Professional Documents
Culture Documents
Research Paper
Uploaded by
Hira BanoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Research Paper
Uploaded by
Hira BanoCopyright:
Available Formats
Neural Mobilization in Pregnant Women with Meralgia Paresthetica
Javaid et al.
Original Article
Effects of Neural Mobilization of Lateral Femoral Cutaneous Nerve on
Neuropathic Pain and Quality of Life in Pregnant Women with Meralgia
Paresthetica
Hira Bano Javaid1 , Ayesha Jamil1* , Mutahhar Hussain2 , Fariha Khalid1
1*
University Institute of Physical Therapy, The University of Lahore, Lahore, Pakistan . 2 National Pain
Clinic Orthopedic and Spine, Lahore, Pakistan.
ABSTRACT
Background: Meralgia paraesthetica is a neurological condition characterized by a tingling, prickling, or
burning sensation on the skin of the anterolateral thigh. It is one of the nerve entrapment syndromes in
pregnant females. There is a need for an effective physical therapy management approach to treat this
disabling condition. Objective: To determine the effects of neural mobilization of lateral femoral
cutaneous nerve on neuropathic pain and quality of life in pregnant women with meralgia paresthetica.
Methods: This quasi-experimental study was conducted from January 2022 to January 2023 in the
physical therapy department of the University of Lahore Teaching Hospital, Lahore. By purposive
sampling technique, 30 pregnant women primarily diagnosed with meralgia paraesthetica and a positive
pelvic compression and neurodynamic test, age ranges from 18 to 40 years and body mass index
≥25kg/m2 were included in the study. Those having other entrapment syndromes or radicular
symptoms and motor weakness, having a history or ongoing cancerous proliferation or active
infection were excluded. Lateral femoral cutaneous nerve mobilization in addition to routine
physiotherapy was provided on alternate days, thrice a week for up to two weeks. Neuropathic pain and
quality of life were the outcome variables measured through the neuropathy pain scale and quality of life
short form health survey-36 respectively at baseline, 1st and 2nd week. SPSS version-24 was used for
statistical analysis. Repeated measure analysis of variance was applied for within group difference of
outcome measure. Results: The mean age of participants was 32.82±3.80 years and the body mass index
was 26.62±1.81 kg/m2 . A statistically significant improvement in pain score was observed from a mean of
62.41±10.39 at baseline to 45.95±10.53 in 1st week and to 29.48±10.90 in 2nd week. All domains of short
form-36 were also significantly improved (p≤0.00). Conclusion: It was concluded that lateral femoral
cutaneous nerve mobilization with conventional physiotherapy in pregnant women with meralgia
paresthetica is significantly effective in reducing neuropathic pain and improving quality of life.
*Correspondence: Ayesha Jamil,
Citations: Javaid HB, Jamil A,
The University of Lahore, Lahore,
Hussain M, Khalid F. Effects of
Pakistan.
neural mobilization of lateral
Email: ayeshabutt031@gmail.com
Access femoral cutaneous nerve on
Keywords: Bernhardt Roth
the article neuropathic pain and quality of life
syndrome; lateral femoral cutaneous
online in pregnant women with meralgia
nerve; neural mobilization; meralgia
paresthetica. The Healer Journal of
paresthetica; neuropathic pain;
Physiotherapy and Rehabilitation
quality of life
Sciences. 2023;3(6):560-568.
DOI: 10.55735/hjprs.v3i6.155
Copyright©2023. The Healer Journal of Physiotherapy and Rehabilitation Sciences.
This work is licensed under Creative Commons Attributions 4.0 International license
The Healer Journal | June Issue | Volume 3 - Issue 6 | Pg. 560
Neural Mobilization in Pregnant Women with Meralgia Pare sthe tica
Javaid et al.
