Professional Documents
Culture Documents
Assignment For Topic 1 - Video .
Uploaded by
Reygine CariñoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assignment For Topic 1 - Video .
Uploaded by
Reygine CariñoCopyright:
Available Formats
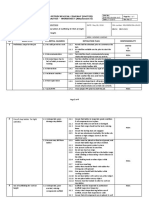
School of Nursing and Allied Health Sciences
1st Semester, AY 2021-2022
INT101 ahs – INTERPROFESSIONAL COLLABORATION in HEALTH
Good evening! Supposedly, this is our first meeting in our class. Instead of meeting you online, may I ask
everyone to do this task in preparation for our next meeting on September 25, 2023.
Instructions:
1. Please watch the video link posted here and do the following:
a. Watch the whole video.
b. While watching the video, take note of what the teams/ group of people are. are doing.
c. Make your own write-up or summary of what they are discussing.
d. Take note of who, what, how, they discuss and share their thoughts during discussion.
e. Include in your write-up anything that comes into your mind of their activities.
f. Prepare this write up /summary in a clean long bond paper. Write at least 500 words.
2. Prepare for the next meeting, share your output, and be able to answer my questions. I will
collect your assignment. Good Luck!
3. Video link: (22 minutes video)
https://www.youtube.com/watch?v=OZWBrXql_3s&t=55s
Prepared by:
Miriam D. Pattugalan, MSN
Level – 3 Instructor
Introduction
- I'm Renata Kulkarni Ave Medical Director for a clinic that oversees the care of patients with
multiple chronic diseases the purpose of this video is to demonstrate the interprofessional
collaborative competencies by visualizing an actual transdisciplinary team in the process of
creating a patient's care plan our clinic focuses on the care of unfunded patients with multiple
chronic diseases who are high utilizers of the hospital or emergency department services these
patients often have difficulty navigating through the healthcare system which can be quite
complex and also face multiple barriers seeking and obtaining care care is delivered through a
transdisciplinary team model our team consists of a provider either a physician a nurse
practitioner or a physician assistant a nurse navigator a social worker and a health promoter or
also known as a community health worker we also have a dietician who participates on the team
there is a clinical pharmacist available in the clinic who consults on all the teams as well together
the team provides not only medical care but also provides a heavy emphasis on education health
literacy and addressing socio-economic barriers to obtaining care we also seek to connect
patients to various resources in the community and subspecialty care you're going to meet the
members of a care team hear about their roles experiences working on a team and observe a
typical case conference where they're discussing a patient's care plan I'm a general internist by
training what is unique to the physician role in this team setting versus a more traditional
hospital setting or clinic setting is that the hierarchy is removed and so my voice in an
interprofessional team is no more important than any other person's voice at the table which is
very rewarding and a gratifying way to practice because you gain a lot from your other team
members and you're really able to lean on them for things that we can't completely handle as
physicians ourselves as the advanced practice registered nurse on our team for I care for our
patients in the clinic and in the home setting and also by phone when necessary during these
visits I use a holistic approach to evaluate and manage new and ongoing patient conditions I
provide comprehensive comprehensive perspective to our patient's healthcare needs this means
that in addition to considering the patient's medical conditions I also imagine evaluate
psychological financial social family circum and family circumstances in order to formulate a
realistic care plan physical examinations interpretation of Diagnostics prescribing patient
education care coordination and communication with other providers or some of the specific
tests I perform daily I also act as a team resource to troubleshoot complex issues in regards to
working with a team we utilize a patient-centered approach to care and consider our patient to
be part of our team as a team we all contribute unique unique skills knowledge and qualities
