Professional Documents
Culture Documents
15 - 93-98 Ujmr 034
Uploaded by
KHADIJA TELAOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
15 - 93-98 Ujmr 034
Uploaded by
KHADIJA TELACopyright:
Available Formats
UJMR, Vol.
7 Number 1, June, 2022, pp 93-98 E-ISSN: 2814 – 1822; P-ISSN: 2616 – 0668
https://doi.org/10.47430/ujmr.2271.015
Received: 5th June, 2022 Accepted: 8th July, 2022
Evaluation of the Haematological Profile of Children Under Five (5) Years
Infected with Malaria Attending Murtala Muhammad Specialist Hospital, Kano-
Nigeria
*Adama Ibrahim Jibril1, Khadija Umar Tela1, Safiyyu Mujitapha Umar1, Iman Maikano
Khalid2 and Muhammad Adamu Abbas2
1
Department of Human Physiology, Faculty of Basic Medical Sciences, College of Health Sciences,
Bayero University Kano
2
Department of Medical Microbiology and Parasitology, Faculty of Clinical Sciences, College of
Health Sciences, Bayero University Kano
*Corresponding Author ✉: maabbas.mph@buk.edu.ng
Abstract
Malaria is a serious public health concern worldwide, particularly in hyper endemic areas of
tropical and subtropical regions, including Nigeria. This study investigated haematological
profile of children under five (5) years infected with malaria attending Murtala Muhammad
Specialist Hospital, Kano-Nigeria. Venous blood was aseptically collected from the ante-
cubital vein. Thick and thin blood films were prepared and viewed under a light microscope
to identify and quantify the malaria parasites. The study involved 160 children randomly
selected: comprising of 80 malaria positive and 80 negative children. Full blood count was
estimated using SYSMEX auto-hematology analyzer (Lincolnshire, Illinois U.S.A.). The results
showed that red blood cells were statistically lower in malaria infected (3.64±1.09×10 6/µL)
compared to the controls (4.16±0.86×10 6/µL). Haemoglobin concentration (HGB) of malaria
infected children was also lower (8.78±3.14g/dl) than that of the control group
(10.56±2.33g/dl). Similarly, hematocrit percentage of the infected children was significantly
lower (25.58±6.28%) compared to the controls of (27.03±7.35%). The platelet count (PLT) of
the malaria children were also lower in the case group (172.27±120.65×10 3/µL) compared to
the controls with (240.73±143.23×10 3/µL), (P>0.05). While the total White Blood Cell counts
(WBC) and its differentials did not show any statistically significant difference between the
malaria infected and the controls (p>0.05). This study clearly demonstrated that malaria
significantly affects the haematological profile of children under five years of age leading
to anemia and thrombocytopenia, with no effects on the white blood cells and differentials.
Keywords: Malaria, Children, Morbidity, Haematological profile.
INTRODUCTION attention in Nigeria, where reports revealed
Malaria is an infectious disease caused by one that it accounted for about 27% and 23% of all
or more of the following Plasmodium species; malaria cases and deaths worldwide,
Plasmodium falciparum (P. falciparum), P. respectively (WHO, 2020). Despite
vivax, P. ovale, P. malariae and P. knowlesi, interventional programs such as the National
transmitted through the bite of an infected Malaria Elimination Programme (NMEP) which
female anopheles mosquito (WHO, 2015). It is involve modalities such as insecticide-treated
widely distributed around the globe, being nets usage, intermittent preventive treatment
mostly endemic in Sub-Saharan Africa, Asia and in pregnancy, effective case management, and
the Americas. It is a major public health burden indoor residual spraying, malaria continues to
in Africa (Bawah et al., 2018). The Africa be a major health problem in Nigeria
region of the WHO accounted for 95% of global (Oluwaseun et al., 2021).
malaria cases and 96% of malaria deaths in Malaria in children can result in many
2020, where children under five years of age complications (Conroy et al., 2019, Waris et
accounted for 80% of all malaria mortality in al., 2021). Among the many complications of
the region (WHO, 2020). Malaria is especially a malaria in children is haematologic
major public health problem that requires most complications (Jiero and Pasaribu 2021).
UMYU Journal of Microbiology Research 93 www.ujmr.umyu.edu.ng
UJMR, Vol. 7 Number 1, June, 2022, pp 93-98 E-ISSN: 2814 – 1822; P-ISSN: 2616 – 0668
Hematological alterations that are thought to Blood sample collection: Blood samples were
characterize malaria are related to the collected using 5 ml syringes from each of the
significant biochemical changes believed to participants, via ante-cubital vein into ethylene
occur during the asexual stage of the life cycle diamine tetra acetic-acid (EDTA) test tubes for
of the malaria parasite (Muwonge et al., 2013). laboratory analyses. .