INTRODUCTION
Meralgia paresthetica (MP) is a peripheral education is paramount and includes weight
sensory mononeuropathy of the lateral femoral management and avoiding tight clothing,
cutaneous nerve (LFCN), characterized by prolonged static postures and staying
pain, numbness, tingling and burning physically active.11 Medical management
sensation over the anterior and outer part of includes the use of anticonvulsants,
the thigh, results from compression, or nonsteroidal anti-inflammatory medicines,
overstretch of the nerve.1 It can affect any tricyclic antidepressants and injections of a
individual at any stage of life2 and is rare nerve block.5,10 Physiotherapy and manual
outside the pregnancy, having spontaneous therapy modalities12 such as icing, soft tissue
and iatrogenic origin.3 The MP is not a and neural mobilization, muscle energy
sickness that puts a person's life in jeopardy techniques (METs), Kinesio taping13 and
but it can lead to morbidity if it is not detected active release therapy are the common
and treated promptly. Several other methods to relieve the symptoms.14
mechanical elements have the potential to Conservative treatment helps around 85
contribute to elevated levels of pressure within percent of patients to recover within three
the abdominal cavity such as being months, whereas cases that are brought on by
overweight, being pregnant, frequently pregnancy typically get better after the baby is
extending the hip, sitting for lengthy periods, born. However, the surgical approach is only
wearing clothing that is overly constricting, or considered if conservative therapies have
seat belts4 and lithotomy position while failed to produce adequate outcomes, or if the
delivery.5 Orthopaedic treatments, in patient's suffering has reached an intolerable
particular pelvic osteotomies and spine level.15 Nerve or Neural mobilization (NM) is
surgeries are examples of the kinds of prudent to avoid unneeded injury or ischemic
iatrogenic causes that might lead to the compression of the LCFN. Pain relief,
development of MP.6 enhanced muscular endurance and flexibility,
and reduction in neural tension and
During the period of pregnancy, the chances mechanosensitivity are the goals of the NM.16
of entrapment neuropathies increase owing to
changes in the physiological, hormonal, and As it increases the flexibility of
metabolic system and biomechanics of the neuromuscular tissues, and there is an increase
body.7 With the increasing trimester, the in both the axoplasmic and intra-neural blood
weight of the fetus puts additional forces on flow that makes it an effective treatment for
the lower back, pelvic girdle and lower limb, the management of MP.17 Only a small
resulting in musculoskeletal pain8 and number of studies have looked into the effects
compression or overstretch on lumbosacral of therapeutic exercises and manual therapy
plexus and peripheral nerves7 causing techniques on neuropathic pain and quality of
discomforts and impairments. The selection of life in meralgia paresthetica.12,13 Moreover, to
treatment options for neuropathies should be our knowledge, there is no such study
safe considering pregnancy which may result conducted on pregnant females besides the
in symptomatic relief and alleviate the higher incidence of MP during pregnancy.
development of chronic symptoms.9 Therefore, this study aims to determine the
effects of the application of neurodynamics
Treatment of MP typically begins with more nerve mobilization of LFCN with
non-invasive conservative therapy.10 Patient conventional physiotherapy on neuropathic
The Healer Journal | June Issue | Volume 3 - Issue 6 | Pg. 561
Neural Mobilization in Pregnant Women with Meralgia Pare sthe tica
Javaid et al.
pain and quality of life in pregnant women conventional physiotherapy including soft
with MP. tissue release, psoas major stretch, and
strengthening exercises i.e. pelvic stabilization
METHODS and abdominal core exercises along with
LFCN mobilization. Neural mobilization was
This quasi-experimental study was a pre- performed on the patient while they were
posttest design with a single group conducted lying on their side with the affected side
in the outpatient physiotherapy department of facing up and their knee bent to a 90-degree
the University of Lahore Teaching Hospital, angle. The therapist then extended and
The University of Lahore, from January 2022 abducted the patient's hip while performing
to January 2023. The ethical approval was the procedure. The nerve stretch was repeated
taken from the Research Ethics Committee of five times, each time with a hold for 10
the University of Lahore (Ref No: REC-UOL- seconds, followed by a rest for 5 seconds. The
259-11-2022). This study was conducted treatment was given on alternate days, for up
using guidelines of Transparent Reporting of to two weeks.
Evaluations of Nonrandomized Designs
(TRENDS)18 and following the declaration of The total duration of the session was about
Helsinki ethical principles. The participant’s thirty minutes and it was given in the physical
enrolment and allocation are summarized in therapy outpatient department. Neuropathic
Figure 1. pain was measured by neuropathy pain scale
(NPS)20 and for the evaluation of quality of
Before recruiting into the study, informed life; short form-36 questionnaire21 was used.
consent was obtained from participants, and Outcomes measures were recorded at baseline
study objectives were explained to them. It before the start of the intervention and at the
was told that there are no potential risks end of 1st week after 3rd treatment session and
involved, and they have the right to withdraw in 2nd week after the 6th treatment session by
from the study at any point. Anonymity and an independent assessor who was unaware of
confidentiality of data were maintained. A the treatment provided. The data was entered
sample size of 30 was calculated using a and analyzed using SPSS version-24. The
population proportion of 0.4319 , the normality of data was checked by the Shapiro-
anticipated proportion of 0.20, a level of Wilk test. The numerical data like age and
significance α=5%, power of test 1-β= 80% score of NPS were presented in the form of
and a 15% dropout rate. Pregnant women mean and standard deviation. Categorical data
presented with complaints of pain, numbness, like BMI, occupation, parity were presented in
tingling or burning sensation, and diagnosed the form of frequency (percentage). Repeated
with MP in the gynecology outpatient measure analysis of variance (ANOVA) was
department were selected using a purposive used for the comparison of repeated measure
sampling technique. Women of age 18 to 40 analysis of variance within the subjects. The
years, having BMI ≥ 25kg/m2 were included significance of the results was determined by
in the study. Further screened through positive p-value (p<0.05). Intention to treat analysis
pelvic compression and neurodynamic test. was used for missing data.
Those having other entrapment syndromes or
radicular symptoms and motor weakness, RESULTS
having a history or ongoing cancerous
proliferation or active infection were excluded The mean age of the participants was
from the study. The participants were given 32.82±3.80 years and the body mass index
The Healer Journal | June Issue | Volume 3 - Issue 6 | Pg. 562
Neural Mobilization in Pregnant Women with Meralgia Pare sthe tica
Javaid et al.
