Professional Documents
Culture Documents
Smileeee 86826468
Uploaded by
Frvrkpop Life0 ratings0% found this document useful (0 votes)
10 views7 pagesMr. Barker had surgery and expected his medical costs would be fully covered under his insurance plan. However, when he received the bill it exceeded his out-of-pocket maximum and included services he thought were covered. He called to ask what he could do and was told he could request the plan review the coverage decision through the appeals process.
Original Description:
infoo
Original Title
Smileeee86826468 - Copy - Copy (2)
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentMr. Barker had surgery and expected his medical costs would be fully covered under his insurance plan. However, when he received the bill it exceeded his out-of-pocket maximum and included services he thought were covered. He called to ask what he could do and was told he could request the plan review the coverage decision through the appeals process.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
10 views7 pagesSmileeee 86826468
Uploaded by
Frvrkpop LifeMr. Barker had surgery and expected his medical costs would be fully covered under his insurance plan. However, when he received the bill it exceeded his out-of-pocket maximum and included services he thought were covered. He called to ask what he could do and was told he could request the plan review the coverage decision through the appeals process.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 7
Mr.
Barker had surgery recently and
expected that he would have certain
services and items covered by the
plan with minimal out-of-pocket costs
because his MA-PD coverage has been
very good. However, when he
received the bill, he was surprised to see
large charges in excess of his maximum
out-of-pocket limit that
included a number of services and items he
thought would be fully covered. He called
you to ask what he could
do? What could you tell him?
You can offer to review the plans appeal
process to help him ask the plan to review
the coverage decision.
Agent Roderick enrolls retiree Mrs.
Martinez in a medical savings account
(MSA) Medicare health plan. The
MSA plan does not offer prescription drug
coverage, so Agent Roderick also enrolls
Mrs. Martinez in a
standalone prescription drug plan (PDP).
What CMS compensation rules apply to
this situation?
This situation is considered a "dual
enrollment," and CMS compensation rules
are
applied to the two plans at once and
independently of each other.
Mr. Singh would like drug coverage, but
does not want to be enrolled into a health
plan. What should you tell
him?
Mr. Singh can enroll in a stand-alone
prescription drug plan and continue to be
covered for Part A and Part B services
through Original Fee-for-Service
Medicare.
ABC is a Medicare Advantage (MA) plan
sponsor. It would like to use its enrollees'
protected health information
to market non-health related products such
as life insurance and annuities. To do so it
must obtain authorization
from the enrollees. Which statement best
describes the authorization process?
Authorization may be obtained by
directing a beneficiary to a website to
provide
consent as long as the website includes a
mechanism for an electronic signature that
is valid under applicable law.
This year you decide to focus your efforts
on marketing to employer and union
groups. Which of the following
statements best describes what you can and
cannot do in order to stay in compliance?
You are not required to submit
communication and marketing materials
specific only
to those employer plans to CMS at the time
of use, but CMS may request and review
copies if employee complaints occur.
During a sales presentation in Ms.
Sullivan's home, she tells you that she has
heard about a type of Medicare
health plan known as Private Fee-for-
Service (PFFS). She wants to know if this
would be available to her.
What should you tell her about PFFS
plans?
A PFFS plan is one of various types of
Medicare Advantage plans offered by
private
entities and she may enroll in one if it is
available in her area.
Mr. Jacob understands that there is a
standard Medicare Part D prescription drug
benefit, but when he looks at
information on various plans available in
his area, he sees a wide range in what they
charge for deductibles,
premiums and cost sharing. How can you
explain this to him?
Medicare Part D drug plans may have
different benefit structures, but on average,
they must all be at least as good as the
standard model established by the
government.
All plans must cover at least the standard
Part D coverage or its actuarial equivalent.
What costs would a
beneficiary incur for prescription drugs in
2019 under the standard coverage?
Standard Part D coverage would require
payment of an annual deductible, 25%
cost-sharing up to the coverage gap, a
portion of costs for both generics and
brandname drugs in the coverage gap, and
co-pays or co-insurance after the coverage
gap.
What types of tools can Medicare Part D
prescription drug plans use that affect the
way their enrollees can
access medications?
