Professional Documents
Culture Documents
IM JobAids 2005 06eng
IM JobAids 2005 06eng
Uploaded by
Aubrey PerezCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
IM JobAids 2005 06eng
IM JobAids 2005 06eng
Uploaded by
Aubrey PerezCopyright:
Available Formats
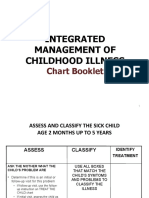
The Integrated Management of Childhood Illness (IMCI) for Diarrhea as seen with Rotavirus Disease
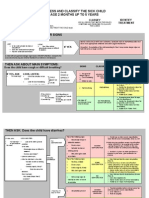
ASSESS ALL SICK CHILDREN AND SICK YOUNG INFANTS. Table 1. Classification Table for Dehydration
1. For ALL sick children ask the mother about the child’s problem IDENTIFY TREATMENT
SIGNS CLASSIFY AS
(Urgent pre-referral treatments are in bold print)
ASK: ► If child has no other severe classification:
Is the child able to drink or
breastfeed? Two of the following signs: - Give fluid for severe dehydration (Plan C below)
General Danger Signs →
2. For ALL sick children • Lethargic or unconscious OR
ASK If child also has another severe classification:
ask the mother about A child with any general danger Does the child vomit • Sunken eyes
the child’s problem, then sign needs URGENT attention; • Not able to drink or SEVERE - Refer URGENTLY to hospital with mother giving frequent
everything? DEHYDRATION
complete the assessment drinking poorly sips of ORS* on the way.
CHECK FOR GENERAL and any pre-referral treatment ASK: • Skin pinch goes back very Advise the mother to continue breastfeeding
DANGER SIGNS immediately so referral is not Has the child had convulsions?
slowly ► If child is 2 years or older and there is cholera in your area,
delayed LOOK
To see if the child is lethargic or give antibiotic for cholera
unconscious ► Give fluid and food for some dehydration (Plan B below):
Two of the following signs: - Give fluid for severe dehydration (Plan C below)
3. For ALL sick children ask the mother about the child’s problem, check for general danger • Restless, irritable ► If child also has a severe classification:
signs, and then ASK about cough or difficulty breathing
• Sunken eyes SOME - Refer URGENTLY to hospital with mother giving frequent
ASK • Drinks eagerly, thirsty DEHYDRATION sips of ORS* on the way.
• For how long? • Skin pinch goes back Advise the mother to continue breastfeeding
• Is there blood in the stool? slowly ► Advise mother when to return immediately
LOOK, LISTEN, FEEL ► Follow-up in 5 days if not improving
• Look at the child’s general condition. Is the child: ► Give fluid and food to treat diarrheoa at home (Plan A below)
→ Lethargic or unconscious? Not enough signs to classify as NO
4. For ALL sick children ► Advise mother when to return immediately
ask the mother about → Restless or irritable? some or severe dehydration DEHYDRATION ► Follow-up in 5 days if not improving
the child’s problem, • Look for sunken eyes
check for general • Offer the child fluid. Is the child:
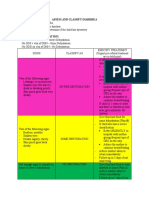
danger signs, ask → Not able to drink or drinking poorly? Table 2. Extra Fluid for Diarrhea and Continued Feeding
about cough or difficulty → Drinking eagerly, thirsty? To treat a child who has diarrhea and NO DEHYDRATION
breathing, and then • Pinch the skin of the abdomen. Does it go back:
→ Very slowly (longer than 2 seconds)? ► Give extra fluid:
ASK: Does the child
have diarrhea? → Slowly? - Give more fluid as usual as soon as diarrhea starts
→ Immediately? - Breastfeed frequently and longer at each feeding
PLAN A:
If yes - If exclusively breastfed, child should be breastfed more frequently than usual
CLASSIFY the child’s illness using the classification table for Treat diarrhea
see right - Teach mother how to mix ORS*
diarrhea and dehydration (Table 1 at right) at home
• If the child has had diarrhea for 14 days or more, classify - Show mother how much fluid to give in addition to usual fluid intake
the child for persistent diarrhea ► Continue feeding
• If the child has blood in the stool, classify the child for ► Return to health center if child is not able to drink or breasfeed, becomes sicker, develops a
dysentery fever. If the child has diarrhea, return if she has blood in stool or is not able to drink or breastfeed
IDENTIFY TREATMENT (Table 2 at right) To treat a child who has diarrhea and SOME DEHYDRATION
PLAN B: (includes an initial treatment of 4 hours in the clinic)
5. For ALL sick children ask the mother about the child’s problem, check for general danger
signs, ask about cough or difficulty breathing, diarrhea and then ask for fever. Treat some ► Determine the amoung of ORS* to give during the first 4 hours
dehydration with ► Show the mother how to give ORS* solution
6. For ALL sick children ask the mother about the child’s problem, check for general danger ORS* ► After 4 hours, reassess the child. If NO DEHYDRATION, choose PLAN A. If the child still has
signs, ask about cough or difficulty breathing, diarrhea, fever and then ask for an ear SOME DEHYRATION, choose PLAN B again
problem.
