Professional Documents
Culture Documents
Protocolo de Estatus Epileptico
Uploaded by
jiovannaescalanteOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Protocolo de Estatus Epileptico
Uploaded by
jiovannaescalanteCopyright:
Available Formats
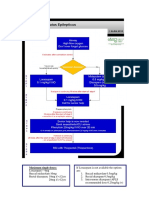
MGH STATUS EPILEPTICUS TREATMENT PROTOCOL
DIAGNOSIS OF STATUS EPILEPTICUS:
1) Generalized convulsive status epilepticus
Continuous convulsive seizure activity lasting > 5 mins
OR, ≥ 2 convulsive seizures without full return to baseline between seizures
2) Non-convulsive status epilepticus (NCSE)
2a) NCSE by strict electrographic criteria (adapted from J Clin Neurophysiol 2005; 22:79-91)
An EEG pattern lasting ≥ 10 secs and satisfying either of the following, qualifies as an electrographic seizure*:
1) Repetitive generalized or focal spikes, sharp-waves, spike-&-wave, or sharp-&-slow wave complexes at ≥3 Hz.
2) Sequential rhythmic, periodic, or quasiperiodic waves at ≥ 1 Hz & unequivocal evolution in frequency
(gradually increases/decreases by ≥ 1 Hz), morphology, or location (gradual spread into or out of a region
involving ≥ two electrodes). Evolution in amplitude alone or in sharpness without other change in morphology
is not enough to satisfy evolution in morphology.
* Intracranial EEG may increase sensitivity of detecting electrographic seizures (AnnNeurol 2014;75(5):771-8).
2b) NCSE by electroclinical or electroradiologic criteria
Rhythmic/periodic EEG activity without evolution and with at least one of the following, qualifies as NCSE:
1) Benzodiazepine trial (see below) demonstrating electrographic or clinical improvement
2) Clear correlation between rhythmic/periodic EEG activity and clinical symptoms
3) CT-PET or MRI neuroimaging showing a pattern of hypermetabolism or diffusion restriction not clinically explained by
another inflammatory or ischemic processes.
Benzodiazepine Trial (adapted from Clin Neurophys 2007;118:1660-1670)
Indication: rhythmic or periodic epileptiform discharges on EEG with concurrent neurological impairment
Monitoring required: EEG, pulse ox, blood pressure, EKG, respiratory rate with dedicated nurse
Give sequential small doses of rapidly acting, short-duration benzodiazepine (e.g., midazolam at 1mg/dose), or a
nonsedating IV anticonvulsant (e.g., levetiracetam, valproic acid, fosphenytoin, or lacosamide). Between doses, repeat
clinical & EEG assessment. Trial is stopped for any of the following:
1) Persistent resolution of the EEG pattern (and examination repeated).
2) Definite clinical improvement.
3) Respiratory depression, hypotension, or other adverse effect.
4) Maximum allowed dose is reached (e.g., 0.2 mg/kg midazolam)
Interpretation: POSITIVE test (i.e., seizure) if the ictal EEG pattern resolves and there is improvement in the patient’s
clinical state and/or appearance of previously absent normal EEG patterns (e.g., return of posterior dominant rhythm).
EQUIVOCAL test if the ictal EEG pattern improves but the patient does not.
TREATMENT OF STATUS EPILEPTICUS:
1) Generalized convulsive status epilepticus: Use protocol on next page
2) Non-convulsive status epilepticus by electrographic, electroclinical, or electroradiologic criteria: No strong evidence to guide
treatment; decision must be made on a case-by-case basis, weighing potential benefits of aggressive treatment (e.g. intubation
and high dose anesthetics) vs potential risks. Benefits: rapid termination of seizures, prevention of seizure-induced secondary
brain injury. Risks: side effects of anesthetics (e.g. hypotension, propofol infusion syndrome), prolonged mechanical ventilation
and ICU course, with attendant risks of infection.
