Professional Documents
Culture Documents
Module 4 Transes
Uploaded by
Joiam GarsanoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Module 4 Transes
Uploaded by
Joiam GarsanoCopyright:
Available Formats
NUR 1210: MATERNAL AND CHILD NURSING
LECTURE | DR. WILFREDO QUIJENCIO – FACULTY OF NURSING
FAR EASTERN UNIVERSITY | BACHELOR OF SCIENCE IN NURSING | 1ST SEMESTER A.Y. 2023-2024
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
DYSTOCIA FACTORS AFFECTING LABOR
• Abnormally slow progress of labor
• Most common contemporary indication of primary PASSENGER PASSAGEWAY POWERS PLACENTA PSYCHE POSITION OF
LABORING
WOMAN
cesarean section Fetal bones Gynecoid Strength, Site of Psychological LABOR:
• It is slower than the expected time frame Suture lines
Fontanels
Anthropoid
Android
Duration and
Frequency of
insertion of
the placenta
state of the
woman
Walking
Standing
• Can arise in the 4Ps of the labor process: Head Meas.
Fetal lie
Platypelloid uterine
contraction Stress factors
Leaning
Tailor sitting
o Power – force that propels the fetus (uterine Fetal attitude,
presentation,
Configuration
and diameter of
(primary
powers of
leading to
hypotonia
Semi-
recumbent
position, the maternal labor), hand knees
contractions) station pelvis involuntary Squatting
o Passenger (the fetus) distensibility of
the lower
urge to push
(secondary
Kneeling
Leaning
o Passageway (the birth canal) uterine
segments,
power)
Frequency
forward with
support
o Psyche (woman’s and family’s perception cervical
dilatation, and
Duration
Interval DELIVERY:
of the event) capacity
distention of
for Intensity Lithotomy
Semi-
the vagina and recumbent
introitus Lateral
DIAGNOSIS OF LABOR Recumbent
• Regular painful uterine contractions accompanied
by any of the following: DYSTOCIA DUE TO ABNORMALITIES OF THE
o Ruptured Membrane PASSENGER
o Bloody show
o Complete cervical dilatation and PASSENGER
effacement • Abnormalities of Presentation and Position
o Occiput Posterior Position
PROBLEMS THAT DEVELOP DURING LABOR OR o Breech Presentation
DELIVERY o Face Presentation
• LABOR: Series of events by which uterine o Brow Presentation
contractions and abdominal pressure expel the fetus • Macrosomia
and placenta from the woman’s body • Conjoined Twins
o Amniotic fluid embolism (fluid enters the • Multiple Pregnancy
woman’s bloodstream – life-threatening to
the woman) POSITION
o Shoulder dystocia (shoulder lodges against • Relationship of reference point on fetal presenting
the pubic bone, and baby is caught in the part to maternal bony pelvis
birth canal)
o O (occiput) in vertex position
• DELIVERY: Actual event of birth o M (mentum or chin) in face presentation
o Labor could start too early (umbilical cord o S (sacrum) in breech position
comes out of the birth canal before the o A (acromion) in shoulder presentation
baby)
• Maternal bony pelvis divided into four quadrants
(right and left anterior; right and left posterior)
o ROA
o LOA
o ROP
o ROA
• Transverse – Right acromio dorso posterior
(RADP). The shoulder of the fetus is to the mother’s
right, and the back is posterior.
• LOA/ROA – most common position favorable for
delivery
• LOP/ROP – usually causes back pain during labor;
may slow the progress of labor; usually rotates
SARDENIA, JOZELLE KAYE 1
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
before delivery to anterior position; rotation may be • Dysfunctional labor
done by physician • Early rupture of the membrane
METHODS TO ESTABLISH FETAL CAUSES OF BREECH PRESENTATION
PRESENTATION AND POSITION • Gestational age less than 40 weeks
• Combined abdominal inspection and palpation • Abnormality in a fetus (Anencephaly,
(Leopold’s maneuver) Hydrocephalus, or Meningocele)
• Vaginal examination • Hydramnios that allows for free fetal movement
• Auscultation of fetal heart tones • Congenital anomaly of the uterus (mid-septum)
• Sonography • Any space-occupying mass in the pelvis (fibroid
• X-ray tumor of the uterus or a placenta pre-via)
• Pendulous abdomen. If the abdominal muscles are
TYPES OF PRESENTATION lax, the uterus may fall so far forward that the fetal
• CEPHALIC head comes to lie outside the pelvic brim, causing
o Vertex / Occiput a breech presentation.
o Brow • Multiple gestation. The presenting infant cannot
o Sinciput turn to a vertex position.
o Face • Unknown factors
• BREECH
o Frank VAGINAL BREECH DELIVERY
o Complete • No traction or manipulation of the infant is used
o Incomplete
• Occurs predominantly in very preterm deliveries
• SHOULDER (24 weeks and below)
• COMPOUND
ASSISTED BREECH DELIVERY
MALPRESENTATION
• Most common type of vaginal breech delivery
• Is presentation other than the vertex presentation • Spontaneously deliver up to the umbilicus
• Any malpresentation will lead to difficult labor and • Maneuvers are initiated to assist in the delivery of
delivery the remainder of the body, arms, and head
o Breech 3%
• If legs do not deliver spontaneously can be assisted
o Face 0.2%
by Pinard maneuver
o Brow 0.01%
o Shoulder 1:300
TOTAL BREECH EXTRACTION
o Compound 1:1000
• Fetal feet are grasped, and the entire fetus is
BREECH PRESENTATION extracted
• Buttocks or lower extremities present first. Types • Noncephalic second twin
are: • TBE for the singleton breech is associated with a
o FRANK: thighs flexed, legs extended on birth injury rate of 25% and a mortality rate of
anterior body surface, buttocks presenting approx. 10%
o FULL / COMPLETE: thighs and legs
flexed, buttocks and feet (squatting FACE PRESENTATION
position) • Asynclitism
o FOOTLING: one or both feet are • Condition of maximal deflexion/extension
presenting • Submentobregmatic diameter presented to pelvis
(9.5 cm)
PREDISPOSING FACTORS
• Placenta previa PREDISPOSING FACTORS
• Polyhydramnios (more than 1000 ml amniotic fluid) • Conditions which favour extension and reduce
/ Oligohydramnios (less than 500 ml amniotic fluid) flexion of the vertex
• Abnormal motor ability • Multiparity
• Anoxia from a prolapsed cord • Prematurity
• Traumatic injury to the aftercoming head • CPD
(intracranial hemorrhage or anoxia)
• Fracture of the spine or arm
SARDENIA, JOZELLE KAYE 2
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
DIAGNOSED PREDISPOSING FACTORS
• In labor • Placenta previa
• Palpation of the eyes, nose, mouth • Multiple pregnancy
• Uterine anomalies
CLASSIFIED • Prematurity
• According to the position of the chin (mentum) • Polyhydramnios
• Mento-anterior – can be delivered vaginally • Multiparity
• 1/3 of face presentation begin as M-P and 2/3 of
these will rotate to M-A MANAGEMENT
• > 37 weeks without C/I consider ECV
MANAGEMENT • If in labor or C/I to ECV exists deliver by C/S
• Re-evaluate and make preliminary choice • Type of uterine incision is considered – classical,
