Professional Documents
Culture Documents
Azithromycin Monograph - Paediatric
Uploaded by
tynOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Azithromycin Monograph - Paediatric
Uploaded by
tynCopyright:
Available Formats
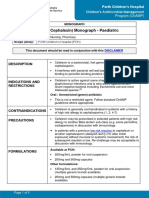
Perth Children’s Hospital
Children’s Antimicrobial Management
Program (ChAMP)
MONOGRAPH
Azithromycin Monograph - Paediatric
Scope (Staff): Medical, Pharmacy, Nursing
Scope (Area): All Clinical Areas
Child Safe Organisation Statement of Commitment
CAHS commits to being a child safe organisation by applying the National Principles for Child Safe
Organisations. This is a commitment to a strong culture supported by robust policies and procedures to
reduce the likelihood of harm to children and young people.
This document should be read in conjunction with this DISCLAIMER
QUICKLINKS
Dosage/Dosage
Administration Compatibility Monitoring
Adjustments
DRUG CLASS
Macrolide antibiotic.(1)
INDICATIONS AND RESTRICTIONS
Azithromycin has a broad spectrum of activity. It is effective against Legionella, Mycoplasma,
Chlamydia, Salmonella, Bordetella pertussis, Rickettsia species, nontuberculous mycobacteria
and some parasites(2)
IV and Oral: Monitored (orange) antibiotic
If the use is consistent with a standard approved indication, this must be communicated to
ChAMP by documenting that indication on all prescriptions (inpatient and outpatient).
The ChAMP team will review if ongoing therapy is required and/or if the order does not meet
ChAMP Standard Indications
If use is not for a standard approved indication, phone approval must be obtained from
ChAMP before prescribing.
Azithromycin Monograph - Paediatric
CONTRAINDICATIONS
Hypersensitivity to azithromycin, erythromycin, macrolide or ketolide antibiotic or any
component of the formulation.(3, 4)
Extended courses of azithromycin should NOT be used in patients undergoing haematopoietic
stem cell transplant (HSCT) for bronchiolitis obliterans (or similar conditions) due to the
increased risk of relapse or death.(4, 5)
PRECAUTIONS
Azithromycin should be used with caution in patients who have hepatic disease. Discontinue
treatment immediately if signs and symptoms of hepatitis and liver dysfunction occur. (6)
Infantile hypertrophic pyloric stenosis is associated with the use of azithromycin in infants, use
with caution in neonates and young infants.(6) The greatest incidence is in the first 2 weeks of
life, reducing after this time with no increase in incidence after 7 weeks of age. (1, 3, 4)
Azithromycin has been shown to prolong the QT interval and should be used with caution in
patients at risk of QT prolongation (including concomitant use of other drugs causing QT
prolongation and cardiac arrhythmias or cardiac insufficiency). For a list of contributing
medications refer to the AMH(1, 3)
Direct sunlight (UV) exposure should be minimised during azithromycin due to possible
photosensitivity reactions.(6)
IV solutions at a concentration of greater than 2mg/mL may result in infusion-site reactions
(pain and local inflammation).(7, 8)
Each 500mg vial of powder for injection contains a minimum of 114mg (4.96mmol) of sodium.
Alternative brands may contain up to 168mg (7.31mmol) of sodium per 500mg vial. Check the
sodium content if the patient is sodium restricted.(7)
Each 200mg/5mL oral suspension contains 3.87grams/5mL of sucrose.(1)
FORMULATIONS
Listed below are products available at PCH, other formulations may be available, check with
pharmacy if required:
200mg/5mL oral suspension for reconstitution 15mL
500mg tablet
500mg powder for injection vial
Imprest location: Formulary One
DOSAGE & DOSAGE ADJUSTMENTS
Neonates: Refer to Neonatal Medication Protocols
Oral:
Bacterial infections (e.g. Mycoplasma pneumonia):
Children ≥ 4 weeks to < 6months:
Not routinely used in children < 6 months of age except in the treatment and prophylaxis of
pertussis or for chlamydia conjunctivitis (see recommended doses below).