Part D plans do not have to cover all
medications. As a result, their formularies,
or
lists of covered drugs, will vary from plan
to plan. In addition, they can use cost
containment techniques such as tiered co-
payments and prior authorization.
You might also like
- Ahip Final Exam Test Questions Latest Version 2022Document32 pagesAhip Final Exam Test Questions Latest Version 2022dmen318j2022No ratings yet
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Summary, Analysis & Review of Philip Moeller’s Get What’s Yours for MedicareFrom EverandSummary, Analysis & Review of Philip Moeller’s Get What’s Yours for MedicareNo ratings yet
- Social Security / Medicare Handbook for Federal Employees and Retirees: All-New 4th EditionFrom EverandSocial Security / Medicare Handbook for Federal Employees and Retirees: All-New 4th EditionNo ratings yet
- Smileeee 86826468Document8 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Maximize Your Medicare (2019 Edition): Understanding Medicare, Protecting Your Health, and Minimizing CostsFrom EverandMaximize Your Medicare (2019 Edition): Understanding Medicare, Protecting Your Health, and Minimizing CostsRating: 5 out of 5 stars5/5 (1)
- Ahip Module 2 (Solved%)Document2 pagesAhip Module 2 (Solved%)WizzardNo ratings yet
- Healthcare Made Easy: Answers to All of Your Healthcare Questions under the Affordable Care ActFrom EverandHealthcare Made Easy: Answers to All of Your Healthcare Questions under the Affordable Care ActNo ratings yet
- Different Types of Medicare Insurance PlanDocument7 pagesDifferent Types of Medicare Insurance PlanGetmy PolicyNo ratings yet
- Textbook of Urgent Care Management: Chapter 22, Health Plan ContractingFrom EverandTextbook of Urgent Care Management: Chapter 22, Health Plan ContractingNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- Medicare Part D DissertationDocument7 pagesMedicare Part D DissertationPayToWritePaperSingapore100% (1)
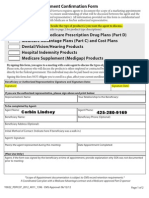
- 2013 Scope of Appointment Form - CORBINDocument2 pages2013 Scope of Appointment Form - CORBINCorbin LindseyNo ratings yet
- Fan Understanding The Insurance ProcessDocument12 pagesFan Understanding The Insurance ProcessWill SackettNo ratings yet
- Scope of Appointment FormDocument2 pagesScope of Appointment Formapi-260208821No ratings yet
- YayooiiDocument7 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- 11522-p Closing The Coverage GapDocument8 pages11522-p Closing The Coverage GapJames LindonNo ratings yet
- This Time Get It Right: Good-Bye ObamaCare: Health Savings Accounts Open the Door to Universal Coverage and Lower CostsFrom EverandThis Time Get It Right: Good-Bye ObamaCare: Health Savings Accounts Open the Door to Universal Coverage and Lower CostsNo ratings yet
- Ahip Module 1Document3 pagesAhip Module 1WizzardNo ratings yet
- Healthcare Reform and You: Key ProvisionsDocument5 pagesHealthcare Reform and You: Key Provisionsapi-252555369No ratings yet
- Health-Care Reform: Insurance Exchanges: Income Solutions Wealth ManangementDocument2 pagesHealth-Care Reform: Insurance Exchanges: Income Solutions Wealth ManangementIncome Solutions Wealth ManagementNo ratings yet
- Medicare Part C Medicare AdvantageDocument3 pagesMedicare Part C Medicare AdvantageJonathan CoutiñoNo ratings yet
- Medicare Private Fee For Service PlansDocument28 pagesMedicare Private Fee For Service PlansMabz BuanNo ratings yet
- Insurance: General Commercial Health Insurance Information 179Document22 pagesInsurance: General Commercial Health Insurance Information 179DeviselvamNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- Medical Billing-Simple ManualDocument17 pagesMedical Billing-Simple ManualKarna Palanivelu80% (25)
