Professional Documents
Culture Documents
Poster
Uploaded by
Lana kamal0 ratings0% found this document useful (0 votes)
5 views1 pageCopyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views1 pagePoster
Uploaded by
Lana kamalCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
Antepartum, Intrapartum, Postpartum Predictors
and Outcomes of Discharge Readiness
Gabriella Malagon-Maldonado, PhD, DNP, APRN, CNS, NEA-BC
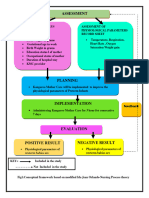
Background Adaptation to Transitions Conceptual Framework Methods
Patient Outcomes •Research Design: Descriptive correlational
• Discharge before a mother is physically and/or repeated measures design
psychologically ready, places the mother and
Antepartum Intrapartum Postpartum
infant at a greater risk of detrimental maternal and •Setting: 72-bed postpartum unit with mother-baby
infant outcomes Nature of Transition Patterns of couplet care in a non-profit women’s specialty
Transition and Conditions Response hospital
Education and Policy
Environmental and Coping and
• Newborns’ and Mothers’ Health Protection Act Adaptation •Sample: 185 postpartum mothers, 18 years of
shortened the length of hospital stay Stimuli Processes age, uneventful post-birth experience, mothers with
• Physical, psychological, and social well-being
Modes infants who were not transferred to the NICU,
needs of mother and infant must be addressed sufficient English or Spanish language skills
prior to discharge
•Twenty-four hours prior to discharge:
Transitions of Care and Financial Implications -Demographic Questionnaire
• Limited improvements in care transitions are Nursing -Readiness for Hospital Discharge Scale
related to understanding the maternal and infant Therapuetics/ -Quality of Discharge Teaching Scale
factors contributing to poor outcomes Interventions
• Reimbursement payments are associated with •Four weeks post-discharge:
nurses’ communication with patients and families -Post-Discharge Coping Difficult Scale
and discharge information -Quality of Discharge Teaching Scale
Purpose Results Implications
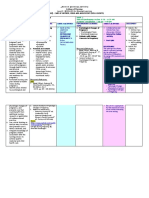
Demographics: Participants’ mean age was 30.8, Q2. Predictors of Coping Difficulty: •The quality of discharge teaching as a predictor
majority were Caucasian (41.6%), married & living
The purpose of this study was to explore the
Variable Statistics of readiness for hospital discharge, post-
with the father of the infant (74.6%), & had a
antepartum, intrapartum, and postpartum factors, bachelor’s degree (31.4%). Majority planned on Predictor Variables Model B SE B Standardized t P
discharge coping, and health care utilization,
including nursing practices, associated with returning to work full-time (43.8%), had an average of provides evidence of the importance of patient
Statistics β
readiness for hospital discharge and the two children, delivered vaginally (61.6%) with an Antepartum Characteristics F(6,60)=5.1 -1.8 0.86 -0.24 -2.1 0.04
and family education
average length of stay 2.9 days, and were P=<0.001
subsequent outcomes after hospitalization. (a) Less than High School R2=0.33
breastfeeding upon discharge (70.8%). Infants’ Education Adjusted •Discharge teaching requires attention to
R2=0.28 -0.2 0.09 -0.27 -2.2 0.03
gestational mean age was 38.9 weeks & length of stay Nursing Interventions
adequacy of content and delivery of information
on average was 2.7 days. influencing a patients’ readiness of hospital
(b) Content difference subscale
Research Questions Variable Statistics Q2. Predictors of Service Utilization:
discharge
Predictor Variables Model B SE B Standardized t P
Q1. Predictors of Readiness: Logistic Regression Statistics
•Conceptualizing and investigating the transition
Outcome Variables Significant B SE B χ2 Odds 95% CI P
1. What antepartum, intrapartum, and postpartum Statistics β
Predictor Ratio home after hospital is essential to improve
factors ,including nursing practices, are Postpartum characteristics F(8,176)=17.5
Variables
organizational structures and processes to
Calls to healthcare PDCDS 0.54 0.22 5.79 1.71 (1.11-2.64) 0.02
predictive of postpartum mothers’ perceptions (a) Infant LOS P=<0.001 -0.21 0.1 -0.2 2.05 0.04
providers facilitate optimal patient outcomes
Calls to hospital Content -1.18 0.44 7.19 0.31 (0.13-0.73) 0.01
of readiness for hospital discharge? Received
Nursing Interventions R2=0.44
Delivery 1.41 0.64 4.78 4.08 (1.16-14.3) 0.03 References/Acknowledgments
(b) Delivery subscale Adjusted 0.45 0.06 0.51 7.06 <0.001 Office/Clinic visits Delivery 1.43 0.5 8.22 4.18 (1.57-11.1) 0.004
PDCDS 0.74 0.34 4.84 2.09 (1.08-4.03) 0.03 References available on handout.
