Professional Documents
Culture Documents
Ped.s2.nng.12.jaundice Pallor and Bleeding
Uploaded by
Lara Patricia TamsiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ped.s2.nng.12.jaundice Pallor and Bleeding
Uploaded by
Lara Patricia TamsiCopyright:
Available Formats
PEDIA 2 • PEDIATRICS II • DIDACTIC PEDIATRICS • MODULE 4 • Neonatology, Nephrology, Genetics & Metabolism (NNG)
SHIFT
JAUNDICE PALLOR AND BLEEDING
2
Wilfredo R. Santos, MD December 12, 2022 LEC #12
● Compete with the binding sites of bilirubin with albumin
LECTURE OUTLINE
High altitude
I. Neonatal Jaundice VI. Management of Neonate with ● Polycythemia(hyperviscosity of the blood)
A. Risk Factors for Elevated Significant Jaundice ● Male sex
Indirect Bilirubin A. Phototherapy ● Trisomy 21
B. Bilirubin Metabolism B. Exchange Transfusion ○ Due to hypothyroidism
C. Unconjugated C. Drugs ○ Thyroid hormone is important in RBC integrity
Hyperbilirubinemia VII. Kernicterus ● Cutaneous Bruising and cephalhematoma
D. Causes of Neonatal Jaundice A. Pathophysiology ● Oxytocin Induction
II. Non-Pathologic Causes of Neonatal B. Signs and Symptoms ○ During labor, oxytocin causes rupture of RBCs.
Jaundice C. Prevention ● Weight Loss
A. Physiologic Jaundice VIII. Hemorrhagic Disease of the ● Delayed Bowel Movements
B. Jaundice Associated With Newborn ● Family history or sibling with physiologic jaundice
Breastfeeding A. Vitamin K Deficiency Bleeding
III. Pathologic Causes of Neonatal (VDKB)
B. BILIRUBIN METABOLISM
Jaundice B. Disseminated Intravascular
A. Increased Production of Coagulopathy
Bilirubin IX. Hematologic Disease in the
B. Decreased Clearance in Neonate
Bilirubin A. Neonatal Anemia
C. Disorders of Conjugation B. Neonatal Polycythemia
IV. Hemolytic Disease of Newborn X. Swallowed Blood Syndrome
A. ABO Incompatibility XI. Plethora in the Newborn Infant
B. RH Incompatibility XII. References
V. Laboratory Evaluation XIII. Review Questions
A. Evaluation of Neonate with XIV. Freedom Wall
Significant Jaundice
important/must know book previous trans lecturer’s key points
I. NEONATAL JAUNDICE
Figure 2. Bilirubin Metabolism
● Sources of heme:
○ 25% from ineffective erythropoiesis due to immature liver and bone
marrow
○ 75% from catabolism of old RBCs
● Once released, heme is acted upon by heme oxygenase (rate-limiting
enzyme) → biliverdin
○ Acted upon by biliverdin reductase → bilirubin
Figure 1. Lower left: Normal, Lower Right: Slightly Plethoric, Upper Right: Jaundiced, ● ● Bilirubin binds to serum albumin and travels to the smooth ER (SER) of
Upper Left: Normal with erythema on body hepatocytes.
○ However, albumin cannot enter the hepatocytes (it is a large substance)
● Condition Marked by High Levels Of Bilirubin In The Blood ○ To be able to enter the SER, bilirubin is taken up by ligandin.
○ Increased bilirubin will cause a yellowish discoloration of skin, ● Conjugation takes place in the SER, facilitated by
sclerae,mucus membranes UDP-glucuronosyltransferase to produce bilirubin glucuronide aka B2 or direct
● 2 Types of Jaundice based on VandenBerg reaction: bilirubin (process: double conjugation)
○ Direct bilirubin – greenish or muddy yellow cast ● Bilirubin Glucuronide is then acted upon by Beta-glucuronidase to become the
○ Indirect bilirubin – bright yellow or orange unconjugated bilirubin that enters the enterohepatic circulation.
● Observed During The 1st week after birth: ○ Used up to be conjugated again in the liver
○ 60% of term babies ● Majority are excreted in the feces as stercobilin and in the urine urobilin,
○ 80% of preterm neonates (more marked jaundice) respectively.
● Results from the accumulation of unconjugated, indirect,nonpolar, lipid-soluble
bilirubin pigment (B1 or Indirect) C. UNCONJUGATED HYPERBILIRUBINEMIA
○ Maybe partly caused by deposition of pigment from conjugated, polar, or
water-soluble bilirubin (B2 or direct) ● May be caused or increased by any factor that:
● Unconjugated bilirubin has the end-product of heme protein catabolism ○ Increases load of bilirubin to be metabolized by the liver (Hemolytic
anemia, polycythemia)
○ Damages or reduces the activity of the transferase enzyme (hypoxia,
A. RISK FACTORS FOR ELEVATED INDIRECT BILIRUBIN infection, thyroid deficiency)
● Maternal Age ○ Competes or blocks the transferase enzyme (drugs)
○ Because of presence of maternal comorbidities and illnesses ○ Leads to an absence or decrease amount of enzyme or reduction of
● Race (Chinese, Korean, Japanese, Native Americans) bilirubin uptake (genetic defect and prematurity)
● Maternal Diabetes
○ Infants of diabetic mothers can have hypoglycemia, which is also a risk D. CAUSES OF NEONATAL JAUNDICE
factor for jaundice
● Prematurity ● Toxic effects are increased by
○ Due to a premature liver that is unable to conjugate bilirubin ○ Hypoproteinemia
● Drugs(Vit.K, Novobiocin, Ceftriaxone, Sulfonamides) ■ Bilirubin should bind with albumin
OFFICIAL TRANS BATCH 2024 1
■ Free bilirubin -enter the blood brain barrier neonates.
○ Competitive binding of drugs (sulfonamides, ceftriaxone) 1. HOW TO DIAGNOSE: CAUSES
○ acidosis/ asphyxia
● Appearing within 24 hours of age
■ Penetrable BBB
○ Hemolytic disease of the newborn: Rh, ABO and minor group
○ Hypoglycemia
incompatibility.
○ Hypothermia
○ Infections: intrauterine viral, bacterial, malaria
○ Sepsis
○ G6PD deficiency
● Appearing between 24-72 hours of life
Physiologic - especially if there is a lack of pertinent PE findings for
pathologic jaundice
■ However, remember that NOT ALL jaundice that occurs between
24-72 hours of life is physiologic.
○ Sepsis neonatorum
○ Polycythemia
○ Concealed hemorrhages: cephalhematoma, subarachnoid bleed, IVH
○ Increased enterohepatic circulation
● Appearing after 72 hours
○ Sepsis neonatorum
○ Neonatal hepatitis
○ Extrahepatic biliary atresia
○ Breast milk jaundice
Figure 3. Factors Causing Increase in Bilirubin (RBC Breakdown, Hypoalbuminemia,
Hypoxia, Acidosis) 2. HOW TO DIAGNOSE: CAUSES
Figure 4. Factors Causing Increase in Bilirubin (Drugs, Hypoalbuminemia, Hypoxia,
Acidosis)
Figure 7. Kramer Grading System.
● Using the Kramer Grading System, you can estimate the bilirubin levels by
inspection of the baby alone.
Figure 5. Factors Causing Increase in Bilirubin (Hypoglycemia, Infection & Inflammation) ○ Face: ~5-6 mg/dL
○ Chest: 8-9 mg/dL
○ Abdomen and upper thigh: ~15 mg/dL
○ Level of the feet: >15 mg/dL
● However, in cases of pallor, the real color of the baby may be masked.
✓ NOTE: The values are approximated by Dr. Santos and may differ from values found in
other references.
II. NON-PATHOLOGIC CAUSES OF NEONATAL JAUNDICE
Figure 6. Factors Causing Increase in Bilirubin (Obstruction, Prolonged NPO)
A. PHYSIOLOGIC JAUNDICE (ICTERUS NEONATORUM)
● Clinical Manifestation ● Time of appearance: usually on the 2nd to 3rd day of life.