Malaria positive patients present with
significantly lower platelet, leukocyte, Malaria microscopy analysis:
lymphocyte, eosinophil, red blood cell, and Slides Preparation and Microscopic View:
hemoglobin (Hb) counts, (Arévalo-Herrera et Slides for microscopy were prepared after
al., 2017, Jiero and Pasaribu 2021). The specimen collection, thick and thin blood smear
number of monocytes and neutrophils tend to were made with the help of a spreader, air-
be higher than in non-malaria-infected patients dried then stained with Giemsa stain. The
(Bakhubaira et al., 2013). The pathological presence or absence of plasmodia parasites and
manifestation of malaria infection in children the number of asexual parasites per 200 WBCs
solely depends on many factors including; were determined using the WHO standard
parasite infectiveness, host susceptibility as guidelines modified (Bawah et al., 2018). After
well as geographical factors. Example; during microscopy and using simple random sampling,
the rainy seasons children are infected with the 80 malaria positive children were selected as
malaria parasite, which destroys erythrocytes experiment group and 80 age-matched non-
causing significant changes in hematological malaria infected children as control group.
parameters (Wickramasinghe et al., 2000,
Ntenda et al., 2019). Hematological alterations Hematological Profiling
may be inducted by several other factors Full blood count: Total white blood cell count
including time after infection, intensity and (TWBC), differential WBC count, Hemoglobin
pattern of transmission of the parasite in the level (Hb), red blood cell count (RBC),
area as well as the strength of host immunity hematocrit (HCT), mean corpuscular volume
(Bawah et al., 2018). (MCV), mean corpuscular hemoglobin (MCH),
Due to its importance, many studies on malaria mean corpuscular hemoglobin concentration
abound in Nigeria, particularly regarding its (MCHC) and platelet count (PLT) were
clinical effects, morbidity and mortality and estimated using SYSMEX auto-hematology
risk factors (Morakinyo et al., 2018). This study analyzer (Lincolnshire, Illinois U.S.A.).
seeks to complement the existing pool of data
by looking at the possible hematological impact Statistical Analysis
of malaria disease among children under 5 Data were obtained and analyzed using IBM
years of age in Kano state-Nigeria, this may Statistical Package for the Social Sciences
provide insight into proper patient management (SPSS) version 22 (IBM Inc., Chicago, IL, USA).
that may lead to a better clinical outcome. The results were summarized as frequencies,
and mean ± standard deviation in tables and
MATERIALS AND METHODS charts. Mean values of total blood count were
This cross sectional study was carried out compared between the malaria positive and
among children under the age of five years with control groups using student’s t-test. P-value of
primary diagnosis of malaria at Murtala <0.05 was considered level of significance at
Muhammad Specialist Hospital, Kano state- 95% confidence interval.
Nigeria.
Inclusion and Exclusion Criteria: Children RESULTS
under 5 years diagnosed with or without The results showed that the mean Haemoglobin
malarial infection at paediatrics of Murtala concentration (HGB) of malaria infected
Muhammad Specialist Hospital Kano were children was significantly lower (9.08±2.30g/dl)
included in this study, while other children compared to that of the control group
above 5 years of age were excluded. (10.77±3.24g/dl), (p<0.05) Table 1. Similarly,
the hematocrit of the infected children was
Ethical Consideration: Ethical clearance for significantly lower (25.58±6.28%) than that of
the study, with number MOH/OFF/797/T.I/1392 the controls of (29.97±7.58%), (p<0.05). The
was obtained from the Research Ethics Mean Corpuscular Haemoglobin Concentration
Committee, Kano state Ministry of health. (MCHC) of malaria infected group was also
Ascent was sought from the guardians of the found to be significantly lower
participating children, having explained to (31.03±8.05g/dL) compared to the controls
them the purpose of the research and its (35.77±4.75g/dL), p<0.05. However, there was
relevance. no significant difference in the mean values of
MCV was 70.50±7.04 and 72.16±11.6 for the
UMYU Journal of Microbiology Research www.ujmr.umyu.edu.ng
94
UJMR, Vol. 7 Number 1, June, 2022, pp 93-98 E-ISSN: 2814 – 1822; P-ISSN: 2616 – 0668
cases and control respectively, p˃0.05. The group was 32.45±7.54. The difference was also
mean value for MCH in the malaria infected not statistically significant, p˃0.05.
group was 25.77±4.48 while that of control
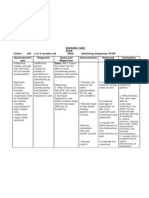
Table 1: Haematological profile of malaria positive and malaria negative patients attending Murtala
Muhammad Specialist Hospital Kano.
