Professional Documents
Culture Documents
Cervical 1 2022 061121
Cervical 1 2022 061121
Uploaded by
CONSTANZA0 ratings0% found this document useful (0 votes)
5 views2 pagesThe panel voted to include recommendations to consider comprehensive genomic profiling via a validated assay or plasma ctDNA assay in the workup for persistent or recurrent cervical cancer based on data showing this could help identify biomarkers and improve access to clinical trials. However, the panel did not support other proposed changes to recommend comprehensive genomic profiling assays instead of tumor mutational burden testing or to add new recommendations related to comprehensive genomic profiling.
Original Description:
GINECO
Original Title
Cervical_1_2022_061121
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe panel voted to include recommendations to consider comprehensive genomic profiling via a validated assay or plasma ctDNA assay in the workup for persistent or recurrent cervical cancer based on data showing this could help identify biomarkers and improve access to clinical trials. However, the panel did not support other proposed changes to recommend comprehensive genomic profiling assays instead of tumor mutational burden testing or to add new recommendations related to comprehensive genomic profiling.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views2 pagesCervical 1 2022 061121
Cervical 1 2022 061121
Uploaded by
CONSTANZAThe panel voted to include recommendations to consider comprehensive genomic profiling via a validated assay or plasma ctDNA assay in the workup for persistent or recurrent cervical cancer based on data showing this could help identify biomarkers and improve access to clinical trials. However, the panel did not support other proposed changes to recommend comprehensive genomic profiling assays instead of tumor mutational burden testing or to add new recommendations related to comprehensive genomic profiling.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
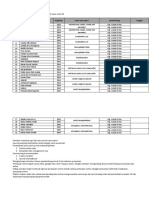
NCCN Guidelines for Cervical Cancer V.1.
2022 –Annual on 06/11/21
Guideline Page Panel Discussion/References Institution Vote
and Request YES NO ABSTAIN ABSENT
CERV-10 and CERV-A Based on the review of data and discussion, the panel 29 0 0 3
External Request consensus was to include the following bullets under Workup
Submission from Foundation Medicine, Inc for persistent or recurrent disease (CERV-10):
(05/14/21) requesting to • Consider comprehensive genomic profiling (CGP) via a
1. Recommend comprehensive genomic validated and/or FDA-approved assay
profiling via a validated and/or FDA-approved • If tissue biopsy of metastatic site is not feasible or tissue
assay in the workup of persistent or recurrent not available, consider CGP via a validated plasma ctDNA
disease (page CERV-10) and Principles of assay
Pathology section (CERV-A) for patients with
“recurrent, progressive, or metastatic disease”
in order to improve patient access to timely
and accurate diagnosis of NCCN-
recommended biomarkers (NTRK fusions,
MMR alterations, Microsatellite instability
(MSI), and tumor mutational burden (TMB)).
2. Allow for CGP via a validated plasma ctDNA
assay as part of the workup for recurrent
disease as a potential alternative to surgical
exploration to determine options for clinical
trial enrollment (CERV-10) and when tissue
biopsy of the metastatic site is not feasible in
metastatic disease in Principles of Pathology
section (CERV-A).
CERV-12 Based on a review of the data and discussion, the panel 0 29 0 3
External Request consensus was not to make changes to the current
Submission from Illumina, Inc (05/13/21) request recommendations.
to amend footnote ff to “Consider tumor
mutational burden (TMB) testing as determined by
a validated and/or FDA-approved
comprehensive genomic profiling (CGP)
assay.”
CERV-A 1 of 3 Based on a review of the data and discussion, the panel 0 29 0 3
External Request consensus was not to make changes to the current
Submission from Illumina, Inc (05/13/21) request recommendations.
to Amend the last bullet point to “Consider TMB
testing through a validated and/or FDA approved
comprehensive genomic profiling (CGP)
assay.”