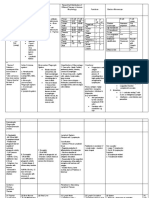
Figure 1: CONSORT Flow Chart
Assessed for Eligibility
(n=50)
Excluded participants (n=20)
Eligibility • Not upto the mark of
inclusion criteria (n=15)
• Refused to take part (n=2)
• Other (n=3)
Non-randomized
Study (n=30)
Allocation
Allocated to group
(n=30)
Received Intervention
(n=30)
Follow up
Lost to Follow-up
(n= 3)
Discontinued
Intervention (n=2)
Analysis
Analysis (n=30)
Intention to Treat
Analysis Applied
(n=5)
The Healer Journal | June Issue | Volume 3 - Issue 6 | Pg. 562
Neural Mobilization in Pregnant Women with Meralgia Pare sthe tica
Javaid et al.
as 26.62±1.81kg/m2 . The socio-demographic on the SF-36 questionnaire from baseline
details and gynecological history of intervention till 2nd week (p≤0.00) using
participants are given in Table 1. The results repeated measure ANOVA (Table 3).
for the neuropathic pain score on NPS showed
that pain was reduced from 62.41± 10.39 at DISCUSSION
the time of recruitment in the study to
29.48±10.90 in 2nd week (p≤0.00). It is also Meralgia Paraesthesia is a sensation of
significant within-group difference was tingling, prickling, or burning of a person's
observed between domains of quality of life skin with no apparent long-term physical
Table 1: Demographics & Gynaecological Details of Study Participants
Characteristics Variable Mean Std. Deviation
Age (in years) 32.82 3.80
Weight (Kgs) 69.90 3.99
Height (cm) 162.12 3.20
Body Mass Index (kg/m2) 26.62 1.81
Frequency Percent
Upper 14 34.1
Socioeconomic status Middle 22 53.7
Lower 5 12.2
Job 20 48.8
Occupation
Housewife 21 51.2
Primi-gravida 7 17.1
Gravida
Multi-gravida 34 82.9
First 10 24.4
Trimester of Pregnancy Second 8 19.5
Third 23 56.1
Yes 11 26.8
History of Episiotomy
No 30 73.2
Previous History of No 32 78
Abortions/ Miscarriage Yes 9 22
The Healer Journal | June Issue | Volume 3 - Issue 6 | Pg. 563
Neural Mobilization in Pregnant Women with Meralgia Pare sthe tica
Javaid et al.
Table 2: Neuropathic Pain Score & Quality at Baseline, 1st and 2nd Week
Background Single Type Single Type of
Pain Score p-value
Neuropathic Pain Pain Always of Pain Time Pain Sometimes
Mean ± SD n (%) n (%) n (%)
Before Treatment 62.41 ±10.394 34 (82.9%) 4 (9.8%) 3 (7.3%)
At 1 st Week 45.95 ±10.537 12 (29.3%) 25 (61.0%) 4 (9.8%) 0.00
At 2 nd Week 29.48 ±10.902 0 (0.0%) 13 (31.7%) 28 (68.3%)
effects. A less common manifestation is improvement in neuropathic pain as well as
formication, the sensation of insects crawling quality of life, which was consistent with the
on or under the skin.9,22 During pregnancy, a findings of our study 13 . Likewise, a study on
woman may experience a variety of physical determining the effects of nerve flossing on
and mental issues, all of which require her to
femoral nerve neuropathy in children with
find solutions to maintain a healthy pregnancy
for both the mother and the unborn child. This hemophilia showed significant improvement
study aims to address the management of in pain scores.23
nerve entrapment neuropathy using nerve
mobilization during pregnancy and the The current study adapted the position of
resulting pain and quality of life. The results neural mobilization in side lying with hip
showed that the neural mobilization of the extension and abduction. A similar study was
lateral femoral cutaneous nerve has proved to conducted on MP patients in which LFCN
have a significant influence on the alleviation neural mobilization and hip flexor self-
of pain, the enhancement of physical and stretching were compared. They concluded
emotional health, and the reduction of limits that hip flexor stretching with a gradual
caused by difficulties of neuropathy to the gluteal muscle strengthening program reduced
body. LFCN neural tension more than neural
mobilization exercises.24 But this study had
MP is relatively a rare condition with less only one participant who was in good health
amount of studies being conducted especially and had no substantial family history or any
medical issues or comorbidities. Furthermore,
with pregnant females and very little research
the exercise position was not suitable for
has been done in the past on how pregnant females, therefore its findings cannot
physiotherapy may be used to treat MP. A be applied to current participants. However,
study on the efficacy of four-week treatment the current study had a few limitations as well,
of exercise therapy and Kinesio taping on such as the control group was not made and
patients with meralgia paresthetica the comparative treatment was not given.
It is recommended that all symptomatic
demonstrated a substantial improvement in the
pregnant females should be referred to
symptoms of meralgia paresthetica as well as
physical therapy for solutions on a physical
the patient's overall quality of life. The
basis without the use of chemical substances.
findings of the outcomes showed an
The Healer Journal | June Issue | Volume 3 - Issue 6 | Pg. 565
Neural Mobilization in Pregnant Women with Meralgia Pare sthe tica
Javaid et al.