that allow us to identify strategies that can lead to improved outcomes for our patients we
communicate with each other frequently both in formal meetings and informally by email and
phone calls at our formal case conferences we review our patient cases and discuss the care plan
and patient as a clinical nurse navigator I serve as the team lead including facilitating the weekly
team meetings additionally I helped to develop revise and communicate interdisciplinary care
plans with the team my role in patient care involves a combination of home visits office visits
and telephone conversations with the patient for the purpose of education assessment and care
coordination my nursing background includes just over three years of intensive care experience
and a Bachelors of Science in Nursing as a medical social worker on a transdisciplinary team my
role is to assist patients in addressing via social concerns and barriers that may hinder them from
being as healthy as they can or hinder them from focusing on their health care needs these
barriers often include family relationships finances housing transportation and mental health
concerns my interactions with patients include bio cyl bio psychosocial assessment individualized
treatment planning care coordination discussion of referral to federal state county and city
programs and education within the hospital system for which I work I've worked for almost five
years all medical social workers must have earned a master of Social Work degree prior to hire
and hold a licensed master of Social Work licensure or licensed clinical social work licensure as a
health promoter community health worker I'm a frontline public health worker whom
establishes trusting relationships with patients to better serve as a liaison link intermediary
between health and social services and the community to facilitate access to services to improve
the quality and cultural competence of service delivery I'm also certified as a clinical nurse
assistant having worked in an ortho trauma unit for seven years before certifying as a health
promoter and community health worker in this interprofessional team I hope patients
understand and incorporate their care plan into their lives considering social and cultural context
I also help identify barriers to the team that they were unaware of in my list of duties i reinforce
education taught to patients with chronic illnesses assist patient with preparation for important
appointments visit patient and hospital and/or patients preferred locations such as home visits
or clinical appointments help locate patients whom have a common active or are homeless
accompany patients to primary care specialty and other health community resource
appointments coach patients in order to promote self-care independence patient advocacy
resource allocation liaison for patient between medical community and community resources
help identify safety hazards in patients dwelling and help manage patient source of
transportation and or communications I am a registered dietitian I have a bachelor's degree in
nutrition and I have been a certified diabetic educator for 11 years and have worked in the
outpatient setting for the past 16 years my role as dietitian with and the team is slightly different
than the other team members and that the dietician is not specifically designated to one team
but instead is designated to three or four different teams I try to schedule as many of my
appointments as home visits because I find that I have a better chance to obtain an accurate
picture of patients lifestyle and also that I tend to have much better rapport with the patient
when I have home visits the majority of the patients I see are for diabetes but in addition to that
I also have referrals for hypertension congestive heart failure high cholesterol celiac disease as
well as a periodic antral tube feeding I rely on communication from my team members for
accurate information as to why I've received the referral as well as what the patient is wanting
out of there I look to my designated advanced practice nurse when I am confronted with a
medical condition outside of my scope of care and for example a patient with a very high blood
sugar during the visit I also periodically make referrals to my other team members when an
patient need arises that is also outside of my scope of care for example if the patient needs to be
accompanied to a specialty appointment okay so in our meeting today I think we're going to talk