Parameter Controls Cases p value
HGB(g/dL) 10.77±3.24 9.08±2.30 0.046
HCT(%) 29.97±7.58 25.58±6.28 0.042
MCV(fl) 72.16±11.64 70.50±7.04 0.062
MCH(pg) 32.45±7.54 25.77±4.48 0.056
MCHC(g/dL) 35.77±4.75 31.03±8.05 0.032
HGB=Heamoglobin, HCT=Haematocrit, MCV=Mean Corpuscular Volume, MCH=Mean Corpuscular
Heamoglobin, MCHC=Mean Corpuscular Heamoglobin Concentration
The results of the WBC count among the malaria infected children was (9.13±3.24×10 3/µL) while
that of the controls was (8.94±4.08×10 3/µL) with no statistically significant difference between the
groups, p˃0.05, figure 1. The RBC counts were lower in malaria infected (3.64±1.09×10 6/µL),
compared to the controls with (4.16±0.86×10 6/µL) there was no statistically significant difference
between the groups too, p˃0.05. The platelet count (PLT) of the malaria children was however
statistically significantly lower in the cases (172.27±120.65×10 3/µL) than the controls
(240.73±143.23×103/µL), (P<0.05).
Figure: 1 Comparisons of WBC, RBC and PLT of the malaria positive and negative patients attending
Murtala Muhammad Specialist Hospital Kano.
The WBC diffrentials (figure 2) showed that the (5.90±4.54%) compared to the controls with
Lymphocytes of the infected were (5.91±5.26%), and the neutrophils (NEUT) of the
(54.89±13.79%) compared to the controls of infected were (43.46±12.72%) compared to the
(57.55±24.42%) the differences were not control with mean value of (36.54±24.48%).
signiicant (P>0.05). Similarly, monocytes (MXN) There were no significant difference in the
of the malaria infected groups were mean values in both cases (P>0.05).
UMYU Journal of Microbiology Research www.ujmr.umyu.edu.ng
95
UJMR, Vol. 7 Number 1, June, 2022, pp 93-98 E-ISSN: 2814 – 1822; P-ISSN: 2616 – 0668
Figure 2: Percentages Lymphocytes (LYM), Monocytes (MXD) and Neutrophils (NEUT) of malaria
positive and negative patients attending Murtala Muhammad Specialist Hospital Kano
DISCUSSION in a cross-sectional study among children in a
Children, especially under five years, are Municipality in Ghana. White blood cell changes
usually susceptible to malaria infection which in malaria depend on factors like;
can result in anaemia that may easily cause parasitaemia, host immune status and the
death. It has been reported that malaria has presence of co-infections (Abdalla and Pasvol
multifactorial mechanisms through which it 2004, Faga et al., 2020, Xin-zhuan et al.,
leads to anemia. For example; increased 2020). The body’s immune response to
damage of parasitized and non-parasitized infections such as malaria may involve
RBCs, is the primary factor leading to anemia neutrophils, macrophages or Natural killer (NK)
development in malaria (White, 2018). cells (Vivier et al., 2011). Findings in this study
Suppressed erythropoiesis during days and or showed no significant changes in monocyte
weeks after acute malaria also contributes to count in parasitemic patients compared to the
anemia (Balarajan et al., 2011) and also do non-parasitemic patients. This was in contrast
shortened red blood cells lifespan and to a previous study which found monocytosis as
increased red cell clearance (White, 2018). one of the most significant observations of
In this study the results showed significant hematological changes among children infected
decreases in RBC, HCT, MCHC and haemoglobin with malaria (Bawah et al., 2018).. Neutrophil
concentration in the malaria positive group counts were also analysed in this study. The
compared to the control group. Reduction of results showed that the mean neutrophil count
these values reflected anaemia as stated by between the parasitemic and non-parasitemic
(Francis et al., 2014). These results were in children was not significantly different. These
line with those reported by (Bawah et al., findings were similar to those from previous
2018; Awoke and Arota, 2019). Malaria has studies in Ghana (Bawah et al., 2018), India
been implicated as a cause of severe anemia, in (Akhtar et al., 2012) and Singapore
association with severe complications, including (Wickramasinghe et al., 2000) respectively,
death (White 2018, Camila et al., 2019). where they reported no significant increase in
White blood cells play crucial role in the body’s neutrophil count between those with malaria
defense against malaria. This study found an and those without malaria. The
overall increase in white blood cell count pathophysiological processes of neutropenia in
among the malaria infected children compared malaria has been reported to involve amplified
to those without malaria, though the increase margination and sequestration of neutrophils
was not statistically significant. This was resulting from the augmented expression of cell
consistent with the findings of Bawah et adhesion molecules (ICAM-1 and VCAM-1) that
al.,(2018) which found increase in WBC count in occurs in malaria (Clark et al., 2006).
children with malaria compared to the controls
UMYU Journal of Microbiology Research www.ujmr.umyu.edu.ng
96
UJMR, Vol. 7 Number 1, June, 2022, pp 93-98 E-ISSN: 2814 – 1822; P-ISSN: 2616 – 0668
Our results also showed no significant was in consonant with that of Oluwaseun et
difference in the total lymphocyte count in al., (2021) and Bawah et al., (2018) who also
malaria parasitaemia, similar to some previous reported a significant decrease in platelets
studies which found lymphocyte count counts in malaria positive patients compared to
remaining unchanged during an acute malaria control group.