Authors: Alice Lam, MD, PhD; M. Brandon Westover, MD, PhD
Approved by: Eric Rosenthal, MD; Andrew Cole, MD; Sydney Cash, MD, PhD; Daniel Hoch, MD, PhD [Last reviewed: 1/9/2015]
Page 1/2
MGH STATUS EPILEPTICUS TREATMENT PROTOCOL
ANTI-CONVULSANT THERAPY CONCURRENT MANAGEMENT
1st line (seizures ongoing for 5-10 mins) STATUS EPILEPTICUS
1) Airway, Breathing, Circulation
Lorazepam 4mg IV (push over 2mins), 2) Vital signs (cont. monitoring): HR, BP, O2, EKG
If szs not controlled within 5mins, repeat 4mg IV x 1 3) Finger stick blood glucose
If no IV access: If glucose low/unk: give thiamine 100mg IV, then D50 (50mL IV)
Diazepam 20mg rectally (using IV sol’n) 4) Obtain IV access ( ≥2 IVs)
or, Midazolam 10mg intranasal/buccal/IM (using IV sol’n). 5) If febrile, tx w/ anti-pyretics, cooling, consider Abx
6) Labs: CBC, BMP, Ca, Mg, Phos, LFTs, troponin, ABG,
tox screen (blood & urine), blood cxs (esp if febrile),
AED levels (in pts w/ prior hx of epilepsy), HCG (females)
If seizures persist
2nd line (10-30 mins)
Choose from the following (may be used in combination): Check anti-convulsant levels post-load and re-bolus if needed
1) Valproic acid 40mg/kg IV (max rate 6mg/kg/min) (see box below for therapeutic levels):
2) Levetiracetam 20mg/kg IV (max rate 100mg/min) PHT, VPA, PHB - send level 1hr after load
3) Phenobarbital 20mg/kg IV (max rate 50-75mg/min) FOS-PHT - send level 2hrs after load
4) Fosphenytoin 20mg PE/kg IV (max rate 150mg PE/min)
or, Phenytoin 20 mg/kg IV (max rate 25-50mg/min)
If no effect, can give additional dose:
Fosphenytoin 10mg PE/kg IV or Phenytoin 10 mg/kg IV
5) Lacosamide 400mg IV over 5 min (need EKG pre/post)
INTUBATE.
If seizures persist
Start continuous EEG monitoring
3rd line (30 - 60 mins) REFRACTORY STATUS EPILEPTICUS
Choose from the following (may be used in combination): Continue maintenance anticonvulsants and adjust doses for therapeutic
1) Midazolam (good choice if BP unstable) level:
Load 0.2mg/kg IV.
Repeat q5mins until szs stop (max load 2mg/kg) MAINTENANCE DOSES & THERAPEUTIC LEVELS
Maint. infusion 0.1--- 2 mg/kg/hr 1) Valproic acid 30-60 mg/kg/day (BID) 70-120 ug/mL
2) Propofol 2) Levetiracetam 2-4 g/day (BID) 25-60 mg/L
Load 2mg/kg IV. 3) Phenobarbital 1-4mg/kg/day (BID) 20-50 mg/mL
Repeat q5mins until szs stop (max load 10mg/kg) 4) Fosphenytoin 5-7 PE/kg/day (TID) 15-25 ug/mL* (total),
Maint. infusion 1---10mg/kg/hr (< 5 if tx > 48hrs) 1.5-2.5 ug/mL (free)
Titrate infusion to stop seizures or induce burst suppression (currently
or, Phenytoin 5-7 mg/kg/day (TID) ‘‘
no evidence to guide best depth / duration of suppression). 5) Lacosamide 400-600mg/day (BID) Unknown
Use IV fluids and pressors to support BP (anesthetic doses required to tx * Total dilantin level should be corrected for patient’s renal function and albumin:
refractory SE are much higher than doses used for routine sedation). http://www.mdcalc.com/phenytoin-dilantin-correction-for-albumin-or-renal-failure/
If there is signifcant renal dysfunction or hypoalbuminemia, check a free dilantin level.
Once sz-free for >24-48hrs, start slow taper of 3rd line meds over 24hrs,
while maintaining high therapeutic levels of AEDs to avoid recurrent szs.
Continue EEG monitoring until sz-free off 3rd line meds for >24 hrs,
Continue workup to determine underlying cause of SE
to monitor for recurrence of non-convulsive szs or NCSE. 1) Neuroimaging - brain MRI (preferred) or head CT
2) Lumbar puncture - evaluate for infection, inflammatory, autoimmune
causes
4th line (> 72 hrs) SUPER-REFRACTORY STATUS EPILEPTICUS
Choose from the following (may be used in combination):
1) Repeat burst suppression for 24-48hrs
2) Add other AEDs (consider CBZ, TOP, not listed above)
3) IV magnesium (bolus 4g, then infuse 2-6g/hr) Treat underlying cause of status epilepticus.
4) Ketamine
Load w/ 1.5mg/kg IV
Repeat q5mins until szs stop (max load 4.5mg/kg)
Maint. infusion at 1.2-7.5mg/kg/hr
5) Pentobarbital (titrate to burst suppression)
Load 5mg/kg IV (max rate 50mg/min).