Page 2 of 7 Children’s Antimicrobial Management Program (ChAMP) Manual
Azithromycin Monograph - Paediatric
Oral:
Children ≥ 6 months:
10mg/kg/dose (to a maximum of 500mg) once daily. (1, 9)
Indication specific doses:
Indication Age Dose Duration
Pertussis ≥ 4 weeks to 10mg/kg/dose (to a maximum of 500mg) 5 days
(treatment and <6months once daily
prophylaxis)(1, 9)
≥ 6 months 10mg/kg/dose (to a maximum of 500mg) 5 days
daily for one day then reduce to
5mg/kg/dose (to a maximum of 250mg)
daily for a further four days
Tonsilitis or ≥ 4 weeks 12mg/kg/dose (to a maximum of 500mg) 5 days
pharyngitis (high once daily
risk beta lactam
allergy)(2)
Prevention of Children 1-6 10mg/kg/dose (to a maximum of 250mg) Review after
exacerbations in years three times a week(12) 12 months
Cystic fibrosis, or
bronchiectasis(4, 9- Children ≥ 6 250mg as a single dose three times a Review after
11)
years AND 25 week 12 months
to <40kg
Children ≥ 6 500mg as a single dose three times a Review after
years AND week. 12 months
≥40kg
Trachoma and ≥ 4 weeks 20mg/kg/dose (to a maximum of 1gram) Single dose
Chlamydia as a single dose. Repeat doses may be
trachomatis required.
conjunctivitis(1, 9, 13)
Post exposure ≥ 4 weeks 12mg/kg/dose (to a maximum of 500mg) 5 days
prophylaxis - once daily
Invasive Group A
Streptococcal
(iGAS) infection(2)
Empiric therapy ≥ 4 weeks 20mg/kg/dose (to a maximum of 1gram) Single dose
post sexual as a single dose
assault(14)
Refer to the Silver book and/or ChAMP Post exposure
prophylaxis following non-occupational exposure to body
fluids (nPEP) guideline.(14)
Page 3 of 7 Children’s Antimicrobial Management Program (ChAMP) Manual
Azithromycin Monograph - Paediatric
IV:
Usual dose: 10mg/kg/dose (to a maximum of 500mg) once daily.(4, 6) Oral azithromycin therapy is
as effective as IV. Consider switching to oral dosing as soon as clinically appropriate. (2)
Renal impairment:
eGFR calculator (Google Chrome®)
No dosage adjustment is recommended for creatinine clearance greater than 10mL/min. (6)
Azithromycin should be used with caution in patients with severe renal impairment (with
creatinine clearance of less than 10mL/min) due to the increased azithromycin AUC and
Cmax.(2, 6, 10)
Hepatic impairment:
There is limited information available on the use of azithromycin in patients with hepatic
impairment; it appears that no dose adjustments are necessary for mild to moderate
impairment.(3, 6) Azithromycin is not recommended in those with severe hepatic
impairment.(10)
RECONSTITUTION & ADMINISTRATION
Oral:
Reconstitute the azithromycin as per the product information. Tap the bottle until all the
powder flows freely, add the volume of water for reconstitution and shake vigorously to
suspend the powder. Store the reconstituted suspension at less than 30°C and discard any
remaining suspension after 10 days. (3)
Oral tablets and liquid can be administered without regard to food. (3)
IV:
Reconstitute each 500mg vial with 4.8mL water for injection to prepare a 100mg/mL solution.
(7)
Once reconstituted, further dilute to a final concentration of 1mg/mL to 2mg/mL and infuse
over 1 or 3 hours as below.(7)
Doses higher than 500mg should be given over 1 hour.(8)
Concentration Duration of infusion
1mg/mL 3 hours
2mg/mL 1 hours
Please note: infusion durations are correct despite the
unusual recommendation.
The infusion of higher concentrations may result in local infusion site reactions (e.g. pain and local
inflammation).(7)
Page 4 of 7 Children’s Antimicrobial Management Program (ChAMP) Manual
Azithromycin Monograph - Paediatric
COMPATIBILITY (LIST IS NOT EXHAUSTIVE)
Compatible fluids:
Glucose 5%
Hartmann’s
Sodium chloride 0.45% and 0.9%
Glucose/ sodium chloride solutions.(7)
Compatible at Y-site:
Compatibilities of IV drugs must be checked when two or more drugs are given concurrently.