• Vaginal delivery appropriate where labor low transverse with the primary purpose to avoid
progressing satisfactorily, average size baby and fetal trauma and asphyxia
adequate sized pelvis • External cephalic version
• Rotation to M-A may occur late in the second stage
• Maneuvers to manually flex the face to facilitate COMPOUND PRESENTATION
delivery abandoned in modern obstetric practice • Implies that another anatomic part, usually an
• Forceps rotation C/I extremity has entered the pelvis along the with
• Outlet forceps for M-A positions acceptable principal vertex or breech presentation
• C/S for persistent non-M-A positions
PREDISPOSING CONDITIONS
BROW PRESENTATION • Prematurity
• Moderate degree of deflexion • Abnormal lies
• Mento-occipital diameter presented to the pelvis • Fetal anomalies
(12.5 cm) • Large pelvic capacities
• May be a transient feature of labor
• 2/3 of the cases are unstable and convert MANAGEMENT
• 1/3 of all women going to labor and delivery has • Labor usually progresses normally
persistent brow • Problem usually solved with the head being forced
past the extremity
PREDISPOSING FACTORS • Cord prolapse a possible complication
• Conditions which favor extension and reduce • May encourage the fetus to remove the extremity
flexion of the vertex • Consider C/S for usual causes or arrest of labor
• Multiparity • Edema / Discoloration of the extremity quickly
• Prematurity resolve
• CPD
MULTIPLE PREGNANCY
DIAGNOSIS • When more than one fetus simultaneously develops
• Palpation of nose, eyes, orbital ridges in the uterus
• Simultaneous development of two fetuses (twins) is
MANAGEMENT the commonest
• Re-evaluate • Although rare
• Manual flexion and rotation to OA sometimes o Triplets (Three fetuses)
possible o Quadruplets (Four fetuses)
o Quintuplets (Five fetuses)
• C/S for persistent brow
o Sextuplets (Six fetuses)
TRANSVERSE / SHOULDER PRESENTATION
VARIETIES
• Long axis of the fetus is perpendicular to that of the
mother • DIZYGOTIC TWINS - most common (two-third);
• Shoulder is usually over the pelvic inlet, with the results from the fertilization of two ova
head lying in one iliac fossa and the breech in the • MONOZYGOTIC TWINS (one-third) results
other from the fertilization of single ovum
SARDENIA, JOZELLE KAYE 3
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
TWIN PREGNANCY LABOR AND DELIVERY
• DIAMNIOTIC DICHORIONIC • Timing of delivery – the benefit of prolonging the
o 72 hours after fertilization pregnancy is outweighed the risk of stillbirth
o Two separate placenta, chorions, and • Uncomplicated dichorionic twins – managed
amnions expectantly and delivery can be around 38 weeks
• DIAMNIOTIC MONOCHORIONIC • Uncomplicated monochorionic twins – delivery at
o 4-8 day after inner cell mass when chorion around 37 weeks
had developed • In cases of prematurity and discordant fetal well
• MONOAMNIOTIC MONOCHORIONIC being exists, timing of delivery should be based on
o After 8th day of fertilization when amniotic parameters of healthy twin
cavity is formed • In case of discordant fetal well-being or an
anomaly, timing of delivery should be based on the
CONJOINED TWINS condition of compromise fetus
• Division occurs after 2 weeks of the development of
embryonic disc METHOS OF DELIVERY
• Siamese twins • CEPHALIC – cephalic presentation – vaginal
• Four types of fusion may occur delivery
o Thoracopagus (commonest) • CEPHALIC – non cephalic presentation –
o Pyopagus (posterior fusion) controversial
o Craniopagus (cephalic) o Vaginal delivery of second non cephalic
o Ischiopagus (caudal) twins whose birthweight <1500gm is safe
o 2nd twin – Breech extraction of non-
ETIOLOGY cephalic twin or internal podalic version of
• Maternal age an unengaged cephalic second twin
• Race and heredity: Black race followed by breech extraction
• Parity: Increasing parity (2.7% in 4th pregnancy) • CESAREAN SECTION
• Heredity o Breech presentation of the first twin –
• Pituitary Gonadotropin similar as singleton breech fetus
• ART – Assisted Reproductive Technology o Locked twins – first fetus breech and
o Ovulation induction with FSH and second cephalic, breech of the first twin
gonadotropin/chlomiphine descends through the birth canal, the chin
o Greater the number of embryos transferred locks between the neck and chin of the
the greater the risk of multiple pregnancy second cephalic presenting co-twin
MATERNAL COMPLICATIONS DYSTOCIA DUE TO ABNORMALITIES OF THE
DURING PREGNANCY DURING LABOR DURING PUERPERIUM PASSAGEWAY
- Nausea and vomiting - Early rupture of - Subinvolution
- Anemia membranes - Infection
- Preeclampsia (25%) - Cord prolapse - Lactation failure PASSAGEWAY
- Hydramnios (10%)
- Antepartum hemorrhage
- Prolonged labor • Refers to the route the fetus must travel from the
- Increased operative
- Malpresentation
interference
uterus through the pelvis
- Preterm labor (50%)
- Mechanical distress - Bleeding o Soft Tissue
- Postpartum hemorrhage o Pelvic Bone
• The soft tissues of the passage includes:
FETAL COMPLICATIONS o Distensible lower uterine segment
• Miscarriage o Cervix
• Prematurity (80%) o Vaginal canal
• Growth Problem (25%) o Pelvic floor muscle
• Intrauterine death o Introitus
• Asphyxia and still birth • Before labor, uterine is made up of the corpus and
• Fetal Anomalies the cervix
• Important factors in the passageway
o Types of pelvis
o Structure of the pelvis (true versus false
pelvis)
o Pelvic inlet diameters
SARDENIA, JOZELLE KAYE 4
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
o Ability of the uterine segment and vaginal MEASUREMENTS
canal to distend, the cervix dilate • Two pelvic measurements are important to
determine the adequacy of the pelvic size
2 DIVISIONS OF THE PELVIS o Diagonal conjugate (AP diameter of the
1. False Pelvis inlet)
2. True Pelvis o Transverse diameter of the outlet
a. Pelvic Inlet • PELVIC INLET MEASUREMENTS
b. Pelvic Cavity o DIAGONAL CONJUGATE (12.5 – 13
c. Pelvic Outlet CM)
▪ from lowest margin of the
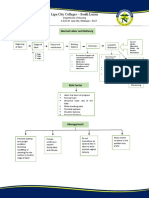
TYPES OF PELVIS symphysis pubis to sacral
• GYNECOID – the true female pelvis promontory
• PLATYPELLOID – wide but flat, kidney-shaped ▪ obtained by vaginal examination
brim ▪ Metal scale fastened to wall for
• ANTHROPOID – oval. Transverse diameter is measuring the diagonal conjugate
narrow, A-P is longer. Ape pelvis diameter as ascertained manually
• ANDROID – heart shape, male pelvis o OBSTETRIC CONJUGATE
(ESTIMATED SUBTRACTING 1.5 – 2
CM TO DIAGONAL CONJUGATION)
▪ From inner surface of symphysis
pubis, slightly below upper
border, to sacral promontory
▪ Shortest distance between sacral
promontory and symphysis pubis
▪ Most important pelvic
measurement
o TRUE CONJUGATE (10.5 – 11 CM)
▪ Conjugate vera
▪ From upper margin of symphysis
pubis to sacral promontory
COMPARISON OF PELVIC TYPES
