Professional Documents
Culture Documents
Ceftriaxone
Uploaded by
alfredolealcorvoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ceftriaxone
Uploaded by
alfredolealcorvoCopyright:
Available Formats
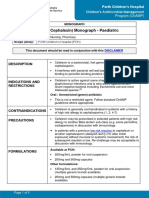
Perth Children’s Hospital
Children’s Antimicrobial Management
Program (ChAMP)
MONOGRAPH
Ceftriaxone Monograph - Paediatric
Scope (Staff): Medical, Pharmacy, Nursing
Scope (Area): All Clinical Areas (Perth Children’s Hospital)
Child Safe Organisation Statement of Commitment
CAHS commits to being a child safe organisation by applying the National Principles for Child Safe
Organisations. This is a commitment to a strong culture supported by robust policies and procedures to
reduce the likelihood of harm to children and young people.
This document should be read in conjunction with this DISCLAIMER
QUICKLINKS
Dosage/Dosage
Administration Compatibility Monitoring
Adjustments
DRUG CLASS
Broad spectrum third generation cephalosporin.(1-3)
INDICATIONS AND RESTRICTIONS
Ceftriaxone is a broad-spectrum cephalosporin with good CSF penetration. It is active against
most community-associated enteric Gram-negative organisms, beta-haemolytic Streptococci and
Streptococcus pneumoniae. It is not active against Enterococci.(1, 2, 4)
For patients admitted to Hospital in the Home (HiTH) from the PCH Emergency Department,
ceftriaxone may be used for cellulitis or lymphadenitis. Refer to HiTH Common Conditions and
Emergency Department Referral Pathways.
Oral: Monitored (orange) antibiotic
• If the use is consistent with a standard approved indication, this must be communicated to
ChAMP by documenting that indication on all prescriptions (inpatient and outpatient).
• The ChAMP team will review if ongoing therapy is required and/or if the order does not meet
ChAMP Standard Indications
• If use is not for a standard approved indication, phone approval must be obtained from
ChAMP before prescribing.
Ceftriaxone Monograph - Paediatric
CONTRAINDICATIONS
• Hypersensitivity to ceftriaxone or any component of the formulation or patients with a history of
high risk allergy to cephalosporins.(1-3)
PRECAUTIONS
• Ceftriaxone may be prescribed in selected patients with high-risk allergy to another Beta-
lactam sub-class (e.g. some penicillins, carbapenems) in discussion with immunology.(1-3)
• Patients with previous low risk reactions to a Beta-lactam (delayed rash >1hr after initial
exposure) without mucosal or systemic involvement) the risk of subsequent reaction to that
agent is low. Re-challenge may be acceptable in discussion with immunology.(3, 5, 6)
• Rapid IV infusion of high doses may result in seizures, especially in patients with renal
impairment.(1, 5)
Neonates less than 44 weeks corrected gestational age:
• Ceftriaxone should be used with extreme caution in neonates less than 41 weeks corrected
gestational age.(2, 3) Cefotaxime is the preferred third-generation cephalosporin in this age
group.(4)
• Ceftriaxone has been associated with fatal systemic calcinosis when used in neonates also
prescribed intravenous calcium containing preparations.(3, 4)
• If ceftriaxone must be used, do NOT administer ceftriaxone and IV calcium containing
products within 48 hours of each other (via the same OR separate infusion lines/sites).(1, 2, 4, 6-8)
• Ceftriaxone is highly protein bound and may displace bilirubin from albumin in neonates,
increasing the risk of bilirubin encephalopathy.(2-4, 6)
Children and infants older than 44 weeks corrected gestational age:
• Ceftriaxone and calcium containing solutions may be administered sequentially (or
concurrently if using separate lines) as long as the lines are flushed well with a compatible
fluid between infusions. (2, 4, 8)
FORMULATIONS
Listed below are products available at PCH, other formulations may be available, check with
pharmacy if required:
• Ceftriaxone 1 g and 2 g vials
Imprest location: Formulary One
DOSAGE & DOSAGE ADJUSTMENTS
Neonates: Refer to Neonatal Medication Protocols
• Ceftriaxone should be avoided in neonates (<44 weeks corrected gestational age). If a third-
generation cephalosporin is required, cefotaxime should be prescribed.