infection (Abdalla et al.,1988; Adedotun et al.,
2013). CONCLUSION
Thrombocytopenia, a condition of low platelet This study has clearly demonstrated that
count, is one of the most commonly reported malaria significantly affects the hematopoieitic
hematological abnormalities in malaria system in children under five years living in
patients. Thrombocytopenia is said to occur Kano state-Nigeria. The most important effects
probably as a result of destruction and removal on hematological parameters observed in the
of platelets by spleen, in addition to platelet study were anemia and thrombocytopenia both
depletion by disseminated intravascular of which can result in catastrophe if not
coagulopathy (Bidaki et al., 2003, Kassa et al., properly managed. The importance of the two
2005 Rasheed et al., 2009). Our study found a haematologic derangements would mean that
strong relationship between thrombocytes all children under the age of five who reported
count and plasmodium infection. The children with malaria should be closely monitored and a
with malaria infection had statistically full blood count be carried out in cases of
significantly lower levels of platelets compared moderate to severe malaria.
to those free of malaria infection. This result
REFERENCES Aden. Turkish Journal of Hematology.
Abdalla, S.H., and Pasvol, G. (2004). Malaria: A 30:394–399.
Hematological Perspective, Volume 4. Balarajan, Y., Ramakrishnan, U., and Özaltin,
London, UK: Imperial College Press. E. (2011). Anemia in low-income and
Abdalla, S.H. (1988). Peripheral blood and bone middle-income countries. Lancet 378:
marrow leucocytes in Gambian children 2123–2135.
with malaria: Numerical changes and Bawah, A.T., Nyakpo, K.T., Ussher, F.A., Alidu,
evaluation of phagocytosis. Annals of H., Dzogbo J.J. et al., (2018).
Tropical Paediatrics 8(4):250–258. Hematological profile of children under
Adedotun, A. A., Salawu, O. T., Morenikeji, O. five years with malaria at the Ho
A. and Odaibo A. B. (2013) Plasmodial Municipality of Ghana. Edorium Journal
infection and haematological of Pediatrics 2018;2:100004P05.
parameters in febrile patients in a Bidaki, Z., and Dalimi, A. (2003). Biochemical
hospital in Oyo town, South-western and hematological alteration in vivax
Nigeria. Journal of Public Health and malaria in Kahnouj city. Journal of
Epidemiology 5(3):144-148. Rafsanjan University of Medical
Akhtar, S., Gumashta, R., Mahore, S., and Sciences. ;3:17–24
Maimoon, S. (2012). Hematological Camila, M., Chaparro, Parminder S. And
changes in malaria: A comparative Suchdev (2019) Anemia epidemiology,
study. IOSR Journal of Pharmacy pathophysiology, and etiology in low-
Biological Science; 2(4):15–19. and middle-income countries. Annals of
Arévalo-Herrera M, Rengifo L, Lopez-Perez M, the New York academy of sciences;
Arce-Plata MI, García J, Herrera S 1450(1): 15-31.
(2017) Complicated malaria in children Clark, I.A., Budd, A.C., Alleva, L.M., and
and adults from three settings of the Cowden, W.B (2006). Human malarial
Colombian Pacific Coast: A prospective disease: A consequence of
study. PLoS ONE 12(9) inflammatory cytokine release. Malaria
Awoke N, Arota A. (2019) Profiles of journal; 10;5:85.
hematological parameters Conroy A. L, Datta D, John C. C. (2019). What
in Plasmodium causes severe malaria and its
falciparum and Plasmodium complications in children? Lessons
vivax malaria patients attending Tercha learned over the past 15 years. BMC
General Hospital, Dawuro Zone, South Medicine. 17(1):52.
Ethiopia. Infection and Drug Resistance Faga D C, Obisike V U, Onah I E and Amuta E U.
5 (12):521-527. (2020). Assessment of Malaria
Bakhubaira S (2013). Hematological parameters Parasitemia and Genotype of Patients
in severe complicated Plasmodium attending two Hospitals in Benue State,
falciparum malaria among adults in
UMYU Journal of Microbiology Research www.ujmr.umyu.edu.ng
97
UJMR, Vol. 7 Number 1, June, 2022, pp 93-98 E-ISSN: 2814 – 1822; P-ISSN: 2616 – 0668
Nigeria. Animal Research International Urban Communities in Southwestern
17(2): 3640 – 3648 Nigeria: A Cross-Sectional Study.
Jiero S., and Pasaribu AP. (2021). Infection and Drug Resistance. 14 3219–
Haematological profile of children with 3232
malaria in Sorong, West Papua, Rasheed, A., Saeed, S. and Khan, S. (2009).