2. What are the factors associated with post- (c) Content difference subscale R2=0.42 0.15 0.04 0.22 3.55 <0.001
Content -0.65 0.31 4.38 0.52 (0.28-0.96) 0.04 Acknowledgements: Drs. Cynthia Connelly, Ruth
discharge coping difficulty and utilization of Received
support and health services? • Qualitative Results: Bush, Jane Georges; Bob and Betty Beyster, USD
• Resources, staff, and delivery of specific • Qualitative Results: School of Nursing and Health Science, and Sharp
information • Health, infant, family needs HealthCare’s Center of Nursing Excellence
You might also like
- 2017 Pcep Specialized Newborn Care 4 PDFDocument171 pages2017 Pcep Specialized Newborn Care 4 PDFmagnumforce 007No ratings yet
- Lesson Plan Antenatal AssessmentDocument5 pagesLesson Plan Antenatal AssessmentDelphy Varghese100% (6)
- Assited Reproductive TechnologyDocument40 pagesAssited Reproductive TechnologySanthosh.S.UNo ratings yet
- Cesarean SectionDocument11 pagesCesarean SectionChristine SaliganNo ratings yet
- Kami Export - I Am Sharing 'PCEP - Book 4 - Specialized Newborn Care - 4th Edition' With YouDocument260 pagesKami Export - I Am Sharing 'PCEP - Book 4 - Specialized Newborn Care - 4th Edition' With YouZeljka Dobric KelecevicNo ratings yet
- Ebn Poster 2Document1 pageEbn Poster 2api-352392191No ratings yet
- Kami Export - I Am Sharing 'PCEP - Book 3 - Neonatal Care - 4th Edition (1) ' With YouDocument466 pagesKami Export - I Am Sharing 'PCEP - Book 3 - Neonatal Care - 4th Edition (1) ' With YouZeljka Dobric KelecevicNo ratings yet
- Toolkit To Support Vaginal Birth and Red PDFDocument159 pagesToolkit To Support Vaginal Birth and Red PDFbarirwandaNo ratings yet
- Dessertation PresentationDocument9 pagesDessertation PresentationKinjal VasavaNo ratings yet
- Womens Health NP DNPDocument1 pageWomens Health NP DNPSundar ChandranNo ratings yet
- CONCEPTUAL FRAN Ida Jean Orlando (3) 46 7Document5 pagesCONCEPTUAL FRAN Ida Jean Orlando (3) 46 7Roopa KatariaNo ratings yet
- PQCNC New Initiative Proposal NASDocument9 pagesPQCNC New Initiative Proposal NASkcochranNo ratings yet
- E-Poster Rcog 2018Document1 pageE-Poster Rcog 2018Ana MarianaNo ratings yet
- Heine Ashley CapstonePosterDocument1 pageHeine Ashley CapstonePosterJudy JneydNo ratings yet
- PicoDocument8 pagesPicoJulliza Joy PandiNo ratings yet
- Ebp Early Implementation of Pediatric Palliative Care PetersonDocument1 pageEbp Early Implementation of Pediatric Palliative Care Petersonapi-742879730No ratings yet
- RLE New FormatDocument5 pagesRLE New FormatRegie Arceo BautistaNo ratings yet
- Bioethics Chapter 1 NotesDocument22 pagesBioethics Chapter 1 NotesJerome CruzNo ratings yet
- FPC in IndiaDocument4 pagesFPC in IndiapriyahospitalNo ratings yet
- ARv 9 B XCZVPB X7 UB50 NG QTF DB B9 PBSV RCGJ JKDocument34 pagesARv 9 B XCZVPB X7 UB50 NG QTF DB B9 PBSV RCGJ JKrezimoralesNo ratings yet
- Cues 1Document2 pagesCues 1Claire SabayNo ratings yet
- CQE 7 Nursing Quality Indicators 1Document24 pagesCQE 7 Nursing Quality Indicators 1Inder Singh YadavNo ratings yet
- Tables and Figure - 30.03.2023Document22 pagesTables and Figure - 30.03.2023JimmyNo ratings yet
- 1 s2.0 S0884217521001738 MainDocument2 pages1 s2.0 S0884217521001738 Mainmia.dubon17213No ratings yet
- Syllabus NCM 109 Care of Mother Child Adolescent at Risk or With ProblemDocument37 pagesSyllabus NCM 109 Care of Mother Child Adolescent at Risk or With Problembrilliant dumay100% (1)
- "Digital Notebook" Theoretical Foundation in NursingDocument7 pages"Digital Notebook" Theoretical Foundation in NursingCyrel Rose TuñacaoNo ratings yet