Children (≥ 4 weeks to 18 years):
Treatment - IV or IM:
• Usual dose: 50 mg/kg/dose (to a maximum of 2 grams) given 24 hourly.(1, 4, 7)
Page 2 of 6 Children’s Antimicrobial Management Program (ChAMP) Manual
Ceftriaxone Monograph - Paediatric
• Meningitis or severe sepsis: 50 mg/kg/dose (to a maximum of 2 grams) given 12 hourly OR
100 mg/kg/dose (to a maximum of 4 grams) given 24 hourly.(1, 4, 7).
Post exposure prophylaxis – IV or IM:
Refer to the Medical Prophylaxis ChAMP empiric guidelines for further information on the use
of ceftriaxone for medical prophylaxis.
Meningococcal prophylaxis:
• Children ≥ 4 weeks and < 12 years of age: 125 mg as a single IM dose.(7)
• Children ≥ 12 years of age: 250 mg as a single IM dose.(7)
Haemophilus influenzae type b (Hib) prophylaxis:
• Children ≥ 4 weeks: 50 mg/kg/dose (to a maximum of 1 gram) IM once daily for TWO days.(1, 7)
Post exposure prophylaxis or treatment of confirmed Gonococcal disease:
• Children ≥ 4 weeks: 50 mg/kg (to a maximum of 500 mg) as a single IM dose.(9, 10)
• Dose should be given in conjunction with an oral dose of azithromycin due to the risk of
resistance.(9, 10)
Dosing in Overweight and Obese Children: Dose based on measured body weight.(11)
Renal impairment:
eGFR calculator
• Dose reduction may be required in cases of significant renal impairment with a creatinine
clearance of less than 10mL/minute/1.73m2.(2, 6)
• Maximum recommended daily dose of 50 mg/kg/DAY or 2 grams per day (whichever is less).(2,
3)
Hepatic impairment:
• No dosage adjustment is required in hepatic impairment unless in conjunction with severe
renal impairment.(2, 3)
RECONSTITUTION & ADMINISTRATION
IV reconstitution:
• The below reconstitution recommendations are brand specific. Please consult product
information for alternative brands.
Vial size Volume of water Concentration Powder volume(5)
for injections
1 gram (AFT brand) 9.4 mL 100 mg/mL 0.6 mL
2 gram (AFT) brand 18.9 mL 100 mg/mL 1.1 mL
Page 3 of 6 Children’s Antimicrobial Management Program (ChAMP) Manual
Ceftriaxone Monograph - Paediatric
• Further dilution with a compatible fluid to a final concentration of 40 mg/mL or less is required
prior to administration.(5, 8)
IM reconstitution:
• Reconstitute each 1 gram (AFT brand) vial with 2.3 mL of lidocaine 1% (10 mg/mL) or water
for injection. This results in a final concentration of 350 mg/mL.(5)
• Please consult product information for alternative brands.
• Note: Preparations with lidocaine 1% (10 mg/mL) as diluent must NEVER be given
intravenously.(5, 8, 12)
Intramuscular Injection Procedure
IV infusion (preferred):
• Dilute the required dose to a final concentration of 40 mg/mL or weaker and infuse over 30
minutes.(5, 8)
• In emergency situations or where there is a clinical need (e.g. HiTH) faster infusion times have
been used.(5, 8)
IV push:
Dilute the required dose to a final concentration of 40 mg/mL or weaker and administer as a
push over 5 to 15 minutes.(5, 8)
IM injection:
Maximum recommended single IM dose is 2 grams. For doses higher than 1 gram, the dose
must be split between 2 sites.(5, 8)
Administer up to 1 gram with a maximum concentration of 350 mg/mL via deep injection into
a large muscle mass (ventrogluteal site is preferred).(5)
COMPATIBILITY (LIST IS NOT EXHAUSTIVE)
Compatible fluids:
Sodium chloride 0.9%,
Glucose 5% and 10%
Glucose/sodium chloride solutions
Mannitol 10%(5)
Compatible at Y-site:
Compatibilities of IV drugs must be checked when two or more drugs are given concurrently.