NCCN Guidelines for Cervical Cancer V.1.2022 –Annual on 06/11/21
Guideline Page Panel Discussion/References Institution Vote
and Request YES NO ABSTAIN ABSENT
CERV-A 1 of 3 Based on a review of the data and discussion, the panel 0 29 0 3
External Request consensus was not to make changes to the current
Submission from Illumina, Inc (05/13/21) request recommendations.
to add a new bullet point to the end under
Pathologic assessment: Comprehensive
genomic profiling with a validated and/or FDA-
approved assay is informative for predicting
rare pantumor targeted therapy opportunities.
CERV-F 1 of 3 Based on the review of the data in the noted reference, the 29 0 0 3
Internal Request panel consensus was to include nivolumab for PD-L1–positive
Consider adding nivolumab for PD-L1 positive tumors as a second-line or subsequent therapy option for
tumors recurrent or metastatic cervical cancer. The panel consensus
supported a category 2A, preferred regimen recommendation.
• Naumann RW, Hollebecque A, Meyer T, et al. Safety and
Efficacy of Nivolumab Monotherapy in Recurrent or
Metastatic Cervical, Vaginal, or Vulvar Carcinoma: Results
From the Phase I/II CheckMate 358 Trial. J Clin Oncol.
2019;37(31):2825-2834.
CERV-F 1 of 3 • Based on a review of the data and discussion, the panel 29 0 0 3
External Request consensus supported making the following change:
Submission from Illumina, Inc (05/13/21) request Footnote h: For the treatment of patients with
to amend footnote h to “For the treatment of unresectable or metastatic tumor mutational burden-high
patients with unresectable or metastatic (TMB-H) [≥10 mutations/megabase (mut/Mb)] tumors, as
tumor mutational burden-high (TMB-H) [≥10 determined by an a validated and/or FDA-approved test,
mutations/megabase (mut/Mb)] tumors, as that have progressed following prior treatment and who
determined by have no satisfactory alternative treatment options.
a validated and/or FDA-approved
comprehensive genomic profiling (CGP) test, • Based on a review of the data and discussion, the panel 0 29 0 3
that have progressed consensus was not to make changes to include
following prior treatment and who have no comprehensive genomic profiling (CGP) to the current
satisfactory alternative treatment options.” recommendations on this page.
You might also like
- Ste Conchem q4m5 Ffhnas Annex PDFDocument31 pagesSte Conchem q4m5 Ffhnas Annex PDFJesus GombaNo ratings yet
- Uterine 2 2020 070720Document2 pagesUterine 2 2020 070720黃靖貽No ratings yet
- Ovarian 1 2022 100721Document7 pagesOvarian 1 2022 100721Lieblingsmensch andipaNo ratings yet
- Pancreas 1 2021 070920Document3 pagesPancreas 1 2021 070920King-Iza CarrNo ratings yet
- v1 2023 BladderDocument3 pagesv1 2023 Bladderhjyjp2sb7mNo ratings yet
- Testicular 1 2021 061920Document1 pageTesticular 1 2021 061920umbrellaNo ratings yet
- BTC 1 2023 021723Document2 pagesBTC 1 2023 021723CITRA AYU APRILIANo ratings yet
- NCCN Guidelines For Uterine Neoplasms V.1.2021 - Annual On 06/12/20Document3 pagesNCCN Guidelines For Uterine Neoplasms V.1.2021 - Annual On 06/12/20Hai TranNo ratings yet
