesPolicy For Patients Requiring One To One ObservationAshraf MullaNo ratings yet
- Explain How You Evaluate Your Own Work and Why It Is Necessary To Do SoDocument4 pagesExplain How You Evaluate Your Own Work and Why It Is Necessary To Do Solilbimbow100% (5)
- Family PlanningDocument6 pagesFamily PlanningShadrackNo ratings yet
- 04 Urinalysis CompetencyDocument20 pages04 Urinalysis Competencyمحمد عبدالواسع المسنيNo ratings yet
- Arero Primary Hospital Consultation ProtocolDocument16 pagesArero Primary Hospital Consultation Protocolsami ketema100% (4)
- Obstetric CA Guidance Document v1.0Document40 pagesObstetric CA Guidance Document v1.0Daniel AbomaNo ratings yet
- Clinic VisitDocument4 pagesClinic VisitHAMIMA PANDAPATANNo ratings yet
- - - ادارة فاينل -Document103 pages- - ادارة فاينل -Alaa OmarNo ratings yet
- نماذج امتحانات اساسيات تمريضDocument84 pagesنماذج امتحانات اساسيات تمريضalwasam55No ratings yet
- Domain 3 ReviewDocument65 pagesDomain 3 ReviewKHALED ANo ratings yet
- Certified Nurse Midwife Delineation PrivilegesDocument6 pagesCertified Nurse Midwife Delineation PrivilegesKesavan Anandha KumarNo ratings yet
- G - GTN IV Infusion MX Nps 2015 v4Document12 pagesG - GTN IV Infusion MX Nps 2015 v4sizaNo ratings yet
- Venepuncture Delegate Notes 0118Document27 pagesVenepuncture Delegate Notes 0118Rohit ShindeNo ratings yet
- Medical ChaperoneDocument8 pagesMedical ChaperoneMd Anwar ShahadatNo ratings yet
- Lemone/Burke/Bauldoff, Medical-Surgical Nursing 6Th Edition Test BankDocument61 pagesLemone/Burke/Bauldoff, Medical-Surgical Nursing 6Th Edition Test Banknurse homeNo ratings yet
- Referral Systems For HEWDocument39 pagesReferral Systems For HEWmohammed AminNo ratings yet
- Referralsystem 161202080450Document21 pagesReferralsystem 161202080450DRx Sonali Tarei100% (1)
- N34 Roles of The RN by BRNDocument8 pagesN34 Roles of The RN by BRNhameunjungNo ratings yet
- Nterdisciplinary Project With Professor FeebackDocument16 pagesNterdisciplinary Project With Professor Feebackapi-627301337No ratings yet
- Module 3 FP Client AssessmentDocument54 pagesModule 3 FP Client AssessmentJhunna TalanganNo ratings yet
- Policy On Break From PracticeDocument6 pagesPolicy On Break From Practicedr.mzmheNo ratings yet
- Covid 19 Guideline For Nutrition ManagementDocument17 pagesCovid 19 Guideline For Nutrition ManagementEdoardo Dalla NoraNo ratings yet
- Clinical Practice GuidelineDocument16 pagesClinical Practice GuidelinerazeghiNo ratings yet
- Opioids - Emergency Department Prescribing 11-22-2013Document3 pagesOpioids - Emergency Department Prescribing 11-22-2013api-240943284No ratings yet
- NURSING PROCEDURES FOR CHN Converted 1Document25 pagesNURSING PROCEDURES FOR CHN Converted 1Genki Fay B. Lequigan100% (1)
- Policy For Handling Storage and Administration of Medicines Within Residential HomesDocument114 pagesPolicy For Handling Storage and Administration of Medicines Within Residential Homesdoctor uroosaNo ratings yet
- Moultonfinal OctDocument10 pagesMoultonfinal Octapi-283173905No ratings yet
- Directives: PR Actice GuidelineDocument8 pagesDirectives: PR Actice GuidelineJanine AndersonNo ratings yet