INCOMPATIBLE drugs:
Ceftriaxone is INCOMPATIBLE with calcium containing intravenous solutions including
parenteral nutrition, Ringer’s and Hartmann’s solution because precipitation may occur. (1, 5, 6,
8)
MONITORING
Renal, hepatic, and haematological function should be monitored weekly with prolonged
therapy (i.e. longer than 7 days) and/or with high dose treatment. (1, 3, 6)
Page 4 of 6 Children’s Antimicrobial Management Program (ChAMP) Manual
Ceftriaxone Monograph - Paediatric
ADVERSE EFFECTS
Common: diarrhoea, nausea, vomiting, pain and inflammation at injection site, rash, headache,
dizziness, allergy, Clostridioides difficile-associated disease, abdominal pain, hepatitis, anaemia,
vulvovaginal candidiasis.(1, 6)
Infrequent: anaphylaxis, angioedema.(1, 6)
Rare: neurotoxicity (e.g. confusion, seizures, encephalopathy), blood dyscrasias (e.g.
neutropenia, agranulocytosis), thrombocytopenia, bleeding, renal impairment, pancreatitis,
cholecystitis, pseudolithiasis (reversible biliary sludge formation due to calcium-ceftriaxone
complex), nephrolithiasis (formation of calcium-ceftriaxone renal stones), severe cutaneous
adverse reactions (SCARs), glucosuria, haematuria, oedema.
Immunologic reactions including eosinophilia, drug fever, urticaria, haemolytic anaemia, Stevens-
Johnson syndrome, toxic epidermal necrolysis, interstitial nephritis, arthritis, serum sickness-like
syndrome.(1, 6)
STORAGE
Store vials below 25˚C and protect from light.(5, 8, 12)
Store syringes prepared by Pharmacy Compounding Service (PCS) between 2 and 8˚C.(5)
INTERACTIONS
This medication may interact with other medications; consult PCH approved references (e.g.
Clinical Pharmacology), a clinical pharmacist or PCH Medicines Information Service on extension
63546 for more information.
**Please note: The information contained in this guideline is to assist with the preparation and administration
of ceftriaxone. Any variations to the doses recommended should be clarified with the prescriber prior to
administration**
Related CAHS internal policies, procedures and guidelines
Antimicrobial Stewardship Policy
ChAMP Empiric Guidelines and Monographs
KEMH Neonatal Medication Protocols
Intramuscular (IM) Injections
References
1. Australian Medicines Handbook. Adelaide, S. Aust.: Australian Medicines Handbook; 2023 [cited
2023 2nd May]. Available from: https://amhonline-amh-net-au.pklibresources.health.wa.gov.au/.
2. Clinical Pharmacology powered by ClinicalKey [Internet]. Elsvier. 2023 [cited 2023 August 3rd].
Available from: https://www-clinicalkey-com.pklibresources.health.wa.gov.au/pharmacology/.
3. Up To Date - Paediatric Drug information [Internet]. Lexicomp. 2023 [cited 2023 July 31st].
Available from: https://www-uptodate-com.pklibresources.health.wa.gov.au/contents/table-of-
contents/drug-information/pediatric-drug-information.
Page 5 of 6 Children’s Antimicrobial Management Program (ChAMP) Manual
Ceftriaxone Monograph - Paediatric
4. Antibiotic Writing Group. Therapeutic Guidelines - Antibiotic. West Melbourne: Therapeutic
Guidelines Ltd; 2022. Available from: https://tgldcdp-tg-org-
au.pklibresources.health.wa.gov.au/etgAccess.
5. Symons K. Ermer J. (editors). Australian injectable drugs handbook. Collingwood: The Society of
Hospital Pharmacists of Australia; 2022.