about mr. John Smith who has had some recent changes so Megan do you want to speak a little
bit more about the changes sure so as I mentioned we we visited yesterday to his residence at
the front steps we learned actually when we got there that he is going to be leaving as of
tomorrow and this was brand new information to him yesterday as well so we this has been sort
of thinking a little bit coming he's living with a few other residents and most of them are pretty
independent and it seems as though mr. Smith has been being watched out for by these
roommates which is very sweet but it's not their responsibility it's not part of what they're
supposed to be there that it was be there for their own services but it seems as though and
separately that they're closing the house so the last of the remains actually moves out tomorrow
as well so that we know and there and in addition to that it he's been leaving the stolen so it's
been seized saved by himself and he has also the severest psychiatric symptoms have been
redundant themselves maybe his medications aren't working at this point maybe his so that
that's something that has recently been visited but he most recently seemed to be having some
visual hallucinations and I saw something on the wall that was very upsetting to him so it
actually resulted in him going to the emergency department and so this I think this has all been
coming coming to a head so Leah that I think most of you know her she runs the recuperative
care program her concepts so she's had a conversation yesterday we happened to be there and
the plan is for him to move in with his mom and stepdad I think we've spoken before he had
some anxiety around Penn stepdad he used to live with them there's dad uses album of stuff
daddy was alcohol and there's been some verbal abuse in the past so he has he's got some he
was pretty anxious about it but recognizes that it's the only other option right now so where I
see us coming in is to really step up our involvement with him provide some wraparound care
and try to fill in where he's been so dependent on Leah and front steps for so long that we really
need to step up our involved and make sure that he gets the care he needs until he gets well
continuing on past the time he gets more housing different housing situation and I can help to
find some programs to help get him out of the house I know that's going to be a focus for him
going forward at least in the interim with hopefully this is just a temporary situation and we can
find him something more sustainable long-term I can help with that and and one thing that I did
hear about recently that I think would be a perfect fit for him is there's a diabetes education
class it sounds like it's it's on Tuesdays I think once a week for a couple hours and if he goes to
seven out of the eight classes he gets a grocery store gift card for about two hundred dollars so I
think that would be right up his alley in several ways so I think Kristin I think you're connected
with the dietitian that runs that program right I know the dietitian that facilitates that so I can
get him in in touch with her okay yeah that upgrade I think that would be a good place to start
so and relating to his housing I will be seeing him tomorrow because his finding is about to
expire is my part so as I'm there while we're waiting for his appointment to start we can start
calling around and seeing if there's any housing opportunities for him since we know his current
situation has to be temporary since he's not comfortable at home well Megan you had
mentioned the hallucinations and some memory and mental health issues and I know he's on
many meds for many chronic conditions and I'm kind of concerned that you know these meds
may be causing some issues for him and and sounds like we may not even know exactly he's on
all of those medications and he's got several specialists so they may not even have the most up-
to-date medication list so our work to reconcile his medication list and then press NC maybe we
can coordinate so that we can communicate the most accurate medication lists to all of his
specialists and his primary care doctor I mean usually since I accompanied him to these
appointments to make sure that there are any changes I also assist in communicating that to all
of his providers I see being stable with his primary care provider yes but um you know just