- Poster ImtiyazDocument1 pagePoster ImtiyazImtiyazAmmarrizaNo ratings yet
- Icu MaternalDocument9 pagesIcu Maternalobgynunand2012No ratings yet
- Community FNCPDocument7 pagesCommunity FNCPCarl Jefferson Pagulayan100% (1)
- Establishing Breastfeeding: Maternity and Neonatal Clinical GuidelineDocument31 pagesEstablishing Breastfeeding: Maternity and Neonatal Clinical GuidelineDevi FitriNo ratings yet
- Cues 123Document1 pageCues 123Dara Arabella AndalesNo ratings yet
- Nursing Care of A Postpartal Woman and FamilyDocument44 pagesNursing Care of A Postpartal Woman and FamilyEvelyn Medina100% (1)
- DESSERTATIONDocument9 pagesDESSERTATIONKinjal VasavaNo ratings yet
- School Nurse Powerpoint Presentation For PSADocument22 pagesSchool Nurse Powerpoint Presentation For PSAmarierose matugasNo ratings yet
- Care of Mother, Child, AdolescentsDocument38 pagesCare of Mother, Child, AdolescentsAN1 M3No ratings yet
- 407 Lisenbee PDFDocument1 page407 Lisenbee PDFVika sagitaNo ratings yet
- MCNCHP 1 NotesDocument3 pagesMCNCHP 1 Noteshannahabigael.cajesNo ratings yet
- 1513 PDFDocument397 pages1513 PDFlider68No ratings yet
- FNCP SampleDocument19 pagesFNCP Samplekeithart fernandezNo ratings yet
- 12th MDCON Madam MiniDocument20 pages12th MDCON Madam MiniMinnie PamutanNo ratings yet
- Critique Presentation: Vaishali Rathava 2 Year M.SC Nursing ROLL NO:-09Document12 pagesCritique Presentation: Vaishali Rathava 2 Year M.SC Nursing ROLL NO:-09VaishaliNo ratings yet
- Post CsDocument2 pagesPost CsAlvin John BarramedaNo ratings yet
- FNCP BeastfeedingDocument1 pageFNCP BeastfeedingRizzy UgayNo ratings yet
- Maternal TransesDocument14 pagesMaternal TransesRhizel Marie Cauilan FariñasNo ratings yet
- Risk Case PresDocument1 pageRisk Case Presestavillok2367No ratings yet
- Alternative Related Learning Experience SY 2021-2022Document3 pagesAlternative Related Learning Experience SY 2021-2022Hannah VillavicencioNo ratings yet
- Nursing Preceptorship Re-Entry PlanDocument4 pagesNursing Preceptorship Re-Entry PlanMae DacerNo ratings yet
- Course Syllabus NCM 107Document8 pagesCourse Syllabus NCM 107EmmyNo ratings yet
- MODULE 3 MAT Prenatal Flexible LearningDocument2 pagesMODULE 3 MAT Prenatal Flexible LearningHas SimNo ratings yet
- SebmharpsterburkettDocument1 pageSebmharpsterburkettapi-355759761No ratings yet
- Best Practices For Transitioning Patients, 65 Years and Older, From The Hospital To Their Next Level of Care That Prevent Avoidable ReadmissionsDocument6 pagesBest Practices For Transitioning Patients, 65 Years and Older, From The Hospital To Their Next Level of Care That Prevent Avoidable ReadmissionsAnnold ochiezyNo ratings yet
- Addressing ACEs and Trauma in Primary Care Setting (AAP)Document7 pagesAddressing ACEs and Trauma in Primary Care Setting (AAP)AdvocateforPedsNo ratings yet
- Community FNCPDocument7 pagesCommunity FNCPSophia A. GoNo ratings yet
- Poster 5Document1 pagePoster 5rezimoralesNo ratings yet
- Obstetric Poster Presentation: Nnovative RogramsDocument1 pageObstetric Poster Presentation: Nnovative RogramsafsdsaadsNo ratings yet
- Dona DasDocument1 pageDona DasDona DasNo ratings yet
- SR MC EducationDocument8 pagesSR MC Educationimas KurniawatyNo ratings yet
- Graduate Nurses in The Intensive Care Unit: An Orientation ModelDocument10 pagesGraduate Nurses in The Intensive Care Unit: An Orientation ModelKhaskheli Nusrat100% (1)
- Fundies QsenDocument9 pagesFundies Qsenapi-534410130No ratings yet