MONITORING
Hepatic and haematological function should be monitored weekly with prolonged therapy at
treatment doses (i.e. longer than 7 days).(4)
For patients on an extended prophylactic course of azithromycin, hepatic (LFT’s) and
haematological (FBC) function should be monitored every three months.(6, 12)
ADVERSE EFFECTS
Common: inflammation and pain at the injection site, nausea, vomiting, diarrhoea, abdominal
pain and cramps, reduced appetite, candida infections, insomnia, pancreatitis. (1, 10)
Infrequent: rash, headache(1, 10)
Rare: hypersensitivity reactions (e.g. anaphylaxis, fixed drug eruptions, Stevens-Johnson
syndrome, interstitial nephritis), psychiatric disturbances, anxiety, ototoxicity (including tinnitus,
dizziness, hearing loss), cholestatic hepatitis, pancreatitis, prolonged QT interval, blood
dyscrasias (e.g. thrombocytopenia), photosensitivity.(1, 6, 10)
Note: Infantile hypertrophic pyloric stenosis is associated with the use of azithromycin in infants.
The greatest incidence is in the first 2 weeks of life, reducing after this time with no increase in
incidence after 7 weeks of age.(1)
STORAGE
Vial: Store below 25°C and protect from light prior to reconstitution.(3, 7)
Oral tablet: Store below 25°C and protect from light and moisture.(3)
Oral powder for suspension: Store dry suspension below 30°C. Once reconstituted, store
the suspension below 30°C. Any suspension remaining after 10 days should be discarded.(3)
INTERACTIONS
This medication may interact with other medications; consult PCH approved references (e.g.
Clinical Pharmacology), a clinical pharmacist or PCH Medicines Information Service on extension
63546 for more information.
**Please note: The information contained in this guideline is to assist with the preparation and administration
of azithromycin. Any variations to the doses recommended should be clarified with the prescriber prior to
administration**
Page 5 of 7 Children’s Antimicrobial Management Program (ChAMP) Manual
Azithromycin Monograph - Paediatric
Related CAHS internal policies, procedures and guidelines
Antimicrobial Stewardship Policy
ChAMP Empiric Guidelines and Monographs
KEMH Neonatal Medication Protocols
References
1. Rossi S, editor. Australian Medicines Handbook. Adelaide, S. Aust.: Australian Medicines
Handbook; 2021.
2. Antibiotic Writing Group. eTG complete. West Melbourne: Therapeutic Guidelines Ltd;
2021. Available from: https://tgldcdp-tg-org-au.pklibresources.health.wa.gov.au/etgAccess.
3. MIMS Australia. MIMS online [full product information]. St Leonards, N.S.W: CMP Medica
Australia.; 2021. p. 1v. (various pagings).
4. Azithromycin Paediatric drug infromation [Internet]. Lexicomp. 2021 [cited 30/06/2021].
5. Increased rate of relapses of haematological malignancies and mortality in haematopoietic
stem cell transplantation (HSCT) patients treated with azithromycin [press release]. Australia:
Pfizer, 12th September 2018.
6. Clinical Pharmacology [Internet]. Elsvier BV. 2021 [cited 8/07/2021]. Available from:
http://www.clinicalpharmacology-ip.com.pklibresources.health.wa.gov.au/default.aspx.
7. Symons K. Ermer J. (editors). Australian injectable drugs handbook. Collingwood: The
Society of Hospital Pharmacists of Australia; 2020.
8. Pediatric Injectable Drugs. Maryland: American Society of Health -System Pharmacists;
2020.
9. Royal Australian College of General Practitioners, Pharmaceutical Society of Australia,
Australasian Society of Clinical and Experimental Pharmacologists and Toxicologists. AMH:
Children's Dosing Companion. Adelaide: Australian Medicines Handbook Pty Ltd; 2020.
10. Paediatric Formulary Committee. BNF for Children: 2020. London: BMJ Group
Pharmaceutical Press; 2021.
11. Management of bronchiectasis in children without cystic fibrosis [Internet]. Lexicomp. 2021
[cited 08/07/2021]. Available from: https://www-uptodate-
com.pklibresources.health.wa.gov.au/contents/management-of-bronchiectasis-in-children-without-
cystic-
fibrosis?search=azithromycin%20bronchiectasis&source=search_result&selectedTitle=3~150&us
age_type=default&display_rank=3#H446347673.