transportation has been an issue you know getting him to his appointments um he always comes
paint companies about foot paint he doesn't have the best diabetic shoe so I'm gonna try to help
him Courtney that but if he loses front steps they are the ones that also assisted him with heel
into the Hermon so that's that's gonna be another issue that we're gonna have to kind of figure
out but he does try to make it to his appointments they never have the updated Med list so
that's been an issue okay so really communicating to the providers is gonna be the key that's
something on and I can work on together reaching out to them that day that actually had a
couple of those points he did earlier last week I accompanied him and she went appointment
with his psychiatrist HEC I see and so hopefully there we can address those the psychiatric
concerns that seem to be having themselves right now they did we just sort of brought it on was
of course the emergency room visit but also of course his psyche Rexha has it increases blood
sugar that's one of a side effects so they decided to put it back on Haldol he's bought it for a few
days now but he does have a history of target dyskinesia as a result of that he's had some hand
tremors so he's a little bit concerned about that but the psychiatrist and mr. Smith decided that
neighboring they would try that at this point also he had kind of the memory that you had
addressed he is a high today to you a cognitive tests on him the Mini Mental Status exam and
you actually did pretty well on it on a scale of 38 out of 25 which is wonderful because it's
demonstrating that he's not having some cognition issues of course but I think demonstrating it
and yesterday living yeah we had discussed that he there's that memory the gaps in there that
short-term memory is really troubling from my perspective so we were hoping that if he scored
low enough on this exam that that would suggest that he would be eligible for disability and
then he could with that associated funding source of Medicare and Medicaid depending on his
work history that he would be able to go ahead and get some neuropsych testing but you can't
get the neuropsych testing unless you have a funding source such as Medicaid or met Medicare
and that will pay for it so so it's kind of crazy for having a high level high score on your
Commission test but also what's going on with memory and getting him some good long-term
insurance coverage so that's one of you guys on that and regarding the memory issues as well as
you guys know I had been doing weekly home visits with him to help fill ins pillbox and make
sure his medications are refilled and that kind of thing so we can try to move those to the
hospital I guess if he's open to that I think he will be to get out of the house so when I do those
it's it's obviously really helpful for me that you have those medication lists and then if you guys
could help to reconcile the medication list so that I'll know what needs to go in his pillbox and
with that we'll also try to make as many of the refill calls as we can during those visits but
sometimes I know there's still some follow-up that he needs to do afterwards to get some
medication so for the most part you know I because he does like his independence as much as
he can have it so I will occasionally send him a reminder to just call the pharmacy and do the
refill sounds great helps him but it wasn't to be a little sent into him he and also he completed
his senior health ILP program when Julie and Julie had recommended that he now that he's
completed that but he continued with an outpatient program where you can actually work and
get a meal he didn't be there a couple days a week and he's also expressed some interest in
doing some al-anon classes to deal with the stress of being at home with his dad and the
potential alcohol abuse that couldn't continue to happen there so they'll be other ways for him
to get out of the houses I think if he's expressed interest yourself he has he actually mentioned
an Austin Clubhouse which I was gonna try to get information for so when I do see him
tomorrow is a cool appointment I was gonna kind of help him do some research and provide
whatever I can find so and if you have any ideas that we know ok so having him see you and I
think we should continue to help him brainstorm somehow she's having kind of the house I'll
definitely do that on my weekly visits and additionally obviously the pillboxes and you know