○ Jaundice follows a cephalocaudal progression ● Pattern: peak on the 2nd to 4th day of life
○ Jaundice usually begins on the ○ Sometimes peak at the 5th day of life
Face (total serum bilirubin ~5mg/dL) ○ The baby could still be physiologically jaundiced at the 4th day of life due
Midabdomen (TSB ~15 mg/dL) to the peak of hyperbilirubinemia
Feet (TSB 20 mg/dL) ● Duration: disappears on the 5th to 7th day or first week of life
○ It may be present few hours after birth or appear during the neonatal Bilirubin levels
period ○ Rise: <5 mg/dL per 24 hours
○ Unconjugated hyperbilirubinemia is bright yellow or orange ○ Maximum total bilirubin (TB)
○ Direct hyperbilirubinemia is greenish or muddy yellow ■ Full term: <12 mg/dL
■ Preterm: <15 mg/dL
Table 1. Causes of Neonatal Jaundice. ○ B2: <2 mg/dL or <20% of TB
CAUSES OF NEONATAL JAUNDICE Abnormal: if B2 is > 2 mg/dL or >20% of TB
EARLY INTERMEDIATE LATE/PROLONGED ● Causes of Physiologic Jaundice
Hemolytic Causes Physiologic Jaundice Conjugated ○ Increased bilirubin load d/t physiologic increase in RBC mass &
● Rh incompatibility Breastfeeding Jaundice hyperbilirubinemia (dark decrease in RBC life span
● ABO incompatibility Breast Milk Jaundice urine, pale stools ■ Newborns have increased hematocrit (~40 to 50) because of
● G6PD Deficiency Sepsis ● Bile duct obstruction hypoxemia in utero
Hemolysis ● Biliary atresia – Polycythemia In Newborn: Hct>65
Congenital Infection Crigler-Najar Syndrome ● Neonatal hepatitis ■ Life span of fetal RBC: 90 days
● TORCH Polycythemia – Versus adult RBC lifespan: up to 120 days
Cephalhematoma Unconjugated – When they rupture, they would give off heme and would be
Bruises ● Physiologic acted upon by heme oxygenase
● Breast Milk jaundice ○ Decrease Immediate Postnatal Bilirubin Uptake due to decreased
● Infection ligandin activity
● Hypothyroidism ■ Even in term but mostly on preterm there is decreased ligandin
✓ NOTE: Refer to Appendix I for the causes of unconjugated hyperbilirubinemia in activity so there is a reduced conjugating capacity for the liver
OFFICIAL TRANS BATCH 2024 2
○ Hepatic (liver transferase) enzyme immaturity for bilirubin conjugation ● Prematurity
causes increase direct bilirubin ○ Prematurity of the liver would have a lower conjugating capacity
○ Increased enterohepatic circulation due to lack of intestinal flora and ● Inborn Errors Of Metabolism (e.g.,galactosemia)
greater proportion of B-glucuronidase among neonates ● Metabolic-Congenital Hypothyroidism
■ Causes hyperbilirubinemia in babies being treated for sepsis. ○ Thyroid hormones contribute to the integrity of the RBC
○ Presence of indirect bilirubin in the umbilical cord
■ Under normal circumstances, the level of IB in the umbilical cord is C. DISORDERS OF CONJUGATION
1-3 mg/dLand rises at a rate of < 5 mg/dL/24 hours
– Explains why physiologic jaundice appears only the 2nd ● Gilbert Syndrome
week of life and peaks on the 4th to 5th week. ○ Mild fluctuating unconjugated hyperbilirubinemia
○ Deficiency or inactivity of bilirubin glucuronyl transferase
■ Only 30% of UGT1A1 is active
B. JAUNDICE ASSOCIATED WITH BREASTFEEDING ○ Congenital or familial disease
○ Exaggerated physiologic jaundice and hyperbilirubinemia of the newborn
1. BREASTFEEDING JAUNDICE
● Crigler-NajjarSyndrome
● Increase bilirubin during the first week of life(usually first 3 days) among fully ○ Familial jaundice
breastfed infants due to both caloric and fluid deprivation ○ Familial nonhemolytic icterus
○ During this time the breast is not producing much milk and is still ○ Types
compatible with the baby because the stomach of the baby is only the ■ Type I: absent UGT1A1
size of a “calamansi”. ■ Type II: deficient UGT1A1
○ During the first 3-5 days of life, babies have decreased intake
○ Affects baby and tends to increase enterohepatic circulation IV. HEMOLYTIC DISEASE OF THE NEWBORN (HDN)
○ Increase indirect bilirubin
● Management: increased breastfeeding frequency A. ABO INCOMPATIBILITY
○ At least 8 to 10x per day
○ Baby should be breastfed until nighttime ● Mother - Blood type O; Baby - Blood type A or B
○ Breastfeed the baby on one breast for 30 mins and then on the other ● Maternal transfer of blood group antibodies against fetal blood type resulting in
side → stimulate release of prolactin and oxytocin → stimulate breast hemolysis of fetal RBCs
milk production ● Mother with O blood type has antibodies of IgG class, which react with A and
● Diagnosis is only for purely breastfed infants B antigens of the baby
● Similar to putting the baby in NPO: decreased peristalsis → increased ● First born is affected
deconjugation by B-glucuronidase ● Manifest with early onset jaundice
● Less severe than Rh incompatibility
● Exchange transfusion may be indicated for severe hyperbilirubinemia
2. BREAST MILK JAUNDICE
Possible adjunct therapy: Metalloporphyrins
● Occurs after the 7th day
○ Maximal jaundice reached during the 2nd to 3rd week
B. Rh INCOMPATIBILITY
● Possible Causes:
○ High levels of glucuronidase facilitating intestinal reabsorption of bilirubin ● Mother: Rh (-) and Baby: Rh (+)
(bilirubin goes back into the enterohepatic circulation) ○ Asians are mostly Rh (+)
○ High concentrations of non-esterified long-chain fatty acids which act as ○ Rh (-) individuals do not have naturally occurring antibodies
inhibitors of hepatic UGT ● Maternal production of antibodies after transplacental exposure to Rh positive
● Pregnanediol inhibits bilirubin conjugation blood then transfer the antibodies to fetal circulation
● Treatment Options ● Prophylactic RhoGAM (Rh Ig) at 28 weeks gestation and delivery
○ Continue breastfeeding & observe ○ OB gives to Rh (-) moms
○ Continue breastmilk feeding and start phototherapy if indicated (e.g., inc ○ Less incidence due to prophylaxis
bilirubin to 25-30 mg/dL after a week) More severe than ABO incompatibility
○ Stop breastfeeding for 48-72 hours if bilirubin levels are critically high (20 RhD is responsible for 90% of Hemolytic Diseases of the Fetus and Newborn
mg/dL) and then treat with phototherapy (not really advised anymore) (HDFN) cases involving the Rh antigen system but other Rh antigens
● Recent literature states that high to critical levels of physiologic breast milk (especially E and c) also can be etiologic.
jaundice can still cause kernicterus especially if the baby has risk factors that Requires Rh-antigen mismatch between the infant and the mother, with prior
may predispose them maternal exposure to RBCs expressing the cognate antigen
Breastfeeding Jaundice: due to feeding problems In short, succeeding pregnancies are affected
● Decreased caloric intake Antigen-antibody reaction causes hemolysis
● Decreased milk supply Hemolysis may happen in utero
Breast Milk Jaundice: there is an innate substance that contribute to the Babies or fetuses with Rh (+) blood may develop hydrops fetalis in utero
jaundice Exchange transfusion may be indicated for severe hyperbilirubinemia
● Substance: non-esterified long chain fatty acids
Table 2. Physiologic vs. Pathologic Jaundice
PHYSIOLOGIC PATHOLOGIC
APpearance After 24 hours Within 24 hours of age
BIli ↑ Increments <5 mg/dL/day >5 mg/dL/day
Peak Term: 4th05th day 1st week (metabolic cause)
Preterm: 7th day
Total Serum Bili <15 mg/dL (usually 0-12 mg/dL) >15 mg/dL
B2: >2 mg/dL or >20% TSB
Duration Clinically not detected after 14 days Jaundice persist after 14 days
Others Usually relates to degree of maturity Stool: clay/white colored
Urine: yellow color may sain
clothes (babies with biliary
atresia)
Figure 8. Rh Incompatibility. Mother is Rh (-) and baby is Rh (+); antibody production;
III. PATHOLOGIC CAUSES OF NEONATAL JAUNDICE baby is then exposed to Rh (-) blood cells and hemolysis occurs. Hydrops fetalis may
● Due to prolonged Indirect Hyperbilirubinemia occur leading to fetal death.
A. INCREASED PRODUCTION OF BILIRUBIN OR BILIRUBIN LOAD ON THE Hemolytic Disease of the Fetus and Newborn
LIVER
Rh Incompatibility
● Hemolytic diseases ○ Sensitization: Rh negative mother + Rh positive first child
○ Rh Incompatibility: Rh (-) mother; Rh (+) baby ■ Fetal-to-maternal transfusion occur only in 50%, hence Rh incompatibility
○ ABO Incompatibility: Type O mother; Type A or B baby does not always lead to Rh sensitization!