12. Expert Opinion. Infectious Diseases.
13. Committee on Infectious Diseases, editor. Red Book 2018. 31st edition ed. Illinois:
American Academy of Pediatrics; 2018.
14. Sexual Health and Blood-borne virus program. Silver book - A guide for managing sexually
transmitted infections. Department of Health - Western Australia; 2020.
Page 6 of 7 Children’s Antimicrobial Management Program (ChAMP) Manual
Azithromycin Monograph - Paediatric
This document can be made available in
alternative formats on request for a person
with a disability.
File Path: W:\Paediatrics\PMH\ChAMP\Monographs\FINALISED\00 Current version 00
Document Owner: Head of Department – Infectious Diseases
Reviewer / Team: Children’s Antimicrobial Management Program Pharmacist
Date First Issued: April 2013 Last Reviewed: July 2021
Amendment Dates: February 2019, July 2021 Next Review Date: July 2024
Approved by: Drugs and Therapeutics Committee Date: August 2021
Endorsed by: Drugs and Therapeutics Committee, Chair Date: August 2021
Standards
Applicable: NSQHS Standards:
NSMHS: N/A
Child Safe Standards: N/A
Printed or personally saved electronic copies of this document are considered uncontrolled
Page 7 of 7 Children’s Antimicrobial Management Program (ChAMP) Manual
You might also like
- Pharmacy Technician Certification Exam ReviewDocument286 pagesPharmacy Technician Certification Exam ReviewKaren Yuu75% (8)
- NCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!From EverandNCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!Rating: 5 out of 5 stars5/5 (4)
- Prescribing Antibiotics and Analgesics in ChildrenDocument4 pagesPrescribing Antibiotics and Analgesics in ChildrenPreetam PatnalaNo ratings yet
- AntibioticGuidelines PrimaryDocument12 pagesAntibioticGuidelines PrimaryHandriyato SukmaNo ratings yet
- Test Bank For Pharmacy Technician Principles and Practice 3rd Edition HopperDocument24 pagesTest Bank For Pharmacy Technician Principles and Practice 3rd Edition Hopperjenniferhoustonmjcfngpbow100% (42)
- CTD Module 1Document29 pagesCTD Module 1Raju Nalla0% (1)
- Activity Based Costing in Health Care Center PDFDocument6 pagesActivity Based Costing in Health Care Center PDFFreddy VargasNo ratings yet
- Medication Safety PDFDocument95 pagesMedication Safety PDFMangayarkarasi ChandrakasanNo ratings yet
- New Vet Jumpstart Guide: Twenty common general practice cases simplifiedFrom EverandNew Vet Jumpstart Guide: Twenty common general practice cases simplifiedNo ratings yet
- DRUG STUDY: Co-Amoxiclav Antibacterial CombinationDocument6 pagesDRUG STUDY: Co-Amoxiclav Antibacterial CombinationKristine Reyes100% (1)
- Pharmacy Letter of Intent InternshipDocument2 pagesPharmacy Letter of Intent InternshipToia ValentinNo ratings yet
- Rovamycin 3868 DR 1256036243912Document6 pagesRovamycin 3868 DR 1256036243912Ahmed El AlfyNo ratings yet
- Application Form Birthing HomeDocument5 pagesApplication Form Birthing HomeKian AlfrzNo ratings yet
- BPD - DART Regiment DexamethasoneDocument4 pagesBPD - DART Regiment Dexamethasonemarkus_danusantosoNo ratings yet
- AmoxcillinDocument7 pagesAmoxcillinRoni Sanchez MalanaNo ratings yet
- Children's Hospital Co-trimoxazole MonographDocument7 pagesChildren's Hospital Co-trimoxazole MonographKnowledge UshambaNo ratings yet