Table 3: Quality of Life on SF-36 scale at Baseline, 1st and 2nd Week
Std
Outcome Variable Time of Assessment Mean p-value
Deviation
Before Treatment 41.0976 8.59594
Physical Function At 1st Week 56.8293 8.78038 0.000
At 2nd Week 72.5610 9.21968
Before Treatment 37.7561 5.07336
Role Limitations
Due to Physical At 1st Week 56.9512 4.99976 0.000
Health
At 2nd Week 76.1463 5.24195
Before Treatment 42.9756 8.64722
Role limitations
due to Emotional At 1st Week 61.8049 8.91970 0.000
Problems
At 2nd Week 80.6341 9.45716
Before Treatment 44.7317 8.30971
Energy/Fatigue At 1st Week 49.6829 8.31095 0.000
At 2nd Week 54.6341 8.38974
Before Treatment 48.5122 4.85861
Emotional Well- At 1st Week 51.4878 5.05530 0.000
Being
At 2nd Week 54.4634 5.38097
Before Treatment 50.8537 4.59653
Social Functioning At 1st Week 55.8049 4.66487 0.000
At 2nd Week 60.7561 5.21431
Before Treatment 45.2683 5.54988
Pain At 1st Week 60.3659 5.35143 0.000
At 2nd Week 75.4634 5.50953
Before Treatment 45.4878 7.79783
General Health At 1st Week 53.4878 7.72697 0.000
At 2nd Week 61.4878 7.74636
The Healer Journal | June Issue | Volume 3 - Issue 6 | Pg. 565
Neural Mobilization in Pregnant Women with Meralgia Pare sthe tica
Javaid et al.
Future studies should be conducted with better Review: Update on Presentation,
methodological quality to determine the Pathophysiology, and Treatment. Health
effects of NM on MP treatment. Psychology Research 2023; 11.
5. Zeliha Karaahmet O, Gurcay E, Ozturk
CONCLUSION D, Guzel S, Cakci A. A rare presentation of
meralgia paraesthetica in limb girdle muscular
The findings concluded that neural dystrophy. Scottish Medical Journal 2018;
mobilization techniques in physical therapy in 63(1): 25-7.
pregnant women with meralgia paresthetica 6. Patijn J, Mekhail N, Hayek S, Lataster
were significantly effective in improving A, van Kleef M, Van Zundert J. Meralgia
neuropathic pain quality and level and quality paresthetica. Evidence‐Based Interventional
of life domains including physical function Pain Medicine: According to Clinical
and health, role limitation in physical and Diagnoses 2011: 155-9.
emotional health, pain, social functioning, 7. Ciafaloni E, Thornburg LL, Bushnell
energy, and general health. CD. Neurological Diseases and Pregnancy: A
Coordinated Care Model for Best
DECLARATIONS Management: Oxford University Press; 2018.
8. Aragão FFd. Dor lombossacral
Consent to participate: Written consent had relacionada à gestação. BrJP 2019; 2: 176-81.
been taken from patients. All methods were 9. Gooding MS, Evangelista V, Pereira
performed following the relevant guidelines L. Carpal tunnel syndrome and meralgia
and regulations. paresthetica in pregnancy. Obstetrical &
Availability of data and materials: Data will gynecological survey 2020; 75(2): 121-6.
be available on request. The corresponding 10. Prasetio AD, Hidayati HB. Diagnosis
author will submit all dataset files. and Recent Management of Meralgia
Competing interests: None Paresthetica. Diagnosis and Recent
Funding: No funding source is involved. Management of Meralgia Paresthetica 2022;
Authors' contributions: All authors read and 99(1): 13-.
approved the final manuscript. 11. Sierra-Silvestre E, Bosello F,
Fernández-Carnero J, Hoozemans MJ,
REFERENCES Coppieters MW. Femoral nerve excursion
with knee and neck movements in supine,
1. Cheatham SW, Kolber MJ, Salamh sitting and side-lying slump: an in vivo study
PA. Meralgia paresthetica: a review of the using ultrasound imaging. Musculoskeletal
literature. International journal of sports Science and Practice 2018; 37: 58-63.
physical therapy 2013; 8(6): 883. 12. Skaggs CD, Winchester BA, Vianin
2. Harney D, Patijn J. Meralgia M, Prather H. A manual therapy and exercise
paresthetica: diagnosis and management approach to meralgia paresthetica in
strategies. Pain Medicine 2007; 8(8): 669-77. pregnancy: a case report. Journal of
3. Madiraca Glasnović D, Šlaus N, Šitum chiropractic medicine 2006; 5(3): 92-6.
M, Pećina M. Meralgia paresthetica–lateral 13. Kalichman L, Vered E, Volchek L.
femoral cutaneous nerve entrapment. Rad Relieving symptoms of meralgia paresthetica
Hrvatske akademije znanosti i umjetnosti using Kinesio taping: a pilot study. Archives
Medicinske znanosti 2021; 547(54-55): 56-63. of physical medicine and rehabilitation 2010;
4. de la Caridad Gomez Y, Remotti E, 91(7): 1137-9.