● Congenital or inheritable RBC disorders (e.g., Thalassemia, G6PD deficiency)
○ Factors that affect the outcome of antigen-positive fetuses:
○ Affects the integrity of the RBC → easy RBC destruction
■ Differential immunogenicity of blood group Ags (RhD Ag being the most
● Others:
○ Sepsis – toxins of the bacteria may destroy RBC immunogenic)
○ Polycythemia – hyperviscosity ■ Threshold effect of fetomaternal transfusions (a certain amt of
○ Extravascular collection of blood (cephalhematoma) immunizing Ag is red to induce maternal immune response)
■ Not all cephalhematoma would manifest this, but only the large ■ Type of Ab response (IgG crosses placenta)
cephalhematoma has a higher incidence of developing jaundice ■ Differences in maternal immune response
B. DECREASED CLEARANCE OF BILIRUBIN
OFFICIAL TRANS BATCH 2024 3
○ Hydrops fetalis: excessive abnormal fluid in 2 or more fetal compartments expNBS: expanded newborn screen
(sin, pleura, pericardium, placenta, peritoneum, amniotic fluid) results to Blood glucose: look if there is hypoglycemia
death in utero/shortly after birth Ammonia and lactate: manifestations of inborn errors of metabolism
○ Hypoglycemia: hyperinsulinism & hypertrophy of pancreatic islet cells in Blood culture: if suspecting infection
PCR: if suspecting TORCH infection
infants with severe HDFN
○ Intrauterine transfusion in infants with signs of severe disease in utero
(hydrops, severe fetal anemia)
VI. MANAGEMENT OF NEONATE WITH SIGNIFICANT JAUNDICE
● If there is an increased risk for bilirubin encephalopathy, institute measures
Table 3. Rh Incompatibility Labs prior and after treatment such as phototherapy.
PRE-TX POST-TX
Coombs’ (DAT) (+) (-)
A. PHOTOTHERAPY
Normal or
Hemoglobin Normal ● Mainstay of therapy for jaundice
In hydrops, as low as 3-4 g/dL
Reticulocyte Increased Low/Normal ● Light source:
Polychromasia with markedly increased ○ Blue fluorescent tubes (420-480 nm)
PBS Bilirubin absorbs light maximally in the blue range (420-470 nm)
nRBCs
Normal ○ Halogen light bulbs
WBC Normal/Elevated
NICU uses blue light
Platelet Thrombocytopenia ○ Rapid effect on bilirubin
PBS: peripheral blood smear ○ Bilirubin more rapidly decreases in blue light than the white light
nRBCs: nucleated RBCs ● Unconjugated hyperbilirubinemia is reduced on exposure to high intensity light
Require 6-12 hr to have a measurable effect
V. LABORATORY EVALUATION Contraindicated in the presence of porphyria
● Total Serum Bilirubin (TSB) or Transcutaneous Bilirubin (TcB) The therapeutic effect of phototherapy depends on the light energy emitted in
○ If there is no capacity to perform TSB, we can do the cephalocaudal the effective range of wavelengths, the distance between the lights and the
clinical examination of jaundice. infant, and the surface area of exposed skin, as well as the rate of hemolysis
○ TSB determination is important for determination of management and in vivo metabolism and excretion of bilirubin
● CBC The use of phototherapy has decreased the need for exchange transfusion in
○ Check for anemia, polycythemia term and preterm infants with hemolytic and nonhemolytic jaundice
○ Check for Hct and sepsis When indications for exchange transfusion are present, phototherapy should
● Blood typing not be used as a substitute; however, phototherapy may reduce the need for
○ Both the mother and baby repeated exchange transfusions in infants with hemolysis
○ Mandatory, especially if the mother is blood type O
○ Check for Rh incompatibility or ABO incompatibility
● Reticulocyte count
○ Increase = ongoing hemolysis and rising bilirubin
○ Increase with hemolysis, either immune or non-immune
○ Immune cases: ABO & Rh incompatibility
○ Non Immune causes: Thalassemias, G6PD deficiency
● Peripheral blood smear
○ Check for Target Cells
○ Microspherocytes - hallmark for ABO incompatibility
● Coombs Test or Antibody test
Figure n. Phototherapy.
○ Will differentiate immune from non-immune causes of hemolysis
○ If (+) Coombs test, but (-) for ABO and Rh incompatibility, suspect for
minor blood group incompatibility.
● Albumin level
○ If low, institute giving albumin to the baby
○ In order for bilirubin to connect to albumin
○ Decreased albumin concentration will lead to increased free bilirubin,
making the baby more prone to develop kernicterus
● Newborn screening panel (CH, G6PD def., Galactosemia)
○ Congenital Hypothyroidism
○ All which may cause jaundice
○ Thalassemia can also be detected in Expanded NBS
● Sepsis work-up
○ If considering sepsis
○ Consisting of: CBC, blood culture, peripheral smear, lumbar puncture for Figure 9. Double phototherapy for too high bilirubin levels.
meningitis
● Transcutaneous bilirubin levels (TcB)
RECOMMENDATIONS FOR PHOTOTHERAPY
○ Transcutaneous Bilirubinometer
● The guidelines refer to the use of intensive phototherapy, which should be
■ like a thermometer: placed on the chest/ forehead of the baby
used when the total serum bilirubin (TSB) exceeds the line indicated for
■ Register bilirubin levels
each category (low, medium, high risk)
■ Non-invasive (no pricking or taking blood from the baby)
● Phototherapy is used even if the baby is not in a high-risk zone of the
■ Has good sensitivity
nomogram.
Serial monitoring
● Low risk infants - ≥ 38 wk and well
○ Predict whether baby has increasing levels of bilirubin
● Medium risk - ≥ 38 wk and with risk factors or 35-36 6/7 wk and well
● High risk - 35-36 6/7 + risk factors
A. EVALUATION OF NEONATE WITH SIGNIFICANT JAUNDICE ● Risk factors: isoimmune haemolytic disease, G6PD def., asphyxia, significant
lethargy, tem. Instability, sepsis, acidosis, or albumin <3.0g/dL (if measured).
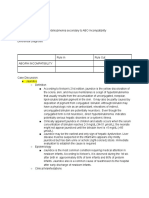
Table 4. Evaluation of a Neonate with Significant Jaundice.
CONCERN POSSIBLE DIAGNOSIS INITIAL LAB TESTS BATCH 2023 TRANS
Jaundice on Day 1 ● Hemolysis CBC, smear, Total, indirect and
● TORCH/Sepsis direct bilirubin, Blood Type and 3. MECHANISMS
● Hepatitis failure syndromes Coomb’s Test ● Photoisomerization
● Internal hemorrhage Converts unconjugated bilirubin from Z-E isomer which is easily excreted
Jaundice requiring ● Hemolysis CBC, smear, Total, indirect and in the bile
Phototherapy ○ ABO Incompatibility direct bilirubin, Blood Type and Reversible photoisomerization reaction converting the toxic native
● TORCH/Sepsis Coomb’s Test unconjugated 4Z,15Z-bilirubin into an unconjugated configurational
Direct, conjugated ● TORCH/Sepsis Hepatic enzymes, ExpNBS, isomer, 4Z,15E-bilirubin which can then be excreted in bile without
hyperbilirubinemia ● Biliary atresia blood glucose, blood ammonia, conjugation
● Other causes of lactate, blood cs, CMV and HSV ● Structural Change
Cholestasis PCR Converts unconjugated bilirubin to lumirubin, which is excreted in the
○ Preterm or term urine in an conjugated state
babies on prolonged Lumirubin, which is an irreversible structural isomer converted from
parenteral nutrition native bilirubin that can be excreted by the kidneys in the unconjugated
● Hepatic failure state
B1 + light → lumirubin
OFFICIAL TRANS BATCH 2024 4
4. COMPLICATIONS INTERMEDIATE-RISK ● Subdivided into upper and lower risk zones by the 75th
ZONE percentile track
● Loose stools
● Low-intermediate risk zone still warrants observation, may
● Erythematous macular rash
request for total bilirubin (especially the indirect type) and
AKA Phototherapy rash
plot the results on the nomogram
Develop due to exposure to light
● Purpuric rash associated with transient phorphyrinemia HIGH-RISK ZONE ● Subdivided by the 95th percentile track
● Overheating ● If the baby has factors (asphyxia, metabolic acidosis, sepsis,
Hyperthermia because of overheating hypoxemia) warrants more aggressive treatment, not just
Body temperature should be monitored and the infant should be shielded phototherapy but also double volume exchange transfusion
from bulb breakage ● Infants are designated as “higher risk” because of the
● Dehydration due to increased insensible water loss and diarrhea potential negative effects of the conditions listed on albumin
Increased insensible water loss secondary to increased temperature and binding of bilirubin, the blood-brain barrier, and the
diarrhea susceptibility of the brain cells to damage by bilirubin
● Hypothermia from exposure
Baby might only be wearing a diaper, the baby is exposed to the outside
environment
● Bronze Baby Syndrome 6. GUIDELINES FOR PHOTOTHERAPY IN HOSPITALIZED INFANTS OF ≥35 WK
Dark, grayish, brown skin discoloration OF GESTATION.
Can occur in the presence of direct hyperbilirubinemia
■ Direct will be more increased than indirect bilirubin
Combined indirect and direct bilirubinemia
– Direct bilirubin > Indirect bilirubin
■ Stop phototherapy because direct bilirubin would not be responsive
for phototherapy
Caused by photo-induced modification of porphyrins present in
cholestatic jaundice
● Cover the eyes and genitalia of the baby since phototherapy may have effects
on the eyes and gonads
Before phototherapy is initiated, the infant’s eyes should be closed and
adequately covered to prevent light exposure and corneal damage
In infants with hemolytic disease, care must be taken to monitor for the
development of anemia, which may require transfusion
○ Anemia may develop despite lowering of bilirubin levels
5. ZONES OF RISK FOR PATHOLOGIC HYPERBILIRUBINEMIA BASED ON
HOUR SPECIFIC SERUM BILIRUBIN LEVELS
Figure 10. Bhutani nomogram. Zones of risk for pathologic hyperbilirubinemia based on
hour specific serum bilirubin levels.