▪ Maybe obtained by x-ray or
ultrasound
• MIDPELVIS MEASUREMENTS
o INTERSPINOUS DIAMETER /
BISPINOUS DIAMETER (10.5 cm)
▪ At the level of the ischial spine
▪ Importance: Engagement of the
fetal head
▪ The space between the inlet and
the outlet
▪ Extends from the lower margin of
the symphesis pubis through the
level of the ischial spines to the tip
the sacrum
o ANTEROPOSTERIOR
DIAMETER (11.5 cm)
▪ Through the level of ischial
spines
o TRANSVERSE OR
INTERSPINOUS (10.5 cm)
o POSTERIOR SAGITTAL (5 cm)
▪ From the midpoint of the
interspinous line to the same
point in sacrum
SARDENIA, JOZELLE KAYE 5
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
o Above ischial spines, station is negative
number
o Below ischial spines, station is positive
number
o “High” or “floating” terms use to denote
unengaged presenting part
• PELVIC OUTLET MEASUREMENTS
o AP DIAMETER (11.5 cm)
▪ Extends from the lower margin of
the symphysis pubis to the tip of
the sacrum
o TRANSVERSE DIAMETER / INTER
ISCHIAL TUBEROUS DIAMETER (10
cm)
▪ Distance between the inner edges
of the ischial tuberosities
o POSTERIOR SAGITTAL DIAMETER
(7.5 cm)
▪ Extends from the tip of the sacrum
to a right-angled intersection with
a line between the ischial
tuberosities
• OUTLET
o Inferior portion of the pelvis, or that
portion bounded in the back by coccyx, on
the sides by the ischial tuberosities and in
the front by the symphysis pubis
o The greatest diameter of the outlet is its
anteroposterior diameter
DIAMETERS OF THE FETAL SKULL
• 2 TRANSVERSE DIAMETERS
o BIPARIETAL DIAMETER
▪ 9.5 cm between 2 parietal
eminences
o BITEMPORAL DIAMETER
▪ 8.2 cm between the furthest points
of the coronal suture of the
temples
• AP OR LONGITUDINAL DIAMETERS
o SUBOCCIPITOBREGMATIC
ENGAGEMENT ▪ 9.5 cm from inferior aspect of the
• Fetal presenting part enters true pelvis (inlet) occiput to the center of the anterior
fontanelle
• May occur two weeks before labor in Primipara;
o SUBOCCIPITOFRONTAL
usually occurs at beginning of labor for Multipara
▪ 10 cm from below the occipital
protruberance to the center of the
STATION
frontal suture
• Measurement of how far the presenting part has o OCCIPITOFRONTAL
descended into the pelvis. Referent is ischial spines, ▪ 11.5 cm bridge of the nose to the
palpated through lateral vaginal walls occipital prominence
• When presenting part is:
o At ischial spines, station is “O”
SARDENIA, JOZELLE KAYE 6
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
o METROVERTICAL OR DISPROPORTION
OCCIPITOMENTAL • There is discrepancy, between the size of the fetus
▪ 13.5 cm measured from the chin to and that of the pelvis
the posterior fontanelle • Due to an average-sized baby in the woman with a
▪ The widest AP diameter small pelvis or a normal pelvis with a big baby or
o SUBMENTOVERTICAL due to a combination of these factors
▪ 11.5 cm from the point where the
chin joins the neck to the highest
point on the vertex
o SUBMENTOBREGMATIC
▪ 9.5 cm from the point where the
chin joins the neck the neck to the
center of the bregma
CONTRACTED PELVIS
ANATOMICALLY
• Defined as one in which the essential diameters of
one or more planes are shortened by at least 0.5 cm
PELVIC INLET CONTACTION
OBSTETRICALLY • Anteroposterior diameter is less than 10 cm
• Any alteration of size and shape of the pelvis • Greatest transverse diameter is less than 12 cm
• Diagonal conjugate < 11.5 cm
• Abnormal bony pelvis secondary to
o Malnutrition
o Kyphosis
o Scoliosis
o Trauma
• History of childhood tuberculosis, rickets, or
poliomyelitis
• Past obstetrical history for prolonged labor and
instrumental delivery
• In primigravida women, engagement is to occur by
the 37th week. Non-engagement or malpresentation
should warrant a suspicious pelvic contraction
OMINOUS SIGNS TO WATCH FOR INCLUDE:
CLINICAL PELVIMETRY • Dysfunctional labor
• Determination of the adequacy of the inlet reaching • Posterior parietal presentation with exaggerated
the promontory of the sacrum obliquity
• Early rupture of membranes
ASSESSMENT OF THE PELVIS
• Increasing of edema of the cervix
• Reaching the sacral promontory • Formation of caput and molding
• Feeling the lateral pelvis wall • Conversion from vertex to face presentation
• Determining the prominence of the ischial spines • Evidence of fetal or maternal distress
• Assessment of the pubic arch
MIDPELVIC INLET CONTACTION
• The sum of the interspinous diameter (10.5 cm) and
the postero sagittal diameter of the midpelvis (5 cm)
falls to 13.5 cm and below
• Inter spinous diameter is less than 10 cm
• When smaller than 8 cm then definite contraction
exists
• Ischial spines are prominent
• Sidewalls are convergent
• Sacrosciatic notch is narrow
• More common that inlet contraction with frequently
associated deep transverse arrest of the fetal head
SARDENIA, JOZELLE KAYE 7
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
• Management of midpelvic contraction is to allow
for the normal forces of labor to push the biparietal
diameter of the head beyond the area of narrowing
• Use of oxytocin is contraindicated
CONTRACTED PELVIC OUTLET SUSPECT IF:
• Interischial tuberous diameter of less than 8 cm • Broadening of the uterine fundus
• Usually associated with midpelvic contraction and • Abnormal lie or presentation
it is the combination of the two • History of repeated abortions
• Produces perineal tears • Abnormal location of the cervix in the vaginal
vault
CERVICAL ABNORMALITIES
• Ff. extensive cauterization of the cervix, it may
become so stenosed that dilatation and effacement
may not take place during labor
• In cases of unyielded cervical stenosis, cesarean
section is carried out
VAGINAL ABNORMALITIES
• Septum can be present that divides that vagina
GENERALLY CONTRACTED PELVIS o LONGITUDINAL SEPTUM
• All the different planes are shortened ▪ cervix to vulva
o INCOMPLETE SEPTUM
• Molding and internal rotation results in arrests in
▪ Upper or lower portion of vagina
occipito posterior position due to associated mid
o TRANSVERSE SEPTUM
pelvic contraction
▪ Upper vagina divided from lower
• Termination by cesarean section is usually done
part
CONTRACTED PELVIS
PELVIC MASSES
• Contraction of pelvic inlet AP < 10 cm; transverse • Gartner Duct cyst may protrude into the vagina
<12 cm and through the introitus
• Contraction of mid pelvis Interischial spinous • Uterine myomas
diameter < 10 cm • Ovarian neoplasm
• Contraction of pelvic outlet Interischial tuberous
diameter < 8cm LOW LYING PLACENTA
• Marginal or low-lying placenta may prevent fetal
SOFT TISSUE DYSTOCIA descent, or worst may give rise to abnormal
• Anatomic abnormalities of the reproductive tract bleeding that cesarean section may be required
may cause abnormal or prolonged labor
• Due to abnormalities in the uterus, cervix, and the