6. Paediatric Formulary Committee. BNF for Children: 2023. London: BMJ Group Pharmaceutical
Press; 2023.
7. Royal Australian College of General Practitioners, Pharmaceutical Society of Australia,
Australasian Society of Clinical and Experimental Pharmacologists and Toxicologists. AMH: Children's
Dosing Companion. Adelaide: Australian Medicines Handbook Pty Ltd; 2022.
8. Pediatric Injectable Drugs. Maryland: American Society of Health -System Pharmacists; 2020.
9. Sexual Health and Blood-borne virus program. Silver book - A guide for managing sexually
transmitted infections. Department of Health - Western Australia; 2020.
10. The Australasian Society for HIV Viral Heaptitis and Sexual Health Medicine. Australian STI
Manegement Guidelines - Gonorrhoea: The Australasian Society for HIV, Viral Heaptitis and Sexual
Health Medicine.; 2023 [Available from: https://sti.guidelines.org.au/sexually-transmissible-
infections/gonorrhoea/.
11. Kendrick JG, Carr RR, Ensom MH. Pediatric Obesity: Pharmacokinetics and Implications for Drug
Dosing. Clin Ther. 2015;37(9):1897-923.
12. MIMS Australia. MIMS online [full product information]. St Leonards, N.S.W: CMP Medica
Australia.; 2022 [cited 2023 21st Mar].
This document can be made available in
alternative formats on request.
File Path: W:\Safety & Quality\CAHS\CLOVERS MEDICAL Pharmacy\Procedures Protocols and
Guidelines\ChAMP\Word
Document Owner: Head of Department – Infectious Diseases
Reviewer / Team: Children’s Antimicrobial Management Program Pharmacist
Date First Issued: April 2013 Last Reviewed: July 2023
Amendment Dates: November 2018; June 2021; July 2023 Next Review Date: July 2026
Approved by: Drugs and Therapeutics Committee Date: August 2023
Endorsed by: Chair, Drugs and Therapeutics Committee Date: August 2023
Aboriginal Impact Statement and Declaration (ISD) Date ISD approved: N/A
Standards
Applicable: NSQHS Standards:
NSMHS: N/A
Child Safe Standards: N/A
Printed or personally saved electronic copies of this document are considered uncontrolled
Page 6 of 6 Children’s Antimicrobial Management Program (ChAMP) Manual
You might also like
- Ceftriaxone Monograph - PaediatricDocument6 pagesCeftriaxone Monograph - PaediatricGheorghe Stefan-SorinNo ratings yet
- CeftriaxoneDocument7 pagesCeftriaxoneGreats HalomoanNo ratings yet
- CiprofloxacinDocument6 pagesCiprofloxacinRasika DaasNo ratings yet
- Cefalexin (Cephalexin) Monograph - Paediatric: DescriptionDocument5 pagesCefalexin (Cephalexin) Monograph - Paediatric: Descriptioneinas omerNo ratings yet
- Azithromycin Monograph - PaediatricDocument7 pagesAzithromycin Monograph - PaediatrictynNo ratings yet
- Gentamicin (Intravenous) Monograph - PaediatricDocument7 pagesGentamicin (Intravenous) Monograph - PaediatrictynNo ratings yet
- FluconazoleDocument5 pagesFluconazoleGreats HalomoanNo ratings yet
- MetronidazoleDocument5 pagesMetronidazoleGwyneth JangadNo ratings yet
- AmoxcillinDocument7 pagesAmoxcillinRoni Sanchez MalanaNo ratings yet
- Enteral InfectionsDocument6 pagesEnteral InfectionsAshley CheungNo ratings yet
- Children's Hospital Co-trimoxazole MonographDocument7 pagesChildren's Hospital Co-trimoxazole MonographKnowledge UshambaNo ratings yet