● For babies ≧35 weeks AOG
Late preterm, terms, or post-term
● Level of bilirubin, decide whether to be placed on phototherapy or exchange
transfusion
● Level of serum bilirubin on the Y-axis, age in hours or period of life of the baby
on the X-axis
Level of bilirubin: 15, baby is only 36 hours of life
■ Baby is now in more than the 95th percentile or the high risk zone
■ Baby needs phototherapy Figure 11. Bhutani nomogram. Guidelines for phototherapy in hospitalized infants of ≥35
Level of bilirubin: 8, baby is 73 hours wk of gestation.
■ Low risk
■ Observe the baby for the progression of jaundice ● Use total bilirubin
– If due to breastfeeding jaundice, just continue breastfeeding Do not subtract direct reacting or conjugated bilirubin
– If other reasons, treat cause ● Risk factors:
Isoimmune hemolytic disease
AAP Management of Hyperbilirubinemia in Newborn infants > 35 weeks Gestation G6PD deficiency
(Nomogram for designation of risk in 2840 well newborns at > 36 weeks’ gestational age Asphyxia
with birth weight of >2000 g or >35 weeks’ gestational age and birth weight of > 2500 g Significant lethargy
based on the hour-specific serum bilirubin values. (reproduced with permission from Temperature instability
Bhutani VK, Johnson L, Sivieri EM. Pediatrics. 1999;103[1]:6-14)) Sepsis
BATCH 2023 TRANS Acidosis
Albumin 3.0 g/dL (if measured)
Table 5. Risk designation of term and near-term well newborns based on their If these risk factors are present, the treatment will be more aggressive
hour-specific serum bilirubin values. ■ In the example earlier, well baby in the high risk zone → start
CLASSIFICATION INFORMATION phototherapy
■ Even if the baby is only at moderate risk but the risk factors are
LOW-RISK ZONE ● Electively and statistically defined by the 40th percentile
present, the treatment will be more aggressive
track
● For well infants 35-37 6/7 wk can adjust TSB levels for intervention around the
● Observe the baby, though the bilirubin will still increase
medium risk line
OFFICIAL TRANS BATCH 2024 5
It is an option to intervene at lower TSB levels for infants closer to 35 ● Precise blood level above which indirect-reacting bilirubin or free bilirubin will
wks (still premature) and at higher TSB levels for those closer to 37 6/7 be toxic to an individual infant is unpredictable
wk ● Studies have shown that kernicterus only occurred in infants with a bilirubin
● It is an option to provide conventional phototherapy in hospital or at home at >20 mg/dL
TSB levels 2-3 mg/dL (35-50 mmol/L) below those shown, but home ● Duration of exposure to high bilirubin levels needed to produce toxic effects is
phototherapy should not be used in any infant with risk factors unknown
Respiratory distress syndrome (RDS) occurs primarily in premature infants ● The more immature the infant is, the greater the susceptibility to kernicterus
This is not applicable to preterm babies, because preterm baby management A. PATHOPHYSIOLOGY
is more aggressive.
● The pathogenesis is multifactorial and involves an interaction between
B. EXCHANGE TRANSFUSION unconjugated bilirubin levels, albumin binding and unbound bilirubin levels,
● Partial removal of infant’s circulating antibody coated RBCs as well as passage across the BBB, and neuronal susceptibility to injury.
unattached antibodies and replace them with donor RBCs that lack the ● Disruption of BBB due to diseases like sepsis, asphyxia, metabolic acidosis,
sensitizing antigen. and maturational changes in BBB permeability affect the risk
○ Double volume exchange ~85% circulating RBCs are replaced ○ If the baby has sepsis, or was asphyxiated, or having episodes of
● Push-pull method hypoxemia: warrants more aggressive therapy
○ Place an umbilical vein catheter on the baby, and draw out the baby’s B. SIGNS AND SYMPTOMS
blood and change it with donor blood
○ Compute aliquot volume of blood to be removed and replaced
○ Fresh 24-hour blood (type O if with ABO incompatibility) 1. ACUTE FORM
○ Done in ABO incompatibility or Rh incompatibility wherein there is an ● Clinical signs and symptoms usually appear 2-5 days after birth in term infants
antigen-antibody reaction and as late as the 7th day in preterm infants
● Complications: ● Hyperbilirubinemia may lead to encephalopathy at any time during the
○ Metabolic acidosis neonatal period
○ Electrolyte imbalance
○ Hypoglycemia Table 6. Phases and Signs and Symptoms
○ Hypocalcemia 1st Phase ● Hypotonia (diminished tendon reflexes), respiratory distress,
○ Thrombocytopenia lethargy, poor feeding, poor suck, and loss of moro reflex
○ Volume overload, st
1 1-2 days are common initial signs
○ Arrhythmias ● Early signs are indistinguishable from those of sepsis,
○ Necrotizing Enterocolitis asphyxia, hypoglycemia, intracranial hemorrhage, and other
○ Infection (portal of entry for microorganisms) acute systemic illnesses in a neonate
○ Graft-versus host disease nd
2 Phase ● Hypertonia of the extensor muscles, opisthotonos (baby
○ Death (due to severe arrhythmia, volume overload, and bleeding)
arches their back and hyperextends neck), high pitched cry,
Middle of 1st week seizure, retrocollis, fever
● Opisthotonos with a bulging fontanel, twitching of the face or
limbs, and a shrill, high-pitched cry
● In advanced cases, convulsions or spasms occur, with
infants stiffly extending their arms in an inward rotation with
the fists clenched
● Rigidity is rare at this late stage
3rd Phase ● Hypotonia, long term neurologic injury, extrapyramidal
disturbances, deafness (high levels of bilirubin can be
After the 1st week deposited in cochlea of the ear)
● (in Nelsons: hypertonia)
2. CHRONIC FORM
Table 7. Chronic Form and Signs and Symptoms
1st Year ● Hypotonia
● Active deep tendon reflexes
Figure 12. Exchange Transfusion ● Obligatory tonic neck reflex
● Delayed motor skills
● Later in the 1st year, the following tend to recur
C. DRUGS
○ Opisthotonos
● Metalloporphyrins ○ Muscle rigidity
○ Not available in the Philippines ○ Irregular movements
○ Inhibits first enzyme heme oxygenase ○ Convulsions
○ Single IM dose on the first day of life (for those with ABO, Rh After 1st Year ● Movement disorders (choreoathetosis, ballismus, tremor)
incompatibility, G6PD, Jehovah’s Witness) may reduce the need for ● Upward gaze
subsequent phototherapy ● Sensorineural hearing loss
■ Jehova’s Witness: they do not wish to receive blood transfusion ○ Due to bilirubin deposition in the cochlea
○ Complication: Transient erythema if the infant is receiving 3rd Phase ● Hypotonia, long term neurologic injury, extrapyramidal
phototherapy disturbances, deafness (high levels of bilirubin can be
○ Data on efficacy, toxicity, and long-term benefits are still being evaluated After the 1st week deposited in cochlea of the ear)
● Intravenous Immune Globulin (IVIg) ● (in Nelsons: hypertonia)
○ For hyperbilirubinemia caused by isoimmune hemolytic disease
○ Adjunctive treatment for hyperbilirubinemia caused by isoimmune
haemolytic disease C. PREVENTION
○ Recommended when serum bilirubin is approaching exchange levels ● Experts recommend predischarge universal screening for hyperbilirubinemia
despite maximal interventions, including phototherapy in the 1st 24-48h after birth and
○ For Coombs’ test (+) hyperbilirubinemia ● Assessment of clinical risk factors for severe jaundice and bilirubin-induced
○ In both ABO and Rh hemolytic disease, presumably by reducing neurologic dysfunction
hemolysis ○ Jaundice within 24 hr: Measure TSB and B2 levels
○ Unknown mechanism ■ If elevated, evaluate for possible hemolytic disease
■ Blocks Fc receptors thereby inhibiting hemolysis (Rh) hemolytic ● Follow-up should be provided within 2-3 days of discharge to all neonates
disease) discharged <48 hr after birth
● Goal of Therapy ● Early follow-up: important for infants <38 wk of gestation
○ Prevent neurotoxicity- Kernicterus (Bilirubin encephalopathy) ● Ongoing lactation promotion, education, support, and follow-up services are
essential throughout the neonatal period
VII. KERNICTERUS ● Mothers should be advised to nurse their infants every 2-3 hr
● Goal of Therapy: Prevent neurotoxicity / Kernicterus (bilirubin encephalopathy) ○ To ensure adequate hydration and caloric intake
○ We don’t want this to happen, so we expose them early on to ○ Avoid routine supplementation with water or glucose water
phototherapy and observe closely ● Potentially Preventable Causes of Kernicterus
● Kernicterus is damage to the brain centers of infants caused by increased ○ Early discharge (<48 hr) with no early follow-up (within 48 hr of
levels of unconjugated-indirect bilirubin (B1) which is free (not bound to discharge); important in near-term infants (35-37 wk of gestation)
albumin). ○ Failure to check the bilirubin level in an infant noted to be jaundiced in
● The free bilirubin enters the BBB and is deposited in the basal ganglia and the 1st 24 hr
brainstem nuclei and this causes all the different neurological manifestations. ○ Failure to recognize the presence of risk factors for hyperbilirubinemia
● Develops in 30% of infants (all gestational ages) with untreated hemolytic ○ Underestimation of the severity of jaundice by clinical (visual)
disease and bilirubin levels >25-30 mg/dL assessment
○ Lack of concern regarding the presence of jaundice
OFFICIAL TRANS BATCH 2024 6
○ Delay in measuring the serum bilirubin level despite marked jaundice or birth Oral vitamin K
delay in initiating phototherapy in the presence of elevated bilirubin levels regimens require
○ Failure to respond to parental concern regarding jaundice, poor feeding, Avoidance of repeated dosing.