vagina; the presence of pelvic masses; scarring of
the birth canal and low implantation of the placenta
UTERINE ABNORMALITIES
• Abnormal fusion of the Mullerian ducts
• Failure of absorption of the septum lead to a variety
of congenital malformations of the uterus
SARDENIA, JOZELLE KAYE 8
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
DYSTOCIA DUE TO ABNORMALITIES OF THE INTENSITY OF CONTRACTIONS
POWER / EXPULSIVE FORCES • MILD
o The uterus is contracting but does not
A. UTERINE CONTRACTION (INVOLUNTARY) become more than minimally tense
• FREQUENCY • MODERATE
o Timed from the beginning of one o The uterus feels firm
contraction to the beginning of the next • STRONG
• REGULARITY o So intense, the uterus feels as hard as
o Discernable pattern; better established as wooden board at the peak of contraction
pregnancy progresses
• INTENSITY B. VOLUNTARY BEARING DOWN EFFORTS
o Strength of contraction; may be determined • After full dilatation of the cervix, the mother can use
by the “depressability” of the uterus during her abdominal muscles to help expel fetus
a contraction. • These efforts are similar to those for defection, but
o Describe as mild, moderate, or strong the mother is pushing out the fetus from the birth
• DURATION canal
o Length of contraction • Contraction of levator ani muscles
o Contraction lasting more than 90 seconds
without a subsequent period of uterine
relaxation may have severe implications
for the fetus and should be reported
LABOR AND DELIVERY
PHASES OF CONTRACTION
• INCREMENT STAGES OF LABOR
o When the intensity of the contraction • STAGE 1
increases o From onset of labor until full dilatation of
• ACME cervix
o When the contraction is at its strongest ▪ Latent phase: 0 - 4 cm
• DECREMENT ▪ Active phase: 4 – 8 cm
o When the intensity decreases ▪ Transition phase: 8 – 10 cm
• STAGE 2
o From full dilatation of cervix to birth of
baby
• STAGE 3
o From birth of baby to expulsion of placenta
• STAGE 4
o Time after birth (usually 1 – 2 hrs) of
immediate recovery
DURATION OF LABOR
• Depends on:
o Regular, progressive uterine contraction
o Progressive effacement and dilatation of
cervix
o Progressive descent of presenting part
SARDENIA, JOZELLE KAYE 9
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
• Average length of Normal Labor: • TRANSITION PERIOD
o 8 – 10 cm cervical dilatation occurs
o The mood of the woman suddenly
changes, and the nature of contractions
intensify
• If cervix is intact, this period is marked by a
sudden gush of amniotic fluid as the fetus is
pushed into the birth canal. Show becomes
prominent.
• Uncontrollable urge to push contractions (a sign
that the second stage of labor is very near)
• Duration of contraction – 60 to 70 secs
• Interval – 30 to 90 seconds
STAGE OF DILATATION
• LATENT PHASE
o Early time in labor
o Cervical dilatation is minimal because
effacement is occurring
o Cervix dilates 0 – 4 cm
STAGE OF EXPULSION
• SECOND STAGE OF LABOR (STAGE OF
EXPULSION)
o Begins with the complete dilatation and
ends with the delivery of the infant
o PRIMI: 80 minutes
o MULTI: 30 minutes
o Power / forces at work: involuntary uterine
contractions of the diaphragmatic and
abdominal muscles
• ACTIVE OR ACCELERATED
o Cervical dilatation reaches 4 – 8 cm
o Rapid increase in duration, frequency, and
intensity of contraction
o Woman fears losing of herself
MECHANISMS OF LABOR / FETAL POSITION
• Changes: (ED FIRE ERE)
o ENGAGEMENT
▪ The head is fixed in the pelvis
o DESCENT
▪ Fetus goes down in the birth canal
o FLEXION
▪ Fetal chin bends toward the chest
o INTERNAL ROTATION
▪ From AP to transverse then AP to
AP
SARDENIA, JOZELLE KAYE 10
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
o EXTENSION FUNCTIONAL DIVISION OF LABOR
▪ The head extends, the forehead, • PREPARATORY DIVISION
nose mouth and chin appears o Includes the latent and acceleration phases
o EXTERNAL ROTATION • DILATATIONAL DIVISION
(RESTITUTION) o labor during which time dilatation
▪ Anterior shoulder rotates proceeds at a rapid rate, occupies the phase
externally to AP position maximum slope of dilatation
o EXPULSION o This is unaffected by sedation or
▪ Delivery of the rest of the body conduction analgesia
• PELVIC DIVISON
o Encompasses both deceleration phase
o Second stage of labor, concurrent with the
maximum slope of descent
o Classical mechanisms of labor that the
involve the cardinal movements of the
fetus in cephalic presentation
PLACENTAL STAGE
• THIRD STAGE OF LABOR (PLACENTA
STAGE)
o Begins with the delivery of the baby and
ends with the delivery of the placenta PHASES OF THE ACTIVE PHASE
o PRIMI: 10 minutes • ACCELERATION PHASE
o MULTI: 10 minutes o Short and variable but is important in
determining the ultimate outcome of labor
POST-PARTUM STAGE o Low acceleration phase generally presages
• FOURTH STAGE OF LABOR (RECOVERY a lower maximum slope and therefore
STAGE) prolonged total labor
o First 2 hours post-partum is the most • PHASE OF MAXIMUM SLOPE
crucial stage of the mother due to unstable o Good measure of the overall efficiency of
vital signs the uterus
o Gives a clear idea of the effectiveness of
NORMAL LABOR PATTERN the force of uterine contraction in
• Friedman in 1954 begun studies to describe a producing dilatation
characteristic sigmoid pattern for labor when • DECELERATION PHASE
analyzed by graphing cervical dilatation against o Reflects fetopelvic relationship
time o Involves retraction of the cervix about the
fetal presenting part
• Friedman’s minimum criteria for subsequent entry
into the active phase of labor are cervical dilatation
rates of 1.2 cm per hour for multiparas. These rates
of dilatation do not start at a specific dilatation
SARDENIA, JOZELLE KAYE 11
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
• Friedman’s data shows that normal labor is • Etiologic factors include excessive sedation or
characterized by rates of maximum descent conduction analgesia, unfavorable cervix (e.g.,
exceeding 1 cm per hour in nulliparas and 2 cm per thick, rigid, uneffaced, undilated), false labor, and
hour in multiparas uterine dysfunction
ABNORMAL LABOR PATTERNS, DIAGNOSTIC
CRITERIA AND METHOS OF TREATMENT
• Prolonged latent phase
• Protracted active phase dilatation
• Protracted descent
• Prolonged deceleration phase
• Secondary arrest of dilatation
• Arrest of descent
• Failure of descent
PROTRACTION DISORDERS
• PROTRACTED ACTIVE PHASE
DILATATION means that the maximum slope of
dilatation
o NULLIPAROUS: less than 1.2 cm per
hour
o MULTIPAROUS: 1.5 cm per hour
• PROTRACTED DESCENT means descent of the
fetal head
o NULLIPAROUS: less than 1 cm per hour
o MULTIPAROUS: 2 cm per hour
• NULLIPARA
o 2 hrs extended to 3 hrs when conduction
analgesia is used
• MULTIPARA
o 1 hour is the limit extended to 2 hrs with
conduction analgesia.