- Cephalexin Use While BreastfeedingDocument8 pagesCephalexin Use While BreastfeedingTilahun MikiasNo ratings yet
- AciclovirDocument8 pagesAciclovirEphrem LemmaNo ratings yet
- CeftriaxoneaftinjDocument18 pagesCeftriaxoneaftinjbarbawurakNo ratings yet
- Avamys 1Document27 pagesAvamys 1girishtrivediNo ratings yet
- ClarithromycinDocument4 pagesClarithromycinGAYATHIRINo ratings yet
- Intravenous Paracetamol: Safe Anaesthesia Liaison GroupDocument3 pagesIntravenous Paracetamol: Safe Anaesthesia Liaison GroupdenanurbaniazharNo ratings yet
- CeftriaxoneDocument60 pagesCeftriaxoneKazamatsu RyoNo ratings yet
- OFRAMAX 250 (Injection) OFRAMAX 1 G (Injection)Document4 pagesOFRAMAX 250 (Injection) OFRAMAX 1 G (Injection)mahgadNo ratings yet
- Nclex 3 With RationaleDocument13 pagesNclex 3 With RationaleMsPocketbook HoarderNo ratings yet
- Habits Are Some of The Strategies RecommendedDocument30 pagesHabits Are Some of The Strategies Recommendedmd.dascalescu2486No ratings yet
- Ceftriaxoneinj DEVADocument11 pagesCeftriaxoneinj DEVAMuhammad AwaisNo ratings yet
- Drug - Guide - Scavenger - Hunt - Docx 16th EditionDocument5 pagesDrug - Guide - Scavenger - Hunt - Docx 16th EditionYousaf FarookNo ratings yet
- Cefoperazone and Sulbactum Combination Therapy GuideDocument3 pagesCefoperazone and Sulbactum Combination Therapy Guideiloveit52252No ratings yet
- Benzathine BenzylpenicillinDocument6 pagesBenzathine BenzylpenicillinPaskalis HarrisNo ratings yet
- cablivi-epar-product-information_enDocument39 pagescablivi-epar-product-information_enSuh TeixeiraNo ratings yet
- Paracetamol Use GuideDocument13 pagesParacetamol Use GuideShashiprakash KshatriyaNo ratings yet
- CIPROFLOXACIN AND DEXAMETHASONE-ciprofloxacin and Dexamethasone Suspension/ Drops Sandoz IncDocument22 pagesCIPROFLOXACIN AND DEXAMETHASONE-ciprofloxacin and Dexamethasone Suspension/ Drops Sandoz IncnnNo ratings yet
- Alben Daz OleDocument5 pagesAlben Daz OleTariqNo ratings yet
- Summary of Recommendations For Child Teen Immunization: (Age Birth Through 18 Years)Document5 pagesSummary of Recommendations For Child Teen Immunization: (Age Birth Through 18 Years)Annie AnnaNo ratings yet
- Pediatric Malaria Treatment & Management: Approach Considerations, Intensive Care, Deterrence and PreventionDocument4 pagesPediatric Malaria Treatment & Management: Approach Considerations, Intensive Care, Deterrence and PreventionVivi DeviyanaNo ratings yet
- Avamys Epar Product Information enDocument30 pagesAvamys Epar Product Information enGrosir KosmetikNo ratings yet
- What Is The Appendix?: Symptoms of AppendicitisDocument6 pagesWhat Is The Appendix?: Symptoms of AppendicitisVonn Bryan CalumiaNo ratings yet
- Pil 1362Document2 pagesPil 1362noornayab2211No ratings yet
- Con 1420782810247Document7 pagesCon 1420782810247AsetonitrileNo ratings yet
- Calpol Tablets Oral Suspension and Paediatric DropsDocument15 pagesCalpol Tablets Oral Suspension and Paediatric DropsDIWAKAR MISHRANo ratings yet
- MEROPENEM-meropenem Injection, Powder, For S Olution APP Pharmaceuticals, LLCDocument27 pagesMEROPENEM-meropenem Injection, Powder, For S Olution APP Pharmaceuticals, LLCcariocatNo ratings yet