PLAN C: To treat a child who has SEVERE DEHYDRATION
7. For ALL sick children ask the mother about the child’s problem, check for general danger Treat severe
signs, ask about cough or difficulty breathing, diarrhea, fever and ear problem. CHECK for dehydration ► Water and salts must be quickly replaced with intravenous fluids
malnutrition and anemia, immunization status and for other problems. quickly
*ORS: Oral Rehydration Solution
Adapted from World Health Organization, IMCI Model Handbook, WHO/FCH/CAH/00.12, Geneva, Switzerland
You might also like
- Set The Fury of EgyptDocument171 pagesSet The Fury of EgyptJango Fett97% (29)
- Management of The Sick Young Infant Age 1 Week Up To 2 MonthsDocument5 pagesManagement of The Sick Young Infant Age 1 Week Up To 2 Monthsapi-19824701No ratings yet
- Maternal and Child Lec Reviewer 1 8Document10 pagesMaternal and Child Lec Reviewer 1 8Keziah Marie Chua Santa-AnaNo ratings yet
- Summary of IMCI Case ManagementDocument2 pagesSummary of IMCI Case Managementjanesky09100% (1)
- EMCPIIDocument9 pagesEMCPIIChaouki Abdallah100% (2)
- Your Baby’s Bottle-feeding Aversion, Reasons and SolutionsFrom EverandYour Baby’s Bottle-feeding Aversion, Reasons and SolutionsRating: 4 out of 5 stars4/5 (23)
- IMCIDocument87 pagesIMCImark100% (3)
- IMCIDocument42 pagesIMCIMichael Anthony ErmitaNo ratings yet
- Assess and Classify The Sick Child Age 2 Months Up To 5 YearsDocument30 pagesAssess and Classify The Sick Child Age 2 Months Up To 5 YearsRommel G. Santiago100% (2)
- CHN FinalDocument41 pagesCHN FinalKeziah Marie Chua Santa-AnaNo ratings yet
- The Imci Strategy ReviewerDocument10 pagesThe Imci Strategy ReviewerDustin Dela CruzNo ratings yet
- Imci Summary Toprank by JadeDocument13 pagesImci Summary Toprank by JadeJade SorongonNo ratings yet
- Plcsim Advanced Docu v10 enDocument47 pagesPlcsim Advanced Docu v10 enRafaelNo ratings yet
- IMCI SL LecDocument143 pagesIMCI SL LecJmarie Brillantes PopiocoNo ratings yet
- Infant Colic, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandInfant Colic, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- IMCIDocument112 pagesIMCIJohann Dexter Malimban GloriosoNo ratings yet
- Raising a Child Living With Epilepsy and SeizuresFrom EverandRaising a Child Living With Epilepsy and SeizuresRating: 5 out of 5 stars5/5 (1)
- Integrated Management of Childhood IllnessesDocument65 pagesIntegrated Management of Childhood IllnessesJocel LañasNo ratings yet
- Integrated Management of Childhood Illness: Chart BookletDocument81 pagesIntegrated Management of Childhood Illness: Chart BookletReadcast EFNo ratings yet
- Care of The Child Applying Integrated Management of Childhood Illnesses (Imci)Document22 pagesCare of The Child Applying Integrated Management of Childhood Illnesses (Imci)Jesena SalveNo ratings yet
- IMCIDocument17 pagesIMCIapi-3707883No ratings yet
- 13 ImciDocument10 pages13 ImciJanely EstreraNo ratings yet
- Sick Young Infants (Referral, Treatment, Oral Drugs) : ImnciDocument46 pagesSick Young Infants (Referral, Treatment, Oral Drugs) : ImnciTanviNo ratings yet
- National Control of Dirrheal Diseases (CDD) Program ObjectivesDocument6 pagesNational Control of Dirrheal Diseases (CDD) Program ObjectivesJoy FucananNo ratings yet
- Assess and Classify DiarrheaDocument2 pagesAssess and Classify DiarrheaAurhea Lyn Mateo PrimeroNo ratings yet
- ImciDocument7 pagesImciFjane camotaNo ratings yet
- IMCI Management 2m-5yearsDocument35 pagesIMCI Management 2m-5yearsRachanaNo ratings yet
- Unit 2 Imnci BSCDocument67 pagesUnit 2 Imnci BSCNdina ElaoNo ratings yet
- GE in ChildrenDocument23 pagesGE in ChildrensamiNo ratings yet
- IMCI SumDocument6 pagesIMCI SumLazo JuleeNo ratings yet