Indonesia. Malaria Journal. Clinical and laboratory findings in acute
4;20(1):126. malaria caused by various Plasmodium
Kassa D, Petros B, Messele T, Admassu A, species. Journal of Pakistan Medical
Adugna F, et al., (2005). Parasito- Association 59:220.
haematological features of acute Xin-zhuan S, Cui Z, and Deirdre A J. (2020)
Plasmodium falciparum and P. vivax Host-Malaria Parasite Interactions and
malaria patients with and without HIV Impacts on Mutual Evolution. Frontiers
co-infection at Wonji Sugar Estate, in Cellular and Infection Microbiology.
Ethiopia. The Ethiopian Journal of Vivier, E., Raulet, D.H, Moretta, A., et al.
Health Development 19(2):132–139. (2011). Innate or adaptive immunity?
Morakinyo, O.M., Balogun, F.M., and The example of natural killer cells.
Fagbamigbe, A.F (2018). Housing type Science 7;331(6013):44–49.
and risk of malaria among under-five Waris R, Aurengzeb B, Raza SH, Waris A, and
children in Nigeria: evidence from the Riaz R. (2021) Clinical Profile and
malaria indicator survey. Malaria Spectrum of Complications of Malaria in
Journal; 17(1):1. doi:10.1186/ s12936- Hospitalized Children at a Tertiary Care
018-2463-6 Hospital. Journal of Rawalpindi Medical
Muwonge, H., Kikomeko, S., Sembajjwe, L.F., College 25(4): 516-520
Seguya, A. and Namugwanya, C. (2013). White, N.J. (2018): Anaemia and
How reliable are hematological malaria. Malaria Journal 17(1):371.
parameters in predicting uncomplicated Wickramasinghe, S.N., and Abdalla, S.H (2000).
Plasmodium falciparum malaria in an Blood and bone marrow changes in
endemic region? ISRN Tropical Medicine malaria. Baillieres Best Practice and
:1–9. Research in Clinical
Ntenda, P.A.M., Chilumpha, S., Mwenyenkulu, Haematology;13(2):277–299.
E.T. et al. (2019). Clinical malaria and World Health Organization. 2015. Malaria
the potential risk of anaemia among Microscopy Quality Assurance Manual.
preschool-aged children: a population- Geneva: World Health Organization
based study of the 2015–2016 Malawi (2009). World Health Organization
micronutrient survey. Infectious (WHO). World Malaria Report.
Diseases of Poverty 8, 95 World Health Organization (2020). World
Oluwaseun, B.A., Zary S.Y. and Meor. F. (2021). Malaria Report: 20 Years of Global
Prevalence, Parasite Density and Progress and Challenges. Geneva:
Determinants of Falciparum Malaria World Health Organization; 2020
among Febrile Children in Some Peri-
UMYU Journal of Microbiology Research 98 www.ujmr.umyu.edu.ng
You might also like
- Hypoglycemia and Anemia Associated With Malaria Among Pregnant Mothers Living With HIV Attending Aminu Kano Teaching Hospital, Kano State-NigeriaDocument6 pagesHypoglycemia and Anemia Associated With Malaria Among Pregnant Mothers Living With HIV Attending Aminu Kano Teaching Hospital, Kano State-NigeriaUMYU Journal of Microbiology Research (UJMR)No ratings yet
- Haematological Changes in Malaria-Infected Children in North-West NigeriaDocument6 pagesHaematological Changes in Malaria-Infected Children in North-West NigeriamubarakNo ratings yet
- A Study of Haematological Profile of Malaria in A Tertiary Care Centre of Western Uttar Pradesh, IndiaDocument5 pagesA Study of Haematological Profile of Malaria in A Tertiary Care Centre of Western Uttar Pradesh, IndiaramperoughNo ratings yet
- Bacteriological Profile of Neonatal Sepsis and Antibiotic Susceptibility Pattern of Isolates Admitted at Kanti Children's Hospital, Kathmandu, NepalDocument6 pagesBacteriological Profile of Neonatal Sepsis and Antibiotic Susceptibility Pattern of Isolates Admitted at Kanti Children's Hospital, Kathmandu, NepalPSIK sarimuliaNo ratings yet
- Research ArticleDocument7 pagesResearch ArticleerikaNo ratings yet
- Cohorte 10 PDFDocument7 pagesCohorte 10 PDFLaura MottaNo ratings yet
- Literature Review of Plasmodium FalciparumDocument6 pagesLiterature Review of Plasmodium Falciparumea83xjp7100% (1)
- 8 Malaria Is An Uncommon Cause of Adult Sepsis in SouthDocument9 pages8 Malaria Is An Uncommon Cause of Adult Sepsis in SouthAhmad Zaki YamaniNo ratings yet