- Ranicef Tablets Cefdinir Tablets 300MG FidsonDocument13 pagesRanicef Tablets Cefdinir Tablets 300MG FidsonWright JohnNo ratings yet
- Ceftin, Zinacef (Cefuroxime) Dosing, Indications, Interactions, Adverse Effects, and More PDFDocument1 pageCeftin, Zinacef (Cefuroxime) Dosing, Indications, Interactions, Adverse Effects, and More PDFMarwa RaeeNo ratings yet
- Accofil Epar Product Information EnDocument155 pagesAccofil Epar Product Information Endora192424No ratings yet
- Calpol Tablets Oral Suspension and Paediatric DropsDocument13 pagesCalpol Tablets Oral Suspension and Paediatric DropsMiscrit ManNo ratings yet
- EMA - Pandemrix® (Vaccin A H1N1 - GSK)Document37 pagesEMA - Pandemrix® (Vaccin A H1N1 - GSK)Tiffany TorresNo ratings yet
- Management of Infection Guidance For Primary Care in IrelandDocument29 pagesManagement of Infection Guidance For Primary Care in IrelandLouise GleesonNo ratings yet
- MIC CefadroxilDocument14 pagesMIC CefadroxilanggiNo ratings yet
- Cefotaxime Drug Class, Uses, Side EffectsDocument3 pagesCefotaxime Drug Class, Uses, Side EffectsKristi WrayNo ratings yet
- Drug InfoDocument11 pagesDrug InfoArjun SinghNo ratings yet
- Taxim-O Dry Syrup: Cefixime Oral Suspension IPDocument7 pagesTaxim-O Dry Syrup: Cefixime Oral Suspension IPJudy AncyNo ratings yet
- IpsaDocument19 pagesIpsaLuisa LopezNo ratings yet
- Guideline 1: Diagnosis of PeritonitisDocument11 pagesGuideline 1: Diagnosis of PeritonitisAnonymous FAyZgchPr6No ratings yet
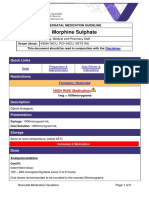
- Morphine SulphateDocument6 pagesMorphine SulphateAdhil LuttooNo ratings yet
- En Web Insert Cefaz NLDocument3 pagesEn Web Insert Cefaz NLAbdul AzizNo ratings yet
- Drug of Treatment For Meningitis: Penicillin Cefotaxime ResistantDocument5 pagesDrug of Treatment For Meningitis: Penicillin Cefotaxime ResistantNama BestNo ratings yet
- Use of Keppra Is Neonatal Seizures at Tygerberg HospitalDocument9 pagesUse of Keppra Is Neonatal Seizures at Tygerberg HospitalKoenaNo ratings yet
- Protocol-012Document17 pagesProtocol-012hatem newishyNo ratings yet
- Student Nurse QuizzesDocument10 pagesStudent Nurse QuizzesElesis samaNo ratings yet
- Extravasations DiagramDocument1 pageExtravasations DiagramJohnNo ratings yet
- FluconazoleDocument4 pagesFluconazoleAyat ElgindyNo ratings yet
- Concise Guide to Clinical Dentistry: Common Prescriptions In Clinical DentistryFrom EverandConcise Guide to Clinical Dentistry: Common Prescriptions In Clinical DentistryNo ratings yet
- NCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!From EverandNCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!Rating: 5 out of 5 stars5/5 (4)
- First Aid KitDocument15 pagesFirst Aid Kitdex adecNo ratings yet
- Types of GastrostomyDocument4 pagesTypes of GastrostomyChad AlsayNo ratings yet
- Emerging Biopharmas Contribution To InnovationDocument60 pagesEmerging Biopharmas Contribution To InnovationGene ParksNo ratings yet
- Use of Misoprostol in Gynecology and Obstetrics 2009Document10 pagesUse of Misoprostol in Gynecology and Obstetrics 2009MemikeMemikeNo ratings yet
- Trademark Final - ChikitDocument9 pagesTrademark Final - ChikitFrances Lipnica PabilaneNo ratings yet