Repeat q5mins until szs stop (max load 15mg/kg)
Maint. infusion 1-10 mg/kg/hr
6) IV pyridoxine (200mg/day)
7) Immune modulation
Steroids (methylprednisolone 1g IV qd x 3-5 days)
and/or IVIG (0.4g/kg/day x 5 days)
and/or plasma exchange (every other day x 5-7 days) Authors: Alice Lam, MD, PhD; M. Brandon Westover, MD, PhD,
7) Ketogenic diet Approved by: Eric Rosenthal, MD; Andrew Cole, MD; Sydney Cash, MD,
8) Therapeutic hypothermia PhD; Daniel Hoch, MD, PhD [Last reviewed: 1/9/2015]
9) Electroconvulsive therapy (ECT)
10) Neurosurgical treatment (eg, resection of focal lesion)
11) TMS Page 2/2
No strong evidence to guide best treatment here.
You might also like
- Fast Facts: Optimización del tratamiento de las fluctuaciones motoras en la enfermedad de Parkinson: Adaptando el tratamiento al pacienteFrom EverandFast Facts: Optimización del tratamiento de las fluctuaciones motoras en la enfermedad de Parkinson: Adaptando el tratamiento al pacienteNo ratings yet
- ConnectorDocument4 pagesConnectoryetaung8No ratings yet
- Management of Status Epilepticus 2022Document8 pagesManagement of Status Epilepticus 2022albert siraitNo ratings yet
- Pediatric Status Epilepticus Pathway-FINALDocument5 pagesPediatric Status Epilepticus Pathway-FINALvural kesikNo ratings yet
- 7698alorithm SeizureDocument3 pages7698alorithm Seizureboromeus abyasa daniswara100% (1)
- Acls Patient Algorithms: Greg Cook's Version of A Phoenix Fire DPT ClasicDocument4 pagesAcls Patient Algorithms: Greg Cook's Version of A Phoenix Fire DPT ClasicDouglas Greg CookNo ratings yet
- Evaluation and Management of Status Epilepticus in ChildrenDocument13 pagesEvaluation and Management of Status Epilepticus in ChildrenAyan BiswasNo ratings yet
- Neurology Paediatric ProtocolDocument44 pagesNeurology Paediatric ProtocolkirannesarajahNo ratings yet
- Estatus EpilépticoDocument16 pagesEstatus EpilépticoLizbeth PalomecNo ratings yet
- Penatalaksanaan Kejang Pada Covid19: Suryo Bantolo Rs DcwakDocument21 pagesPenatalaksanaan Kejang Pada Covid19: Suryo Bantolo Rs DcwakWidyadarya Triyono PutriNo ratings yet
- Ventura County Medical Center: Mi Thrombolysis, Management ofDocument3 pagesVentura County Medical Center: Mi Thrombolysis, Management ofblackcat657No ratings yet
- Emergency Viva (Full)Document48 pagesEmergency Viva (Full)ashokarathnasingheNo ratings yet
- Status EpilepticusDocument28 pagesStatus EpilepticusDaniel AlfredNo ratings yet
- TivaDocument35 pagesTivaCharan Pal Singh100% (1)
- CH 8Document12 pagesCH 8Олександр РабошукNo ratings yet
- Epinephrine Dosage and AdministrationDocument9 pagesEpinephrine Dosage and AdministrationTushar GhuleNo ratings yet
- Acls Algorithms 2012Document12 pagesAcls Algorithms 2012Prashanth KumarNo ratings yet
- 1300 Status Epilepticus Guideline NouriDocument2 pages1300 Status Epilepticus Guideline NouriNani BernstorffNo ratings yet
- StatusEpilepticus Pocket CardDocument2 pagesStatusEpilepticus Pocket CardDiana MihaiNo ratings yet
- Thrombolytic TherapyDocument16 pagesThrombolytic TherapyAnonymous nrZXFwNo ratings yet
- StatusDocument14 pagesStatusSyeda HaniaNo ratings yet
- Surgical Adult Critical Care Ref SheetDocument3 pagesSurgical Adult Critical Care Ref Sheetsgod34100% (1)
- Statusepilepticus Pocket CardDocument2 pagesStatusepilepticus Pocket Cardisadora5794No ratings yet
- Animal Models For Antiepileptic Drugs: Dr. Jitendra Agrawal Second Year ResidentDocument41 pagesAnimal Models For Antiepileptic Drugs: Dr. Jitendra Agrawal Second Year ResidentnikuNo ratings yet
- Epinephrine and other emergency drug doses and indicationsDocument5 pagesEpinephrine and other emergency drug doses and indicationsColette Marie PerezNo ratings yet