or lethargy above medications
Phenobarbital, phenytoin, warfarin, rifampin, isoniazid – interfere with
VIII. HEMORRHAGIC DISEASE OF THE NEWBORN vitamin K levels/absorption
● Neonates have a unique hemostatic system that places them at high risk for *Cholestasis impairs absorption of the fat-soluble vitamins
hemorrhagic complications, especially in the presence of illness or other stress **ICH is more common in classic VKDB
○ Plasma levels of the vitamin K–dependent coagulation factors (II, VII, IX,
X, protein C, protein S) and antithrombin: low at birth and do not reach ● If a mother is known to be receiving such drugs late in gestation, an infant PT
adult ranges until 6 mo of age should be measured using cord blood, and the infant immediately given
○ Thrombin generation and platelet function are also altered in normal 1-2 mg of vitamin K intravenously
newborns ○ If PT is greatly prolonged and fails to improve, or in the presence of
■ Consequently, both congenital and acquired bleeding disorders significant hemorrhage: 10-15 mL/kg of fresh-frozen plasma should
that affect primary or secondary hemostasis can manifest in the be administered.
newborn period
● Hemorrhage in a healthy neonate: suggests an inherited coagulation defect 1. LABORATORY FINDINGS
or immune-mediated thrombocytopenia
● Bleeding symptoms in a sick neonate: more likely to reflect underproduction Table 9. Laboratory Findings in VKDB
or consumption of coagulation factors and/or platelets LABS RESULT
● Congenital hemorrhagic disorders such as hemophilia can present with RBC morphology, factor I (fibrinogen), fibrin split Normal
bleeding in the newborn period products, bleeding time, clot retraction, platelet count
● Common acquired hemorrhagic disorders: vitamin K deficiency bleeding, and function
DIC, and immune-mediated thrombocytopenia
aPTT PROLONGED
PT PROLONGED
A. VITAMIN K DEFICIENCY BLEEDING (VKDB) Factor II, VII, IX and X levels DECREASED
● Factors 2, 7, 9, 10 (Vit. K dependent factors) are physiologically LOW
○ Vitamin K: facilitates posttranscriptional carboxylation of these factors 2. TREATMENT
■ Therefore, in the absence of carboxylation, such factors form
● Vitamin K
PIVKA (proteins induced in vitamin K absence), which have
○ Prophylactic dose: 0.5-1mg Vit K1 by
greatly reduced function
■ IM route IM route of vitamin K prophylaxis remains the method of
○ Characterized by hemorrhage that is most frequently GI, nasal,
choice
subgaleal, intracranial, or post circumcision
● Oral vitamin K is less effective in preventing late-onset
○ Prodromal or warning signs (mild bleeding) may occur before serious
vitamin K deficiency bleeding and thus cannot be
intracranial hemorrhage
recommended for routine therapy.
■ Affected infants appear well but with massive hematemesis,
■ However, such vitamin K prophylaxis is not uniformly effective to
hematochezia
prevent all hemorrhagic disease particularly in exclusively
● Classically, vitamin K deficiency bleeding occurs early in the newborn period,
breastfed and premature infants.
typically between day 2 and 7 of life, and most often in exclusively
■ Safe; not associated with an increased risk of childhood cancer or
breastfeeding infants who did not receive vitamin K prophylaxis at birth
leukemia
● Severe Vit K def. is more common in premature infants
○ Treatment dose: 1-5mg Vit K1 IV or oral
○ Caused by lack of free vitamin K from mother
● Fresh frozen plasma
■ Hence, we give exogenous vitamin K to babies
○ Rich in clotting factors
○ Coupled with absence of bacterial intestinal flora normally
○ Dose: 10-20 ml/kg
responsible for the synthesis of vitamin K
● Associated Conditions:
○ Responsive to (and entirely prevented by) exogenous vitamin K B. DISSEMINATED INTRAVASCULAR COAGULOPATHY
therapy ● Consumption of coagulation factors and bleeding
■ Should be distinguished from rare congenital deficiencies of ● Can present with either bleeding or thrombosis, and usually with evidence
clotting factors that are unresponsive to vitamin K, which can of end-organ damage and increased mortality
occur in otherwise well-appearing infants ● Affected infants often premature or very sick (toxic-looking)
○ Prematurity: poor placental transfer ● Clinical course frequently characterized by asphyxia, hypoxia, acidosis,
○ Diet: Breastmilk is a poor source of vitamin K shock or infection
■ Thus, hemorrhagic complications are more frequent in breastfed ○ End result of severe sepsis - DIC
than in formula-fed infants ● Treatment: correcting primary clinical problem and blood component
○ Altered bacterial colonization: prolonged antibiotic use transfusion (e.g., FFP)
■ In cases of sepsis, we give antibiotics to kill both normal flora and ○ If the cause is infection, treat the infection
pathogenic organisms ○ Give FFP if plasma is low; RBCs if RBCs are low
○ Hepatocellular disease or GI obstruction: malabsorption of Vitamin K
and impaired synthesis of clotting factors
Table 8. Hemorrhagic Diseases of the Newborn (VKDB in Infancy)
PARA- EARLY CLASSIC LATE
METER
Age 0-24 hours 2-7 days 1-6 months
Medications during Malabsorption of
pregnancy that the fat-soluble
interfere with vitamin K such as
vitamin K in:
absorption or Cholestasis*
function: Exclusive (biliary atresia,
(anticonvulsant breastfeeding hepatitis, cystic
Causes &
phenytoin or and those who did fibrosis),
Risk
phenobarbital, not receive
factors
anticoagulant prophylactic Vit K at Abetalipoprotein
warfarin, anti TB birth deficiency
drugs rifampin and
isoniazid), Idiopathic (Asian
cholesterol breastfed infants),
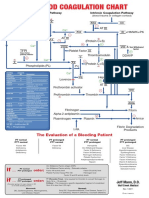
lowering Figure 13. Diagnosis of Bleeding in the Newborn.
medications Warfarin ingestion
ICH**, GI, Umbilicus skin, GI, ICH
ICH, GI, Umbilicus IX. HEMATOLOGIC DISORDERS IN THE NEONATE
ENT-mucosal (30-60%)
Site of Intra-abdominal ● Anemia
Cutaneous ENT-mucosal
Bleeding Subgaleal ○ Hemolytic Disease of the Newborn
Injection sites Thoracic
Cephalhematoma ● Polycythemia
Post-Circumcision Injection sites
Maternal Vit K Parenteral and ● Bleeding/hemorrhage
(20mg) prophylaxis Parenteral Vitamin K high-dose oral Vit ○ Hemorrhagic Disease of the Newborn
Prevention and postnatal at birth K during periods
administration to of cholestasis
infant soon after
OFFICIAL TRANS BATCH 2024 7
Table 10. Hemolytic vs Hemorrhagic Disease of the Newborn ○ G6PD deficiency: most common RBC enzymopathy
Hemolytic Hemorrhagic ○ Pyruvate kinase (PK) deficiency: 2nd most common RBC enzymopathy
Vit K Deficiency and may also be associated with neonatal jaundice and bizarre
Other name Erythroblastosis fetalis morphology featuring acanthocytes
Bleeding
Etiology ABO or Rh incompatibility Low Vit. K ○ Congenital Spherocytosis: most common RBC membrane disorder
Clinical ○ Hereditary elliptocytosis (HE), hereditary pyropoikilocytosis (HPP)
Jaundice Hemorrhage ● Immune hemolysis
Presentation
○ Isoimmune hemolytic anemia (Rh/ABO incompatibility)
● Non-immune hemolysis
A. NEONATAL ANEMIA ○ Bacterial sepsis, TORCH infections
● Indicated by a central venous hemoglobin <13 g/dL or a hematocrit of
<40% Table 12. ABO vs Rh Incompatibility
● Normal term Hgb at birth: 14-20 g/dL ABO Incompatibility Rh Incompatibility
● Normal reticulocyte count: 3-7% Frequency Common Unusual
● Etiologies: Occurrence in first-born Yes Very low
○ Hemorrhagic anemia Mother’s Blood Type O Rh (-)
○ Hemolytic anemia A or B
○ Hypoplastic anemia Infant’s Blood Type (A is more antigenic than Rh (+)
B)
Predictably severe in
subsequent No Usually
pregnancies
Stillbirth/hydrops Rare Frequent
Pallor Minimal Marked
Jaundice Mild-moderate Prominent, Severe
Hepatosplenomegaly No Yes
Incidence of late anemia Uncommon Common
IgM (majority)
Antibody Type IgG
IgG or IgA
RBC antibody titer May help predict severity May not correlate with
implication of fetal disease. fetal disease
Figure 14. DDx of Neonatal Anemia. Coombs Test +/-
+
(direct) (Usually positive)
Hemoglobin Moderately low Very low
01. HEMORRHAGIC ANEMIA Serum Bilirubin
Variably elevated Markedly elevated
● Blood loss: most common cause of neonatal anemia. (indirect)
○ Repeated or frequent phlebotomy for routine laboratory tests, Microspherocytes – Nucleated RBCs,
especially from premature or acutely ill neonates: one of the most RBC Morphology
hallmark polychromasia
common causes of anemia. Reticulocyte Count Increased Increased
● Antepartum blood loss Yes (antenatal fetal
○ Transplacental/fetomaternal bleeding Need for Antenatal Mx No
transfusion)
■ Caused by bleeding from the fetal into the maternal circulation, Phototherapy Yes Yes
either before or during delivery.