- Nursing LeadershipDocument2 pagesNursing LeadershipReita RyuzakiNo ratings yet
- Ccrn Certification Examination Practice Questions and Answers with Rationale: First EditionFrom EverandCcrn Certification Examination Practice Questions and Answers with Rationale: First EditionRating: 5 out of 5 stars5/5 (1)
- Jurnal Persiapan Persalinan 1Document12 pagesJurnal Persiapan Persalinan 1rina astutiNo ratings yet
- Celand Interval BirthDocument33 pagesCeland Interval Birthinggar ratnakusumaNo ratings yet
- Hypoxic-Ischemic Encephalopathy (HIE)Document9 pagesHypoxic-Ischemic Encephalopathy (HIE)Ritu VermaNo ratings yet
- Comfort MeasuresDocument2 pagesComfort Measuresapi-550428187No ratings yet
- Diagnosis and Management of Ectopic Pregnancy-A Basic View Through LiteratureDocument2 pagesDiagnosis and Management of Ectopic Pregnancy-A Basic View Through LiteraturefprasasyaaNo ratings yet
- L03 - History Taking & Physical ExaminationDocument34 pagesL03 - History Taking & Physical ExaminationLemi teshomeNo ratings yet
- Nursing Update - DeliveryDocument1 pageNursing Update - DeliveryPatricia Bawiin †No ratings yet
- Hormones & Menstruation CycleDocument11 pagesHormones & Menstruation Cyclehiral mistryNo ratings yet
- The Short Child Review Article DR Azriyanti 2021Document10 pagesThe Short Child Review Article DR Azriyanti 2021tee qarafiNo ratings yet
- Articulo 4Document6 pagesArticulo 4Eduardo GarcíaNo ratings yet
- Case Scenario 10Document1 pageCase Scenario 10Mart Juaresa YambaoNo ratings yet
- OSCE On 14/3/2008: Describe Gynaecoid PelvisDocument82 pagesOSCE On 14/3/2008: Describe Gynaecoid PelvisKahing LiNo ratings yet
- Augmentation of Labour: Nabhan A, Boulvain MDocument8 pagesAugmentation of Labour: Nabhan A, Boulvain MMade SuryaNo ratings yet
- 1 Complications of L&D PowerDocument84 pages1 Complications of L&D PowerMarlon Glorioso II100% (1)
- CHN 1 Final Rle 1 Prenatal CareDocument4 pagesCHN 1 Final Rle 1 Prenatal CareYuunaFuentesLegaspiNo ratings yet
- Uganda National Adolesecent Health PolicyDocument27 pagesUganda National Adolesecent Health PolicyBashir KabuyeNo ratings yet
- Checklist DeliveryDocument3 pagesChecklist DeliveryChristian Paul PerezNo ratings yet
- Breech PresentationDocument46 pagesBreech PresentationushaNo ratings yet
- Country Profile: Philippines: Philippines Community Health Programs JANUARY 2015Document37 pagesCountry Profile: Philippines: Philippines Community Health Programs JANUARY 2015JB VillanuevaNo ratings yet
- Dapus PneumoniaDocument2 pagesDapus PneumoniaWiwin Angela KhairNo ratings yet
- Pre-Natal Development: (Review of Related Literature)Document15 pagesPre-Natal Development: (Review of Related Literature)Jamica Anne Rias CostinianoNo ratings yet
- DMCN 13653Document17 pagesDMCN 13653Dwi ApriyantiNo ratings yet
- Name: Meldred J. Lelis Course/Year: BEED-1: Activity 1: Let's Watch!Document9 pagesName: Meldred J. Lelis Course/Year: BEED-1: Activity 1: Let's Watch!Meldred J. LelisNo ratings yet
- Ultrasound of Congenital Fetal Anomalies: Differential Diagnosis and Prognostic Indicators. Second EditionDocument30 pagesUltrasound of Congenital Fetal Anomalies: Differential Diagnosis and Prognostic Indicators. Second EditionDevanshNo ratings yet
- Care of The Mother and The FetusDocument99 pagesCare of The Mother and The FetusBea Bianca CruzNo ratings yet
- Paracervical BlockDocument4 pagesParacervical BlockpolygoneNo ratings yet
- Joernal AKI Di GambiaDocument9 pagesJoernal AKI Di GambiaUci SelviaNo ratings yet
- ch8 QuizDocument2 pagesch8 QuizsrwcougarNo ratings yet