Momah DU, et al. Meralgia Paresthetica
The Healer Journal | June Issue | Volume 3 - Issue 6 | Pg. 566
Neural Mobilization in Pregnant Women with Meralgia Pare sthe tica
Javaid et al.
14. Knapik JJ, Reynolds K, Orr R, Pope R. nonrandomized/quasi-experimental study
Load carriage-related paresthesias (Part 2): designs. JAMA surgery 2021; 156(9): 879-80.
Meralgia paresthetica. Journal of special 19. Van Slobbe A, Bohnen A, Bernsen R,
operations medicine: a peer reviewed journal Koes B, Bierma-Zeinstra S. Incidence rates
for SOF medical professionals 2017; 17(1): and determinants in meralgia paresthetica in
94-100. general practice. Journal of neurology 2004;
15. Schwaiger K, Panzenbeck P, Purschke 251: 294-7.
M, et al. Surgical decompression of the lateral 20. Kim KH, Abdi S. Rediscovery of
femoral cutaneous nerve (LFCN) for Meralgia nefopam for the treatment of neuropathic pain.
paresthetica treatment: Experimental or state The Korean journal of pain 2014; 27(2): 103-
of the art? A single-center outcome analysis. 11.
Medicine 2018; 97(33). 21. Nelson EC, Batalden PB. Patient-
16. Javaid HB, Jamil A, Hussain M, based quality measurement systems. Quality
Khalid F. Effects of Neural Mobilization of Management in Healthcare 1993; 2(1): 18-30.
Lateral Femoral Cutaneous Nerve on 22. Hirsch K, Säemann M, Walter C, et al.
Neuropathic Pain and Quality of Life in Decrease of peripheral resistance after
Pregnant Women with Meralgia Paresthetica: intraoperative administration of iloprost in
Neural Mobilization in Pregnant Women with patients with and without type 2 diabetes
Meralgia Paresthetica. The Healer Journal of mellitus and with peripheral arterial occlusive
Physiotherapy and Rehabilitation Sciences disease. Diabetes and Vascular Disease
2023; 3(6). Research 2020; 17(5): 1479164120930589.
17. Santana HS, Fernandes de Oliveira I, 23. Hamed SA, Zoheiry IM, Waked NM,
Medrado A, Nunes S. Neurodynamic Mahmoud LSE-D. Effect of Neurodynamics
mobilization and peripheral nerve Nerve Flossing on Femoral Neuropathy in
regeneration: A narrative review. Int J Haemophilic Patients: A randomized
Neurorehabilitation 2015; 2(2): 2376- controlled study. Journal of Musculoskeletal
0281.1000163. & Neuronal Interactions 2021; 21(3): 379.
18. Haynes AB, Haukoos JS, Dimick JB. 24. Haddad S. The Effects of Hip Flexor
TREND reporting guidelines for Length on Neural Tension in Meralgia
Paresthetica: Azusa Pacific University; 2019.
The Healer Journal | June Issue | Volume 3 - Issue 6 | Pg. 567
You might also like
- Acquired Brain Injury: An Integrative Neuro-Rehabilitation ApproachFrom EverandAcquired Brain Injury: An Integrative Neuro-Rehabilitation ApproachNo ratings yet
- Dor NeuropaticaDocument6 pagesDor NeuropaticaNélio AraújoNo ratings yet
- Clinical Neurophysiologist - The Comprehensive Guide: Vanguard ProfessionalsFrom EverandClinical Neurophysiologist - The Comprehensive Guide: Vanguard ProfessionalsNo ratings yet
- Relieving Symptoms of Meralgia Paresthetica Using Kinesio Taping - A Pilot StudyDocument3 pagesRelieving Symptoms of Meralgia Paresthetica Using Kinesio Taping - A Pilot StudyAdam MorrellNo ratings yet
- Effect of Spencer Muscle Energy Technique and Proprioceptive Neuromuscular Facilitation in Adhesive CapsulitisDocument6 pagesEffect of Spencer Muscle Energy Technique and Proprioceptive Neuromuscular Facilitation in Adhesive CapsulitisShaik RowfaNo ratings yet
- Journal Homepage: - : IntroductionDocument5 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Nonpharmacologic Management of Pain: Scott F. Nadler, DODocument7 pagesNonpharmacologic Management of Pain: Scott F. Nadler, DOGopi KrishnanNo ratings yet
- Background:: TH ST THDocument6 pagesBackground:: TH ST THRahayu WindariNo ratings yet
- Efficacy of Contra-Lateral Neurodynamics On Median Nerve Extensibility in Cervical Radiculopathy PatientsDocument6 pagesEfficacy of Contra-Lateral Neurodynamics On Median Nerve Extensibility in Cervical Radiculopathy PatientsSylvia Grace100% (1)
- Comparison of Conservative Exercise Therapy With and Without Maitland Thoracic Manipulative Therapy in Patients With Subacromial Pain: Clinical TrialDocument8 pagesComparison of Conservative Exercise Therapy With and Without Maitland Thoracic Manipulative Therapy in Patients With Subacromial Pain: Clinical Trialelchinovichileno420No ratings yet