assessing him for the various concerns that we have we know he has the the memory issues and
other clinical things going on so I can help keep an eye on those and check vitals and things like
that as well and speaking of those weekly visits I wanted to mention to you Kristin the last home
visit that we had with him he mentioned that he was having a low blood sugar whenever he was
getting off the bus one day and so he went to the convenience store to buy a diet coke and drink
that in hopes of remedying his low blood sugar so between you and I maybe we can both give
him some education on on diabetes and hypoglycemia which on Tuesdays I try to do is usually on
Tuesdays okay so how about if I go see him on every Thursday sure sounds great reinforce that
appropriate treatment with the memory concerns I think that's probably gonna be our plan is to
just continue to reinforce things with him oh and he mentioned to me that he's concerned with
his living with his mother that his stepfather is not really giving him access to the food in the
house and also I've heard that the food in general there is very high high in fat which is really
bad for his gastroparesis and limited stomach motility so I was thinking I'm gonna with meals on
wheels they actually have a low fiber pureed option for people with gastroparesis that's great I
didn't know that yeah so I don't get a hot meal every day of the week doesn't have snack as well
so only that supplement as well okay well does she reckon me get it will address concerns and
another thing that we you and I could work together on usually when he comes in for his weekly
or when I see him at home or now it's probably gonna be in the hospital his weekly visit we
reconcile his calendar I know he has a lot of specialists and appointments and things like that so
that's one thing maybe you and I can both work on is reinforcing that calendar and just making
sure that it's updated with every appointment you go to that the follow-up appointment is listed
on his calendar and I'll hope to reinforce that and get that reconciled every time I see him
weekly so we can create a web document that we can all see so sure whoever sees him I can
take a recent coffee at waffle absolutely right and I know he keeps his own calendar as well so
just making sure that that document is updated with his calendar so the one last thing I would
like to bring him up to the office and just evaluate his recent ER visit his recent psychiatry visit
and sort of consolidate everything make sure that there's nothing that we're doing that's making
him worse or causing the hallucinations he's got definitely got polypharmacy as an issue and in
addition to that he's medically complex has multiple comorbidities which could be causing there
could be a metabolic things causing his hallucinations so we definitely want to rule those things
out yeah and I'll make sure that my next visit with him for pillbox and assessment and everything
actually happens at the hospital I think he'll be fine with that and in that way we can send him to
the lab while he's here great thanks a lot good night then and he comes in a week and a half or
something we should be able to see she able to tell you how he's feeling about his symptoms if it
is in fact a psychiatric as opposed something else great great okay thanks all right thanks [Music]
[Music] [Music]
You might also like
- Reflective JournalDocument3 pagesReflective Journalapi-302591810100% (6)
- RequirementsDocument4 pagesRequirementsReneé CamilleNo ratings yet
- 1.02 FCM Trans - The Five Star DoctorDocument3 pages1.02 FCM Trans - The Five Star DoctorMineTagraNo ratings yet
- NCM 102 Reflections Week 2Document4 pagesNCM 102 Reflections Week 2Lordgelyn Diane ViernesNo ratings yet
- Midterm Evaluation - With CommentsDocument16 pagesMidterm Evaluation - With Commentsapi-31372043975% (4)
- Health Coaching - A Powerful Approach To Support Self-Care: BotheredDocument5 pagesHealth Coaching - A Powerful Approach To Support Self-Care: BotheredGONDHES CHANNELNo ratings yet
- Evoe Spring SpaDocument7 pagesEvoe Spring SpaAravind LiverpoolNo ratings yet
- 1.botswana CELEBRATIONS OverviewDocument34 pages1.botswana CELEBRATIONS OverviewYunus ElonNo ratings yet
- Mclemore Synthesis EssayDocument4 pagesMclemore Synthesis Essayapi-283558804No ratings yet
- Reflection PaperDocument8 pagesReflection Paperapi-508903095No ratings yet