- Cervical 1-2023 Transparency 0627-28 2022 Final 2Document2 pagesCervical 1-2023 Transparency 0627-28 2022 Final 262010710087No ratings yet
- Gastric Transparency 1 2022 090821Document6 pagesGastric Transparency 1 2022 090821MazielAndreaGaragattiMonteroNo ratings yet
- Colorectal 1 20266 080221Document8 pagesColorectal 1 20266 080221edwardNo ratings yet
- Breast 1 2021 082720Document10 pagesBreast 1 2021 082720Karlito Dela CruzNo ratings yet
- Gastric TF 1-2023 - 012723Document2 pagesGastric TF 1-2023 - 012723MazielAndreaGaragattiMonteroNo ratings yet
- Uterine 1 2018 042417Document2 pagesUterine 1 2018 042417黃靖貽No ratings yet
- Gastric TF 1 2023 083022Document2 pagesGastric TF 1 2023 083022MazielAndreaGaragattiMonteroNo ratings yet
- Bladder 5 2021 092421Document1 pageBladder 5 2021 092421Benny KurniawanNo ratings yet
- HeadandNeck 1 2023 063022 PDFDocument3 pagesHeadandNeck 1 2023 063022 PDFMia StrantonNo ratings yet
- Hepatobiliary 1 2020 013120Document3 pagesHepatobiliary 1 2020 013120shah hassaanNo ratings yet
- HCC 1 2023 021723Document2 pagesHCC 1 2023 021723dr.ishapoudelNo ratings yet
- Bone 1 2022 052121Document1 pageBone 1 2022 052121Leise Kestia Rosalyn LimpelehNo ratings yet
- Bladder 1 2021 091820Document4 pagesBladder 1 2021 091820Robert ChristevenNo ratings yet
- Ovarian 1 2017 022417Document1 pageOvarian 1 2017 022417Komang Prawira Nata NugrahaNo ratings yet
- Thyroid 1 2018 101317Document1 pageThyroid 1 2018 101317Carla Mae MoraNo ratings yet
- Sarcoma 1 2019 062218Document4 pagesSarcoma 1 2019 062218Nanda GemaNo ratings yet
- Hepatobiliary 1 2022 020922Document2 pagesHepatobiliary 1 2022 020922mpNo ratings yet
- Gastric - 3 - 2021 - 052821 2Document1 pageGastric - 3 - 2021 - 052821 2Wikrom Keng WromKiNo ratings yet
- Colon Rectal 1 2019 022719Document1 pageColon Rectal 1 2019 022719agustienNo ratings yet
- BCell 1 2021 092220Document8 pagesBCell 1 2021 092220umbrellaNo ratings yet
- Neuroendocrine 1 2021 110920Document2 pagesNeuroendocrine 1 2021 110920Andrei BuruianăNo ratings yet
- Uterine 4 2019 082619Document1 pageUterine 4 2019 082619黃靖貽No ratings yet
- Neat 1 2022 03282022Document3 pagesNeat 1 2022 03282022Janel MendozaNo ratings yet
- Gastric 4 2020 121120Document1 pageGastric 4 2020 121120Angie SuárezNo ratings yet
- CNS 1 2020 100419Document5 pagesCNS 1 2020 100419Amit KumarNo ratings yet
- Esoph 4-2022 TF 081722Document2 pagesEsoph 4-2022 TF 081722umbrellaNo ratings yet
- B-Cell Lymphomas - 1 - 2022 - 012122Document3 pagesB-Cell Lymphomas - 1 - 2022 - 012122umbrellaNo ratings yet
- MPN Annual 082222 FinalDocument2 pagesMPN Annual 082222 FinalwidweedNo ratings yet
- Thyroid NotesDocument2 pagesThyroid NotesAllyssa Denisse LozadaNo ratings yet
- Uveal Melanoma TF 1 - 2022 - 030722Document2 pagesUveal Melanoma TF 1 - 2022 - 030722djapefilipovicNo ratings yet
- Kidney 1 2022 043021Document6 pagesKidney 1 2022 043021Rendy Aprilianus JiwonoNo ratings yet
- Comment: BRCA Mutations and Those Without, and Since BRCADocument2 pagesComment: BRCA Mutations and Those Without, and Since BRCARadu SerescuNo ratings yet