- Current Literature Review On MalariaDocument6 pagesCurrent Literature Review On Malariaea3h1c1p100% (1)
- Reported Incidence of Fever For Under-5 Children in Zambia: A Longitudinal StudyDocument7 pagesReported Incidence of Fever For Under-5 Children in Zambia: A Longitudinal StudyBassim BirklandNo ratings yet
- AnemiaDocument9 pagesAnemiaJhonatan David Diaz IdarragaNo ratings yet
- JurnaL MalariaDocument10 pagesJurnaL Malariamufida harianiNo ratings yet
- MDR Somalia EID March 2013Document3 pagesMDR Somalia EID March 2013hirsi200518No ratings yet
- Incidence of Plasmodium Infections and Determinant Factors Among Febrile Children in A District of Northwest Ethiopia A Cross-Sectional StudyDocument18 pagesIncidence of Plasmodium Infections and Determinant Factors Among Febrile Children in A District of Northwest Ethiopia A Cross-Sectional StudyMegbaruNo ratings yet
- Impact of Malaria at The End of Pregnancy On Infant Mortality and MorbidityDocument9 pagesImpact of Malaria at The End of Pregnancy On Infant Mortality and MorbidityDebby Astasya AnnisaNo ratings yet
- The Silent Anaemia Epidemic in ChildrenDocument5 pagesThe Silent Anaemia Epidemic in ChildrenInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Anemia2014 108593Document9 pagesAnemia2014 108593AaronMaroonFive100% (1)
- 21, Malaria Vs Dengue 2020Document4 pages21, Malaria Vs Dengue 2020Raquel FernandezNo ratings yet
- Research Article: Risk Factors and Prevention Strategies of Nosocomial Infection in Geriatric PatientsDocument6 pagesResearch Article: Risk Factors and Prevention Strategies of Nosocomial Infection in Geriatric Patientschristian demasabuNo ratings yet
- A Study of Thrombocytopenia in Malaria and Its Prognostic SignificanceDocument6 pagesA Study of Thrombocytopenia in Malaria and Its Prognostic SignificanceBobby Faisyal RakhmanNo ratings yet
- Caselli 2014Document5 pagesCaselli 2014AdrianaGallardoTapiaNo ratings yet
- Plasmodium Falciparum Gametocyte Dynamics in Areas of Different Malaria EndemicityDocument22 pagesPlasmodium Falciparum Gametocyte Dynamics in Areas of Different Malaria EndemicityAlemayehu Letebo AlbejoNo ratings yet
- Rheumatoid Arthritis A Single Center Egyptian Experience CorretedDocument11 pagesRheumatoid Arthritis A Single Center Egyptian Experience CorretedSara EhabNo ratings yet
- Ref 5 PDFDocument6 pagesRef 5 PDFGabriyah HamzahNo ratings yet
- Clinico-Epidemiological Profile and Predictors of Outcome in Children With Diphtheria: A Study From Northern IndiaDocument6 pagesClinico-Epidemiological Profile and Predictors of Outcome in Children With Diphtheria: A Study From Northern IndiamariaprincesitaNo ratings yet
- Jurnal Risk FX SepsisDocument7 pagesJurnal Risk FX SepsiswilmaNo ratings yet
- BongDocument1 pageBongRod Reynon BorceNo ratings yet
- 217170-Article Text-534583-1-10-20211109Document8 pages217170-Article Text-534583-1-10-20211109SMA N 1 TOROHNo ratings yet
- Prevalence of Malaria Among Patients at The Sino-Gabonese Friendship Hospital in Franceville A Two-Year Retrospective StudyDocument8 pagesPrevalence of Malaria Among Patients at The Sino-Gabonese Friendship Hospital in Franceville A Two-Year Retrospective StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Bacteriological Prevalence Tuberculosis Among Children Seen Health Facilities Nasarawa State Nigeria 2576 8484 EAST 18 121Document5 pagesBacteriological Prevalence Tuberculosis Among Children Seen Health Facilities Nasarawa State Nigeria 2576 8484 EAST 18 121fatimakh462No ratings yet
- Rotavirus Epidemiology in Bangui, Central African Republic, 2008Document2 pagesRotavirus Epidemiology in Bangui, Central African Republic, 2008Mark ReinhardtNo ratings yet
- Research Article: Machine Learning-Based Model To Predict The Disease Severity and Outcome in COVID-19 PatientsDocument10 pagesResearch Article: Machine Learning-Based Model To Predict The Disease Severity and Outcome in COVID-19 Patientsamin mohNo ratings yet