o Common cause of prolonged 2nd stage is
persistent occiput posterior position
• A prolonged latent phase is one longer than 20 hrs
in nulliparous or 14 hrs in multiparous women
SARDENIA, JOZELLE KAYE 12
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
POWERS: FORCE OF LABOR • COMPLICATION
• Ineffective uterine force o Fetal Anoxia
o Hypotonic uterine dysfunction
o Hypertonic uterine dysfunction MANAGEMENT
o Uncoordinated contractions • Provide comfort measures
• Bedrest or position changes
• Hydration
• Mild sedation
• Tocolytics
• Caesarean delivery
PREVENTION OF DYSFUNCTIONAL LABOR
HYPOTONIC CONTRACTION • No CPD
• Maintain a serum glucose level
• NUMBER OF CONTRACTIONS
• Prevent fluid and electrolyte loss
o Not more 2 or 3 occurring in 10-minute
period • Reduce psychological stress
• RESTING TONE • Provide measures to reduce pain
o Less than 10 mmHg • Maintain a side lying position
• STREGTH OF CONTRACTIONS • Keeping the bladder empty
o Does not rise above 25 mmHg
• PHASE OF LABOR
o Active
• SYMPTOM
o Painless
ETIOLOGY
• Overstretching of the uterus – large baby, multiple
babies, polyhydramnios, multiparity
• Bowel or bladder distention, preventing descent
• Excessive use of analgesia
THERAPEUTIC INTERVENTIONS
• Oxytocin
• Ambulation
• Nipple stimulation
• Enema
• Amniotomy
HYPERTONIC CONTRACTIONS
• RESTING TONE
o More than 15 mmHg
• CONTRACTIONS
o Frequent prolonged contractions that are
not productive
• PHASE OF LABOR
o Latent
• SYMPTOM
o Painful
• CAUSE
o Occurs because the muscle fibers of the
myometrium do not repolarize or relax
after contraction, thereby “wiping it clean”
to accept a new pacemaker stimulus
SARDENIA, JOZELLE KAYE 13
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
LABOR COMPLICATIONS fetal distress in 30 minutes → rate 16 – 20
gtts/min
UTERINE INERTIA • AMNIOTOMY
• Sluggishness of contraction o Done with Cervical Dilation = 4 cm; Check
FHR and quality of amniotic fluid
CAUSE
• Inappropriate use of analgesics NURSING CONSIDERATION
• Pelvic bone contraction • Monitor uterine contraction → potential for rupture
• Poor fetal position • Monitor flow rate regularly
• Overdistention – due to multiparity, multiple • Turn off IV with any abnormality in FHR or
pregnancy, polyhydramnios, or excessively large contractions
baby • Watch out for complications
• Prostaglandin administration
MANAGEMENT o Route: Oral or IV (never IM causes
• Stimulation of labor by oxytocin administration or irritation)
amniotomy o Effect is slower than oxytocin
PRECIPITATE DELIVERY INSTRUMENTAL DELIVERIES
• Labor and delivery that is completed in < 3 hrs due • Incidence: 4.5% of vaginal deliveries
to multiparity or following oxytocin administration • Forceps delivery: 0.8%
or amniotomy • Vacuum deliveries: 3.7%
• Success Rate: 99%
EFFECTS o Reflects appropriate choice of candidates
• Extensive lacerations
• Abruptio placenta FORCEPS DELIVERY
• Hemorrhage due to sudden release of pressure → • Use of metal instruments to extract the fetus from
shock the birth canal
• When at +3 / +4 and sagittal suture line is in an AP
INDUCED LABOR position in relation to the outlet (e.g., Simpson,
• Stages of labor and birth occurs due to chemical or Elliot, Piper for breech presentation)
mechanical
• Performed to save the mother or fetus from PURPOSES
complications which may cause death • Shorten second stage of labor because of fetal
distress; maternal exhaustion; maternal disease –
INDICATIONS cardiac, pulmonary complication
• Maternal – toxemia • Ineffective pushing due to anesthesia
• Placental accidents • Prevent excessive pounding of fetal head against
• Premature rupture of membrane perineum (low forceps for premature)
• Fetal: DM – terminated at about 37 weeks AOG if • Poor uterine contraction or rigid perineum
indicated
PREREQUISITES
• Excessive size
• Post maturity • Pelvis adequate, no disproportion
• Fetal head is deeply engaged
PREREQUISITES TO INDUCE LABOR • Cervix is completely dilated and effaced
• No Cephalon – Pelvic Dislocation • Membranes have ruptured
• Fetus is already viable > 32 weeks AOG • Vertical presentation has been established
• Single fetus in longitudinal lie and is engaged • Rectum and bladder are empty
• Ripe cervix – fully or partially effaced; Cervical • Anesthesia is given for sufficient perineal relaxation
Dilatation at least 1 – 2 cm and to prevent pain
PROCEDURE FOR INDUCED LABOR
• OXYTOCIN ADMINISTRATION
o 10 IU of Pitocin in 1000 ml of D5W at a
slow rate of 8 gtts/min given initially → no
SARDENIA, JOZELLE KAYE 14
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
FORCEPS DELIVERY
• TYPES: Low or Mid Forceps Delivery
COMPLICATIONS
• Forceps marks – noticeable only for 24 – 48 hours
• Bladder or rectal injury
• Facial paralysis
• Ptosis
• Seizures
• Epilepsy TYPES
• Cerebral Palsy • LOW SEGMENT
o The method of choice
o Incision is made in the lower uterine
segment
o Thinnest and most passive part during
active labor
o ADVANTAGES:
▪ Minimal blood loss
RISKS: INSTRUMENTAL DELIVERY ▪ Incision is easier to repair
▪ Lower incidence of post-partum
MATERNAL RISKS infection
▪ No possibility of uterine rupture
• Perineal Injury (extension of episiotomy)
• Vaginal and Cervical lacerations
• Postpartum hemorrhage
FETAL RISKS
• Intracranial hemorrhage
• Cephalhematoma
• Facial / Brachial palsy
• Injury to the soft tissue of face and forehead
• Skull fracture • LOWER VERTICAL INCISION
o Recommended in:
CESAREAN DELIVERY ▪ Bladder or lower uterine segment
• CESAREAN SECTION ▪ Adhesions from previous
o Birth through a surgical incision on the operations
abdomen ▪ Anterior Placenta Previa
▪ Transverse lie
INDICATIONS
• Cephalon-pelvic disproportion (CPD)
• Severe Toxemia
• Placental Accidents
• Fetal Distress
• Previous classic CS – done prior to onset of labor
pains; scheduled birth
SARDENIA, JOZELLE KAYE 15
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
PREOPERATIVE CARE • Age: Adolescent or 40 years old above
• Check vital signs, uterine contractions, and FHR primigravids
• Physical examination; routine laboratory tests;
blood typing and cross matching MANAGEMENT
• Abdomen is shaved from level of the xiphoid • If no bleeding; no CD, good FHT, medication is
process below the nipple line, extending out to the given
flanks on both sides up to the upper thirds of the o Ethyl alcohol IV – blocks release of
thighs Oxytocin