- A Guide for Medical Case Managers: Stop Loss Insurance for Medical ProfessionalsFrom EverandA Guide for Medical Case Managers: Stop Loss Insurance for Medical ProfessionalsNo ratings yet
- Eow HC Aca Upheld 062812Document4 pagesEow HC Aca Upheld 062812marshall_johnso6704No ratings yet
- Scope of Appointment Form 2011 UniversalDocument2 pagesScope of Appointment Form 2011 UniversalvmgreekNo ratings yet
- Affordable Care Act Literature ReviewDocument4 pagesAffordable Care Act Literature Reviewdkrnkirif100% (1)
- New Solvency Advocate Walker 17Document4 pagesNew Solvency Advocate Walker 17saifbajwa9038No ratings yet
- The Shifting Landscape of The US Healthcare System Through The ACA and Specific InitiativesDocument3 pagesThe Shifting Landscape of The US Healthcare System Through The ACA and Specific InitiativesPhoebe MwendiaNo ratings yet
- Medicare Term PaperDocument4 pagesMedicare Term Paperafdtzvbex100% (1)
- Research Paper On MedicaidDocument7 pagesResearch Paper On Medicaidafnkhujzxbfnls100% (1)
- Overview of Insurance ScenarioDocument31 pagesOverview of Insurance Scenarionirmal_satNo ratings yet
- Health Insurance Marketplace Notice - Rev 2020Document3 pagesHealth Insurance Marketplace Notice - Rev 2020andre krysaNo ratings yet
- FS PrivateInsuranceDocument2 pagesFS PrivateInsuranceIndiana Family to FamilyNo ratings yet
- The Insider’s Guide to Obamacare’s Open Enrollment (2015-2016)From EverandThe Insider’s Guide to Obamacare’s Open Enrollment (2015-2016)No ratings yet
- If You Are Well: Health and Wellness Tips for the Empowered Health Care ConsumerFrom EverandIf You Are Well: Health and Wellness Tips for the Empowered Health Care ConsumerNo ratings yet
- A Better Medicare. A Better You: MD Medicarechoice, IncDocument19 pagesA Better Medicare. A Better You: MD Medicarechoice, Inclancastd54No ratings yet
- Welcome To Medicare!: Things To Think About When You Compare Medicare Drug CoverageDocument4 pagesWelcome To Medicare!: Things To Think About When You Compare Medicare Drug CoverageAlsayed General HospitalNo ratings yet
- ObamacareintranetDocument3 pagesObamacareintranetapi-157096525No ratings yet
- MD Medicarechoice Florida Optimum MB: Section I - Introduction To The Summary of Benefits ForDocument18 pagesMD Medicarechoice Florida Optimum MB: Section I - Introduction To The Summary of Benefits Forlancastd54No ratings yet
- Medicare Supplement Insurance, Aug 2011Document16 pagesMedicare Supplement Insurance, Aug 2011Jon EnglekingNo ratings yet
- Health Insurance GlossaryDocument13 pagesHealth Insurance GlossaryvivekNo ratings yet
- Obamacare Basics: Understanding The Affordable Care ActDocument3 pagesObamacare Basics: Understanding The Affordable Care ActFindLaw100% (1)
- Medical Billing Terminology and MeaningsDocument7 pagesMedical Billing Terminology and MeaningsMarynaNo ratings yet
- Health Care Reform Act: Critical Tax and Insurance RamificationsFrom EverandHealth Care Reform Act: Critical Tax and Insurance RamificationsNo ratings yet
- YayooiiDocument7 pagesYayooiiFrvrkpop LifeNo ratings yet
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smileeee 86826468Document6 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smile Eee 86826468Document6 pagesSmile Eee 86826468Frvrkpop LifeNo ratings yet
- YayooiiDocument4 pagesYayooiiFrvrkpop LifeNo ratings yet