Infrequent
■ Decreased or absent fetal movement: most common antenatal Exchange Transfusion Frequent
(for very high levels)*
presentation and should be associated with a high degree of
clinical suspicion Maybe
Maybe
■ After delivery, infant pallor, hypotension, and poor perfusion IVIG RhoGAM prevents
(no role)
will indicate severe anemia sensitization
■ Classic Kleihauer-Betke test *Sometimes in ABO incompatibility, even if the bilirubin level is not that high, we still do
– Used to diagnose FMH exchange transfusion if the baby continues to be anemic.
– Gold standard; identifies fetal erythrocytes containing HbF
resistant to acid elution 03. HYPOPLASTIC ANEMIA
– Labor intensive, highly dependent on the skills of the ● Congenital disease: Diamond-Blackfan Syndrome (usually do not manifest
technician, and often not available as a rapid or point-of-care jaundice but have other features)
test
■ Flow cytometry
– More precise test to quantify fetal cells in the maternal
circulation.
○ Anomalies of the umbilical cord
○ Twin-to-twin transfusion
● Intrapartum blood loss
○ Traumatic rupture of the umbilical cord
○ Placental abnormalities (placenta previa, abruptio placenta)
● Postnatal blood loss
○ External: bleeding from umbilicus
○ Internal: subgaleal hemorrhage, visceral organ hemorrhage (liver,
spleen, adrenal)
● Acute vs. Chronic Blood Loss
Table 11. Acute vs. Chronic Blood Loss
ACUTE BLOOD LOSS CHRONIC BLOOD LOSS
● Acute distress: pallor, shallow ● Marked pallor disproportionate
breathing, tachycardia, shock to the evidence of distress
● Hemoglobin may be normal ● Hemoglobin low at birth
initially then drops quickly ● RBC: hypochromic,
within 24 hours microcytic,
● No hepatosplenomegaly anisopoikilocytosis
● RBC: normochromic, ● Low serum iron at birth
macrocytic ● Course generally uneventful
● Normal serum iron ● May cause heart failure if Figure 14. Syndromes Associated with Congenital Hyporegenerative Anemia – See
● Prompt treatment of anemia severe appendix for a bigger picture.
necessary to prevent death ● Treatment: iron therapy
● Treatment: NSS, packed RBC ● Acquired diseases: bacterial and viral (TORCH, parvovirus B19) infections
transfusion
1. LABORATORY DIAGNOSIS
02. HEMOLYTIC ANEMIA ● CBC with peripheral blood smear & reticulocyte count
● Congenital erythrocyte defect ○ RBC indices
○ β-hemoglobinopathies such as sickle cell disease and β-thalassemia: do ● DAT
not present in the neonatal period ● Serum bilirubin
■ As a result of the protective effect of high levels of HbF in the first ● Blood typing of infant and mother
few months of life. ● Maternal Indirect Antiglobulin Test for erythrocyte alloantibodies
● Kleihauer-Betke test: to identify fetal RBCs in maternal circulation
OFFICIAL TRANS BATCH 2024 8
■ Associated with a significant reduction in the # of blood
transfusions per infant
■ But also a significantly increased risk of ROP
B. NEONATAL POLYCYTHEMIA
● Central hemoglobin or hematocrit (Hct) exceeding 2 standard deviations (SD)
above the normal value for gestational and postnatal age
○ For a full term infant:
■ Hemoglobin concentration is ≥22 g/dL
■ Central venous hematocrit of >65%
○ Measuring the central hemoglobin using an automated blood
counter is important because both peripheral (heelstick) and capillary
tube microcentrifugation yield higher Hct values than central values, by
up to 15%
○ Timing is also important; because of fluid shifts in the newborn period,
Hct peaks during the 1st 2-3 hr of life.
● Dehydration should also always be considered as a cause
● Hyperviscosity
○ May be accentuated because neonatal RBCs are large and have
decreased deformability which together predispose stasis in the
microcirculation
■ May be the primary issue
01. PLACENTAL HYPERPERFUSION
● Twin-to-twin transfusion
● Maternofetal transfusion
● Delayed cord clamping: most common cause in term infants
02. PLACENTAL INSUFFICIENCY
● SGA Infants
● Post-maturity
● Maternal hypertension
Figure 15. Approach to Anemia in Newborn Infants. Doc added alpha-thalassemia
syndromes and infection under abnormal peripheral blood smear.
03. ENDOCRINE AND METABOLIC DISORDERS
2. TREATMENT ● CAH
● Neonatal thyrotoxicosis (neonatal Graves’ disease)
● Delayed Cord Clamping
● Maternal diabetes
○ 1-3 mins after cessation of cord pulsation
○ Beneficial in preventing anemia
○ Results in delivery of an extra 20-40mL of blood and 30-35mg of iron to 04. MISCELLANEOUS
the baby ● Trisomies 13, 18, 21 (Patau, Edwards, Down)
○ Asymptomatic polycythemia ● Beckwith-Wiedemann syndrome
● Blood Transfusion
○ Depends on the severity of symptoms, Hgb levels, presence of
1. CLINICAL FEATURES
co-morbid diseases that interfere with oxygen delivery
(bronchopulmonary dysplasia, cyanotic congenital heart disease, ● S/sx of polycythemia can result from hyperviscosity or metabolic
respiratory distress syndrome) disturbances, or both
■ Especially if the babies would be on ventilatory support ○ Hyperviscosity: sluggish blood flow causing decreased tissue perfusion
○ Relatively common among premature and very-low-birthweight (VLBW) ● Symptoms often appear in the first few hours of life but can be delayed by up
infants. to 2-3 days
● Reported adverse outcomes: speech deficits, abnormal fine motor control,
Table 13. Suggested Transfusion Thresholds reduced IQ, school problems, and other neurologic abnormalities
(+) Respiratory Support (-) Respiratory Support ○ Underlying etiology (chronic intrauterine hypoxia) is likely the
Postnatal determinant of these outcomes rather than polycythemia itself.
Hgb Conc in g/dL (Hct %) ● Irritability or lethargy
Age
● Tachypnea and cyanosis
Week 1 11.5 (35%) 10.0 (30%)
● Plethora
Week 2 10.0 (30%) 8.5 (25%) ● Hypoglycemia
Week 3 8.5 (25%) 7.5 (23%) ● Jitteriness
● Poor feeding
○ Blood products ● Thrombosis
■ Leukocyte-reduced or CMV-seronegative Packed RBCs (to ● Seizures (hyperviscous blood may go to CNS and result to thrombosis)
reduce risk of CMV transmission) or
■ Irradiated PRBCs (to remove GVHD risk but does not eliminate 2. SEVERE COMPLICATIONS (HYPERVISCOSITY)
the risk of CMV transmission.)
■ Amount: estimated at 10-20 mL/kg ● Seizures
● Stroke
● Pulmonary hypertension
● NEC
● Renal vein thrombosis
● Renal failure
■ Rate: 3-5 mL/kg/ hr, with a slower rate preferred for very small,
acutely ill infants with a tenuous fluid status 3. MANAGEMENT
■ Duration: should be completed within 4 hours.