• Retention catheter is inserted to constant drainage o Vasodilan IV – vasodilator
to keep the bladder away from the operative site o Ritodrine – muscle relaxant per orem
• Preoperative medication is usually only atropine o Bricanyl – bronchodilator
sulfate • Pain meds are kept to a minimum to prevent
• No narcotics → causes respiratory depression in respiratory depression
the NB • Steroids (glucocorticoids) for maturation of fetal
lung → surfactant production
POSTOPERATIVE CARE • Anesthesia preferred – caudal, spinal or infiltration
• Deep breathing, coughing exercises, turning from – do not affect the infant
side to side
• Ambulate after 12 hours
• Monitor vital signs
• Watch for signs of hemorrhage – inspect lochia;
feel fundus
• Breastfeeding should be started 24 hrs after
delivery
• Most common complication: Pelvic thrombosis
AMNIOTIC FLUID EMBOLISM SHOULDER DYSTOCIA
• Forced into an open maternal uterine fluid flood • Inability to deliver a baby’s shoulders after its
sinus through some defect in the membranes or head has emerged
after partial premature separation of the placenta
• The baby’s shoulder has become impacted
• Solid particles in the amniotic fluid enter maternal
circulation and reach the lungs as emboli behind the mother’s pubic symphysis
• One that requires additional obstetrical
maneuvers ff. the failure of gentle downward
traction on the fetal head to effect delivery of
the shoulders
SIGNS AND SYMPTOMS
• Dramatic RISKS
• Sudden inability to breathe, sits up, grasps chest • Macrosomia
and sharp chest pain
• Turns pale then → bluish gray color • Gestational diabetes
• Death may occur in a few minutes • Previous shoulder dystocia
• Instrumental vaginal delivery
MANAGEMENT • Heightened awareness that a shoulder
• Emergency measures to maintain life: IV, oxygen, dystocia might occur in a particular case
CPR • Diagnosis
• Provide intensive care in the ICU • Operational control / situational awareness
• Keep family informed
• Maneuvers
• Provide emotional support
o McRoberts maneuver
PREMATURE LABOR AND DELIVERY o Suprapubic pressure
• Uterine contractions occur before 37th week of o Woods maneuver
gestation o Rubin’s maneuver
• Pre-eclampsia
• Placenta Previa
SARDENIA, JOZELLE KAYE 16
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
CAUSES
• Malpresentation
• Prematurity
• Polyhydramnios
• Multiple pregnancy
MANAGEMENT • PROM
• CLEIDOTOMY • CPD
o Fracturing the fetal clavicle • Obstetric interventions
• SYMPHYSIOTOMY
o Cutting the pubic symphysis MANAGEMENT
• ZAVENELI • Cord pulsations
o Returning the fetal head to the pelvis for • CTG shows variable decelerations
delivery of the baby via caesarean section
• Fundal pressure causes bradycardia
o
• Meconium stained liquor
• Lift presenting part off the cord
• Instruct patient NOT to push
• Position
o Knee chest
o Trendelenburg
o Exaggerated position
• Vulvar pad
• Replacement of cord
• Tocolysis
• Funic reduction
o Manual replacement of cord into uterus
o Cord gently pushed above presenting part
• Expedite delivery
• Prepare for newborn resuscitation
PROM
• PREMATURE RUPTURE OF MEMBRANES
(PROM)
o Spontaneous rupture of fetal membranes
before onset of labor
• PRETERM PREMATURE RUPTURE OF
MEMBRANE (PPROM)
o Rupture of membranes before onset of
labor in pregnancies between 28 – 37
weeks
CORD PROLAPSE
• TERM PREMATURE RUPTURE OF
• In a prolapse, the umbilical cord drops (prolapses)
MEMBRANE (TPRM)
through the open cervix into the vagina ahead of the
o Rupture of membranes before onset of
baby
labor beyond 37 weeks
• The cord can then become trapped against the
baby’s body during delivery
SARDENIA, JOZELLE KAYE 17
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
CAUSES
• Unknown but hypothesized
o Vaginal and cervical infections
o Incomplete cervix
o Nutritional deficiencies
o Polyhydramnios
o Fetal malpresentation
o Multiple gestation or a large baby
o Occupational fatigue
o Vaginal exams
RISKS
• Preterm labor
• Umbilical cord prolapse
• Umbilical cord compression
• Chorioamnionitis
• Pulmonary hypoplasia
• Placental abruption
• Neonatal infection UTERINE RUPRTURE
• Stillbirth / Neonatal death • Occurs when the uterus undergoes more straining
than it is capable of sustaining
SIGNS AND SYMPTOMS
• Vaginal discharge CAUSE
o Gush of fluid • Scar from previous CS
o Leaking of fluid • Unwise use of oxytocin
• Cramping • Overdistension
• Contractions • Faulty presentation
• Back pain • Prolonged labor
PRETERM PREMATURE RUPTURE OF
MEMBRANE (PPROM)
• Sudden gush of clear vaginal fluid with
oligohydramnios
• Speculum exam
• Pooling
• Nitrazine paper test
• Ferning
CHORIOAMNIONITIS
• Clinical diagnosis with all the ff: SIGNS AND SYMPTOMS
o Maternal fever • Sudden severe pain
o Uterine tenderness • Hemorrhage and clinical signs of stock
o Confirmed PROM • Change in abdominal contour
o Absence of URI or UTI
MANAGEMENT
MANAGEMENT OF PROM
• Hysterectomy
PREVIABLE < 24 weeks PULMONARY HYPOPLASIA
PRETERM
PREMATURITY
24 – 35 weeks
TERM
INFECTION
36+ weeks
BEFORE VIABILITY
INDUCE LABOR
< 24 weeks
HOME BED REST
(PULMONARY HYPOPLASIA)
HOSPITALIZE
PRETERM VIABLE
MATERNAL STEROIDS
24 – 35 weeks
CERVICAL CULTURES
(PREMATURITY)
7 DAYS AMPIC+ERYTHRO
AT TERM
36+ WEEKS PROMPT DELIVERY
(INFECTION)
SARDENIA, JOZELLE KAYE 18
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
THIRD STAGE OF LABOR o Placental chorionic villi grow through the
• Remains most unpredictable and dangerous stage of uterine myometrium and often adhere to
labor from the mother’s point of view abdominal structures (bladder or intestine)
• Retained placenta / undelivered placenta – 1 – 2%
NURSING MANAGEMENT
RETAINED PLACENTA • Identify placenta accrete in the client
• If the placenta is undelivered at 30 minutes it should • Assist with rapid treatment and intervention
be considered to be “retained” • Provide physical and emotional support
• Provide client and family education
CAUSES OF RETAINED PLACENTA
ABNORMALITIES OF THE PLACENTA
• Placenta partly or wholly attached
• Placenta develops from the chorion frondosum, the
• Placenta separated but undelivered
part in contact with the most vascular decidua
• Any developmental abnormality may have a clinical
BRANDT-ANDREWS METHOD
significance
• Cord is pulled gently the other hand presses the
• More or less than whole chorion develops
uterus upwards to prevent inversion
functional villi and the placenta occupies the greater