- B Dailey Philosophy of Nursing Paper3 23 15Document8 pagesB Dailey Philosophy of Nursing Paper3 23 15api-283673800No ratings yet
- Angelica M.docx LFD 17Document3 pagesAngelica M.docx LFD 17Angelica Malacay RevilNo ratings yet
- Final Reflective JournalDocument2 pagesFinal Reflective Journalramyharoon2004No ratings yet
- Mid Term EvaluationDocument6 pagesMid Term Evaluationapi-338285420No ratings yet
- Final Casa RehabDocument11 pagesFinal Casa Rehabapi-283970192No ratings yet
- Expanded and Extended Role of Pediatric Nurse: S. K Mohana SundariDocument34 pagesExpanded and Extended Role of Pediatric Nurse: S. K Mohana SundariShivangi SharmaNo ratings yet
- Intro Page - Practice Summary PaperDocument4 pagesIntro Page - Practice Summary Paperapi-467110214No ratings yet
- Nursing PhilosophyDocument11 pagesNursing Philosophyawoerne1No ratings yet
- NURS 2021H Clinical Course Evaluation Final Evaluation: Please Circle The Appropriate OutcomeDocument11 pagesNURS 2021H Clinical Course Evaluation Final Evaluation: Please Circle The Appropriate Outcomeapi-301240348No ratings yet
- 4140 Nursing PhilosophyDocument8 pages4140 Nursing PhilosophyZoe RaineNo ratings yet
- MesarahDocument7 pagesMesarahapi-271855323No ratings yet
- Personal Philosophy 2Document8 pagesPersonal Philosophy 2api-283679121No ratings yet
- Conversation Job Interview Group 7Document3 pagesConversation Job Interview Group 7Chrishadi Yulian PutraNo ratings yet
- LFJ FormatDocument3 pagesLFJ Formatdennise reyesNo ratings yet
- Reflection of Practicum ExperiencesDocument5 pagesReflection of Practicum Experiencesapi-385503945No ratings yet
- Practice Summary Paper For PortfolioDocument9 pagesPractice Summary Paper For Portfolioapi-290938460No ratings yet
- Professionalism (استرداد)Document12 pagesProfessionalism (استرداد)bilalokijNo ratings yet
- Week 9 DiscussionDocument2 pagesWeek 9 Discussionapi-239034911No ratings yet
- Roles of health care team members in patient educationDocument5 pagesRoles of health care team members in patient educationkrezia daasinNo ratings yet
- BSN Pgcs Reflection - KimDocument11 pagesBSN Pgcs Reflection - Kimapi-458308352No ratings yet
- Aw Professional Meeting Reflection 1Document2 pagesAw Professional Meeting Reflection 1api-652071746No ratings yet
- Service Learning ProposalDocument6 pagesService Learning Proposalapi-301861602100% (1)
- Term PAPERDocument11 pagesTerm PAPERacebobro.bonifaceNo ratings yet
- Philosophy of Nursing PaperDocument8 pagesPhilosophy of Nursing Paperapi-496088094No ratings yet
- Reflection Family MedicineDocument3 pagesReflection Family MedicineStanley SekwenaNo ratings yet
- Ana Self AssessmentDocument7 pagesAna Self Assessmentapi-301349934No ratings yet
- Personal Philosophy and Reflection On NursingDocument8 pagesPersonal Philosophy and Reflection On Nursingapi-663253917No ratings yet
- Professional Progress Introduction Nursing 489 Purpose of AssignmentDocument5 pagesProfessional Progress Introduction Nursing 489 Purpose of Assignmentapi-283315953No ratings yet
- Personal Nursing PhilosophyDocument7 pagesPersonal Nursing Philosophyapi-708278194No ratings yet
- E-Portfolio - Philosophy of NursingDocument2 pagesE-Portfolio - Philosophy of Nursingapi-353669394No ratings yet
- Building Trust Through Family AssessmentDocument1 pageBuilding Trust Through Family AssessmentDiana Andrea AyongaoNo ratings yet
- Nur403 IntropagesummaryprojectDocument6 pagesNur403 Intropagesummaryprojectapi-529373199No ratings yet
- FesarahDocument8 pagesFesarahapi-271855323No ratings yet
- A Description of Your Role Including Direct Patient CareDocument4 pagesA Description of Your Role Including Direct Patient Careد.شەماڵ احمد : پزیشکی دەرمانسازNo ratings yet
- MinesingernDocument7 pagesMinesingernapi-644332177No ratings yet
- The Roles of Nurses in IndonesiaDocument3 pagesThe Roles of Nurses in IndonesiaAdi SubagioNo ratings yet
- 1 Running Head: Practice Summary PaperDocument11 pages1 Running Head: Practice Summary Paperapi-544117547No ratings yet
- O Applies Appropriate Knowledge of Major Health Problems To Guide Nursing PracticeDocument5 pagesO Applies Appropriate Knowledge of Major Health Problems To Guide Nursing Practiceapi-529216367No ratings yet
- Dykstra, Amber ServicelearningDocument7 pagesDykstra, Amber Servicelearningapi-284180001No ratings yet
- Philosophy of NursingDocument8 pagesPhilosophy of Nursingapi-300623329No ratings yet
- AnnettiDocument6 pagesAnnettiapi-643874601No ratings yet