● If capillary HCT >65% confirm with a venous sample and treat
○ Risks
dehydration
■ Hemolytic and nonhemolytic transfusion reactions
● Asymptomatic hydration (enteral or IV) and observation
■ Exposure to blood product preservatives & toxins
● Symptomatic or worsens despite hydration or HCT >70% reduction of
■ Volume overload
hematocrit by partial exchange transfusion with NSS
■ ROP, NEC, GVH reaction
○ Lowers Hct and viscosity acutely and improves acute symptoms but may
■ Transfusion-acquired infections (CMV, HIV, parvovirus, Hepa B &
not affect long-term outcome in polycythemic infants
C)
○ May cause increased risk of NEC
● Recombinant Human Erythropoietin (rhEPO)
● All polycythemic infants: closely monitored for Ins and Outs, blood glucose
○ Treatment of chronic or anticipated anemia to eliminate or decrease
and bilirubin levels
transfusions
○ Used for anemia of prematurity (physiologic underproduction of RBCs
until 2nd month of life due to relative polycythemia and right shift in O2 X. SWALLOWED BLOOD SYNDROME
dissociation curve; prolonged in preterm infants) ● Differential for GI bleeding
■ Particularly, VLBW infants ● Blood or bloody stools are passed
○ Must be supplemented with oral iron ● Usually 2nd or 3rd day of life
○ No strong indication for routine use
OFFICIAL TRANS BATCH 2024 9
● Cause: swallowed maternal blood during delivery or from a fissure in mother’s
nipple
● APT test – determines whether blood is maternal or fetal in origin
○ (+): maternal
○ Bloody stool + NaOH color reaction
■ (+) yellow-brown: blood is maternal in origin
■ (-) persistent pink: fetal origin (fetal Hgb is alkali-resistant)
XI. PLETHORA IN THE NEWBORN INFANT
● Ruddy, deep red-purple appearance associated with high HCT
○ Often d/t polycythemia
● Increased incidence: increased at high altitude, post-term, VLGA, recipient of
twin-twin transfusion, after delayed cord clamping, infants with diabetic or HTN
mothers, trisomy 13, 18, 21, hypothyroidism
● Clinical manifestations: irritability, lethargy, tachypnea, respiratory distress,
cyanosis, feeding disturbances, hyperbilirubinemia, hypoglycemia,
thrombocytopenia
● Many affected infants are asymptomatic
● Severe complications: seizures, stroke, pulmonary HTN, NEC, renal vein
thrombosis, and renal failure
● Management
○ Asymptomatic + HCT 60-70% close monitoring and hydration only
(enteral or IV fluids)
○ Symptomatic or HCT >70-75%, or with hyperviscosity: partial exchange
transfusion with NSS
XII. REFERENCES
● Santos, W.R. (2022), Jaundice, Pallor, and Bleeding [PowerPoint
Presentation]. Manila, Philippines: Faculty of Medicine and Surgery, University
of Santo Tomas, PEDIATRICS 2
● Kliegman, R. (2020). Nelson textbook of pediatrics (Edition 21.). Philadelphia,
PA: Elsevier.
● Batch 2023 trans
XIII. REVIEW QUESTIONS
CTBA/TF
1. What is the first enzyme in the bilirubin metabolism?
A. Heme Oxygenase
B. Bilirubin reductase
C. Glucoronyl Reductase
D. GLucoronyl Transferase
2. What is the treatment for Rh incompatibility?
A. Fresh frozen plasma
B. Rhogam
C. Erythropoietin
D. Factor 8
AB
OFFICIAL TRANS BATCH 2024 10
XIV. APPENDIX
Appendix I.
INCREASED BILIRUBIN INCREASED ENTEROHEPATIC DECREASED CLEARANCE OF METABOLIC CONDITIONS INBORN ERRORS OF
PRODUCTION CIRCULATION UNCONJUGATED BILIRUBIN METABOLISM
Hemolysis (immune-mediated- Insufficient breast milk/feeding Prematurity Hypothyroidism Galactosemia
heritable)
Pyloric stenosis G6PD deficiency Hypopituitarism Gilbert syndrome
Extravasation (cephalhematoma)
Bowel obstruction Cigler-Najjar syndrome (I and II)
Polycythemia
Ileus Breast milk jaundice due to other
Sepsis bilirubin UGT1A1 mutations
Disseminated intravascular Tyrosinemia
coagulation
Hypermethioninemia
Macrosomic infants of diabetic
mothers
*G6PD = glucose-6-phosphate dehydrogenase; UGT1A1 = uridine diphosphate-glucuronosyltransferase, family 1, polypeptide A1
XV. FREEDOM WALL
● Write whatever you want here: anything that will make our batch smile after reading a long trans.
● You can remove this section if you don’t want to include this anymore.
OFFICIAL TRANS BATCH 2024 11
You might also like
- Neonatal Jaundice: Understanding and Preventing KernicterusDocument12 pagesNeonatal Jaundice: Understanding and Preventing Kernicterusn_akash3977No ratings yet
- Approach To Patients With Jaundice, Abdominal Swelling, and AscitesDocument17 pagesApproach To Patients With Jaundice, Abdominal Swelling, and AscitesLINDSLEY GONo ratings yet
- Ped CHG S3 L03 CholestasisDocument9 pagesPed CHG S3 L03 CholestasisLara Patricia TamsiNo ratings yet
- Neonatal JaundiceDocument6 pagesNeonatal JaundiceDoc Prince CaballeroNo ratings yet
- Neonatal Indirect HyperbilirubinemiaDocument14 pagesNeonatal Indirect HyperbilirubinemiaValen CadenaNo ratings yet
- 10 NNJ 1Document22 pages10 NNJ 1ahmed shorshNo ratings yet
- CC Lec - Liver DiseasesDocument3 pagesCC Lec - Liver DiseasesFallen GwiyeobdaNo ratings yet
- Care of Neonate With HyperbilirubinemiaDocument11 pagesCare of Neonate With HyperbilirubinemiaKakali ChakrabortyNo ratings yet
- Final Jaundice1Document43 pagesFinal Jaundice1ahmad solehinNo ratings yet
- Neonatal JaundiceDocument23 pagesNeonatal Jaundiceamid sultanNo ratings yet
- Conjugated Bilirubin Direct Bilirubin Unconjugated Bilirubin Indirect BilirubinDocument12 pagesConjugated Bilirubin Direct Bilirubin Unconjugated Bilirubin Indirect BilirubinTanviNo ratings yet
- Neonatal JaundiceDocument95 pagesNeonatal JaundiceChidi MbatuegwuNo ratings yet
- M. JaundiceDocument9 pagesM. JaundiceRoselle Joy D. RosalejosNo ratings yet
- Neonatal Jaundice: Bilirubin MetabolismDocument2 pagesNeonatal Jaundice: Bilirubin MetabolismghsNo ratings yet
- Neonatal Jaundice 2023Document31 pagesNeonatal Jaundice 2023Demelash SolomonNo ratings yet
- Neonatal Jaundice: by GudetaDocument52 pagesNeonatal Jaundice: by GudetaGudeta shegerNo ratings yet
- Neonatal Jaundice: Intensive Care Nursery House Staff ManualDocument3 pagesNeonatal Jaundice: Intensive Care Nursery House Staff ManualLinna SriwaningsiNo ratings yet
- Neonatal JaundiceDocument54 pagesNeonatal JaundiceTheresa MendoncaNo ratings yet
- Neonatal Jaundice Guide: Causes, Symptoms and TreatmentDocument44 pagesNeonatal Jaundice Guide: Causes, Symptoms and Treatmentmarco luenaNo ratings yet
- Neonatal JaundiceDocument11 pagesNeonatal JaundiceImAlien OrGodNo ratings yet
- Pediatrics - Neonatal Jaundice PDFDocument2 pagesPediatrics - Neonatal Jaundice PDFJasmine KangNo ratings yet
- MLT 502 - Immunohaematology IIDocument42 pagesMLT 502 - Immunohaematology IISanjay Kumar SanjuNo ratings yet
- BiliDocument63 pagesBiliFu Xiao ShanNo ratings yet
- Neonatal Jaundice: Addisu AnDocument38 pagesNeonatal Jaundice: Addisu AnAbiy AliyeNo ratings yet
- Neonatal Hyperbilirubinemia: Mahlet Abayneh Assistant Professor of PediatricsDocument41 pagesNeonatal Hyperbilirubinemia: Mahlet Abayneh Assistant Professor of PediatricsBegashawNo ratings yet
- Issue End of LifeDocument28 pagesIssue End of LifeYURISDHA AFRIZALNo ratings yet
- Neonatal Jaundice: Causes, Evaluation and ManagementDocument22 pagesNeonatal Jaundice: Causes, Evaluation and ManagementAnkur WadheraNo ratings yet
- Sol SeminarDocument15 pagesSol SeminarJimach Bol WieNo ratings yet
- JaundiceDocument14 pagesJaundiceEd Marie GonzagaNo ratings yet
- Jaundice-Neonatal 2016Document45 pagesJaundice-Neonatal 2016Awatef AbushhiwaNo ratings yet