• Slight see-sawing motion is imparted by both hands
part of the uterine
• PLACENTA BIPARTITA
PLACENTA ACCRETA
o Partly divided into two lobes, with
• Rare cause of retained placenta
connecting vessel
• Abnormal adherence of placenta to the uterine
• PLACENTA MEMBRANACEA
muscle due to a defect of decidual formation
o Unduly large and thin
• Can be partial or complete where bleeding is absent o Not only develops from chorionic
• Attempts at manual removal open the blood sinuses frondosum but chorionic levae so whole of
causing severe bleeding ovum is practically covered
• PLACENTA SUCCENTURIATA
o Vascular connection between main and
accessory lobes
o Accessory lobe is retained and manually
removed
• PLACENTA CIRCUMVALLATA
o Membranes appear to be attached
internally to the placental edge and on the
periphery there is a ring of thick whitish
tissue which is in fact a fold of infarcted
chorion
• PLACENTA VELAMENTOSA
o Distance away from the attachment of the
• PLACENTA ACCRETA cord and the vessels
o Placental chorionic villi adheres to the o Cord at the edge of the placenta
superficial layer of the uterine o Divide in the membranes
myometrium o If they cross the lower pole of the chorion
• PLACENTA INCRETA – yasa previa
o Placental chorionic villi invade deeply into • BATTLEDORE PLACENTA
the uterine myometrium o Cord has a marginal instead of a central
• PLACENTA PERCRETA insertion
o No clinical significance
SARDENIA, JOZELLE KAYE 19
MODULE 4: NURSING CARE OF THE CLIENT DURING LABOR AND DELIVERY
o Six or seven loops are drawn tightly round
the neck
o Fetus descends the cord tightens
o Blood supply is interrupted
o Baby is stillborn
o True knots are seen quite often but
Wharton’s jelly usually prevents actual
obstruction by kinking
o False knots are protuberances of
connective tissues matrix, sometimes
containing varices
• SINGLE UMBILICAL ARTERY
o Sometimes associated with congenital
abnormalities in the fetus
CLINICAL SIGNIFICANCE
• Post-partum hemorrhage
• Subinvolution
• Retained placenta
• Sepsis
• Abortion
• Premature labor
• Fetal malformation
• Fetal death
PLACENTA BIPARTITA PLACENTA MEMBRANACEA
PLACENTA SUCCENTURIATA PLACENTA CIRCUMVALLATA
PLACENTA VELAMENTOSA SINGLE UMBILICAL ARTERY
BATTLEDORE PLACENTA
SARDENIA, JOZELLE KAYE 20
You might also like
- Abnormal Labor: Ina S. Irabon, MD, Fpogs, FPSRM, FpsgeDocument51 pagesAbnormal Labor: Ina S. Irabon, MD, Fpogs, FPSRM, FpsgeMa. Bernadette PinedaNo ratings yet
- Stages of Labor FlowchartDocument1 pageStages of Labor FlowchartXyrelle GambalozaNo ratings yet
- PARTOGRAPHDocument2 pagesPARTOGRAPHZairah Mae BangguiyaoNo ratings yet
- RA 9710 MCW English Brochure (Inner Page) FINALDocument1 pageRA 9710 MCW English Brochure (Inner Page) FINALRuby CasasNo ratings yet
- EmbryologyDocument15 pagesEmbryologyKoushal Sharma, JammuNo ratings yet
- Non Alcoholic Fatty Liver DiseaseDocument1 pageNon Alcoholic Fatty Liver DiseaseKIM LORIE YAP PASCUALNo ratings yet
- Male and Female Reproductive SystemsDocument24 pagesMale and Female Reproductive SystemsBry EsguerraNo ratings yet
- ObstetricDocument4 pagesObstetricIsabel Bibat DavidNo ratings yet
- FORM Pembuatan ICRA - NewDocument3 pagesFORM Pembuatan ICRA - NewJosepb SimarmataNo ratings yet
- Pathophysiology 2Document1 pagePathophysiology 2Jannele BernadasNo ratings yet
- ICRADocument9 pagesICRAMaiova N. Annisa100% (1)
- Recruitment of Accounts Officers and Personnel Officers in State Power Companies of RajasthanDocument21 pagesRecruitment of Accounts Officers and Personnel Officers in State Power Companies of RajasthanAbhi JainNo ratings yet
- How To Conduct A Safe Delivery and Pregnancy For Your Pelvic FloorDocument35 pagesHow To Conduct A Safe Delivery and Pregnancy For Your Pelvic FloorMunifah YusriyahNo ratings yet
- Routes of Administration PDFDocument1 pageRoutes of Administration PDFnazbeen.ahmadiNo ratings yet
- 1598ititchiwaa Wak WakDocument46 pages1598ititchiwaa Wak WakRon AgamataNo ratings yet
- Silliman Notes Political Law Suggested Answers 1987 2006Document46 pagesSilliman Notes Political Law Suggested Answers 1987 2006Dux Alair L0% (1)
- Reproductive System MMDocument1 pageReproductive System MMKhaled Abdel-saterNo ratings yet
- Census FormDocument21 pagesCensus Formann29No ratings yet
- Table of Reviewed StudiesDocument9 pagesTable of Reviewed StudiesyusficaNo ratings yet
- Reproductive SystemDocument104 pagesReproductive SystemJohn Rick PerezNo ratings yet
- Parasite - Table - 2015 - 2 - .PDF Filename UTF-8''Parasite Table 2015Document2 pagesParasite - Table - 2015 - 2 - .PDF Filename UTF-8''Parasite Table 2015Shayma K MaaliNo ratings yet
- PERIODICAL INCREMENT CERTIFICATE - OrgDocument1 pagePERIODICAL INCREMENT CERTIFICATE - OrgKumar100% (1)
- Risk Analysis: Working at HeightDocument1 pageRisk Analysis: Working at Heightsappy2shailNo ratings yet
- 2015 FIGO CONSENSUS GUIDELINES ON INTRAPARTUM FETAL MONITORING - PPT Video Online DownloadDocument1 page2015 FIGO CONSENSUS GUIDELINES ON INTRAPARTUM FETAL MONITORING - PPT Video Online DownloadDesiree Jolly Dela CruzNo ratings yet
- Biology (Purple)Document10 pagesBiology (Purple)F4AC1 (31) WONG CHI KEI, ALICENo ratings yet
- ReproDocument1 pageReproKarylle TaborNo ratings yet
- Week 9 Temporary RestorationsDocument11 pagesWeek 9 Temporary RestorationsAhmed TalalNo ratings yet
- Format For Tracking & Tagging of Pregnancies For The Month of August - 2019Document12 pagesFormat For Tracking & Tagging of Pregnancies For The Month of August - 2019Vallepu MahendrakumarNo ratings yet
- Jan 2023 JJIMSDocument6 pagesJan 2023 JJIMSRajan PaulNo ratings yet
- First FloorDocument1 pageFirst FloorKirankumar Rohit264No ratings yet
- Ind Safety Gen Duties Persons Employed EDocument2 pagesInd Safety Gen Duties Persons Employed EKassimNo ratings yet
- RCM-Corp-Service Tax-V-10.03-26112012Document5 pagesRCM-Corp-Service Tax-V-10.03-26112012Suresh KumarNo ratings yet
- Hsslive Xii Zoology Vijayabheri 2024Document4 pagesHsslive Xii Zoology Vijayabheri 2024ajithaprabhath123No ratings yet
- Potential Failure Mode and Effect Analysis: (Process Fmea)Document9 pagesPotential Failure Mode and Effect Analysis: (Process Fmea)SACHIN KUMARNo ratings yet
- Next LevelDocument1 pageNext LevelDavid GoodwinNo ratings yet
- P Section 5 Obstetric EmergenciesDocument6 pagesP Section 5 Obstetric EmergenciesgadisegallNo ratings yet