- Azithromycin NMFv1.0 Full 20180620Document5 pagesAzithromycin NMFv1.0 Full 20180620Lütfiye ÖzlemNo ratings yet
- Ceftriaxone Monograph - PaediatricDocument6 pagesCeftriaxone Monograph - PaediatricGheorghe Stefan-SorinNo ratings yet
- CeftriaxoneDocument6 pagesCeftriaxonealfredolealcorvoNo ratings yet
- Gentamicin (Intravenous) Monograph - PaediatricDocument7 pagesGentamicin (Intravenous) Monograph - PaediatrictynNo ratings yet
- AciclovirDocument8 pagesAciclovirEphrem LemmaNo ratings yet
- FluconazoleDocument5 pagesFluconazoleGreats HalomoanNo ratings yet
- MetronidazoleDocument5 pagesMetronidazoleGwyneth JangadNo ratings yet
- CiprofloxacinDocument6 pagesCiprofloxacinRasika DaasNo ratings yet
- Empiric Antibiotic Guidelines For Paediatric Intensive Care Unit (PICU)Document7 pagesEmpiric Antibiotic Guidelines For Paediatric Intensive Care Unit (PICU)Benny Chris TantoNo ratings yet
- Enteral InfectionsDocument6 pagesEnteral InfectionsAshley CheungNo ratings yet
- Amoxicillin (Amoxycillin) : PresentationDocument4 pagesAmoxicillin (Amoxycillin) : PresentationRavikiran SuryanarayanamurthyNo ratings yet
- ClarithromycinDocument4 pagesClarithromycinGAYATHIRINo ratings yet
- Cefalexin (Cephalexin) Monograph - Paediatric: DescriptionDocument5 pagesCefalexin (Cephalexin) Monograph - Paediatric: Descriptioneinas omerNo ratings yet
- Bacterial Meningitis HSV Encephalitis: Therapeutic Guidelines AntibioticDocument2 pagesBacterial Meningitis HSV Encephalitis: Therapeutic Guidelines AntibioticBetari DhiraNo ratings yet
- Paediatric Protocols Kenya PDFDocument35 pagesPaediatric Protocols Kenya PDFMusab Ahmed HirshiNo ratings yet
- Calpol Tablets Oral Suspension and Paediatric DropsDocument15 pagesCalpol Tablets Oral Suspension and Paediatric DropsAndrew PartridgeNo ratings yet
- Prescribing On The Neonatal Unit Feb2010Document54 pagesPrescribing On The Neonatal Unit Feb2010madimadi11No ratings yet
- Guideline: Antibiotic Drug Monitoring: Aminoglycosides and GlycopeptidesDocument8 pagesGuideline: Antibiotic Drug Monitoring: Aminoglycosides and GlycopeptidesKenRodulfReyesVillaruelNo ratings yet
- Health Conditions Health Conditions Alzheimer's & Dementia Anxiety Arthritis Asthma & Allergies Breast Cancer Cancer Cardiovascular Health COVID-19Document52 pagesHealth Conditions Health Conditions Alzheimer's & Dementia Anxiety Arthritis Asthma & Allergies Breast Cancer Cancer Cardiovascular Health COVID-19BSRT1A BERBANO, IAN JEWEL M.No ratings yet
- Amoxicillin 125 MG 250 MG 5 ML Oral SuspensionDocument16 pagesAmoxicillin 125 MG 250 MG 5 ML Oral SuspensionAshrafNo ratings yet
- Alben Daz OleDocument5 pagesAlben Daz OleTariqNo ratings yet
- K25. Malaria Pada AnakDocument39 pagesK25. Malaria Pada AnakayapillaiNo ratings yet
- Acyclovir (Systemic) - Pediatric Drug Information - UpToDate PDFDocument34 pagesAcyclovir (Systemic) - Pediatric Drug Information - UpToDate PDFAndreea LupuNo ratings yet
- ANTIBIOTIC POLICY FOR Sassoon Hospital & BJGMC, PuneDocument32 pagesANTIBIOTIC POLICY FOR Sassoon Hospital & BJGMC, Puneshah007zaadNo ratings yet
- Icu Antibiotic GuidelinesDocument4 pagesIcu Antibiotic GuidelinesTia MonitaNo ratings yet
- NAG Urinary Tract InfectionsDocument14 pagesNAG Urinary Tract InfectionsJun JimenezNo ratings yet