- Five-Star DoctorDocument2 pagesFive-Star DoctorPatricia Denise Orquia100% (3)
- Personal Essay: Student Name Institution Affiliation Course Name and Number Professor's Name Due DateDocument7 pagesPersonal Essay: Student Name Institution Affiliation Course Name and Number Professor's Name Due DateyellowishmustardNo ratings yet
- Group 4 - Team WhatsAppDocument14 pagesGroup 4 - Team WhatsAppSulaiman Abibat DamilolaNo ratings yet
- LFDDocument3 pagesLFDVhince Norben PiscoNo ratings yet
- CCNI Practice Reflection Work Sheet .Document4 pagesCCNI Practice Reflection Work Sheet .stevemsteNo ratings yet
- Nur460 PGC Reflection PaperDocument10 pagesNur460 PGC Reflection Paperapi-541746043No ratings yet
- 4140 Personal Philosophy PaperDocument9 pages4140 Personal Philosophy Paperapi-507789841No ratings yet
- Childhood Hospital Experiences Inspire Nursing CareerDocument2 pagesChildhood Hospital Experiences Inspire Nursing CareerEvelyn MukNo ratings yet
- RiverspdpDocument15 pagesRiverspdpapi-241413796No ratings yet
- Megan Baitey Practice Philosophy and GoalsDocument3 pagesMegan Baitey Practice Philosophy and Goalsapi-540729446No ratings yet
- Running Head: Nursing Philosophy Paper 1Document7 pagesRunning Head: Nursing Philosophy Paper 1api-354406700No ratings yet
- CECILIA CHERYL LIYADI Fix DirDocument2 pagesCECILIA CHERYL LIYADI Fix Dirbeauty asriNo ratings yet
- Schedule of Reports EDUC 208 School Personnel AdministrationDocument3 pagesSchedule of Reports EDUC 208 School Personnel AdministrationAdrian PanganNo ratings yet
- Process Quality - III - 2005 - 2010 - Outcome or Impact QualityDocument2 pagesProcess Quality - III - 2005 - 2010 - Outcome or Impact QualityLuiciaNo ratings yet
- Doccure-HAMS Group PresentationDocument12 pagesDoccure-HAMS Group PresentationShams IstehaadNo ratings yet
- 3 Giving Suggestion (About Health)Document9 pages3 Giving Suggestion (About Health)dedeh rositaNo ratings yet
- SOP Service Apartment OperatorDocument4 pagesSOP Service Apartment OperatoradibazinunNo ratings yet
- Teacher'S Health Examination RecordDocument2 pagesTeacher'S Health Examination RecordYule Espinosa AbayNo ratings yet
- Jubail United Petrochemical Company (United) Job Safety Analysis - Worksheet (Attachment V)Document4 pagesJubail United Petrochemical Company (United) Job Safety Analysis - Worksheet (Attachment V)Muhammad Umar GondalNo ratings yet
- FactSheet SeniorCentersDocument2 pagesFactSheet SeniorCentersNurul pattyNo ratings yet
- NOTRE DAME OF TACURONG COLLEGE Health Services Action Plan S.Y. 2012-2013Document3 pagesNOTRE DAME OF TACURONG COLLEGE Health Services Action Plan S.Y. 2012-2013Gjc ObuyesNo ratings yet
- AR2020Document186 pagesAR2020Eugene TanNo ratings yet
- 22Document88 pages22Resvian RemboyNo ratings yet
- Part 1. Assessing Eyes: Unit 4 Patient Assessment 3 (Eyes and Ears)Document4 pagesPart 1. Assessing Eyes: Unit 4 Patient Assessment 3 (Eyes and Ears)rinaNo ratings yet
- Futuristic Nursing PDFDocument39 pagesFuturistic Nursing PDFRudra prasad SahuNo ratings yet
- 10.1 AstringentsDocument32 pages10.1 AstringentsSaha DirllahNo ratings yet
- NIAGARA Cranial Flap (v2) 5Document1 pageNIAGARA Cranial Flap (v2) 5marceloNo ratings yet
- Pain ProposalDocument19 pagesPain ProposalAhsan AzamNo ratings yet
- Answer Keys Structure 7 February 2021Document7 pagesAnswer Keys Structure 7 February 2021anon_294803392No ratings yet
- Assignment/ Tugasan - Health and Wellness 2Document14 pagesAssignment/ Tugasan - Health and Wellness 2Metran Electrical & ITNo ratings yet
- Jadwal Dokter TerbaruDocument1 pageJadwal Dokter Terbaruphn kitchen idNo ratings yet
- Bed Bath Assessment FormDocument4 pagesBed Bath Assessment FormTemahlungwaneNo ratings yet
- Scaffolding standards and rolesDocument20 pagesScaffolding standards and rolesMounir Boutaghane100% (1)
- Protocol For Suicide Risk Assessment and ManagementDocument67 pagesProtocol For Suicide Risk Assessment and ManagementMdEssaNo ratings yet
- Batea Northparkes E48Document11 pagesBatea Northparkes E48CARLOS OSIEL SEBASTIÁN VALDÉSNo ratings yet
- Final Springlife & ShubhDocument5 pagesFinal Springlife & Shubhdeepanshu jainNo ratings yet
- Bess-Sm-3q90041-Qams-003 Method of Statement - Cable Termination PDFDocument5 pagesBess-Sm-3q90041-Qams-003 Method of Statement - Cable Termination PDFChristian BulaongNo ratings yet
- Invisalign G5 BrochureDocument6 pagesInvisalign G5 BrochureAndreea-Paula PădureNo ratings yet