Professional Documents
Culture Documents
Yayooii
Uploaded by
Frvrkpop Life0 ratings0% found this document useful (0 votes)
6 views6 pagesMr. Diaz will not pay any penalty for signing up for Part B late as he had continuous employer coverage until age 68.
Mr. Roberts' open enrollment period for a skilled nursing facility will continue for two months after his discharge.
Starting in 2020, the Part B deductible will no longer be covered by Medigap plans for new enrollees.
Mrs. Radford must have Part A and B to enroll in a Medicare Advantage plan.
Medicare will cover Mrs. Shields' skilled nursing services for the first 20 days, then she will pay coinsurance until day 100.
The POS option of some HMOs may allow Mr. Polanski to
Original Description:
infoo
Original Title
Yayooii - Copy (3)
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentMr. Diaz will not pay any penalty for signing up for Part B late as he had continuous employer coverage until age 68.
Mr. Roberts' open enrollment period for a skilled nursing facility will continue for two months after his discharge.
Starting in 2020, the Part B deductible will no longer be covered by Medigap plans for new enrollees.
Mrs. Radford must have Part A and B to enroll in a Medicare Advantage plan.
Medicare will cover Mrs. Shields' skilled nursing services for the first 20 days, then she will pay coinsurance until day 100.
The POS option of some HMOs may allow Mr. Polanski to
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views6 pagesYayooii
Uploaded by
Frvrkpop LifeMr. Diaz will not pay any penalty for signing up for Part B late as he had continuous employer coverage until age 68.
Mr. Roberts' open enrollment period for a skilled nursing facility will continue for two months after his discharge.
Starting in 2020, the Part B deductible will no longer be covered by Medigap plans for new enrollees.
Mrs. Radford must have Part A and B to enroll in a Medicare Advantage plan.
Medicare will cover Mrs. Shields' skilled nursing services for the first 20 days, then she will pay coinsurance until day 100.
The POS option of some HMOs may allow Mr. Polanski to
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 6
Mr.
Diaz continued working with his
company and was insured under his
employer's group plan until he reached
age 68. He has heard that there is a
premium penalty for those who did not
sign up for Part B when first eligible
and wants to know how much he will have
to pay. What should you tell him?
Mr. Diaz will not pay any penalty because
he had continuous coverage under his
employer's plan.
Mr. Roberts is enrolled in an MA plan. He
recently suffered complications following
hip replacement surgery. As
a result, he has spent the last three months
in Resthaven, a skilled nursing facility. Mr.
Roberts is about to be
discharged. What advice would you give
him regarding his health coverage options?
His open enrollment period as an
institutionalized individual will continue
for two
months after the month he moves out of the
facility.
What impact, if any, will the Medicare
Access and CHIP Reauthorization Act of
2015 (MACRA) have upon
Medigap plans?
The Part B deductible will no longer be
covered for individuals newly eligible for
Medicare starting January 1, 2020.
Mrs. Radford asks whether there are any
special eligibility requirements for
Medicare Advantage. What should
you tell her?
. Mrs. Radford must be entitled to Part A
and enrolled in Part B to enroll in Medicare
Advantage
Mrs. Shields is covered by Original
Medicare. She sustained a hip fracture and
is being successfully treated for
that condition. However, she and her
physicians feel that after her lengthy
hospital stay she will need a month
or two of nursing and rehabilitative care.
What should you tell them about Original
Medicare's coverage of care
in a skilled nursing facility?
Medicare will cover Mrs. Shields' skilled
nursing services provided during the first
20
days of her stay, after which she would
have a coinsurance until she has been in
the
facility for 100 days.
Mr. Polanski likes the cost of an HMO plan
available in his area, but would like to be
able to visit one or two
doctors who aren't participating providers.
He wants to know if the Point of Service
(POS) option available with
some HMOs will be of any help in this
situation. What should you tell him?
The POS option might be a good solution
for him as it will allow him to visit out-
ofnetwork providers, generally without
prior approval. However, he should be
aware that
it is likely he will have to pay higher cost-
sharing for services from out-of-network
providers.