- IMCI Management Less Than 2 MonthsDocument36 pagesIMCI Management Less Than 2 MonthsRachanaNo ratings yet
- Assessment of Diarrheoa FINAL (Autosaved)Document26 pagesAssessment of Diarrheoa FINAL (Autosaved)Mary MenuNo ratings yet
- 7 - Nursing Management of GIT Disorders 3 RD 1444Document34 pages7 - Nursing Management of GIT Disorders 3 RD 1444Faisal M.AlruwailiNo ratings yet
- 08 Diarrhoea 2Document8 pages08 Diarrhoea 2Chika JonesNo ratings yet
- ImciDocument2 pagesImciNiño CarmeLo MondasNo ratings yet
- Integrated Management ofDocument39 pagesIntegrated Management ofABEGAIL BALLORANNo ratings yet
- Osce Review - BSN Ii: SN RMPBDocument28 pagesOsce Review - BSN Ii: SN RMPBJoan VenidaNo ratings yet
- Ntegrated Anagement of Hildhood Llness: ( ( ( (Integrated Management Childhood IllnessDocument103 pagesNtegrated Anagement of Hildhood Llness: ( ( ( (Integrated Management Childhood IllnessAriel ZapantaNo ratings yet
- The Integrated Management of Childhood IllnessDocument83 pagesThe Integrated Management of Childhood Illnesssay04yaocincoNo ratings yet
- Group 3 - Week 8 (Nur192)Document29 pagesGroup 3 - Week 8 (Nur192)Cristine JanolinoNo ratings yet
- Integrated Management of Childhood Illnes1Document5 pagesIntegrated Management of Childhood Illnes1Ryan VocalanNo ratings yet
- Integrated Management of Chilhood IllnessesDocument12 pagesIntegrated Management of Chilhood Illnessescorpuzdarryl3No ratings yet
- This Document and The Information Thereon Is The Property of PHINMA Education (Department of Nursing)Document12 pagesThis Document and The Information Thereon Is The Property of PHINMA Education (Department of Nursing)Retiza EllaNo ratings yet
- Integrated Management of Childhood IllnessDocument52 pagesIntegrated Management of Childhood IllnessRitz CelsoNo ratings yet
- Imci Diarrhoea Homework#2Document9 pagesImci Diarrhoea Homework#2Cherub ChuaNo ratings yet
- Imci Booklet 69 70Document2 pagesImci Booklet 69 70Ivan MaximusNo ratings yet
- Integrated Management of Childhood IllnessesDocument7 pagesIntegrated Management of Childhood IllnessesMae Alexes TamañoNo ratings yet
- S3 - Under 2 MonthDocument45 pagesS3 - Under 2 MonthBelay GezahegnNo ratings yet
- Osce Review - BSN Ii: SN RMPBDocument35 pagesOsce Review - BSN Ii: SN RMPBJoan VenidaNo ratings yet
- Management of The Sick Young Infant Age 1 Week Up To 2 MonthsüüüDocument3 pagesManagement of The Sick Young Infant Age 1 Week Up To 2 MonthsüüüJonah MaasinNo ratings yet
- IMCIDocument7 pagesIMCImarlou agananNo ratings yet
- Daily Health ChecksDocument1 pageDaily Health Checksapi-451039239No ratings yet
- Dehydration in ChildrenDocument24 pagesDehydration in ChildrenDani AsmareNo ratings yet
- Case 3 Group3 BSN2B Actvity 3Document2 pagesCase 3 Group3 BSN2B Actvity 3Xena IngalNo ratings yet
- 8.2 Opportunistic Infections in Children Living With HIV-Part 1 Bacteria & Fungal OIsDocument43 pages8.2 Opportunistic Infections in Children Living With HIV-Part 1 Bacteria & Fungal OIsdawalgari srivanireddyNo ratings yet
- The Imci StrategyDocument7 pagesThe Imci StrategyJeanette OchonNo ratings yet
- Communicable DiseaseDocument15 pagesCommunicable DiseasereooooNo ratings yet
- Imci2007 Part 1Document33 pagesImci2007 Part 1api-3709260No ratings yet
- Vomiting in ChildrenDocument3 pagesVomiting in Childrenartz_dhanaNo ratings yet
- IMCIDocument17 pagesIMCIErnest Jerome MalamionNo ratings yet
- Management of The Sick Child Aged 2 Months Up To 5 Years: Severe DehydrationDocument2 pagesManagement of The Sick Child Aged 2 Months Up To 5 Years: Severe DehydrationMonique LeonardoNo ratings yet
- Integrated Management of Childhood IllnessDocument43 pagesIntegrated Management of Childhood IllnessMark LugtuNo ratings yet