- Severe Sepsis-Associated Morbidity and Mortality Among Critically Ill Children With CancerDocument8 pagesSevere Sepsis-Associated Morbidity and Mortality Among Critically Ill Children With CancerFaki D'pasnizerNo ratings yet
- Trombosit Dan ParasitDocument5 pagesTrombosit Dan ParasitSaraswati Wulandari HartonoNo ratings yet
- Nej Mo A 0807381Document12 pagesNej Mo A 0807381Mildred MontNo ratings yet
- Immunogenicity of Fractional-Dose Vaccine During A Yellow Fever Outbreak - Preliminary ReportDocument9 pagesImmunogenicity of Fractional-Dose Vaccine During A Yellow Fever Outbreak - Preliminary Reportrizki agusmaiNo ratings yet
- Trends and Determinants of Maternal Mortality in Mizan-Tepi University Teaching and Bonga General Hospital From 2011 - 2015: A Case Control StudyDocument8 pagesTrends and Determinants of Maternal Mortality in Mizan-Tepi University Teaching and Bonga General Hospital From 2011 - 2015: A Case Control StudyTegenne LegesseNo ratings yet
- Acta Tropica 209 2020 105544Document11 pagesActa Tropica 209 2020 105544cdsaludNo ratings yet
- Goldman Miller Vaccine Hospitalization Study HETDocument11 pagesGoldman Miller Vaccine Hospitalization Study HETGeeleegoatNo ratings yet
- Pneumonia FrancisDocument6 pagesPneumonia Francistihitna yosefNo ratings yet
- Research Article Clinical and Epidemiological Determinants of Lower Respiratory Tract Infections in Hospitalized Pediatric PatientsDocument7 pagesResearch Article Clinical and Epidemiological Determinants of Lower Respiratory Tract Infections in Hospitalized Pediatric Patientshasemana hasemanaNo ratings yet
- Literature Review On Malaria in GhanaDocument8 pagesLiterature Review On Malaria in Ghanaea3mfh42100% (1)
- Determinants of Malaria Control Programs For Children Under 5 Years at Mubende Regional Referral Hospital in Central UgandaDocument12 pagesDeterminants of Malaria Control Programs For Children Under 5 Years at Mubende Regional Referral Hospital in Central UgandaKIU PUBLICATION AND EXTENSIONNo ratings yet
- Hematological Abnormalities in Patients With Malaria and Typhoid in Tamale Metropolis of GhanaDocument6 pagesHematological Abnormalities in Patients With Malaria and Typhoid in Tamale Metropolis of GhanakynatroemanNo ratings yet
- Megbaru 10 PDFDocument7 pagesMegbaru 10 PDFMegbaruNo ratings yet
- 1471 2334 13 123Document10 pages1471 2334 13 123Laurelle Winnie Kouankep WandjiNo ratings yet
- Pharmaceutical Sciences: Acute Complications and Mortality Spectrum in Bacterial MeningitisDocument5 pagesPharmaceutical Sciences: Acute Complications and Mortality Spectrum in Bacterial MeningitisiajpsNo ratings yet
- 80 Iajps80122017 PDFDocument4 pages80 Iajps80122017 PDFBaru Chandrasekhar RaoNo ratings yet
- Thrombocytopenia As An Index of Plasmodium Falciparum Severity in Adult Population A Review PaperDocument2 pagesThrombocytopenia As An Index of Plasmodium Falciparum Severity in Adult Population A Review PaperInternational Journal of Innovative Science and Research Technology100% (1)
- Iran FungusDocument7 pagesIran FungusHaruka KanataNo ratings yet
- Detectable Viral Load and Human Immuno Deficiency Drug ResistanceDocument11 pagesDetectable Viral Load and Human Immuno Deficiency Drug ResistanceFelistus KanjiraNo ratings yet
- Antibiotic Coated Shunt ManuscriptDocument6 pagesAntibiotic Coated Shunt ManuscriptBilal ErtugrulNo ratings yet
- Nwalozie RMdoiideDocument11 pagesNwalozie RMdoiideijmb333No ratings yet
- Impact of Rotavirus Vaccine Introduction On Rotavirus Hospitalizations Among Children Under 5 Years of Age World Health Organization African Region 20082018clinical Infectious DiseasesDocument4 pagesImpact of Rotavirus Vaccine Introduction On Rotavirus Hospitalizations Among Children Under 5 Years of Age World Health Organization African Region 20082018clinical Infectious DiseasesKajelcha FikaduNo ratings yet
- MCN 12870Document31 pagesMCN 12870Megan HarperNo ratings yet
- Pinda FynDocument7 pagesPinda FynCaballero X CaballeroNo ratings yet
- Relative Trends in Hospitalizations and Mortality Among Infants by The Number of Vaccine DosesDocument11 pagesRelative Trends in Hospitalizations and Mortality Among Infants by The Number of Vaccine DosesBobNo ratings yet