- Smileeee 86826468Document4 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- YayooiiDocument7 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument7 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument4 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- Patient Census: Francisca Apao Uy Memorial HospitalDocument4 pagesPatient Census: Francisca Apao Uy Memorial HospitalildefonsoNo ratings yet
- Artikel HipertensiDocument7 pagesArtikel HipertensiEdy ZulfiarNo ratings yet
- 2019 Call For Abstract - FETP International Night 2019Document3 pages2019 Call For Abstract - FETP International Night 2019iffakarinaNo ratings yet
- Independent Midwifery PracticeDocument18 pagesIndependent Midwifery Practiceneeta rajesh bhide100% (3)
- Nueva EtiquetaDocument1 pageNueva EtiquetaAnderson Manuel Marquez NuñezNo ratings yet
- Dynamics of Disease TransmissionDocument30 pagesDynamics of Disease TransmissionSyed Sanan shahNo ratings yet
- Supportdoc Pharmacy Reference-GuideDocument2 pagesSupportdoc Pharmacy Reference-GuidePSmNo ratings yet
- Levels of PreventionDocument19 pagesLevels of PreventionKristina JunioNo ratings yet
- Leave Application FormDocument2 pagesLeave Application FormRPh Krishna Chandra Jagrit50% (2)
- Central Directory Individuals BasicDocument3,755 pagesCentral Directory Individuals BasicNaveenJainNo ratings yet
- Multimodal EssayDocument5 pagesMultimodal Essayapi-491425110No ratings yet
- The Historical Background of The Department of Health: JUNE 23, 1898Document3 pagesThe Historical Background of The Department of Health: JUNE 23, 1898Altha Monica Sta MariaNo ratings yet
- Medicare NotesDocument10 pagesMedicare NotesJazmine Royall0% (1)
- National Vision and Strategic Framework For Midwifery - 2022Document18 pagesNational Vision and Strategic Framework For Midwifery - 2022sarfraz.mariyamNo ratings yet
- VSO Our Side of The Story Uganda - Full ReportDocument68 pagesVSO Our Side of The Story Uganda - Full ReportVSONo ratings yet
- Cheat Sheet Series Medicare Part C Medicare AdvantageDocument2 pagesCheat Sheet Series Medicare Part C Medicare AdvantageGirish KaimalNo ratings yet
- SOAL LINK-SMK-BAHASA INGGRIS-Kur2006-UTM-1819Document5 pagesSOAL LINK-SMK-BAHASA INGGRIS-Kur2006-UTM-1819Rosyid KhoirudinNo ratings yet
- Pharmaceutical InnovationDocument348 pagesPharmaceutical Innovationsoreliaac100% (2)
- Kandungan Buku Perinatal Care Manual 4th Edition - 1jun2022Document14 pagesKandungan Buku Perinatal Care Manual 4th Edition - 1jun2022Zarif SyafiqNo ratings yet
- What's Missing GameDocument25 pagesWhat's Missing GameJohn Paolo OcampoNo ratings yet
- Health Survey and Development CommitteeDocument10 pagesHealth Survey and Development CommitteeNidhiNo ratings yet
- Interface Such As A Zoo, Farm or Animal Market.: CarriersDocument3 pagesInterface Such As A Zoo, Farm or Animal Market.: CarriersGuga MamiseishviliNo ratings yet
- Dr. LakshmayyaDocument5 pagesDr. LakshmayyanikhilbNo ratings yet
- Universal Health Coverage in Morocco The Way To Reduce Inequalities ADocument8 pagesUniversal Health Coverage in Morocco The Way To Reduce Inequalities AChaymae SahraouiNo ratings yet
- Managing Change - From Health Policy To Practice (Palgrave 2015) PDFDocument276 pagesManaging Change - From Health Policy To Practice (Palgrave 2015) PDFbrskopjeNo ratings yet
- Org ChartDocument1 pageOrg ChartLia HanafieNo ratings yet
- DCNF Vs Hhs Nov 2020Document302 pagesDCNF Vs Hhs Nov 2020SY LodhiNo ratings yet
- 01-06-12 Comparison US EU Biosimilars RegimesDocument5 pages01-06-12 Comparison US EU Biosimilars RegimesPuneet ChandelNo ratings yet
- Sulfadiazine OralDocument1 pageSulfadiazine OralMariatul KiptiahNo ratings yet
- Why We Need Health Technology Assessment - 230708 - 091544Document8 pagesWhy We Need Health Technology Assessment - 230708 - 091544Nour ElsabahNo ratings yet