- Core Concepts:: Bilirubin MetabolismDocument9 pagesCore Concepts:: Bilirubin MetabolismManasye AlanNo ratings yet
- Core Concepts Bilirrubin MetabolismDocument9 pagesCore Concepts Bilirrubin MetabolismAngelina ChunNo ratings yet
- Common Neonatal Problems 2016Document161 pagesCommon Neonatal Problems 2016Dejen TakeleNo ratings yet
- Neonatal Jaundice: Aetiology, Diagnosis and Treatment: Current Issues in Neonatal CareDocument6 pagesNeonatal Jaundice: Aetiology, Diagnosis and Treatment: Current Issues in Neonatal CareLaila AzizahNo ratings yet
- ) Jaundice PDFDocument4 pages) Jaundice PDFAzzNo ratings yet
- Liver Function: An Overview of Its Vital Roles and Disorders/TITLEDocument45 pagesLiver Function: An Overview of Its Vital Roles and Disorders/TITLEpuno ric100% (1)
- Nej M 200102223440807Document10 pagesNej M 200102223440807fajriNo ratings yet
- Jaundice: A Guide to DiagnosisDocument49 pagesJaundice: A Guide to DiagnosisAbdelrahman MokhtarNo ratings yet
- Liver Function & Disorders - PHARMD4Document29 pagesLiver Function & Disorders - PHARMD4AhjNo ratings yet
- Neonatal JaundiceDocument48 pagesNeonatal JaundiceRemy MartinsNo ratings yet
- 1 Core Concepts Bilirubin MetabolismDocument9 pages1 Core Concepts Bilirubin Metabolismlink0105No ratings yet
- Neonatal Jaundice & HyperbilirubinemiaDocument23 pagesNeonatal Jaundice & HyperbilirubinemiaMeseret Hamer ZewdieNo ratings yet
- JAUNDICE ReportDocument33 pagesJAUNDICE ReportMirzi CuisonNo ratings yet
- Jaundice FinalDocument30 pagesJaundice FinalFrances GrefalNo ratings yet
- Jaundice Clinical Manifestation and Pathophysiology A Review ArticleDocument3 pagesJaundice Clinical Manifestation and Pathophysiology A Review ArticleHany ZutanNo ratings yet
- Hyper Bilirubin Emi ADocument36 pagesHyper Bilirubin Emi ASai Krishna MaddiralaNo ratings yet
- Physiological and Pathological Jaundice in NewbornsDocument21 pagesPhysiological and Pathological Jaundice in NewbornsTina Ann JohnNo ratings yet
- Icterus Neonatorum/ Jaundice: 07/12/2021 Rupinder DeolDocument83 pagesIcterus Neonatorum/ Jaundice: 07/12/2021 Rupinder DeolShivangi SharmaNo ratings yet
- Neonatal Hyperbilirubinemia: Julniar M Tasli Herman Bermawi Afifa RamadantiDocument57 pagesNeonatal Hyperbilirubinemia: Julniar M Tasli Herman Bermawi Afifa RamadantiRurie Awalia SuhardiNo ratings yet
- Bilirubin Metabolism: Hd. - Msc. (Biochemistry)Document18 pagesBilirubin Metabolism: Hd. - Msc. (Biochemistry)MuhamadMarufNo ratings yet
- Pathophysiology and Treatment of Neonatal HyperbilirubinemiaDocument6 pagesPathophysiology and Treatment of Neonatal HyperbilirubinemiaPrei BaltazarNo ratings yet
- Icter - Definitii Si EtiologieDocument60 pagesIcter - Definitii Si EtiologieAlexandraNo ratings yet
- Hemolytic Disease of Newborn GuideDocument41 pagesHemolytic Disease of Newborn GuideRaja100% (3)
- HyperbilirubinemiaDocument49 pagesHyperbilirubinemiaKeith LajotNo ratings yet
- 19.neonatal JaundiceDocument42 pages19.neonatal JaundiceWilhellmuss MaukaNo ratings yet
- Neonatal Jaundice ModuleDocument4 pagesNeonatal Jaundice ModuleSubhash BeraNo ratings yet
- Neonatal Jaundice Cme 3Document56 pagesNeonatal Jaundice Cme 3Arief NorddinNo ratings yet
- IctericiaDocument19 pagesIctericiadavid pinedaNo ratings yet
- Pediatric Blood Transport DisordersDocument3 pagesPediatric Blood Transport Disordersmaaisley.yebanNo ratings yet
- Nelson's Hour Q - Disorders of Malabsorption & Acute Gastroenteritis in ChildrenDocument1 pageNelson's Hour Q - Disorders of Malabsorption & Acute Gastroenteritis in ChildrenLara Patricia TamsiNo ratings yet
- Nelson's Hour Q - Disorders of Malabsorption & Acute Gastroenteritis in ChildrenDocument1 pageNelson's Hour Q - Disorders of Malabsorption & Acute Gastroenteritis in ChildrenLara Patricia TamsiNo ratings yet
- IgA NephropathyDocument5 pagesIgA NephropathyLara Patricia TamsiNo ratings yet
- BiochemistryDocument383 pagesBiochemistrybalajimeie92% (12)
- BPIDocument40 pagesBPILara Patricia TamsiNo ratings yet
- Blood Transfusions - TGH Policies & ProceduresDocument4 pagesBlood Transfusions - TGH Policies & ProceduresMark Anthony FranciscoNo ratings yet
- MANGUNE - BSP1E - Module 2 - Online Activity (Tissues) Comic SansDocument6 pagesMANGUNE - BSP1E - Module 2 - Online Activity (Tissues) Comic SansClark Joshua ManguneNo ratings yet
- Euglobulin Lysis Therapeutic: Monitor of FibrinolysisDocument5 pagesEuglobulin Lysis Therapeutic: Monitor of FibrinolysisomarNo ratings yet
- Blood Clotting ChartDocument1 pageBlood Clotting ChartBianca SimionescuNo ratings yet
- RODAKS Hematology Clinical Principles and Applications 4th PDFDocument885 pagesRODAKS Hematology Clinical Principles and Applications 4th PDFGail Ibanez89% (28)
- 13.histology LectureDocument64 pages13.histology LecturepashaNo ratings yet
- HematologyDocument158 pagesHematologyKrisyah Niqoule Valdez67% (3)
- Fluid ResuscitationDocument23 pagesFluid ResuscitationDunstan Abel SambatangNo ratings yet
- Vte Clinical Update Final - 190207 - 1 - LR FinalDocument6 pagesVte Clinical Update Final - 190207 - 1 - LR FinalSantosh SinghNo ratings yet
- HRM Week 2 - Introduction 2020 - PrintDocument34 pagesHRM Week 2 - Introduction 2020 - PrintShiv SookunNo ratings yet
- Blood Cell Count ExperimentDocument6 pagesBlood Cell Count ExperimentCloudCrescentNo ratings yet
- FasciaeDocument54 pagesFasciaeSantiago Orihuela0% (1)
- Chapter 9 ExamDocument9 pagesChapter 9 Examraw4rillNo ratings yet
- Muscular SystemDocument27 pagesMuscular SystemYOSHINo ratings yet
- Understanding Your A1C Test ResultsDocument1 pageUnderstanding Your A1C Test Resultslewisch81No ratings yet
- Dicionario NihonDocument10 pagesDicionario NihonMario GuedesNo ratings yet
- Blood: A Vital Transport SystemDocument33 pagesBlood: A Vital Transport SystemCORONEL, SOPHIANo ratings yet
- Defense of Learning Capstone Blood DriveDocument20 pagesDefense of Learning Capstone Blood Driveapi-194147189No ratings yet
- Connective TissuesDocument5 pagesConnective Tissuesraphael100% (1)
- Human Anatomy 101 EmbryologyDocument4 pagesHuman Anatomy 101 EmbryologyKonstantinos TheodosiadisNo ratings yet
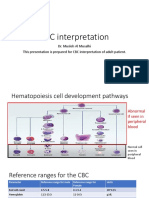
- CBC interpretation guideDocument37 pagesCBC interpretation guideMusleh Al MusalhiNo ratings yet
- Department of Laboratory Medicine: Haematology Test Result Unit Biological Reference Interval Complete Blood Count (CBC)Document3 pagesDepartment of Laboratory Medicine: Haematology Test Result Unit Biological Reference Interval Complete Blood Count (CBC)abhilash eNo ratings yet
- Transes Anaphy BloodDocument5 pagesTranses Anaphy BloodPia LouiseNo ratings yet
- Facts About FFPDocument5 pagesFacts About FFPVicky HadiNo ratings yet
- 2014 Course BookDocument285 pages2014 Course BookWafaa AdamNo ratings yet
- RH Isoimmunization DR SamiraDocument37 pagesRH Isoimmunization DR Samiragynaecology2010100% (2)
- Disseminated Intravascular CoagulationDocument37 pagesDisseminated Intravascular CoagulationmarciantoroNo ratings yet
- 03 C2022 ClinPath 1.03 Hemostasis and ThrombosisDocument7 pages03 C2022 ClinPath 1.03 Hemostasis and ThrombosisJolaine ValloNo ratings yet
- Buletin LP 1Document5 pagesBuletin LP 1Georgiana RosulescuNo ratings yet
- Maharana Pratap College of DentistryDocument24 pagesMaharana Pratap College of DentistryprinceNo ratings yet