- Guidelines: Recommendations On Screening For Colorectal Cancer in Primary CareDocument9 pagesGuidelines: Recommendations On Screening For Colorectal Cancer in Primary CarezhazhapatrisaNo ratings yet
- NCCN Guidelines For Multiple Myeloma V.3.2016 - Web Teleconference Interim Update On 12/14/15Document3 pagesNCCN Guidelines For Multiple Myeloma V.3.2016 - Web Teleconference Interim Update On 12/14/15Robert DwitamaNo ratings yet
- Esophageal 2 2021 02112Document1 pageEsophageal 2 2021 02112gowtham thakutNo ratings yet
- Opc23hssr Learning Objectives Volume 1Document4 pagesOpc23hssr Learning Objectives Volume 1Toni Player936No ratings yet
- 013 - Surgeon-Led-Clinical-Trials-in-Pancrea - 2023 - Surgical-Oncology-Clinics-of-NorDocument9 pages013 - Surgeon-Led-Clinical-Trials-in-Pancrea - 2023 - Surgical-Oncology-Clinics-of-NorDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- NSCLC 3 2022 030922Document1 pageNSCLC 3 2022 030922WG InvestingNo ratings yet
- Costs Associated With Complications Are Lower With Capecitabine Than With 5-Fluorouracil in Patients With Colorectal CancerDocument12 pagesCosts Associated With Complications Are Lower With Capecitabine Than With 5-Fluorouracil in Patients With Colorectal CancerDelfina HuangNo ratings yet
- Pembrolizumab For Treating Persistent Recurrent or Metastatic Cervical Cancer (Published 2 Jan 2024)Document9 pagesPembrolizumab For Treating Persistent Recurrent or Metastatic Cervical Cancer (Published 2 Jan 2024)K. O.No ratings yet
- Ascopost Com Issues November 25 2022 Asco Publishes Rapid Guideline Update On PaDocument4 pagesAscopost Com Issues November 25 2022 Asco Publishes Rapid Guideline Update On PadanishNo ratings yet
- Metastatic Pancreatic CancerDocument16 pagesMetastatic Pancreatic CancerJorge Osorio100% (1)
- Pancreatic Cancer Literature ReviewDocument10 pagesPancreatic Cancer Literature Reviewea813c29No ratings yet
- Aml 1 2019 072718Document2 pagesAml 1 2019 072718Dhev GianfrancoNo ratings yet
- Screeenig Genetico NCCN 2009Document30 pagesScreeenig Genetico NCCN 2009Gabriela Zavaleta CamachoNo ratings yet
- CML 1 2023 051722Document1 pageCML 1 2023 051722DanuNo ratings yet
- PARPi in Ca Ovary - ASCO 2022Document7 pagesPARPi in Ca Ovary - ASCO 2022danishNo ratings yet
- Singh2020 Colitis UlseratifDocument19 pagesSingh2020 Colitis UlseratifFriska AirynNo ratings yet
- Neuroendocrine 1 2019 121318Document2 pagesNeuroendocrine 1 2019 121318Andrés Bello MunguíaNo ratings yet
- 2024 American Society of Clinical Oncology Genitourinary (ASCO-GU) Cancers SymposiumDocument8 pages2024 American Society of Clinical Oncology Genitourinary (ASCO-GU) Cancers SymposiumJad DegheiliNo ratings yet
- Vaughn 2005Document7 pagesVaughn 2005nimaelhajjiNo ratings yet
- DiagnosticimpactofCEAandCA15 3onchemotherapy2022Document8 pagesDiagnosticimpactofCEAandCA15 3onchemotherapy2022Viriya WimantoNo ratings yet
- Breast Cancer Complications and Prognosis LastDocument42 pagesBreast Cancer Complications and Prognosis Lastalalmaee1No ratings yet
- PET MRI Emerging Clinical Applications in OncologyDocument17 pagesPET MRI Emerging Clinical Applications in Oncologyalfred benedict bayanNo ratings yet