- Paracetamol - Infusion: Presentation DoseDocument2 pagesParacetamol - Infusion: Presentation Dosecupri yantiNo ratings yet
- Treatment of Tuberculosis .2Document59 pagesTreatment of Tuberculosis .2Alexander Santiago Parel0% (1)
- Paracetamol Package InsertDocument3 pagesParacetamol Package InsertDiane ApostolNo ratings yet
- New Zealand Data Sheet: 1. Product NameDocument15 pagesNew Zealand Data Sheet: 1. Product NameMhd IjlalNo ratings yet
- Paediatric Pam I DR On Ate IV MonographDocument2 pagesPaediatric Pam I DR On Ate IV MonographDouglas MutenyoNo ratings yet
- Cilastati Imipenem Drug InfoDocument19 pagesCilastati Imipenem Drug InfoCosmina GeorgianaNo ratings yet
- CeftriaxoneDocument7 pagesCeftriaxoneGreats HalomoanNo ratings yet
- Leukemia Treatment Regimens 7937Document3 pagesLeukemia Treatment Regimens 7937Irfan FathurrahmanNo ratings yet
- Handbook of Clinical Drug Data 10th Edition Dosage GuideDocument21 pagesHandbook of Clinical Drug Data 10th Edition Dosage GuideYulia Putri CarlianaNo ratings yet
- Analgesia Guidelines PaediatricDocument23 pagesAnalgesia Guidelines PaediatricsyahmiNo ratings yet
- Analgesik/Pire Tik Dosis Sediaan Obat DOA OOA Drug Interaction Paracetamol IVDocument9 pagesAnalgesik/Pire Tik Dosis Sediaan Obat DOA OOA Drug Interaction Paracetamol IVNicole NgoNo ratings yet
- FluconazoleDocument4 pagesFluconazoleeucaNo ratings yet
- Pedoman Penggunaan Antibiotik Pada PasienDocument5 pagesPedoman Penggunaan Antibiotik Pada PasienErvina Lie100% (1)
- Pharmacologic Drug StudyDocument16 pagesPharmacologic Drug StudyBSRT1A BERBANO, IAN JEWEL M.No ratings yet
- GMADocument32 pagesGMABSRT1A BERBANO, IAN JEWEL M.No ratings yet
- Managing Complications of Nephrotic SyndromeDocument6 pagesManaging Complications of Nephrotic SyndromeRagabi RezaNo ratings yet
- Dexamethasone Neomed v2.0Document4 pagesDexamethasone Neomed v2.0dian kurniasariNo ratings yet
- Champ Empiric Antimicrobial Guidelines: Consider Investigation and Treatment For Pertussis And/Or Chlamydia TrachomatisDocument2 pagesChamp Empiric Antimicrobial Guidelines: Consider Investigation and Treatment For Pertussis And/Or Chlamydia TrachomatistynNo ratings yet
- CalculationsDocument4 pagesCalculations869452SalmanNo ratings yet
- MorphineDocument8 pagesMorphineEstherlee ThompsonNo ratings yet
- Paediatric Bone Infection GuideDocument11 pagesPaediatric Bone Infection GuideDorica GiurcaNo ratings yet
- Analgesia Guidelines PaediatricDocument28 pagesAnalgesia Guidelines PaediatricGumarbio Setiadi ZakariaNo ratings yet
- Status AsthmaticusDocument29 pagesStatus AsthmaticusDavid OlsonNo ratings yet
- Medication Fact Sheets: 3rd Edition ContributorsDocument50 pagesMedication Fact Sheets: 3rd Edition ContributorsIndumathi ThangathirupathiNo ratings yet
- Profil Ampicillin SulbactamDocument12 pagesProfil Ampicillin SulbactamasriNo ratings yet
- Champ Empiric Antimicrobial Guidelines: Consider Investigation and Treatment For Pertussis And/Or Chlamydia TrachomatisDocument2 pagesChamp Empiric Antimicrobial Guidelines: Consider Investigation and Treatment For Pertussis And/Or Chlamydia TrachomatistynNo ratings yet
- Gentamicin (Intravenous) Monograph - PaediatricDocument7 pagesGentamicin (Intravenous) Monograph - PaediatrictynNo ratings yet