Mr. Lopez takes several high cost
prescription drugs. He would like to enroll
in a standalone Part D prescription
drug plan that is available in his area. In
what type of Medicare Health Plan can he
enroll?
Private Fee-for-Service (PFFS) plan that
does not include drug coverage.
Monica is an agent focused on serving
seniors eligible for Medicare. As she
reviews her records, she is trying to
determine which of the following items are
considered compensation. What do you tell
her?
I. Commissions
II. Bonuses
III. Mileage reimbursement
IV. Referral fees
I, II, and IV only
You might also like
- Ahip Module 2 (Solved%)Document2 pagesAhip Module 2 (Solved%)WizzardNo ratings yet
- Social Security / Medicare Handbook for Federal Employees and Retirees: All-New 4th EditionFrom EverandSocial Security / Medicare Handbook for Federal Employees and Retirees: All-New 4th EditionNo ratings yet
- Medicare NotesDocument10 pagesMedicare NotesJazmine Royall0% (1)
- Summary, Analysis & Review of Philip Moeller’s Get What’s Yours for MedicareFrom EverandSummary, Analysis & Review of Philip Moeller’s Get What’s Yours for MedicareNo ratings yet
- Ahip Module 1Document3 pagesAhip Module 1WizzardNo ratings yet
- Ahip Final Exam Test Questions Latest Version 2022Document32 pagesAhip Final Exam Test Questions Latest Version 2022dmen318j2022No ratings yet
- Smileeee 86826468Document8 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- Smileeee 86826468Document7 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- YayooiiDocument7 pagesYayooiiFrvrkpop LifeNo ratings yet
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument7 pagesYayooiiFrvrkpop LifeNo ratings yet
- Smile Eee 86826468Document6 pagesSmile Eee 86826468Frvrkpop LifeNo ratings yet
- Medicare Part C Medicare AdvantageDocument3 pagesMedicare Part C Medicare AdvantageJonathan CoutiñoNo ratings yet
- Different Types of Medicare Insurance PlanDocument7 pagesDifferent Types of Medicare Insurance PlanGetmy PolicyNo ratings yet
- Training Manual (New)Document16 pagesTraining Manual (New)fahhad lashari100% (3)
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- 11522-p Closing The Coverage GapDocument8 pages11522-p Closing The Coverage GapJames LindonNo ratings yet
- How Insurance WorksDocument8 pagesHow Insurance WorksKing4RealNo ratings yet
- Fan Understanding The Insurance ProcessDocument12 pagesFan Understanding The Insurance ProcessWill SackettNo ratings yet
- Gim GimDocument15 pagesGim GimroyjeenaelizabethNo ratings yet
- Health Companion 12 - 2011an-02Document2 pagesHealth Companion 12 - 2011an-02sprashant5No ratings yet
- A Better Medicare. A Better You: MD Medicarechoice, IncDocument19 pagesA Better Medicare. A Better You: MD Medicarechoice, Inclancastd54No ratings yet
- Ba25180st Rev0912 WBDocument6 pagesBa25180st Rev0912 WBJamesMyersNo ratings yet
- YayooiiDocument4 pagesYayooiiFrvrkpop LifeNo ratings yet
- MD Medicarechoice Florida Optimum MB: Section I - Introduction To The Summary of Benefits ForDocument18 pagesMD Medicarechoice Florida Optimum MB: Section I - Introduction To The Summary of Benefits Forlancastd54No ratings yet
- Medicare Part D DissertationDocument7 pagesMedicare Part D DissertationPayToWritePaperSingapore100% (1)
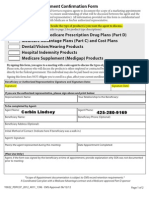
- Scope of Appointment FormDocument2 pagesScope of Appointment Formapi-260208821No ratings yet
- Health Insurance in IndiaDocument7 pagesHealth Insurance in Indianetsavy71No ratings yet