- Expert Advice For Today's Ob/Gyn: ObstetricsDocument48 pagesExpert Advice For Today's Ob/Gyn: ObstetricsMariana HernandezNo ratings yet
- Infection Control Risk AssesmentDocument5 pagesInfection Control Risk Assesmentnurul kartikasariNo ratings yet
- Work Posture Mindmap - Aisa Indra Wahyuni 1104228026Document1 pageWork Posture Mindmap - Aisa Indra Wahyuni 1104228026aisa indrawahyuniNo ratings yet
- MindmapDocument1 pageMindmapChoco MousseNo ratings yet
- Design and Process Fmea WorksheetDocument4 pagesDesign and Process Fmea WorksheetEnrico Luis Caube BalisalisaNo ratings yet
- Appendix M - Labor AlgorithmDocument1 pageAppendix M - Labor AlgorithmMeity ElvinaNo ratings yet
- Placental AbnormalitiesDocument3 pagesPlacental AbnormalitiesThakoon TtsNo ratings yet
- Main Program Grid: Saturday Sunday Tuesday Wednesday MondayDocument1 pageMain Program Grid: Saturday Sunday Tuesday Wednesday MondayFranklin Salirrosas CernaNo ratings yet
- ROLLON - JOHN CARLO - IWAR - August 3-7Document2 pagesROLLON - JOHN CARLO - IWAR - August 3-7john carlo rollonNo ratings yet
- Trend Report Patient:: Device Settings As ofDocument6 pagesTrend Report Patient:: Device Settings As ofChandru NatarajanNo ratings yet
- Parkland Trauma Soft TissueDocument14 pagesParkland Trauma Soft TissueJulieNo ratings yet
- Infection Control Risk Assesment: Failure of Prevention ActivitiesDocument6 pagesInfection Control Risk Assesment: Failure of Prevention Activitiesgoris100% (1)
- PhysicalActivityBrochure Finalv2 FIXEDDocument3 pagesPhysicalActivityBrochure Finalv2 FIXEDagNo ratings yet
- HR - Checklist-2017Document2 pagesHR - Checklist-2017khallushaik424No ratings yet
- Session03 - Mechanical VibrationDocument7 pagesSession03 - Mechanical Vibrationعبدالرحمن منصورNo ratings yet
- PETROMASTOIDDocument7 pagesPETROMASTOIDAhlen Chris TuazonNo ratings yet
- Resume File: Health Care Cert. Full-Time Part-Time Remote Worker Future HireDocument1 pageResume File: Health Care Cert. Full-Time Part-Time Remote Worker Future HireAbdullah FasehNo ratings yet
- Endocrine Physiology) 22. Female Reproductive Cycle - Menstrual Cycle - KeyDocument1 pageEndocrine Physiology) 22. Female Reproductive Cycle - Menstrual Cycle - Keyhasanatiya41No ratings yet
- Formulir ICRADocument2 pagesFormulir ICRAretnoNo ratings yet
- Plan А Survive: ImmortalityDocument1 pagePlan А Survive: ImmortalityMNo ratings yet
- Or Rudimentary Minute Spine: Schistosoma Japonicum Oncomelania QuadrasiDocument1 pageOr Rudimentary Minute Spine: Schistosoma Japonicum Oncomelania QuadrasiMaikka IlaganNo ratings yet
- G.K.S.N.Abenayaka CV PDFDocument1 pageG.K.S.N.Abenayaka CV PDFLasantha JayawicramaNo ratings yet
- Ob2rle Sas 12Document15 pagesOb2rle Sas 12Aira Mae R. AndradaNo ratings yet
- Destructive OperationDocument12 pagesDestructive OperationBezawit TesfahunNo ratings yet
- 19 - Vaginal DeliveryDocument16 pages19 - Vaginal DeliveryGen XNo ratings yet
- ObgynDocument67 pagesObgyndaniel tesfayeNo ratings yet
- Obstetrics MCQ Questions & Answers - DapzoiDocument21 pagesObstetrics MCQ Questions & Answers - DapzoiFarah FarahNo ratings yet
- Ebook Gabbes Obstetrics Essentials Normal Problem Pregnancies PDF Full Chapter PDFDocument67 pagesEbook Gabbes Obstetrics Essentials Normal Problem Pregnancies PDF Full Chapter PDFandre.davis379100% (27)
- Ob Finals Williams SamplexDocument86 pagesOb Finals Williams SamplexJustine MembridoNo ratings yet
- Post Partum Haemorrhage-1Document29 pagesPost Partum Haemorrhage-1medical chroniclesNo ratings yet
- (CC) Malpresentation and DeliveryDocument6 pages(CC) Malpresentation and DeliveryDaryl Gay NanoNo ratings yet
- Labor - Diagnosis and Management of An Abnormal First Stage - UpToDateDocument13 pagesLabor - Diagnosis and Management of An Abnormal First Stage - UpToDatesandrogvaladzeNo ratings yet
- Pregnancy Induced Hypertension (PIH)Document15 pagesPregnancy Induced Hypertension (PIH)Aiman ArifinNo ratings yet
- B.ING Kel 5aDocument17 pagesB.ING Kel 5arina puspitaNo ratings yet
- Cmca Lec MidtermDocument43 pagesCmca Lec MidtermKate Onniel RimandoNo ratings yet
- Johana M. AladinDocument14 pagesJohana M. AladinquoraismadelisNo ratings yet
- Multiple pregNANCYDocument83 pagesMultiple pregNANCYDoc RaymondNo ratings yet
- Wiklund2012 (Indication)Document8 pagesWiklund2012 (Indication)Noah Borketey-laNo ratings yet
- Vacuum Assisted DeliveryDocument2 pagesVacuum Assisted Deliveryalyssa marie salcedoNo ratings yet
- Mayzen Tita Loka - RMIK B1 - Praktikum 13 Lat 12 - KSGKDocument2 pagesMayzen Tita Loka - RMIK B1 - Praktikum 13 Lat 12 - KSGKTita LokaNo ratings yet
- The Cesarean Section Rate in Cases With Premature Rupture of Membrane (Prom) at 36Th Week of Pregnancy or LaterDocument5 pagesThe Cesarean Section Rate in Cases With Premature Rupture of Membrane (Prom) at 36Th Week of Pregnancy or LaterBob IrsanNo ratings yet
- Subject - Obstetrics and Gynecology Batch - BBA (HA) IV Sem. Submit To - Dr. Jyoti Joshi Ma'am Submit by - Shivam Rajput & Umesh ChoyalDocument19 pagesSubject - Obstetrics and Gynecology Batch - BBA (HA) IV Sem. Submit To - Dr. Jyoti Joshi Ma'am Submit by - Shivam Rajput & Umesh ChoyaldevNo ratings yet
- Fetal Malpresentation and Malposition - LecturioDocument17 pagesFetal Malpresentation and Malposition - LecturiomeddcrossNo ratings yet
- Midterm PathoDocument76 pagesMidterm PathoApril Iren Claire BalabalaNo ratings yet
- 2-Post TermDocument13 pages2-Post TermAbc DefNo ratings yet
- OBII - 16 Postterm Pregnancy - PDF Version 1Document6 pagesOBII - 16 Postterm Pregnancy - PDF Version 1Felina CabadingNo ratings yet
- NCM 109 MCN Finals Topic 1 Problems With The PassengerDocument3 pagesNCM 109 MCN Finals Topic 1 Problems With The PassengerQUEZON, BRITNEY KIM E.No ratings yet
- Placental AbruptionDocument34 pagesPlacental Abruptionrosekatekate929No ratings yet
- Operative DeliveryDocument19 pagesOperative DeliveryMtwe ZakayoNo ratings yet
- USMLE Step 2 CK Lecture Notes 2018 MPPS Book Set (PDFDrive) - 657-662Document6 pagesUSMLE Step 2 CK Lecture Notes 2018 MPPS Book Set (PDFDrive) - 657-662antonela alarcon loayzaNo ratings yet
- Cs ObgDocument44 pagesCs ObghulwanvashaliNo ratings yet
- A Prospective Study On The Maternal Outcome in Cases of Previous One Cesarean SectionDocument6 pagesA Prospective Study On The Maternal Outcome in Cases of Previous One Cesarean SectionIJAR JOURNALNo ratings yet