- BRK 2017 RsamDocument38 pagesBRK 2017 RsamratnaNo ratings yet
- 361 - Grammar Revision Advanced Level Test Quiz Online Exercise With Answers 1Document5 pages361 - Grammar Revision Advanced Level Test Quiz Online Exercise With Answers 1ZulBachrakNo ratings yet
- Nejmra 1912719Document12 pagesNejmra 1912719band pulmounandNo ratings yet
- Susanti Santalia - 1706039345 IIIDocument4 pagesSusanti Santalia - 1706039345 IIIsusanti santaliaNo ratings yet
- Liver CancerDocument4 pagesLiver CancerZhyraine Iraj D. CaluzaNo ratings yet
- Breast: Kurt'S NotesDocument4 pagesBreast: Kurt'S NotesfadoNo ratings yet
- Asc 2017 Meeting ProgramDocument102 pagesAsc 2017 Meeting ProgramHerman LoNo ratings yet
- Seminars in Diagnostic Pathology: Hao Chen, Amanda L. Strickland, Diego H. CastrillonDocument11 pagesSeminars in Diagnostic Pathology: Hao Chen, Amanda L. Strickland, Diego H. CastrillonEftychia GkikaNo ratings yet
- NCCNTB Breast-Cancer 06.29.20 2up-1Document41 pagesNCCNTB Breast-Cancer 06.29.20 2up-1dianaNo ratings yet
- BIO 101 Chapter 8Document13 pagesBIO 101 Chapter 8mkmanNo ratings yet
- Case Report BM Covid ARPDocument3 pagesCase Report BM Covid ARPfirmanNo ratings yet
- Eosin Y: Georgios Nikolaou PapanikolaouDocument2 pagesEosin Y: Georgios Nikolaou PapanikolaouShara AboNo ratings yet
- 1 SMDocument6 pages1 SMolgaNo ratings yet
- Hospital TUMOR BOARD: Terms of ReferenceDocument7 pagesHospital TUMOR BOARD: Terms of ReferenceNandakishore RajkumarNo ratings yet
- Activ One Policy WordingDocument55 pagesActiv One Policy WordingAditya SinghNo ratings yet
- CHHiP Supplementary AppendixDocument91 pagesCHHiP Supplementary AppendixRaul Matute MartinNo ratings yet
- 7 F1 EURAMOS1 AA Protocol COSS 31072007 Gesamt PDFDocument457 pages7 F1 EURAMOS1 AA Protocol COSS 31072007 Gesamt PDFJemma ArakelyanNo ratings yet
- Central Nervous System Cancers: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Document178 pagesCentral Nervous System Cancers: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Hermanto YuliusNo ratings yet
- Breast Cancer Prediction in PythonDocument6 pagesBreast Cancer Prediction in PythonIJRASETPublicationsNo ratings yet
- Sarcoma SpecialistDocument5 pagesSarcoma SpecialistaminudinrahmanNo ratings yet
- Eau Eanm Estro Esur Isup Siog Guidelines On Prostate CancerDocument212 pagesEau Eanm Estro Esur Isup Siog Guidelines On Prostate CancerZahraNo ratings yet
- Eng GR-11 Hy 2023 Set A-3Document9 pagesEng GR-11 Hy 2023 Set A-3Priya Suriyakumar100% (1)
- Mindray Elastography Solution - 20210603 - Final-1Document34 pagesMindray Elastography Solution - 20210603 - Final-1Suze C.No ratings yet
- Practice - EXAM 3 - Student VersionDocument5 pagesPractice - EXAM 3 - Student VersionSanders AnitaNo ratings yet
- Questions On Modal VerbsDocument1 pageQuestions On Modal VerbsJack ChanNo ratings yet
- 1 s2.0 S0753332216313294 MainDocument12 pages1 s2.0 S0753332216313294 MainMariaNo ratings yet
- Hosneara Begum - Aastha ConcentDocument2 pagesHosneara Begum - Aastha ConcentAbul HasnatNo ratings yet