- Obamacare Fact SheetDocument1 pageObamacare Fact Sheetapi-254040217No ratings yet
- Scope of Appointment Form 2011 UniversalDocument2 pagesScope of Appointment Form 2011 UniversalvmgreekNo ratings yet
- Health InsuranceDocument13 pagesHealth InsuranceTroy MirandaNo ratings yet
- Ppo BR MD Pref Sta PR VaDocument16 pagesPpo BR MD Pref Sta PR VaMichael D ReevesNo ratings yet
- Medicare Private Fee For Service PlansDocument28 pagesMedicare Private Fee For Service PlansMabz BuanNo ratings yet
- 2013 Scope of Appointment Form - CORBINDocument2 pages2013 Scope of Appointment Form - CORBINCorbin LindseyNo ratings yet
- Medicare AssignmentDocument13 pagesMedicare AssignmentmivbciwlfNo ratings yet
- Introduction DekaDocument6 pagesIntroduction Dekaidil2023No ratings yet
- CME Beginners Gude Medicare EbookDocument5 pagesCME Beginners Gude Medicare EbookAnonymous qEHjKlXjNo ratings yet
- 2006 Medicare Part D Payments: Total Drug Spend Troop Out of Pocket Cost Portion Covered by MedicareDocument5 pages2006 Medicare Part D Payments: Total Drug Spend Troop Out of Pocket Cost Portion Covered by MedicareVinodh KumarNo ratings yet
- Math - Mental IllnessDocument5 pagesMath - Mental Illnessapi-493788043No ratings yet
- Medicare: Socialsecurity - GovDocument24 pagesMedicare: Socialsecurity - Govtreb trebNo ratings yet
- Summary of Benefits: For Bcbsga Mediblue Access (Ppo)Document44 pagesSummary of Benefits: For Bcbsga Mediblue Access (Ppo)J MillerNo ratings yet
- What Is An HMO Plan?Document8 pagesWhat Is An HMO Plan?fahhad lashariNo ratings yet
- Health Insurance 2Document32 pagesHealth Insurance 2roquiemayursaizNo ratings yet
- #6 The Democratic Voter, February 1, 2012 #6 Small SizeDocument8 pages#6 The Democratic Voter, February 1, 2012 #6 Small Sizedisaacson1No ratings yet
- US HealthcareDocument3 pagesUS HealthcareRaghu TejaNo ratings yet
- Healthcare Reform and You: Key ProvisionsDocument5 pagesHealthcare Reform and You: Key Provisionsapi-252555369No ratings yet
- 2024 Medicare Costs Guide-2Document11 pages2024 Medicare Costs Guide-2Mohammed Ishaq s.mNo ratings yet
- HumanaChoice SNP-DE H5216-267 Summary of BenefitsDocument24 pagesHumanaChoice SNP-DE H5216-267 Summary of Benefitsadela EstradaNo ratings yet
- 10 Facts About Health Insurance You Should Never IgnoreDocument12 pages10 Facts About Health Insurance You Should Never IgnoreKristine ReyesNo ratings yet
- FS PrivateInsuranceDocument2 pagesFS PrivateInsuranceIndiana Family to FamilyNo ratings yet
- Medicare Term PaperDocument4 pagesMedicare Term Paperafdtzvbex100% (1)
- On Health InsuranceDocument33 pagesOn Health InsuranceVenkat Reddy Arrabiri0% (1)
- ESC H BAND FAQsDocument8 pagesESC H BAND FAQsRamesh DeshpandeNo ratings yet
- Eow HC Aca Upheld 062812Document4 pagesEow HC Aca Upheld 062812marshall_johnso6704No ratings yet
- Smileeee 86826468Document7 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smileeee 86826468Document6 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smileeee 86826468Document5 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smileeee 86826468Document4 pagesSmileeee 86826468Frvrkpop LifeNo ratings yet
- Smile Eee 86826468Document6 pagesSmile Eee 86826468Frvrkpop LifeNo ratings yet
- YayooiiDocument4 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument4 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument7 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument7 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- YayooiiDocument6 pagesYayooiiFrvrkpop LifeNo ratings yet