- PQ Art 37583-10Document7 pagesPQ Art 37583-10Vinay KumarNo ratings yet
- Effects of Adding A Neurodynamic Mobilization To Motor Control Training in Patients With Lumbar Radiculopathy Due To DiscDocument33 pagesEffects of Adding A Neurodynamic Mobilization To Motor Control Training in Patients With Lumbar Radiculopathy Due To Discmarcelogascon.oNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument5 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Effect of NMES Vs Isometric Exercise in OA of Knee-With-Cover-Page-V2 Removed RemovedDocument5 pagesEffect of NMES Vs Isometric Exercise in OA of Knee-With-Cover-Page-V2 Removed RemovedZahra SativaniNo ratings yet
- MEGHA A S Project Ppt-1Document20 pagesMEGHA A S Project Ppt-1Sachin AbsNo ratings yet
- Hes 005 Session 12 SasDocument12 pagesHes 005 Session 12 SasJose Melmar Autida AutenticoNo ratings yet
- Effect of Cervical Lateral Glide Over Neural TissuDocument13 pagesEffect of Cervical Lateral Glide Over Neural TissurobertorodrigoNo ratings yet
- Hes 005 Session 12 SasDocument12 pagesHes 005 Session 12 SasBread PartyNo ratings yet
- A Comparative Study To Determine The Efficacy of Routine Physical Therapy Treatment With and Without Kaltenborn Mobilization On Pain and Shoulder Mobility in Frozen Shoulder PatientsDocument4 pagesA Comparative Study To Determine The Efficacy of Routine Physical Therapy Treatment With and Without Kaltenborn Mobilization On Pain and Shoulder Mobility in Frozen Shoulder Patientsfi.afifah NurNo ratings yet
- Efficacy of Tens Vs PNF in Relieving Acute Cervical Osteoarthritic PainDocument10 pagesEfficacy of Tens Vs PNF in Relieving Acute Cervical Osteoarthritic PainTJPRC PublicationsNo ratings yet
- Paraparesis in Pregnancy: A Rare Presentation: AbstractDocument2 pagesParaparesis in Pregnancy: A Rare Presentation: AbstractVivek KumarNo ratings yet
- Yo MPDocument4 pagesYo MPRo KohnNo ratings yet
- PQ Art 45906-10Document4 pagesPQ Art 45906-10Vinay KumarNo ratings yet
- 1 s2.0 S1413355523000163 MainDocument12 pages1 s2.0 S1413355523000163 Maincarlosso16hotmail.comNo ratings yet
- PNF Ombro 04Document10 pagesPNF Ombro 04Isaias AlmeidaNo ratings yet
- File PDFDocument6 pagesFile PDFJulenda CintarinovaNo ratings yet
- Research Report: G Fryer, J Carub, S MclverDocument7 pagesResearch Report: G Fryer, J Carub, S MclverMitchTolontanNo ratings yet
- Research CPT OngoingDocument2 pagesResearch CPT OngoingYuvraj AtholeNo ratings yet
- Effects of Mobilization, Stretching and Traction in Sports Professionals With Cervical Radiculopathies - For MergeDocument20 pagesEffects of Mobilization, Stretching and Traction in Sports Professionals With Cervical Radiculopathies - For MergeVidya VS100% (1)
- Evidence Based Physiotherapy Management of A Cervical Radiculopathy PatientDocument9 pagesEvidence Based Physiotherapy Management of A Cervical Radiculopathy PatientDr Abdallah BahaaNo ratings yet
- RPG Na Recuperação de Pacientes Com Cervicalgia PDFDocument9 pagesRPG Na Recuperação de Pacientes Com Cervicalgia PDFHildemar ShirataNo ratings yet
- Gharbaoui 10-1055-s-0035-1571255Document6 pagesGharbaoui 10-1055-s-0035-1571255Le Manh ThuongNo ratings yet
- Effectiveness of Core Stabilization Exercises and Routine Exercise Therapy in Management of Pain in Chronic Non-Specific Low Back Pain A Randomized Controlled Clinical Trial PDFDocument5 pagesEffectiveness of Core Stabilization Exercises and Routine Exercise Therapy in Management of Pain in Chronic Non-Specific Low Back Pain A Randomized Controlled Clinical Trial PDFFelipe solis jimenez100% (1)
- Chiropractic & OsteopathyDocument10 pagesChiropractic & OsteopathyjebabalanNo ratings yet
- JPR 11 3151Document10 pagesJPR 11 3151Andani TNo ratings yet
- Ughreja Myofascial ReleaseDocument9 pagesUghreja Myofascial Releasecris.endo.ceNo ratings yet
- Kiiko Matsumotos Clinical StrategiesDocument1 pageKiiko Matsumotos Clinical Strategiestiera0% (1)
- Multidisciplinary Manual Therapy Management of Cervicogenic Headache: A Case ReportDocument9 pagesMultidisciplinary Manual Therapy Management of Cervicogenic Headache: A Case ReportChirag MunjalNo ratings yet
- 2010 - Rehabilitation Procedures in The Management of Spasti PDFDocument17 pages2010 - Rehabilitation Procedures in The Management of Spasti PDFEmmanuel RamosNo ratings yet