- Exercise E F QDocument10 pagesExercise E F QCarol EleserioNo ratings yet
- WEEK 13 RLE IMCI ClassDocument73 pagesWEEK 13 RLE IMCI ClassCristina Bantilan MontenegroNo ratings yet
- CHN Rle Pointers and Review NotesDocument6 pagesCHN Rle Pointers and Review NotesKeziah Marie Chua Santa-AnaNo ratings yet
- Nur 146 RleDocument47 pagesNur 146 RleKeziah Marie Chua Santa-AnaNo ratings yet
- Safety Work Permit: Purok Lansong, Barangay Tambler, General Santos City Tel. No.: (083) 552-1831Document1 pageSafety Work Permit: Purok Lansong, Barangay Tambler, General Santos City Tel. No.: (083) 552-1831glenn umaliNo ratings yet
- Cambridge Price ListDocument13 pagesCambridge Price ListManuthi HewawasamNo ratings yet
- Gas Processors Suppliers Association GPSA Eng (Bookos - Org) - 701-821!1!60!1!20Document20 pagesGas Processors Suppliers Association GPSA Eng (Bookos - Org) - 701-821!1!60!1!20Karen Vl100% (1)
- CG - Mini Project - ReportDocument37 pagesCG - Mini Project - ReportMeghana100% (1)
- SSC JE 2023 Electrical EngineeringDocument65 pagesSSC JE 2023 Electrical Engineeringgamers die hardersNo ratings yet
- Pubblicita Residential Ventilation VMC 120123Document116 pagesPubblicita Residential Ventilation VMC 120123PaulKajzerNo ratings yet
- Research ProposalDocument8 pagesResearch Proposalpearson cosmasNo ratings yet
- Proficy HMI/SCADA - iFIX: River ErverDocument46 pagesProficy HMI/SCADA - iFIX: River Erverchris75726No ratings yet
- Organic Chemistry Lab Manual, Chem221 - Fall2012 - LabManualDocument111 pagesOrganic Chemistry Lab Manual, Chem221 - Fall2012 - LabManualdanthetoasterNo ratings yet
- Afbeeldingen: Full Galar Map With DLCDocument1 pageAfbeeldingen: Full Galar Map With DLCGarron PardoNo ratings yet
- C++ Question BankDocument19 pagesC++ Question BankChethanNo ratings yet
- 2.4.1 - Training-Exam-ManualDocument35 pages2.4.1 - Training-Exam-ManualJohn Rey NavioNo ratings yet
- Lbce Process Standards:: Link-BeltDocument4 pagesLbce Process Standards:: Link-BeltErissonNo ratings yet
- Cookery Kitchen Tools and EquipmentDocument25 pagesCookery Kitchen Tools and EquipmentNORIE MATEMATICO MERCADONo ratings yet
- Plant Disease Identification: A Comparative Study: Shriroop C. Madiwalar Medha V. WyawahareDocument6 pagesPlant Disease Identification: A Comparative Study: Shriroop C. Madiwalar Medha V. WyawahareKishore JNo ratings yet
- Modelling: - A Model Is A Simplified Representation ofDocument23 pagesModelling: - A Model Is A Simplified Representation ofCH126 Dhruv SonaniNo ratings yet
- Consumer Relations Case-9Document29 pagesConsumer Relations Case-9Ameera MazlanNo ratings yet
- M.e.estDocument2 pagesM.e.estShiyamala JeyakumarNo ratings yet
- 2 Z Hongyu, Laser-Induced Colours On Metal SurfacesDocument8 pages2 Z Hongyu, Laser-Induced Colours On Metal SurfacesAurgenblickNo ratings yet
- Remembering The Kana - Part 1+ 2 - Hiragana + KatakanaDocument153 pagesRemembering The Kana - Part 1+ 2 - Hiragana + KatakanaNaunetkiya88% (8)
- Tiar Pramono PDFDocument9 pagesTiar Pramono PDFTiar PramonoNo ratings yet
- Research TVL12Document3 pagesResearch TVL12Chris - Ann Mae De LeonNo ratings yet
- Design and Fabrication of Amphibious Bicycle: June 2015Document36 pagesDesign and Fabrication of Amphibious Bicycle: June 2015Amanuel GetachewNo ratings yet
- EMA Process ValidationDocument15 pagesEMA Process Validationdr3azzamNo ratings yet
- Gauss Law Lab ExampleDocument6 pagesGauss Law Lab ExampleAnthony MajinianNo ratings yet
- DElta HMI PDFDocument4 pagesDElta HMI PDFNader_Al_QahfNo ratings yet
- Ja Biztown Journal: Biztee Lab WorksDocument5 pagesJa Biztown Journal: Biztee Lab Worksapi-439426007No ratings yet