- Interview With A Famous Clandestine LSD Chemist From Hallucinogens - A Forensic Guide'Document2 pagesInterview With A Famous Clandestine LSD Chemist From Hallucinogens - A Forensic Guide'Mahdi_al_Dajjal100% (1)
- Lecture 1 - SolutionsDocument87 pagesLecture 1 - Solutionsapi-3707297100% (8)
- Fifi SpeechDocument2 pagesFifi SpeechDesi NovitaNo ratings yet
- Colloidal Silver Guidebook IDocument28 pagesColloidal Silver Guidebook Iagaia123100% (5)
- Rapid FTIR method for quantification of paracetamol in pharmaceuticalsDocument7 pagesRapid FTIR method for quantification of paracetamol in pharmaceuticalsari twovNo ratings yet
- Drug PDFDocument159 pagesDrug PDFRantyRizkiNo ratings yet
- Sun Pharma Announces Divestment of US Manufacturing Unit (Company Update)Document1 pageSun Pharma Announces Divestment of US Manufacturing Unit (Company Update)Shyam SunderNo ratings yet
- CIA-I 202 - Marketing Management-II Topic List - Sheet1Document2 pagesCIA-I 202 - Marketing Management-II Topic List - Sheet1Akash PawarNo ratings yet
- Atanasov Et Al (2015) Discovery and Resupply of Pharmacologically Active Plant-Derived Natural Product A ReviewDocument33 pagesAtanasov Et Al (2015) Discovery and Resupply of Pharmacologically Active Plant-Derived Natural Product A ReviewGenio Concedo TresdeseosNo ratings yet
- Modified Release Drug Delivery TechnologyDocument1,048 pagesModified Release Drug Delivery Technologyprasad_ram88No ratings yet
- MR Novi UapDocument25 pagesMR Novi UapAuliadi AnsharNo ratings yet
- Evaluation of Pretreatment Analgesia and Endodontic Treatment For Postoperative Endodontic PainDocument4 pagesEvaluation of Pretreatment Analgesia and Endodontic Treatment For Postoperative Endodontic PainRocioNo ratings yet
- Fever with Chills and Rigors: A Case of MalariaDocument19 pagesFever with Chills and Rigors: A Case of MalariaREETHUNo ratings yet
- Glyburide PDFDocument3 pagesGlyburide PDFHannaNo ratings yet
- Immunosuppressive AgentsDocument36 pagesImmunosuppressive AgentsFlorensa Teolina NdruruNo ratings yet
- Quality Manual TemplateDocument34 pagesQuality Manual Templatesakib445100% (3)
- In Vitro and in Vivo Test Methods For The Evaluation of Gastroretentive Dosage FormsDocument29 pagesIn Vitro and in Vivo Test Methods For The Evaluation of Gastroretentive Dosage FormsAnton SikorskyiNo ratings yet
- S License FM-CSVlrd-02 29july2016Document2 pagesS License FM-CSVlrd-02 29july2016Apple Mae Princess RacpanNo ratings yet
- Placebo Studies Ritual TheoryDocument10 pagesPlacebo Studies Ritual Theoryapi-443830029No ratings yet
- Catalogo de Precios Trasnacional 08-06-19Document52 pagesCatalogo de Precios Trasnacional 08-06-19darinelNo ratings yet
- I. Introduction - Basic PharmacologyDocument4 pagesI. Introduction - Basic Pharmacologymdgayas70100% (2)
- Medsyn Lab Biotech Product ListDocument108 pagesMedsyn Lab Biotech Product Listsrivastavadarsh312No ratings yet
- Plan Autopsy Surgeons ReportDocument4 pagesPlan Autopsy Surgeons ReportKristal Macasaet MauhayNo ratings yet
- Ah102 Syllabus 20180417Document7 pagesAh102 Syllabus 20180417api-410716618No ratings yet
- Customer 1Document24 pagesCustomer 1Filan SetiawanNo ratings yet