- Role of Physio in Neurological Disorders.Document17 pagesRole of Physio in Neurological Disorders.Maheen AnwaarNo ratings yet
- Jurnal Mengurangi Nyeri Meningkatkan Kualitas DepresiDocument6 pagesJurnal Mengurangi Nyeri Meningkatkan Kualitas DepresiPerdanaNo ratings yet
- Effectiveness of Myofascial Release and Muscle Energy Technique On Pectoralis Minor Length in Subjects With Shoulder Impingement Syndrome A Comparative StudyDocument10 pagesEffectiveness of Myofascial Release and Muscle Energy Technique On Pectoralis Minor Length in Subjects With Shoulder Impingement Syndrome A Comparative StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Effect of Lowintensity Laser Acupuncture and Reflexology in Relieving Dysmenorrhea A Randomized Control TrialDocument4 pagesEffect of Lowintensity Laser Acupuncture and Reflexology in Relieving Dysmenorrhea A Randomized Control TrialMohamed Serag El-deinNo ratings yet
- cln63 6p0763Document8 pagescln63 6p0763marcelonorisNo ratings yet
- Preliminary Clinical Evaluation of Acupuncture Therapy in Patients With Postpartum SciaticaDocument7 pagesPreliminary Clinical Evaluation of Acupuncture Therapy in Patients With Postpartum SciaticasemnasNo ratings yet
- Treating Lumbar SpondylosisDocument10 pagesTreating Lumbar SpondylosisDiyya Awaliah Nurhakiimah IbrahimNo ratings yet
- 10 1 1 1021 5805Document14 pages10 1 1 1021 5805echo_10No ratings yet
- Role of Therapeutic Exercises in Neurogenic Thoracic Outlet SyndromeDocument4 pagesRole of Therapeutic Exercises in Neurogenic Thoracic Outlet SyndromeGeraldine Alvarez ANo ratings yet
- # SMWLMDocument9 pages# SMWLMMahmoud Abo AlfaNo ratings yet
- Veterinary Neurologic Rehabilitation The Rationale For ADocument9 pagesVeterinary Neurologic Rehabilitation The Rationale For ACarolina Vargas VélezNo ratings yet
- Manual Physical Therapy, Cervical Traction, and Strengthening Exercises in Patients With Cervical Radiculopathy: A Case SeriesDocument10 pagesManual Physical Therapy, Cervical Traction, and Strengthening Exercises in Patients With Cervical Radiculopathy: A Case SeriesKanwal KhanNo ratings yet
- Case Report: Manual Therapy and Exercise To Improve Outcomes in Patients With Muscle Tension Dysphonia: A Case SeriesDocument12 pagesCase Report: Manual Therapy and Exercise To Improve Outcomes in Patients With Muscle Tension Dysphonia: A Case SeriesNicolas DiaconoNo ratings yet
- Efficacy of Lumbar Mobilization On Postpartum Low Back Pain in Egyptian Females: A Randomized Control TrialDocument12 pagesEfficacy of Lumbar Mobilization On Postpartum Low Back Pain in Egyptian Females: A Randomized Control TrialAlekaNo ratings yet
- Effectiveness of Manual Traction and Other Physiotherapy Treatment in The Management of Painful Cervical RadiculopathyDocument5 pagesEffectiveness of Manual Traction and Other Physiotherapy Treatment in The Management of Painful Cervical RadiculopathyAgus Dwiyana NMNo ratings yet
- Clinical Efficacy of The Mulligan Maneuver For Cervicogenic Headache RCTDocument11 pagesClinical Efficacy of The Mulligan Maneuver For Cervicogenic Headache RCTDavid FehertyNo ratings yet
- Effect of Neural Mobilization Exercises in Patients With Low Back-Related Leg Pain With Peripheral Nerve Sensitization: A Prospective, Controlled TrialDocument11 pagesEffect of Neural Mobilization Exercises in Patients With Low Back-Related Leg Pain With Peripheral Nerve Sensitization: A Prospective, Controlled TrialJaniNo ratings yet
- PNF ConceptDocument8 pagesPNF ConceptSolrac Adle B. SevillaNo ratings yet
- Spinal Cord Stimulation, MILD Procedure, and Regenerative Medicine, Novel Interventional Nonopioid Therapies in Chronic PainDocument7 pagesSpinal Cord Stimulation, MILD Procedure, and Regenerative Medicine, Novel Interventional Nonopioid Therapies in Chronic PainRobert MacedoNo ratings yet
- 166-Article Text-300-1-10-20190603Document4 pages166-Article Text-300-1-10-20190603Achmad JunaidiNo ratings yet
- Subcutaneous Prolotherapy Treatment of Refractory Knee, Shoulder, and Lateral Elbow PainDocument4 pagesSubcutaneous Prolotherapy Treatment of Refractory Knee, Shoulder, and Lateral Elbow PainEsteban J CaletaNo ratings yet
- Human Ear Worksheet PDFDocument3 pagesHuman Ear Worksheet PDFRamisaNo ratings yet