- Jurnal Respi - Comparison of IGRA AssayDocument5 pagesJurnal Respi - Comparison of IGRA AssaykaynabilNo ratings yet
- Predictors For Low Coverage of Uptake of Second Dose of Measles Vaccine Among Children in Sub-Saharan Africa 2023 A Systematic Review and Meta-AnalyDocument19 pagesPredictors For Low Coverage of Uptake of Second Dose of Measles Vaccine Among Children in Sub-Saharan Africa 2023 A Systematic Review and Meta-AnalyPutraNo ratings yet
- Adenomiosis CX ConservadoraDocument12 pagesAdenomiosis CX Conservadorajuan carlos pradaNo ratings yet
- Achalasia EsophagiaDocument4 pagesAchalasia EsophagiaRee AhmedNo ratings yet
- Nle Final Coaching Jul 3-4-2021Document1 pageNle Final Coaching Jul 3-4-2021Linsae HiyasNo ratings yet
- CUA Cost Utility AnalysisDocument10 pagesCUA Cost Utility AnalysisGloryNo ratings yet
- Resultados SaludDignaDocument2 pagesResultados SaludDignaAdriana RamosNo ratings yet
- Geriatric ...... Dental CareDocument39 pagesGeriatric ...... Dental CareDelvine AderoNo ratings yet
- Incentive SpirometryDocument5 pagesIncentive Spirometryrachelmores12No ratings yet
- Test CaeDocument3 pagesTest CaegabiNo ratings yet
- Equine Field SurgeryDocument6 pagesEquine Field SurgeryRuchiNo ratings yet
- Structural Organisation in AnimalsDocument23 pagesStructural Organisation in AnimalsMothi KarunaNo ratings yet
- 9814774723Document467 pages9814774723Ortopedia FabioNo ratings yet
- NCP - Ineffective Airway ClearanceDocument4 pagesNCP - Ineffective Airway ClearanceKen RegalaNo ratings yet
- Local AnestheticsDocument47 pagesLocal AnestheticsKeerthi LakshmiNo ratings yet
- STS Video ScriptDocument2 pagesSTS Video ScriptCynthia Y De VeraNo ratings yet
- Maternal and Foetal Outcomes in Pregnancy With Gestational Thrombocytopenia: A Prospective Observational StudyDocument6 pagesMaternal and Foetal Outcomes in Pregnancy With Gestational Thrombocytopenia: A Prospective Observational StudyIJAR JOURNALNo ratings yet
- Massage Intake FormDocument2 pagesMassage Intake Formapi-253959832No ratings yet
- Forgiveness Therapy: An Empirical Guide For Resolving Anger and Restoring HopeDocument6 pagesForgiveness Therapy: An Empirical Guide For Resolving Anger and Restoring HopeTanveerraza DaisyNo ratings yet
- Pharmacology Test 1 Drug ListDocument20 pagesPharmacology Test 1 Drug ListSHRIKANTNo ratings yet
- Cardioogy and Nephrology, MCQ'sDocument5 pagesCardioogy and Nephrology, MCQ'sLong Live PakistanNo ratings yet
- Non-Melanoma Skin Cancer of The Head and Neck 2015Document214 pagesNon-Melanoma Skin Cancer of The Head and Neck 2015Alejandro Santini BlascoNo ratings yet
- Test 1 Part 1 TapecsriptDocument19 pagesTest 1 Part 1 TapecsriptMerryNo ratings yet
- Comprehensive Periodontics Dental Hygienist 4th Weinberg Test Bank PDFDocument8 pagesComprehensive Periodontics Dental Hygienist 4th Weinberg Test Bank PDFEmeka NnajiNo ratings yet
- Essay 2 Working With Crisis and Trauma Draft 1 DO THHIS ONE Auto Saved) Auto Saved) Auto Saved)Document26 pagesEssay 2 Working With Crisis and Trauma Draft 1 DO THHIS ONE Auto Saved) Auto Saved) Auto Saved)Emily SummersNo ratings yet
- Acutepainmanagement: Nabil Moussa,, Orrett E. OgleDocument13 pagesAcutepainmanagement: Nabil Moussa,, Orrett E. OgleMahmoud AbouelsoudNo ratings yet
- Gicaro CED101IEWrittenOutputDocument15 pagesGicaro CED101IEWrittenOutputAlyssa GicaroNo ratings yet
- COVID-19 and The Need For Dynamic State Capabilities:: An International ComparisonDocument30 pagesCOVID-19 and The Need For Dynamic State Capabilities:: An International ComparisonTomas TomicNo ratings yet
- Intro To AromatherapyDocument58 pagesIntro To AromatherapyrameshgounderNo ratings yet
- Class V Amalgam CavityDocument65 pagesClass V Amalgam CavityJasper Tan Min ZhenNo ratings yet
- Freud and AnesthesiaDocument5 pagesFreud and AnesthesiaRaluca LNo ratings yet
- Pathophysiology of Upper Gastrointestinal BleedingDocument1 pagePathophysiology of Upper Gastrointestinal BleedingkimmybapkiddingNo ratings yet