- The Yocum Library Online Database Passwords: All SubjectsDocument3 pagesThe Yocum Library Online Database Passwords: All SubjectsJHSNo ratings yet
- Full Report XeriaDocument11 pagesFull Report XeriaHamierul MohamadNo ratings yet
- Answers 1Document68 pagesAnswers 1Miguel Angel HernandezNo ratings yet
- SimNowUsersManual4 6 1Document271 pagesSimNowUsersManual4 6 1MichelleNo ratings yet
- Sudkabel Garnituren ENGDocument20 pagesSudkabel Garnituren ENGShin Hye ParkNo ratings yet
- Spezia 041510Document11 pagesSpezia 041510Paulo H TavaresNo ratings yet
- Azam in 30 DuaDocument3 pagesAzam in 30 DuafaizaninNo ratings yet
- Helping Slides Pipelining Hazards SolutionsDocument55 pagesHelping Slides Pipelining Hazards SolutionsA NNo ratings yet
- Hotels Review Classification FinalDocument34 pagesHotels Review Classification FinalPurvaNo ratings yet
- SP7 PDFDocument1,025 pagesSP7 PDFkushaljp8989No ratings yet
- CV Achmad AgusDocument11 pagesCV Achmad AgusWoori ConsultingNo ratings yet
- Banking Financial InstitutionsDocument252 pagesBanking Financial Institutionspraise ferrerNo ratings yet
- Ocrsm Assignment 1Document13 pagesOcrsm Assignment 1Vaishnavi LoyaNo ratings yet
- Data Mining ToolsDocument9 pagesData Mining Toolspuneet0303No ratings yet
- The Sniper - Storey PDFDocument177 pagesThe Sniper - Storey PDFJose Luis95% (19)
- Measurement of Hardness of Rubber CompoundsDocument8 pagesMeasurement of Hardness of Rubber CompoundsDarshan VariaNo ratings yet
- Physiology of LactationDocument5 pagesPhysiology of LactationJosephNo ratings yet
- Factura/Invoice: Et 1, Cernavoda, ConstantaDocument1 pageFactura/Invoice: Et 1, Cernavoda, ConstantaMadalina TibaNo ratings yet
- Thesis Statement, Topic Sentence, and Supporting Details: Paul Christian Reforsado AbadDocument29 pagesThesis Statement, Topic Sentence, and Supporting Details: Paul Christian Reforsado AbadMicole BrodethNo ratings yet
- Visualization BenchmarkingDocument15 pagesVisualization BenchmarkingRanjith S100% (1)
- Practical Mix Design of Concrete2Document3 pagesPractical Mix Design of Concrete2Jiabin LiNo ratings yet
- S. P. Rosenbaum (Auth.) - Edwardian Bloomsbury - The Early Literary History of The Bloomsbury Group Volume 2-Palgrave Macmillan UK (1994)Document573 pagesS. P. Rosenbaum (Auth.) - Edwardian Bloomsbury - The Early Literary History of The Bloomsbury Group Volume 2-Palgrave Macmillan UK (1994)HilmiNo ratings yet
- Chap 6 MCQDocument3 pagesChap 6 MCQMahad SheikhNo ratings yet
- Defence10 BookDocument58 pagesDefence10 BookYash ChanneNo ratings yet
- Best Freight Forwarding ERP Software - CargoNet PDFDocument19 pagesBest Freight Forwarding ERP Software - CargoNet PDFGo cargonetNo ratings yet
- Hybrid Solar Chimney With Salt Water Desalination and Power GenerationDocument4 pagesHybrid Solar Chimney With Salt Water Desalination and Power GenerationAishwaryaNo ratings yet
- English Language Unit 1 May 2011Document3 pagesEnglish Language Unit 1 May 2011Kieran RichardsNo ratings yet
- Vaccum FilterationDocument6 pagesVaccum FilterationAkshay bhuranNo ratings yet
- Synthesis of Sufanilic AcidDocument4 pagesSynthesis of Sufanilic AcidWinston Jake Gerolaga0% (1)
- Hw-n300 ZP Fullmanual 00 Eng Spa 180713Document62 pagesHw-n300 ZP Fullmanual 00 Eng Spa 180713NIVARDO ÑAUPA MOROCCONo ratings yet