- Chronic Limb Ischaemia: MR Hanif Hussein Consultant Vascular Surgeon, HKLDocument35 pagesChronic Limb Ischaemia: MR Hanif Hussein Consultant Vascular Surgeon, HKLZulzaire ZulkefliNo ratings yet
- HordeolumDocument6 pagesHordeolumDesy SusantiNo ratings yet
- Diarrhoea Patient InformationDocument3 pagesDiarrhoea Patient InformationIgor DemićNo ratings yet
- Existing Restoration - Clinical Status: Secondary Caries Marginal Integrity Biomechanical FormDocument47 pagesExisting Restoration - Clinical Status: Secondary Caries Marginal Integrity Biomechanical FormDaniel WangNo ratings yet
- اسئلة امتحان الفصل الاول حشوات الجذورDocument7 pagesاسئلة امتحان الفصل الاول حشوات الجذورJowan EmadNo ratings yet
- Analisis Lama Waktu Pelayanan Laboratorium Di Rumah Sakit Umum Daerah Pasaman BaratDocument8 pagesAnalisis Lama Waktu Pelayanan Laboratorium Di Rumah Sakit Umum Daerah Pasaman Baratdina filanNo ratings yet
- Ebook John Murtaghs General Practice Companion Handbook PDF Full Chapter PDFDocument67 pagesEbook John Murtaghs General Practice Companion Handbook PDF Full Chapter PDFroberto.duncan209100% (27)
- BGH Case SlipsDocument7 pagesBGH Case SlipsLoungayvan BatuyogNo ratings yet
- The Pediatric Physical Exam:: Who, When, What and Why?Document26 pagesThe Pediatric Physical Exam:: Who, When, What and Why?Carlo Emmanuel SantosNo ratings yet
- Re-Test SUBJECT-English Core Class - Xi Time: 2 Hrs. M.M: 50 General InstructionsDocument8 pagesRe-Test SUBJECT-English Core Class - Xi Time: 2 Hrs. M.M: 50 General InstructionsSunilDwivediNo ratings yet
- Integumentary System: Burns and Wounds Clinical Case Study: Degree Burn Depth in Dermal Layers Description ImageDocument6 pagesIntegumentary System: Burns and Wounds Clinical Case Study: Degree Burn Depth in Dermal Layers Description ImageGabrielitoNo ratings yet
- Antimicrobial Effect of Aqueous Banana Peel Extract, IraqDocument4 pagesAntimicrobial Effect of Aqueous Banana Peel Extract, IraqLilis KhusnulNo ratings yet
- Exercise 2Document6 pagesExercise 2Gwyneth Marie DayaganNo ratings yet
- Case Analysis PediatricsDocument31 pagesCase Analysis PediatricsLYNDLY AGAGEONo ratings yet
- Ontogeny and Phylogeny of Immune SystemDocument3 pagesOntogeny and Phylogeny of Immune SystemPM Basiloy - AloNo ratings yet
- Day 1 - GynacologyDocument204 pagesDay 1 - GynacologyTingting GeNo ratings yet
- Chapter 17 Mood Disorders and SuicideDocument13 pagesChapter 17 Mood Disorders and Suicidemyer pasandalanNo ratings yet
- Product CatalogDocument32 pagesProduct Catalogharshad koyandeNo ratings yet
- BAJADO, Allyssa Mae D. Microbiology 1Document25 pagesBAJADO, Allyssa Mae D. Microbiology 1Hernandez SakuraNo ratings yet
- Liver BiopsyDocument3 pagesLiver BiopsyBiway RegalaNo ratings yet
- Ectopic Pregnancy Nursing Care PlansDocument27 pagesEctopic Pregnancy Nursing Care Plansviper7967880% (20)
- Breast Cancer Mind MapDocument1 pageBreast Cancer Mind Maprjbar arian 69No ratings yet
- 2012 OiteDocument256 pages2012 Oiteaddison wood100% (4)
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument6 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationRenea Joy ArruejoNo ratings yet
- Human Papillomavirus InfectionDocument78 pagesHuman Papillomavirus InfectionJoaquín PeñaNo ratings yet
- Vandana Raut Tata Memorial Centre 31yrsDocument2 pagesVandana Raut Tata Memorial Centre 31yrsvandanaNo ratings yet
- Hepatology Research - 2023 - Yoshiji - Management of Cirrhotic Ascites Seven Step Treatment Protocol Based On The JapaneseDocument12 pagesHepatology Research - 2023 - Yoshiji - Management of Cirrhotic Ascites Seven Step Treatment Protocol Based On The JapaneseSarah FaziraNo ratings yet
- AGAINST COVID Vaccines: Follow Protocol C For at Least 21 Days + Protocol K at The Place of The InjectionDocument11 pagesAGAINST COVID Vaccines: Follow Protocol C For at Least 21 Days + Protocol K at The Place of The Injectionearl-e-birdNo ratings yet
- Nursing Pharmacology Sample Exam QuestionsDocument3 pagesNursing Pharmacology Sample Exam QuestionsDhreambhig Ahrchorphul100% (1)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (32)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (82)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (27)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)