- Management of North American Pit Viper EnvenomationDocument1 pageManagement of North American Pit Viper EnvenomationtynNo ratings yet
- Beta-Lactam AllergyDocument5 pagesBeta-Lactam AllergytynNo ratings yet
- CCS Drug Infusions v5.0Document95 pagesCCS Drug Infusions v5.0tynNo ratings yet
- MonographsDocument208 pagesMonographstynNo ratings yet
- Fosphenytoin and Phenytoin - Adult/Pediatric - Inpatient Clinical Practice GuidelineDocument15 pagesFosphenytoin and Phenytoin - Adult/Pediatric - Inpatient Clinical Practice GuidelinetynNo ratings yet
- EU and FDA GMP Regulations ComparisonDocument6 pagesEU and FDA GMP Regulations ComparisonTri-Sure More Than ClosuresNo ratings yet
- Guidance For Provision of A Pharmacist Only Medicine LevonorgestrelDocument3 pagesGuidance For Provision of A Pharmacist Only Medicine LevonorgestrelYusri KardoNo ratings yet
- Penggolongan Obat 1Document27 pagesPenggolongan Obat 1Dias Angga PerdanaNo ratings yet
- Pharmacovigilance EnglishDocument4 pagesPharmacovigilance EnglishImmad AlviNo ratings yet
- Data 29 Maret 2021Document201 pagesData 29 Maret 2021debbyNo ratings yet
- April Joyce C. Oaperina ABM 12-B Mariano Que - Founder of Mercury DrugstoreDocument2 pagesApril Joyce C. Oaperina ABM 12-B Mariano Que - Founder of Mercury DrugstoreaprilNo ratings yet
- Error Prone AbbreviationsDocument2 pagesError Prone AbbreviationsNahat IlyetNo ratings yet
- 1.5 Toxicokinetic ModelsDocument27 pages1.5 Toxicokinetic ModelsKattyVilloTaNo ratings yet
- 1803ict Gary Monday4pm Scanlan Jordan s5054901 MajorassignmentDocument8 pages1803ict Gary Monday4pm Scanlan Jordan s5054901 Majorassignmentapi-319771684No ratings yet
- Stavovi Trudnica o SamomedikacijiDocument4 pagesStavovi Trudnica o SamomedikacijiБојана ТркуљаNo ratings yet
- Drug Information Request FormDocument2 pagesDrug Information Request FormAman UpadhyayNo ratings yet
- Health Care in The PhilippinesDocument5 pagesHealth Care in The PhilippinescgaudierNo ratings yet
- Rajeshoswal June 2011Document12 pagesRajeshoswal June 2011Rajesh OswalNo ratings yet
- List 14 07 21Document93 pagesList 14 07 21Herowati WidjajaNo ratings yet
- 9 Mô hình hai ngăn, Không tuyến tính, PKPDDocument45 pages9 Mô hình hai ngăn, Không tuyến tính, PKPDthuong nguyen thiNo ratings yet
- Umesh Pharma 1507821908 - 365Document22 pagesUmesh Pharma 1507821908 - 365Training and PlacementNo ratings yet
- Talib Hashmi's ResumeDocument1 pageTalib Hashmi's ResumeRahul TripathiNo ratings yet
- Tracey Jones (Desertation)Document63 pagesTracey Jones (Desertation)David Abdul KonnehNo ratings yet
- 116 318 1 PBDocument12 pages116 318 1 PBDwi YaniNo ratings yet
- BCS Classification of Some Drugs:: S/No Medicine Strength Solubility Permeability ClassDocument6 pagesBCS Classification of Some Drugs:: S/No Medicine Strength Solubility Permeability Classmuhammad shoaibNo ratings yet
- Guindon-Lesson Plan Drug-Food InteractionsDocument2 pagesGuindon-Lesson Plan Drug-Food InteractionsApril GuindonNo ratings yet
- Customer Relationship Management in The Pharmaceutical IndustryDocument9 pagesCustomer Relationship Management in The Pharmaceutical IndustryUchenna 'Bonex' OgbonnaNo ratings yet
- Adaptive Market Leadership: Epipen Case 2016-2018Document5 pagesAdaptive Market Leadership: Epipen Case 2016-2018Tanvi RastogiNo ratings yet