- Status EpilepsiDocument11 pagesStatus EpilepsiNurul aulia AbdullahNo ratings yet
- NICU Drugs GuideDocument49 pagesNICU Drugs GuideArhanNo ratings yet
- Malignan HipertermiaDocument10 pagesMalignan HipertermiaAstrid Ghea GayatriNo ratings yet
- Eclampsia-Icu Management ProtocolDocument3 pagesEclampsia-Icu Management ProtocolmatentenNo ratings yet
- 3 Combined AHA BLS ACLS Updates CombinedDocument5 pages3 Combined AHA BLS ACLS Updates Combinedamanrup randhawa100% (1)
- COVID MX BsmmuDocument2 pagesCOVID MX BsmmuNuhiat NahreenNo ratings yet
- Status EpilepticusDocument3 pagesStatus EpilepticusVandeosNo ratings yet
- Acls Algorithms 2012Document12 pagesAcls Algorithms 2012kivuNo ratings yet
- Status Epilepticus - APLSDocument3 pagesStatus Epilepticus - APLSMuhammadafif SholehuddinNo ratings yet
- ACLS Book (New)Document23 pagesACLS Book (New)Essa AyazNo ratings yet
- Management Protocol of Septic Shock: DiagnosisDocument3 pagesManagement Protocol of Septic Shock: Diagnosissky nutsNo ratings yet
- ACLS Pocket Guide SummaryDocument5 pagesACLS Pocket Guide Summarydragnu100% (1)
- Severe TBI 2017Document18 pagesSevere TBI 2017DM internaNo ratings yet
- Anaesthetic Considerations For IOMDocument2 pagesAnaesthetic Considerations For IOMTanvir HasanNo ratings yet
- Paediatricshouseofficerguidehospitalkulim 151026150042 Lva1 App6891Document14 pagesPaediatricshouseofficerguidehospitalkulim 151026150042 Lva1 App6891Nadia SalwaniNo ratings yet
- ACLS Medications & ProtocolsDocument4 pagesACLS Medications & ProtocolsRommel OliverasNo ratings yet
- Obat Ayu (Anestesi)Document11 pagesObat Ayu (Anestesi)Ayu PratiwiNo ratings yet
- ACLS Algorithms Adult 2010 Revised May 31 2011Document12 pagesACLS Algorithms Adult 2010 Revised May 31 2011arturschander3614No ratings yet
- Guidelines For Use of Fentanyl (SUBLIMAZE: Chief IndicationsDocument2 pagesGuidelines For Use of Fentanyl (SUBLIMAZE: Chief IndicationssamuelNo ratings yet
- Postoperative Pain Management Doc 7648Document8 pagesPostoperative Pain Management Doc 7648Muthuvigneswaran ChidambaranathanNo ratings yet
- Acute Seizure Management GuideDocument36 pagesAcute Seizure Management GuideontakecilNo ratings yet
- Status Epilepticus and ICPDocument9 pagesStatus Epilepticus and ICPjoomds51No ratings yet
- O&G Off-Tag Assesment Logbook: Traces-Pdf-248732173Document9 pagesO&G Off-Tag Assesment Logbook: Traces-Pdf-248732173niwasNo ratings yet
- Class 1: (0.06-0.08%) : American Society of Anesthesiologist Physical Status ClassificationDocument64 pagesClass 1: (0.06-0.08%) : American Society of Anesthesiologist Physical Status ClassificationNerak LuNo ratings yet
- Febrile SeizureDocument32 pagesFebrile SeizureShiva Valeska ArdhaniswariNo ratings yet
- Sedation of Patients in Intensive Care Unit: 1-Benzodiazepines (BNZS)Document5 pagesSedation of Patients in Intensive Care Unit: 1-Benzodiazepines (BNZS)subvig67% (3)
- Dopamine - IV AdministrationDocument4 pagesDopamine - IV AdministrationAlexandra RainNo ratings yet
- null-1Document60 pagesnull-1tbuyinza21apNo ratings yet
- Dor Sedação EmCritDocument30 pagesDor Sedação EmCritGonçalo MirandaNo ratings yet
- PCCN Clinical Guideline for Status EpilepticusDocument3 pagesPCCN Clinical Guideline for Status EpilepticusAlex GasnasNo ratings yet
- Status Epilepticus and Its Management AssignmentDocument11 pagesStatus Epilepticus and Its Management AssignmentStanley KarugaNo ratings yet
- EVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYFrom EverandEVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYNo ratings yet