- Chapter 018Document18 pagesChapter 018dtheart2821100% (2)
- JCI Newsletter May 8 IPSGDocument6 pagesJCI Newsletter May 8 IPSGAhmad HaririNo ratings yet
- Design, Evaluation, and Translation of Nursing InterventionsFrom EverandDesign, Evaluation, and Translation of Nursing InterventionsNo ratings yet
- Natural and Artificial Methods of ContraceptionDocument40 pagesNatural and Artificial Methods of ContraceptionelynNo ratings yet
- "Rape-Adjacent": Imagining Legal Responses To Nonconsensual Condom RemovalDocument28 pages"Rape-Adjacent": Imagining Legal Responses To Nonconsensual Condom RemovalLarryDCurtisNo ratings yet
- Moral and Non-Moral Standards in The PhilippinesDocument7 pagesMoral and Non-Moral Standards in The PhilippinesNeil Harbee AquaticsNo ratings yet
- Notes of Sexual & Adolescent Reproductive Health From Lecturer, Year 4 Upgrading, 2019-2020Document35 pagesNotes of Sexual & Adolescent Reproductive Health From Lecturer, Year 4 Upgrading, 2019-2020SONGA AmriNo ratings yet
- Community MedicineDocument24 pagesCommunity MedicineSrinidhi Nandhini PandianNo ratings yet
- Contraceptive Comparison ChartDocument1 pageContraceptive Comparison ChartdryasirsaeedNo ratings yet
- Apa Essay FormatDocument11 pagesApa Essay FormatMeranda M ChaviraNo ratings yet
- Status Quo Ante: The Elements of The RH LawDocument2 pagesStatus Quo Ante: The Elements of The RH LawPandie yenNo ratings yet
- Saw Palmetto - MedlinePlus SupplementsDocument6 pagesSaw Palmetto - MedlinePlus SupplementsjonascarvNo ratings yet
- Position PaperDocument3 pagesPosition PaperAravela Liwag GillacoNo ratings yet
- Contraceptive Scenario in IndiaDocument17 pagesContraceptive Scenario in IndiaAnand DasNo ratings yet
- AbortionDocument14 pagesAbortionRizabel VillapandoNo ratings yet
- Exam 03.2017 FullDocument50 pagesExam 03.2017 Fullmichal ben meronNo ratings yet
- Family Planing and HomosexualityDocument10 pagesFamily Planing and HomosexualityMansour NyangNo ratings yet
- Population Dynamics, Environment and Poverty - Revised 2013Document202 pagesPopulation Dynamics, Environment and Poverty - Revised 2013jtmukui2000No ratings yet
- 2015 World Population Data Sheet - Eng PDFDocument23 pages2015 World Population Data Sheet - Eng PDFFlorin CiucăNo ratings yet
- Family PlanningDocument16 pagesFamily PlanningAnas Abdul SalamNo ratings yet
- Documents HUMSS C GROUP 3Document10 pagesDocuments HUMSS C GROUP 3jerica joaquinNo ratings yet
- Breast Pain - History TakingDocument6 pagesBreast Pain - History TakingValencia FooNo ratings yet
- Reproductive Health LectureDocument12 pagesReproductive Health Lecturebanana cueNo ratings yet
- Sex Guide For The YoungDocument12 pagesSex Guide For The YoungValarie WalkerNo ratings yet
- Lesthaeghe PDR 2010Document42 pagesLesthaeghe PDR 2010Marta GomezNo ratings yet
- 16 Reproduction Notes Igcse BiologyDocument29 pages16 Reproduction Notes Igcse Biologyasmatullahmohammed2No ratings yet
- Gyne & Obes. Step.1st BitsDocument70 pagesGyne & Obes. Step.1st BitsSkyNo ratings yet
- Health 8 WK 8 Final VersionDocument4 pagesHealth 8 WK 8 Final VersionMarlon Joseph D. ManzanoNo ratings yet