- Science: Quarter 1 Module 1: Volcanoes, Earthquakes, and Mountain RangesDocument38 pagesScience: Quarter 1 Module 1: Volcanoes, Earthquakes, and Mountain RangesMaria LayupanNo ratings yet
- Ode To The Spell Checker TCHDocument1 pageOde To The Spell Checker TCHCamila PaulucciNo ratings yet
- 01.shurangama Mantra - 1st VerseDocument1 page01.shurangama Mantra - 1st Versetrung tranNo ratings yet
- Ship Constructor Structure TutorialDocument237 pagesShip Constructor Structure TutorialRodrigo Horta100% (1)
- 515 AMA Must DO QuestionsDocument217 pages515 AMA Must DO QuestionsVenkataRajuNo ratings yet
- The Strange and Beautiful Sorrows of Ava Lavender by Leslye Walton - PrologueDocument10 pagesThe Strange and Beautiful Sorrows of Ava Lavender by Leslye Walton - PrologueWalker BooksNo ratings yet
- KZN OUTER WEST Development ProjectsDocument25 pagesKZN OUTER WEST Development ProjectsDurban Chamber of Commerce and IndustryNo ratings yet
- Dzone Trend Report Containers 2021Document52 pagesDzone Trend Report Containers 2021Diacamo MankungiNo ratings yet
- 03 IoT Technical Sales Training Industrial Wireless Deep DiveDocument35 pages03 IoT Technical Sales Training Industrial Wireless Deep Divechindi.comNo ratings yet
- Bacterial Recombination MCQsDocument3 pagesBacterial Recombination MCQsJon HosmerNo ratings yet
- Access 2013 Beginner Level 1 Adc PDFDocument99 pagesAccess 2013 Beginner Level 1 Adc PDFsanjanNo ratings yet
- Ritangle 2018 QuestionsDocument25 pagesRitangle 2018 QuestionsStormzy 67No ratings yet
- T e 2552731 Describe The Creature Writing Worksheet - Ver - 2Document3 pagesT e 2552731 Describe The Creature Writing Worksheet - Ver - 2Minah ZamanNo ratings yet
- 2018 Nissan Qashqai 111809Document512 pages2018 Nissan Qashqai 111809hectorNo ratings yet
- Maceda Vs Energy Reg BoardDocument4 pagesMaceda Vs Energy Reg BoardJay Mark Esconde100% (1)
- SITXFSA001 - Assessment A - Short Answer - V2-1Document34 pagesSITXFSA001 - Assessment A - Short Answer - V2-1Namwetayeka Richald WanihaNo ratings yet
- MalayoDocument39 pagesMalayoRoxanne Datuin UsonNo ratings yet
- HG532s V100R001C01B016 version notesDocument3 pagesHG532s V100R001C01B016 version notesKhaled AounallahNo ratings yet
- Dividend PolicyDocument16 pagesDividend PolicyJhaden CatudioNo ratings yet
- Conciliar Post Reference GuideDocument9 pagesConciliar Post Reference GuideBenjamin WinterNo ratings yet
- A. Music G8 Fourth QuarterDocument7 pagesA. Music G8 Fourth Quarterjason bernalNo ratings yet
- Far Eastern Shipping Vs CADocument2 pagesFar Eastern Shipping Vs CAAnonymous 5MiN6I78I0No ratings yet
- African Journalof Auditing Accountingand FinanceDocument13 pagesAfrican Journalof Auditing Accountingand FinanceTryl TsNo ratings yet
- Techniques To Prevent Food SpoilageDocument30 pagesTechniques To Prevent Food SpoilageCourtney GrahamNo ratings yet
- Simulation of Spring: Date: Martes, 25 de Agosto de 2020 Designer: Solidworks Study Name: Resorte 1 Analysis TypeDocument10 pagesSimulation of Spring: Date: Martes, 25 de Agosto de 2020 Designer: Solidworks Study Name: Resorte 1 Analysis TypeIván D. ArdilaNo ratings yet
- RVM100 Instruction ManualDocument7 pagesRVM100 Instruction ManualRubénNo ratings yet
- Cyber Crime and Law ClassDocument99 pagesCyber Crime and Law ClassMohd ShifanNo ratings yet
- Icon-Architects Executive Profile - For HealthcareDocument14 pagesIcon-Architects Executive Profile - For HealthcareMuhammad Noshad RizviNo ratings yet
- JAWABAN UTS Bahasa Inggris II Keperawatan Dewi YuniarDocument3 pagesJAWABAN UTS Bahasa Inggris II Keperawatan Dewi Yuniarovan maysandyNo ratings yet
- Medicard Phil Inc. vs. CIRDocument2 pagesMedicard Phil Inc. vs. CIRhigoremso giensdksNo ratings yet